Spoon feeding baby breast milk
Spoon, Cup and Paced Bottle Feeding
Feedback
View more
Spoon feeding
Cup feeding
Paced Bottle Feeding
Supplemental Nursing System (SNS) and Nipple Shields
Some reasons for different feeding methods include:
- Baby or mother's health and medical condition
- Mother is not making enough milk for a number of reasons including breast injury, and surgery
- Separation of mother and baby (for example, illness, surgery, or adoption)
- Use of necessary medication that is not safe to take while breastfeeding/nursing.
| How do I know if my baby is hungry? | ||||||||
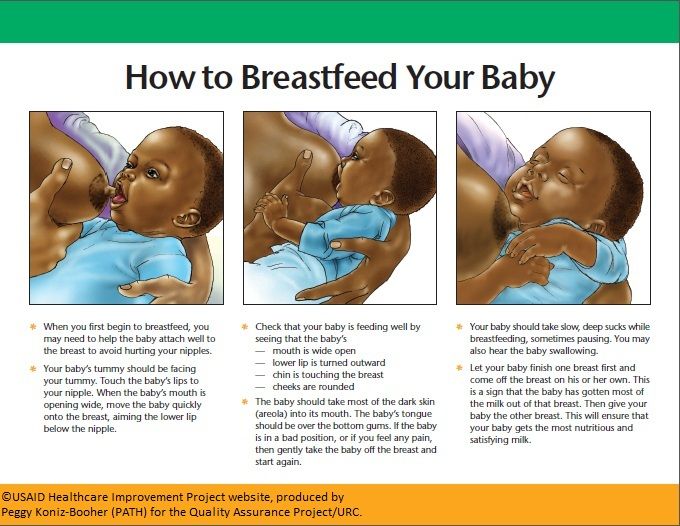
Babies need to feed a lot in the early days. Your baby has many ways to tell you they are hungry. These signs are called feeding cues. Your baby is hungry when you see these feeding cues:
Your baby is full when:
Following your baby's feeding cues will:
Remember.
| ||||||||
| Skin-to-Skin: Get to know your baby | ||||||||
What is Skin-to-Skin?
Skin-to-Skin Right after Birth
Older Babies Enjoy Skin-to-Skin too | ||||||||
| How do I know my baby is getting enough milk? | ||||||||
| Most mothers will make as much milk as their baby wants. The amount of milk made depends on the amount of milk removed from the breast by feeding, pumping or expressing.
|
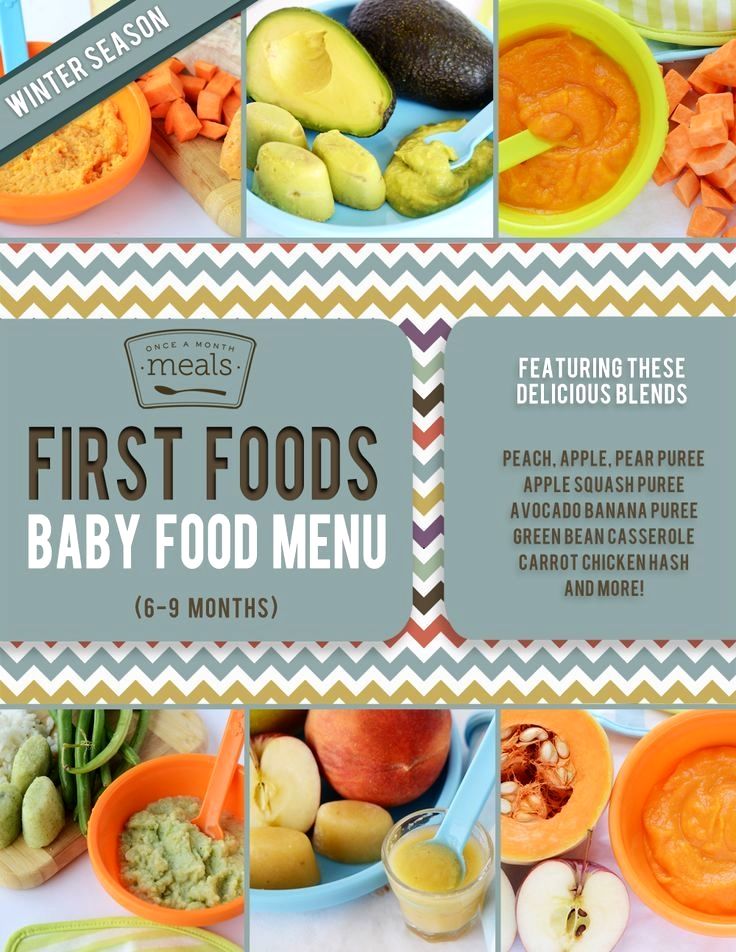
Spoon feeding
You can give expressed breast milk to your baby using a spoon. This method works best if your baby leads it and controls the speed of the feeding . Spoon feeding your baby instead of using an artificial nipple can help to reduce the risk of nipple confusion.
