Aap baby food guidelines
Infant Food and Feeding
Based upon evidence, a number of desired behaviors were identified as critical to helping families foster healthy active living for their infant. For each desired behavior you can explore the evidence, learn what parents told us about these behaviors, identify opportunities to promote healthy behaviors at the point of care, review how to start conversations and access messages and resources to support families. Also available to inform your counseling is the Onset and Patterns of Risk Behaviors during Infancy Timeline located above this section.
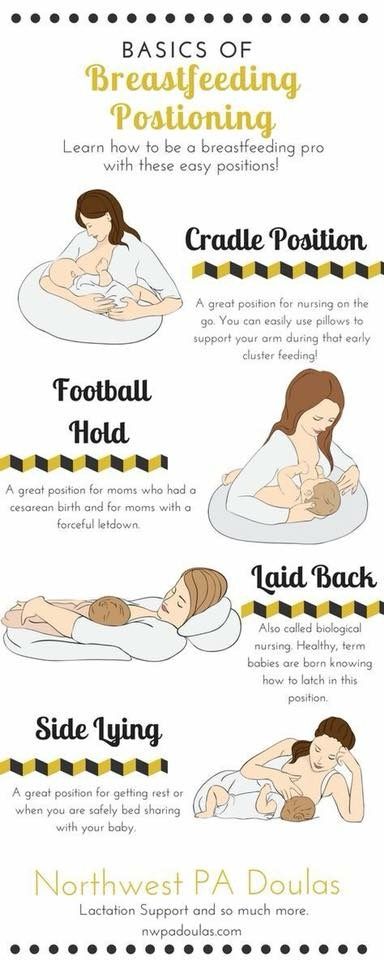
Breastfeeding
- Exclusive breastfeeding for approximately 6 months.
- Continue breastfeeding until the baby's first birthday or longer while mutually desired by mother and baby.
-
- Breastfed babies who are breastfed for at least 6 months are less likely to be overweight.
- The duration of breastfeeding also is inversely related to the risk of obesity.
- A reduction of 40% in the incidence of type 2 diabetes mellitus is reported, reflecting the long-term positive effect of breastfeeding on weight control and feeding self-regulation.
- 80% of mothers expect to breastfeed yet only 14% are exclusively breastfeeding at 6 months.
- Critical periods for breastfeeding cessation are transition home from hospital, 6-8 weeks, transition back to work, and between 6-8 months due to self-weaning and/or introduction of solids.
- Breastfed babies who are breastfed for at least 6 months are less likely to be overweight.
-
- Breastfeeding was harder than they expected. Many tried but did not maintain.
- Surprised to learn that breastfeeding can impact obesity and many felt this info could impact decisions around duration.
-
- Support new mothers in breastfeeding. Provide lactation services at your office or know about sources of lactation support in your community.
- Provide ongoing encouragement for breastfeeding at well visits. Ask patients about challenges or concerns.
- Let mothers know It is wonderful that they are breastfeeding their baby. And that breastfeeding is great for their baby and has health benefits for them too.
- If mothers are returning to work assure them that with careful planning and a few resources they can make breastfeeding work.
- Remind families that babies reap the benefits of breastfeeding for their entire first year!
- Support new mothers in breastfeeding. Provide lactation services at your office or know about sources of lactation support in your community.
-
Newborn, early months:
- It is so great that you are breastfeeding your baby. It can be very rewarding but challenging too. How is breastfeeding going for you? Do you have any concerns about breastfeeding your baby?
- Can you tell me about a typical feeding experience? Tell me how your family and friends (spouse, grandparents, etc) are supporting you with feeding your baby?
For 2 or 4 month visit:
- It is wonderful that you are continuing to breastfeed your baby.
 Are you exclusively breastfeeding?
Are you exclusively breastfeeding? - Are you returning to work? Many women continue to successfully breast feed after returning to work. Tell me about your feelings about this. Are there any questions I can answer to help you during this time of transition?
