When does the baby start feeding from placenta
When does the placenta form, and what does it do? Learn all about the placenta.
One of the many remarkable things about pregnancy is that you're not only growing a new human being, but also an entirely new organ. And pretty much everything your baby needs to develop and thrive flows through it. Find out all about the amazing placenta, including when it forms and what it does.
What is the placenta?
The placenta is a pancake-shaped organ that develops within the wall of your uterus and connects to your baby though the umbilical cord. By the end of pregnancy, it grows to be about 9 inches in diameter and about an inch thick at the center.
What does the placenta do?
- It delivers oxygen and nutrients (such as vitamins, glucose, and water) from your body to the baby's, and processes the waste products from your baby.
- It produces the hormones that help your baby grow and develop.
- It allows antibodies to pass to your baby from your bloodstream.
These antibodies protect against certain bacterial infections and viral illnesses, like diphtheria and measles, until after your baby is born and old enough to get their first vaccinations.
When does the placenta form?
The placenta starts forming as early as six days after fertilization. At this point your baby-to-be is a hollow ball of several hundred cells called a blastocyst. The blastocyst attaches to the lining of the uterus, usually near the top. This is called implantation, and it's completed by day 9 or 10.
The wall of the blastocyst is one cell thick except in one area, where it's three to four cells thick. In the thickened area, the inner cells develop into the embryo. The outer cells throughout the embryo burrow into the lining of the uterus and develop into the placenta.
The placenta produces several hormones that help maintain the pregnancy, including human Chorionic Gonadotropin (hCG), which prevents the ovaries from releasing eggs and stimulates the ovaries to produce estrogen and progesterone continuously. (Home pregnancy tests measure levels of hCG in your urine.)
(Home pregnancy tests measure levels of hCG in your urine.)
The placenta is fully formed by 18 to 20 weeks but continues to grow throughout pregnancy. At delivery, it weighs about 1 pound.
How the placenta works
The placenta connects to the umbilical cord through thousands of microscopic "fingers" of tissue (chorionic villi) containing a network of blood vessels that connect to the embryo's circulatory system. The villi are formed by 6 weeks of pregnancy, and your blood fills the spaces around them by 12 weeks. When your blood comes in contact with the villi, nutrients are exchanged for waste through the villi walls.
The villi also act as a filter, preventing some viruses and bacteria from reaching your baby, while allowing molecules of everything you ingest as well as antibodies and gases to pass through.
How do babies get nutrients in the womb?
Your baby needs nourishment from the get-go. Until the placenta is developed enough to provide nutrients, your baby receives nutrients from the lining of the uterus, called the endometrium.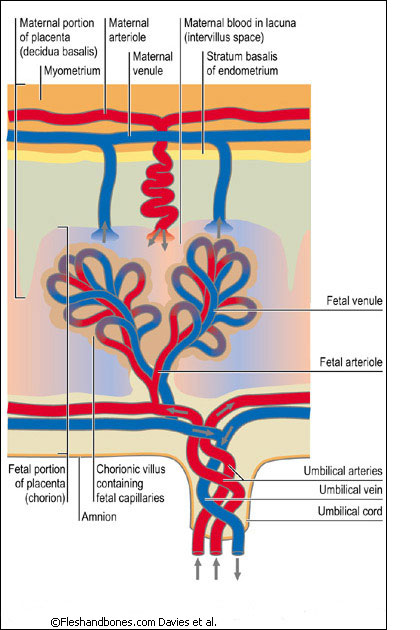 (These same endometrial cells will quickly multiply to form the placenta.)
(These same endometrial cells will quickly multiply to form the placenta.)
In the early weeks of pregnancy, glands in the uterine lining secrete glucose, which it stores as glycogen. At first, this glycogen is the only source of nourishment for your baby.
At about 8 to 12 weeks into pregnancy, the placenta takes over as a nutrient source for your baby. (And at this point the uterus stops secreting glycogen.) Here's how it works:
- When you eat, the food travels to your stomach, where it's broken down (digested) into glucose, fats, vitamins, minerals, and protein.
- The nutrients are absorbed into your bloodstream and travel to the placenta.
- Blood vessels in the umbilical cord pass the nutrients from the placenta to vessels that flow from the umbilical cord to the baby. At this point, your baby will begin to gain weight more quickly. The umbilical cord also returns waste products from your baby to the placenta and into your circulation for elimination.
Wondering how fast the food you eat reaches your baby? It depends on how quickly the food is digested and enters your bloodstream. Some foods may take several hours, while substances like caffeine can enter your bloodstream and cross the placenta in a very short time. For more information, watch our video on how food reaches your baby.
Harmful substances that cross the placenta
Along with all the good things that are transferred to your baby, some harmful ones can cross the placenta too. These include alcohol, nicotine, and illegal drugs as well as some medications.
No safe level has been established for alcohol consumption during pregnancy, and experts recommend not drinking any amount while you're expecting. The same goes for smoking and using illegal drugs. Although marijuana is legal in some states, experts recommend against using it during pregnancy.
Use caution when taking prescribed and over-the-counter medications during pregnancy because most cross the placenta. Although many medications are considered safe for your baby, a few are known to cause birth defects. And for many drugs, there simply is not enough research to know their effects on an unborn baby. Your provider can help you determine whether the benefits of a certain drug outweigh the risks in your case.
Although many medications are considered safe for your baby, a few are known to cause birth defects. And for many drugs, there simply is not enough research to know their effects on an unborn baby. Your provider can help you determine whether the benefits of a certain drug outweigh the risks in your case.
Although the placenta acts as a barrier to most bacteria, some viruses and small bacteria can cross it. Many have no effect, but others can be harmful to a developing baby. That's one reason why it's important to get all recommended vaccinations before and during pregnancy, including a flu shot and a Tdap vaccine to protect against tetanus, diphtheria, and pertussis (whooping cough).
Both the flu and pertussis can be life-threatening for babies, and getting these vaccines while you're pregnant enables antibodies to pass through the placenta that will protect your newborn from catching these illnesses. Getting your COVID vaccine and boosters will help protect you from infection and will also provide your baby with antibodies through the placenta (and your breast milk, if you breastfeed).
Here are a few other things you can do to promote a healthy placenta and a healthy baby:
- Go to all your prenatal checkups and work with your healthcare provider to manage any health conditions, such as high blood pressure, which can cause problems with the placenta.
- Don't smoke or use drugs. Placental problems, like placental abruption, are more common in women who smoke, use illegal drugs (like cocaine and heroin), or abuse medications (like opioids).
Delivering the placenta
A few minutes after your baby is born, the placenta detaches from the wall of your uterus and is delivered through your vagina. This is called the "afterbirth."
You'll have a few contractions, but this stage of childbirth usually lasts only about five to 30 minutes and feels more like menstrual cramps than labor pains. (If you're having a c-section, your doctor will remove the placenta manually.)
If you want, and if you've made prior arrangements with your provider, you can save the placenta. Some women believe that encapsulating and eating the placenta after birth helps them recover faster, though there's no scientific evidence to support this claim.