- Put a bib on your baby, because some breast milk may spill.
- Sit your baby up on your lap using one hand to support your baby's upper back and neck.
- Bring spoon to your baby's mouth and tip so that the breast milk just touches your baby's lips.
 It should NOT be poured into your baby's mouth.
It should NOT be poured into your baby's mouth. - Your baby will lap the breast milk up by moving his tongue forward.
- Allow your baby time to swallow before refilling spoon and offering more breast milk. This will let your baby control the speed of the feeding.
Cup feeding
Babies of all ages are able to drink from a cup (even small premature babies). You can start giving expressed breast milk in a small plastic or glass cup such as a medicine cup .
- Put a bib on your baby, because some breast milk may spill.
- Sit your baby up on your lap using one hand to support your baby's upper back and neck.
- Place edge of the cup gently against your baby's bottom lip and tip so that the breast milk just touches your baby's lips. It should NOT be poured into your baby's mouth. Your baby will lap the breast milk up by moving his tongue forward.
- Keep cup tipped during feeding so that the breast milk is always in contact with your baby's lips.
 This will let your baby control the speed of the feeding.
This will let your baby control the speed of the feeding.
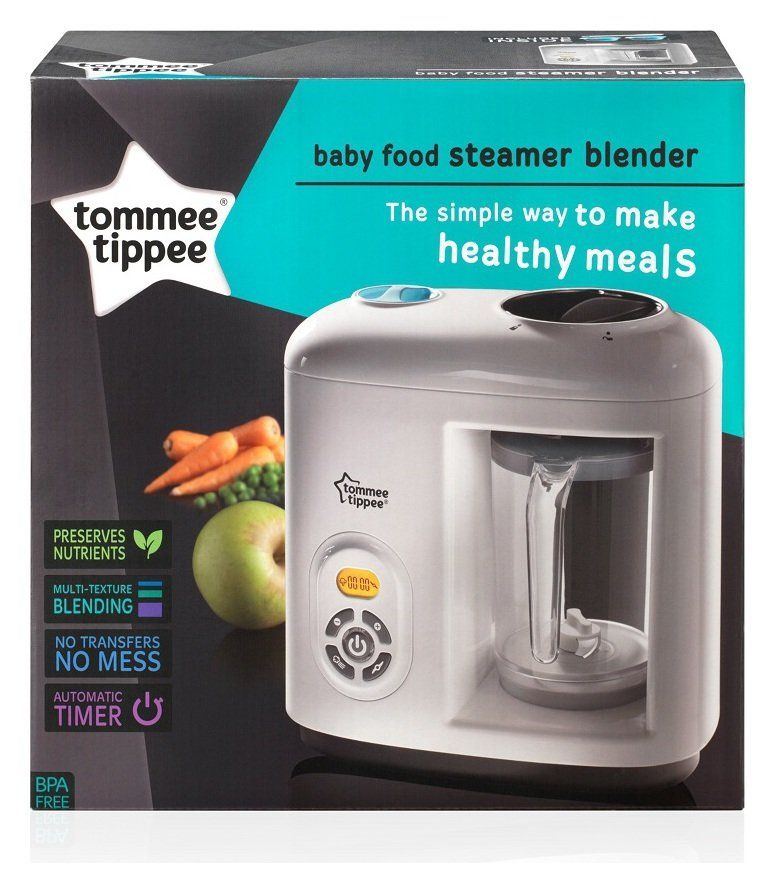
Paced Bottle Feeding
The way a baby sucks on a bottle nipple or pacifier is very different from how a baby sucks at the breast. For this reason it is best to not introduce any bottles until after breastfeeding is going well. This is usually about 4 to 6 weeks after your baby is born. Giving your baby a bottle before breastfeeding is going well can affect breastfeeding/nursing including building up your milk supply.
