Should you feed a baby after they vomit
How to Know Whether You Should
Your baby just threw up all the milk they’ve chugged down so far, and you’re wondering if it’s OK to continue feeding. How soon should you feed your baby after vomiting?
It’s a good question — just about every parent has likely pondered this. Spit-up is almost a rite of passage for babies (and parents). Baby vomiting is also common and can happen for many reasons. Most of the causes aren’t serious.
The short answer — because you may have a very fussy baby on your hands and want to get back to them ASAP — is yes, you can usually feed your baby after they vomit all over your favorite sweater, sofa throw, and rug.
Here’s just about everything you need to know about feeding your baby after vomiting.
Baby vomit and spit-up are two different things — and they can have different causes. Spitting up is common in babies under the age of 1 year. It typically happens after feeding. Spit-up is usually an easy flow of milk and saliva that dribbles from your baby’s mouth. It often happens with a burp.
Spit-up is normal in healthy babies. It can happen for several reasons. About half of all babies 3 months and under have a type of acid reflux called infant reflux.
Spit-up from infant reflux is especially bound to happen if your baby has a full stomach. Being careful not to overfeed a bottle-fed infant can help. Spitting up typically stops by the time your baby is a year old.
On the other hand, vomiting is typically a more forceful throwing-up of milk (or food, if your baby is old enough to eat solids). It happens when the brain signals the muscles around the stomach to squeeze.
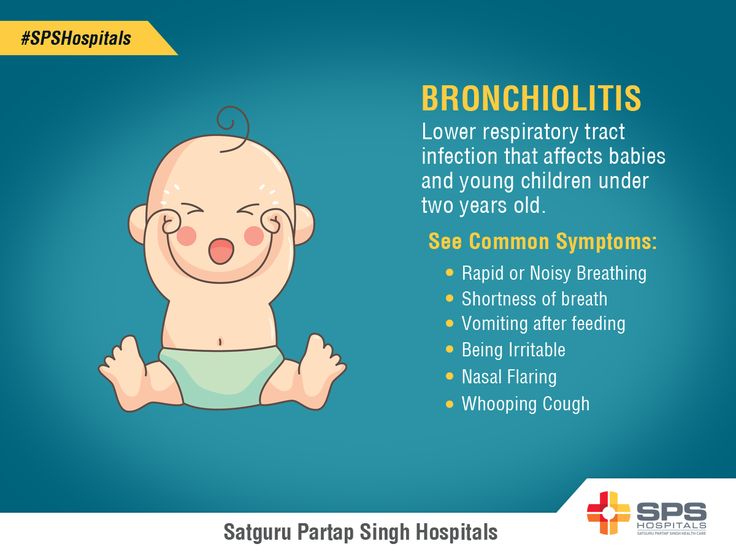
Vomiting (like gagging) is a reflex action that can be triggered by a number of things. These include:
- irritation from a viral or bacterial infection, like the stomach bug
- fever
- pain, such as from a fever, earache, or vaccination
- blockage in the stomach or intestines
- chemicals in the blood, like medicine
- allergens, including pollen; very uncommon in babies under 1 year
- motion sickness, such as during a car ride
- dizziness, which might happen after being twirled around too much
- being upset or stressed
- strong smells
- milk intolerance
Vomiting is also common in healthy babies, but it might mean that your baby has caught a bug or is feeling a bit under the weather.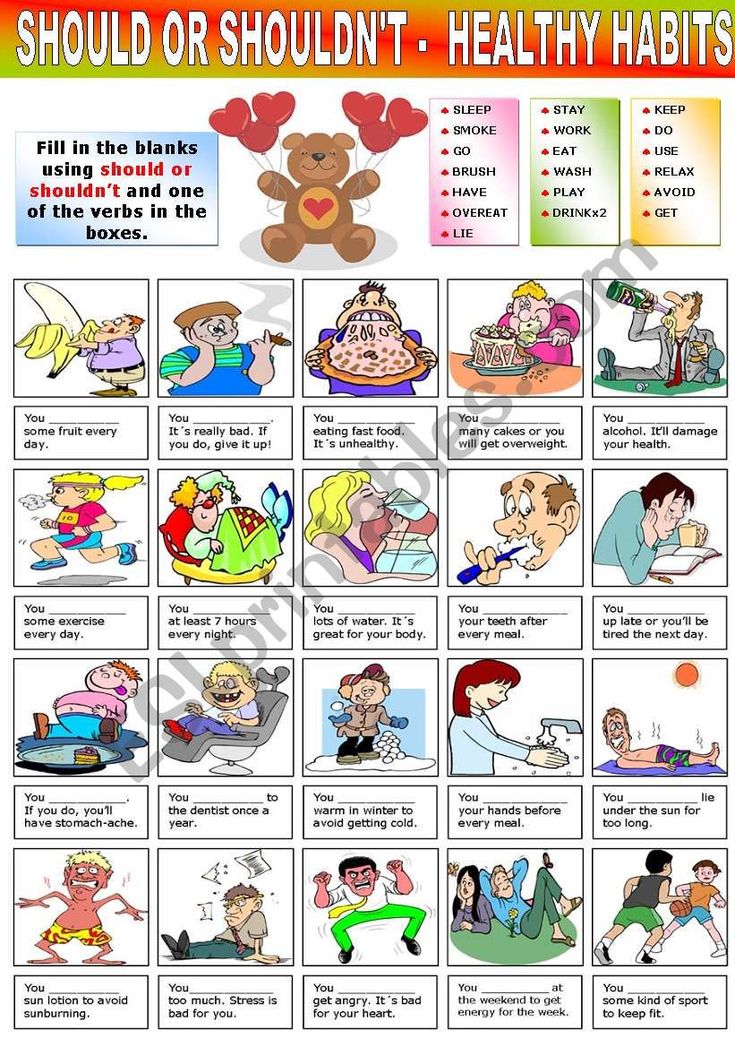
Too much vomiting can cause dehydration and even weight loss in very serious cases. Milk feeding can help prevent both of these. Offer your baby a feeding after they’ve stopped throwing up. If your baby is hungry and takes to the bottle or breast after vomiting, go right ahead and feed them.
