What to feed a baby with sickness and diarrhoea
Vomiting and Diarrhea in Children
Am Fam Physician. 2001;63(4):775-776
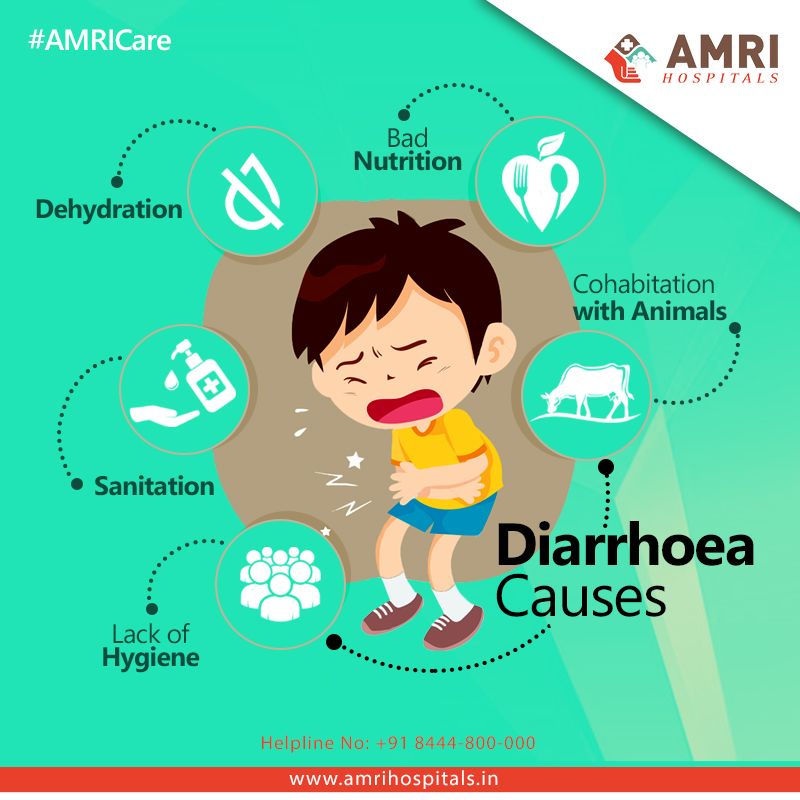
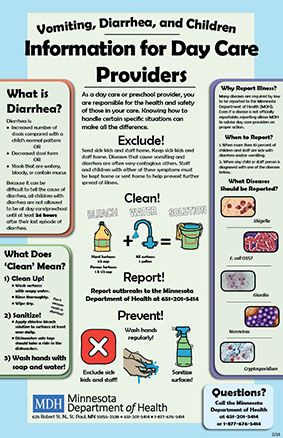
What causes vomiting and diarrhea?
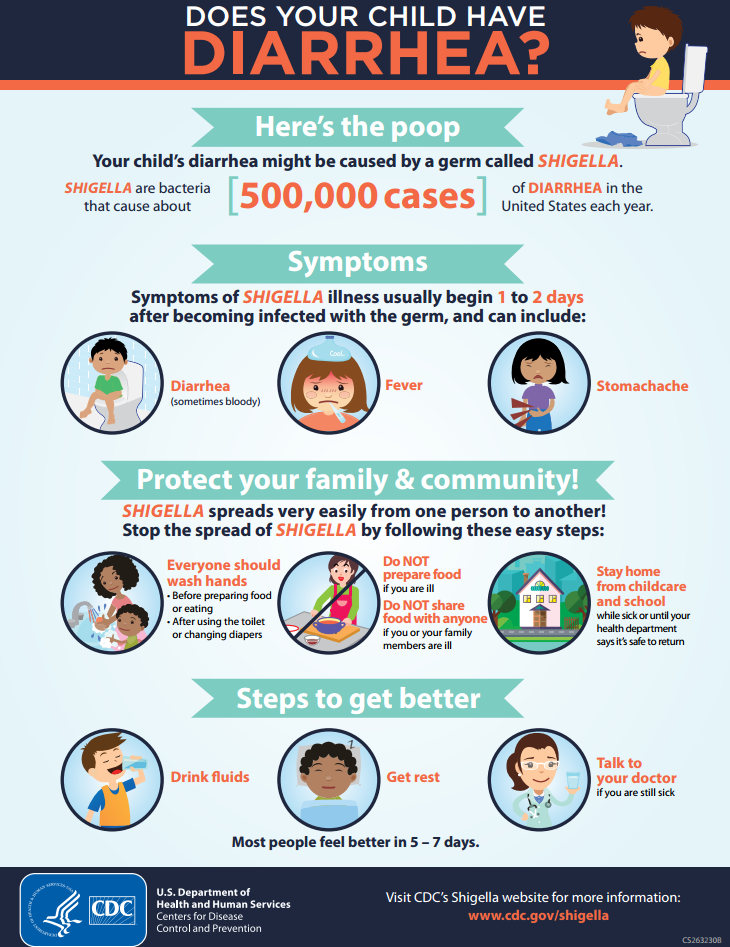
Vomiting (throwing up) and diarrhea (frequent, watery bowel movements) can be caused by viruses, bacteria, parasites, foods that are hard to digest (such as too many sweets) and other things.
