Sns baby feeding
Nursing Supplementers - La Leche League GB
If your baby needs a supplement of expressed breastmilk or formula, a nursing supplementer can help you enjoy the closeness of breastfeeding while your milk production increases.
You can use a supplementer to:
- Stimulate breastmilk production while feeding infant formula or expressed mil, without using bottles.
- Breastfeed an adopted baby.
- Breastfeed as a non-birth parent.
- Maintain breastfeeding if your milk production isn’t able to meet your baby’s needs eg insufficient glandular tissue.
- Maintain breastfeeing if your milk production is compromised eg breast surgery or reduction.
- Encourage a baby who is reluctant to breastfeed.
- Breastfeed a baby who is unable to feed effectively because of sucking or health problems. However this will only work if you baby can feed well enough to obtain milk.
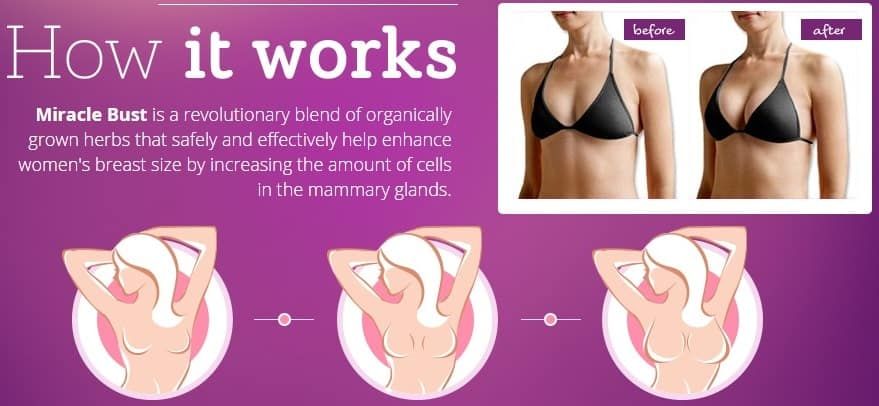
How it works
How to use
Available products
Different supplements
How to use a nursing supplementer
Cleaning
Eliminating supplements
Seek Support
How it works
A nursing supplementer lets a baby get any supplement he needs at the breast without using bottles. The supplementer container holds the milk, which travels through a tube into your baby’s mouth while he breastfeeds. As he swallows, he continues sucking, stimulating your milk production.
If you are breastfeeding expressing your milk, and giving top-ups to your baby, you may find it simpler to use a supplementer, which allows all the feeding to happen at the breast.
A good latch-on
It’s especially important that your baby latches on deeply at the breast when you are using a supplementer. Get help with positioning and attachment so your baby can get milk from the breast as well as from the supplementer.
Different supplements
Expressed breastmilk Your expressed breastmilk is the first choice for a supplement. If your baby has feeding difficulties, expressing will help you maintain and increase your milk production. To find our more about increasing your supply, see our article How to Increase Your Milk Supply. And for more information on Expressing Your Milk our article can help.
Donor milk Human milk banks provide pasteurized, screened donor milk.
Infant formula Concentrated and ready-to-feed forms of infant formula are less likely to clog nursing supplementer tubing than powdered forms. Although expensive, ready-to-feed formula may also be more convenient when you are out and about or at home without help. Powdered infant formula is not sterile, so always follow the NHS guidelines for preparing it.
Available products
Disposable bag system This uses disposable sterile plastic bags with a top opening and a single tube. Milk only flows when a baby sucks and it is discreet to use as the bags are not bulky or noisy. You can also feed lying down without fear of leaks. When your baby sucks, the flow increases as the flow of milk from your breast decreases. This reinforces proper suckling, making the most of your milk production. (As in photograph above.)
Bottle system This system uses a bottle with a tube for each breast, making switching sides easy or for twins. Each tube can be clamped. Three tube widths are available. Sets can be cleaned and reused. (As seen in the photograph below.)
Each tube can be clamped. Three tube widths are available. Sets can be cleaned and reused. (As seen in the photograph below.)
Homemade system You can make your own supplementer using an ordinary baby bottle, bottle teat and an infant nasogastric feeding tube (size #5 french, 52-75 length). Tubing can be obtained from online suppliers. (As seen in the first and last photos in this article.)
Cut a small hole in the bottle teat so the tube fits tightly. Thread the tube through the teat from the inside and attach the teat normally so the end of the tube sits in the supplement. The tube end is rounded and won’t hurt your baby’s mouth. Pierce a second hole in the teat, or use a teat with a vent to allow air in so your baby won’t need to suck harder as the bottle empties. The bottle needs to stay upright. You may find tucking it into your bra keeps it in place.
