2 month old baby vomits after feeding
Why This Happens and What to Do
It can be difficult to tell the difference between vomit and spit-up. Both might look the same since your baby is currently on a steady of diet of milk or formula. The main difference is in how they come out.
Spit-up usually happens before or after a burp and is most common in babies under the age of 1 year. Spit-up will easily flow from your baby’s mouth — almost like white, milky drool.
Vomit typically comes out forcefully (whether you’re a baby or an adult). This is because vomiting happens when the muscles around the stomach are triggered by the brain’s “vomiting center” to squeeze it. This forces whatever is in the stomach to be hurled out.
In a baby’s case, vomit may look like milky spit-up but have more clear stomach juices mixed into it. It may also look like milk that has been fermented for a little while — this is called “cheesing.” Yes, it sounds gross. But the texture probably won’t bother you when you see it — you’ll be more concerned with baby’s well-being.
Your baby may also cough or make little retching noises before they vomit. This is likely the only warning you’ll have to grab a towel, bucket, burp cloth, sweater, your shoe — hey, anything.
Additionally, spit-up is normal and can happen at any time. Your baby will only vomit if there’s a digestive issue or they have another illness.
Feeding difficulty
Babies have to learn everything from scratch, including how to feed and keep the milk down. Along with spit-up, your baby may vomit occasionally after being fed. This is most common in the first month of life.
It happens because your baby’s tummy is still getting used to digesting food. They also have to learn to not gulp milk down too fast or overfeed.
Post-feeding vomiting typically stops after the first month. Give your baby more frequent, smaller feeds to help stop the vomit.
But let your pediatrician know if your baby vomits often or has very forceful vomits. In some cases, it might be a sign of something other than feeding difficulty.
Stomach flu
Also known as the tummy bug or “stomach flu,” gastroenteritis is a common cause of vomiting in babies and children. Your baby may have cycles of vomiting that come and go for about 24 hours.
Other symptoms in babies may last for 4 days or longer:
- watery, runny poop or mild diarrhea
- irritability or crying
- poor appetite
- stomach cramps and pain
The tummy bug can also cause a fever, but this is actually less common in babies.
Gastroenteritis usually looks a lot worse than it is (thank goodness!). It’s typically caused by a virus that goes away by itself in about a week.
In babies, severe gastroenteritis can lead to dehydration. Call your pediatrician immediately if your baby has any signs of dehydration:
- dry skin, mouth, or eyes
- unusual sleepiness
- no wet diapers for 8 to 12 hours
- weak cry
- crying without tears
Infant reflux
In some ways, babies really are like tiny adults. Just like adults of any age can have acid reflux or GERD, some babies have infant reflux. This can lead to baby vomiting in the first weeks or months of your baby’s life.
Just like adults of any age can have acid reflux or GERD, some babies have infant reflux. This can lead to baby vomiting in the first weeks or months of your baby’s life.
Vomiting from acid reflux happens when the muscles at the top of the stomach are too relaxed. This triggers baby vomiting shortly after feeding.
In most cases, the stomach muscles strengthen, and your baby’s vomiting goes away on its own. Meanwhile, you can help slow down the vomiting by:
- avoiding overfeeding
- giving smaller, more frequent feeds
- burping your baby often
- propping your baby up in an upright position for about 30 minutes after feeding
You can also thicken milk or formula with more formula or a bit of baby cereal. Caveat: Check with your pediatrician before you try this. It might not be suitable for all babies.