Some women believe that encapsulating and eating the placenta after birth helps them recover faster, though there's no scientific evidence to support this claim.
Also note that some experts think eating the placenta may be harmful, as there are potential risks, including infection and heavy metal contamination. Be sure to discuss this topic with your provider if it's something you're considering.
Learn more:
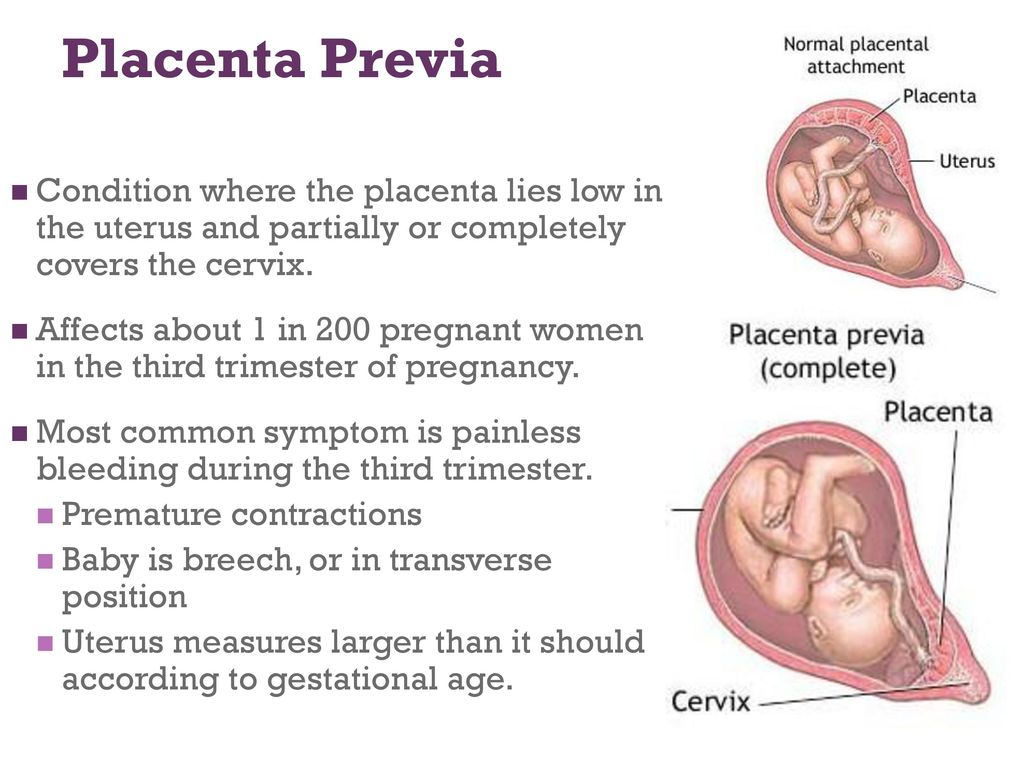
Placenta previa
Placenta accreta
Slideshow: Fetal development, week by week
advertisement | page continues below
When Does the Placenta Form? All About This Unique Organ
Pregnancy involves some pretty wild changes to your body. Did you know that in addition to growing a human, you’re also growing a whole new organ?
While you’re over here dealing with fatigue, cravings, sore boobs, and nausea, behind the scenes, your body is tirelessly working on two very important things: a baby and a placenta.
It’s true: Even early on, the placenta — an organ that’s made of both fetal and maternal tissue — is growing right alongside your little one.
Your body goes through rapid changes during pregnancy — especially in the early months. To support this process, you need a lifeline to help your baby eat and breathe. The placenta, an organ that develops inside your uterus, provides a connection between you and your baby.
This connection (via the umbilical cord) is what helps to sustain your developing baby throughout pregnancy. Necessary nutrients, oxygen, and antibodies pass from the placenta through the umbilical cord and to your baby.
Your placenta also works in reverse, meaning that it removes waste products and carbon dioxide from the baby’s blood back to your blood.
Since the placenta keeps your blood separate from your baby’s blood, it also helps to keep some bacteria and viruses out of the womb, protecting the fetus from infections.
In addition to being a lifeline to your baby, the placenta also produces and secretes hormones directly into the bloodstream to help support pregnancy and fetal growth. These hormones include:
These hormones include:
- progesterone
- estrogen
- oxytocin
- human chorionic gonadotropin
- human placental lactogen
Pregnancy involves a complex series of events, one of which is the formation of the placenta. In general, once the fertilized egg implants in the uterine wall, the placenta begins forming. But the ball starts rolling several days before implantation.
When you ovulate, an egg leaves the ovary to travel through the fallopian tube in hopes of being fertilized. If successful, the ovulated egg meets up with a spermatozoid to begin formation of the fetus. This ovulated egg is called a zygote. Over the course of a few days, the zygote will complete many cell divisions in the fallopian tube.
When the zygote reaches the uterus, these cell divisions continue, and then the zygote becomes a blastocyst. At this stage, some cells begin to form into the placenta and others begin to form the fetus. The blastocyst embeds in the endometrium (aka implantation).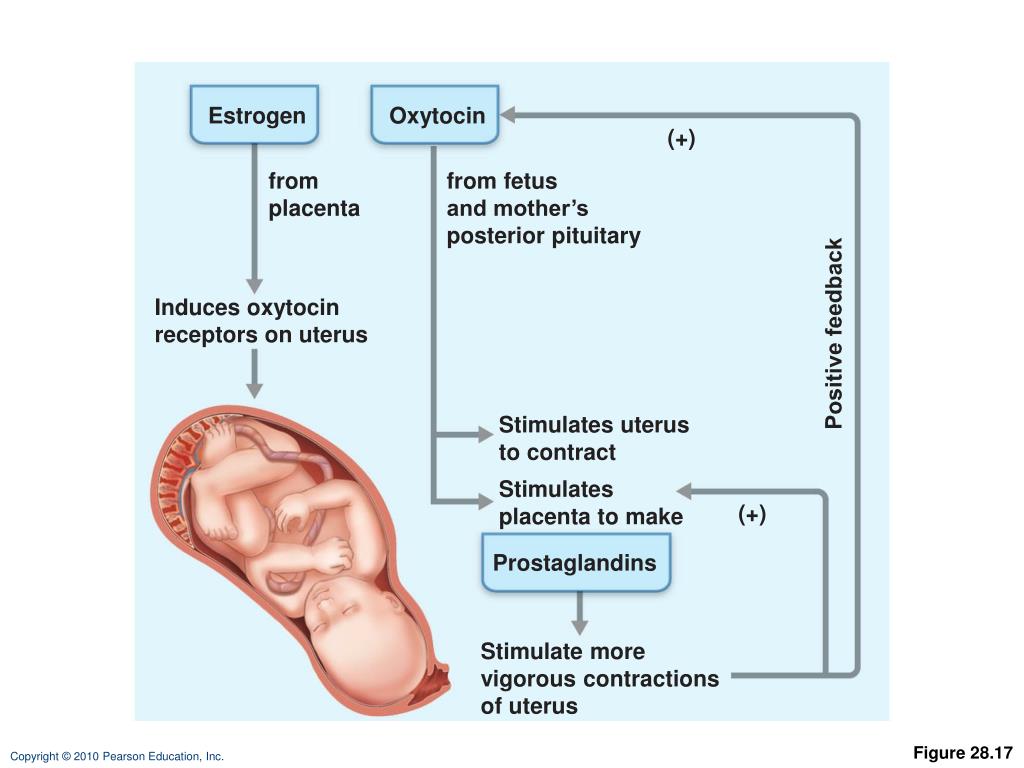
To help support pregnancy, the placenta produces a hormone called human chorionic gonadotropin (hCG). (This is the hormone measured by a pregnancy test, which is why you won’t get a positive test until after implantation.)
