What is a food baby belly
Bloated or a food baby? What’s the difference?
Morgan Sandeman, Bupa Accredited Practicing Dietitian and Health Coach says bloating and a full stomach can both:
- Feel uncomfortable
- Make your stomach look bigger
- Worsen throughout the day
- Be exacerbated by meals
- Resolve overnight
But the key difference is bloating doesn’t always happen after eating.
“Bloating is a sensation of tummy swelling that’s sometimes described as the feeling of an inflated balloon in the belly,” she explains. “But feeling full is when someone knows they have consumed a large portion of food or fluid, and the abdomen may be distended making you feel like loosening your pants.”
The old undoing the top button of your jeans after Christmas lunch feeling – you know the one!
Morgan says while your stomach bulging after a meal is likely the result of overeating, the cause of bloating can be harder to pinpoint.
What causes bloating?Research shows at least half of Australian adults experience unpleasant gut symptoms like bloating, gas and constipation.
And for 1 in 7 – it can be distressing.
Morgan says the most common cause of stomach pain and bloating is excess intestinal gas.
“That might be from swallowing air when you eat too fast or drink a lot of carbonated drinks,” says Morgan. “If you get a bloated stomach after eating, it may be a digestive issue.”
“Bloating is often caused by changes in your diet, for example if you have eaten a large portion of rich, fatty or salty food or if you have a low or inconsistent amount of dietary fibre intake on a daily basis.”
Regular bloating can be caused by other problems like:
- Constipation
- Coeliac disease
- Food intolerance (such as gluten, wheat or lactose)
- Irritable Bowel Syndrome (IBS)
- Hormones
- Stress
Most people can prevent bloating with some tweaks to their lifestyle.
“I recommend starting with eating the recommended amount of fibre each day, focusing on including a variety of the three types of fibre. ”
”
That means a mix of:
Soluble fibre: Oats, seeds and fruit and vegetable flesh
Insoluble fibre: Wholegrain breads and cereals, nuts and fruit and vegetable skin
Resistant starch: Banana, pasta, rice, potato, and chickpeas
If you’re not used to eating a lot of fibre, start gradually so that you don’t overwhelm your system.
Yes, that might mean you’ll be tooting a bit more than usual initially.
“But once it starts sweeping through your digestive system, it will help clean out the fermenting faecal matter that’s stuck in there,” says Morgan.
And if that sentence doesn’t stop you reaching for the snacks…
“Fibre also tells your body to drink more water, and it makes you feel full sooner so that you don’t eat too much,” adds Morgan. “And finally, fibre is a prebiotic that helps feed and promote the good bacteria in your gut.”
Processed foods are also big bloaters, because they’re low in fibre but high in salt and fat.
“Salt causes water retention, and fat slows down the digestive process because it takes longer to digest and all of these things can lead to constipation and bloating,” says Morgan. “Processed foods are also low in nutrition, so they will leave you feeling hungrier even after you’ve consumed a lot of calories - this leads to more eating and deepening the problem.”
Morgan also recommends:
- Drinking enough water: To keep your digestive tract working well, preventing constipation.
- Regular exercise: To prevent water retention and keep your bowels moving.
- Eating mindfully: Take your time to chew thoroughly and stop before you are full.
- Noticing sensitivities: Whether it’s alcohol or particular foods, purely paying attention can help you notice which ingredients you are most sensitive to.
Any ongoing bloating is worth looking into. Especially if it:
Especially if it:
- Lasts more than a week
- Is painful
- Is getting progressively worse
- Has other symptoms like fever, vomiting or bleeding
If you’re planning to see doctor or dietitian Morgan says it’s a good idea to keep a diary and track things like:
- The duration of the bloating
- Your regular diet
- Any foods that impact bloating
- The time-of-day symptoms appear or worsen
- Whether stress affects bloating
- If hormones are a factor
- Any associated symptoms
It is possible to be both bloated and full – they’re not mutually exclusive.