Photo courtesy of Michelle Green
How to use a nursing supplementer
Introduce the tube into your baby’s mouth along with the breast at the very beginning of a breastfeed by placing it between your baby’s upper lip and cupped tongue. If your baby doesn’t like the feel of the tube on the roof of his mouth try placing it so it lies along his tongue. Or, slip the tube into the corner of your baby’s mouth once he is well-attached at the breast.
If your baby doesn’t like the feel of the tube on the roof of his mouth try placing it so it lies along his tongue. Or, slip the tube into the corner of your baby’s mouth once he is well-attached at the breast.
You may need to extend the tube past the end of your nipple – experiment to see what works for your baby. The tube can be secured to your breast with medical tape. Taping along the tube is generally more secure than taping across it.
To hold the tube in position some mothers use fabric sticking plasters cut from a long strip. They thread the tube under the non-sticky sections.
The tube can be easily removed while the plasters stay in place, reducing skin irritation from tape removal and providing a guide for positioning each time.
Milk flow – too fast or too slow?
Constant milk flow can cause ineffective feeding as your baby will not need to actively suck to get milk. When using a supplementer you will see the milk travel along the tube to your baby’s mouth.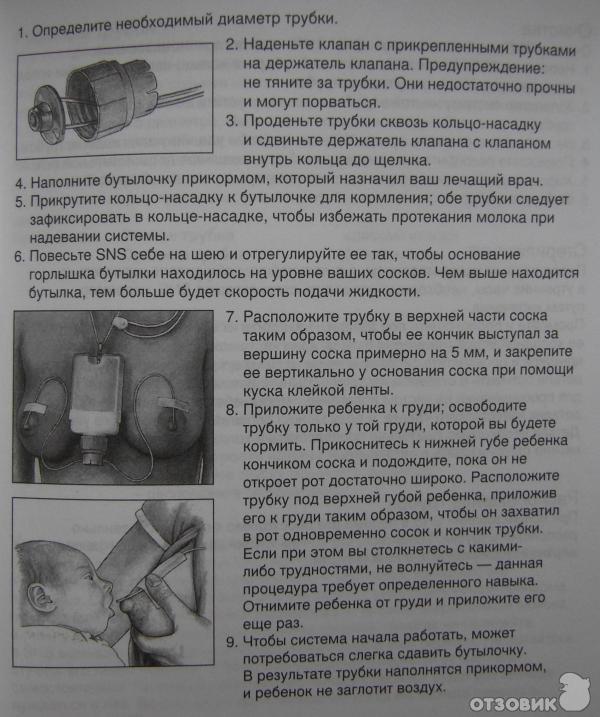 Adjust the tube position and container height so your baby gets milk quickly when he starts sucking. Check he isn’t overwhelmed with milk, especially if he has heart or breathing difficulties or is premature.
Adjust the tube position and container height so your baby gets milk quickly when he starts sucking. Check he isn’t overwhelmed with milk, especially if he has heart or breathing difficulties or is premature.
Slow down the flow of milk by lowering the milk container, raising the tubing or using thinner tubing. Or pinch the tube to slow or stop milk flow. If using the bottle system, stop milk flowing by clamping the tube in the slots in the bottle likd. To speed up milk flow, raise the bottle, use wider tubing or use two tubes at the same breast. You may need to adjust the tube in your baby’s mouth to create more suction.
Cleaning
To avoid having to throw away tubing when milk had dried inside, force cold water through the tube at least three times straight after use, using the bottle of a 5-10ml syringe. Using warm water may cause fat to cling to the sides of the tube.
For commercial supplementers follow the manufacturers’ cleaning instructions. For homemade systems, follow the NHS guidance when cleaning the bottles and teats. Wash the tubing with hot soapy water, rinse with clean water and force air through the tube (or spin the tube fast) to dry. Take extra care if using infant formula. Store the clean supplementer parts in a sealed container in the fridge.
Wash the tubing with hot soapy water, rinse with clean water and force air through the tube (or spin the tube fast) to dry. Take extra care if using infant formula. Store the clean supplementer parts in a sealed container in the fridge.
Nasogastic tubes should not be boiled, steamed or chemically sterilised as they are not designed for multiple uses. If your baby is at a higher risk of infection, a commercial system may be a safer option than a homemade system. Replace the nasogastric tube when it starts to stiffen, after about a week.
Eliminating supplements
The use of infant formula is sometimes essential to meet a baby’s nutritional needs. You may need to use formula as a stopgap measure, while you work to increase your milk production. Supplementing with formula without protecting your milk supply may reduce the duration of your breastfeeding experience.
