Symptoms of food sensitivity in babies
Infant Allergies and Food Sensitivities
Human breast milk typically does not cause allergic reactions in breastfeeding infants, but mothers sometimes worry that their babies may be allergic to something that they themselves are eating and passing into their breast milk. In fact, only two or three out of every one hundred babies who are exclusively breastfed demonstrate an allergic reaction—and that’s most often to the cow’s milk in their mother’s diet. In this case, the infant may show signs of severe colic, abdominal discomfort, or a skin rash such as eczema or hives, or may react with vomiting, severe diarrhea (often with blood in the stool), or difficulty breathing that lasts up to several hours after breastfeeding.
If you note any of these symptoms, contact your pediatrician right away. While rare—especially among breastfed babies—milk allergies can be severe or fatal. Most babies eventually outgrow their allergy to cow’s milk, although food allergies to other substances may be lifelong.
Breastfeeding exclusively for the first six months of life has been shown to significantly lessen the risk and severity of food allergies in families with a strong history of them. Exclusive breastfeeding or breastfeeding in combination with partially or extensively hydrolyzed infant formula also reduces the risk for eczema, a condition of excessively dry and easily irritated skin.
So far, there is no evidence that avoiding certain foods while breastfeeding can help prevent your child from developing allergies or asthma. The exception to that might be eczema: some studies suggest that avoiding certain foods may reduce your baby’s risk for developing eczema. Still, if your family has experienced severe food allergies, you might consider limiting your intake of milk and dairy products, fish, eggs, peanuts, and other nuts during pregnancy and while breastfeeding. Monitor your baby carefully for skin rashes, breathing problems, unusual stools, or other allergic symptoms, and be sure to tell your pediatrician about your family’s medical history.
A few mothers notice minor reactions to other foods in their diet. Some babies cry, fuss, or even nurse more often after their mother has eaten spicy or "gassy" foods (such as cabbage). These reactions differ from allergies in that they cause less-serious symptoms (no rashes or abnormal breathing) and almost always last less than twenty-four hours.
If your baby reacts negatively every time you eat a certain type of food and you find this troubling, you can just avoid that particular food temporarily. If these symptoms continue on a daily basis and last for long periods, they may indicate colic rather than food sensitivity. Talk with your pediatrician about this possibility, if eliminating various foods has no effect on your child’s symptoms.
- Last Updated
- 11/2/2009
- Source
- New Mother's Guide to Breastfeeding, 2nd Edition (Copyright © 2011 American Academy of Pediatrics)
The information contained on this Web site should not be used as a substitute for the medical care and advice of your pediatrician. There may be variations in treatment that your pediatrician may recommend based on individual facts and circumstances.
There may be variations in treatment that your pediatrician may recommend based on individual facts and circumstances.
Food allergy vs. food intolerance: What is the difference and can I prevent them?
What is an allergy?
An allergy happens when a person’s immune system treats a substance (allergen) like an inappropriate invader. The body will try to protect itself by releasing a chemical into the body called histamine. This chemical is what causes the symptoms that are unpleasant or even dangerous. The reaction can start very suddenly, even after being exposed to a small amount of the allergen.
Allergens can get into the body in different ways. They can be:
- inhaled (such as dust or pollen),
- ingested as food (some common ones are nuts, eggs or shellfish),
- ingested as medication (such as penicillin),
- injected by an insect sting (like a bee or wasp venom), or
- absorbed through the skin (such as poison ivy).
What foods are common allergens?
Any food can trigger an allergic reaction, but the most common are:
- peanuts
- tree nuts
- eggs
- shellfish
- fish
- milk
- soy
- wheat
Are there any foods I should avoid while breastfeeding to prevent my child from getting allergies?
You don’t need to avoid milk, egg, peanut or other foods while breastfeeding. There is no evidence that avoiding certain foods will prevent allergy in your child.
Is there a particular formula I should use to prevent allergies?
If breastfeeding is not an option or if you choose not to breastfeed, use a store-bought iron-fortified infant formula for the first 9 to 12 months. The formula should be cow’s milk-based. There is no evidence that soy-based or hydrolyzed formula will prevent your child from developing an allergy.
Should I wait to offer common food allergens to my baby for the first time?
- Don't delay.
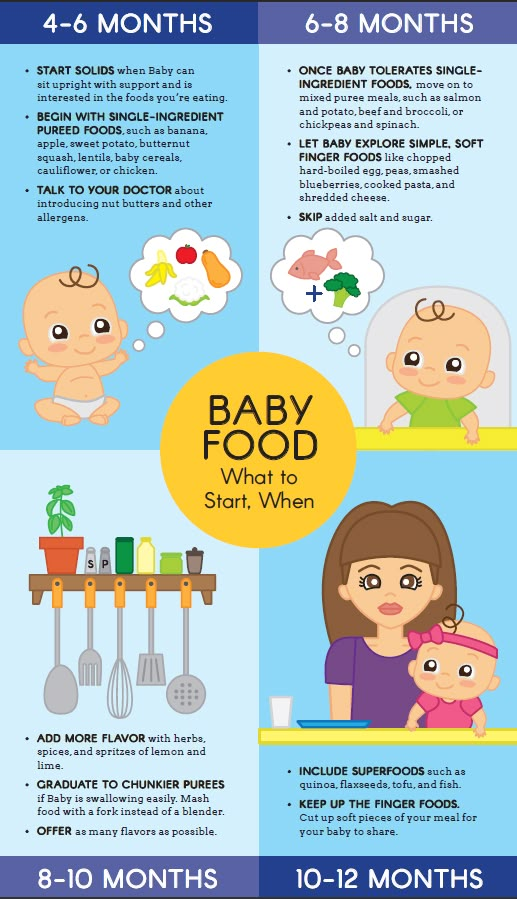
 In infants at low risk for food allergy, common food allergens can also be introduced at around 6 months of age to try to prevent an allergy.