Liquid feeding after vomiting can sometimes even help settle your baby’s nausea. Start with small amounts of milk and wait to see if they vomit again. Your baby might vomit the milk right back up, but it’s better to try than not.
If your little one is at least 6 months old and doesn’t want to feed after throwing up several times, offer them water in a bottle or a spoon. This can help prevent dehydration. Wait a short while and try feeding your baby again.
In some cases, it’s better not to feed a baby right after vomiting. If your baby is throwing up because of an earache or fever, they may benefit from medication first.
Most pediatricians recommend pain medications like infant Tylenol for babies in their first year. Ask your doctor about the best medication and dosage for your baby.
Ask your doctor about the best medication and dosage for your baby.
If giving pain medication based on your doctor’s advice, wait about 30 to 60 minutes after doing so to feed your little one. Feeding them too soon might cause another bout of vomiting before the meds can work.
Motion sickness isn’t common in babies under the age of 2 years, but some babies may be more sensitive to it. If your baby vomits from motion sickness, it’s better not to offer a feeding afterward.
You’re in luck if your baby likes to nod off in the car. Wait until you’re out of the car to feed your baby milk.
Baby vomiting can be worrying, but it usually goes away by itself — even if your baby has the stomach bug. Most babies with gastroenteritis don’t need medical treatment. This means that most of the time, you’ll have to bravely wait out your baby’s vomiting.
But sometimes, throwing up is a sign that something’s not right. You know your baby best. Trust your gut and call their doctor if you feel your little one is unwell.
In addition, take your baby to a doctor immediately if they’ve been vomiting for 12 hours or longer. Babies and children can dehydrate quickly from too much vomiting.
Also call your baby’s pediatrician if your baby can’t hold anything down and has signs and symptoms of being unwell. These include:
- constant crying
- pain or discomfort
- refusal to feed or drink water
- diaper that hasn’t been wet for 6 hours or longer
- diarrhea
- dry lips and mouth
- crying without tears
- extra sleepiness
- floppiness
- vomiting blood or fluid with black flecks (“coffee grounds”)
- lack of smile or response
- vomiting green fluid
- bloated tummy
- blood in bowel movements
You won’t usually have any control over when or how much your baby vomits. When it happens on occasion, repeat this mantra to help you cope: “Healthy babies sometimes vomit.”
However, if your baby often vomits (or spits up) after feeding, you may be able to take some preventative steps. Try these tips:
Try these tips:
- avoid overfeeding
- give your baby smaller, more frequent feeds
- burp your baby often between feeds and after feeds
- prop up your baby so they’re upright for at least 30 minutes after feeding (but don’t prop your baby up for sleep or use anything to position them in their crib or elevate their mattress)
If your baby has a tummy bug and is old enough to eat solid foods, avoid feeding solids for about 24 hours. A liquid diet can help the stomach settle after a bout of vomiting.
Vomiting and spit-up are common in healthy babies. In most cases, you can milk feed shortly after your baby vomits. This helps to prevent your baby from getting dehydrated.
In some cases it’s best to wait a little while before trying to feed your baby again. If you’re giving your child medication like pain and fever relievers, wait a bit so the meds don’t come back up.
If your baby is vomiting a lot or seems otherwise unwell, call your pediatrician immediately. If you’re unsure if your baby’s vomiting or spit-up is cause for concern, it’s always best to check with your doctor.
If you’re unsure if your baby’s vomiting or spit-up is cause for concern, it’s always best to check with your doctor.
Vomiting (0-12 Months)
Is this your child's symptom?