So, if you’re regularly eating when you’re not hungry or indulging in unbalanced portions, Morgan recommends practicing the ‘Hunger Level Scale’ or Mindful Eating.
That simply means asking yourself how hungry you really are – and slowing down and enjoying every mouthful.
“Feeling full is a delayed reaction because it takes a while for the food you eat to actually reach your stomach,” says Morgan. “Most people eat enough to be full before they can actually feel that they are.”
How to Treat and Prevent a Bloated Baby Belly
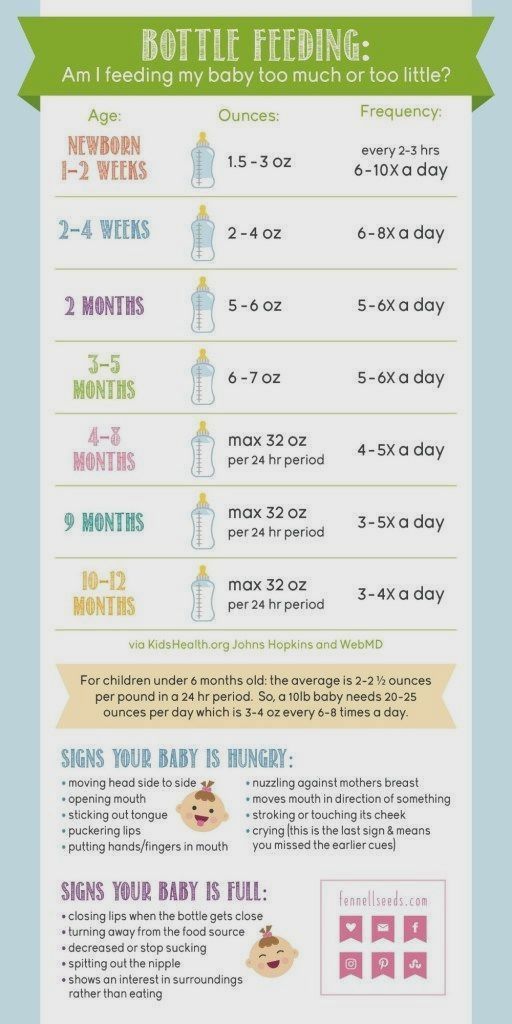
Gas is particularly common in infants between one and four months, as their digestive systems are still developing. Read on to learn more about infant gas relief and effective ways to relieve gas.
Why do babies get bloated bellies?
Many things can result in a gassy baby. Infants often swallow air when they’re crying, sucking a pacifier, and eating (whether milk comes from a bottle or a breast).
Babies can become gassy if they swallow excessive air in the wrong feeding position, if they eat too much, or if they’re constipated. Newborn babies may also have allergies or intolerances to ingredients in formula or breast milk, leading to gas. Furthermore, infants’ digestive systems are still developing and learning to effectively process food, stool, and gas.
Take a quiz
Find out what you can do with our Health Assistant
Foods that make breastfed babies gassy
If you’re breastfeeding, certain gas-inducing foods that you eat may also make your baby gassy. Some foods that can make breastfed babies gassy include:
- Foods rich in fiber, particularly any food that contains bran
- Fruits such as apricots, peaches, prunes, pears, and plums
- Citrus fruits
- Green vegetables such as broccoli, brussels sprouts, artichokes, asparagus, and cabbage
- Starchy vegetables such as potatoes and cauliflower
- Other starchy foods such as corn and pasta
- Dairy products
- Chocolate, carbonated beverages, and caffeine
Effective positions to relieve gas
One of the ways to relieve infant gas is to try holding your baby in different positions. Burping babies helps remove some of the air that babies swallow when eating. Try to use different positions while burping that feel comfortable for both of you. Try one of these three positions to relieve gas:
Try one of these three positions to relieve gas:
- Sit upright and hold your infant against your chest. In this position, your baby’s chin will be on your shoulder while you support them with your hand. Gently pat your baby on the back.