Over the course of your pregnancy, the placenta grows from a few cells into an organ that will eventually weigh about 1 pound. By week 12, the placenta is formed and ready to take over nourishment for the baby. However, it continues to grow throughout your pregnancy. It’s considered mature by 34 weeks.
Under normal conditions, the placenta will attach to the wall of your uterus. As pregnancy progresses, it will move with your growing uterus.
Since the placenta plays such a significant role during pregnancy, it’s helpful to know when it takes over key functions such as hormone production and providing nutrients to your baby.
Although each pregnancy is different, you can expect the placenta to take over around weeks 8 to 12 of pregnancy, with 10 weeks being the average time for most women.
This doesn’t mean that your own hormone production and nutrition aren’t important. In fact, as far as nutrition goes, the placenta “taking over” means that what you consume can now reach your baby via the umbilical cord and placenta.
Those who get pregnant via in vitro fertilization or have hormone deficiencies may need progesterone supplementation in the first trimester. These individuals are often able to stop taking this hormone once the placenta begins its own production.
Many women look forward to the second trimester — energy levels rise, hormone levels begin to balance out, and morning sickness subsides. But why does everything seem to get better?
As already mentioned, towards the end of the first trimester (around week 10), the placenta takes over the production of progesterone. This helps reduce nausea and vomiting. For many mamas, this means an end to morning sickness.
And what if your morning sickness doesn’t go way? The placenta may play a role in that case, too.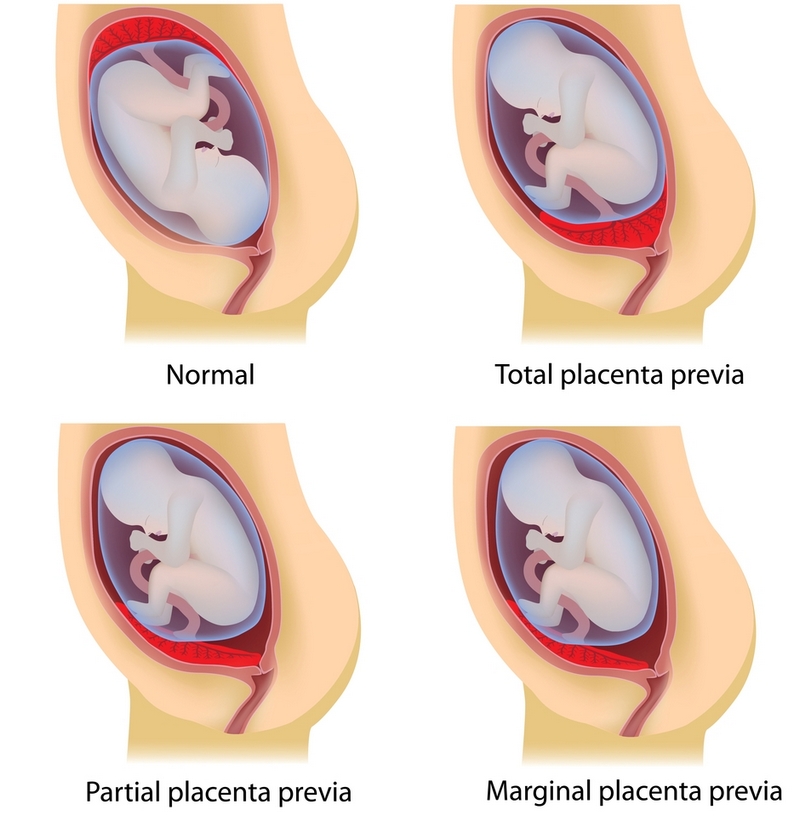
If you happen to have a higher concentration of a protein called GDF15 in your blood, those frequent bouts of nausea and vomiting may continue for some time.
One study found that women who reported vomiting in the second trimester had a higher level of maternal circulating GDF15 concentrations around week 15 of pregnancy.
The good news? Researchers speculate that high levels of GDF15 could mean that the placenta is developing properly. It could also help explain why some women have hyperemesis gravidarum, which is an extreme form of morning sickness.
The placenta usually attaches to the side or at the top of the uterus, but this is not always the case. Sometimes, it can develop in the wrong location or attaches too deeply, leading to placenta disorders.
Even if you experience a healthy pregnancy, complications with the placenta can still occur. That said, these conditions typically happen as a result of factors, like:
- genetics
- maternal age
- high blood pressure
- carrying multiples
- previous cesarean deliveries
- substance use
- previous placental problems
- abdominal trauma
The good news is your doctor will monitor many of these conditions throughout your pregnancy and work with you on a delivery plan.
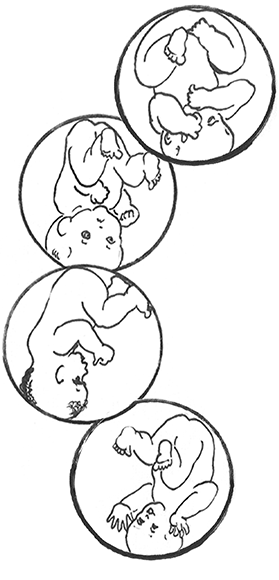
Placenta previa is a condition that causes the placenta to grow in the lowest part of the womb, typically within 2 centimeters from the cervical opening. As a result, the placenta covers all or part of the cervix. If the placenta is completely covering the cervix, this can cause bleeding during delivery and most likely will require a C-section for delivery.
Placental abruption is a serious condition that causes the placenta to detach from the wall of the uterus during pregnancy or birth. Symptoms include vaginal bleeding and back or abdominal pain.
Placenta accreta happens when part or all of the placenta is embedded too deep into the uterine wall.
Anterior placenta indicates that the placenta has attached to the front of the stomach. Typically, this isn’t an issue — it’s really just a normal variant — but tell your doctor if you feel decreased fetal movement.
Retained placenta indicates that part of the placenta is still in the womb after childbirth. If the placenta does not deliver within a certain amount of time, generally 30 minutes (but can be as long as 60 minutes), your doctor will perform a procedure to remove the placenta.
Placental insufficiency is diagnosed when the placenta cannot deliver an adequate supply of oxygen and nutrients to the fetus, which can result in pregnancy complications. Your doctor will monitor this condition throughout pregnancy.
If this is your first pregnancy, then you might be surprised to learn that delivering your baby is not the only stage of childbirth. After setting your sights on that beautiful bundle of joy, get ready for stage three of childbirth — delivering the placenta.