Cold and flu
Babies catch colds and flus easily because they have shiny new immune systems that are still developing. It doesn’t help if they’re in day care with other sniffling kiddos, or they’re around adults that can’t resist kissing their little faces.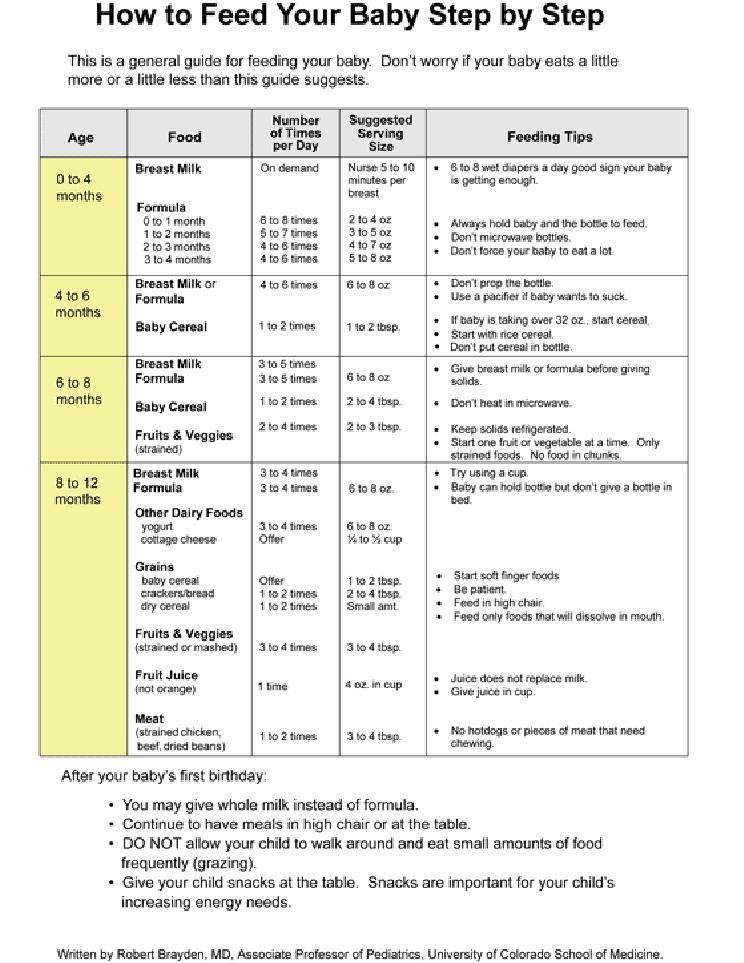 Your baby may have up to seven colds in their first year alone.
Your baby may have up to seven colds in their first year alone.
Cold and flu can cause different symptoms in babies. Along with a runny nose, your baby may also have vomiting without a fever.
Too much mucus in the nose (congestion) can lead to a nasal drip in the throat. This can trigger bouts of forceful coughing that sometimes cause vomiting in babies and children.
As in adults, colds and flu in babies are viral and go away after about a week. In some cases, sinus congestion may turn into an infection. Your baby will need antibiotics to treat any bacterial — not viral — infection.
Ear infection
Ear infections are another common illness in babies and children. This is because their ear tubes are horizontal rather than more vertical like in adults.
If your little one has an ear infection, they might have nausea and vomiting without a fever. This happens because an ear infection can cause dizziness and loss of balance. Other symptoms of ear infections in babies include:
- pain in one or both ears
- tugging or scratching at or near the ears
- muffled hearing
- diarrhea
Most ear infections in babies and children go away without treatment.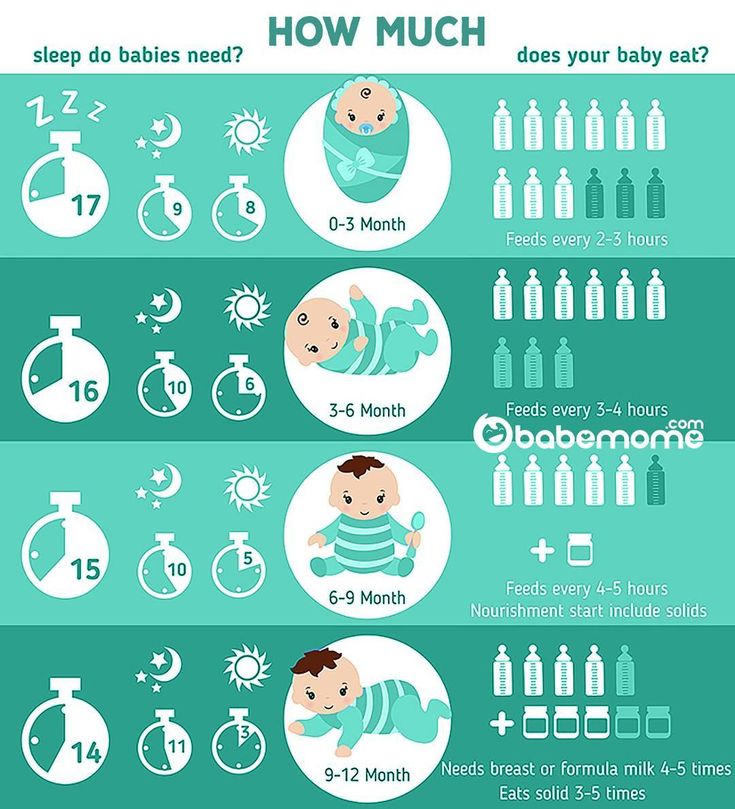 However, it’s important to see a pediatrician in case your baby needs antibiotics to clear up the infection. In rare cases, a serious ear infection can damage a baby’s tender ears.