- Hold your infant sitting up across your knee or in your lap. In this position, you will be gently supporting your baby’s head and chest by holding their chin. With the heel of your hand on your baby’s chest, be careful to hold your baby’s chin and not their throat. With your other hand, pat your baby’s back gently.
- Lay your baby face down on your lap. In this position, support your baby’s head and ensure that it’s higher than their chest. Pat their back gently.
Flo was recommended to me by my OB-GYN. It helps me track my periods in order to have better health and does it in a personalized way. It also helps me identify patterns in my daily life activities, from workout patterns to mood trackers. Most importantly, it allows me to understand my body in a better way, according to the data input and analysis.
Most importantly, it allows me to understand my body in a better way, according to the data input and analysis.
Tips to help your gassy baby feel better
Gas can affect both bottle-fed and breastfed babies equally. A frequently gassy baby is usually no cause for concern and quite normal. You can follow certain tips to help relieve your infant’s gas and make them feel better.
1. Change your equipment
If your baby is gassy from bottle-feeding, it might help to try a different kind of nipple and bottle combination. Soft nipples, which contour along your baby’s lips and mouth, can help prevent the accident flow of excess air when your baby is drinking.
Furthermore, the milk should be able to flow slowly and gradually so the baby has enough time to drink without gulping it excessively. While bottle-feeding, it’s best for babies to take between 20 minutes and one hour to finish eating.
If they finish in five minutes, they are gulping too quickly and swallowing excess air. In cases like these, the nipple flow is probably too large for their age. Try switching to a nipple with a slower flow.
In cases like these, the nipple flow is probably too large for their age. Try switching to a nipple with a slower flow.
2. Adjust the feeding position
While bottle-feeding or nursing your infant, adjust their feeding position to prevent a bloated baby belly. Keep their head higher than their stomach.
This position helps the milk move to the bottom of the stomach and the air to the top, which helps the baby burp. You can also use a nursing pillow to provide support and tip the nursing bottle slightly up so that there are no air bubbles in the nipple.
3. Burp your baby
One of the best ways to provide gas relief is to burp your baby as they nurse and after. Instead of burping them while they are feeding, though, wait for them to take a break or slow down.
Otherwise, they may get upset, cry, and swallow more air in the process. Use the burping position that is most comfortable for them.
Massage might also be helpful in relieving gas in your baby.
4. Be careful about foods
To provide your infant with gas relief, talk to their doctor about foods that may cause extra gas. Some fruit juices contain sorbitols or sugar alcohols that babies can’t absorb, causing gas. The doctor will also make sure your baby is getting all the essential nutrients they need.
If you are breastfeeding, foods you’ve eaten can also cause your baby to be gassy. If you give your baby formula, you can try switching brands. Some brands claim to prevent gas.
Reasons to call a doctor
Most of the time, it’s normal for an infant to have gas and it’s treatable. In rare instances, more serious problems of the digestive tract can also cause gas. You should contact the doctor immediately if your infant exhibits any of the following:
- They are vomiting, aren’t passing stools, or have blood in their stools.
- They are extremely fussy. If you aren’t able to calm your baby, a doctor can check to rule out any problems.
- They have a high temperature.
 If the rectal temperature of your baby is 100.4 F ( 38 °C) or more, make sure a doctor rules out an infection. If your baby is younger than three months and has a fever, take them to a doctor immediately.
If the rectal temperature of your baby is 100.4 F ( 38 °C) or more, make sure a doctor rules out an infection. If your baby is younger than three months and has a fever, take them to a doctor immediately.
It is very common for babies to become gassy, and there are a number of reasons for that. Babies swallow air while crying, sucking a pacifier, and eating. Furthermore, babies’ digestive systems are still developing, which can sometimes lead to gas and a bloated belly. A gassy baby may belch, burp, pass gas, and have a hard distended tummy. You can follow certain tips to help relieve gas and make your baby feel better. In rare instances, certain symptoms may indicate a more serious problem. If your baby is experiencing gas along with other, more serious symptoms, get them checked by a doctor.
