What to do when baby throws up food
Vomiting in children and babies
It's normal for babies and children to vomit occasionally. In most cases, it will last no longer than one to two days and isn't a sign of anything serious.
The most common cause of vomiting in children and babies is gastroenteritis. This is an infection of the gut usually caused by a virus or bacteria, which also causes diarrhoea. The symptoms can be unpleasant but your child will usually start to feel better after a few days.
However, persistent vomiting can sometimes cause your child to become severely dehydrated and occasionally it can be a sign of something more serious, such as meningitis.
This page outlines what to do if your child keeps vomiting and describes some of the common causes of vomiting in children and babies.
If your child has a high temperature, you can also read a separate page about fever in children.
What to do
If your child vomits, you should keep a close eye on them. Trust your instincts and contact your GP immediately if you're worried.
If the cause is just a tummy bug, your child should still be feeling well enough to eat, play and be their usual self. In this case, keep feeding them as normal and offer them regular drinks (see below).
But if they don't seem themself – for example, if they're floppy, irritable or less responsive – they may be seriously ill, so you should get medical help immediately.
When to get medical advice
You should contact your GP if:
- your child is repeatedly vomiting and is unable to hold down fluids
- you think they're dehydrated – symptoms of dehydration can include a dry mouth, crying without producing tears, urinating less or not wetting many nappies, and drowsiness
- their vomit is green or contains blood
- they have been vomiting for more than a day or two
Go to your nearest accident and emergency (A&E) department if your child is vomiting and develops sudden and severe tummy pain, or they're floppy, irritable or less responsive
Call 999 for an ambulance or go to your nearest A&E department immediately if they're vomiting and have a headache, stiff neck and a rash.
Looking after your child at home
In most cases, you can treat your child safely at home. The most important thing you can do is make sure they keep drinking fluids to prevent dehydration.
If your baby is vomiting, carry on breastfeeding or giving them milk feeds. If they seem dehydrated, they will need extra fluids. Ask your GP or pharmacist whether you should give your baby oral rehydration solution.
Oral rehydration solution is a special powder that you make into a drink. It contains sugar and salts to help replace the water and salts lost through vomiting and diarrhoea.
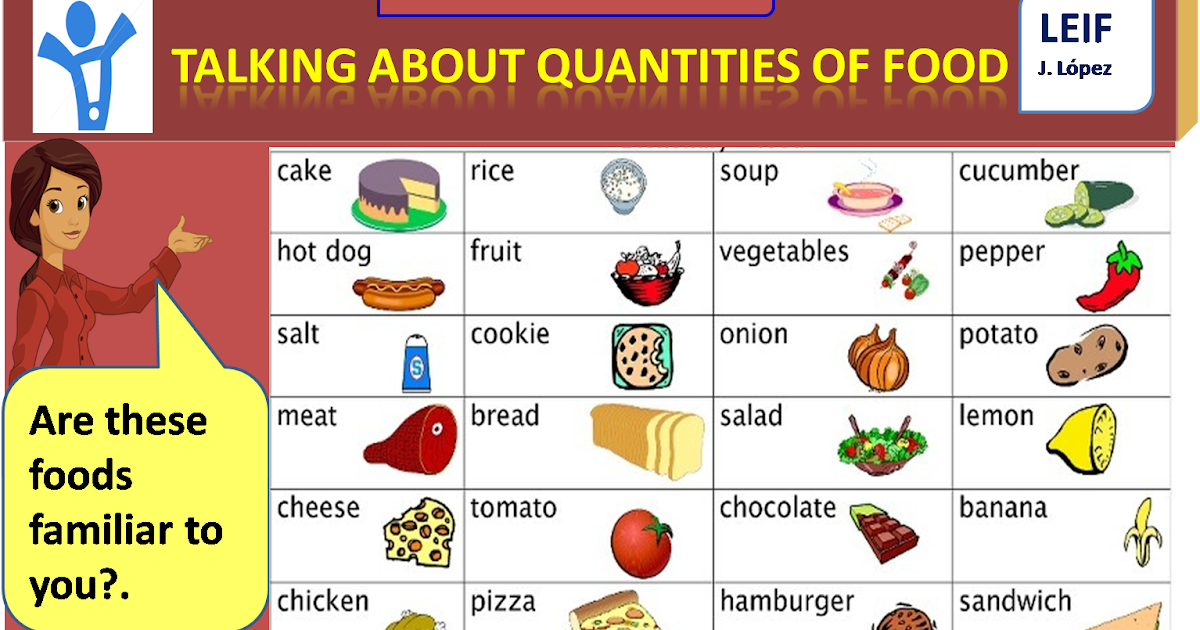
Children who are vomiting should keep taking small sips of clear fluid, such as water or clear broth. Fruit juice and fizzy drinks should be avoided until they're feeling better. If they're not dehydrated and haven't lost their appetite, it's fine for your child to eat solid foods as normal.