However, it’s important to see a pediatrician in case your baby needs antibiotics to clear up the infection. In rare cases, a serious ear infection can damage a baby’s tender ears.
Overheating
Before you swaddle your baby or put them in that adorable fluffy bunny suit, check the temperature outside and in your home.
While it’s true that the womb was warm and cozy, babies can overheat quickly in hot weather or in a very warm house or car. This is because their tiny bodies are less able to sweat out heat. Overheating might cause vomiting and dehydration.
Overheating can lead to heat exhaustion or in much more serious cases, heatstroke. Look for other symptoms like:
- pale, clammy skin
- irritability and crying
- sleepiness or floppiness
Immediately remove clothing and keep your baby out of the sun and away from heat. Try to breastfeed (or give your baby water if they’re 6 months or older). Get urgent medical attention if your baby doesn’t seem their usual self.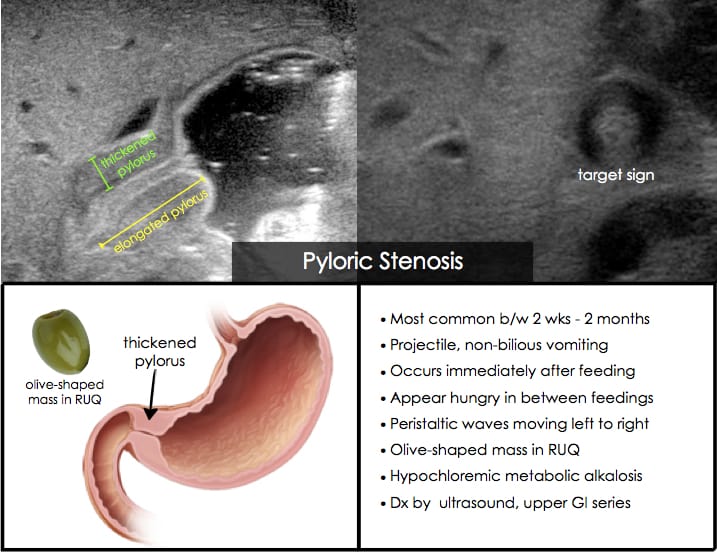
Motion sickness
Babies below the age of 2 years don’t commonly get motion or car sickness, but some babies may get sick after a car ride or being twirled around — especially if they’ve just eaten.
Motion sickness can make your baby dizzy and nauseous, leading to vomiting. It might be more likely to happen if your baby already has an upset tummy from bloating, gas, or constipation.
Strong smells and windy or bumpy roads can also make your baby dizzy. Nausea triggers more saliva, so you might notice more dribble before your baby vomits.
You can help prevent motion sickness by traveling when your baby is ready to sleep. (Great trick if your baby loves to sleep in the car!) A sleeping baby is less likely to feel queasy.
Keep their head well supported in the car seat so it doesn’t move around too much. Also, avoid going for a drive right after giving your baby a full feed — you want your baby to digest the milk, not wear it.
Milk intolerance
A rare kind of milk intolerance is called galactosemia. It happens when babies are born without a certain enzyme needed to break down sugars in milk. Some babies with this condition are even sensitive to breast milk.
It happens when babies are born without a certain enzyme needed to break down sugars in milk. Some babies with this condition are even sensitive to breast milk.
It can cause nausea and vomiting after drinking milk or any kind of dairy products. Galactosemia can also cause a skin rash or itching in both babies and adults.
If your baby is formula fed, check the ingredients for any dairy, including milk proteins.
Most newborns are screened at birth for this rare condition and other illnesses. This is usually done with a heel prick blood test or a urine test.
In the rare event that your baby has this, you’ll know it very early on. Make sure your baby completely avoids milk to help stop vomiting and other symptoms.
Pyloric stenosis
Pyloric stenosis is a rare condition that happens when the opening between the stomach and intestines is blocked or too narrow. It can lead to forceful vomiting after feeding.