Enteral nutrition (tube feeding)
What is enteral nutrition?
Sometimes during treatment and recovery, children with cancer cannot get the calories and nutrients they need orally. Tube feeding, or enteral nutrition, provides nutrition in the form of a liquid or mixture given through a tube that is inserted into the stomach or intestines. Some medications may also be delivered through such a tube (probe).
Tube feeding, or enteral nutrition, provides nutrition in the form of a liquid or mixture given through a tube that is inserted into the stomach or intestines. Some medications may also be delivered through such a tube (probe).
Typically, the tube is inserted in two ways:
- Through the nose (non-surgical method)
- Through a small incision in the abdomen (surgical method)
Most commonly used are nasogastric tubes and gastrostomy tubes. But there are several types of enteral feeding tubes that differ in the method of insertion and location in the digestive tract.
Sometimes the patient is simply not able to eat enough calories or protein. There is no fault in this. It is important to help your child understand that nutritional support is not a punishment. Most children get used to the enteral feeding tube quickly. It is important that the child does not touch or pull the phone. Follow skin care instructions at the insertion site to avoid irritation or infection.
A nasogastric tube is inserted into the stomach or small intestine through the nose and throat.
Enteral feeding tube types
Enteral feeding tube connects to the stomach or small intestine. The location depends on how the patient tolerates the formula and how well their body is able to digest the nutrients. If possible, they try to place the probe in the stomach so that digestion occurs naturally.
There are 5 types of enteral feeding tubes:
Nasogastric Tube . A nasogastric tube is inserted into the stomach through the nose. It passes through the throat, esophagus and into the stomach.
Nasojejunal Probe . A nasojejunal tube is similar to a nasogastric tube but passes through the entire stomach into the small intestine.
Gastrostomy Tube (Gastrostomy Probe) . A gastrostomy tube is inserted through a small incision in the skin. The probe in this case passes through the wall of the abdominal cavity directly into the stomach.
Gastrojejunostomy tube (gastrojejunostomy probe) . The gastrojejunostomy tube is inserted into the stomach like a gastrostomy tube, but passes through the stomach into the small intestine.
Jejunostomy Probe . A jejunostomy tube is inserted through a small incision in the skin and passed through the abdominal wall into the small intestine.
Nasal tubes, including nasogastric and nasojejunal tubes, are generally used for short-term enteral feeding, usually not more than 6 weeks. The probe comes out of the nostril and is attached to the skin with adhesive tape. Nasogastric and nasojejunal tubes have a number of advantages, such as a low risk of infection and a simple insertion procedure. However, the probe must be attached to the face, and this worries some children. Other children may have problems with the nasogastric tube due to chemotherapy, which irritates the skin and mucous membranes.
Surgical insertion tubes - gastrostomy tube, gastrojejunostomy tube and jejunostomy tube - are used for longer periods of time or if a nasal tube cannot be placed in the child. The opening in the abdominal wall through which the probe is inserted is called the stoma. A long tube or a "button" (low profile) probe may be visible on the patient's body. After healing, the stoma is usually pain free and the child can perform most daily activities.
The opening in the abdominal wall through which the probe is inserted is called the stoma. A long tube or a "button" (low profile) probe may be visible on the patient's body. After healing, the stoma is usually pain free and the child can perform most daily activities.
-
Insertion of nasogastric and nasojejunal tubes
-
Gastrostomy, gastrojejunostomy and jejunostomy insertion
After healing, the stoma usually does not hurt. The child can perform most daily activities.
Side effects of enteral nutrition
The most common side effects of enteral nutrition are nausea, vomiting, stomach cramps, diarrhoea, constipation and bloating.
