10 week old baby sick after feeding
Reflux in babies - NHS
Reflux is when a baby brings up milk, or is sick, during or shortly after feeding. It's very common and usually gets better on its own.
Check if your baby has reflux
Reflux usually starts before a baby is 8 weeks old and gets better by the time they're 1.
Symptoms of reflux in babies include:
- bringing up milk or being sick during or shortly after feeding
- coughing or hiccupping when feeding
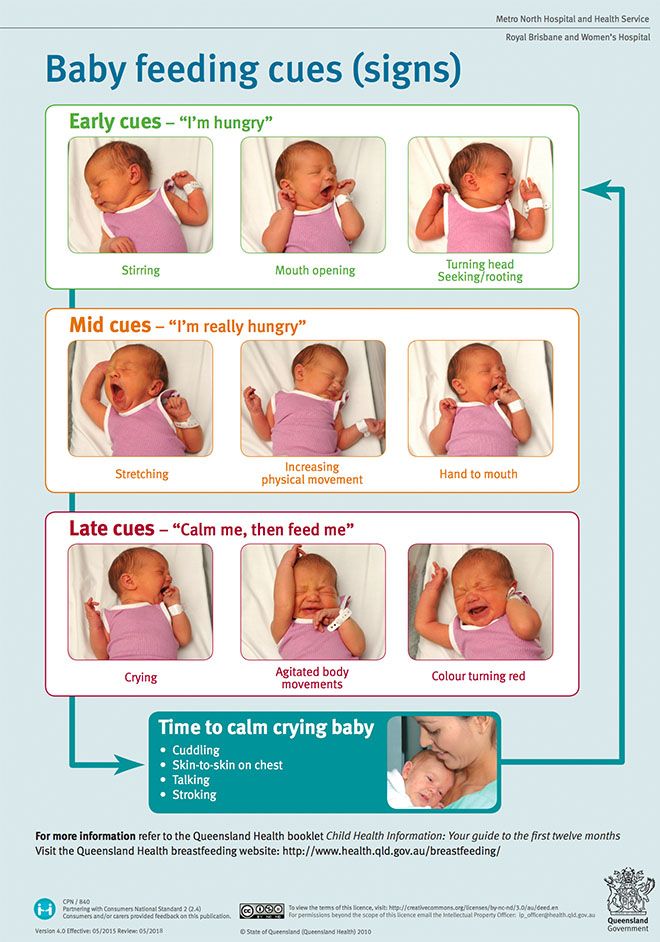
- being unsettled during feeding
- swallowing or gulping after burping or feeding
- crying and not settling
- not gaining weight as they're not keeping enough food down
Sometimes babies may have signs of reflux but will not bring up milk or be sick. This is known as silent reflux.
Things you can try to ease reflux in babies
Your baby does not usually need to see a doctor if they have reflux, as long as they're happy, healthy and gaining weight.
Do
-
ask a health visitor for advice and support
-
get advice about your baby's breastfeeding position or how to bottle feed your baby
-
hold your baby upright during feeding and for as long as possible after feeding
-
burp your baby regularly during feeds
-
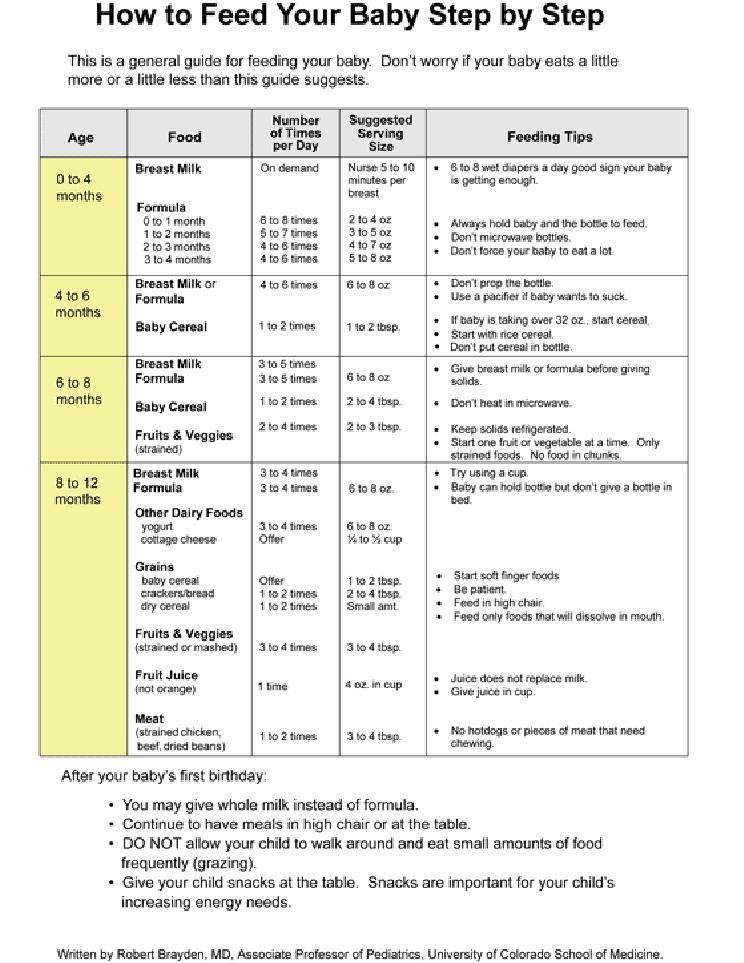
give formula-fed babies smaller feeds more often
-
make sure your baby sleeps flat on their back (they should not sleep on their side or front)
Non-urgent advice: See a GP if your baby:
- is not improving after trying things to ease reflux
- gets reflux for the first time after they're 6 months old
- is older than 1 and still has reflux
- is not gaining weight or is losing weight
Urgent advice: Ask for an urgent GP appointment or call 111 if your baby:
- has vomit that's green or yellow, or has blood in it
- is projectile vomiting (being sick with more force than usual)
- has blood in their poo