If your baby has pyloric stenosis, they may be hungry all the time.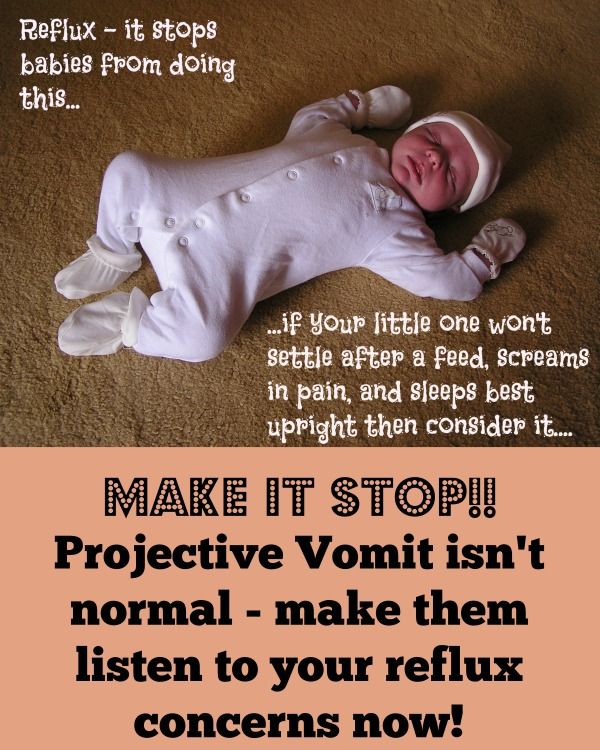 Other symptoms include:
Other symptoms include:
- dehydration
- weight loss
- wave-like stomach contractions
- constipation
- fewer bowel movements
- fewer wet diapers
This rare condition can be treated with surgery. Tell your pediatrician immediately if your baby has any of the symptoms of pyloric stenosis.
Intussusception
Intussusception is a rare intestinal condition. It affects 1 in every 1,200 babies and most commonly happens at the age of 3 months or older. Intussusception can cause vomiting without a fever.
This condition happens when the intestines are damaged by a virus or other health conditions. The damaged intestine slips — “telescopes” — into another part of the intestine.
Along with vomiting, a baby may have severe stomach cramps that last for about 15 minutes. The pain can cause some babies to curl their knees up to their chest.
Other symptoms of this intestinal condition include:
- fatigue and tiredness
- nausea
- blood or mucus in bowel movements
If your baby has intussusception, treatment can push the intestine back into place. This gets rid of vomiting, pain, and other symptoms. Treatment includes using air in the intestines to gently move the intestines. If that doesn’t work, keyhole (laparoscopic) surgery heals this condition.
This gets rid of vomiting, pain, and other symptoms. Treatment includes using air in the intestines to gently move the intestines. If that doesn’t work, keyhole (laparoscopic) surgery heals this condition.
See your baby’s pediatrician if your baby has vomiting for longer than 12 hours. Babies can get dehydrated quickly if they’re vomiting.
Get immediate medical attention if your baby is vomiting and has other symptoms and signs like:
- diarrhea
- pain or discomfort
- constant or forceful coughing
- hasn’t had a wet diaper for 3 to 6 hours
- refusing to feed
- dry lips or tongue
- few or no tears when crying
- extra tired or sleepy
- weakness or floppy
- won’t smile
- swollen or bloated stomach
- blood in diarrhea
Baby vomiting without a fever can happen because of several common illnesses. Your baby will likely have one or more of these several times in the first year. Most of these causes go away on their own, and your little one will stop vomiting without any treatment.
But too much vomiting can lead to dehydration. Check for signs of dehydration and call your pediatrician if you’re not sure.
Some causes of baby vomiting are more serious, but these are rare. Your baby will need medical care for these health conditions. Know the signs and remember to keep the doctor’s number saved in your phone — and take a deep breath. You and baby got this.
Infant Vomiting - HealthyChildren.org
My baby vomits a lot. Is this a sign of a problem?
Because many common childhood illnesses can cause vomiting, you should expect your child to have this problem several times during these early years. Usually it ends quickly without treatment, but this doesn’t make it any easier for you to watch. That feeling of helplessness combined with the fear that something serious might be wrong and the desire to do something to make it better may make you tense and anxious. To help put your mind at ease, learn as much as you can about the causes of vomiting and what you can do to treat your child when it occurs.
Vomiting vs Spitting Up
First of all, there’s a difference between real vomiting and just spitting up. Vomiting is the forceful throwing up of stomach contents through the mouth. Spitting up (most commonly seen in infants under one year of age) is the easy flow of stomach contents out of the mouth, frequently with a burp.