There may be other side effects:
- Infection and irritation at the insertion site
- Probe misaligned or falling out
- Lung ingestion of formula
Most side effects can be avoided by following the care and nutrition instructions.
Feeding babies with tubes in place
It is the responsibility of the nutritionist to provide the baby with all the necessary nutrients. In children with cancer, an enteral feeding tube is often used in addition to what the child can eat normally. However, some patients have to enter all the nutrients through a tube.
The patient is prescribed a mixture containing:
- Calories
- Fluid
- Carbohydrates
- Fats
- Protein
- Vitamins and minerals
Standard formulas are suitable for many patients. For babies, it is preferable to use breast milk. Some children need special formulas that take into account their characteristics: the presence of allergies, diabetes or digestive problems.
It is very important for family members to work closely with a nutritionist. Nutritional needs may change due to changes in the child's health or side effects such as vomiting or diarrhea.
Types of enteral feeding
There are three types of enteral feeding - bolus, continuous and gravity.
Bolus feeding - large doses of the mixture are given to the patient by tube several times a day. This species is closest to the usual diet.
Continuous feed - Electronic pump delivers small doses of formula for several hours. Some children may need continuous feeding to reduce nausea and vomiting.
Gravity Feeding - A bag of formula is placed on the IV stand and a predetermined amount of formula is dripped through the tube at a slow rate. The duration of such nutrition depends on the needs of the patient.
Enteral feeding at home
Children can go home with a feeding tube. The doctors will ensure that family members know how to feed and care for the probe. Family members need to pay attention to the following issues:
- Weight gain or loss
- Vomiting or diarrhea
- Dehydration
- Infection
Formulas, Consumables, and Equipment Required:
- Formula: Most enteral formulas are sold ready-made.
 Some are available as a powder or liquid to mix with water.
Some are available as a powder or liquid to mix with water. - Syringe
- Adapter tube (if the child has a button tube for long-term enteral nutrition)
- Pump (with continuous power)
- Feeding formula bag with tubing (for continuous feeding)
- IV Stand (gravity fed)
General tips for enteral feeding at home:
- Always wash your hands with soap and water before feeding your baby.
- Make sure the baby's head is above the stomach.
- Throw away any ready-made or homemade formulas that have been opened and kept in the refrigerator for 24 hours or more.
- Store mixed formulations in the refrigerator and discard after 24 hours.
- Ready-to-use formulas do not need to be refrigerated.
- Do not empty the syringe completely during feeding.
- Wash the syringe (and transfer tube, if used) with warm water and dishwashing detergent after each use.
- Watch for signs of nausea, vomiting, bloating or irritability while feeding.
 If you notice these signs, stop feeding and contact your doctor immediately.
If you notice these signs, stop feeding and contact your doctor immediately. - Check the skin around the injection site for signs of irritation or infection.
-
Modified November 2018
A CHILD HAS A STOMACH
How often do we hear from our children, “Oh, my stomach hurts!”. Children complain in the morning when they are going to kindergarten or school, and in the evening when they go to bed, and during meals with the words “I don’t want to anymore.” At the same time, parents react differently: who runs to call an ambulance, and someone brushes it off, “you always come up with something.” How not to be mistaken, what to do if the child complained about the tummy.
Children rarely lie just like that. Sometimes a child may say that his stomach hurts in order to attract his mother, without even experiencing discomfort in his stomach, but this is still an alarming bell, because he did not complain about his leg, head or something else, which means he periodically experiences pain or stomach discomfort!
Children of preschool and primary school age will complain of pain not only when they experience real pain, but also with flatulence (increased gas formation) and nausea and rumbling in the stomach and discomfort in the stomach. When a child says “I can’t do it any more, my stomach hurts” while eating, do not rush to scold him. He cannot say “I have a feeling of early satiety”, but most likely he has this particular pathological symptom, which occurs with gastritis, functional dyspepsia and other diseases.