Can vomiting and diarrhea be dangerous for children?
They can be. Vomiting and diarrhea can be harmful to children because they can cause dehydration. Dehydration occurs when too much fluid is lost from the body. Young babies can become dehydrated very quickly, but dehydration can occur in a child of any age. Signs of dehydration include:
Irritability
Not eating as well as usual
Weight loss
Not urinating (“peeing”) as often as usual
Urine that is darker than usual
Fast heartbeat
Dry mouth
Thirst (babies may show thirst by crying and being irritable and eager to drink when something is offered)
Sunken eyes
No tears when crying
Sunken soft spot in babies younger than 18 months
Skin that isn't as springy as usual
How can I prevent dehydration?
If your child has had several bouts of vomiting or diarrhea, he or she will need to drink fluids to replace those lost with vomiting and diarrhea. Encourage your child older than two years to drink water and other clear fluids. Ask your doctor about giving your baby or toddler oral rehydration solution (ORS), which contains the right mix of salt, sugar, potassium and other elements to help replace lost body fluids.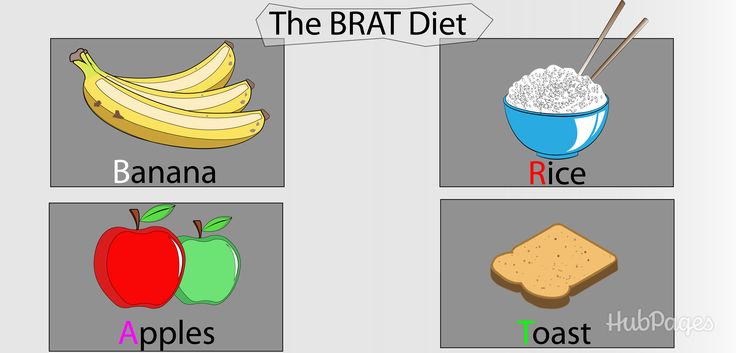
What can I give my older child to drink?
Children older than two years can have drinks such as apple juice, chicken broth, sports drinks (Gatorade), ginger ale or tea. Plain water can cause problems, such as lowering the amount of salt or sugar in the blood.
Should I give my child ORS?
If your child is younger than two years and you are worried that he or she is dehydrated, ask your doctor about using ORS. ORS comes as a powder that you mix with water, or a liquid that is already mixed and as frozen popsicles.
Brands of ORS include Pedialyte, Rice-Lyte, Rehydralyte and the World Health Organization's Oral Rehydration Solution (WHO-ORS). Ask your doctor about which one to use.
Should I feed my child during sickness?
Yes. Even though eating may cause the amount of diarrhea to increase, your child will be able to get some nutrients from the food. This may prevent your child from losing too much weight and help your child get better quicker.
Breast-fed babies.
 If you are breast-feeding, keep breast-feeding while you give ORS.
If you are breast-feeding, keep breast-feeding while you give ORS.Formula-fed babies. If you have been giving your baby formula, some doctors suggest switching from formula to ORS for up to 12 to 24 hours and then switching back to giving formula. Talk to your doctor about what to do.
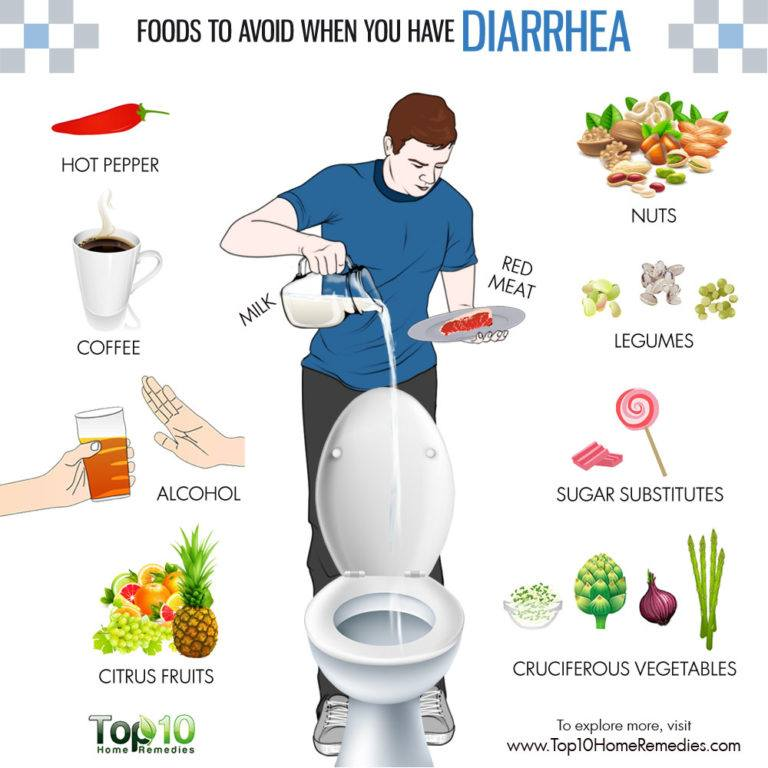
Children on food. Children should begin eating within about 12 to 24 hours after starting to take ORS. Avoid foods with a lot of sugar and fat, such as ice cream, gelatin, pudding and fried foods.