In infants at low risk for food allergy, common food allergens can also be introduced at around 6 months of age to try to prevent an allergy. - For children considered at high risk of developing an allergy (e.g., they have a parent or sibling with an allergic condition, or they have other allergies, such as eczema), consider introducing common food allergens at around 6 months of age, but not before 4 months.
- When introducing foods that are common food allergens, try offering no more than 1 per day. Wait 2 days before you introduce another. This makes it easier to identify a food that may have caused a reaction.
- Once you offer these foods to your child, it’s important to continue to offer them on a regular basis.
- If you have concerns, speak to your health care provider.
How will I know if my child has a food allergy?
Most often, your child will have to eat a food more than once before you know they are allergic. For example, the first time your child is exposed to nuts, there will probably be no reaction. If they develop an allergy to nuts, the next exposure could be more serious.
If they develop an allergy to nuts, the next exposure could be more serious.
What are the signs of an allergic reaction to food?
An allergic reaction can affect many different body parts. Symptoms can include:
- itchy mouth and throat when eating certain foods,
- hives (raised red, itchy bumps on the skin),
- stomach trouble (diarrhea, cramps, nausea, vomiting),
- swelling of the face or tongue, or
- trouble breathing.
What is anaphylaxis?
Allergic reactions can be very serious, even life-threatening. In rare cases, a child may have a rapid and severe reaction to an allergen. This is called anaphylactic shock or anaphylaxis. It can happen within minutes or up to 2 hours after being exposed to an allergen.
What are the symptoms of anaphylaxis?
A severe allergic reaction can cause:
- difficulty breathing,
- swelling of the face, throat, lips, and tongue (in cases of food allergies),
- rapid drop in blood pressure,
- dizziness,
- unconsciousness,
- hives,
- tightness of the throat,
- hoarse voice,
- lightheadedness.

If any of these happen to your child, go the nearest emergency department or call 911 immediately.
Do children outgrow food allergies?
Many children outgrow food allergies, especially if the allergy started before age 3. Allergies to milk, for example, will usually go away. However, some allergies, like those to nuts and fish, probably won’t go away.
What is food intolerance?
Food intolerance is different from an allergy. It is not caused by an immune reaction. Food intolerance will cause discomfort, but it’s not dangerous to your child.
How can I tell if my child has food intolerance?
Your child may experience bloating, loose stools, gas or other symptoms after eating a specific food. Even though this reaction is not dangerous, if it causes your child discomfort you might want to avoid those foods in the future.
What is lactose intolerance?
Lactose intolerance happens when the body doesn’t produce enough of the enzyme lactase to fully break down the sugar (lactose) found in most dairy products.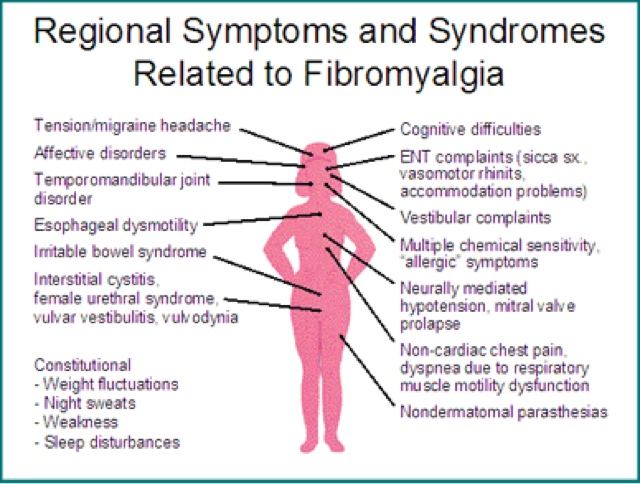 It is rare in young children and usually only develops after 3 years of age. While some young children adjust to the lack of this enzyme, some will have problems for life.
It is rare in young children and usually only develops after 3 years of age. While some young children adjust to the lack of this enzyme, some will have problems for life.
If your child is lactose intolerant, you can give them the calcium they need by offering lactose-free or lactose-reduced milk.
While none of these items will provide enough calcium on their own, it’s also healthy to offer:
- fortified soy milk,
- yogurt,
- canned salmon and sardines with edible bones,
- oranges or fortified orange juice,
- broccoli,
- almonds, and
- pinto beans.
Many of these foods do not provide enough vitamin D. Talk to your doctor about whether a supplement of vitamin D would be right for your child.