During this last leg of delivery, your uterus will continue to contract, allowing the placenta to separate from the uterine wall and eventually through the birth canal for delivery.
If you had a vaginal birth, this process takes about 30 minutes. For mamas that deliver via cesarean, your doctor will remove the placenta.
To move things along, your doctor may ask you to push, or they may massage your uterus. In some cases, they may give you Pitocin to help make the uterus contract.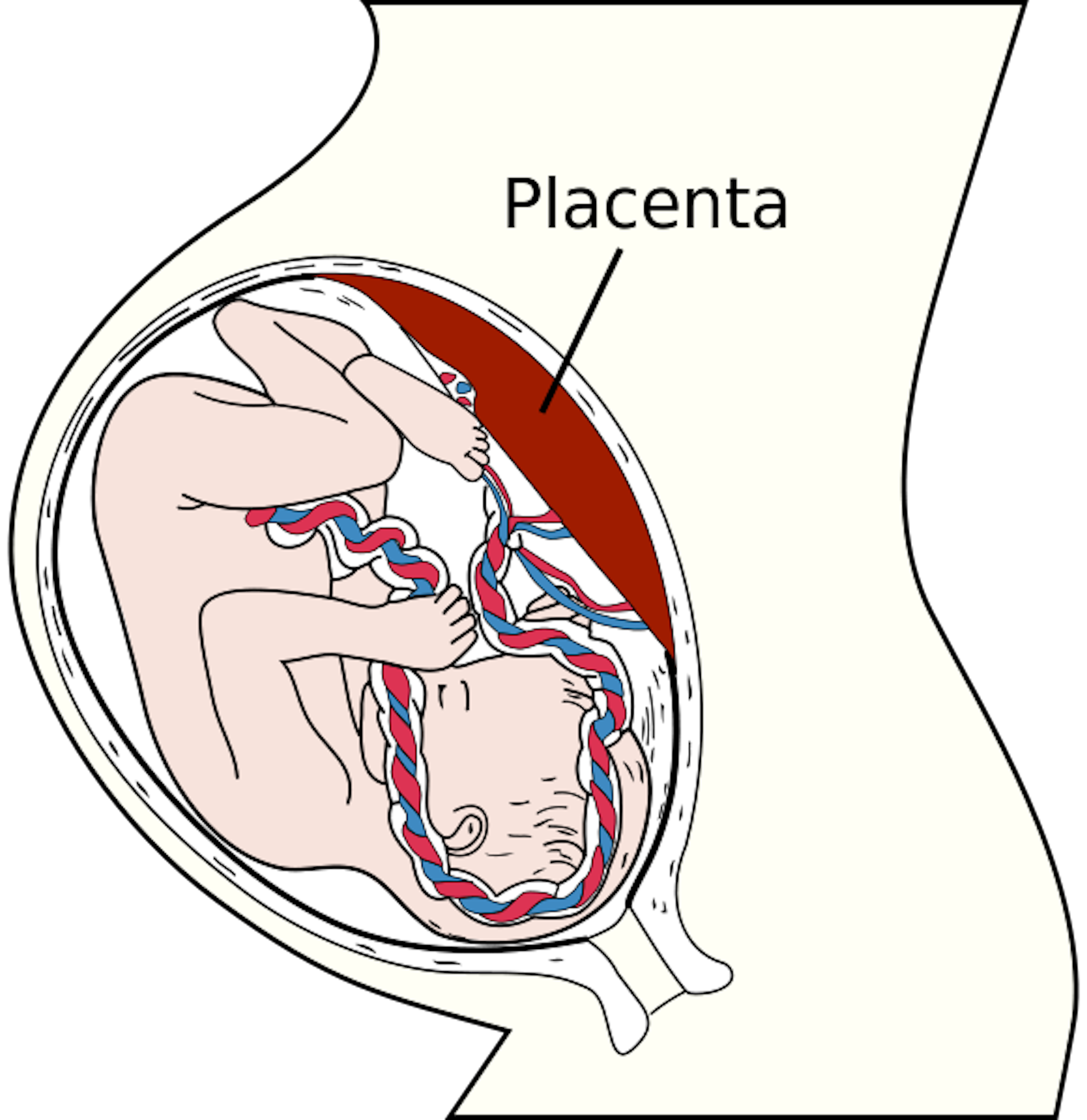 Or, they may recommend a little skin-to-skin contact with your baby to help your uterus contract.
Or, they may recommend a little skin-to-skin contact with your baby to help your uterus contract.
The placenta is an essential organ that provides oxygen and nutrients to your developing baby. It also plays a significant role in the health of your pregnancy.
Throughout your pregnancy, the placenta grows and changes shape. If you experience any symptoms such as bleeding from the vagina, abdominal pain, or back pain, contact your doctor immediately. These may be signs of a more serious condition like placenta previa.
Significance of the placenta, or the "other side" of the baby, during pregnancy
The placenta begins to form at the site of implantation of the fertilized egg at 6-7 weeks of pregnancy, it is fully formed at the 4th month of pregnancy. In the future, the placenta gradually increases, and at the end of pregnancy, its diameter reaches 15–18 centimeters, and its weight is 500 grams.
The placenta consists of placental tissues and blood vessels.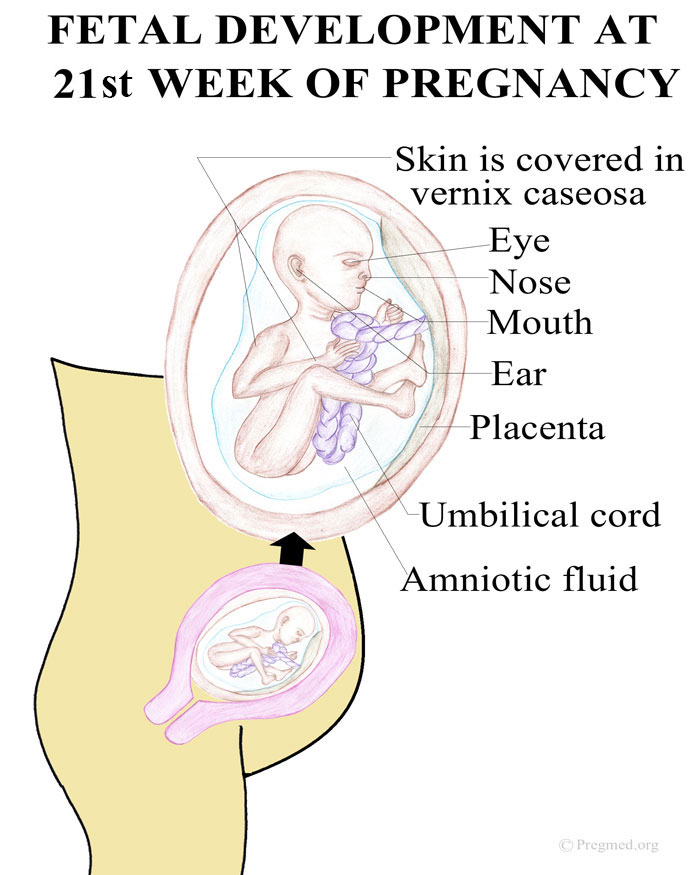 On the one hand, with small blood vessels, it is attached to the wall of the uterus, and on the other hand, it is covered with fetal membranes, to which the umbilical cord is attached. Genetically and biologically, the placenta is of fetal origin, and its functionality depends on the blood composition and circulation of the mother.