If your child has had diarrhea, dairy products are best avoided for three to seven days. Sometimes bland foods are recommended for the first 24 hours. Foods that are bland include bananas, rice, applesauce, toast and unsweetened cereals. If these foods don't bother your child, other foods can be added over the next 48 hours. Most children can return to normal eating habits in about three days after the vomiting and diarrhea stop.
Should I give my child medicine to stop diarrhea?
This usually isn't needed.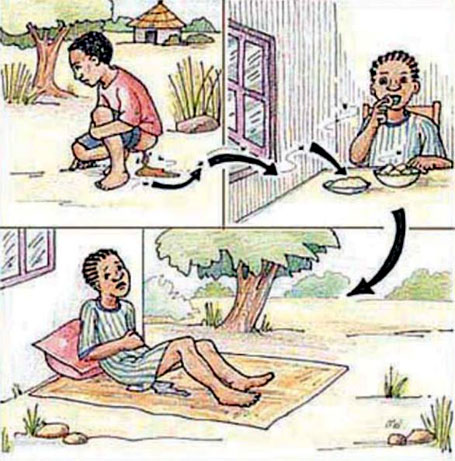 Diarrhea doesn't usually last long. If it is caused by an infection, diarrhea is a way for the body to get rid of the infection. Giving medicines that stop diarrhea may interfere with the body's efforts to get rid of the infection. Antibiotics are usually not necessary either. Talk to your family doctor if you think your child needs medicine.
Diarrhea doesn't usually last long. If it is caused by an infection, diarrhea is a way for the body to get rid of the infection. Giving medicines that stop diarrhea may interfere with the body's efforts to get rid of the infection. Antibiotics are usually not necessary either. Talk to your family doctor if you think your child needs medicine.
Call your doctor if your child is vomiting or has diarrhea and:
Is younger than six months.
Is older than six months and has a fever higher than 101.4°F.
Has signs of dehydration.
Has been vomiting longer than eight hours or is vomiting with great force.
Has stools that are bloody or slimy.
Has blood or green slime in the vomit.
Hasn't passed urine in eight hours.
Could have swallowed something that could be a poison.
Has a stiff neck.
Is listless or unusually sleepy.
Has had tummy pain for more than two hours.
Diet for Vomiting and Diarrhea (Infant/Toddler)
Vomiting and diarrhea are common in babies and young children. They can quickly lose too much fluid and become dehydrated. This is the loss of too much water and minerals from the body. This can be serious and even life threatening. When this occurs, body fluids must be replaced. This is done by giving small amounts of liquids often.
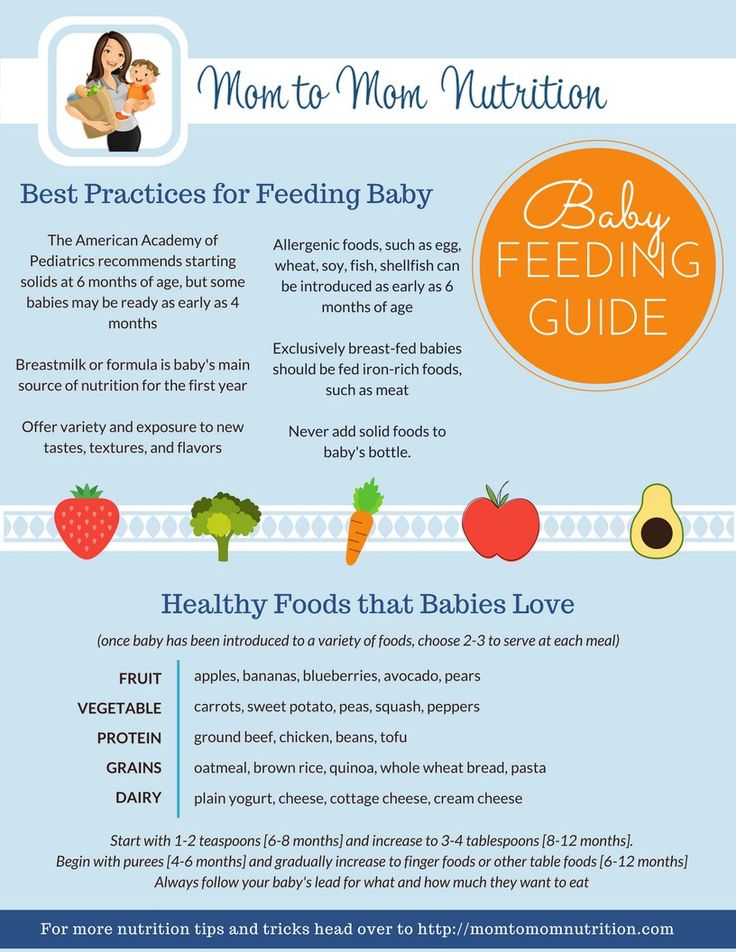
For babies, breastmilk or formula is the best fluid. Breastmilk can help reduce how serious the diarrhea is. But if your child shows signs of dehydration, their healthcare provider may tell you to use an oral rehydration solution. This can replace lost minerals called electrolytes. It can be used in addition to breast or bottle feedings. Oral rehydration solution may also reduce vomiting and diarrhea. You can buy it at grocery stores and pharmacies without a prescription.