When should I call the doctor?
It is hard to diagnose food allergies. If your child has a reaction to a food, you will need to see your doctor. Your doctor will refer you to an allergist for the right testing.
If a serious allergy is confirmed, your doctor may prescribe a medication (e.g. EpiPen or Allerject), a needle that will protect your child right away if they are exposed to the allergen.
More information from the CPS
Additional resources
Reviewed by the following CPS committees
- Allergy Section
- Community Paediatrics Committee
- Nutrition and Gastroenterology Committee
Last updated: March 2021
90,000 symptoms and treatment. Signs, causes and diagnosis of food allergies in a child.Food allergies in children are the body's response to certain foods. The most common type of response is that mediated by antibodies of the Ig E type. There is a cell-mediated immunological response that appears later. The atypical condition is accompanied mainly by atopic dermatitis or disorders of the digestive system.
On the other hand, food can also cause a reaction if it comes into contact with the skin or comes into contact with the respiratory tract.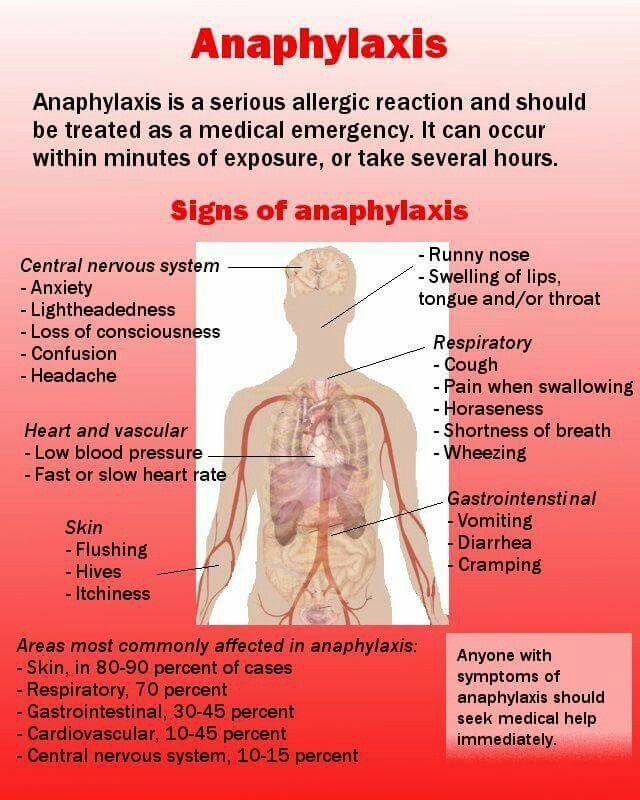 In the first case, this can lead to dermatitis and urticaria; in the second - to problems associated with the respiratory apparatus (asthma or rhinitis).
In the first case, this can lead to dermatitis and urticaria; in the second - to problems associated with the respiratory apparatus (asthma or rhinitis).
Currently there are several types:
1. On the protein of a chicken egg. It develops during the production of Ig E immunoglobulins in the body, directed against egg whites. The most common risk factor is hereditary predisposition. It usually occurs between the ages of 1 and 5 years. It is characterized by reddening of the skin, itching, urticaria, swelling of the lips and eyelids. Vomiting, abdominal pain and diarrhea are possible. Less commonly, respiratory manifestations occur, which may be accompanied by shortness of breath and difficulty swallowing. They are very serious, so the patient should see a doctor the moment they start to occur.
2. For fish and seafood. Established by the immune response, which is mediated by Ig E - antibodies specific to fish. It is noted in the first years after birth and coincides with the introduction of fish into the diet. It may persist for decades or a lifetime. Signs appear after consumption and by inhalation of fumes generated during cooking.
It may persist for decades or a lifetime. Signs appear after consumption and by inhalation of fumes generated during cooking.
3. For milk. It has a hereditary basis, although environmental factors also participate in its development. It is characteristic mainly for the first year of life. The severity of the clinical picture depends on the degree of sensitization and the amount of milk consumed. The most common manifestations are skin (70% of cases). There is also abdominal pain, loose stools, vomiting, or trouble swallowing.
4. On vegetables and fruits. Most common cause in patients over 5 years of age. About 33% of children are intolerant to fruits and only 7% to vegetables. It is manifested by itching, swelling of the lips and tongue, the appearance of red spots or scars on the skin, dermatitis. There may also be signs of the gastrointestinal tract and respiratory apparatus.
5. On nuts, legumes and cereals. In 50% of cases, reactions are so severe that they can even lead to death. This species is the most dangerous when compared with others, because it develops at lightning speed.
In 50% of cases, reactions are so severe that they can even lead to death. This species is the most dangerous when compared with others, because it develops at lightning speed.
There is an allergy to food in a child against the background of:
-
genetic predisposition;
-
reducing the protective functions of the intestinal mucosa;
-
a large amount of food consumed, etc.
In circumstances where tolerance fails, the immune system mounts an IgE antibody response against a particular food. The process begins in the intestines (although it may affect other areas such as the respiratory system or the skin).