- has a swollen or tender tummy
- has a very high temperature or they feel hot or shivery
- keeps being sick and cannot keep fluid down
- has diarrhoea that lasts for over a week or has signs of dehydration
- will not stop crying and is very distressed
- is refusing to feed
Also call your GP or 111 if you have any other concerns about your baby.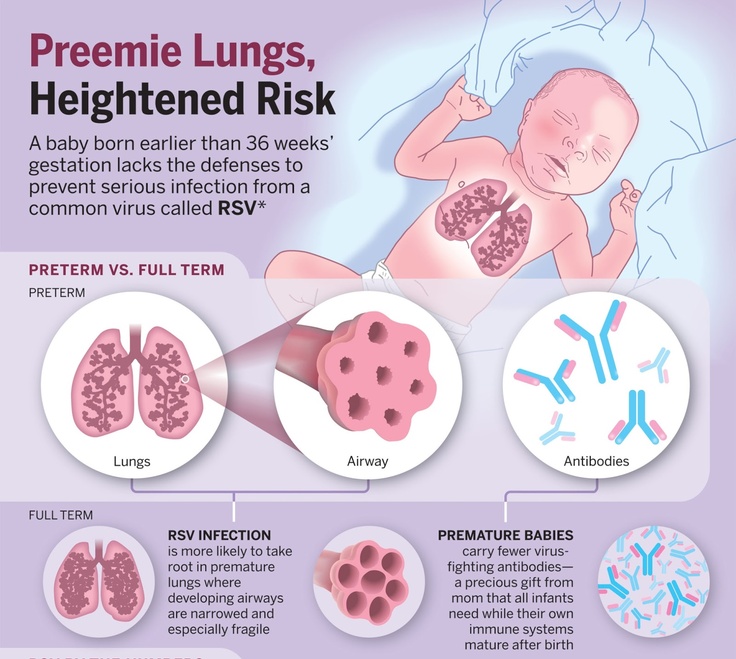
Treatment for reflux in babies
A GP or specialist may sometimes recommend treatments for reflux.
If your baby is formula-fed, you may be given:
- a powder that's mixed with formula to thicken it
- a pre-thickened formula milk
If the thickening powder does not help or your baby is breastfed, a GP or specialist might recommend medicines that stop your baby's stomach producing as much acid.
Very rarely, surgery might be needed to strengthen the muscles to stop food or milk travelling back up. This is usually only after trying other things or if their reflux is severe.
Causes of reflux
Reflux usually happens because your baby's food pipe (oesophagus) has not fully developed, so milk can come back up easily.
Your baby's oesophagus will develop as they get older and the reflux should stop.
Page last reviewed: 13 December 2021
Next review due: 13 December 2024
Vomiting (0-12 Months)
Is this your child's symptom?
- Vomiting (throwing up) stomach contents
- Other names for vomiting are puking, barfing and heaving
Causes of Vomiting
- Viral Gastritis. Stomach infection from a stomach virus is the most common cause. Also called stomach flu. A common cause is the Rotavirus. The illness starts with vomiting. Watery loose stools may follow within 12-24 hours.
- Food Allergy. Vomiting can be the only symptom of a food reaction. The vomiting comes on quickly after eating the food. Uncommon in infants, but main foods are eggs and peanut butter.