In cases of severe dehydration or vomiting, a child may need to go to a hospital to have IV (intravenous) fluids.
Giving liquids and feeding
For breast or formula feedings:
-
Continue the breast or formula feedings. Do this unless your healthcare provider says otherwise.
-
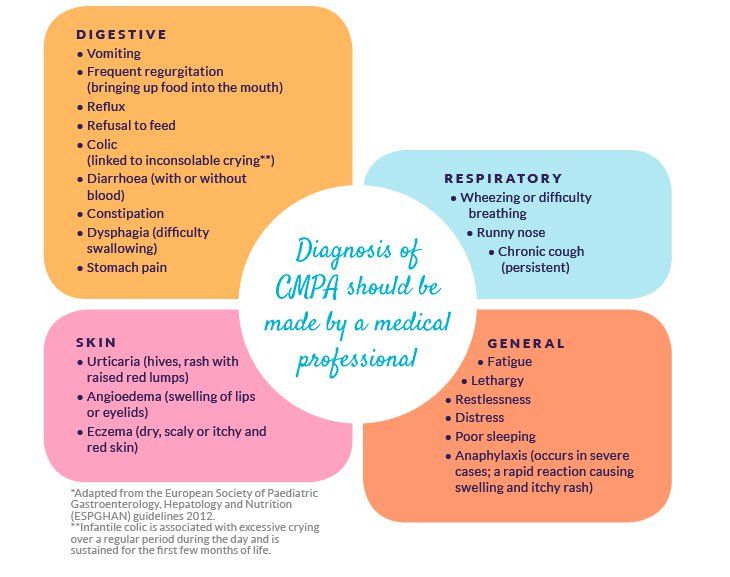
If you use formula, the healthcare provider may tell you to try a different kind of formula. A common cause of vomiting in newborns is a problem with formula.
-
Give your baby short, frequent feedings. Feed every 30 minutes for 5 to 10 minutes at a time over a period of 2 to 3 hours. This will help give your baby more fluids.
-
If vomiting or diarrhea doesn't stop, the provider may tell you to give a formula with no lactose, or low lactose.
 Lactose is a milk sugar that can be hard to digest. Follow the provider's advice about what type of formula to give your baby.
Lactose is a milk sugar that can be hard to digest. Follow the provider's advice about what type of formula to give your baby.
If using oral rehydration solution:
-
Follow the healthcare provider's instructions when giving the solution to your baby. Oral rehydration solution may be alternated with breast or formula feedings.
-
Use only prepared, purchased oral rehydration solution. Don't make your own solution.
-
Give your baby short, frequent feedings. Feed every 30 minutes for 2 to 3 hours. This will help replace lost electrolytes.
-
If vomiting or diarrhea gets better after 2 to 3 hours, you can stop the oral rehydration solution. Resume breastmilk or full-strength formula for all feedings.
For children on solid foods:
-
Follow the diet your child's healthcare provider advises.
-
If desired and tolerated, your child may eat regular food.
-
If unable to eat regular food, your child can drink clear liquids such as water, or suck on ice chips. Don't give high-sugar fluids such as juice or soda. Give small amounts of food and drink often.
-
If clear liquids are tolerated, slowly increase the amount. Alternate these fluids with oral rehydration solution as your healthcare provider advises.
-
Your child can start a regular diet 12 to 24 hours after diarrhea or vomiting has stopped. Continue to give plenty of clear liquids.
Follow-up care
Follow up with your child’s healthcare provider, or as advised. If a stool sample was taken or cultures were done, call the healthcare provider for the results as instructed.
Call 911
Call 911 if your child has any of these symptoms:
When to get medical advice
Call your child’s healthcare provider right away if any of these occur:
-
Fever (see "Fever and children" below)
-
Belly (abdominal) pain that gets worse
-
Constant lower right abdominal pain
-
Repeated vomiting after the first 2 hours on liquids
-
Occasional vomiting for more than 24 hours
-
Continued severe diarrhea for more than 24 hours
-
Blood in vomit or stool (black or red color)
-
Refusal to drink or feed
-
Dark urine or no urine for 8 hours, no tears when crying, sunken eyes, or dry mouth
-
Fussiness or crying that can't be soothed
-
Abnormal drowsiness
-
New rash
-
More than 8 diarrhea stools in 8 hours
-
Diarrhea lasts more than 1 week on antibiotics
Fever and children
Use a digital thermometer to check your child’s temperature. Don’t use a mercury thermometer. There are different kinds and uses of digital thermometers. They include:
Don’t use a mercury thermometer. There are different kinds and uses of digital thermometers. They include:
-
Rectal. For children younger than 3 years, a rectal temperature is the most accurate.