Again, speak to your GP or pharmacist if you're concerned about dehydration. They may recommend an oral rehydration solution for your child. Contact your GP or practice nurse if your child is unable to hold down oral rehydration solution.
Contact your GP or practice nurse if your child is unable to hold down oral rehydration solution.
If your child has diarrhoea and is vomiting, they shouldn't go to school or any other childcare facility until 48 hours after the last episode of diarrhoea or vomiting.
Read more about treating gastroenteritis in children.
Causes of vomiting in children
There are a number of possible causes of vomiting in children, which are described below.
Gastroenteritis
Gastroenteritis is an infection of the gut. It's a common cause of vomiting in children and usually lasts a few days.
Food allergy
Food allergies can cause vomiting in children, as well as other symptoms, such as a raised, red, itchy skin rash (urticaria) and swelling of the face, around the eyes, lips, tongue or the roof of the mouth.
Watch out for foods that may bring on vomiting and see your GP for a diagnosis if you think your child may have a food allergy.
Other infections
Vomiting can sometimes be a sign of an infection other than gastroenteritis, such as urinary tract infections (UTIs), middle ear infections, pneumonia or meningitis.
Contact your child's GP if they're vomiting and experiencing additional symptoms of an infection, such as a high temperature (fever) and irritability.
Appendicitis
Appendicitis is a painful swelling of the appendix, a finger-like pouch connected to the large intestine. It causes severe tummy pain that gets worse over time.
If your child has tummy pain that's gradually getting worse, contact your GP, or if they aren't open call NHS 24's 111 service immediately. You should call 999 for an ambulance if they have pain that gets worse quickly and spreads across their tummy.
In most cases of appendicitis, the appendix will need to be surgically removed as soon as possible.
Poison
Accidentally swallowing something poisonous can cause your child to vomit. If you think this is the case, contact your GP immediately or take your child to your nearest accident and emergency (A&E) department.
Causes of vomiting in babies
These include:
- gastroenteritis
- a food allergy or milk intolerance
- gastro-oesophageal reflux – where stomach contents escape back up the gullet
- too big a hole in the bottle teat, which causes your baby to swallow too much milk
- accidentally swallowing something poisonous
- congenital pyloric stenosis – a condition present at birth where the passage from the stomach to the bowel has narrowed, so food is unable to pass through easily; this causes projectile vomiting
- a strangulated hernia – your baby will vomit frequently and cry as if they are in a lot of pain; this should be treated as a medical emergency
- intussusception (where the bowel telescopes in on itself) – as well as vomiting, your baby may look pale, floppy and have symptoms of dehydration
Vomiting (0-12 Months)
Is this your child's symptom?
- Vomiting (throwing up) stomach contents
- Other names for vomiting are puking, barfing and heaving
Causes of Vomiting
- Viral Gastritis.
 Stomach infection from a stomach virus is the most common cause. Also called stomach flu. A common cause is the Rotavirus. The illness starts with vomiting. Watery loose stools may follow within 12-24 hours.