- Coughing. Hard coughing can also cause your child to throw up. This is more common in children with reflux.
- Serious Causes. Vomiting alone should stop within about 24 hours. If it lasts over 24 hours, you must think about more serious causes. An example is a kidney infection. A serious cause in young babies is pyloric stenosis. See below for more on this.
Pyloric Stenosis (Serious Cause)
- The most common cause of true vomiting in young babies.
- Onset of vomiting is age 2 weeks to 2 months
- Vomiting is forceful. It becomes projectile and shoots out.
- Right after vomiting, the baby is hungry and wants to feed. ("hungry vomiter")
- Cause: The pylorus is the channel between the stomach and the gut. In these babies, it becomes narrow and tight.
- Risk: Weight loss or dehydration
- Treatment: Cured by surgery.
Vomiting Scale
- Mild: 1 - 2 times/day
- Moderate: 3 - 7 times/day
- Severe: Vomits everything, nearly everything or 8 or more times/day
- Severity relates even more to how long the vomiting goes on for.
 At the start of the illness, it's common for a child to vomit everything. This can last for 3 or 4 hours. Children then often become stable and change to mild vomiting.
At the start of the illness, it's common for a child to vomit everything. This can last for 3 or 4 hours. Children then often become stable and change to mild vomiting. - The main risk of vomiting is dehydration. Dehydration means the body has lost too much fluid.
- The younger the child, the greater the risk for dehydration.
Dehydration: How to Tell
- The main risk of vomiting is dehydration. Dehydration means the body has lost too much water.
- Vomiting with watery diarrhea is the most common cause of dehydration.
- Dehydration is a reason to see a doctor right away.
- Your child may have dehydration if not drinking much fluid and:
- The urine is dark yellow and has not passed any in over 8 hours.
- Inside of the mouth and tongue are very dry.
- No tears if your child cries.
- Slow blood refill test: Longer than 2 seconds. First, press on the thumbnail and make it pale. Then let go. Count the seconds it takes for the nail to turn pink again.
 Ask your doctor to teach you how to do this test.
Ask your doctor to teach you how to do this test.
When to Call for Vomiting (0-12 Months)
Call 911 Now
- Can't wake up
- Not moving
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Dehydration suspected. No urine in over 8 hours, dark urine, very dry mouth and no tears.
- Stomach pain when not vomiting. Exception: stomach pain or crying just before vomiting is quite common.
- Age less than 12 weeks old with vomiting 2 or more times. Exception: normal spitting up.
- Vomited 3 or more times and also has diarrhea
- Severe vomiting (vomits everything) more than 8 hours while getting Pedialyte (or breastmilk)
- Head injury within the last 24 hours
- Weak immune system. Examples are sickle cell disease, HIV, cancer, organ transplant, taking oral steroids.
- Vomiting a prescription medicine
- Fever over 104° F (40° C)
- Fever in baby less than 12 weeks old.
 Caution: Do NOT give your baby any fever medicine before being seen.
Caution: Do NOT give your baby any fever medicine before being seen. - Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Contact Doctor Within 24 Hours
- All other infants (age less than 1 year) with vomiting. See Care Advice while waiting to discuss with doctor.
Seattle Children's Urgent Care Locations
If your child’s illness or injury is life-threatening, call 911.
- Bellevue
- Everett
- Federal Way
- Seattle
Care Advice for Vomiting
- What You Should Know About Vomiting:
- Most vomiting is caused by a viral infection of the stomach.
- Vomiting is the body's way of protecting the lower gut.
- The good news is that stomach illnesses last only a short time.
- The main risk of vomiting is dehydration. Dehydration means the body has lost too much fluid.
- Here is some care advice that should help.
- Most vomiting is caused by a viral infection of the stomach.
- Formula Fed Babies - May Give Oral Rehydration Solution (ORS) for 8 Hours:
- If vomits once, give half the regular amount of formula every 1 to 2 hours.
- If vomits formula more than once, offer ORS for 8 hours. If you don't have ORS, use formula until you can get some.
- ORS is a special fluid that can help your child stay hydrated. You can use Pedialyte or the store brand of ORS. It can be bought in food stores or drug stores.
- Spoon or syringe feed small amounts. Give 1-2 teaspoons (5-10 mL) every 5 minutes.
- After 4 hours without throwing up, double the amount.
- Return to Formula. After 8 hours without throwing up, go back to regular formula.

- Breastfed Babies - Reduce the Amount Per Feeding:
- If vomits once, nurse half the regular time every 1 to 2 hours.
- If vomits more than once, nurse for 5 minutes every 30 to 60 minutes. After 4 hours without throwing up, return to regular nursing.