-
Forehead (temporal). This works for children age 3 months and older. If a child under 3 months old has signs of illness, this can be used for a first pass. The provider may want to confirm with a rectal temperature.
-
Ear (tympanic). Ear temperatures are accurate after 6 months of age, but not before.
-
Armpit (axillary). This is the least reliable but may be used for a first pass to check a child of any age with signs of illness.
 The provider may want to confirm with a rectal temperature.
The provider may want to confirm with a rectal temperature. -
Mouth (oral). Don’t use a thermometer in your child’s mouth until they are at least 4 years old.
Use the rectal thermometer with care. Follow the product maker’s directions for correct use. Insert it gently. Label it and make sure it’s not used in the mouth. It may pass on germs from the stool. If you don’t feel OK using a rectal thermometer, ask the healthcare provider what type to use instead. When you talk with any healthcare provider about your child’s fever, tell them which type you used.
Below are guidelines to know if your young child has a fever. Your child’s healthcare provider may give you different numbers for your child. Follow your provider’s specific instructions.
Fever readings for a baby under 3 months old:
Fever readings for a child age 3 months to 36 months (3 years):
-
Rectal, forehead, or ear: 102°F (38.
 9°C) or higher
9°C) or higher -
Armpit: 101°F (38.3°C) or higher
Call the healthcare provider in these cases:
-
Repeated temperature of 104°F (40°C) or higher in a child of any age
-
Fever of 100.4° F (38° C) or higher in baby younger than 3 months
-
Fever that lasts more than 24 hours in a child under age 2
-
Fever that lasts for 3 days in a child age 2 or older
© 2000-2022 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.
Was this helpful?
Yes No
Tell us more.
Check all that apply.
Wrong topic—not what I was looking for.
It was hard to understand.
It didn't answer any of my questions.
I still don't know what to do next.
Other.
NEXT ▶
Last question: How confident are you filling out medical forms by yourself?
Not at all A little Somewhat Quite a bit Extremely
Thank You!
Diet for diarrhea in a 1-year-old child
When a child is sick, it is always a serious test for a family. Moreover, if the baby has vomiting, frequent loose stools, fever, he refuses to eat. In such cases, parents naturally face the question: what to do?
Moreover, if the baby has vomiting, frequent loose stools, fever, he refuses to eat. In such cases, parents naturally face the question: what to do?
The first thing to do is to see a doctor. In most cases, this condition is associated with an acute intestinal infection and can lead to serious consequences for the baby. And timely treatment allows you to quickly deal with the problem.
The second significant issue facing the parents of a sick child is the issue of proper nutrition. Unfortunately, you can still find recommendations to stop feeding a child during diarrhea, but this should not be done categorically.
Important!
It has been proven that "water-tea" breaks and starvation diets significantly weaken the protective functions of the child's body and lead to a delay in recovery processes in the intestines. Therefore, at present, most pediatricians insist on the mandatory continuation of the child's nutrition in case of acute intestinal infections, but with the obligatory consideration of the latest achievements in nutrition.
The main principles for managing the nutrition of a child with diarrhea should be:
| Phased | The development of the disease has a staging, each stage must correspond to certain approaches to diet therapy |
| Accounting for the age of the child | Each age should have its own products and its own schemes for their purpose |
| Accounting for the severity of the disease |
There are three main stages of diet therapy. The first stage corresponds to the acute period of the disease, when the maximum manifestations of the disease are noted (vomiting, loose stools, fever), and the child may refuse his usual diet. During this period, proper nutrition is an integral part of treatment. And the success of treatment largely depends on the correct organization of diet therapy in a child.
The second stage is the recovery period. There are no longer those manifestations of the disease that were noted in the baby in the acute period, the child has an appetite, he becomes more active, but it must be remembered that any acute intestinal infection leads to significant changes in the child's body. This is a violation of the microflora of the gastrointestinal tract, and dysfunction of enzyme systems, bile secretion and other digestive processes. It takes time to restore the correct functioning of the gastrointestinal tract, which requires a sparing diet at this stage. Violation of the diet during this period can lead to the formation of a chronic pathology of the gastrointestinal tract.
There are no longer those manifestations of the disease that were noted in the baby in the acute period, the child has an appetite, he becomes more active, but it must be remembered that any acute intestinal infection leads to significant changes in the child's body. This is a violation of the microflora of the gastrointestinal tract, and dysfunction of enzyme systems, bile secretion and other digestive processes. It takes time to restore the correct functioning of the gastrointestinal tract, which requires a sparing diet at this stage. Violation of the diet during this period can lead to the formation of a chronic pathology of the gastrointestinal tract.