Over time, you may be able to reduce the amount of supplement your baby needs as your milk production increases.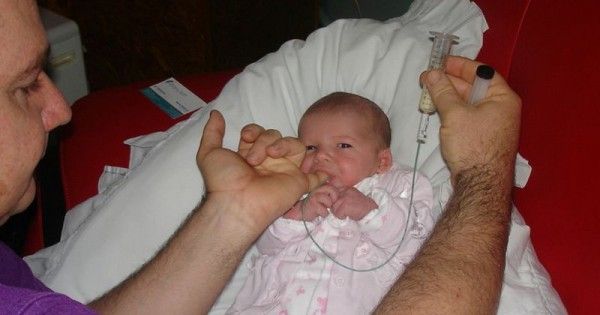 Expressing in between feeds will signal to your breasts to make more milk and give you some milk for the next feed. For more on Increasing Your Milk Supply, see our article.
Expressing in between feeds will signal to your breasts to make more milk and give you some milk for the next feed. For more on Increasing Your Milk Supply, see our article.
Begin the feed with your baby taking milk just from the breast. When he is no longer swallowing regularly start the supplementer. If your baby is reluctant to nurse at all, start the milk flowing at the beginning of a feed to get him started. As your breasts start to make more milk you will notice your baby takes less supplement, especially at certain times of day.
For more information on managing and reducing supplements see My Baby Needs More Milk and Relactation and Induced Lactation.
Seek support
Whether using a supplementer as a temporary or a long-term solution, support from your local LLL Leader and group can be a great help. For individual face-to-face help or a home visit, you could also consult a board certified lactation consultant (IBCLC) or specialist breastfeeding clinic.
Written by Karen Butler, Sue Upstone & mothers of LLLGB.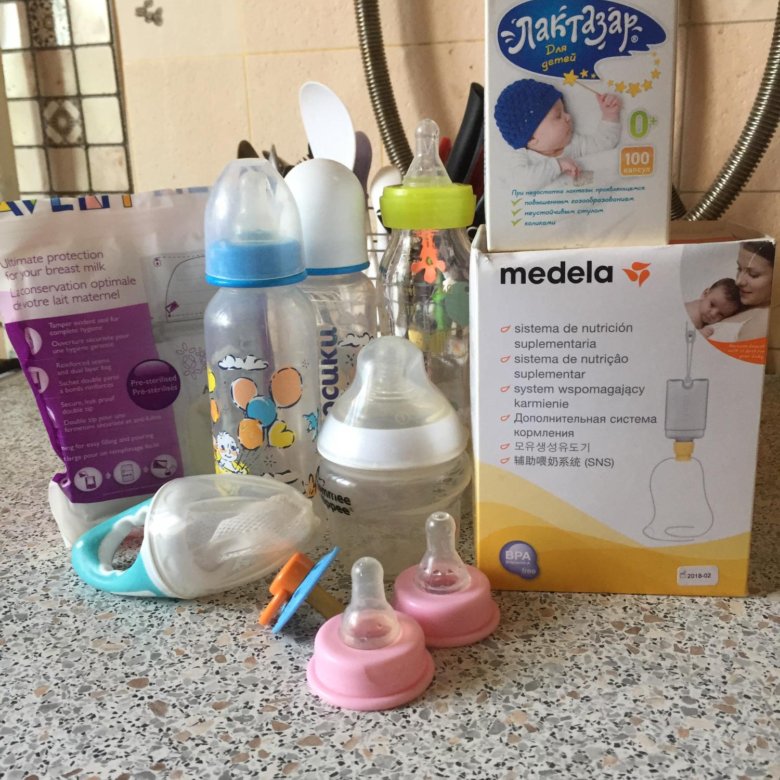 Photos courtesy of Lynn Adams, Rae Vacher Lowe and Alison Widdup.
Photos courtesy of Lynn Adams, Rae Vacher Lowe and Alison Widdup.
Further reading
Comfortable Breastfeeding
My Baby Needs More Milk
My Baby Won’t Breastfeed
Expressing Your Milk
Hand Expressing Your Breastmilk
How to Increase Your Milk Supply
Using donor milk and formula to support breastfeeding
Nipple Confusion
Relactation and Induced Lactation
Mothers’ stories
In praise of at breast supplementers
Breastfeeding with a nursing supplementer
LLLI articles
At breast supplementer nursing
Books
The Womanly Art of Breastfeeding. LLLI. London: Pinter & Martin, 2010.
Exclusively Pumping Breastmilk. Casemore, S. Gray Lion Publishing, 2014
Making More Milk Second Edition. Marasco, L and West, D., NY: McGraw-Hill, 2019.