Paced bottle feeding is when you control or pace the flow of milk to be like breastfeeding/nursing. It also helps your baby keep breastfeeding/nursing behaviours while they feed from the bottle. Here is how to pace feeds:
- Hold your baby in an upright position, supporting their head and neck with your hand.
- Feed your baby skin-to-skin if possible.
- Use a wide-based, slow-flow nipple.
- Touch your baby's upper lip with the bottle nipple until your baby opens their mouth wide.

- Tip bottle horizontally. Let your baby pull the nipple into their mouth so their lips close on the wide base of the bottle nipple.
- Keep nipple partially full as it will help your baby control flow better. Your baby will naturally swallow air during feeds.
- If your baby gets tense or gulps, stop feed. Stop the feed by tilting bottle down to stop flow but keeping bottle nipple in contact with your baby's lower lip. This way your baby can pull the nipple back into their mouth.
- Your baby will learn to take breaks and 3 to 5 second pauses on their own usually after the fourth or fifth suck and as needed.
- When you think your baby is nearly full, twist and remove bottle keeping the nipple lying on your baby's lip as described above. If your baby takes bottle again, let your baby feed for a short period (for example, 5-10 swallows) and repeat process. When your baby has had enough to drink they will not open their mouth when you try to give them the bottle.
 This is 1 sign a baby uses to let you know they are full.
This is 1 sign a baby uses to let you know they are full. - Throw away any breast milk left in the bottle after the feeding.
Supplemental Nursing System (SNS) and Nipple Shields
You should not start the use of these aids on your own. Talk to a Lactation Consultant or your health care provider about if you need to use them. To find a Lactation Consultant in your area, visit Ottawa Valley Lactation Consultants.
Do you have more questions about parenting?
- Speak with a Public Health Nurse. Call the Ottawa Public Health Info Centre at 613-PARENTS [613-727-3687] (TTY: 613-580-9656) or email Ottawa Public Health at [email protected]
- Connect with a Public Health Nurse and other parents on the Parenting in Ottawa Facebook page
- There are a variety of services to make it easier for your child to grow up healthy in Ottawa
September 2019
Partners
6 Different Ways To Feed Your Baby Expressed Breastmilk (Or Formula)
There are various reasons why a mother may feed her baby expressed breastmilk (EBM).
For example, her newborn may not be latching on, she may be taking a break from direct breastfeeding to help heal sore and damaged nipples, she may be topping her baby up as her baby may not be feeding optimally from the breast yet, or she may be going out without her baby.
When it comes to feeding your baby (who predominantly feeds directly from the breast) in any other way, often the first, and sometimes only, method that comes to mind is a bottle.
However, there are various methods to do this. Particularly when breastfeeding is important to you, the potential impact a particular method can have on your baby’s ability to breastfeed needs to be considered.
All methods appear to have risks and benefits. Speaking about your individual situation with an International Board Certified Lactation Consultant (IBCLC) or a volunteer breastfeeding counsellor can help you select the most suitable method for you and your baby.
Here are 6 ways to feed your baby expressed breastmilk (or formula).![]()
#1: Bottle feeding
A bottle is probably the most common alternative feeding method. In many ways, bottle feeding is seen as convenient and socially acceptable. A bottle may be a method of choice if other alternative methods have been unsuccessful or if large volumes are needed.
However, there are some drawbacks associated with the use of the bottle such as:
- Overfeeding. This is likely one reason why formula feeding increases the risk of obesity
- Differences in a baby’s tongue and jaw movements when bottle feeding, compared to breastfeeding. This may be a reason why formula feeding increases the risk of malocclusions
- Differences in flow. When a baby drinks from a bottle she can bring on the flow immediately and get a more consistent faster flow than when feeding at the breast. This may increase the risk of a baby developing a preference for bottle-feeding
- Lack of skin-to-skin contact with the baby. Skin-to-skin contact is important as it helps boost oxytocin (the ‘feel good’ hormone) levels and helps to regulate a baby’s heart rate, temperature, and blood sugar levels
- Undermining a mother’s confidence in breastfeeding.
