When should you feed your baby cereal
When, What, and How to Introduce Solid Foods | Nutrition
For more information about how to know if your baby is ready to starting eating foods, what first foods to offer, and what to expect, watch these videos from 1,000 Days.
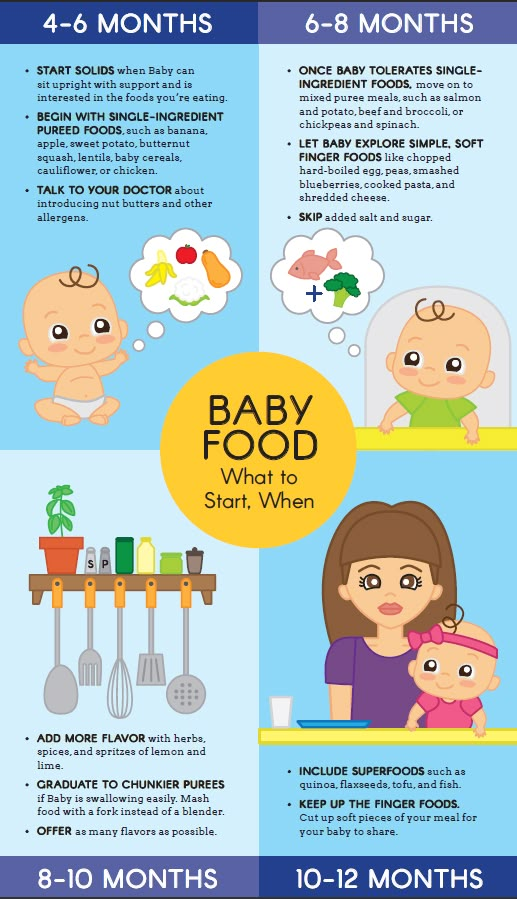
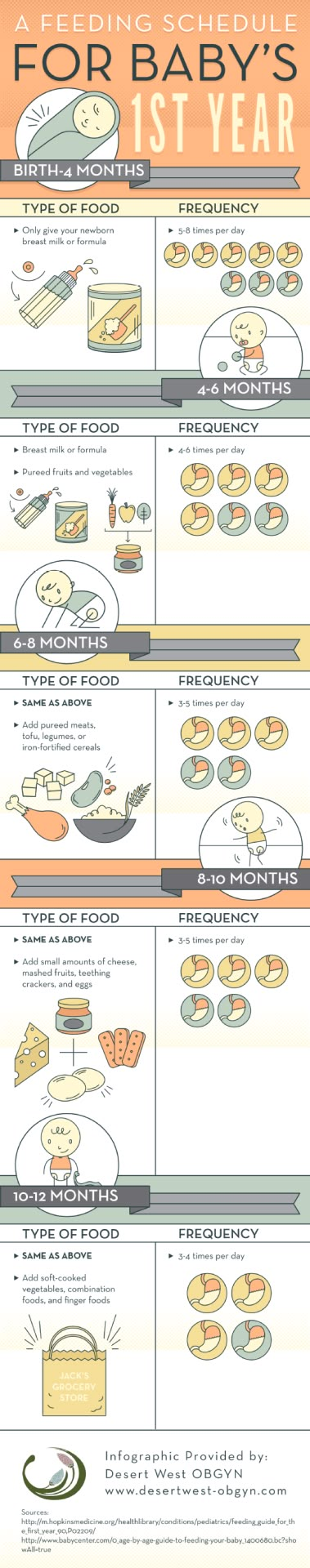
The Dietary Guidelines for Americans and the American Academy of Pediatrics recommend children be introduced to foods other than breast milk or infant formula when they are about 6 months old. Introducing foods before 4 months old is not recommended. Every child is different. How do you know if your child is ready for foods other than breast milk or infant formula? You can look for these signs that your child is developmentally ready.
Your child:
- Sits up alone or with support.
- Is able to control head and neck.
- Opens the mouth when food is offered.
- Swallows food rather than pushes it back out onto the chin.
- Brings objects to the mouth.
- Tries to grasp small objects, such as toys or food.
- Transfers food from the front to the back of the tongue to swallow.
What Foods Should I Introduce to My Child First?
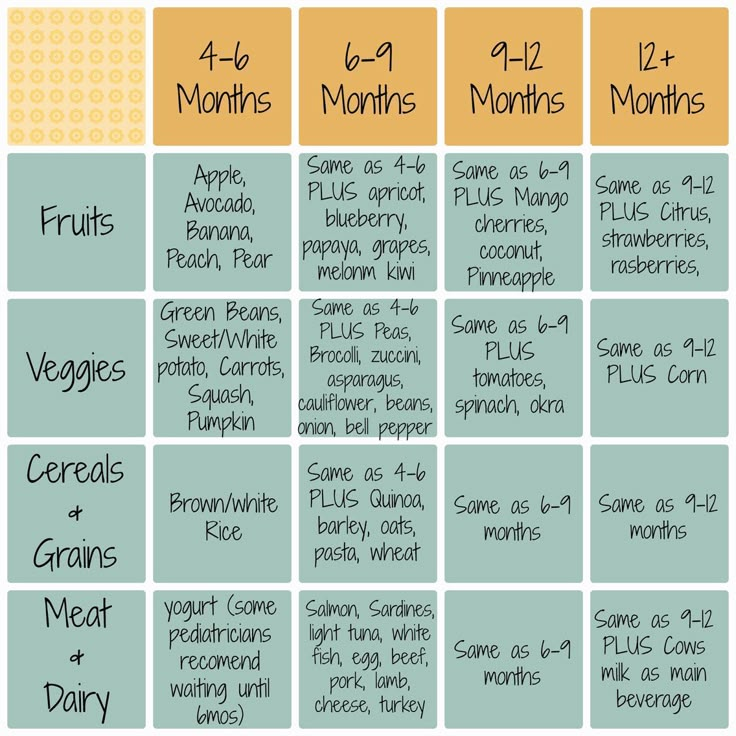
The American Academy of Pediatrics says that for most children, you do not need to give foods in a certain order. Your child can begin eating solid foods at about 6 months old. By the time he or she is 7 or 8 months old, your child can eat a variety of foods from different food groups. These foods include infant cereals, meat or other proteins, fruits, vegetables, grains, yogurts and cheeses, and more.