Stomach infection from a stomach virus is the most common cause. Also called stomach flu. A common cause is the Rotavirus. The illness starts with vomiting. Watery loose stools may follow within 12-24 hours. - Food Allergy. Vomiting can be the only symptom of a food reaction. The vomiting comes on quickly after eating the food. Uncommon in infants, but main foods are eggs and peanut butter.
- Coughing. Hard coughing can also cause your child to throw up. This is more common in children with reflux.
- Serious Causes. Vomiting alone should stop within about 24 hours. If it lasts over 24 hours, you must think about more serious causes. An example is a kidney infection. A serious cause in young babies is pyloric stenosis. See below for more on this.
Pyloric Stenosis (Serious Cause)
- The most common cause of true vomiting in young babies.
- Onset of vomiting is age 2 weeks to 2 months
- Vomiting is forceful.
 It becomes projectile and shoots out.
It becomes projectile and shoots out. - Right after vomiting, the baby is hungry and wants to feed. ("hungry vomiter")
- Cause: The pylorus is the channel between the stomach and the gut. In these babies, it becomes narrow and tight.
- Risk: Weight loss or dehydration
- Treatment: Cured by surgery.
Vomiting Scale
- Mild: 1 - 2 times/day
- Moderate: 3 - 7 times/day
- Severe: Vomits everything, nearly everything or 8 or more times/day
- Severity relates even more to how long the vomiting goes on for. At the start of the illness, it's common for a child to vomit everything. This can last for 3 or 4 hours. Children then often become stable and change to mild vomiting.
- The main risk of vomiting is dehydration. Dehydration means the body has lost too much fluid.
- The younger the child, the greater the risk for dehydration.

Dehydration: How to Tell
- The main risk of vomiting is dehydration. Dehydration means the body has lost too much water.
- Vomiting with watery diarrhea is the most common cause of dehydration.
- Dehydration is a reason to see a doctor right away.
- Your child may have dehydration if not drinking much fluid and:
- The urine is dark yellow and has not passed any in over 8 hours.
- Inside of the mouth and tongue are very dry.
- No tears if your child cries.
- Slow blood refill test: Longer than 2 seconds. First, press on the thumbnail and make it pale. Then let go. Count the seconds it takes for the nail to turn pink again. Ask your doctor to teach you how to do this test.
When to Call for Vomiting (0-12 Months)
Call 911 Now
- Can't wake up
- Not moving
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Dehydration suspected.
 No urine in over 8 hours, dark urine, very dry mouth and no tears.
No urine in over 8 hours, dark urine, very dry mouth and no tears. - Stomach pain when not vomiting. Exception: stomach pain or crying just before vomiting is quite common.
- Age less than 12 weeks old with vomiting 2 or more times. Exception: normal spitting up.
- Vomited 3 or more times and also has diarrhea
- Severe vomiting (vomits everything) more than 8 hours while getting Pedialyte (or breastmilk)
- Head injury within the last 24 hours
- Weak immune system. Examples are sickle cell disease, HIV, cancer, organ transplant, taking oral steroids.
- Vomiting a prescription medicine
- Fever over 104° F (40° C)
- Fever in baby less than 12 weeks old. Caution: Do NOT give your baby any fever medicine before being seen.
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Contact Doctor Within 24 Hours
- All other infants (age less than 1 year) with vomiting.
 See Care Advice while waiting to discuss with doctor.
See Care Advice while waiting to discuss with doctor.
Seattle Children's Urgent Care Locations
If your child’s illness or injury is life-threatening, call 911.
- Bellevue
- Everett
- Federal Way
- Seattle
- Virtual Urgent Care
Care Advice for Vomiting
- What You Should Know About Vomiting:
- Most vomiting is caused by a viral infection of the stomach.
- Vomiting is the body's way of protecting the lower gut.
- The good news is that stomach illnesses last only a short time.
- The main risk of vomiting is dehydration. Dehydration means the body has lost too much fluid.
- Here is some care advice that should help.