Vomiting occurs when the abdominal muscles and diaphragm contract vigorously while the stomach is relaxed. This reflex action is triggered by the “vomiting center” in the brain after it has been stimulated by:
Nerves from the stomach and intestine when the gastrointestinal tract is either irritated or swollen by an infection or blockage
Chemicals in the blood (e.g., drugs)
Psychological stimuli from disturbing sights or smells
Stimuli from the middle ear (as in vomiting caused by motion sickness)
Causes of Vomiting
The common causes of spitting up or vomiting vary according to age. During the first few months, for instance, most infants will spit up small amounts of formula or breastmilk, usually within the first hour after being fed. This “cheesing,” as it is often called, is simply the occasional movement of food from the stomach, through the tube (esophagus) leading to it, and out of the mouth. It will occur less often if a child is burped frequently and if active play is limited right after meals. This spitting up tends to decrease as the baby becomes older, but may persist in a mild form until ten to twelve months of age. Spitting up is not serious and doesn’t interfere with normal weight gain.
During the first few months, for instance, most infants will spit up small amounts of formula or breastmilk, usually within the first hour after being fed. This “cheesing,” as it is often called, is simply the occasional movement of food from the stomach, through the tube (esophagus) leading to it, and out of the mouth. It will occur less often if a child is burped frequently and if active play is limited right after meals. This spitting up tends to decrease as the baby becomes older, but may persist in a mild form until ten to twelve months of age. Spitting up is not serious and doesn’t interfere with normal weight gain.
Occasional vomiting may occur during the first month. If it appears repeatedly or is unusually forceful, call your pediatrician. It may be just a mild feeding difficulty, but it also could be a sign of something more serious.
Persistent Vomiting
Between two weeks and four months of age, persistent forceful vomiting may be caused by a thickening of the muscle at the stomach exit. Known as hypertrophic pyloric stenosis, this thickening prevents food from passing into the intestines. It requires immediate medical attention. Surgery usually is required to open the narrowed area. The important sign of this condition is forceful vomiting occurring approximately fifteen to thirty minutes or less after every feeding. Anytime you notice this, call your pediatrician as soon as possible.
Known as hypertrophic pyloric stenosis, this thickening prevents food from passing into the intestines. It requires immediate medical attention. Surgery usually is required to open the narrowed area. The important sign of this condition is forceful vomiting occurring approximately fifteen to thirty minutes or less after every feeding. Anytime you notice this, call your pediatrician as soon as possible.
GERD
Occasionally the spitting up in the first few weeks to months of life gets worse instead of better—that is, even though it’s not forceful, it occurs all the time. This happens when the muscles at the lower end of the esophagus become overly relaxed and allow the stomach contents to back up. This condition is known as gastroesophageal reflux disease, or GERD. This condition usually can be controlled by doing the following:
Thicken the milk with small amounts of baby cereal as directed by your pediatrician.
- Avoid overfeeding or give smaller feeds more frequently.

- Burp the baby frequently.
- Leave the infant in a safe, quiet, upright position for at least thirty minutes following feeding.
If these steps are not successful, your pediatrician may refer you to a gastrointestinal (GI) specialist.
Infection
After the first few months of life, the most common cause of vomiting is a stomach or intestinal infection. Viruses are by far the most frequent infecting agents, but occasionally bacteria and even parasites may be the cause. The infection also may produce fever, diarrhea, and sometimes nausea and abdominal pain. The infection is usually contagious; if your child has it, chances are good that some of her playmates also will be affected.
Rotaviruses are a leading cause of vomiting in infants and young children, with symptoms often progressing to diarrhea and fever. These viruses are very contagious, but are becoming less common than in the past, due to the availability of a vaccine that can prevent the disease. The rotavirus is one of the viral causes of gastroenteritis, but other types of viruses—such as noroviruses, enteroviruses, and adenoviruses—can cause it as well.
The rotavirus is one of the viral causes of gastroenteritis, but other types of viruses—such as noroviruses, enteroviruses, and adenoviruses—can cause it as well.
Occasionally infections outside the gastrointestinal tract will cause vomiting. These include infections of the respiratory system, infections of the urinary tract otitis media, meningitis , and appendicitis. Some of these conditions require immediate medical treatment, so be alert for the following trouble signs, whatever your child’s age, and call your pediatrician if they occur.
Blood or bile (a green-colored material) in the vomit
Severe abdominal pain
Strenuous, repeated vomiting
Swollen or enlarged abdomen
Lethargy or severe irritability
Convulsions
Signs or symptoms of dehydration, including dry mouth, absent tears, depression of the "soft spot", and decreased urination
Inability to drink adequate amounts of fluid
Vomiting continuing beyond twenty-four hours
The information contained on this Web site should not be used as a substitute for the medical care and advice of your pediatrician. There may be variations in treatment that your pediatrician may recommend based on individual facts and circumstances.