Other websites
Homemade Supplemental Nursing System
NHS leaflet: Guide to bottle feeding
Increasing milk production
Nursing Supplementers
Please note: LLLGB does not endorse any particular breastfeeding product, aid or device or brand. La Leche League GB supports the International Code of Marketing of Breast-milk Substitutes and subsequent relevant World Health Assembly Resolutions (referred to together as “the Code”). For more information about LLLGB’s support of the Code, see here.
La Leche League GB supports the International Code of Marketing of Breast-milk Substitutes and subsequent relevant World Health Assembly Resolutions (referred to together as “the Code”). For more information about LLLGB’s support of the Code, see here.
Nursing Trainer System: www.lact-aid.com
Supplemental Nursing System: www.medela.co.uk
This information is available in printed form from the LLLGB shop.
Copyright LLLGB 2022.
What Is a Supplemental Nursing System?
Written by WebMD Editorial Contributors
In this Article
- How Does a Supplemental Nursing System Work?
- When is an SNS Used?
- Types of Supplemental Nursing Systems
- Tips to Increase Your Milk Supply
You might have heard the old adage ‘breast is best’ when it comes to feeding your baby. Sometimes, despite your best efforts, your baby’s introduction to breastfeeding doesn’t go as planned. This can happen for many reasons, but it’s usually due to low milk production.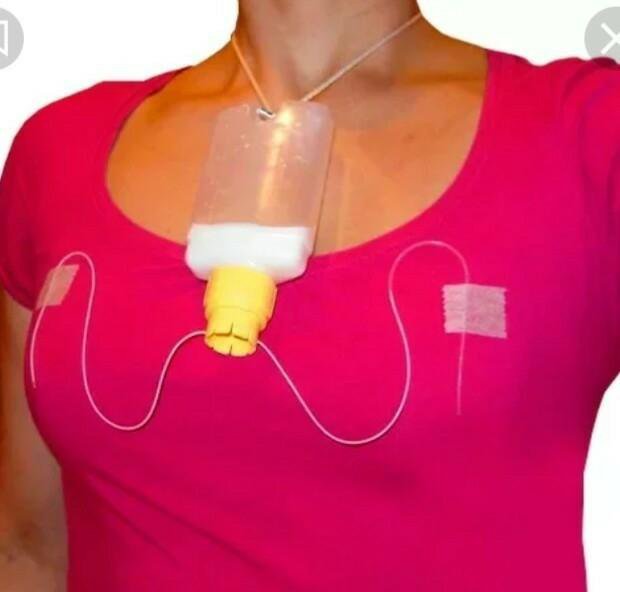 That’s where a supplemental nursing system comes in.
That’s where a supplemental nursing system comes in.
A supplemental nursing system is a device that brings nutrition to your baby as you breastfeed. Milk or formula is stored in containers, with tubes attached, that deliver the food to your hungry baby’s mouth as they breastfeed.
How Does a Supplemental Nursing System Work?
Supplemental nursing systems can look different, but all serve the same basic function. Generally, there is a bottle or small bag filled with infant formula or breast milk. Small tubes draw milk from the bottle and deliver it to your baby, often at the same time as you breastfeed.
The tubes are usually fastened to the mother using medical tape. This ensures that the fluid becomes the same temperature as the mother, and the baby can nurse comfortably.
There are many advantages to using a supplemental nursing system (SNS). When a mother’s milk production is low, the baby can get frustrated and have difficulty latching onto the nipple. With an SNS, the baby receives enough milk from both the breast and the tube to be satisfied.
When is an SNS Used?
An SNS is used when your breasts don’t produce enough milk for your baby. Using an SNS isn’t just for your baby. It also helps the mother produce more milk.
When the breast is stimulated through nursing, your body produces a hormone called prolactin. Prolactin is the hormone that encourages milk production, and mothers who have a low milk supply are usually low in prolactin.
A low milk supply can happen for many reasons such as:
- You’ve had breast surgery
- You smoke or drink alcohol
- You’re lacking sleep
- You're on certain birth control
- You give your baby formula and don’t breastfeed
- You start your baby on solid foods before they’re 4-6 months old
Types of Supplemental Nursing Systems
There are a few types of supplemental nursing systems that you can choose from. Consult with a lactation consultant to see which option might work for you and your baby.
Homemade system. If you’re new to supplemental nursing, you might want to try a homemade option before buying a new system. You can use a regular baby bottle with a rubber teat and an infant nasogastric feeding tube. Nurses and lactation consultants often keep these tubes handy for new mothers.
If you’re new to supplemental nursing, you might want to try a homemade option before buying a new system. You can use a regular baby bottle with a rubber teat and an infant nasogastric feeding tube. Nurses and lactation consultants often keep these tubes handy for new mothers.