When the patient consumes a "dangerous" product, the antigen associated with Ig E is found on the surface of basophils and mast cells. At this time, their activation occurs, and histamine and other inflammatory substances are released.
It manifests itself in the first two hours after eating, if a dangerous factor is included in the diet.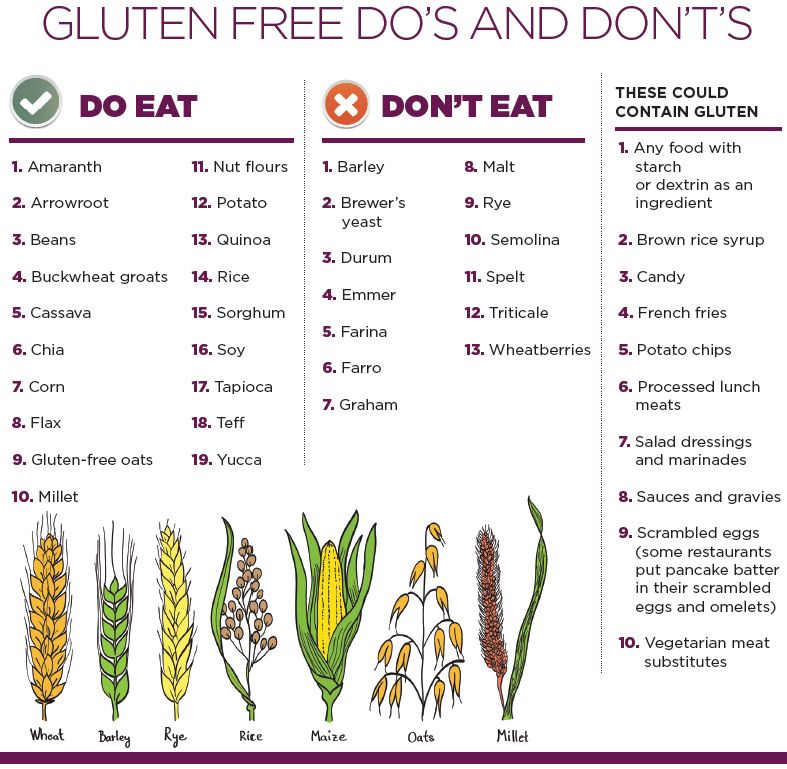 One or more organs are affected, including the skin, gastrointestinal tract, mucous membranes, respiratory and cardiovascular systems. The severity of the course depends on the reactivity of the affected organ, the general well-being of the patient and the characteristics of the factor that causes an atypical response.
One or more organs are affected, including the skin, gastrointestinal tract, mucous membranes, respiratory and cardiovascular systems. The severity of the course depends on the reactivity of the affected organ, the general well-being of the patient and the characteristics of the factor that causes an atypical response.
Main features:
-
Skin manifestations. Urticaria - the appearance of a small rash. Accompanied by redness, itching and peeling. It is localized mainly on the face and neck, hands, forearms and elbows. May be complicated by the addition of a bacterial infection.
-
Respiratory manifestations. Rhinitis is accompanied by nasal congestion, profuse watery discharge and repeated sneezing. In rare cases, a sore throat and coughing join.
-
Respiratory involvement. In patients with asthma, bronchospasm may be present in the context of anaphylaxis (a severe systemic condition). Anaphylaxis is dangerous because, if not adequately treated, it can be fatal.
-
Damage to the digestive tract. Accompanied by diarrhea, abdominal pain, nausea and vomiting. The stool undergoes a change, which most often liquefies.
Other manifestations are itching in the mouth and throat, as well as in the eye area. Difficulty swallowing, dizziness, fainting, swelling of the eyelids, face, lips and tongue are possible.
The danger lies in the fact that this condition is gradually aggravated if time does not take any measures:
1. First, against the background of sensitization, the body develops dermatitis.
2. Then the respiratory system is affected in the form of atopic rhinitis.
3. If the antigen is not excluded, then bronchial asthma manifests.
The most dangerous complication is anaphylactic shock. It develops rapidly - 1-3 minutes after contact with the antigen. It is characterized by bronchospasm, laryngeal edema and collapse, which can be fatal if not treated on time.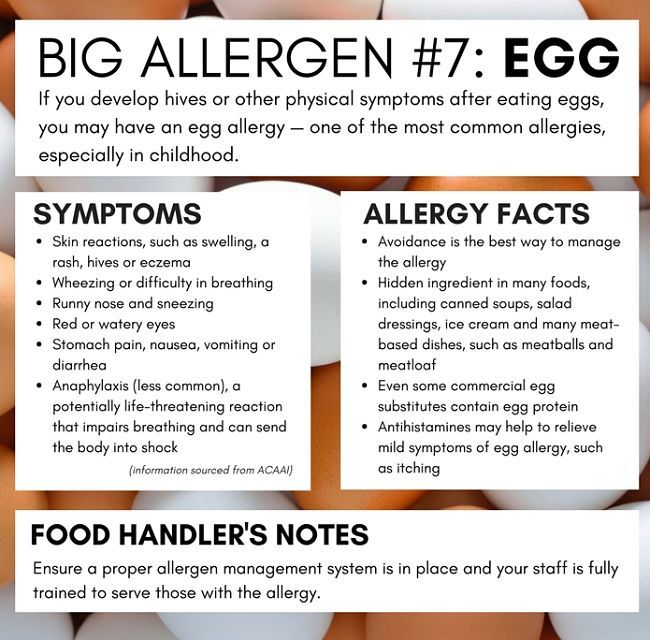
In many cases, people confuse a specific reaction of the body with an individual intolerance. There is definitely some similarity between them, but we are talking about different pathologies. Excessive sensitivity appears after eating as a response of the body, while with intolerance, protective functions do not interfere. The main causes of intolerance are usually metabolic disorders of certain substances.