 Particularly if a mother uses a bottle to frequently top up her baby, she may see her baby guzzle more than she needs from the bottle time and time again. The message this can send to the mother is that she is inadequate, or that she isn’t producing enough milk for her baby.
Particularly if a mother uses a bottle to frequently top up her baby, she may see her baby guzzle more than she needs from the bottle time and time again. The message this can send to the mother is that she is inadequate, or that she isn’t producing enough milk for her baby.
When feeding a baby from a bottle, it’s important to ensure the feed is paced to assist in the regulation of her intake and suck, swallow, and breathing. This can also help to reduce the risk of problems such as breast refusal.
When bottle feeding your baby:
- Have her sit upright and gradually lower her back as milk is removed from the bottle.
- Hold her in close to your body
- Alternate from which arm she is held at each feed. This helps ensure her alternate visual fields are used which may assist with her brain and eye development
- Break the suction every so often and move it to the side of her mouth before resuming the feed
- Follow her cues. She may not want to finish all the milk in the bottle.

Are You Getting BellyBelly’s Baby Week By Week Emails?
We think they’re the best on the internet!
Click to get the FREE weekly updates our fans are RAVING about.
#2: Spoon feeding
Spoon feeding can be a great way to deliver small amounts of milk (e.g. colostrum) to babies who are not latching or feeding properly.
For example, some babies may be particularly sleepy due to drugs used during the birthing process or jaundice. Small amounts of milk delivered by spoon may help rouse some babies, who aren’t latching, to latch on and feed.
A particularly beneficial aspect of spoon feeding is that it allows the baby to determine her own feeding pace.
#3: Cup feeding
Particularly when cleanliness is suboptimal, cup-feeding can be a viable, safe alternative method to provide expressed breastmilk or formula to babies.
Cup feeding encourages a baby’s tongue to move down and forward, similar to tongue movement during breastfeeding. Cup feeding with a correct and safe technique allows a baby to control her intake and pause when necessary to reorganize her breathing.
Cup feeding with a correct and safe technique allows a baby to control her intake and pause when necessary to reorganize her breathing.
Cup feeding can expose the preterm infant to the smell and taste of human milk, and provide a positive oral feeding experience for the baby without disrupting the breastfeeding process.
Research has demonstrated that cup feeding (as compared to bottle feeding) increases the likelihood that preterm babies will be fully breastfed at discharge home.
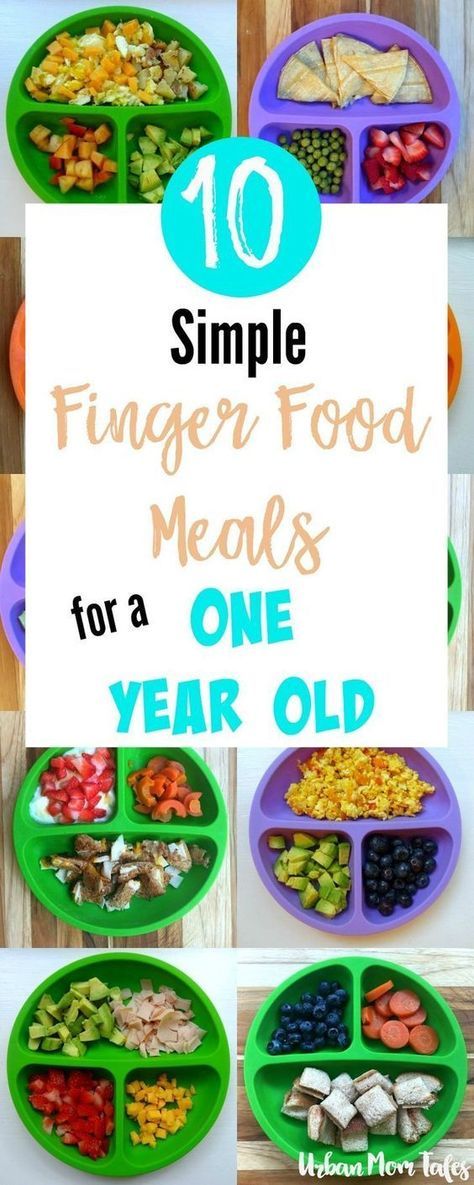
Particularly when small to moderate volumes of milk are being delivered to young babies in the short term, cup feeding (e.g. from a medicine cup) can be a great option. For older babies, cup feeding (e.g. from a sippy cup, no-spill cup, cup with a straw) can also be a great alternative feeding method.