- Vomiting (throwing up) stomach contents
- Other names for vomiting are puking, barfing and heaving
Causes of Vomiting
- Viral Gastritis. Stomach infection from a stomach virus is the most common cause. Also called stomach flu. A common cause is the Rotavirus. The illness starts with vomiting. Watery loose stools may follow within 12-24 hours.
- Food Allergy. Vomiting can be the only symptom of a food reaction. The vomiting comes on quickly after eating the food. Uncommon in infants, but main foods are eggs and peanut butter.
- Coughing. Hard coughing can also cause your child to throw up. This is more common in children with reflux.
- Serious Causes. Vomiting alone should stop within about 24 hours.
 If it lasts over 24 hours, you must think about more serious causes. An example is a kidney infection. A serious cause in young babies is pyloric stenosis. See below for more on this.
If it lasts over 24 hours, you must think about more serious causes. An example is a kidney infection. A serious cause in young babies is pyloric stenosis. See below for more on this.
Pyloric Stenosis (Serious Cause)
- The most common cause of true vomiting in young babies.
- Onset of vomiting is age 2 weeks to 2 months
- Vomiting is forceful. It becomes projectile and shoots out.
- Right after vomiting, the baby is hungry and wants to feed. ("hungry vomiter")
- Cause: The pylorus is the channel between the stomach and the gut. In these babies, it becomes narrow and tight.
- Risk: Weight loss or dehydration
- Treatment: Cured by surgery.
Vomiting Scale
- Mild: 1 - 2 times/day
- Moderate: 3 - 7 times/day
- Severe: Vomits everything, nearly everything or 8 or more times/day
- Severity relates even more to how long the vomiting goes on for.
 At the start of the illness, it's common for a child to vomit everything. This can last for 3 or 4 hours. Children then often become stable and change to mild vomiting.
At the start of the illness, it's common for a child to vomit everything. This can last for 3 or 4 hours. Children then often become stable and change to mild vomiting. - The main risk of vomiting is dehydration. Dehydration means the body has lost too much fluid.
- The younger the child, the greater the risk for dehydration.
Dehydration: How to Tell
- The main risk of vomiting is dehydration. Dehydration means the body has lost too much water.
- Vomiting with watery diarrhea is the most common cause of dehydration.
- Dehydration is a reason to see a doctor right away.
- Your child may have dehydration if not drinking much fluid and:
- The urine is dark yellow and has not passed any in over 8 hours.
- Inside of the mouth and tongue are very dry.
- No tears if your child cries.
- Slow blood refill test: Longer than 2 seconds. First, press on the thumbnail and make it pale. Then let go. Count the seconds it takes for the nail to turn pink again.
 Ask your doctor to teach you how to do this test.
Ask your doctor to teach you how to do this test.
When to Call for Vomiting (0-12 Months)
Call 911 Now
- Can't wake up
- Not moving
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Dehydration suspected. No urine in over 8 hours, dark urine, very dry mouth and no tears.
- Stomach pain when not vomiting. Exception: stomach pain or crying just before vomiting is quite common.
- Age less than 12 weeks old with vomiting 2 or more times. Exception: normal spitting up.
- Vomited 3 or more times and also has diarrhea
- Severe vomiting (vomits everything) more than 8 hours while getting Pedialyte (or breastmilk)
- Head injury within the last 24 hours
- Weak immune system. Examples are sickle cell disease, HIV, cancer, organ transplant, taking oral steroids.
- Vomiting a prescription medicine
- Fever over 104° F (40° C)
- Fever in baby less than 12 weeks old.
 Caution: Do NOT give your baby any fever medicine before being seen.
Caution: Do NOT give your baby any fever medicine before being seen. - Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Contact Doctor Within 24 Hours
- All other infants (age less than 1 year) with vomiting. See Care Advice while waiting to discuss with doctor.
Seattle Children's Urgent Care Locations
If your child’s illness or injury is life-threatening, call 911.
- Bellevue
- Everett
- Federal Way
- Seattle
Care Advice for Vomiting
- What You Should Know About Vomiting:
- Most vomiting is caused by a viral infection of the stomach.

- Vomiting is the body's way of protecting the lower gut.
- The good news is that stomach illnesses last only a short time.
- The main risk of vomiting is dehydration. Dehydration means the body has lost too much fluid.
- Here is some care advice that should help.
- Most vomiting is caused by a viral infection of the stomach.
- Formula Fed Babies - May Give Oral Rehydration Solution (ORS) for 8 Hours:
- If vomits once, give half the regular amount of formula every 1 to 2 hours.
- If vomits formula more than once, offer ORS for 8 hours. If you don't have ORS, use formula until you can get some.
- ORS is a special fluid that can help your child stay hydrated. You can use Pedialyte or the store brand of ORS. It can be bought in food stores or drug stores.
- Spoon or syringe feed small amounts. Give 1-2 teaspoons (5-10 mL) every 5 minutes.