- If continues to vomit, switch to pumped breastmilk. (ORS is rarely needed in breastfed babies. It can be used if vomiting becomes worse).
- Spoon or syringe feed small amounts of pumped milk. Give 1-2 teaspoons (5-10 mL) every 5 minutes.
- After 4 hours without throwing up, return to regular feeding at the breast. Start with small feedings of 5 minutes every 30 minutes. As your baby keeps down the smaller amounts, slowly give more.
- Pumped Breastmilk Bottle-Fed Infants - Reduce the Amount per Feeding:
- If vomits once and bottle-feeding breastmilk, give half the regular amount every 1-2 hours.
- If vomits more than once within last 2 hours, give 1 ounce (30 mL) every 30 to 60 minutes.

- If continues to vomit, give 1-2 teaspoons (5-10 mL) every 5 minutes. Only if not tolerating breastmilk, switch to ORS (e.g., Pedialyte) for every 5 minutes for a few hours.
- After 4 hours without vomiting, return to regular feedings. Start with 1 ounce (30 mL) every 30 minutes and slowly increase as tolerated.
- Stop All Solid Foods:
- Avoid all solid foods and baby foods in kids who are vomiting.
- After 8 hours without throwing up, gradually add them back.
- If on solid foods, start with starchy foods that are easy to digest. Examples are cereals, crackers and bread.
- Do Not Give Medicines:
- Stop using any drug that is over-the-counter for 8 hours. Reason: Some of these can make vomiting worse.
- Fever. Mild fevers don't need to be treated with any drugs. For higher fevers, you can use an acetaminophen suppository (such as FeverAll). This is a form of the drug you put in the rectum (bottom).
 Ask a pharmacist for help finding this product. Do not use ibuprofen. It can upset the stomach.
Ask a pharmacist for help finding this product. Do not use ibuprofen. It can upset the stomach. - Call your doctor if: Your child vomits a drug ordered by your doctor.
- Try to Sleep:
- Help your child go to sleep for a few hours.
- Reason: Sleep often empties the stomach and removes the need to vomit.
- Your child doesn't have to drink anything if his stomach feels upset and he doesn't have any diarrhea.
- Return to Child Care:
- Your child can return to child care after the vomiting and fever are gone.
- What to Expect:
- For the first 3 or 4 hours, your child may vomit everything. Then the stomach settles down.
- Vomiting from a viral illness often stops in 12 to 24 hours.
- Mild vomiting and nausea may last up to 3 days.
- Call Your Doctor If:
- Vomits clear fluids for more than 8 hours
- Vomiting lasts more than 24 hours
- Blood or bile (green color) in the vomit
- Stomach ache present when not vomiting
- Dehydration suspected (no urine in over 8 hours, dark urine, very dry mouth, and no tears)
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Last Reviewed: 02/19/2023
Last Revised: 12/30/2022
Copyright 2000-2023 Schmitt Pediatric Guidelines LLC.
Memo for discharge from the maternity hospital
Memo for discharge from the maternity hospital
The first month of life (the neonatal period) is the period of the child's getting used to new living conditions. He now has a different environment and a different diet. You and your little one are getting used to each other again. We hope that our memo will help you during this period. You will succeed! Love works wonders. We wish you success!