Here is a video about cup-feeding a baby.
#4: Finger feeding
Like with cup feeding, finger feeding assists in keeping a baby’s tongue down and forward.
If done properly, finger feeding puts the baby in control of her intake too.
It can be used to help rouse a sleepy newborn, who isn’t latching, to latch on and breastfeed.
#5: Syringe feeding
While syringe feeding may be used to rouse a baby if only a few drops are used, there are some drawbacks associated with its use such as it:
- May increase risk of aspiration
- May result in pursed lip configuration
- Does not facilitate breastfeeding
- Does not allow a baby to control how much she gets.
#6: Breastfeeding supplementer
A breastfeeding supplementer allows direct breastfeeding to continue while simultaneously stimulating the breast to produce more milk. It provides a reward to the baby for feeding at the breast and removes the need for use of other supplemental feeding methods such as a bottle.
For some mothers, however, a breastfeeding supplementer can be tricky to get the hang of using and can be difficult to clean. For a breastfeeding supplementer to work, the baby must be willing to breastfeed and the mother needs a keen, positive attitude as using one involves a considerable commitment by the mother.
For a breastfeeding supplementer to work, the baby must be willing to breastfeed and the mother needs a keen, positive attitude as using one involves a considerable commitment by the mother.
A breastfeeding supplementer is likely the best method choice if supplementation is likely to be required on a longer term basis such as to induce lactation (e.g. for an adopted baby), to relactate, or for mothers with ongoing low supply issues.
In summary, when selecting an alternative feeding method, it’s important to consider:
- Its cost and availability
- How easy it is to use and clean
- If it causes any stress to your baby
- How long it’s anticipated to be used
- Your preference
- Its potential impact on breastfeeding.
Remaining confident in your ability to breastfeed is important so that you don’t feel like you have to continue with the alternative feeding method once the need is over.
Recommended Reading:
- Choosing A Teat Most Like The Breast – 4 Surprising Facts
- How Often Should I Feed My Breastfed Baby?
- How Often Should I Feed My Baby Formula? 3 Things To Know
How to supplement a baby with donor milk from a spoon
donate milk
Find milk
A regular teaspoon is a great way to supplement with donor milk. It just takes a little getting used to. Some mothers complain that the cub does not understand what to do. But in order to eat from it, he does not have to understand anything! The process is fully supervised by an adult. Many home midwives recommend the spoon for feeding small and premature babies who are born at home if they cannot or weakly suckle.
It just takes a little getting used to. Some mothers complain that the cub does not understand what to do. But in order to eat from it, he does not have to understand anything! The process is fully supervised by an adult. Many home midwives recommend the spoon for feeding small and premature babies who are born at home if they cannot or weakly suckle.
An ordinary teaspoon or dessert spoon does not look like a breast at all, so when supplementing in this way, it is very unlikely that the breast will refuse and that the grip will deteriorate (unlike a bottle). We all have this cutlery in the kitchen and it is always at hand, they are easy to clean, and they are not afraid to lose them. If colostrum is expressed into a spoon and supplemented directly from it, then precious drops are not smeared on the dishes due to their density and surface tension of the liquid. An older kid gradually acquires the skill of eating from a spoon.
But it really takes a little practice and skill to master this method of supplementing. It would be great if someone who already knows how to do it well can show you how to spoon feed in practice - in this case, almost everyone masters the technology the first time. If a mother is traveling with a child, then it must be borne in mind that it can be problematic to supplement with a spoon in a car or train - milk spills due to shaking. Some mothers note that when giving out large volumes of food with a spoon, babies lose the habit of sucking, and very hungry children can be annoyed by a pause when scooping up food.
It would be great if someone who already knows how to do it well can show you how to spoon feed in practice - in this case, almost everyone masters the technology the first time. If a mother is traveling with a child, then it must be borne in mind that it can be problematic to supplement with a spoon in a car or train - milk spills due to shaking. Some mothers note that when giving out large volumes of food with a spoon, babies lose the habit of sucking, and very hungry children can be annoyed by a pause when scooping up food.