- After 4 hours without throwing up, double the amount.
- Return to Formula. After 8 hours without throwing up, go back to regular formula.

- Breastfed Babies - Reduce the Amount Per Feeding:
- If vomits once, nurse half the regular time every 1 to 2 hours.
- If vomits more than once, nurse for 5 minutes every 30 to 60 minutes. After 4 hours without throwing up, return to regular nursing.
- If continues to vomit, switch to pumped breastmilk. (ORS is rarely needed in breastfed babies. It can be used if vomiting becomes worse).
- Spoon or syringe feed small amounts of pumped milk. Give 1-2 teaspoons (5-10 mL) every 5 minutes.
- After 4 hours without throwing up, return to regular feeding at the breast. Start with small feedings of 5 minutes every 30 minutes. As your baby keeps down the smaller amounts, slowly give more.
- Pumped Breastmilk Bottle-Fed Infants - Reduce the Amount per Feeding:
- If vomits once and bottle-feeding breastmilk, give half the regular amount every 1-2 hours.
- If vomits more than once within last 2 hours, give 1 ounce (30 mL) every 30 to 60 minutes.
- If continues to vomit, give 1-2 teaspoons (5-10 mL) every 5 minutes. Only if not tolerating breastmilk, switch to ORS (e.g., Pedialyte) for every 5 minutes for a few hours.
- After 4 hours without vomiting, return to regular feedings. Start with 1 ounce (30 mL) every 30 minutes and slowly increase as tolerated.
- Stop All Solid Foods:
- Avoid all solid foods and baby foods in kids who are vomiting.
- After 8 hours without throwing up, gradually add them back.
- If on solid foods, start with starchy foods that are easy to digest. Examples are cereals, crackers and bread.
- Do Not Give Medicines:
- Stop using any drug that is over-the-counter for 8 hours. Reason: Some of these can make vomiting worse.
- Fever. Mild fevers don't need to be treated with any drugs. For higher fevers, you can use an acetaminophen suppository (such as FeverAll). This is a form of the drug you put in the rectum (bottom).
 Ask a pharmacist for help finding this product. Do not use ibuprofen. It can upset the stomach.
Ask a pharmacist for help finding this product. Do not use ibuprofen. It can upset the stomach. - Call your doctor if: Your child vomits a drug ordered by your doctor.
- Try to Sleep:
- Help your child go to sleep for a few hours.
- Reason: Sleep often empties the stomach and removes the need to vomit.
- Your child doesn't have to drink anything if his stomach feels upset and he doesn't have any diarrhea.
- Return to Child Care:
- Your child can return to child care after the vomiting and fever are gone.
- What to Expect:
- For the first 3 or 4 hours, your child may vomit everything. Then the stomach settles down.
- Vomiting from a viral illness often stops in 12 to 24 hours.
- Mild vomiting and nausea may last up to 3 days.
- Call Your Doctor If:
- Vomits clear fluids for more than 8 hours
- Vomiting lasts more than 24 hours
- Blood or bile (green color) in the vomit
- Stomach ache present when not vomiting
- Dehydration suspected (no urine in over 8 hours, dark urine, very dry mouth, and no tears)
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.

Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Last Reviewed: 01/31/2023
Last Revised: 12/30/2022
Copyright 2000-2023 Schmitt Pediatric Guidelines LLC.
Rotavirus in a child
Rotavirus in children: symptoms, treatment, prevention.
Rotavirus infection is an acute infectious disease with fecal-oral transmission, characterized by lesions of the gastrointestinal tract by the type of gastroenteritis with the development of dehydration (dehydration) syndrome.
Rotavirus is the leading cause of gastroenteritis in children under 5 years of age. .In Russia, it is most often recorded in the winter-spring period. nine0005
Causes of infection:
The causative agent is rotavirus, belongs to the family
RNA viruses. Types 1-4, 8 and 9 of the virus are considered infectious for humans.
The source of infection is a person (a patient or a virus shedder). The number of asymptomatic carriers of the virus among children can reach 5-7%. The virus is able to remain viable in the external environment for several months, is stable at low temperatures, and quickly dies when heated. nine0005
In general, in the Russian Federation, the proportion of sick children under 1 year of age is 20.6%, at the age of 1–2 years - 44.7%. By the age of 2, almost every child has at least 1 rotavirus infection and more than 2/3 fall ill again. Given the high contagiousness (infectiousness), it is a common cause of outbreaks in organized groups (kindergarten, school) and hospitals.