If your child is eating infant cereals, it is important to offer a variety of fortifiedalert icon infant cereals such as oat, barley, and multi-grain instead of only rice cereal. Only providing infant rice cereal is not recommended by the Food and Drug Administration because there is a risk for children to be exposed to arsenic. Visit the U.S. Food & Drug Administrationexternal icon to learn more.
How Should I Introduce My Child to Foods?
Your child needs certain vitamins and minerals to grow healthy and strong.
Now that your child is starting to eat food, be sure to choose foods that give your child all the vitamins and minerals they need.
Click here to learn more about some of these vitamins & minerals.
Let your child try one single-ingredient food at a time at first. This helps you see if your child has any problems with that food, such as food allergies. Wait 3 to 5 days between each new food. Before you know it, your child will be on his or her way to eating and enjoying lots of new foods.
Introduce potentially allergenic foods when other foods are introduced.
Potentially allergenic foods include cow’s milk products, eggs, fish, shellfish, tree nuts, peanuts, wheat, soy, and sesame. Drinking cow’s milk or fortified soy beverages is not recommended until your child is older than 12 months, but other cow’s milk products, such as yogurt, can be introduced before 12 months. If your child has severe eczema and/or egg allergy, talk with your child’s doctor or nurse about when and how to safely introduce foods with peanuts.
How Should I Prepare Food for My Child to Eat?
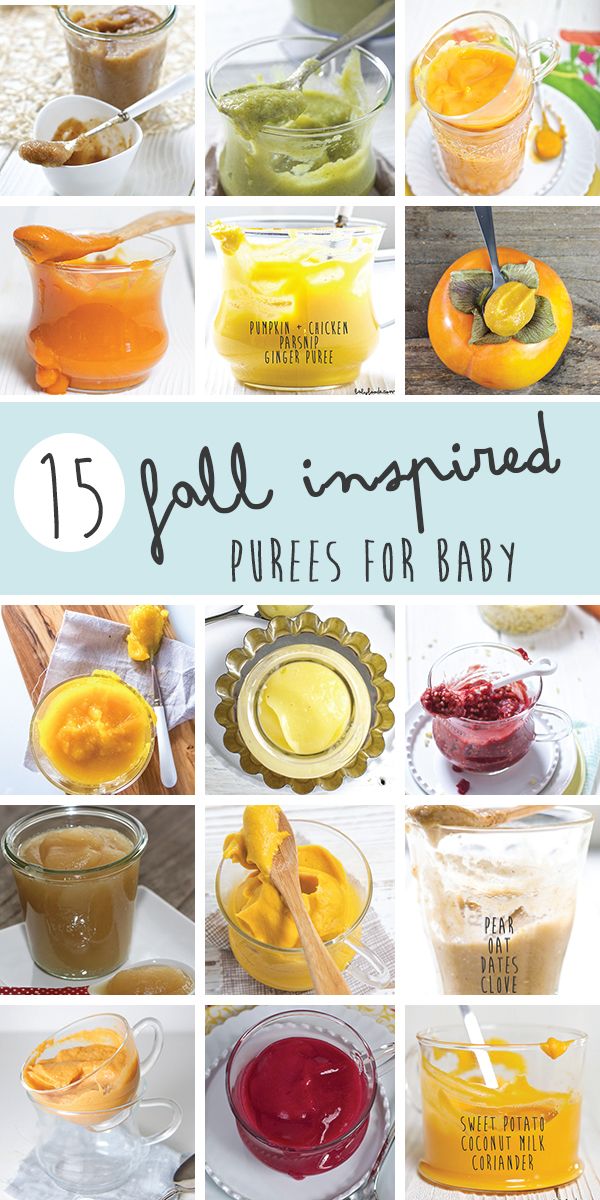
At first, it’s easier for your child to eat foods that are mashed, pureed, or strained and very smooth in texture. It can take time for your child to adjust to new food textures. Your child might cough, gag, or spit up. As your baby’s oral skills develop, thicker and lumpier foods can be introduced.
Some foods are potential choking hazards, so it is important to feed your child foods that are the right texture for his or her development. To help prevent choking, prepare foods that can be easily dissolved with saliva and do not require chewing. Feed small portions and encourage your baby to eat slowly. Always watch your child while he or she is eating.
Here are some tips for preparing foods:
- Mix cereals and mashed cooked grains with breast milk, formula, or water to make it smooth and easy for your baby to swallow.
- Mash or puree vegetables, fruits and other foods until they are smooth.
- Hard fruits and vegetables, like apples and carrots, usually need to be cooked so they can be easily mashed or pureed.
- Cook food until it is soft enough to easily mash with a fork.
- Remove all fat, skin, and bones from poultry, meat, and fish, before cooking.
- Remove seeds and hard pits from fruit, and then cut the fruit into small pieces.
- Cut soft food into small pieces or thin slices.
- Cut cylindrical foods like hot dogs, sausage and string cheese into short thin strips instead of round pieces that could get stuck in the airway.
- Cut small spherical foods like grapes, cherries, berries and tomatoes into small pieces.
- Cook and finely grind or mash whole-grain kernels of wheat, barley, rice, and other grains.
Learn more about potential choking hazards and how to prevent your child from choking.
Top of Page
When Can You Start Feeding Your Baby Rice Cereal
Adding solid foods to your baby’s diet is a big milestone, and you may be wondering when to begin the process and what foods to start with. In the past, single grain infant cereals have been the traditional first choice when transitioning to solid foods, with rice cereal being one of the more popular ones. These days, though it is still OK to start with cereal, experts say that there is no evidence that introducing foods in a certain order provides any advantage for your baby (though babies do tend to like cereal).
In the past, single grain infant cereals have been the traditional first choice when transitioning to solid foods, with rice cereal being one of the more popular ones. These days, though it is still OK to start with cereal, experts say that there is no evidence that introducing foods in a certain order provides any advantage for your baby (though babies do tend to like cereal).
Keep in mind that experts highly recommend giving rice cereal as part of a mixed diet of single ingredient choices, rather than as an exclusive food.