- Most vomiting is caused by a viral infection of the stomach.
- Formula Fed Babies - May Give Oral Rehydration Solution (ORS) for 8 Hours:
- If vomits once, give half the regular amount of formula every 1 to 2 hours.
- If vomits formula more than once, offer ORS for 8 hours. If you don't have ORS, use formula until you can get some.
- ORS is a special fluid that can help your child stay hydrated. You can use Pedialyte or the store brand of ORS. It can be bought in food stores or drug stores.
- Spoon or syringe feed small amounts. Give 1-2 teaspoons (5-10 mL) every 5 minutes.
- After 4 hours without throwing up, double the amount.
- Return to Formula. After 8 hours without throwing up, go back to regular formula.
- Breastfed Babies - Reduce the Amount Per Feeding:
- If vomits once, nurse half the regular time every 1 to 2 hours.
- If vomits more than once, nurse for 5 minutes every 30 to 60 minutes. After 4 hours without throwing up, return to regular nursing.
- If continues to vomit, switch to pumped breastmilk. (ORS is rarely needed in breastfed babies. It can be used if vomiting becomes worse).
- Spoon or syringe feed small amounts of pumped milk. Give 1-2 teaspoons (5-10 mL) every 5 minutes.
- After 4 hours without throwing up, return to regular feeding at the breast. Start with small feedings of 5 minutes every 30 minutes. As your baby keeps down the smaller amounts, slowly give more.
- Pumped Breastmilk Bottle-Fed Infants - Reduce the Amount per Feeding:
- If vomits once and bottle-feeding breastmilk, give half the regular amount every 1-2 hours.
- If vomits more than once within last 2 hours, give 1 ounce (30 mL) every 30 to 60 minutes.
- If continues to vomit, give 1-2 teaspoons (5-10 mL) every 5 minutes. Only if not tolerating breastmilk, switch to ORS (e.g., Pedialyte) for every 5 minutes for a few hours.
- After 4 hours without vomiting, return to regular feedings. Start with 1 ounce (30 mL) every 30 minutes and slowly increase as tolerated.
- Stop All Solid Foods:
- Avoid all solid foods and baby foods in kids who are vomiting.
- After 8 hours without throwing up, gradually add them back.
- If on solid foods, start with starchy foods that are easy to digest. Examples are cereals, crackers and bread.
- Do Not Give Medicines:
- Stop using any drug that is over-the-counter for 8 hours. Reason: Some of these can make vomiting worse.
- Fever. Mild fevers don't need to be treated with any drugs. For higher fevers, you can use an acetaminophen suppository (such as FeverAll). This is a form of the drug you put in the rectum (bottom).
 Ask a pharmacist for help finding this product. Do not use ibuprofen. It can upset the stomach.
Ask a pharmacist for help finding this product. Do not use ibuprofen. It can upset the stomach. - Call your doctor if: Your child vomits a drug ordered by your doctor.
- Try to Sleep:
- Help your child go to sleep for a few hours.
- Reason: Sleep often empties the stomach and removes the need to vomit.
- Your child doesn't have to drink anything if his stomach feels upset and he doesn't have any diarrhea.
- Return to Child Care:
- Your child can return to child care after the vomiting and fever are gone.
- What to Expect:
- For the first 3 or 4 hours, your child may vomit everything. Then the stomach settles down.
- Vomiting from a viral illness often stops in 12 to 24 hours.
- Mild vomiting and nausea may last up to 3 days.
- Call Your Doctor If:
- Vomits clear fluids for more than 8 hours
- Vomiting lasts more than 24 hours
- Blood or bile (green color) in the vomit
- Stomach ache present when not vomiting
- Dehydration suspected (no urine in over 8 hours, dark urine, very dry mouth, and no tears)
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.

Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Last Reviewed: 03/17/2023
Last Revised: 12/30/2022
Copyright 2000-2023 Schmitt Pediatric Guidelines LLC.