On the one hand, with small blood vessels, it is attached to the wall of the uterus, and on the other hand, it is covered with fetal membranes, to which the umbilical cord is attached. Genetically and biologically, the placenta is of fetal origin, and its functionality depends on the blood composition and circulation of the mother.
The function of the placenta is to feed and protect
The main function of the placenta is to provide various metabolic processes between mother and fetus. In addition, the placenta secretes into the mother's blood circulation hormones - choriongonadotropins, progesterone - necessary for the normal course of pregnancy. From the 7th to 8th weeks of pregnancy, the placenta begins to produce estrogen. Delivering nutrients to the fetus from the mother and removing the waste products of the fetal metabolism, the placenta ensures the exchange of oxygen and carbon dioxide.
The function of the placenta is also to provide passive immunity to the fetus.
For example, if a mother is vaccinated against influenza, the resulting antibodies are transferred to the fetus through the placenta and protect the newborn and infant from severe influenza illness for 6 months after birth.
The immune system works in a similar way if a mother receives a whooping cough vaccine and a vaccine against Covid-19 infection during pregnancy. The doctor points out that this principle does not work against all infections - not all vaccines against infectious diseases provide the transfer of antibodies to the fetus.
For example, influenza and Covid-19 may or may not cross the placenta. It is known that the probability of infection with the Covid-19 virus is quite small for the fetus - only 0.4-5% of cases. The devastating effect of Covid-19 on pregnancy is harm specifically for the woman’s body – the mother’s lack of oxygen leaves consequences for the child.
In general, the placenta protects against many infections, but does not protect against syphilis, toxoplasmosis, listeriosis, Zika virus. If the mother gets these infections during pregnancy, the fetus can be born with serious congenital abnormalities. The period of pregnancy in which the woman fell ill is also important.
If the mother gets these infections during pregnancy, the fetus can be born with serious congenital abnormalities. The period of pregnancy in which the woman fell ill is also important.
When the placenta becomes involved in protecting the baby
An egg that has been fertilized and begins to divide takes time to reach the uterus and implant itself in its soft tissue, or endometrium. Only when this has happened does the placenta begin to form and choriongonadotropin is released. Thus, in the tissues of the uterus, the placenta begins to form from the moment when the fertilized egg is implanted in the wall of the uterus. Placental tissues during the entire pregnancy are transformed and continue to grow.
As soon as a woman finds out that she is pregnant (most often this is the 5-6th week of pregnancy), it is necessary to start living in the healthiest way possible. In the first weeks, the child's organs are formed, the genesis of organs occurs, when it is critically important to live in the most healthy way and follow the doctor's recommendations on lifestyle.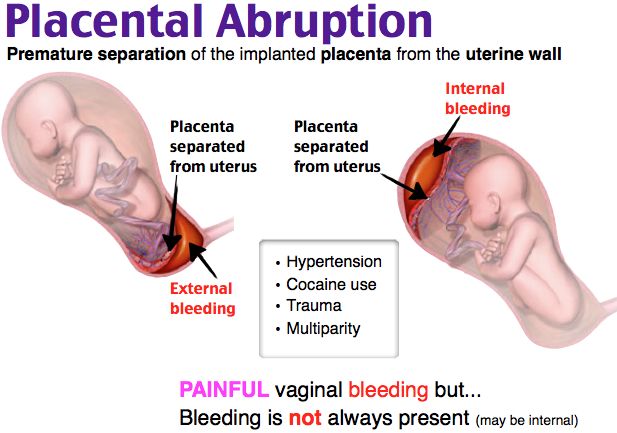 The placenta also begins to work.
The placenta also begins to work.
“We can say that the placenta performs a transport function rather than protection. It lets medicines, infections, nutrients, alcohol, etc. through. How much it passes and what it filters depends on various circumstances. Higher molecular weight drugs cross the placenta less. For example, insulin and heparin, which is a blood-thinning drug, cross the placenta minimally. In general, absolutely any medication crosses the placenta, ”explains doctor Katrina Kalnina.
When the placenta finishes its job
The placenta is not a perpetual organ. If the pregnancy is overdue, then at the birth of the placenta, you can see that there are such small pieces of pebbles in it - calcifications. With a sonographic examination, it is possible to determine what the degree of age of the placenta is. There are three stages - from 0 to 3.
The last - third - stage indicates that the placenta is so mature that it can signal to the brain that labor can begin.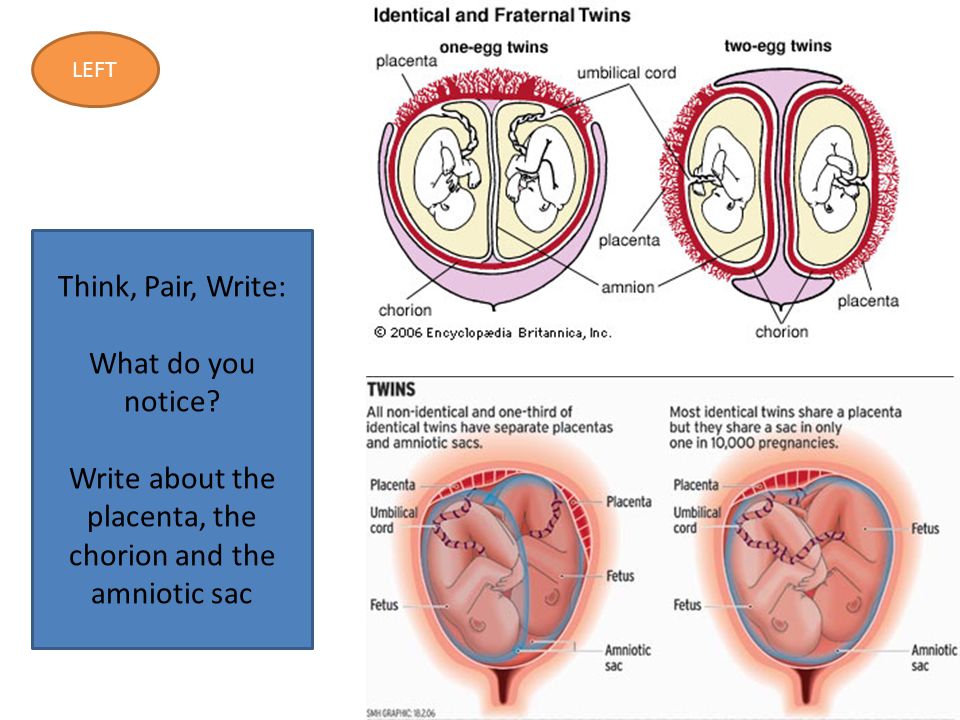
Calcifications can be seen even a few weeks before delivery, but there is no reason to worry. This does not mean that preterm labor is approaching or that the baby is not getting enough oxygen.