Feed your baby on demand, and if the baby does not wake up for more than 3 hours, you can try to wake him up for feeding, including at night. Keep your baby on your chest for at least 20 minutes. Do not give your child any drink or food or food other than your own milk unless your pediatrician has specifically prescribed it for you.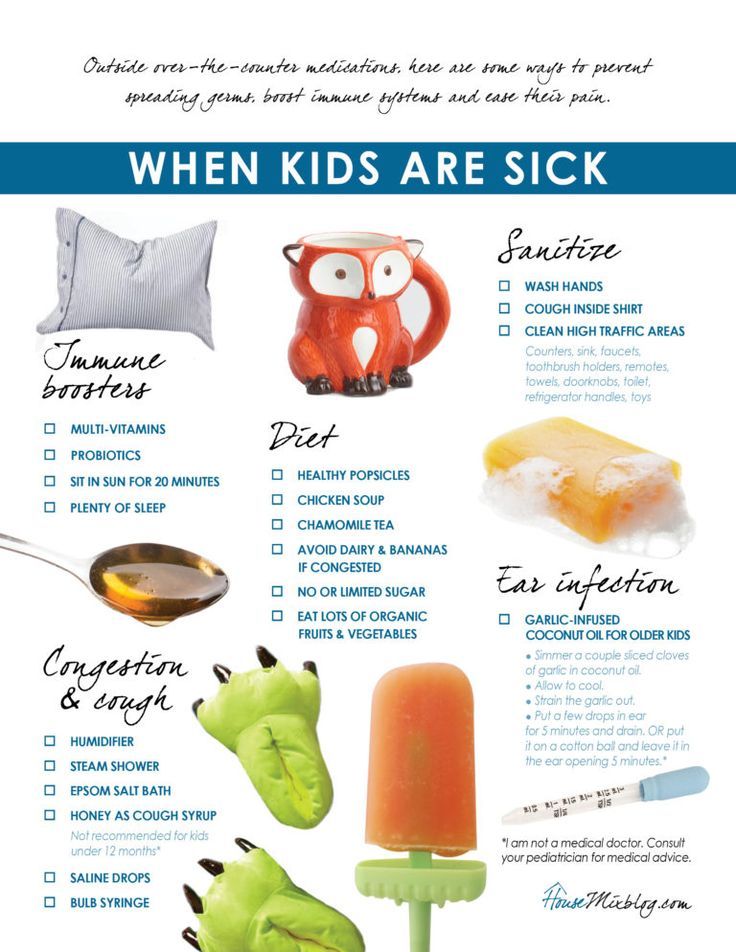 There is no need to express milk, just give the baby the opportunity to completely empty the breast, and then there will be as much milk as necessary. If, in your opinion, the child is not full, you can offer him another breast, but on the next feeding, start with the breast from which you finished feeding.
There is no need to express milk, just give the baby the opportunity to completely empty the breast, and then there will be as much milk as necessary. If, in your opinion, the child is not full, you can offer him another breast, but on the next feeding, start with the breast from which you finished feeding.
The temperature in the room where the baby is located should be 22 - 25 degrees (if your baby weighs more than 3 kg). At this temperature, the baby can be dressed in a diaper, sliders, a blouse with a long sleeve. If his feet are cold, then you can wear socks. You don't need to wear a hat. Short air baths are useful for strengthening the child's immunity. They are carried out during dressing, leaving him naked for 5-7 minutes. Do not swaddle your baby in diapers. For many months he was able to move freely, and when he became too crowded, he was born to find a new freedom. You need to change the vest at least 2 times a day (in the morning and in the evening after bathing), and sliders as they get dirty.
Ventilate the room at least 3 times a day. During airing, take the baby to another room or dress a little warmer (put on a hat, cover with a blanket).
It is possible to bathe a child even if the umbilical cord has not fallen off. Just dry the umbilical cord after bathing. Wash your child every time after a bowel movement. If the child has only urinated, there is no need to wash. Wash the girl from front to back. Do not allow your child to be in a soiled diaper. It is not necessary to boil water. Potassium permanganate should not be added to water - it “dries the skin” and kills not only “harmful”, but also “beneficial” microbes for our blood. Not more than 2 times a week, you can add a decoction of the children's bathing collection to the water. With soap, crumbs should be washed only once a week. The temperature of the water for bathing is 36 - 37 ° C, and for rinsing after bathing is 35 - 36 ° C. Water should be poured so much that the baby's body is completely covered with water. Do not be afraid that water will get into the ears (child up to 9lived in the water for months, and, as an adult, he will swim and dive) just dry them after bathing and put on a hat until your hair is dry. Where you bathe, the air temperature should be at least 22 °C. If you bathe in a room, do not forget to cover the window.
Do not be afraid that water will get into the ears (child up to 9lived in the water for months, and, as an adult, he will swim and dive) just dry them after bathing and put on a hat until your hair is dry. Where you bathe, the air temperature should be at least 22 °C. If you bathe in a room, do not forget to cover the window.
After bathing, pat dry with a soft towel. Do not rub the skin, it is very delicate. Treat the folds with vaseline (or baby) oil. First behind the ears, then the neck, armpits, elbow creases, popliteal, inguinal and buttocks. When using disposable diapers, lubricate the skin of the buttocks with a special diaper cream.
If the umbilical cord hasn't fallen off, don't worry. By 2 weeks of age, shedding usually occurs on its own. If this does not happen, your pediatric health visitor or your local pediatrician will advise you.
The most important thing is to keep the cord clean and dry. If the umbilical cord has fallen off, then the so-called umbilical wound is formed. It can be treated with a 0.5% alcohol solution of chlorhexidine, it can be treated with an alcohol solution of brilliant green. Stretch the edges of the umbilical wound well with a cotton swab moistened with one of the listed solutions, treat the wound in a circle from the inside out. If the umbilical wound is dry and clean throughout the day, the skin around the normal color after bathing, simply dry it with a clean cotton swab. If the skin around the umbilical wound is reddened or pus or cloudy whitish discharge comes out of the wound, seek medical attention immediately.