When a child says “I can’t do it any more, my stomach hurts” while eating, do not rush to scold him. He cannot say “I have a feeling of early satiety”, but most likely he has this particular pathological symptom, which occurs with gastritis, functional dyspepsia and other diseases.
If your child complains of abdominal pain in the morning, it may not be because of the desire to stay at home, but he has the so-called "fasting pains", one of the signs of gastroduodenitis, peptic ulcer. Or maybe he just doesn't want to have breakfast, and not because he's stubborn, but because his enzymes haven't "woken up" yet. Feeding such children a "full" breakfast is not possible, and it is not necessary. Let the child eat a portion of yogurt with tea, and in kindergarten or at school (i.e. 2 hours after waking up) he will have a second breakfast.
The child may complain about the stomach when he wants to go to the toilet. More often this happens with constipation, when the process of emptying the intestines is painful. It may be that at present defecation in such children is already painless, but earlier, the stool was accompanied by severe pain and the child REMEMBERED this! Now the little (but not necessarily the little) little man has a fear - "it will hurt now."
It may be that at present defecation in such children is already painless, but earlier, the stool was accompanied by severe pain and the child REMEMBERED this! Now the little (but not necessarily the little) little man has a fear - "it will hurt now."
What is abdominal pain and when does it appear. The sensation of pain is the body's response to irritation of pain receptors located in the walls of internal organs (stomach, intestines) or a capsule covering an organ, such as the liver. When stretching the wall, capsule, inflammation, we experience pain. With spasm of the muscular organs, with pain in the abdomen, it is primarily the intestines, the receptors are also irritated and we feel pain. Abdominal pain may be due to irritation of the peritoneum - a sheet of tissue covering the internal organs of the abdomen. This is more often observed in acute surgical pathology, such as appendicitis.
Pain can be acute, when a person feels a "prick", such pain is often compared with a "dagger pain" or dull - aching pain, of moderate intensity.
Pain can be chronic, when a person complains day after day, but not necessarily all the time. The pain can let go and return again, while the degree of intensity can be different from acute cramping to dull, barely distinguishable.
By localization, the pain can be diffuse - when the pain is the whole abdomen and localized, when you can specify the painful point.
Pain may be associated not with a disease of the internal organ, but with damage to the nervous system, both central and peripheral. With a tumor in the brain, pain can be in different places, incl. and in the abdomen, with pain often accompanied by vomiting. With autonomic dysfunction, abdominal pain may be accompanied by pallor of the skin, nausea, vomiting, and cold sweat.
What to do if your child complains of abdominal pain. Firstly, do not panic, talk to the child about how it hurts, where, while not forgetting that young children cannot localize the pain and will often point to the navel, even if they have pain under the ribs. Do not demonstratively neglect the complaint, even if you think that this is an invention of the baby. Talk to him, promise to give a pill, go to the doctor, do an examination. Never frighten a child with a visit to a doctor or any examination, in the future the child may be afraid of medical institutions and will hide complaints from you, which will lead to late diagnosis of the disease.
Do not demonstratively neglect the complaint, even if you think that this is an invention of the baby. Talk to him, promise to give a pill, go to the doctor, do an examination. Never frighten a child with a visit to a doctor or any examination, in the future the child may be afraid of medical institutions and will hide complaints from you, which will lead to late diagnosis of the disease.
If the child complains of abdominal pain, ask when the child last pooped, maybe he is constipated. Parents should daily monitor the defecation of the child, not only the preschooler, but also the younger schoolchild, and at an older age, you should regularly ask your child if he had stool today, what consistency, if there were any impurities (blood, mucus, not digested food). Often parents do not pay attention to such an IMPORTANT physiological process as defecation, but given the frequency, consistency of stool, the presence of impurities, the doctor will be able to prescribe NECESSARY examinations (and not all that are in the arsenal of modern medicine), which will allow you to quickly diagnose and prescribe treatment.