Why does the baby spit up after feeding?
search support iconSearch Keywords
Regurgitation is a common condition in newborns and infants and is most often a normal variant. However, it is not uncommon for parents to worry if their baby is spitting up frequently, believing that it is due to nutritional or health problems in general. Sometimes these fears are not unfounded, and regurgitation really has a pathological origin. What is its cause and when should you really consult a doctor about this?
Regurgitation - Return of a small amount of food (uncurdled or partially curdled milk) from the stomach up the digestive tract: into the esophagus and further into the oral cavity. According to statistics, at least 1 time during the day, at least 50% of babies from 0 to 3 months old can spit up, more than 60% of children 3-4 months old, and in 5% of children spit up continues up to the year 1 .
According to statistics, at least 1 time during the day, at least 50% of babies from 0 to 3 months old can spit up, more than 60% of children 3-4 months old, and in 5% of children spit up continues up to the year 1 .
Regurgitation in newborns is considered a physiological process. It is caused by a number of factors, including:
- Features of the structure of the upper digestive tract in babies
- In newborns and infants up to a year of life, the stomach has a spherical shape. It holds a small amount of food, besides, the release from it into the duodenum is slower in comparison with children after the year 2 .
- Weakness of the lower esophageal sphincter that separates the esophagus from the stomach
- Normally, the lower esophageal sphincter should tightly "close" the esophagus, allowing food to pass into the stomach and not allowing it to enter back into the upper digestive tract. However, in young children (up to a year), the muscles of the esophageal sphincter are poorly developed, and it does not do its job very well 2 .

- Slow movement of food through the gastrointestinal tract
- The neuromuscular system of newborns is immature. It does not ensure the proper movement of food through the esophagus, causing regurgitation.
One of the important risk factors contributing to regurgitation in newborns is aerophagia. This is the swallowing of large amounts of air during feedings. This happens when the baby is not properly attached to the breast, the mother has a lack of breast milk, or the bottle is in the wrong position in the child who receives the mixture. The size of the opening in the nipple also matters - if it is too large, the newborn swallows a lot of air 3 .
With aerophagia, the baby becomes capricious, restless immediately after feeding. Noticeable bloating. If the baby spits up immediately after a feed, the milk (or formula) remains practically fresh, uncurdled 3 .
Promotes regurgitation after feeding and a predominantly horizontal position of the baby during the day, combined with relatively high intra-abdominal pressure 4 . Therefore, the correct position of the baby after feeding is so important. To avoid regurgitation of an excessive amount of stomach contents, after feeding, it is necessary to hold the baby in an upright “column” position for some time (10-20 minutes), lightly patting on the back and allowing excess air to “exit”.
Therefore, the correct position of the baby after feeding is so important. To avoid regurgitation of an excessive amount of stomach contents, after feeding, it is necessary to hold the baby in an upright “column” position for some time (10-20 minutes), lightly patting on the back and allowing excess air to “exit”.
Regurgitation in many newborns can be provoked by other situations in which pressure in the abdominal cavity increases and stomach contents are thrown into the esophagus, in particular 3 :
- tight swaddling;
- stool disorders, in particular constipation;
- long, forced cry and some others.
Want to avoid common feeding problems?
Start with a baby bottle with an anti-colic system that helps you avoid common feeding problems such as colic, gas and spitting up*
How can you tell the difference between normal spitting up and vomiting?
Sometimes regurgitation is considered a manifestation of disorders in the digestive tract of children. Due to the constant reflux of acidic stomach contents into the upper sections, inflammation and other complications may develop, including growth retardation, a decrease in hemoglobin levels, and others. Therefore, it is important for parents to understand where the line is between physiological and pathological regurgitation 1 .
Due to the constant reflux of acidic stomach contents into the upper sections, inflammation and other complications may develop, including growth retardation, a decrease in hemoglobin levels, and others. Therefore, it is important for parents to understand where the line is between physiological and pathological regurgitation 1 .