The third stage of diet therapy is aimed at a gradual transition to the usual diet for this baby. Breastfed babies should continue to breastfeed. If the baby is bottle-fed, the doctor will prescribe a formula that matches the baby's condition. In children older than one year, it is necessary to exclude whole milk from the diet, they are also shown the appointment of fermented milk products as a diet therapy, the favorable properties of which are due to a number of positive qualities: the presence of lactic acid gives the product pronounced bactericidal properties and inhibits the growth of pathogenic microflora, the positive effect of these products on intestinal microbiocenosis, the secretory function of the digestive glands and intestinal motility, and they also have immunomodulatory properties.
One of the important components of diet therapy is the use of dairy-free cereals with pro- and synbiotics. Clinical studies have shown that the appointment of this diet therapy contributes to a more rapid relief of the main symptoms of intestinal dysfunction, as well as the restoration of intestinal microflora.
Choose foods for the diet
It is most correct to start with rice porridge, as it has pronounced sorption properties and helps to stop diarrhea. As the child recovers, oatmeal and buckwheat porridge can be included in the diet.
Vegetables and fruits are an important component in the first stage of diet therapy. Preference should be given to products that contain pectin (baked apple, boiled carrots), as they contribute to the sorption of pathogens and their toxins. At the first stage of diet therapy, the use of fresh vegetables and fruits, as well as juices, is not shown.
The second stage - the patient's condition improves, the child becomes active, appetite improves, and in some children it even becomes elevated, which is often perceived by parents as a signal for increased nutrition.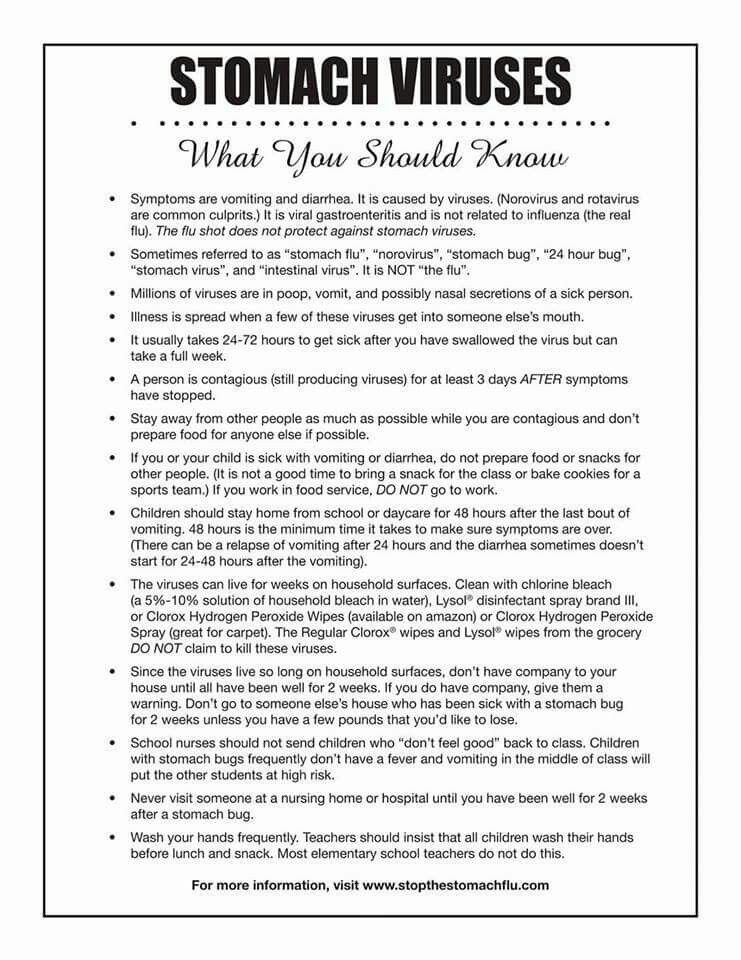 It is absolutely impossible to do this, since the child's body has not yet recovered from the disease. During this period, it is necessary to continue eating sour-milk, lactose-free and low-lactose products. An obligatory component of diet therapy is the use of nutrition with probiotics.
It is absolutely impossible to do this, since the child's body has not yet recovered from the disease. During this period, it is necessary to continue eating sour-milk, lactose-free and low-lactose products. An obligatory component of diet therapy is the use of nutrition with probiotics.
The third stage is the gradual expansion of the diet according to the age of the child. At this stage, the most justified is the widespread use of probiotic foods in order to restore and maintain the function of the gastrointestinal tract and its microbiocenosis.
What to feed a child with diarrhea at first?