Find out how to safely give rice cereal to your baby, and what other infant cereals you might want to give instead.
What Is Rice Cereal?
Rice cereal for babies has been a traditional first food for infants who are being introduced to eating solids. The most common type is a dry powdered cereal, to which liquid is added to form an oatmeal-like consistency, but it can also be purchased premixed. It's one of the single grain cereals that have been recommended for infants when they start on solid foods.
It's one of the single grain cereals that have been recommended for infants when they start on solid foods.
Is Rice Cereal Safe for Your Baby to Eat?
It’s OK to include rice cereal in your baby’s diet as long as you’re not exclusively feeding your baby rice cereal.
The reason experts recommend rice cereal be limited is because of the naturally occurring levels of inorganic arsenic in rice (in this case inorganic refers to the arsenic’s specific chemical compound bound with carbon).
As rice is grown, the plant absorbs more inorganic arsenic from its environment compared to other crops. Arsenic is a naturally occurring element that can enter the food supply through water, soil, or air.
When body weight is considered, a baby’s intake of inorganic arsenic through rice cereal could be three times more than an adult’s. Eating too much rice cereal as an infant can cause long-term health problems.
What Infant Cereals Can You Give Your Baby Instead of Rice Cereal?
Instead of rice cereal, you can offer another single grain infant cereal such as oat or barley cereal. You can find many of these infant cereals in premixed or dry versions to which you would add breast milk, formula, or water to create a consistency that your baby will like.
Look for cereals that are specifically made for babies because they will be fortified with nutrients like iron and zinc that your baby needs.
Just remember that when introducing new foods — including different types of infant cereals — do so gradually, offering one new food at a time, and then waiting a couple of days before adding another food, to watch for any possible allergic reactions. Once your baby has become accustomed to eating solids, feel free to offer a variety of single ingredient, soft foods.
How Many Times a Day Should You Feed Your Baby Infant Cereal?
When your little one is just starting on solids, spoon-feed your baby a small amount of infant cereal once or twice a day, ideally just after he’s been bottle-fed or breastfed.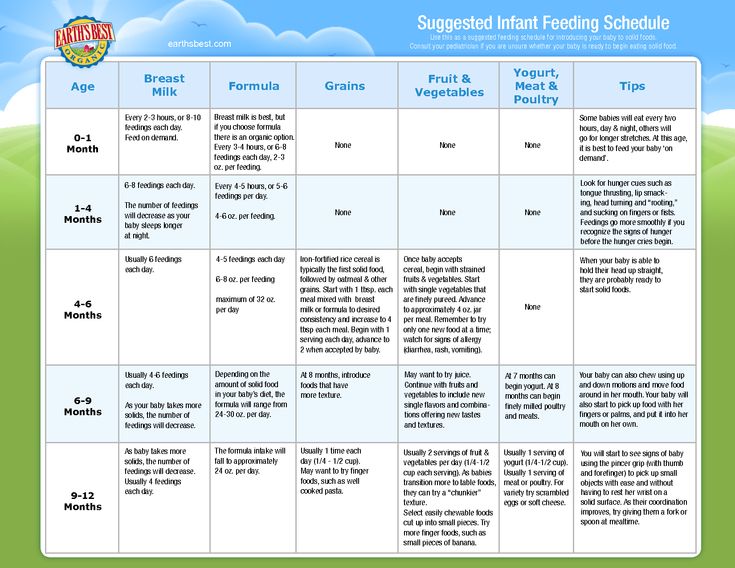 Start with one or two teaspoons of cereal so that your baby can get accustomed to this new food.
Start with one or two teaspoons of cereal so that your baby can get accustomed to this new food.
Eventually you can introduce other foods one at a time—and you can even make your baby’s food at home.
Are Other Rice Products Safe to Give Your Baby?
Not necessarily. You can give rice to your older baby as part of a varied and balanced diet. However, it’s best to avoid certain rice-based products like rice syrup, often used as a sweetener in processed foods, as well as rice milk, which should not be used as a substitute for cow's milk.
If your child has turned 1 and is sensitive or allergic to cow’s milk, your healthcare provider will be able to recommend milk alternatives if needed, and can also weigh in on any rice products you’re considering giving.
At What Age Should You Start Feeding Your Baby Infant Cereals?
For most babies, 6 months is a good age to start to introduce solid foods, which can include infant cereals. Breast milk or formula will continue to provide most of your baby's nutrition for the first 12 months.
Breast milk or formula will continue to provide most of your baby's nutrition for the first 12 months.
Waiting until this age is important because by this point your baby would have outgrown a natural reflex that all babies are born with that causes them to push their tongue against anything inserted into their mouths. Most babies grow out of this tongue thrust reflex between 4 and 5 months.
Can You Give a Baby Younger Than 6 Months Infant Cereals?
Most babies are not ready for solid foods, including infant cereals, until they are about 6 months old, though some babies could be ready a month or two earlier. Experts recommend that babies be breastfed or bottle-fed (with expressed breast milk or formula until 6 months of age.
How Do You Prepare Dry Infant Cereal for Your Baby?
If you’re using dry cereal, mix one tablespoon of dry cereal with four tablespoons of breast milk, formula, or water; or follow the recommended directions on the container.
Be sure not serve the cereal from a bottle for reasons we mention in the next section. Gradually, you can add less liquid to the dry cereal to find a thickness your baby likes.
Can You Feed Your Baby Cereal in a Bottle?
Although this might be a practice you’ve heard of, don't feed your baby cereal in a bottle unless your baby’s healthcare provider says otherwise. Feeding your baby through a bottle can lead to unnecessary calories—she may consume more food than she actually needs.
Although rice cereal may have been a popular choice, experts now say there are other infant cereals and first foods that may be safer for your baby. If you’re ever unsure about which infant cereal to give, or need advice about expanding your baby's menu, reach out to your baby’s healthcare provider for advice.