During childbirth, the placenta does its work until the third stage of labor. That is, after the birth of the child, which is the second stage of labor, the third, or the birth of the placenta, follows, which lasts about 30 minutes.
There are situations in which, as soon as the baby is born, the woman is given an injection of oxytocin, which helps the uterus to contract. This is called active management of the placental period, and it is an effective method of preventing bleeding. At the birth of the placenta, the mother continues to push, and if you pull a little on the umbilical cord, the placenta comes out by itself. When the placenta is born, it is examined and assessed for any piece left in the uterus. If the placenta still does not separate, it is removed manually. If any piece of the placenta or fetal membrane remains in the uterus, it is necessary to abrade the uterine cavity.
If any piece of the placenta or fetal membrane remains in the uterus, it is necessary to abrade the uterine cavity.
Possible problems and pathologies
There are more serious and less serious pathologies of the placenta. In the anatomical sense, there may be changes and deviations in the shape of the placenta from the norm, for example, it has an additional lobe or the umbilical cord is attached not in the middle, but in the membranes of the fetus or at the very edge. Sometimes this can be seen on ultrasonography, and sometimes these features are only discovered after childbirth. But there are more serious pathologies that require medical supervision or intervention.
Location of the placenta
Advertisement
Advertisement
Normally, the placenta forms in the upper part of the uterus, but there are times when it is attached directly to the front of the mother's abdomen in the uterus. In this case, the woman will feel the movements of the baby later, but this in no way affects the process of pregnancy or the development of the fetus.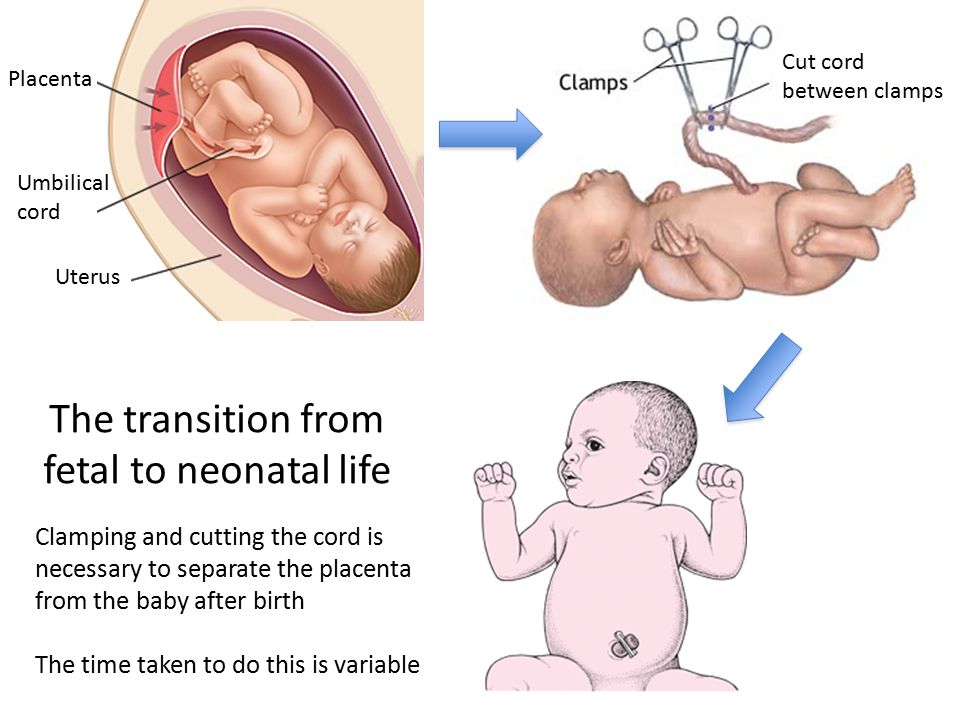 Worse, if the placenta is located low or even closes the mouth of the uterus, that is, it is presenting. True, how the birth will take place can only be said in the last trimester of pregnancy, since along with the growth of the uterus over time, the placenta can “rise”.
Worse, if the placenta is located low or even closes the mouth of the uterus, that is, it is presenting. True, how the birth will take place can only be said in the last trimester of pregnancy, since along with the growth of the uterus over time, the placenta can “rise”.
If even in the third trimester USG shows that the placenta is too low, then it is unlikely that it will rise higher. This means that the woman herself will not be able to give birth and will have to have a caesarean section, because when the cervix opens, the placenta can exfoliate and bleeding can begin. In the worst case scenario, neither mother nor child may survive. The woman herself cannot influence the location of the placenta or its elevation.
Preeclampsia
Disease of the placenta - preeclampsia - is possible only in pregnant women. If a woman has preeclampsia, her entire body, including the placenta, narrows and spasms the blood vessels, which also significantly complicates the placental circulation and thus directly affects the well-being and growth of the fetus.
The baby is not getting enough nutrients and oxygen, so fetal growth retardation may occur. In turn, the mother has a greater risk of placental abruption, which threatens her life and the life of the baby.
Globally, high-risk pregnant women are advised to take prophylactic aspirin early in pregnancy (weeks 12-16), which reduces the risk of preeclampsia. The high-risk group includes women who have high blood pressure during pregnancy; the older the mother, the greater the risk of preeclampsia; in cases of multiple pregnancy; in the presence of systemic autoimmune and chronic kidney disease, diabetes and obesity.
Placental abruption
Placental abruption is a life-threatening condition for mother and baby. Usually it is associated with adverse circumstances during pregnancy, but the reasons why this can happen can most often not be foreseen in advance. If most of the placenta has separated, there may be abdominal pain and bleeding.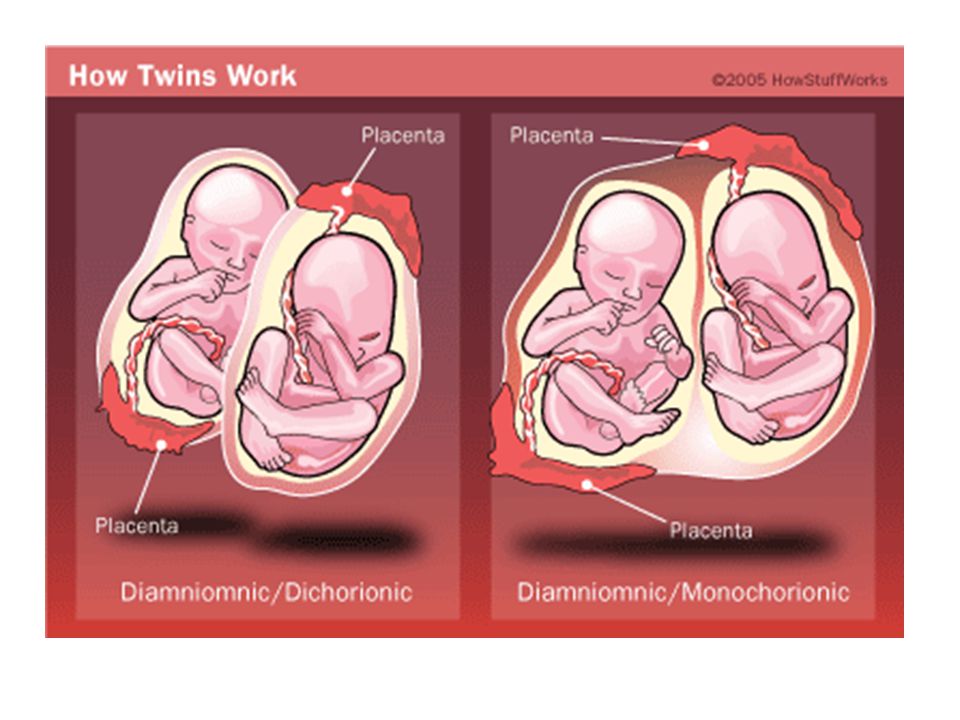 Sometimes the blood does not come out and remains at the placenta.