It can be treated with a 0.5% alcohol solution of chlorhexidine, it can be treated with an alcohol solution of brilliant green. Stretch the edges of the umbilical wound well with a cotton swab moistened with one of the listed solutions, treat the wound in a circle from the inside out. If the umbilical wound is dry and clean throughout the day, the skin around the normal color after bathing, simply dry it with a clean cotton swab. If the skin around the umbilical wound is reddened or pus or cloudy whitish discharge comes out of the wound, seek medical attention immediately.
Wash your child in the morning using cotton wool soaked in boiled water, and when the child grows up, wash under running water, just as you wash yourself. Washing your baby's eyes is only necessary if it is specifically recommended by your doctor. If necessary, you can clean the baby's nose (because if nasal breathing is difficult, the baby cannot suckle the breast). Remember that when cleaning the auditory and nasal passages, do not use hard objects.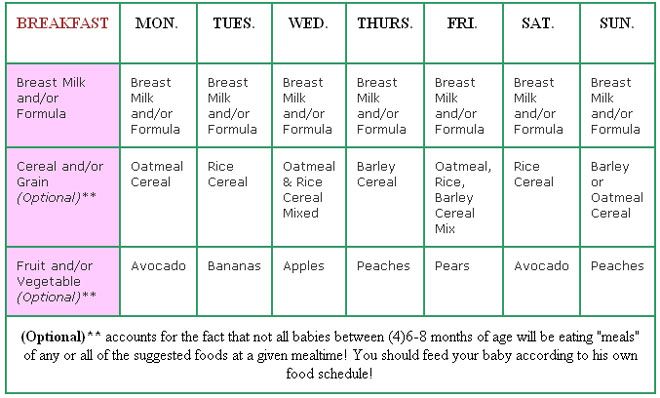 Twist the cotton flagellum between your fingers or palms, moisten it with vaseline oil and clean the nasal passages in turn with rotational movements. Sometimes 3 to 4 drops of saline in each nasal passage can help. The ear canals do not need to be cleared. You can only clean the auricle (for example, if the child burped up and milk got into the ear). If you think that the ear canal still needs to be cleaned, then seek the help of medical professionals. Never drip your milk into your baby's nose, eyes, or ears. It is a breeding ground for microbes.
Twist the cotton flagellum between your fingers or palms, moisten it with vaseline oil and clean the nasal passages in turn with rotational movements. Sometimes 3 to 4 drops of saline in each nasal passage can help. The ear canals do not need to be cleared. You can only clean the auricle (for example, if the child burped up and milk got into the ear). If you think that the ear canal still needs to be cleaned, then seek the help of medical professionals. Never drip your milk into your baby's nose, eyes, or ears. It is a breeding ground for microbes.
Trim your nails very carefully with special scissors. First, treat the scissors and nails with alcohol, then carefully trim the nails.
Never leave your child on a table, bed or sofa unattended (even if you think he cannot roll over). In general, do not leave the child alone for a long time! Co-sleeping in the same bed with parents (and with other children) is not safe from the point of view of possible asphyxia. Co-sleeping can be a risk factor for suffocation of the baby. Sleeping in the parent's bedroom is optimal, but not in the parent's bed. Place the crib next to yours, lower the side rail. On the one hand, this will ensure the safety of the baby, on the other hand, you will be in close proximity to your child and you will not have to jump up several times at night. It will be convenient for you to feed the baby at night, and then, without getting up, shift it to the crib.
Sleeping in the parent's bedroom is optimal, but not in the parent's bed. Place the crib next to yours, lower the side rail. On the one hand, this will ensure the safety of the baby, on the other hand, you will be in close proximity to your child and you will not have to jump up several times at night. It will be convenient for you to feed the baby at night, and then, without getting up, shift it to the crib.
We wish you and your baby health and happiness and are always ready to help you. If you have any difficulties, you can consult by phone about breastfeeding or the child's condition.
Contact number of the breastfeeding support group: 8(8443)31-71-43, 8(8443)31-01-89
Conditions requiring urgent consultation with the local doctor:
esophagus and genus) of milk that has just been eaten, but not yet digested in the stomach. Regurgitation may occur during or immediately after feeding. If the number of regurgitations per day is more than 5, they are plentiful and come out like a fountain, while the child slowly gains or loses weight, is restless, does not sleep well and often cries - these are reasons for immediate medical attention.