If signs of hypersensitivity appear, you should immediately consult a doctor. The specialist will collect a detailed medical history to try to establish which factors are "dangerous" and establish a temporal relationship between food intake and the onset of symptoms.
Skin tests in some cases can diagnose a specific reaction. A positive result does not necessarily mean that sensitivity is present, but a negative result indicates that the patient is unlikely to be sensitive to the food. After receiving a positive skin test, an allergist may need to perform an oral follow-up to establish a definitive diagnosis.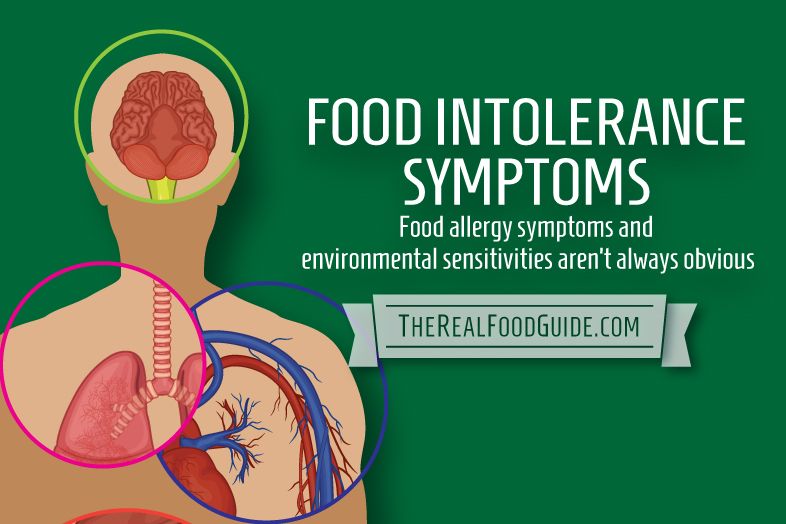
Currently, the only remedy against the negative impact of the provoking factor is the elimination of the dangerous substance from the diet. This recommendation seems simple, but far from reality. Proper diet involves constant monitoring to rule out exposure to present and latent antigens that appear in processed foods. It is recommended to study the composition when meals are prepared outside the home to avoid accidental contact with antigens. Unfortunately, not everyone manages to exclude contact.
In recent decades, special therapies have begun to be developed aimed at changing the immune response and acquiring oral tolerance. These methods are known as oral desensitization or allergy vaccines, which may show promise for specific reactions to milk, peanuts, and eggs. For individualized treatment recommendations, contact your pediatrician or allergist.
Full recovery is possible only with early detection of factors and their exclusion from the diet. If dietary recommendations are followed, recurrence of the disease can be prevented.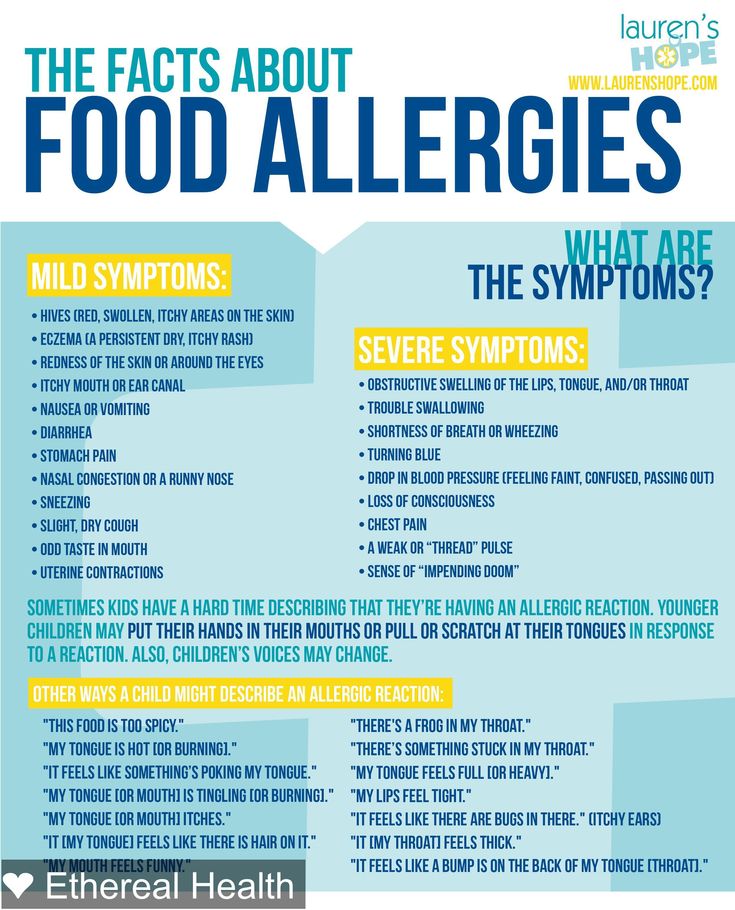 Some children spontaneously recover as oral tolerance increases. Many "outgrow" the disease, but you should not count on it.