Mechanism of transmission of rotavirus - fecal-oral: realized by food, water and household contact. Given the extremely high contagiousness of rotavirus and the resistance of the pathogen to household chemicals, even very strict hygiene measures (including washing hands after each contact with the patient) can often be ineffective.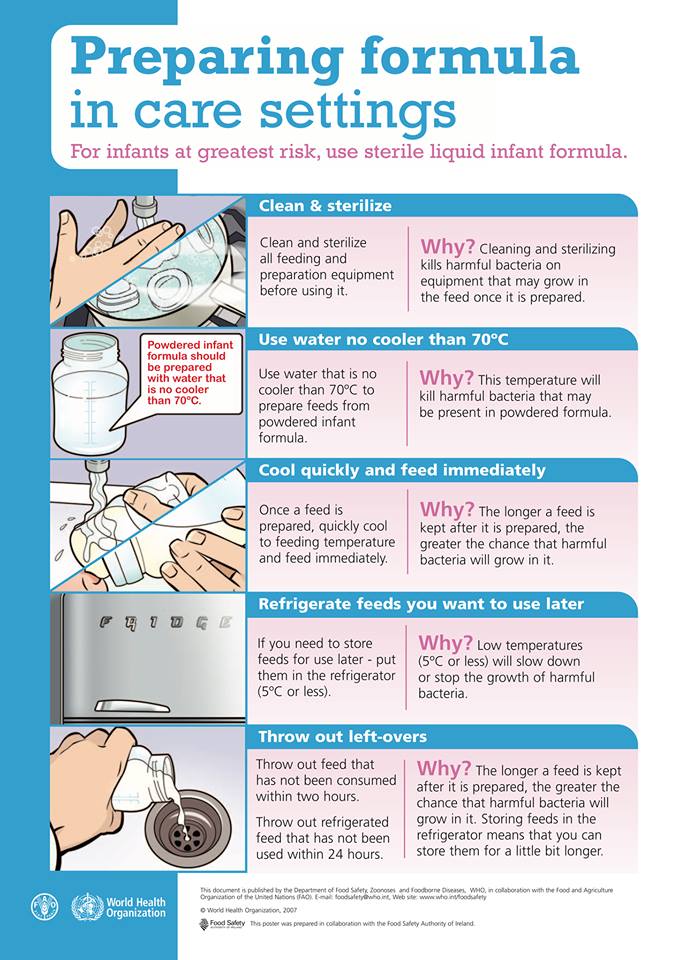 The incubation period is only a few days - on average from 1 to 3 days. nine0005
The incubation period is only a few days - on average from 1 to 3 days. nine0005
Clinical picture
The main symptoms of rotavirus gastroenteritis are general intoxication (fever, lethargy, vomiting, headache) and changes in the gastrointestinal tract: abdominal pain, frequent loose watery stools. Rotavirus gastroenteritis is characterized by two variants of the onset of the disease: acute (about 90% of patients), when all the main symptoms appear on the 1st day of the disease, and subacute, when 1-2 symptoms (usually abdominal pain and intoxication) for 2-3 days diseases are joined by diarrhea, vomiting, fever. nine0005
General infectious syndrome. Most cases of rotavirus infection begin acutely with a rise in temperature to febrile numbers (38.0 degrees) or even hyperthermia, but the duration of fever, despite its severity, rarely exceeds 2-4 days. Fever is accompanied by symptoms of intoxication: weakness, lethargy, loss of appetite up to the development of anorexia and adynamia in severe forms of the disease. In older children with mild forms, the disease can occur against the background of subfebrile temperature with moderate symptoms of intoxication or their absence. nine0035
In older children with mild forms, the disease can occur against the background of subfebrile temperature with moderate symptoms of intoxication or their absence. nine0035
Syndrome of local changes (gastritis, gastroenteritis and/or enteritis). One of the first, and often the leading manifestation of rotavirus infection, is vomiting. It can occur simultaneously with diarrhea or precede it, be repeated or repeated in nature for 1-2 days. The gastrointestinal tract is affected by the type of gastroenteritis or (less often) enteritis. Diarrheal syndrome in rotavirus infection is one of the most important and persistent manifestations, in some cases determining the clinical picture of the disease. The chair is plentiful, watery, frothy, yellow in color, without visible pathological impurities, or with a small amount of clear mucus, sometimes there is a characteristic sour smell of stools. The frequency of stools on average does not exceed 4-5 times a day, but in young children it can reach 15-20 times. The duration of diarrhea on average ranges from 3 to 7 days, but it can persist for a longer time (up to 10-14 days, more often in young children). Rotavirus infection is characterized by a combination of diarrhea with flatulence, which is most pronounced in children of the first year of life. Painful abdominal syndrome with rotavirus infection appears at the onset of the disease. Abdominal pains of varying severity may be diffuse or localized in the upper abdomen, and there may also be episodes of cramping pains. nine0005
The duration of diarrhea on average ranges from 3 to 7 days, but it can persist for a longer time (up to 10-14 days, more often in young children). Rotavirus infection is characterized by a combination of diarrhea with flatulence, which is most pronounced in children of the first year of life. Painful abdominal syndrome with rotavirus infection appears at the onset of the disease. Abdominal pains of varying severity may be diffuse or localized in the upper abdomen, and there may also be episodes of cramping pains. nine0005
Dehydration syndrome. The severity of the course of rotavirus gastroenteritis is determined by the amount of pathological fluid loss with vomiting and diarrhea and the development of exsicosis (dehydration) I-II, less often II-III degree. The degree of exicosis in patients depends not only on the severity of pathological losses of fluid and electrolytes, but also on the adequacy of the ongoing rehydration therapy (adequate fluid replacement). The following signs signal the development of dehydration: constant thirst, sunken eyes and a large fontanel, dry skin, sclera and mucous membranes. The skin becomes earthy-gray, the lips become bright and dry, the skin turgor decreases, and the amount of urine decreases. The most dangerous condition is the stage of dehydration, in which thirst is replaced by a complete refusal to drink and there is a pronounced decrease in urination up to its complete absence. nine0005