There may be variations in treatment that your pediatrician may recommend based on individual facts and circumstances.
Regurgitation and vomiting in children
Regurgitation syndrome is one of the most common reasons for parents of young children to visit a pediatrician and a surgeon. The causes of regurgitation in children under 1 year old are different: anatomical and functional features, neurological disorders, infectious processes, malformations or other problems. The mechanism that prevents regurgitation and vomiting in children is very complex and depends on the anatomical structure and physiological processes of the child. The formation of this mechanism occurs in the last trimester of pregnancy and continues in the first months of a child's life. Although regurgitation and vomiting can be a symptom of various diseases, in themselves these processes are physiological, i.e. normal. The pathological reflux of stomach contents into the esophagus is called gastroesophageal reflux, and the mechanism that prevents vomiting is called the antireflux mechanism.
Anti-reflux mechanism in children
In children, the nervous regulation of the antireflux mechanism is very complex and easily disturbed under the influence of external and internal factors. Regurgitation and vomiting easily occur in children with an immature antireflux mechanism, if the mode or volume of feeding is incorrectly selected, as a reaction to artificial mixtures, at the slightest sign of infectious processes. This is especially often observed in children with intrauterine growth retardation and premature babies, as well as in severe pregnancy and toxicosis, caesarean section, complicated childbirth, etc.
When to see a doctor
Despite the fact that moderate spitting up in a child under 6 months is considered a variant of the norm, parents should definitely tell the pediatrician about this during a routine examination. The reason for serious concern and immediate examination of the child is an increase in the frequency or increase in the volume of regurgitation, the appearance of streaks of blood or bile impurities, a lag in recruitment or weight loss, and high temperature. In this case, it is urgent to consult a surgeon to rule out surgical causes.
In this case, it is urgent to consult a surgeon to rule out surgical causes.
Diagnostics
In most cases, an ultrasound examination (ultrasound) is necessary to establish an accurate diagnosis and select the correct treatment. An experienced doctor of ultrasound diagnostics helps to establish the correct diagnosis in more than half of the cases. Sometimes, for a more accurate diagnosis, a flexible gastroscopy, X-ray examination, or computed tomography of the abdominal organs is performed.
When surgery is required
Pyloric stenosis, or impaired patency of the gastric outlet, is the cause of the most severe regurgitation syndrome (vomiting "fountain") in children under 2 months, accompanied by severe weight loss and progressive deterioration of the child's condition. This disease requires urgent surgical care. In leading clinics, such operations are performed using a minimally invasive laparoscopic method. The current level of development of surgery and pediatric anesthesiology allows the use of endoscopic surgery techniques even in children in the first weeks of life.
There are also other causes of regurgitation that require surgical intervention, such as hiatal hernia, chalazia (gaping) of the esophagus, and others. These malformations are characterized by a violation of the formation of the antireflux mechanism and lead to constant regurgitation in a child, impaired weight gain, decreased appetite, chronic cough, bronchial asthma, and anemia. If drug therapy is ineffective, then a gastrofundoplication operation is indicated, in which an artificial antireflux valve is surgically formed. Like many other interventions, in modern children's clinics this operation is performed laparoscopically - with less trauma, minimal blood loss, minimal cosmetic defect and a quick recovery of the child after the operation.
Of course, vomiting and regurgitation can be symptoms of many other diseases and occur at any age of the child. Thus, vomiting is often observed in acute appendicitis and intestinal obstruction, it can be a symptom of an intestinal infection, intoxication, etc.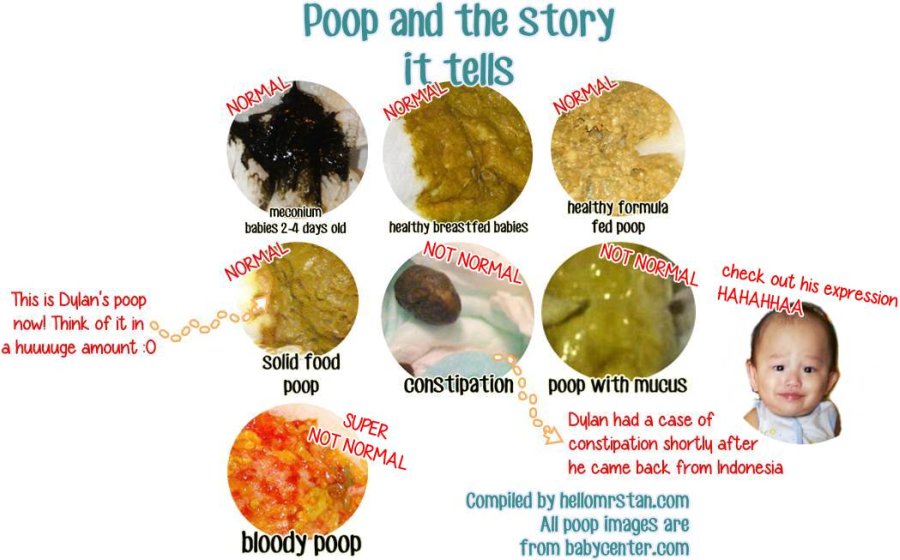 In addition to the disease itself, vomiting and profuse regurgitation are dangerous because the child loses a large amount of water and salts necessary for life, which can lead to dehydration - exsicosis. The younger the child, the faster the disruption of compensatory mechanisms and the worsening of his condition. Therefore, the appearance in a child of symptoms of vomiting or severe regurgitation in young children requires immediate medical attention to identify the causes, establish the correct diagnosis and select the optimal treatment, and, if necessary, surgical.