Some children spontaneously recover as oral tolerance increases. Many "outgrow" the disease, but you should not count on it.
Our medical center employs more experienced specialists in the field of allergology. Thanks to the modern equipment of the clinic, we conduct a comprehensive diagnosis, determining the true cause. Already after the first visit to the medical center, the result is noticeable.
To talk with a specialist, you can come to the clinic, use an online consultation or call a doctor at home. An allergist will tell you how to treat food allergies in a child and give recommendations on how to prevent the development of complications.
We promptly respond to additions and price changes in the price list. In order to avoid misunderstandings, it is recommended to clarify the full list of services and their cost in the clinic's registry or by calling 8-495-104-35-35.
The price list posted on the site is not an offer. Medical services are provided on the basis of a concluded contract.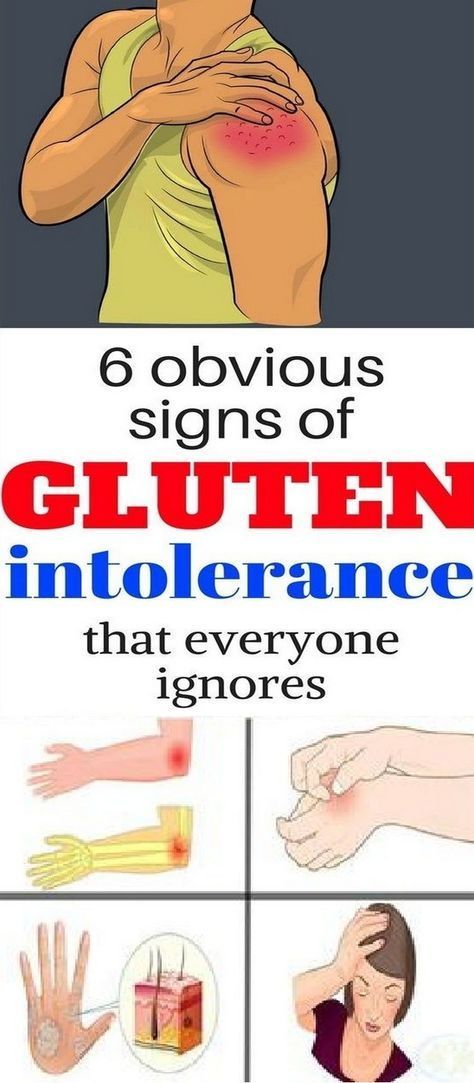
Prevention of food allergies in children
And in the first year of a child's life, food allergies are the most common.
The leading risk factor for the development of allergies in a child is the presence of a burdened heredity in the family. If this is one of the parents, then the chances of getting sick and staying healthy in a child are approximately 50 x 50. At the same time, the likelihood of developing an allergy in a baby is much higher if female relatives are susceptible to it. If both mom and dad suffer from allergies, then the probability of an allergic reaction is already 75%.
A very important risk factor for developing allergies is also nutrition of the expectant mother during pregnancy . Excessive enthusiasm for allergenic products (for example, milk and dairy products), even if the mother herself is not allergic to them, can provoke the development of the disease in the baby both immediately after birth and also in the prenatal period.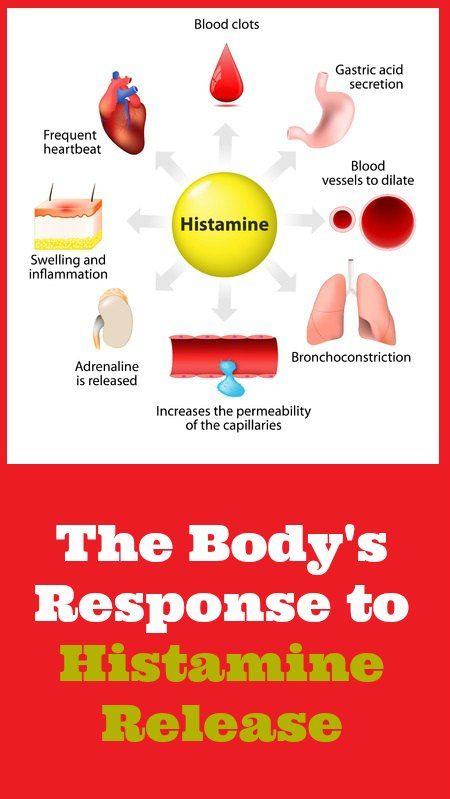
Allergy manifestations in young children
The main manifestations of allergy in children of the first year of life are dermatitis ( itching, redness, peeling, rash, scratching, dryness or weeping of the skin) and dyspepsia - regurgitation, vomiting, loose stools or constipation, increased gas formation, abdominal pain. The baby becomes restless, naughty, often cries, as it seems, for no reason, eats and sleeps poorly. Very rarely, there may be a cough, the appearance of elements of urticaria on the skin, Quincke's edema - swelling of the eyelids, lips or the entire face, larynx. All these violations most often occur within 24-48 hours after the use of an allergenic product. But often the allergy "accumulates" in the child's body, while he eats food that is not suitable for him day after day. In this case, the disease is delayed and manifests itself within 5-7 days, gradually increasing.