The following signs signal the development of dehydration: constant thirst, sunken eyes and a large fontanel, dry skin, sclera and mucous membranes. The skin becomes earthy-gray, the lips become bright and dry, the skin turgor decreases, and the amount of urine decreases. The most dangerous condition is the stage of dehydration, in which thirst is replaced by a complete refusal to drink and there is a pronounced decrease in urination up to its complete absence. nine0005
Syndrome of catarrhal changes. In 60-70% of patients with rotavirus infection, upper respiratory catarrh occurs, which may precede bowel dysfunction. It is characterized by moderate hyperemia and graininess of the posterior pharyngeal wall, soft palate and palatine arches, nasal congestion, coughing. However, the presence of catarrhal phenomena in some cases may be due to a concomitant respiratory viral infection, especially during the period of a seasonal increase in the incidence. nine0005
Extraintestinal complications:
- dehydration
- secondary infection
- possible development of seizures
- improper water regimen RVGE can cause cerebral edema, DIC, acute renal failure and other life-threatening conditions
nine0005
The most disturbing signs! (Need to call SMP )
- severe weakness and lethargy, almost constant sleep, or vice versa, incessant anxiety
- incessant vomiting
- the inability to drink the child
- no urination or very rare concentrated urine
- in children under one year old - retraction of the fontanel nine0005
- blood in the stool
Disease prognosis:
The prognosis of the disease with adequate hydration is usually favorable, the duration of the disease rarely exceeds 5-7 days. After a history of rotavirus gastroenteritis, a child may become re-infected due to seasonal changes in circulating rotavirus serotypes, but a history of natural infection may reduce the severity of subsequent infections. nine0005
After a history of rotavirus gastroenteritis, a child may become re-infected due to seasonal changes in circulating rotavirus serotypes, but a history of natural infection may reduce the severity of subsequent infections. nine0005
Diagnosis:
ELISA feces and OKI test (also includes PCR testing for other types of viruses that cause acute intestinal infections, salmonellosis and dysentery)
First aid:
- Abundant fractional drink. For this, it is preferable to use specialized saline solutions - Regidron, Regidron - Bio. In the first hours, in order not to provoke vomiting, you can give 1 tsp. or st.l. every 5 - 10 minutes. nine0005
IMPORTANT TO REMEMBER! For a day, depending on age, the child should drink at least 1 - 1.5 liters of water. Therefore, especially in the first knocks of the child, you SHOULD continue to drink in a dream, controlling that the child does not choke.
- Place a small child on its side so that in the event of an attack of vomiting, it does not choke on vomit.
- Antipyretics - only if the temperature is above 38.5.
- the first 3 hours after vomiting do not feed, then in small portions. nine0005
Breastfeeding must continue!
- In the acute period, for the accelerated normalization of stool and removal of the virus from the body, astringent and adsorbing substances are used (carbolene, polyphepan, smecta, enterosgel, etc.)
Diet:
In the treatment of intestinal infections that provoke the development of fermentopathy, special attention is paid to the diet. Since during the development of the pathological process, the activity of a number of digestive enzymes, in particular lactase, is disrupted, in the acute period of the disease, whole milk and dairy products should be excluded from the child's diet and the intake of foods rich in carbohydrates (sweet fruits, fruit juices, pastries, legumes) should be limited. culture). Also, in the acute period of the disease, it is not allowed to feed children with meat, broths, meat products, fatty and fried foods. Food is given to a sick child often, in small portions. The list of allowed products includes mucous porridges, vegetable purees and soups, white crackers and baked apples. nine0005
Food is given to a sick child often, in small portions. The list of allowed products includes mucous porridges, vegetable purees and soups, white crackers and baked apples. nine0005
Breastfeeding in the presence of an intestinal infection is not stopped, since breast milk contains antibodies that neutralize rotavirus and immunoglobulins that facilitate the course of the disease.
Common errors:
- Giving antibiotics. In this case, the culprit is a virus and any antibiotic is completely powerless against it. It will not bring any benefit, only increase the likelihood of complications. nine0005
- with profuse diarrhea, the use of any antidiarrheal drugs such as loperamide (without consulting a doctor). Their intake can increase intoxication, lengthen the recovery period.