Sometimes the blood does not come out and remains at the placenta.
A pregnant woman begins to have pain in the lower part of her abdomen, then the pressure drops sharply, she feels cold and sweats. If the pain is severe, the pregnant woman should be taken to the hospital immediately.
If the placenta separates, the pregnant woman may lose consciousness. If only a small part of the placenta is separated, coagulation occurs and then recovery. In this case, the symptoms may be minimal. If a pregnant woman begins to bleed, she should be examined immediately, as the baby may not be getting enough oxygen. This can lead to distress and death of the fetus. In case of suspected placental abruption, you should immediately go to the hospital! If placental abruption is extensive, a caesarean section is performed.
Placenta accreta
Pathological placenta ingrowth into the wall of the uterus is a condition that threatens the health and life of a woman, which can result in a hysterectomy, or removal of the uterus.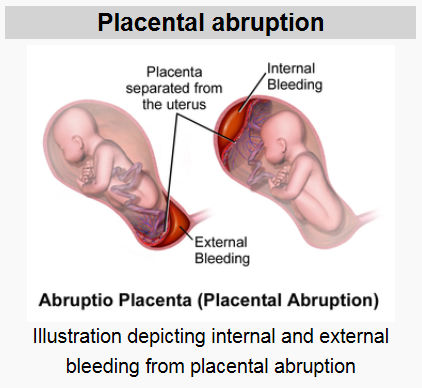 Most often, these are the consequences of previous caesarean sections or other manipulations in the uterine cavity - abortion, abrasion of the uterine cavity, removal of polyps, or any activity that affects and affects the condition of the uterine wall.
Most often, these are the consequences of previous caesarean sections or other manipulations in the uterine cavity - abortion, abrasion of the uterine cavity, removal of polyps, or any activity that affects and affects the condition of the uterine wall.
Dr. Katrina Kalnina notes that many women today do not appreciate how far-reaching the consequences of a caesarean section can be. Each subsequent pregnancy is associated with greater risks of placenta accreta.
If, during a caesarean section, it is determined that the placenta has grown in, it is estimated on what area and how deep this happened. Previously, to save their lives, women made the decision to remove the uterus, but in recent years they have been trying to follow a different tactic - the uterus is sutured, leaving the placenta in it, and in the coming weeks the placenta separates itself. The risk of inflammation and complications increases, but this is an opportunity to preserve the uterus and the woman's fertility.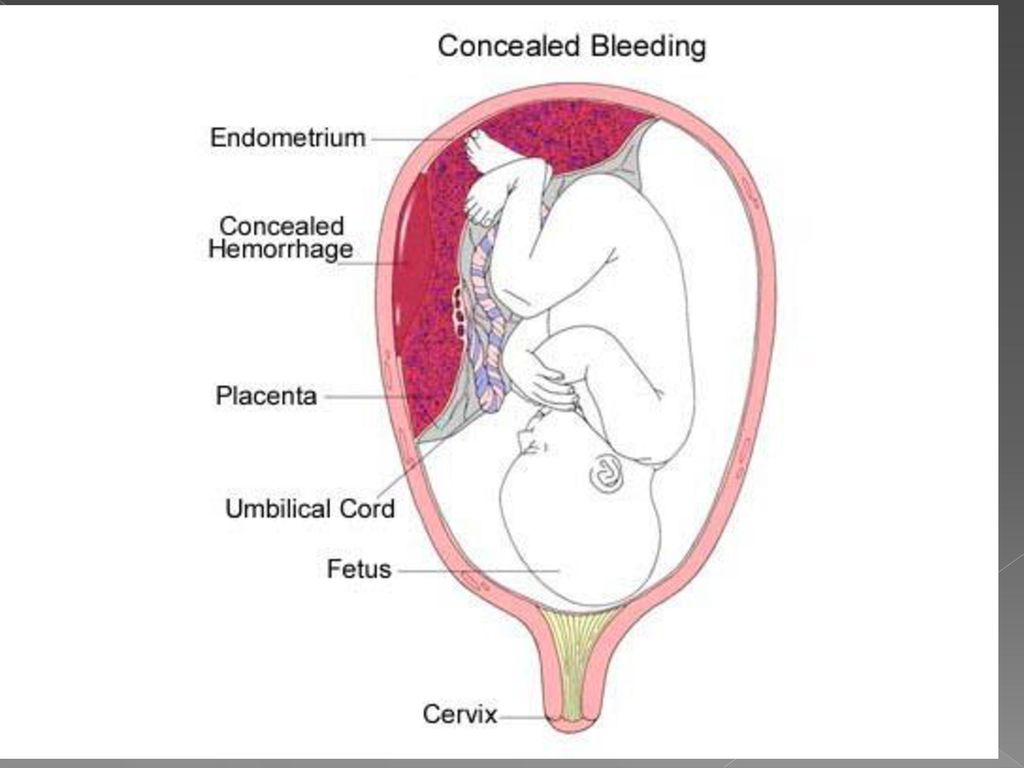
Another method that is gentle on the uterus - the placenta is cut out together with the wall of the uterus into which the placenta has grown, the scar is sewn up and the uterus is preserved. If there was placenta ingrown, then there is a higher risk that this problem will recur next time. Placenta ingrowth can be detected by ultrasonography, and sometimes magnetic resonance is also performed.
If twins are expected
If there is one fetus, then there is one placenta that supplies it with everything it needs. It is more difficult if the pregnancy is multiple.
The best option is if each twin has their own placenta, or bichorionic placenta. If two twins share the same placenta, it is a monochorionic placenta. In such pregnancies, there is a possibility that the vessels of both fetuses are connected, and one twin receives more nutrients and oxygen than the other. As a result, it turns out that one twin has too much of everything, and the other does not have enough.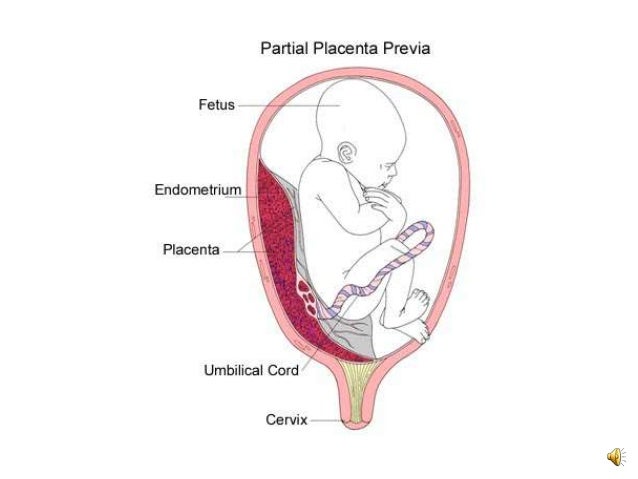 Such difficult pregnancies can be quickly corrected.