2. Colic is a bout of irritability, excitement or crying in children associated with pain in the intestines due to excessive gas formation. Often, colic occurs during feeding: the child suddenly screams, behaves restlessly, draws his legs. Episodes of anxiety lasting more than 3 hours a day and at least 3 days a week require medical attention.
3. The stool of a newborn should be homogeneous, mushy, free of blood and mucus. If the child's intestines are emptied less than 1 time in 2 days and there is anxiety, bloating, decreased appetite, and the presence of frequent watery stools, a consultation is required.
4. A healthy baby sleeps 18 to 22 hours a day. He wakes up, asks for breasts, begins to suck, and here at the breast again falls asleep, having completed the meal. Reduced activity and lethargy during the day are indications for examining a child.
5. The appearance and intensification of jaundice after 3 days (jaundice is a condition in which the level of bilirubin in the blood rises, which is deposited in the tissues, gives the skin, mucous membranes and eyeball proteins a tint from lemon to orange), pallor, marbling, cyanosis - indications for visiting a doctor.
Best regards, staff of the perinatal center No. 1
If a child falls ill - articles from the specialists of the clinic "Mother and Child"
Archegova Galina Altafovna
Gastroenterologist, Gastroenterologist for children, Nutritionist
MD GROUP Clinical Hospital
It is known that children in the first months of life rarely get sick, for example, SARS. This is due not only to the fact that they do not visit public places, but also to the fact that there are protective factors in their blood that were passed on to them by their mothers. Gradually, the level of these factors decreases, and the likelihood of respiratory disease, respectively, increases.
If a child of the first 6 months of life has a viral infection, which theoretically should be protected by immunity inherited from the mother, then this is a situation that goes beyond the norm. Therefore, in this case, you should immediately consult a doctor. Even if the disease is mild, only in the form of a runny nose and sneezing.
Even if the disease is mild, only in the form of a runny nose and sneezing.
If a child of the second half of life, who already “has the right” to get sick, falls ill, then in cases of a mild form of the disease with a temperature within 38 °, with minor symptoms of a cold, one can independently, based on one’s own experience, begin treatment using certain means.
It has been known for many years that one of the protective factors, interferon, is weakly secreted at temperatures below 38°C, which can weaken the immune response in general. Therefore, there is no reason to consider a decrease in temperature in all cases as necessary. In addition, the use of antipyretics can lead to side effects.
When the temperature rises, the skin vessels dilate, which allows the body to balance heat production and heat loss. Therefore, it is not necessary to wrap up a feverish child, to cover him with blankets, this can only impede heat transfer. There is no need to be afraid that the temperature will “roll over the top”, will rise indefinitely. In the vast majority of patients, the temperature does not exceed 39°. However, at higher temperatures, the heat output may not match its products.
In the vast majority of patients, the temperature does not exceed 39°. However, at higher temperatures, the heat output may not match its products.
Such a situation - it is called a malignant temperature - is extremely dangerous. It is not difficult to recognize it - while the surface of the child's body acquires a motley "marble" color, the skin, especially the hands and feet, remains cold despite the fever. In these cases, it is necessary to rub the skin vigorously until it turns red and give an antipyretic. A child with a fever should be put to bed and provided with plenty of fluids to prevent excessive fluid loss.
If a child is ill, the first thing to do is DON'T PANIC. Most problems are born out of panic. Call your pediatrician immediately.
Before he arrives, take a temperature measurement.
Make sure that the room where the child is located is ventilated and the air is fresh. Don't forget to increase your drinking. Experts note that if the child drinks enough, then you can not be afraid that the temperature will pose a danger to him.
There is a very small group of children who, in response to any infection, overreact, that is, they immediately develop a high temperature, heart and lung failure, loss of consciousness, convulsions immediately occur. Therefore, if a child's temperature creeps up, despite the measures you take, the bill goes to hours and minutes.
The easiest and best way out in this situation is to call an emergency aid or a pediatrician and hospitalize the baby in a hospital, where all the necessary examinations will be performed and treatment prescribed, and, most importantly, the child will be under the supervision of a doctor around the clock, since the children have a condition can get heavy in a matter of hours.
As the head of the children's consultative and diagnostic center of the Perinatal Medical Center, which includes not only a polyclinic, but also a boxed department for infants and older children, I categorically do not advise you to go to hospitals yourself, “choosing” a hospital. For this, there is emergency care, which, in accordance with the diagnosis, will take the child to a specialized medical institution, depending on the availability of vacant places in it.
For this, there is emergency care, which, in accordance with the diagnosis, will take the child to a specialized medical institution, depending on the availability of vacant places in it.