Cut a small slit into the rubber teat and push the end of the tube through it down to the supplement fluid. Poke a hole through the teat, or use one with a vent. That way, your baby won’t face too much resistance as they empty the bottle. Note, the tubes aren’t built to be sterilized, so you’ll have to toss them when they become hard.
Disposable bag system. This system comes with sterile disposable bags that hold breast milk or a supplement. The bags are small and they hang from a string around the mother’s neck. A small, thin tube runs from the top of the bag to the baby’s mouth. The milk only flows when the baby is latched onto the tube and breast, which potentially eliminates any mess. The supplement bags are small and discreet, making them ideal for travel and feeding when out.
The supplement bags are small and discreet, making them ideal for travel and feeding when out.
Bottle system. The bottle system uses two bottles, each with a tube attached. This makes switching sides a little easier. There are usually different tube widths to choose from. Both the bottles and tubes can be cleaned, making this a more eco-friendly option. You can use clamps to stop the milk from flowing or unclamp to feed your baby. Adjust the tube width to tailor the supply to your baby’s needs.
Tips to Increase Your Milk Supply
While supplemental nursing systems can be very helpful, a goal of SNS is to stimulate the mother’s hormone production to increase milk supply. Follow these tips to help increase your supply to your baby’s demand:
- Breastfeed every time your baby is hungry, which could be as often as every two hours in the early months.
- Try to let the baby nurse from both breasts at each feeding.
- Try to avoid bottles and dummies in the first few weeks.
 While you’re still establishing your milk supply, you’ll need all of the hormone prolactin you can get. Your body makes the hormone when your baby latches.
While you’re still establishing your milk supply, you’ll need all of the hormone prolactin you can get. Your body makes the hormone when your baby latches. - Eat a healthy diet, and get as much sleep as possible.
- Pump when you’re away from your baby. It can help increase your milk supply.
SNS Medela feeding system - 7612367041164
Our advantages
Delivery on the day of order
Delivery works 7 days a week across the Crimea from 10:00-20:00
Wide range
children under 5 years old.
Quality Assurance
All items in my Lvenok stores carry a manufacturer's warranty. nine0004
Promotions and discounts
Be the first to know about promotions, discounts and special offers from moy Lvenok store.
Convenient self-delivery
You can pick up the order yourself in one of the stores in Simferopol.
Own warehouse
All goods are placed in moy Lvenok's warehouse equipped for storing children's goods.
Payment methods
You can pay for the purchase in any way: cash to the courier, bank card to the courier, card according to the details. nine0004
- 3520 R
In stock
3168 r
VIP discount card price in retail stores
Description
SNS MEDELA M 009 feeding system.0005
The Supplemental Nursing System (SNS) strengthens the unique bond between mother and baby, allowing you to achieve ever better breastfeeding results. This is made possible by the fact that when breastfeeding with SNS, a newborn baby can get exactly as much milk as he needs.
Indications for use
- Feeding foster children
- Restoration of lactation;
- Lack of milk and during the formation of lactation; nine0049
- Feeding of immature children with weak sucking reflex;
Features
- No risk of teat damage
- Helps maintain close contact between mother and baby
- Supports milk production
- The system is equipped with a graduated container for formula, which allows you to control milk consumption, the ability to make sucking easier for your baby by gently squeezing the bottle
- The cup is equipped with an adjustable neck cord that allows you to adjust the flow of milk, positioning the bottle above or below the nipples. depending on the situation
- The kit includes a medical hypoallergenic plaster, which can be used to fix the capillaries on the chest.
- Promotes the development of the correct sucking reflex in children
Reviews
SNS Medela feeding system
Brand:
Medela
View:
7612367041164
Previous Next
Our advantages
Delivery on the day of order
Delivery works 7 days a week across the Crimea from 10:00-20:00
Wide range
and children under 5 years of age. nine0004
nine0004
Quality Assurance
All items in moy Lvenok stores come with a manufacturer's warranty.
Promotions and discounts
Be the first to know about promotions, discounts and special offers from moy Lvenok store.
Convenient self-delivery
You can pick up the order yourself in one of the stores in Simferopol.
Own warehouse
All goods are placed in moy Lvenok's warehouse equipped for storing children's goods. nine0004
Payment methods
You can pay for the purchase in any way: cash to the courier, bank card to the courier, card according to the details.
The goods of this brand
are bought with this product
Do not forget to buy
,90,000 feeding the admirable child - our story Nadezhda Kasinskaya
July 12, 2011 9000 9000 9000 9000 9000 9000. first weeks together.
first weeks together.
End of May. We see our son for the first time. He is six weeks old. In the thirty-degree heat, they carried him out to us in a hat, dressed and wrapped in a blanket. He is funny and all kind of awkward, with a huge pink pacifier.