As your baby transitions to solid foods, you deserve lots of rewards for all those diaper changes.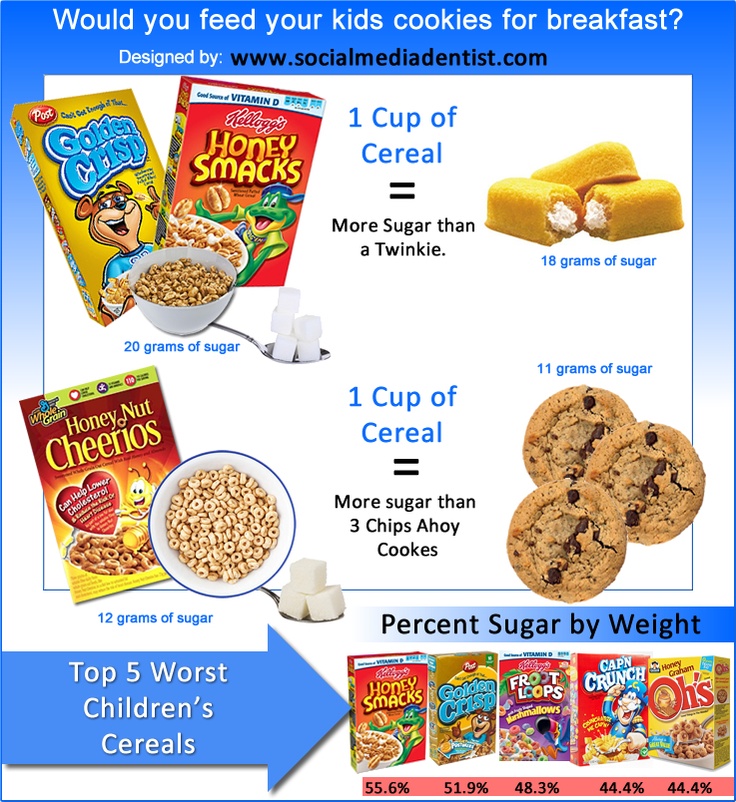 Download the Pampers Club app to get rewards for all your Pampers purchases.
Download the Pampers Club app to get rewards for all your Pampers purchases.
How we wrote this article The information in this article is based on the expert advice found in trusted medical and government sources, such as the American Academy of Pediatrics and the American College of Obstetricians and Gynecologists. You can find a full list of sources used for this article below. The content on this page should not replace professional medical advice. Always consult medical professionals for full diagnosis and treatment.
norm, how many times a day, color
So many experiences are connected with how a newborn baby "walks big". Mom is worried about the frequency of the stool, its color, consistency. So how do you determine if the crumbs are all right with digestion? Perhaps he needs help?
Many mothers know that it is very important to monitor the baby's stool, and during the examination, the pediatrician is always interested in how the baby walks in a big way. This information is one of the most important points in diagnosing the health of the crumbs. Unfortunately, quite often mothers mistakenly interpret the completely natural and safe states of the baby. And because of these mistakes, they can start unnecessary treatment and worry about the baby for no good reason. So let's figure out how a baby's chair should look like and when to worry and when not.
This information is one of the most important points in diagnosing the health of the crumbs. Unfortunately, quite often mothers mistakenly interpret the completely natural and safe states of the baby. And because of these mistakes, they can start unnecessary treatment and worry about the baby for no good reason. So let's figure out how a baby's chair should look like and when to worry and when not.
Immediately after childbirth
When the baby is in the mother's tummy, he receives all the necessary substances and trace elements through the umbilical cord. The digestive system of the crumbs does not work, but his stomach is not empty. The baby sucks his fingers, opens his mouth and thus swallows a small amount of amniotic fluid. When the baby is born, this substance will be in his intestines and will gradually come out as the baby is attached to the chest and his digestive system begins to work.
So, the first stool of the baby is meconium: dark, plasticine-like feces.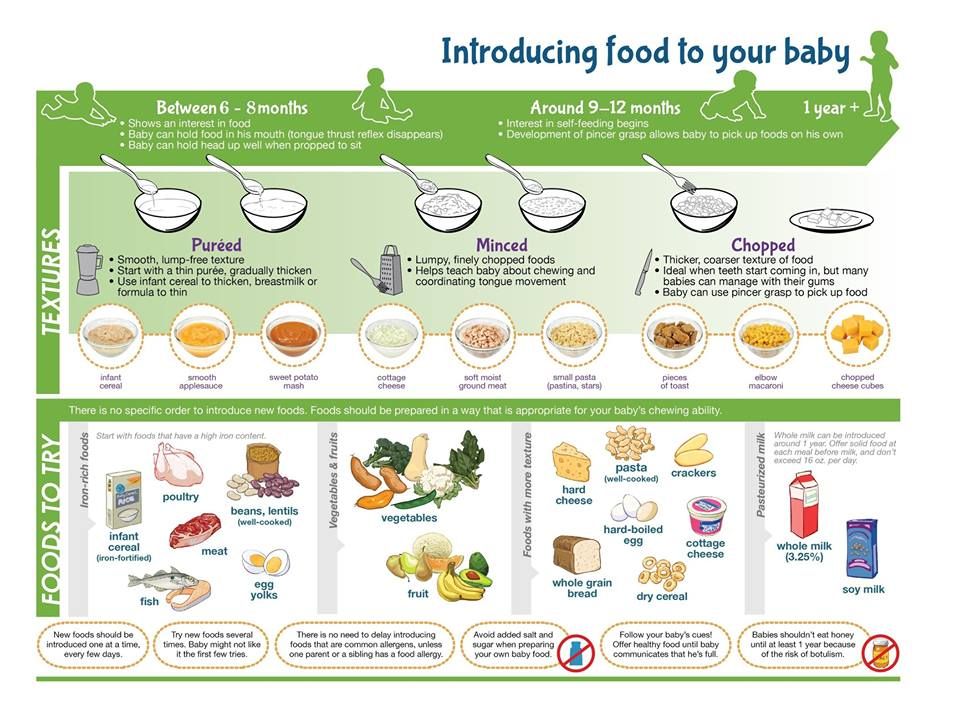 So the baby recovers the first day or two. Sometimes it gives him discomfort: the baby worries, cries, pushes, before he manages to go big. However, this is not always the case - many children recover easily, only slightly pushing.
So the baby recovers the first day or two. Sometimes it gives him discomfort: the baby worries, cries, pushes, before he manages to go big. However, this is not always the case - many children recover easily, only slightly pushing.