- freshly cooked rice;
- bananas;
- natural apple juice;
- boiled potatoes;
- boiled chicken meat;
- crackers and stale bread;
- lean fish;
- weak tea.
how to treat and what to feed? How to treat dehydration in a child
You carefully followed the preventive measures - washed your hands and fruits, watched the shelf life of food, but the child still caught diarrhea and vomiting.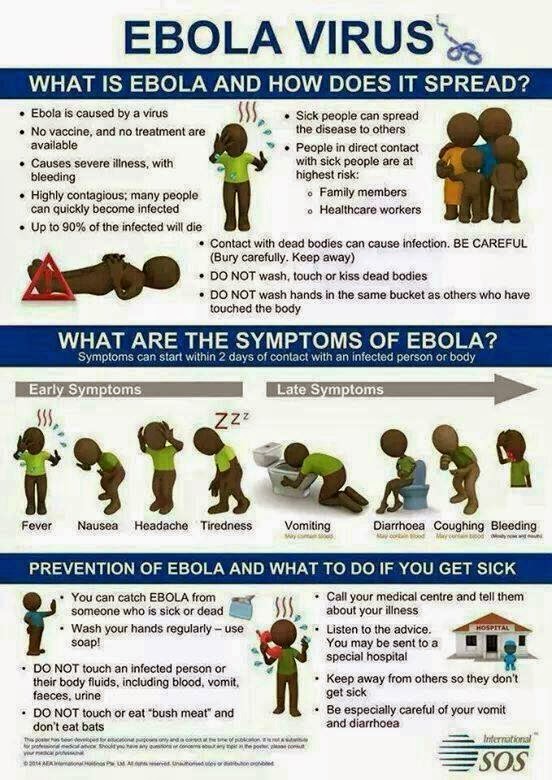 How to treat an intestinal infection or poisoning? How to compensate for dehydration in a child? What diet to follow during illness? Says blogger Dr. Daria.
How to treat an intestinal infection or poisoning? How to compensate for dehydration in a child? What diet to follow during illness? Says blogger Dr. Daria.
The main treatment for intestinal infections is to correct the dehydration that may result from vomiting or diarrhea.
Signs of dehydration (when the situation is close to critical):
- the child pees less than once every 4-6 hours;
- cries without tears;
- the fontanel sinks in the baby;
- dry tongue and mouth;
- severe drowsiness;
- decrease in skin elasticity when the collected fold does not straighten out for a long time.
Antivirals are generally ineffective in these situations, interferons are not proven effective, and antibiotics should only be prescribed by a doctor if infection is confirmed. You need to understand that the independent and uncontrolled prescription of antibiotics can increase diarrhea, and in the future, immunity to certain types of antibiotics will form, and there will be nothing to treat.
Antimicrobials stand apart, they are also called intestinal antiseptics. Usually they are not absorbed from the intestines, they are quite safe and can be used on their own in acute situations when you are on a trip and do not know the cause of the disease: poisoning or a viral infection. Such drugs will work well for food poisoning, but personally I prefer to start and most often be limited to sorbent therapy. In viral infections, intestinal antiseptics are ineffective.
How to treat a child with diarrhea and vomiting
- Correction of dehydration - replenishment of fluid, glucose, sodium salts, chlorine, which are primarily needed for the functioning of the most important systems: cardiovascular and nervous. Drinking with water, strongly diluted compote. If any intake of liquid causes vomiting, you have to drink from a spoon or from a syringe, little by little, but often.
It is not necessary to deny breastfeeding to babies, but try to combine it with drinking clean water, since breast milk is still food and can provoke vomiting more.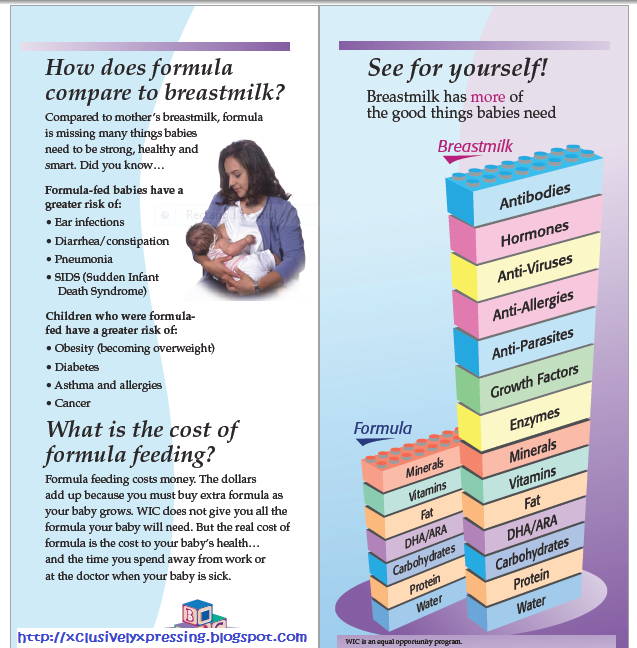
"He doesn't drink water", "I can't do it" - what to say to these parents' excuses? You need to understand that the state of severe dehydration is life-threatening, especially for babies, in whom a critical condition can occur very quickly. Therefore, if you cannot cope on your own, call an ambulance, and instead of drinking, you will be offered an intravenous drip of liquid.
There are ready-made preparations for replenishing the water-salt balance. For adults, Regidron is traditionally used, but for children under 3 years old this is not the best option, since for babies it contains too much sodium, and this is a risk of developing vascular disorders and increasing diarrhea.