The technology of feeding with a spoon is as follows:
We scoop up about a quarter of the volume of the spoon, touch it with the bottom side to the lower lip of the newborn, wait until the mouth opens, and put the spoon into a well-opened mouth. We put it in, and quite deeply on the tongue, so that at least 2/3 of the spoon goes into the mouth. We tip it over and wait for the swallowing movement, when the baby covers his mouth and begins to push the spoon out with his tongue. Pushes - pull out, give the next spoon. All this time, the child lies at an angle of about 30 degrees on the knee or on the crook of the mother's elbow.
Pushes - pull out, give the next spoon. All this time, the child lies at an angle of about 30 degrees on the knee or on the crook of the mother's elbow.
After a little practice, the process goes pretty fast, much faster than you read the description.
When a child is full, he usually either closes his mouth and refuses to open it before the next meal, or starts spitting out food.
Examples of videos of supplementary feeding with a spoon:
This is the first milk baby of the "Milk Mom" - Svet, here it is shown supplementary feeding with donor milk:0003
Sources:
- Personal experience
- Internet community "Lyalechka"
Feeding with expressed milk | breastfeeding
When can I start breastfeeding my baby with expressed breast milk? How to do it right? Is it worth worrying that the child will confuse the pacifier with the breast? In this article we will answer your questions.
Share this information
When can I start breastfeeding my baby?
If your baby is healthy and breastfeeding well, there is no need to give him expressed milk. For the first four weeks, you work together to start and increase milk production, and your baby also learns to suckle properly at the breast. There is not yet enough scientific evidence on this, 1 but there is an opinion that bottle feeding in the first month may adversely affect the process of establishing breastfeeding.
However, if the newborn is unable to latch on or suckle for some reason, start expressing milk as soon as possible after birth. Read more about this in our articles on coping with problems in the first week, breastfeeding premature babies and babies with special needs, and seeking help from your healthcare provider.
How to feed your baby with expressed breast milk?
There are many expert feeding solutions that allow you to give your baby expressed milk in a variety of ways, depending on your and your baby's needs.
For example, the innovative Calma smart pacifier only lets milk through when the baby creates a vacuum by suckling. This means that when feeding from a bottle, he will make the same movements with his tongue and jaws as when sucking at the breast. 2.3 The Calma Smart Soother was developed with input from breastfeeding experts at the University of Western Australia. When using this pacifier, the baby can suck, swallow, pause and breathe in the same way as when breastfeeding. 4 Preservation of natural sucking skills allows the baby to easily transition from breast to bottle and back.
In addition, Medela also offers regular bottle teats* in two versions that produce milk at different rates. All Medela* nipples can be placed directly on bottles used for expressing milk, minimizing the risk of spillage.
If you need to feed your baby with expressed milk, but you do not want to bottle feed him until he is learning to breastfeed, you can use a sippy cup* for temporary feeding. The baby will be able to drink milk from such a mug, but you should be careful not to spill the milk. For the first time, it is advisable to feed the child from a drinking cup under the supervision of the attending physician in order to learn how to do it correctly.
The baby will be able to drink milk from such a mug, but you should be careful not to spill the milk. For the first time, it is advisable to feed the child from a drinking cup under the supervision of the attending physician in order to learn how to do it correctly.
If your baby needs to be supplemented with expressed milk in addition to regular breastfeeding, the Supplementary Feeding System (SNS)* can be used. It is equipped with a thin, flexible capillary that can be clipped close to the nipple to give your baby expressed milk while breastfeeding. Thanks to this, the baby suckles the breast for longer, thereby developing sucking skills and stimulating the production of milk from the mother. This can be helpful when there is a shortage of breast milk, as well as when feeding adopted or surrogate children.
If the baby is unable to breastfeed because he is too weak or has a congenital disease, you can use the Special Needs Cup*, which releases milk with gentle pressure, making it suitable for feeding these babies.
How to teach a child to bottle feed?
If breastfeeding is going well and you decide to start bottle feeding your baby with expressed breast milk, follow these guidelines.
Start early and take your time
Don't wait until the first day of work or the first time you leave the house to start bottle feeding your baby. Start accustoming your baby to small portions of expressed milk a couple of weeks before the desired date, calmly and without haste. Gradually build up to one full serving of pumped milk from a bottle.