If the mother is worried that her baby is spitting up, keep track of when this happens and count the total number of spit ups per day. Normally, regurgitation usually occurs after eating (the child burps after each feeding), lasts no more than 20 seconds and repeats no more than 20-30 times a day. With pathology, the problem manifests itself at any time of the day, regardless of when the baby was fed. Their number can reach 50 per day, and sometimes more 1 .
The amount of discharge during regurgitation also matters. With normal, physiological regurgitation, it is approximately 5 - 30 ml. If this volume fluctuates between 50 and 100 ml, it is already defined as profuse vomiting. When the range of the jet of vomit is up to 50 cm, doctors talk about "vomiting a fountain." A variant of atonic vomiting is possible, when the contents of the stomach flow "sluggishly". It occurs with atony of the stomach (decrease in muscle tone of the stomach wall) and disruption of the esophagus 1 .
When the range of the jet of vomit is up to 50 cm, doctors talk about "vomiting a fountain." A variant of atonic vomiting is possible, when the contents of the stomach flow "sluggishly". It occurs with atony of the stomach (decrease in muscle tone of the stomach wall) and disruption of the esophagus 1 .
Vomiting in babies is a warning sign. Doctors are especially alarmed by repeated vomiting, a fountain, with an admixture of bile, in combination with constipation. Vomiting can lead to the development of dehydration, acid-base imbalance and other consequences, therefore, if it occurs, you should urgently contact a pediatrician to find out the cause and begin treatment. A doctor's consultation is necessary if the child is spitting up a lot (more than 15-30 ml at a time), with a frequency of more than 50 episodes per day 1.3 .
Physiological regurgitation: symptoms
Regurgitation in newborns, which is considered a normal variant and does not cause concern to pediatricians 3 :
- usually continues for a certain period of time;
- is characterized by slow, "passive" leakage; if the baby spits up a fountain, it is better to consult a doctor;
- has a sour smell of curdled milk;
- occurs without the participation of muscles - the baby does not strain during regurgitation;
- does not affect the general well-being of the baby.
How to help a newborn who spit up often?
If the baby is healthy, no medication is prescribed for spitting up. To help the child allow simple measures based on lifestyle changes and feeding.
- Frequent feeding of the baby
It is known that the baby is more prone to spit up if his stomach is full. To improve the situation, it is recommended to feed the baby more often, avoiding oversaturation, best of all - on demand 5 .
- Correct feeding technique
Every feeding, the mother must ensure that the baby does not swallow too much air during suckling. When sucking, there should be no loud, smacking, clicking sounds. You also need to control that the baby captures the nipple along with the areola.
- Choosing the right bottle and nipple
If the newborn is bottle-fed and receiving formula, it is important to choose the right bottle and nipple. The hole in it should be such that the milk flows out in drops, and not in a stream. The nipple must not be filled with air
The hole in it should be such that the milk flows out in drops, and not in a stream. The nipple must not be filled with air New Anti-colic bottle with AirFree valve
The AirFree valve prevents air from entering the baby's stomach.
- Baby standing upright after eating
To allow air that has entered the digestive tract during meals to escape, it is important to keep the newborn upright for 10-20 minutes after feeding 4 .
- Ensure the correct position of the baby during sleep
To reduce the negative impact of the acidic contents of the stomach on the esophagus, it is necessary to put the baby to sleep in the supine position. The side or prone position, which many pediatricians used to recommend, is no longer recommended. It was found to be associated with an increased risk of sudden infant death syndrome 5 .
If parents notice alarming symptoms, such as spitting up too often or large volume, etc.
 , it is important to consult a pediatrician without delay. This will allow you to identify the real problem in time and help the baby grow up healthy and happy.
, it is important to consult a pediatrician without delay. This will allow you to identify the real problem in time and help the baby grow up healthy and happy.
References1 Zakharova I. N., Andryukhina E. N. Regurgitation and vomiting syndrome in young children // Pediatric pharmacology, 2010. V. 7. No. 4.