If everything is in order with the baby, he was put to the breast in time and fed on demand, then his stool gradually changes. On the third or fifth day, the baby has the so-called "transitional stool", partly consisting of meconium, which is still in the gastrointestinal tract, partly from digested colostrum and milk. As a rule, streaks appear first in the meconium mass, then the feces gradually turn yellow. By the end of the first week, the baby's stool usually acquires the features of a normal infant: yellow, rather liquid.
When should you worry? If the baby did not go down in a big way in the first two days, it is necessary to consult a doctor. There are children with individual characteristics who will continue to do this less often than most babies. However, the cause of the stool retention should be determined by the doctor. If the crumbs have some kind of problem with intestinal patency, help will be needed immediately, but you should not diagnose your baby without a doctor.
However, the cause of the stool retention should be determined by the doctor. If the crumbs have some kind of problem with intestinal patency, help will be needed immediately, but you should not diagnose your baby without a doctor.
We are at home
On the third or fifth day, the mother receives milk, and the baby has a fairly stable stool by the end of the first week. The literature sometimes says that the stool of newborns is "creamy", and this confuses mothers, who begin to suspect that something is not right with the crumbs. In reality, the stool of a healthy baby is liquid and not always homogeneous. The normal color of feces is yellow and its shades. You may notice lumps, a little mucus - it's not scary. Do not be afraid if the baby's feces have a greenish tint for up to three months due to the immaturity of the liver enzyme systems and the characteristics of bilirubin metabolism, such a condition has the right to be and also does not require treatment.
Many mothers sometimes worry that the baby's stool "suddenly" becomes watery and the baby walks in a big way with abundant gas, a sharp sound. Doctors in this case often suspect lactase deficiency. In reality, things usually go like this. In the period from 3 weeks to a month and a half, the baby has frequent growth spurts, so at certain moments the baby literally “hangs on the chest” to help the mother produce more milk. Within a day or a few, the baby needs to breastfeed more often and longer than before, and the mother begins to suspect that there is not enough milk. As a result, she often begins to shift the baby from one breast to another, and the baby receives mostly "forward" milk, which comes at the beginning of feeding from each breast. This milk is rich in carbohydrates and proteins, the baby is actively growing from it, however, the stool is liquid and gassy because of this milk (sometimes the “result” looks frothy if the baby is held over a pot or basin when he needs to clear out, and the mother can observe the consistency chair). In this situation, there is no need to panic - just the baby does not need to be constantly shifted from one breast to another, fearing that he is starving.
Doctors in this case often suspect lactase deficiency. In reality, things usually go like this. In the period from 3 weeks to a month and a half, the baby has frequent growth spurts, so at certain moments the baby literally “hangs on the chest” to help the mother produce more milk. Within a day or a few, the baby needs to breastfeed more often and longer than before, and the mother begins to suspect that there is not enough milk. As a result, she often begins to shift the baby from one breast to another, and the baby receives mostly "forward" milk, which comes at the beginning of feeding from each breast. This milk is rich in carbohydrates and proteins, the baby is actively growing from it, however, the stool is liquid and gassy because of this milk (sometimes the “result” looks frothy if the baby is held over a pot or basin when he needs to clear out, and the mother can observe the consistency chair). In this situation, there is no need to panic - just the baby does not need to be constantly shifted from one breast to another, fearing that he is starving. Give the baby the opportunity to get "hind" milk, rich in fats, which will not cause flatulence and stay longer in the intestines.
Give the baby the opportunity to get "hind" milk, rich in fats, which will not cause flatulence and stay longer in the intestines.
In this situation (when the baby suddenly begins to clearly suck more milk), the mother may feel insecure and start drinking lactic teas. From this, more carbohydrates again begin to flow into her milk and the baby's stool becomes more liquid and with gases.
Similar problems due to "front" milk occur in the case of improper attachment to the breast, as a result of which the baby swallows the air and interrupts feeding itself, or simply cannot get "hind" milk. The best way out in this situation is to consult with a breastfeeding specialist to correct the application technique and stop panicking that the baby "does not have enough milk."
In short, don't worry if your baby has problems with this type of stool. Of course, the flora of his intestines is unstable, it is just beginning to be established - it takes at least three to four months.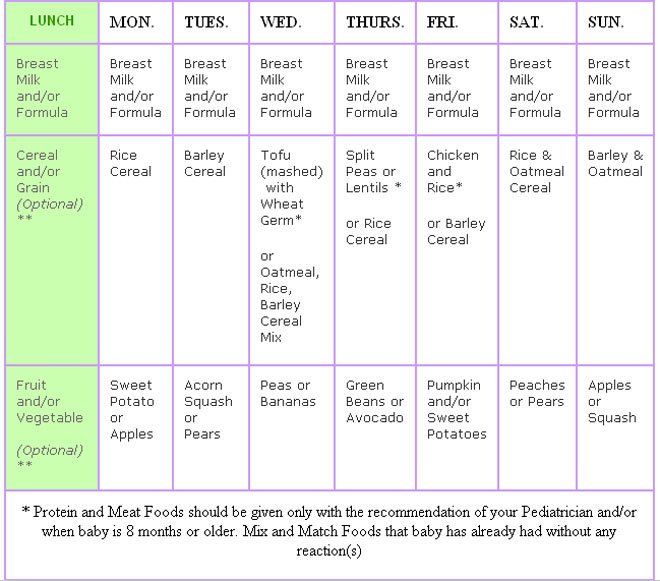 Your task is simply to feed the baby on demand and correctly and not to rush to treat him for imaginary diseases.
Your task is simply to feed the baby on demand and correctly and not to rush to treat him for imaginary diseases.
Delayed stool
Mothers worry not only about the appearance of the stool, but also because of its periodicity. How often should the baby "do things"? Normally, the baby walks in a big way several times a day, usually after feeding. However, in some children, the norm may be a chair and once a day, and even once every few days. Typically, these children have an anatomically weak anterior abdominal wall and intestinal motility. Such a periodicity of the stool can be considered the norm, if the baby still walks more regularly, the stool is of normal consistency and, in general, the baby is cheerful and cheerful and does not suffer from colic. It's not worth worrying. However, if the baby is allergic, then you need to do everything possible so that he goes to the toilet at least once a day. Atopic dermatitis is much more severe if the baby does not empty the intestines often enough - consult a doctor about this.