So-called low-osmolar solutions have been developed for children: Biogaya, Regidron Bio, Hydrovit (there are other preparations, but they have disadvantages - they contain chemical flavors or potential allergens (carrots), which are toxic with excessive use of herbs, such as fennel).
- Sorbents intake.
 These are substances that absorb and collect toxic metabolic products during poisoning. In evidence-based medicine, it is believed that taking such drugs shortens the time of diarrhea by about a day, but it seems to me that this is not bad, especially since, according to my observations, very often you can get by with only sorbents and no more drugs will be needed.
These are substances that absorb and collect toxic metabolic products during poisoning. In evidence-based medicine, it is believed that taking such drugs shortens the time of diarrhea by about a day, but it seems to me that this is not bad, especially since, according to my observations, very often you can get by with only sorbents and no more drugs will be needed.
Sorbents also have a fixative property, which is valuable in intestinal disorders.
Be sure to follow the rules of taking: the sorbent is taken at least one hour before meals and 1.5–2 hours after. The more pronounced the problem of diarrhea, the more often the sorbent can be taken, observing the dosages by age or weight.
- Taking medications to restore intestinal microflora . Unfortunately, it is very difficult to predict which drug is suitable for whom and whether it will work, since the intestinal microflora is different for everyone, it is also difficult to prove the effect, but it is not forbidden to try to use them.
 But not in one go with sorbents.
But not in one go with sorbents. - Antipyretics are used as needed. Please note that if the intestinal problems are associated with a virus, then by bringing down the temperature below 38.5 °, you lengthen the recovery time.
- Antispasmodics. Drugs that reduce cramps and pain in the abdomen are best taken after a doctor's examination, since when used independently, you can mask the signs of dangerous diseases similar to infectious diseases, such as appendicitis.
How to eat in case of poisoning or intestinal infection
The main purpose of the diet for acute intestinal problems:
- maximum mechanical, chemical and thermal respect for the gastrointestinal tract, reduction of fermentation processes;
- food must have enveloping, absorbent, astringent properties;
- food should be mashed, without coarse fibers that stimulate motor skills;
- food is warm, but neither cold nor hot;
- food intake should not require large enzyme costs (in case of poisoning, the pancreas produces fewer enzymes), give a load on the liver (fatty, fried, spicy).
 Strict exclusion of all variants of dairy and sour-milk products.
Strict exclusion of all variants of dairy and sour-milk products.
My tips for eating on poison days:
- Listen to yourself or observe your child's needs. If you do not feel like eating, then in the first days of the acute period - only sorbents and drinking with electrolyte mixtures.
- If you are still hungry and eating does not cause frequent stools and vomiting, follow the food requirements above.
- Enter products in a specific order.
- Slowly, within 2 weeks, return to your usual diet. Why smoothly, if you want cucumbers and cutlets? In order not to undermine the digestive organs that are working at the limit, otherwise the inflammatory process may become chronic or last longer.
Accordingly, you will no longer absorb and synthesize vitamins, the incoming food will be digested worse, forming allergization, skin problems.
- An ideal product for digestion is cereals, in our case polished white rice, buckwheat, oatmeal.
 Grated, boiled for a long time in water. Cereals better contribute to the restoration of microflora.
Grated, boiled for a long time in water. Cereals better contribute to the restoration of microflora.
If you feel sick and vomit or cereals stagnate in the stomach for a long time, causing heaviness (and there is hunger), you can eat fast-carbohydrate, starchy foods: wheat crackers, dryers, instant baby cereals (buckwheat, rice), mashed potatoes (sweet potato, parsnip) , starchy non-acidic jelly. They are better for assimilation, worse for microflora.
- Drink tea, cocoa without sugar and additives, eat blueberries. These foods are rich in tannin, which has astringent properties. However, do not overdo it: tannin also dehydrates. From herbs, St. John's wort or chamomile is quite suitable.
- Refined sugar is undesirable, as it stimulates the growth of "bad" microflora, but in small quantities, for example, it is present in electrolyte mixtures.
How to feed a child after poisoning
The general scheme of nutrition is something like this:
Days 1-3 — fasting with desoldering, or rice-cereals (ideal) or fast-carb options — drying, starchy jelly.
4-5th day - cereals, you can try some boiled vegetables.
6-7th day - cereals and thermally processed vegetables.
8-9th day - you can add a baked apple, egg white.
10-11th day - fish, some seasonal fruits.
12-14th day - optional legumes, meat, seeds, nuts.
I consciously do not include milk, but if you really like dairy products, then include them also after the 14th day.
And now I'll give you a couple of recipes so you don't get bored when you're sick.
Blueberry jelly
Pour 30 g of blueberries with water, boil for 10–15 minutes, insist on low heat, strain, add sugar, boil. 10 g of potato starch, diluted with cold water, without letting it boil, remove from heat and add a couple of drops of lemon.
Kissel can be poured over pudding made from semolina frozen in a mold.
Boiled rice meatballs
Egg white option (if quick recovery) for days 4-6.
Rinse the rice, boil as much as possible, mix with whipped protein, put in a mold and cook in a steam or oven.