– What, will you take it right away? Maybe think more? We haven't examined him yet…
We won't think about it. We sign the consent and refusal of further medical examination, in guardianship we are promised to issue documents as soon as possible.
Documents are really processed quickly. The head physician calls somewhere, looks for someone who is not there, goes herself with certificates so that they sign it faster, takes everything to guardianship, they immediately prepare all the documents - on the second day they are already on the table of the head of the city administration. nine0004
...and get stuck there for two weeks - he just doesn't get to his office to sign. Fortunately, after a few days I am allowed to go to the hospital with the child. There we spend eight days together, almost without leaving the stuffy ward - you can walk in the yard only at the time specially allotted for this, you can’t stagger along the corridors.
There we spend eight days together, almost without leaving the stuffy ward - you can walk in the yard only at the time specially allotted for this, you can’t stagger along the corridors.
In these eight days I manage, to the indignation of the nurses, to “accustom the child to hands” and co-sleeping, wean from the regimen, and switch to bottles with a nipple for premature babies, with a very slow flow - and by the end of this time for the first time hear him cry. Before that, he did not cry at all, only groaned in displeasure when it was time for feeding. nine0004
He didn't want to be held at all, he strained and waited to be put to bed. He fell asleep only when you leave the room, and woke up abruptly if you approached the bed. They fed him from a pacifier with a huge hole. I heard the doctor swear at the nurse, who again enlarged the hole in the nipple, because the children were eating too slowly. He really ate slowly - after the first sip, he squeezed his mouth and turned away so as not to choke.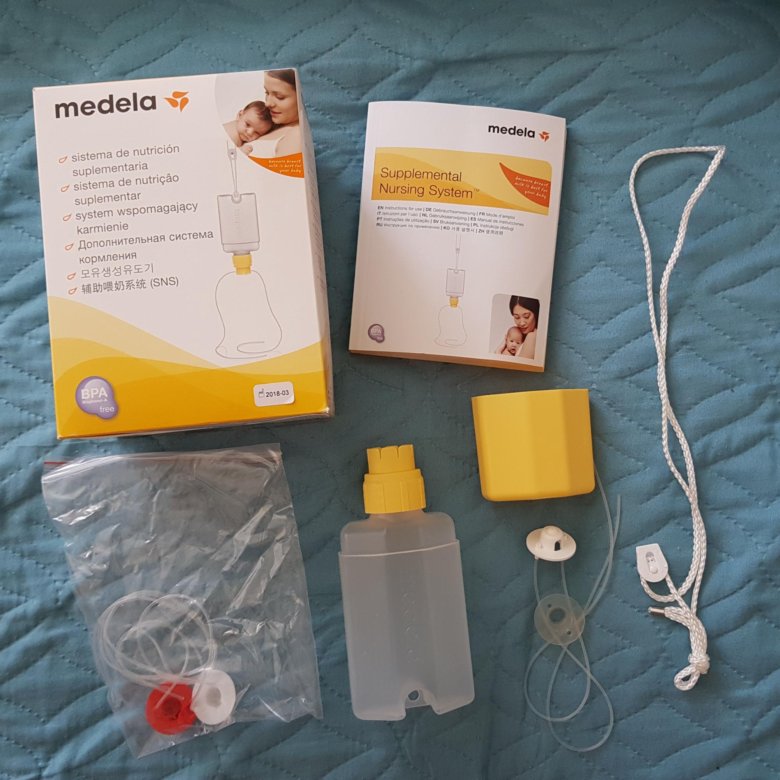
Initially, we planned to try to give the child a breast, and if he takes it easily, try to partially breastfeed together (we have a family of two mothers, I have never been pregnant, my wife gave birth and fed older daughters up to more than two years each) . And if he doesn’t take it, then, of course, we were not going to spend a lot of time and effort on this - after all, we have two older children, dogs and work, although at home, but without maternity leave. Therefore, we did not prepare for feeding in advance. In addition, until the last moment we did not know exactly what age our child would be - our only condition was that he be the youngest in the family, that is, not older than two years. nine0004
We are at home! First difficulties.