In addition to the disease itself, vomiting and profuse regurgitation are dangerous because the child loses a large amount of water and salts necessary for life, which can lead to dehydration - exsicosis. The younger the child, the faster the disruption of compensatory mechanisms and the worsening of his condition. Therefore, the appearance in a child of symptoms of vomiting or severe regurgitation in young children requires immediate medical attention to identify the causes, establish the correct diagnosis and select the optimal treatment, and, if necessary, surgical.
Experienced pediatricians and surgeons are on duty around the clock at the EMC Children's Clinic, providing emergency and planned care to children of all ages, starting from the first days of life.
If surgical treatment is required, the method of choice in our clinic is minimally invasive endoscopic surgery, which in most cases allows the child to go home on the day of the operation. The operation is accompanied by an experienced anesthesiologist, who individually selects modern and safe anesthesia for each child. Postoperative wards are equipped with high-tech equipment, where round-the-clock monitoring systems are installed, and a separate nurse continuously monitors the condition of small patients.
The operation is accompanied by an experienced anesthesiologist, who individually selects modern and safe anesthesia for each child. Postoperative wards are equipped with high-tech equipment, where round-the-clock monitoring systems are installed, and a separate nurse continuously monitors the condition of small patients.
In the comfortable hospital of the EMC Children's Clinic, parents can stay with their child all the time, round-the-clock visits are open for relatives and friends, which ensures maximum comfort for the child and parents.
Article | Neurotic vomiting in children
Bobylova M.Yu. (neurologist)
Vomiting in children is not an independent disease, but a manifestation of various diseases. Vomiting can be caused by disorders of the gastrointestinal tract, metabolic diseases, tonsillitis, inflammation of the nasopharynx, pneumonia, influenza, SARS, acute appendicitis. Such vomiting is treated by a pediatrician.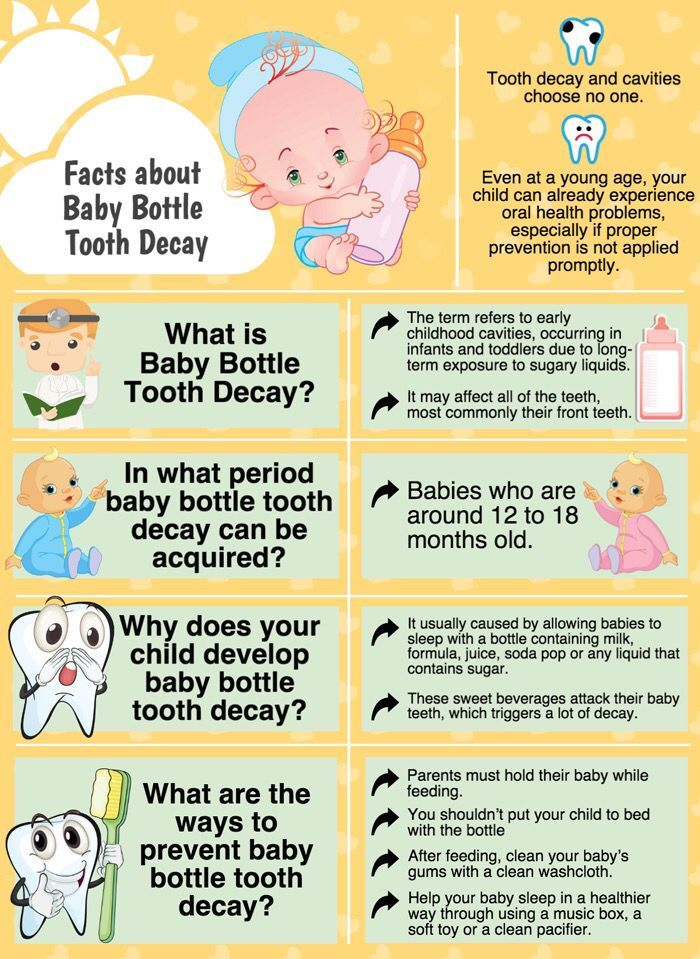 But there are also vomiting associated with dysfunction of the central nervous system. It develops in children of the first months of life who have undergone hypoxia during fetal development or childbirth. After 6 months, habitual vomiting is often associated with improper introduction of complementary foods if the child is force fed. Also, vomiting can be a sign of increased intracranial pressure. Vomiting attacks are characteristic of the childhood form of migraine.