Prophylaxis:
There is specific prevention against rotavirus - vaccination
Vaccination (Rotatec). The course consists of three doses with an interval of administration from 4 to 10 weeks. The first administration of the vaccine at the age of 6 to 12 weeks. Last injection before 32 weeks of age. (Compatible with any vaccines from the national calendar except BCG) nine0005
The course consists of three doses with an interval of administration from 4 to 10 weeks. The first administration of the vaccine at the age of 6 to 12 weeks. Last injection before 32 weeks of age. (Compatible with any vaccines from the national calendar except BCG) nine0005
Also:
Patients with mild forms of rotavirus infection t are isolated at home for 7 days, after which the sick person can be admitted to an organized team (including children) on the basis of a doctor's certificate of recovery without additional virological examination.
• Use only boiled water for drinking; nine0005
• Thorough washing of hands before eating;
• Pre-washing fruits and vegetables with a brush;
• Sufficient heat treatment of food.
Services
PediatricianPediatric infectious disease specialistPediatric gastroenterologistWhat to feed a child with vomiting: principles of sparing nutrition
During and after a child's vomiting, parents should review the diet.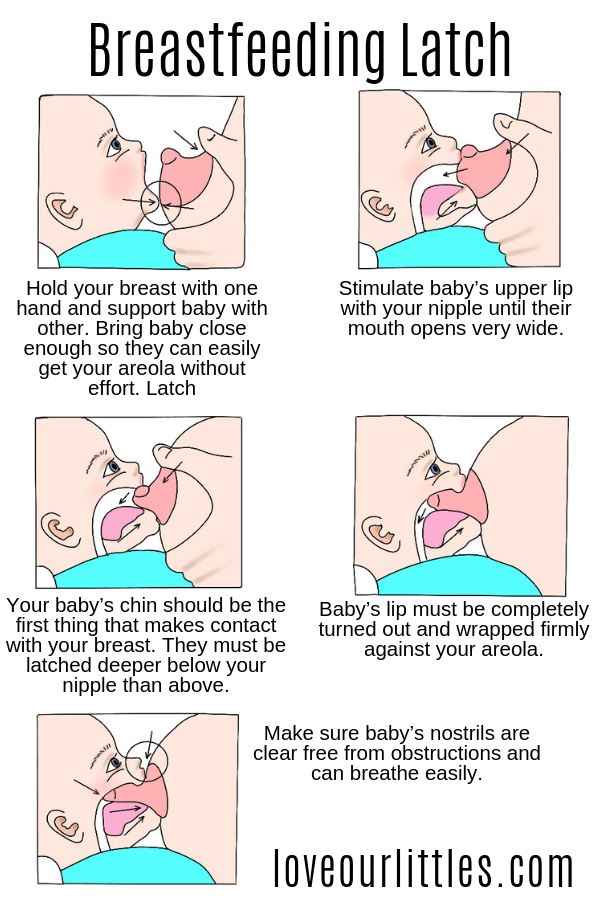 This condition disrupts the electrolyte balance, microflora, and causes dehydration. The body does not take food well - the rich taste and smell of the dish can provoke nausea, in addition, appetite often decreases. What to feed the baby? nine0005
This condition disrupts the electrolyte balance, microflora, and causes dehydration. The body does not take food well - the rich taste and smell of the dish can provoke nausea, in addition, appetite often decreases. What to feed the baby? nine0005
Contents [ show ]
- Why children vomit
- What to do after vomiting and what to feed the child?
- Sample daily menu for a child over one year old
- What foods not to eat when vomiting
- Tips for parents when a baby vomits
- Drinking regimen for vomiting
Why children vomit
The following problems can provoke vomiting:
disease;
Vomiting accompanies diseases more serious than ordinary food poisoning: appendicitis, helminthiasis, kidney failure, intestinal obstruction. But in this case it is combined with other characteristic symptoms. nine0005
In addition, vomiting is a natural human reaction to feeding against will. Don't be surprised if you run into her when you try to feed your baby when he doesn't want to. This is not a whim of a child. So his body reacts to the excess portion size. Another situation in which vomiting can begin is exposure to a new, most often exotic food with an unusual smell, taste or texture.
What to do after vomiting and how to feed the child?
In case of poisoning, the digestive organs begin to suffer. The mucous membranes become inflamed, nausea and diarrhea occur. The body loses a huge amount of water, dehydration occurs, which can lead to serious consequences. nine0005
First of all, you need to compensate for the lack of liquid - give weak, slightly sweet black tea, you can also green, dried fruit compotes, pharmacy (for example, Regidron) or a salt solution prepared by yourself.