Choose a time
Ideally, at the first bottle feeding, the baby should be hungry, but not too hungry - in this state, he is as relaxed as possible.
Let others feed
Your baby is used to feeding from your breast, so when you offer him a bottle it can be confusing. The process can go faster if the first time the baby is bottle-fed by someone else while you are not in the room, so that your sight and smell do not embarrass the baby.
Maintain optimal temperature
Your baby will be more willing to eat expressed milk if the temperature is around 37°C, close to body temperature.
Dip a nipple in milk
Try dipping a nipple in expressed milk before offering it to your baby. This way it will taste and smell like your breast milk. Lightly touch the baby's upper lip with the nipple to open the mouth.
Choose the right position for bottle feeding
Feed your baby on demand and keep him reclining during feeding. Never bottle feed your baby when he is lying or sitting, otherwise he may choke. Listen to the wishes of the child - take as many pauses as he needs. You can even try to shift it from one hand to another during feeding.
Be patient
Don't worry if your baby doesn't take the bottle right away - it may take several tries. If he pushes the bottle away or starts crying, calm him down, wait a few minutes and try again. If he still doesn't want to bottle feed, wait a few more minutes and breastfeed him as usual. Repeat the bottle experiment at a different time of day.
If he still doesn't want to bottle feed, wait a few more minutes and breastfeed him as usual. Repeat the bottle experiment at a different time of day.
How much pumped milk should I give my baby?
All children are different. Research shows that between the ages of one and six months, a baby can consume between 50 and 230 ml of milk per feeding. To start, prepare about 60 ml and observe how much your baby needs - more or less. You will soon realize how much milk he usually eats. Just never force him to finish the cooked portion.
How can I keep my baby safe when bottle feeding?
Always clean and sterilize your breast pump and bottles according to the manufacturer's instructions. Wash your hands before expressing, pouring milk, and feeding your baby. Follow our instructions for safely storing and thawing your expressed milk.
If breastmilk needs to be warmed, place the bottle or bag in a bowl of warm water or a heater or under running water at a maximum of 37°C. Never heat breast milk in the microwave or on the stove.
Never heat breast milk in the microwave or on the stove.
Will the baby be able to transition from breast to bottle?
Some mothers worry that if they start bottle feeding too early, they will get used to the artificial nipple and not want to breastfeed. Others, on the contrary, are worried that if the child is not immediately accustomed to the bottle, then he will no longer eat from it. In general, in these cases, they say that the child confuses the nipple with the breast.
Experts disagree on whether such confusion is a problem. 1 Without a doubt, it is easier for a baby to suckle milk from a regular bottle with a nipple, which does not require a vacuum, than from the breast, since the milk flows faster, also under the influence of gravity. And some babies really have clear preferences: only the breast or only the nipple. However, many babies are comfortable suckling both the breast and the pacifier.
If you are unable to feed your baby with expressed breast milk, seek help from a lactation consultant or specialist.
Literature
1 Zimmerman E, Thompson K. Clarifying nipple confusion. J. Perinatol. 2015;35(11):895-899. - Zimmerman I., Thompson K., "On the issue of breastfeeding." J Perinatol (Journal of Perinatology). 2015;35(11):895-899.
2 Geddes DT et al. Tongue movement and intra-oral vacuum of term infants during breastfeeding and feeding from an experimental teat that released milk under vacuum only. Early Hum Dev . 2012;88(6):443-449. - Geddes D.T. et al., "Language Movements and Oral Vacuum Generation in Term Infants During Breastfeeding and Feeding from an Experimental Vacuum-Delivery Teat". Airlie Hume Dev. 2012;88(6):443-449.
3 Segami Y et al. Perioral movements and sucking pattern during bottle feeding with a novel, experimental teat are similar to breastfeeding. J. Perinatol. 2013;33(4):319-323. - Segami I. et al.



 Occasional "red, brick-coloured" staining (uric acid crystals) is normal until day 3. At 3 days old has at least 3 brown/green/yellow, soft stools.
Occasional "red, brick-coloured" staining (uric acid crystals) is normal until day 3. At 3 days old has at least 3 brown/green/yellow, soft stools.
 5 oz) per week. They usually double their birth weight by 3 to 6 months.
5 oz) per week. They usually double their birth weight by 3 to 6 months.