Babies also have physiological delays in stool at the age of one and a half to five months. Here it is important to monitor the condition of the baby. If he experiences discomfort, you should consult a doctor. Children can hold back their stools for psychological reasons, just as adults sometimes cannot go to the toilet if they are nervous. Do not panic because of a one-time problem, but if the problem persists or recurs, consult your doctor.
However, in babies there are not just "delays" of the stool, but also real constipation. Constipation is called not only when the baby does not go to the toilet at all, but also feces "peas", overdried, when a bowel movement is difficult. What could be the reason?
Regular constipation is usually caused by improper feeding of the crumbs. However, this condition can also occur if the mother does everything right, but she has her own health problems, for example, with the thyroid gland. Medications can also be the cause of constipation. For example, intestinal weakness is provoked by all kinds of sedative mixtures and drugs, which are often prescribed to children by neurologists at an early age. Even cough medicines or tooth gels can cause constipation. In any case, the doctor should deal with this. You should not give your baby medicines and laxatives on your own, or act on it mechanically with an enema or gas tube. It is better to discuss with the doctor the issues of feeding, drug treatment and the lifestyle of the baby - so you can understand the problem.
For example, intestinal weakness is provoked by all kinds of sedative mixtures and drugs, which are often prescribed to children by neurologists at an early age. Even cough medicines or tooth gels can cause constipation. In any case, the doctor should deal with this. You should not give your baby medicines and laxatives on your own, or act on it mechanically with an enema or gas tube. It is better to discuss with the doctor the issues of feeding, drug treatment and the lifestyle of the baby - so you can understand the problem.
Weaning time
Of course, when you start to introduce complementary foods, the baby's stool pattern changes. First of all, you need to remember that the task of the first complementary foods (at 5, 6 months) is not to feed, but to help adapt to new tastes, to new food. Give the baby complementary foods in the amount of "lick" and only gradually move on to doses "with a marigold" or "half a teaspoon". Recall that you need to introduce one product into the diet of crumbs so that you can understand how and what the baby reacts to.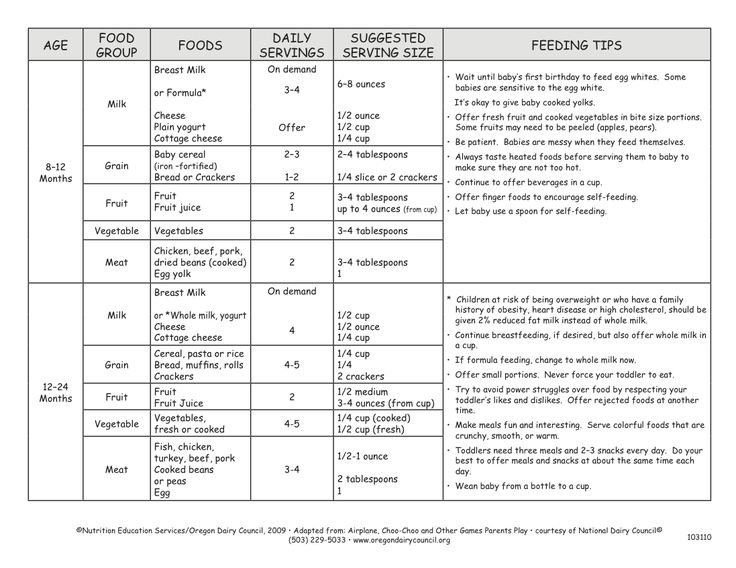 Quite often, as soon as we give the baby “with a fingernail” some food, it is not digested - we find the product in the feces almost in its original form. Within one or two days, this is normal, the baby’s body has not figured out the new component in the stomach, but if this continues on the third day, the product must be removed from the diet, since it is obvious that the baby is not yet ready to accept it. You need to take a break for a week or two, without offering the baby anything but the breast, then try again with another product.
Quite often, as soon as we give the baby “with a fingernail” some food, it is not digested - we find the product in the feces almost in its original form. Within one or two days, this is normal, the baby’s body has not figured out the new component in the stomach, but if this continues on the third day, the product must be removed from the diet, since it is obvious that the baby is not yet ready to accept it. You need to take a break for a week or two, without offering the baby anything but the breast, then try again with another product.
The baby's body can also react more violently, for example, with loose stools and abdominal pain, and sometimes with allergies. In this case, you also need to cancel the product and keep the baby breastfed so that the gastrointestinal tract calms down.
When you introduce protein to your baby, he may react with constipation. To avoid this, you need to remember simple rules. Proteins require more liquid, so if this is your baby's first food (for example, cottage cheese), give him more breast milk. If you started introducing proteins when the baby is already drinking liquid, provide him with a drink. Do not worry about the fact that the introduction of new products has to be postponed - nothing terrible will happen to the baby. And be especially calm about the opinion that at 6-7 months the child needs to be given meat products so that he grows well. Not all children are able to absorb such a protein; for many, even a homogenized meat product at this age will lead to constipation and overload the kidneys. Let the baby eat breast milk for a longer time and receive vegetables and fruits as complementary foods - this way you will avoid many problems with the stool.
If you started introducing proteins when the baby is already drinking liquid, provide him with a drink. Do not worry about the fact that the introduction of new products has to be postponed - nothing terrible will happen to the baby. And be especially calm about the opinion that at 6-7 months the child needs to be given meat products so that he grows well. Not all children are able to absorb such a protein; for many, even a homogenized meat product at this age will lead to constipation and overload the kidneys. Let the baby eat breast milk for a longer time and receive vegetables and fruits as complementary foods - this way you will avoid many problems with the stool.
In general, mothers' concern about baby's stool is quite justified: after all, this is an important diagnostic symptom that allows you to understand a lot about the baby's condition. However, it must be remembered that not all situations require intervention, and most problems can be solved simply by correcting feeding mistakes. Do not rush to treat the baby and resort to medication, start with a diet.
Do not rush to treat the baby and resort to medication, start with a diet.