Such difficult pregnancies can be quickly corrected.
NOTICE
Genetic tests
Since the placenta contains the same genetic material as the baby, pieces of placenta are used in genetic screening. A biopsy of the chorionic villi, if necessary, is carried out from the 11th to the 14th week - tissue from the placenta is taken with a needle. This is a fairly accurate method for determining the hereditary diseases of a child. There is a threat of spontaneous abortion in 0.2–1% of cases. Most often, this is checked for common pathologies of trisomies, if possible problems are identified at the first screening.
Wondering about the placenta
- Mother and baby's blood is filtered through the placenta but never mixed. At the end of pregnancy, 500 ml of the mother's blood passes through the placenta every minute.
- The placenta is an immune system messenger that helps the mother's and baby's immune systems communicate.
 During pregnancy, the placenta prevents the mother's body from considering the fetus as a foreign body and rejecting it. During the third trimester, the placenta transfers the mother's antibodies to the baby, which is the basis of the baby's immune defense for another 6 months after birth.
During pregnancy, the placenta prevents the mother's body from considering the fetus as a foreign body and rejecting it. During the third trimester, the placenta transfers the mother's antibodies to the baby, which is the basis of the baby's immune defense for another 6 months after birth. - The placenta prepares a woman's body for breastfeeding. It produces a hormone that suppresses the production of mother's milk during pregnancy, and after the birth of the placenta, the mother's body receives a signal that it is time to produce milk.
How the baby is nourished in the womb
In the first two weeks after fertilization, while the egg has not yet had time to implant into the uterine wall and acquire the placenta, it receives nutrients from its thickened inner shell - the yolk sac.
From the fourth week, the embryo receives the oxygen and nutrients it needs through the chorionic villi, which then transforms into the placenta - a reliable home for the baby, which protects him, and is also the main organ that exchanges between mother and fetus.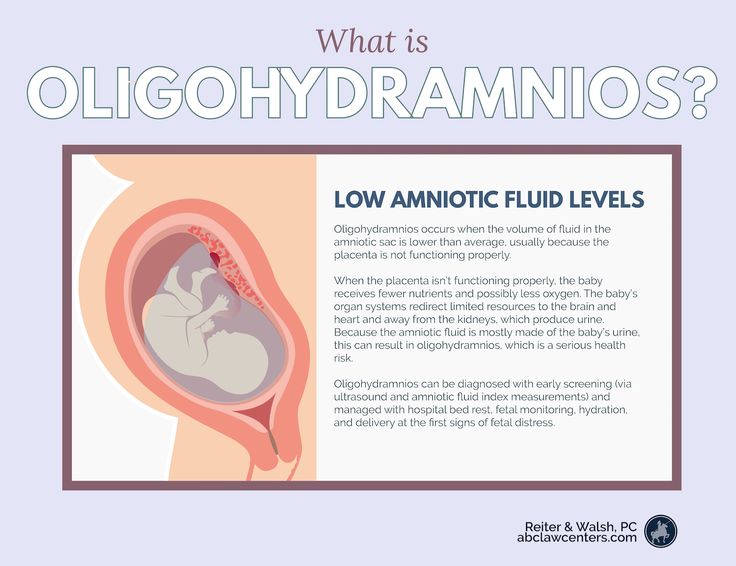 The placenta is also called the baby's place. This is a temporary organ that is formed and works only during pregnancy.
The placenta is also called the baby's place. This is a temporary organ that is formed and works only during pregnancy.
It is through the placenta that the baby communicates with the mother's body. From here, it receives proteins necessary for the structure of tissues, carbohydrates for energy and maintenance of the body, and fats, vitamins and minerals for proper metabolism. Through the placenta, the child also receives oxygen - without it, the body of the fetus cannot exist. All metabolic products are also excreted through the placenta. The placenta protects the child from infection, prevents immunological conflict between the foreign tissues of the mother and the child, and supplies both organisms with the hormones necessary for their development.
Read also: How to restore the breast after pregnancy
its bones and soft tissues. The fetus developing in the uterus requires a certain amount of proteins, fats, carbohydrates, vitamins and minerals.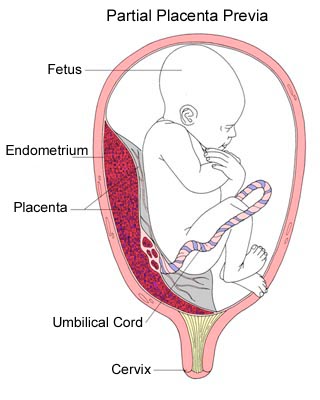 All these substances enter the mother's body with food, are broken down in the digestive system to simple molecules and absorbed into the blood, which delivers all the vital components to the fetus.
All these substances enter the mother's body with food, are broken down in the digestive system to simple molecules and absorbed into the blood, which delivers all the vital components to the fetus.
The womb is a unique microsystem that protects the baby and constantly adapts to its changing needs. Mother and fetus organisms work in unison. Even a slight change in the level of one of the indicators of the composition of the child's blood instantly causes a compensatory reaction of the mother's body. This feedback guarantees the supply of all nutrients, vitamins and minerals necessary for the normal growth and development of the baby. At the same time, this ensures the removal of the waste products of the fetus from its body.
The fetus is connected to the mother's body through the placenta and vessels that form the umbilical cord. The umbilical cord is made up of two arteries and a vein, similar to a cord with several ropes, which are twisted together and covered with a sheath. This makes the umbilical cord extremely durable. The umbilical cord can twist and turn, and the force of blood flow in the arteries keeps it taut so your baby can't get tangled up in it. During pregnancy, the length and width of the umbilical cord increases with the growth of the fetus.
This makes the umbilical cord extremely durable. The umbilical cord can twist and turn, and the force of blood flow in the arteries keeps it taut so your baby can't get tangled up in it. During pregnancy, the length and width of the umbilical cord increases with the growth of the fetus.
During pregnancy, the placenta also changes to meet the nutritional needs of the fetus. It controls the transfer of nutrients from mother to baby, as well as hormones and other substances. However, if the mother's diet is deficient in nutrients, the placenta will not be able to fully develop to provide the fetus with an effective supply. The low nutrient content of the mother's blood will permanently inhibit the normal functioning of the placenta. The placenta becomes unnecessary when the umbilical cord is cut - at this moment all the organs of the child begin to function independently.
Read also: Why shouldn't pregnant women wear heels?
The baby is able to extract from the mother's body some of the substances he needs, for example, most often this refers to calcium, which is washed out of the mother's bones if this mineral is absent in her diet.