Nagornaya 2900 V., Limarenko M. P., Logvinenko N. G. Experience with the use of domperidone in suspension in young children with regurgitation syndrome // Child Health, 2013. No. 5 (48).
3 Zakharova IN Regurgitation and vomiting in children: what to do? //Pediatrics. Supplement to Consilium Medicum, 2009. No. 3. S. 58-67.
4 Zakharova I. N., Sugyan N. G., Pykov M. I. Regurgitation syndrome in young children: diagnosis and correction // Effective pharmacotherapy, 2014. No. 3. P. 18-28.
5 Vandenplas Y. et al. Pediatric gastroesophageal reflux clinical practice guidelines: joint recommendations of the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN) and the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition (ESPGHAN) //Journal of pediatric gastroenterology and nutrition.
 2009; 49(4): 498-547.
2009; 49(4): 498-547. You are leaving the Philips Healthcare (“Philips”) official website. Any links to third party websites that may be included on this site are provided solely as a convenience to you. Philips makes no warranties regarding any third party websites or the information they contain.
I understand
You are about to visit a Philips global content page
Continue
You are about to visit the Philips USA website.
I understand
Regurgitation in infants
Regurgitation in children of the first year of life. Recommendations for young parents.
Parents have a lot of questions with the birth of a child. Moreover, it has been noted that almost all parents face the most exciting problems regarding the health of the baby, since all of them are mostly physiological, passing as the child grows and the work of all systems of his body becomes established.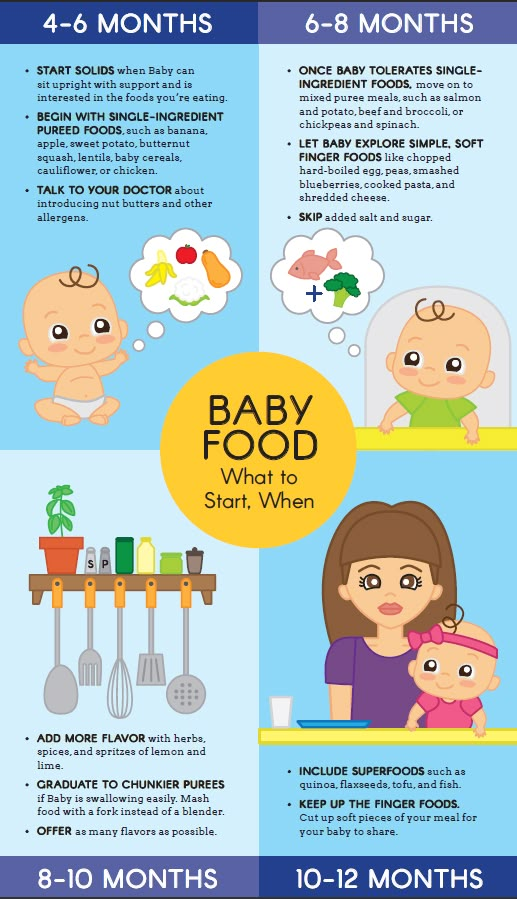 After all, a newborn child is not a small adult, absolutely all the organs and systems of the baby will not only grow in size, but also mature. However, even an understanding of this fact does not reduce the anxiety of parents when any deviations appear in the child's condition, even if they pass over time.
After all, a newborn child is not a small adult, absolutely all the organs and systems of the baby will not only grow in size, but also mature. However, even an understanding of this fact does not reduce the anxiety of parents when any deviations appear in the child's condition, even if they pass over time.
One of these exciting problems is regurgitation in children of the first year of life. According to statistics, a fairly large percentage of all infants, namely from 25% to 80%, have manifestations of the so-called regurgitation syndrome. Moreover, in half of the children, it is stubborn. What is the reason for such a high frequency of this syndrome? And what is it all about - regurgitation?
Regurgitation is the reflux of stomach contents into the mouth shortly after ingestion in infants, predominantly in the first six months of life. There are a number of reasons for the occurrence of regurgitation, both physiological and related to the care and feeding of the baby.