Text: Anna Babina
Consultant: Olga Ivanovna Tkach, pediatrician, Center for Traditional Obstetrics
Nursing nipple care | Breast Care
Breastfeeding is good for you and your baby, but it can be a real challenge for the nipples. Check out our tips and tricks to help reduce the pain.
Share this information
Sioned Hilton, health visitor, neonatal nurse and lactation consultant:
A mother of three, Sioned Hilton has been supporting families with newborns and young children for over 30 years. She provides advice on breastfeeding and pumping, both in clinics and at home. In addition, Schoned writes articles for parenting magazines, attends conferences, and conducts seminars for attending physicians.
New mothers often hear: "Breastfeeding doesn't have to be painful." However, in the early days, many are faced with the opposite.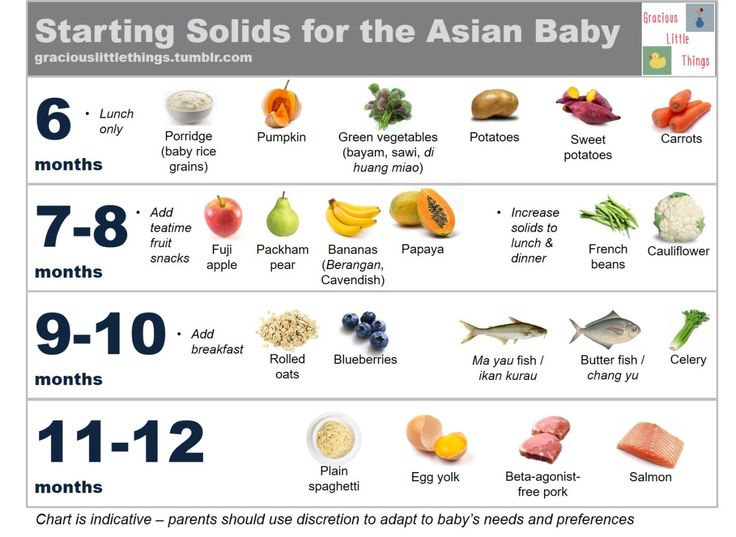
In most women during pregnancy, the nipples enlarge and become more sensitive. When a newborn baby begins to suckle, it creates a certain pressure, and this is a completely new and unfamiliar sensation for a woman (at least for a first-time mother).
Feedings can be prolonged for a long time, sometimes up to an hour, and the child may ask to be breastfed up to 13 times a day. 1 This sucking, pressure and saliva of the baby can cause sore nipples.
Remember how your lips crack in the wind and sun. The more often you lick them, the more they will dry and become inflamed. Therefore, lips require good hydration to soften, protect and speed up the healing of cracks. The same thing happens with nipples.
However, sore nipples usually don't last more than a couple of weeks and go away as your baby and your breasts get used to breastfeeding. It is important to start nipple care as early as possible to prevent the situation from worsening. Therefore, if your nipples become very inflamed, crack or bleed, contact your doctor as soon as possible.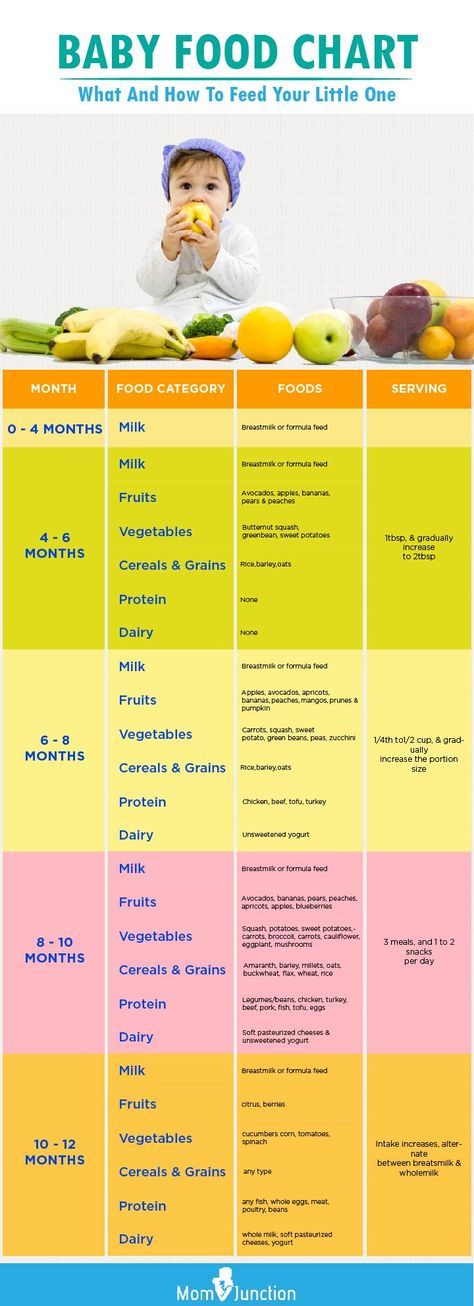 2
2
Prevention is better than cure, so check out our tips.
Check your baby's latch-on
Correct latch is the key to pain-free breastfeeding. When putting the baby to the breast, point the nipple towards his palate. This will allow him to grab the nipple and the part of the areola (the darker skin around the nipple) underneath. When the nipple and part of the breast is in the baby's mouth, feeding is taking place correctly. 3
For the first few days, see a lactation consultant or specialist to check for proper latch. He will be able to give you advice on how to solve problems and recommend other feeding positions that will make it less painful for you to feed your baby.
Check tongue frenulum
Tongue frenulum (ankyloglossia) occurs in 4-11% of
newborns. 4 At the same time, the strip of skin that attaches the tongue to the bottom of the mouth - the so-called frenulum - is too short. A child with a shortened frenulum will not be able to open his mouth wide enough to latch onto the breast well, and his tongue will not cover the lower gum when sucking. As a result, the baby will be nervous, and your nipples may become inflamed.
As a result, the baby will be nervous, and your nipples may become inflamed.