Allergenic products
For children of the first half of life who are on artificial and mixed feeding, allergens can be cow and goat milk proteins, soy protein (that is, adapted mixtures made on their basis).
Babies, who are receiving complementary foods , and older children can be allergic to more than obligate allergens ( citrus fruits, strawberries, strawberries, chicken eggs, fish, seafood and caviar, nuts, honey and other bee products, some spices, chocolate), but also quite ordinary products (chicken, veal, beef, wheat and rye flour, vegetables, buckwheat, etc. that do not cause hypersensitivity in other children. Currently, food colorings and flavor enhancers are becoming significant allergens , which are added in the industrial production of food and sweets
Food allergy: treatment or prevention?
Allergy is a chronic disease. Of course, allergies, like any other disease, can be treated . At the same time, it is impossible to completely cure allergies, but long-term remission can be achieved. Treatment is prescribed only by a doctor and includes the identification and removal of the causative allergen, diet, the use of antiallergic drugs, active external therapy using various ointments and creams.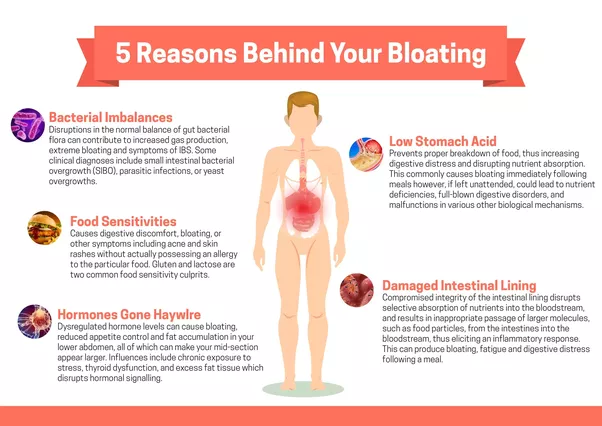
However, the best thing to do is to try to prevent the baby from developing food allergies. And you need to start prophylaxis more before pregnancy , having been examined by an allergist at the slightest suspicion of an allergy. Perhaps the expectant mother will need to take special medications that will prepare her immunity for the birth of a baby. During the period of expectation of the child , it is necessary to avoid not only foods that are unsuitable for the mother, but also to limit any allergenic foods. Today, these include not only traditional citrus fruits and strawberries, but also dairy products, gluten, eggs, fish, soy
Nutrition for mother and baby
After the birth of a baby, the prevention of food allergies consists of several components
When breastfeeding, nutrition of a nursing mother is very important. She should continue to follow the diet and avoid the allergenic foods mentioned above in her diet.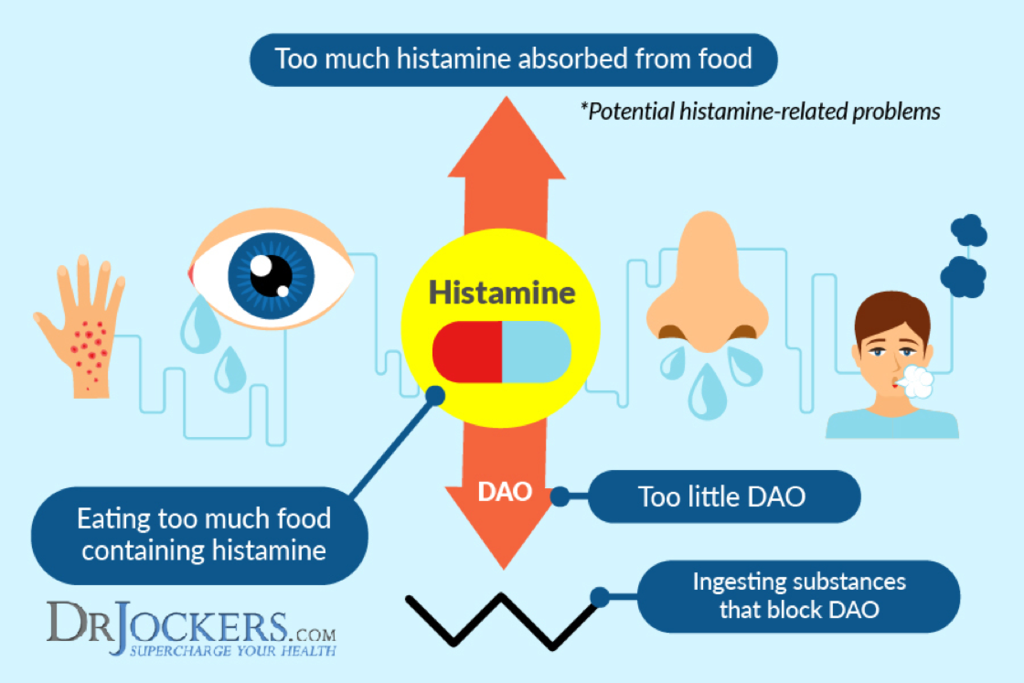
If the child is on artificial or mixed feeding, the following factors must be taken into account when selecting a mixture:
- The bulk of the mixtures are prepared on the basis of whole cow's milk, therefore, in fact, they are obviously ALLERGENIC
- Children at risk for the development of food allergies are prescribed preventive and even therapeutic mixtures in which whole cow protein is subject to partial or complete hydrolysis
- Cow and goat milk proteins are cross-allergic. Therefore, mixtures based on goat's milk are NOT INTENDED for therapeutic nutrition of children with food allergies.