From the point of view of the characteristics of the child's body:
- The stomach is not elongated, as in an adult, but spherical in shape.
- Insignificant volume of the stomach.
- The sphincter (circular muscle), which opens the entrance to the stomach when food passes through the esophagus and closes it at the time of digestion, is rather weak, while the "pylorus", the same muscle, but at the junction of the stomach into the duodenum, is stronger. This feature contributes to the occurrence of regurgitation. A cavity closed on one side arises and with an increase in pressure in the cavity of the stomach, a weak sphincter opens and a reverse reflux of food into the esophagus is formed, and from there the oral or nasal cavity.
- It follows that overfeeding a child or swallowing air during feeding, contribute to an increase in pressure in the stomach, and therefore will inevitably lead to regurgitation.
- The presence of constipation in a child, increased flatulence, bloating can also cause unpleasant symptoms.

Regurgitation:
- Starts suddenly, without any previous symptoms.
- Occur without tension of the muscles of the anterior abdominal wall.
- Not accompanied by pallor, sweating, impaired well-being of the child.
- The child is still active, with a good appetite, and sufficient weight gain.
- Abundant regurgitation. In quantitative terms - from half to the full volume that was introduced in one feeding, especially if this situation is repeated in more than half of the feedings.
- The child has insufficient weight gain. A very formidable sign is the loss of body weight from the original and / or a decrease in the number of urination of the child less than 8 - 10 times a day.

- There are certain symptoms associated with the broncho-pulmonary system, recurrent cough, especially the occurrence of pneumonia in children of the first six months of life.
- The general condition of the child is disturbed.
- Profuse vomiting of previously eaten food with an admixture of bile (the contents of the vomit becomes yellow), especially if the child does not have a stool.
- Pediatrician - Your first assistant, having assessed the condition of the child, will be able to say whether your worries were in vain or it is still necessary to show the baby to others specialists, as well as prescribe treatment, if necessary.
- A neurologist, as a number of neurological problems that occur in a small child can also be accompanied by regurgitation (hydrocephalic syndrome, perinatal damage to the central nervous system).

- Pediatric surgeon. Some of the diseases, one of the signs of which may be vomiting, require emergency surgical intervention (pyloric stenosis, intestinal obstruction).
As usual, we start with the normalization of routine moments:
- Do not overfeed the child, it is better to reduce the single amount of food, but feed more often
- When breastfeeding, make sure that the baby has a good grip on the nipple (together with the areola). Never stop breastfeeding!
- When feeding from a bottle, try to avoid swallowing air when sucking (using special bottles, adjusting the diameter of the hole in the nipple)
- Put the baby on the tummy before feeding
- When feeding, keep the baby in a raised position (not horizontal!), as well as after feeding - the baby should be upright for about 20-30 minutes
- Do not wear clothes that tighten the baby's stomach, avoid sudden movements in relation to the baby in the first half an hour - an hour after feeding, do not put it on the stomach immediately after eating
- If the child spits up in his sleep, when putting him to bed, make sure that the head end of the bed is raised by 10-15 cm.
 so that the baby does not roll over in a dream on his back.
so that the baby does not roll over in a dream on his back.
In addition to regime moments, there are other methods of treating regurgitation in children. All of them are prescribed only by a pediatrician!
- The first of these methods is the prescription of special therapeutic mixtures. These mixtures contain so-called thickeners (starch, locust bean gum), which form a denser food bolus in the stomach, and thereby prevent it from being thrown back into the oral cavity. The choice of mixture depends on many related factors, for example, frequent or rare stools in a child, whether there are signs of lactase deficiency, and so on. The pediatrician, taking into account all the individual characteristics of your baby, will select the necessary mixture. At the same time, you must understand that such treatment, and this is the treatment, will be prescribed for a certain period and in the required amount. That is, only some part of the mixture that your child receives will be replaced with a medicinal one, and upon reaching the results, the baby will return to his usual diet.