At home it turns out that he does not take my breasts at all, he yells and turns away. He doesn't know how to find breasts. When he is hungry, he opens his mouth, as for the letter "s", and waits for the pacifier to be pushed deeper into his mouth.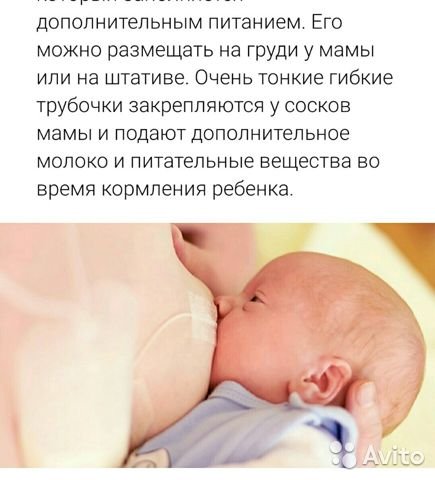 Even if you manage to put the nipple in your mouth, the tube from the SNS (breast feeding system) remains outside, and you have to start over. The wife still has a little milk in her chest after feeding her eldest daughter, he takes her breast and sucks for a while. But she was tired of five years of feeding her elders, and for me it suddenly turned out to be very important. We decide that I will try to feed despite the difficulties. The second mother takes care of the house, older children and dogs. I have work and food. nine0004
Even if you manage to put the nipple in your mouth, the tube from the SNS (breast feeding system) remains outside, and you have to start over. The wife still has a little milk in her chest after feeding her eldest daughter, he takes her breast and sucks for a while. But she was tired of five years of feeding her elders, and for me it suddenly turned out to be very important. We decide that I will try to feed despite the difficulties. The second mother takes care of the house, older children and dogs. I have work and food. nine0004
There are enough difficulties. During our hospital life, we have established some familiar rhythm with him. I understood what he wanted, and I could satisfy his needs - give a bottle, take him in my arms. At home, I suffer from the fact that I know what he needs - a bottle of formula, but I do not want to give it to him. He yells. I literally jump around with him in my arms, jumping around the room so that he calms down and takes his breast. Does not work. I give a bottle and get even more upset. In addition, while still in the hospital, he began to have colic, and in the evenings he yells in his arms too. I want to quit everything and not torment myself and the child, but I think about how I will regret in two years that I did not try to feed at least two weeks. After two weeks it should be easier. Where I got this term from, I don't know. But I believe in him. nine0004
I give a bottle and get even more upset. In addition, while still in the hospital, he began to have colic, and in the evenings he yells in his arms too. I want to quit everything and not torment myself and the child, but I think about how I will regret in two years that I did not try to feed at least two weeks. After two weeks it should be easier. Where I got this term from, I don't know. But I believe in him. nine0004
Then it dawns on me: I pour a little bit of the mixture into the SNS, the rest goes into the bottle. Yells - I give a bottle, calmed down - I try to give a breast. For the first time, he barely finishes 10 ml of the mixture from SNS. After a couple of feedings, the bottle is no longer needed. But a new problem appears - the nipples are very sore, sometimes to tears. The grip is correct - this is a plus from the fact that the child does not want to take the breast: he does not cling to it incorrectly with a death grip. They tell me that such pain, which is at the beginning of feeding, but quickly passes, is a good sign, which means that the child changes the shape of the nipple for himself. I like this idea. The pain immediately becomes easier to endure. nine0004
I like this idea. The pain immediately becomes easier to endure. nine0004
Two weeks is indeed sufficient. During this time, the breast changes, becomes soft, it is easier to give it to the child. He himself begins to look for the chest, while it is barely noticeable, but he already opens his mouth. Already it turns out to feed lying down. The pain in the nipples is almost gone. I feed only through SNS, even on the street - after the bottles he again refuses to breastfeed. There is no milk, and I begin to think that it may not appear. It's a shame. But I still feel like feeding via SNS is more natural than bottle feeding. nine0004
Month at home. First drops of milk!