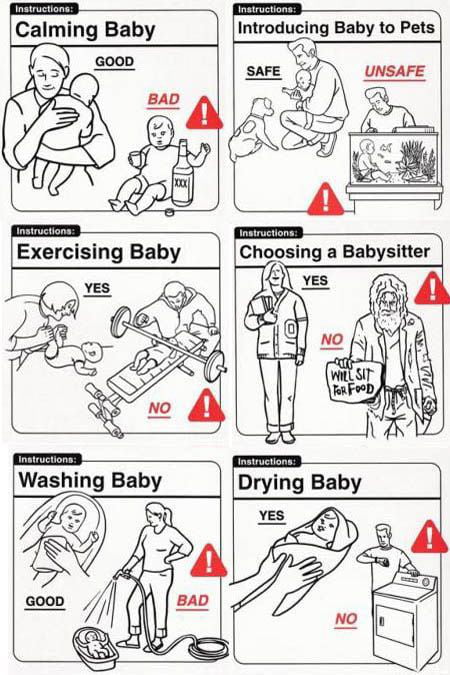
For newborns, follow the following feeding schedule :
- When breastfeeding: before the condition returns to normal, do not breastfeed the baby for at least 3-6 hours - this may provoke a new attack of vomiting. Drinking is allowed. When the vomiting has passed, you can return to the usual feeding pattern. nine0214
- When formula-feeding: with the approval of a pediatrician, stop feeding, give the newborn only water. When the condition normalizes, start offering the mixture at first in small portions, gradually returning to the usual ones.
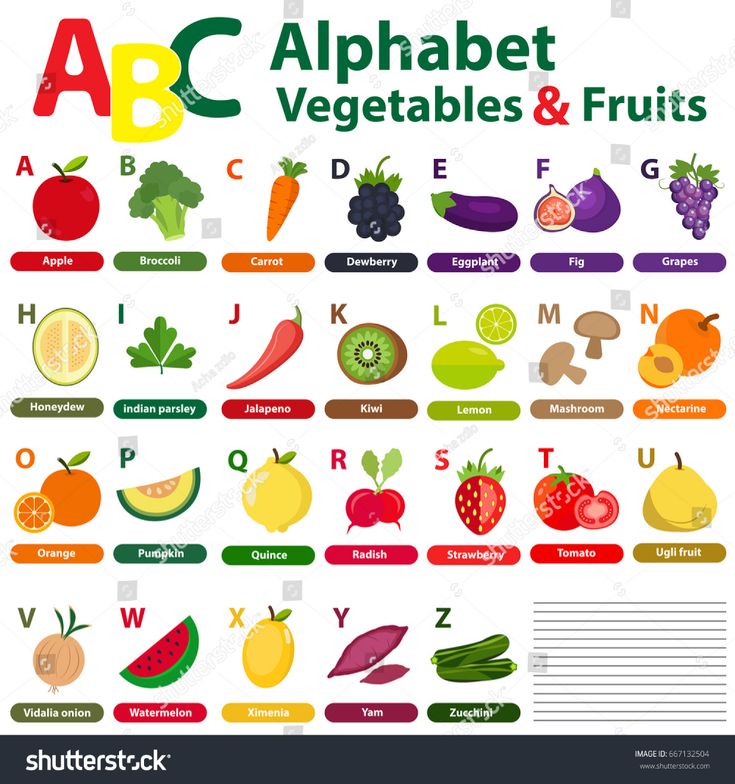
If complementary foods have already been introduced, on the first day after vomiting, offer:
- first courses: chicken broth, rice soup, soups with broccoli or homemade noodles;
- biscuits;
- boiled round rice porridge (mucilaginous). nine0214
A day after the baby has been poisoned, second courses can also be included in the diet. Buckwheat or rice porridge will do. Cook them with water, formula, breast or cow's milk diluted with water.
Cook them with water, formula, breast or cow's milk diluted with water.
Gradually, as with the introduction of complementary foods, return to the menu the dishes familiar to the child in accordance with his age - meat soufflé, vegetable / fruit puree, fish, cottage cheese, eggs.
Older children (from 8-12 months) can include in the diet not very fatty fish, lean broth with chicken, boiled rice, and a baked apple will not harm. Introduce fruits later - they contain acids that can irritate the stomach lining already damaged by vomiting. Bananas, pears and apples are suitable, preferably boiled or baked, wait a while with sour berries and fruits. nine0005
Sample daily menu for a child older than one year old
If the child has already become familiar with the main complementary foods and almost switched to a common table, after vomiting, you can make the following menu for the day:
| Meals | Breakfast | 1. 1 boiled egg 2.  Oatmeal, buckwheat or rice porridge Oatmeal, buckwheat or rice porridge 3. Sweet tea with cookies | |
|---|---|---|---|
| Snack Lunch | 1. Chicken stock 2. Cooks prepared from white bread | ||
| 9030 | 1. BURNEN YOURSEN YEARS | 9030||

 nine0214
nine0214