But there are also vomiting associated with dysfunction of the central nervous system. It develops in children of the first months of life who have undergone hypoxia during fetal development or childbirth. After 6 months, habitual vomiting is often associated with improper introduction of complementary foods if the child is force fed. Also, vomiting can be a sign of increased intracranial pressure. Vomiting attacks are characteristic of the childhood form of migraine.
In infants , especially in the first 3 months of life, regurgitation of a small amount of food (15-30 ml) 2-3 times a day is a common occurrence that disappears with the growth of the child. The horizontal position of the baby and the relatively large amount of food predispose to the occurrence of regurgitation in healthy infants. It is also characteristic of regurgitation when swallowing air during breastfeeding, when there is not enough breast milk in the mammary gland, or when the baby does not capture the areola. With artificial feeding - swallowing of air occurs when the nipple is not completely filled with milk, when there is a large hole in the nipple, when the position of the bottle during artificial feeding is horizontal.
With artificial feeding - swallowing of air occurs when the nipple is not completely filled with milk, when there is a large hole in the nipple, when the position of the bottle during artificial feeding is horizontal.
Swallowing air is more common in infants who are hyperexcitable, greedily sucking, and also with general muscular hypotension.
Regurgitation, unlike vomiting, occurs suddenly, does not affect the behavior and general well-being of the child, while children do not lose weight gain.
Helping a baby with spitting up: firstly, immediately after feeding and during sleep, you should hold the baby in an upright position. If regurgitation has occurred, it is necessary to turn the child's head to one side, toilet the child's nose and mouth (clean it from food debris). Wash and caress the baby.
Feeding rules must be observed: the baby should be fed in a semi-upright position, which helps to expel swallowed air. These babies should sleep with their heads up.
If regurgitation is frequent and profuse, and the baby begins to lag behind in weight, then this may be a manifestation of a disease of the stomach or intestines (pylorospasm or pylostenosis). It is necessary to contact a pediatrician for timely examination, diagnosis, treatment and prevention of complications.
Neurological disorders as a cause of vomiting in a child
The vomiting center of a person is located in the brain, therefore, in case of any damage to the head (trauma, infection, vegetative-vascular dystonia, increased intracranial pressure), vomiting occurs not associated with food intake and fever .
Vomiting in children under 1 year of age is associated with hypoxia during fetal development and at birth.
Neurotic vomiting develops as a manifestation of neurotic reactions in response to nasty and undesirable actions: coercion, protest against punishment, feeding. Functional vomiting in such children is more often combined with refusal to eat, with selectivity in food, behavioral changes, and stubbornness. More common is functional vomiting in children who are emotional, easily excitable, vulnerable. There are no signs of intoxication of the body, pain in the stomach, diarrhea or temperature in the child. This behavior requires prompt treatment to a neurologist.
More common is functional vomiting in children who are emotional, easily excitable, vulnerable. There are no signs of intoxication of the body, pain in the stomach, diarrhea or temperature in the child. This behavior requires prompt treatment to a neurologist.
Vomiting in children, even if it is not accompanied by diarrhea and fever, requires the attention of parents. In no case should you self-medicate, since for each disease the methods of treatment are different.
Only a doctor can recognize the causes of the problem after a series of examinations. To clarify the cause of constant vomiting in a child, it is necessary to clarify when it began, what kind of character it is (periodic, after each feeding), whether it is somehow connected with food intake and with the time of day. Important information about possible diseases is also provided by the diagnosis of vomit. The masses are checked for the presence of mucus, bile, milk, blood, digested and undigested food debris. When making a diagnosis, the age of the child is taken into account.