A week later, almost a month after we brought our son home, the first drops of milk appear. Gradually, there is more milk, it begins to splash in thin streams. I periodically try to drink Motilium, but quickly start to forget to take a pill and quit, do without drugs. According to our estimates, in another month my milk is enough for a quarter or maybe a third of my son's needs.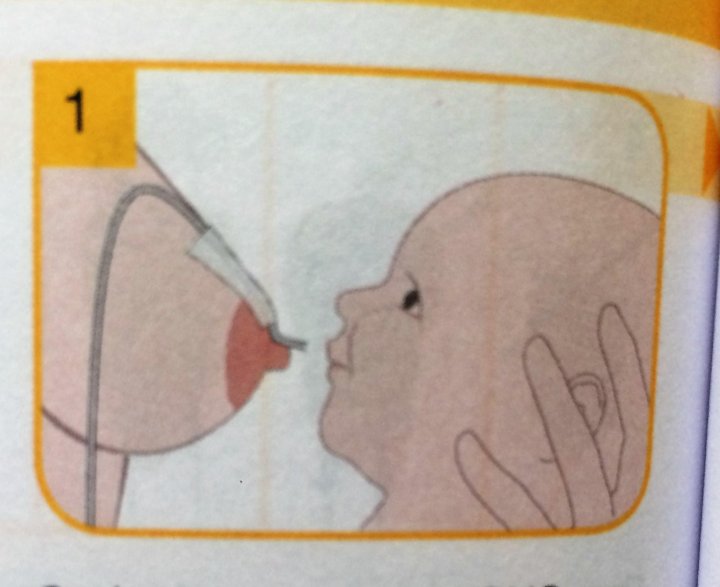 I try to offer him breasts without SNS, but most of the time he refuses. Only after six months of his life at home, when he is already 8 months old, he agrees to suck during the day without SNS - however, only in a sling and only on the run, as in the first days of feeding. But this is already good - now you can leave the house without SNS and a backpack with the mixture, do not wash straws in a public toilet and do not stir the mixture between the shelves in the store. nine0004
I try to offer him breasts without SNS, but most of the time he refuses. Only after six months of his life at home, when he is already 8 months old, he agrees to suck during the day without SNS - however, only in a sling and only on the run, as in the first days of feeding. But this is already good - now you can leave the house without SNS and a backpack with the mixture, do not wash straws in a public toilet and do not stir the mixture between the shelves in the store. nine0004
On the other hand, he starts waking up very often at night. We understand that, despite the fact that he already ate quite a lot of complementary foods and we tried to give formula from a sippy during the day, he simply switched to a night feeding regimen. On breastfeeding, this would not be a problem - we sleep together and it is convenient for me to feed in my sleep, but without SNS, he refuses to suck, and the second mother has to get up 5-7 times a night, wash SNS and make mixture.
At the same time, it seems to us that I should have enough milk. We are told that SNS is just a habit that can be unlearned. I'm very worried that I can't do it. Getting up at night is hard, we do not get enough sleep. In addition, he does not sleep well during the day, even in a sling on me, he hardly falls asleep and wakes up from the slightest rustle. nine0004
We are told that SNS is just a habit that can be unlearned. I'm very worried that I can't do it. Getting up at night is hard, we do not get enough sleep. In addition, he does not sleep well during the day, even in a sling on me, he hardly falls asleep and wakes up from the slightest rustle. nine0004
Breastfeeding is resourceful friend of foster mother!
Now overshadows the second mother. We decide not to give up SNS, since it is so important to him, but to switch from formula to water so that we don’t have to get up at night. We will be translating gradually: firstly, now he simply refuses SNS with water or even a slightly more diluted mixture. Secondly, he needs to learn to eat during the day so as not to remain hungry without a nightly mixture. And third, we're not sure how safe it is for him to drink that much water overnight. We hope that gradually he will eat more during the day and wake up less often at night. We calculate that if you remove half a spoon a week - he immediately notices more and refuses - then after two months you can completely abandon the mixture. nine0004
nine0004
And so it turns out that as we very little by little remove the mixture, he begins to eat more during the day, wake up less at night, and even agrees to occasionally suck at night without SNS at all. By eleven months of the baby, we remove the formula altogether. Now that I can sleep at night, the need to use SNS does not bother me so much, and I no longer make a conscious effort to refuse it - when I grow up enough to be able to agree with him in words, then I will try. However, the baby himself is increasingly agreeing to suck at the breast without a tube at night. Two months later, he falls asleep twice in a row at night without SNS. Then days go by without her. Then he drops it behind the sofa. It is difficult to move the sofa, so we get it only after a few days. The child does not need it for a long time. nine0004
Breastfeeding - close relationship with the baby
The baby is now one year and three months old. He does not hang on his chest like our older children, and eats a lot of "adult" food. He suckles only under certain conditions and does not settle down with the breast. I seem to have very little milk now - even when he was sick and hung on his chest around the clock, and immediately after that he abruptly refused to suck because of a runny nose - his chest did not fill up at all. However, he only sleeps with his breast - two or three times during the day and for a night's sleep, wants to suck two or three more times a day, and sucks for a long time in the morning, because of which we can sleep an extra two hours. nine0004
He suckles only under certain conditions and does not settle down with the breast. I seem to have very little milk now - even when he was sick and hung on his chest around the clock, and immediately after that he abruptly refused to suck because of a runny nose - his chest did not fill up at all. However, he only sleeps with his breast - two or three times during the day and for a night's sleep, wants to suck two or three more times a day, and sucks for a long time in the morning, because of which we can sleep an extra two hours. nine0004
Breastfeeding turned out to be much more important to me than I expected. It seemed to me very wrong and unnatural to bottle feed him and give him a pacifier. In addition, it turned out that after the first weeks of getting used to breastfeeding, even with SNS, I was much more comfortable than from a bottle - during feeding, my hands are free and I can do other things. When I breastfeed, I spend much more time with my baby than when I bottle-fed him.