The doctor or lactation consultant must examine the baby to make this diagnosis. The problem of a shortened bridle is solved by a simple undercutting procedure. It is performed by a doctor, and is usually done without blood and does not require anesthesia. Cutting the bridle allows you to restore the normal feeding mechanism almost instantly. 5
Less common in children is a short frenulum of the upper lip. In this case, it is necessary to dissect the skin that connects the upper lip to the gum. A shortened frenum of the tongue or upper lip in a newborn is not always detected during the examination conducted immediately after birth, so if you think that this is what is causing your nipples pain, seek medical advice as soon as possible. 4
Breastfeeding tips for nipples
- Wash your breasts with water only when you shower or bathe. Small bumps on the areola (Montgomery's glands) secrete oil that moisturizes and protects your nipples.
 Soaps and shower gels can strip away this natural defense, causing dryness and irritation. 6
Soaps and shower gels can strip away this natural defense, causing dryness and irritation. 6 - Pat the nipples gently with a soft towel or simply let them air dry. In the past, women were often advised to rub their nipples to make them stiffer, but thankfully, such advice is a thing of the past!
- No need to wash breasts or nipples before feeding. The bacteria found on the surface of the breast actually help the baby's intestinal microflora to develop. 7
- Fresh breast milk helps to heal cracked nipples, 8 so rub a few drops of milk into them before and after feeding.
- Change your bra pads often if they get wet. This will reduce the risk of bacterial and fungal infections, including thrush. 6
- It is not necessary to increase the intervals between feedings to give the nipples a "rest". For a baby to be healthy and grow well, it needs to be fed on demand. Remember, frequent feeding stimulates and maintains milk production, so keep feeding despite the pain.
 9
9
Healthy Teat Care Products
- Pure lanolin teat cleaner, a natural product derived from sheep's wool. It moisturizes and promotes healing of the nipples. This cream is safe for the baby, so it does not need to be washed off before feeding.
- Hydrogel Pads* can be applied to sore nipples to relieve pain while feeding and help promote healing. They can even be stored in the refrigerator to enhance the soothing cooling effect.
- Breast pads* fit inside a bra. They help prevent nipple irritation from clothing and have air holes to help nipples heal.
- Nursing bras** are made from breathable material such as cotton or a special fabric that dries quickly and wicks moisture away from sore nipples.
- Nursing pads* are special silicone pads that fit over the nipples. They have small holes through which milk flows when you are breastfeeding. The pads help to protect the skin underneath and help the baby to better latch on to the nipple by making the nipple stiffer.
 Do not use nursing pads for a long time. If you have problems or pain, contact your healthcare professional or lactation consultant.
Do not use nursing pads for a long time. If you have problems or pain, contact your healthcare professional or lactation consultant.
When to Seek Medical Care
The soreness should go away as your nipples and baby get used to breastfeeding. It is worth repeating that the main cause of sore nipples is improper grip. If your lactation consultant has not been able to resolve your pain while feeding, see another specialist and a third if necessary.
If nipple pain persists or if you notice unusual symptoms, talk to your doctor. The appearance of white spots or flakes on the nipples may be a sign of thrush, whitish or bluish nipples may indicate a circulation disorder such as Raynaud's disease (vasospasm), and pus and redness indicate an infection. 2
Literature
1 Kent JC et al. Volume and frequency of breastfeedings and fat content of breast milk throughout the day. Pediatrics. 2006;117(3): e 387-395. - Kent J.S. et al., "Amount and frequency of breastfeeding and fat content of breast milk during the day." Pediatrix (Pediatrics). 2006;117(3):e387-95.
- Kent J.S. et al., "Amount and frequency of breastfeeding and fat content of breast milk during the day." Pediatrix (Pediatrics). 2006;117(3):e387-95.
2 Berens P et al. Academy of Breastfeeding Medicine. ABM Clinical Protocol#26: Persistent pain with breastfeeding. Breastfeeding Medicine. 2016;11(2):46-53. - Behrens, P. et al., Academy of Breastfeeding Medicine, AVM Clinical Protocol #26: Persistence of Breastfeeding Pain. Brestfeed Med (Breastfeeding Medicine). 2016;11(2):46-53.
3 Cadwell K. Latching - On and Suckling of the Healthy Term Neonate: Breastfeeding Assessment. J Midwifery & Women's Health. 2007;52(6):638-42. — Cadwell, K., "Latching and sucking in healthy newborns: evaluation of breastfeeding." F Midwifery Women Health. 2007;52(6):638-642.
4 Segal LM et al. Prevalence, diagnosis, and treatment of ankyloglossia: methodological review. Canadian Family Physician. 2007;53(6):1027-1033. - Segal L.M. et al., Incidence, Diagnosis, and Treatment of Ankyloglossia: A Methodological Review. Canadian Family Physic. 2007;53(6):1027-1033.
5 O'Shea JE et al. Frenotomy for tongue - tie in newborn infants. The Cochrane Library. 2017. - O'Shea J.I. et al., "Dissection of the frenulum in the newborn", The Cochrane Labrery (Cochrane Library), 2017.
6 Jacobs A et al. S3-guidelines for the treatment of inflammatory breast disease during the lactation period. Geburtshilfe und Frauenheilkunde. 2013;73(12):1202-1208. - Jacobs A. et al., "Recommendations S -3 for the treatment of inflammatory diseases of the breast during breastfeeding. Geburtskhilfe und Frauenheilkünde. milk bacterial communities and establishment and development of the infant gut microbiome JAMA pediatrics 2017;171(7):647-654 - P. S. Pannaraj et al., "Bacterial communities in breast milk and their association with the occurrence and development of the neonatal gut microbiome." JAMA pediatric. 2017;171(7):647-654.
8 Mohammadzadeh A et al. The effect of breast milk and lanolin on sore nipples. Saudi medical journal. 2005;26(8):1231-1234. — Mohammedzade A. et al., "Effects of breast milk and lanolin on sore nipples." Saudi Medical Journal. 2005;26(8):1231-1234.
9 Kent JC et al. Principles for maintaining or increasing breast milk production. J Obstet , Gynecol , & Neonatal Nurs . 2012;41(1):114-121. - Kent J.S. et al., "Principles for Maintaining and Increasing Milk Production". J Obstet Ginecol Neoneutal Nurs. 2012;41(1):114-121.