A pediatrician, an allergist-immunologist will help you choose the right breast milk substitute suitable for a particular child. The sooner competent diet therapy is started, the sooner remission will come
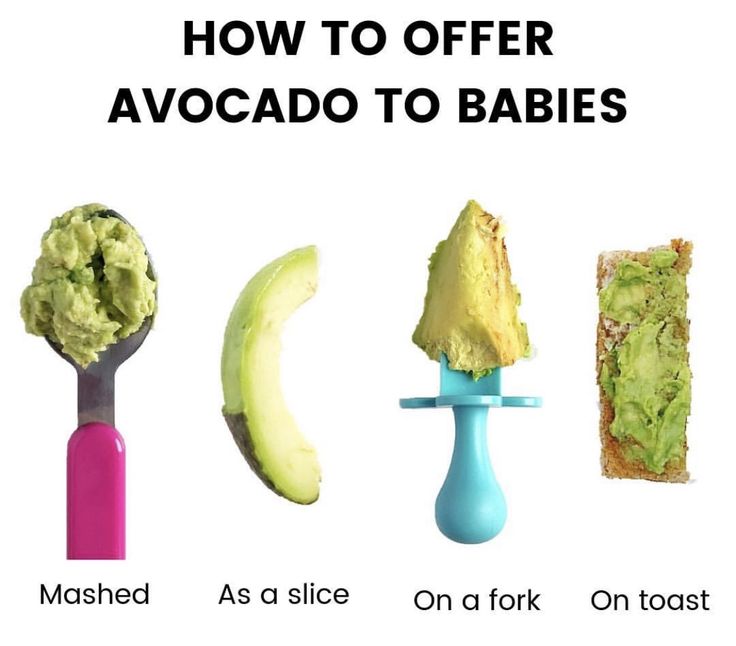
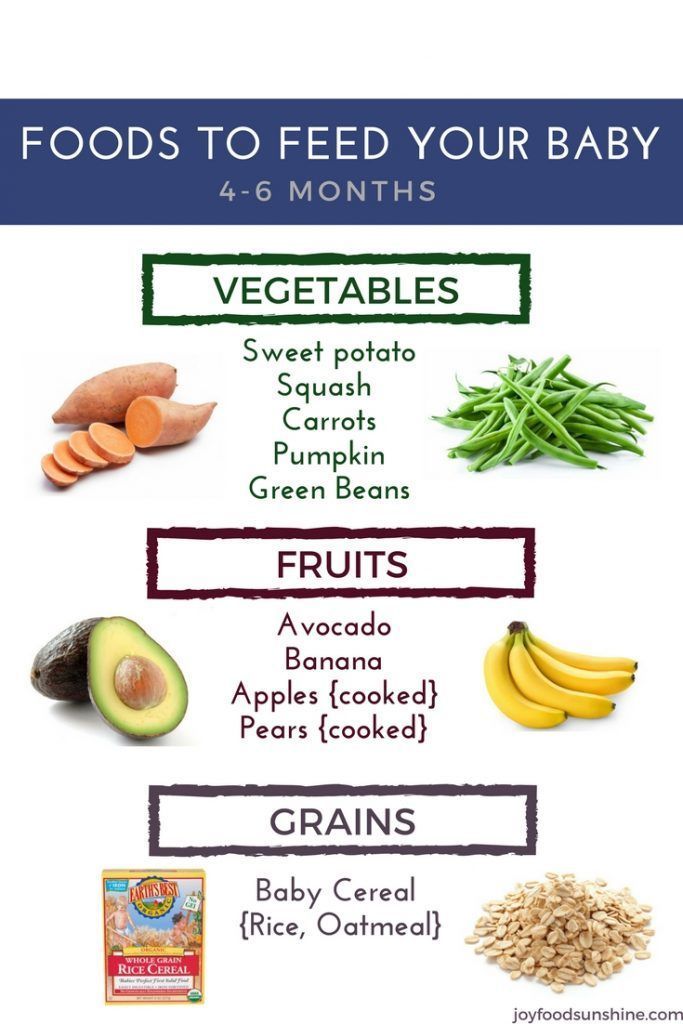
You need to be very careful with the introduction of complementary foods .
Breast-fed babies are recommended to introduce new products after 6 months, and for formula-fed babies from 4 months of age.