I would like to note that the conditions of his stay in the hospital are of great importance for a child, especially at an early age. Individual wards - boxes, round-the-clock stay of a mother with a child, everything necessary for a comfortable stay, modern materials in interior decoration, colors of walls and floors - taking into account the favorable psychological impact on the child - all this is available in the rehabilitation department of the Perinatal Medical Center. In addition, the uniqueness of this department for Moscow lies in the fact that the Center has not only a children's hospital, but also a polyclinic children's department, and specialized traveling children's teams. Thus, the principles of continuity and phasing are fully respected. In the event of a critical situation, a team of pediatricians goes to provide medical assistance and, if necessary, the child is transported to the children's boxed department. Therefore, it is not for nothing that the medical staff of the PMC departments is considered one of the most qualified, because they have to deal with the most difficult situations.
Therefore, it is not for nothing that the medical staff of the PMC departments is considered one of the most qualified, because they have to deal with the most difficult situations.
Of course, a child's illness is a misfortune. But faith in the successful resolution of the situation, in the child’s own strengths and strengths, and the professionalism of doctors can work wonders. The purpose of our article is not to intimidate future and current parents, but to warn. Convince to be as attentive as possible to the health of the child. After all, as you know, forewarned is forearmed. So, if you notice even minimal deviations in the condition of the baby, then do not treat yourself, consult your doctor.
For every family, the most important thing in life is the happiness and health of their child. But, unfortunately, children often get sick. We sincerely wish you and your children good health, but if the child gets sick, try to "pull yourself together" and do not panic! Your task is to help your child as much as possible! Emotions should fade into the background.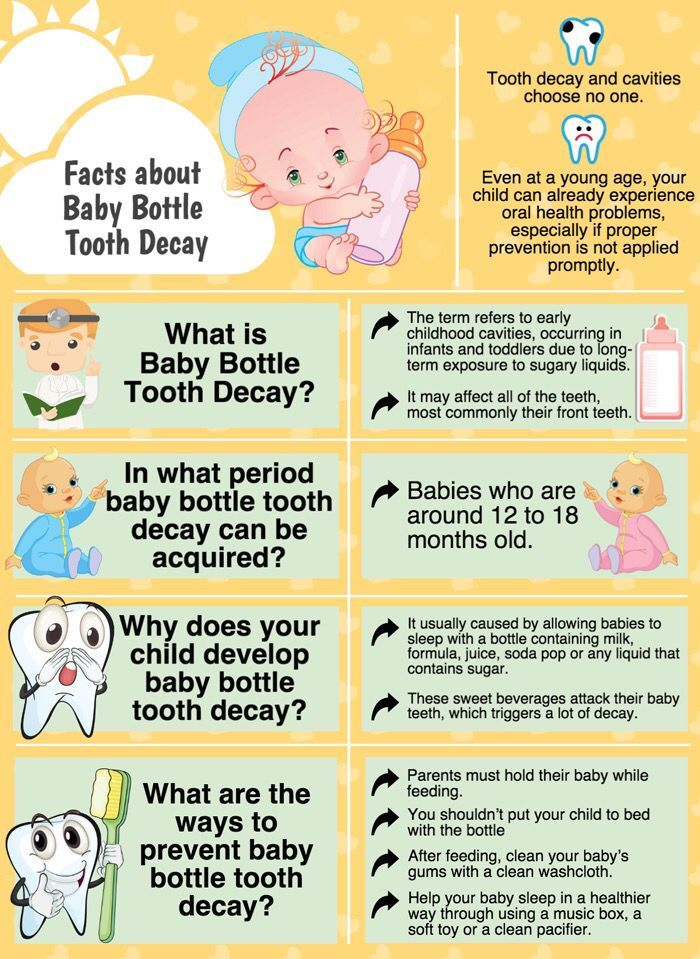
Make an appointment
to the doctor - Archegova Galina Altafovna
Clinical Hospital MD GROUP
Gastroenterology Pediatric gastroenterology
By clicking on the send button, I consent to the processing of personal data
Attention! Prices for services in different clinics may vary. To clarify the current cost, select the clinic
The administration of the clinic takes all measures to update the prices for programs in a timely manner, however, in order to avoid possible misunderstandings, we recommend that you check the cost of services by phone / with the managers of the clinic
Clinical Hospital MD GROUPClinical Hospital Lapino-1 "Mother and Child"Children's Clinic KG "Lapino" in New Riga (branch)Clinic "Mother and Child" KuntsevoClinic "Mother and Child" SavelovskayaClinic "Mother and Child" South-WestClinic "Mother and child" Novogireevo
All directionsKinesiotherapy for childrenSpecialist consultations (adults)Specialist consultations (children)Massage / manual therapy for childrenTherapeutic research
01.