- Are you having any challenges maintaining exclusive breastfeeding?
For 6 and 9 month visit:
- It is wonderful that you are still breastfeeding. Is there anything can I do to support you in your breastfeeding?
-
HALF Message(s):
Lots of parents are surprised to find out that babies who are breastfed for at least 6 months are less likely to be overweight or obese as they get older. Breastfeeding can be a lot of work, but it’s a great way to bond with your baby and help him stay healthy.HALF Resources:
For realistic parent derived strategies for breastfeeding refer parents to the following sections on healthychildren. org/growinghealthy:
org/growinghealthy:Quick Tips: Keep Your Child Healthy widget.
Simply select Breastfeeding to generate the results.Food and Feeding Infants.
Also take advantage of the HealthyGrowth app to create personalized patient education for your patient.
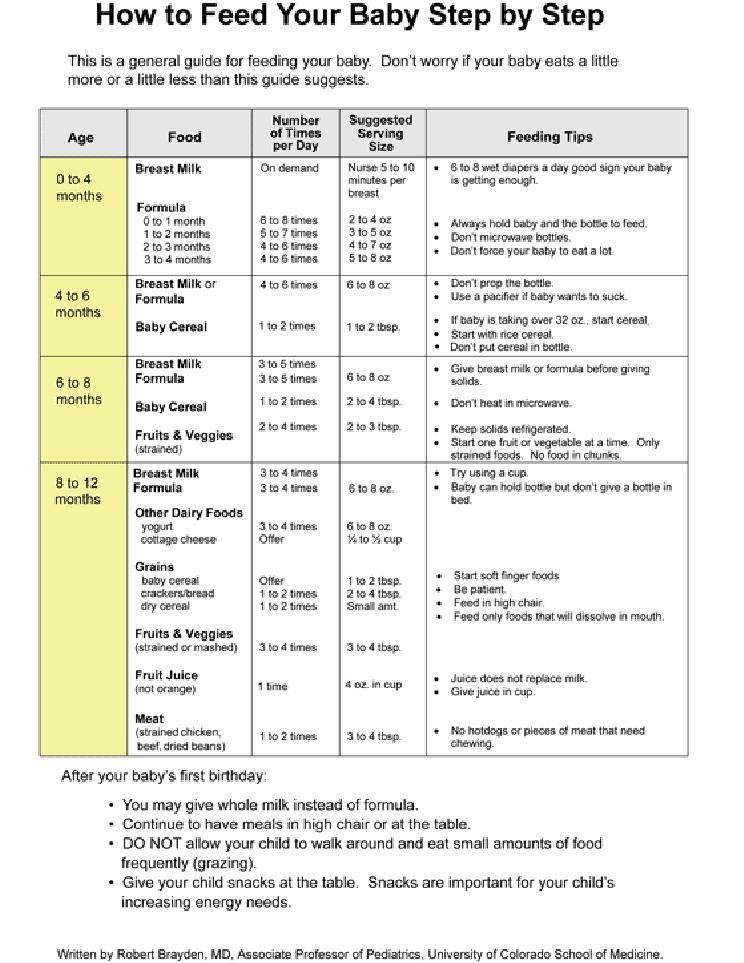
Bottle Feeding
Practice appropriate bottle feeding practices:
- Avoid bottle propping
- Only breastmilk or formula in bottle unless otherwise directed by physician
-
- Inadequate feeding practices associated with bottle feeding of infant formula or use of bottle feeding as a methods to soothe infants can contribute to greater energy intake.
- It is not uncommon for mothers add cereal to the bottle in the belief that doing so will help the infant sleep longer.
- A substantial number of families introduce solids early especially if they perceive the infant as fussy.
- Inattention to a child’s hunger and satiety cues has been associated with infant overfeeding.
-
- Other family members and friends were influencers and provided “evidence” that cereal in the bottle helped baby sleep.
- Parental exhaustion/desire for sleep is a big motivator to add cereal to the bottle.
-
- If parent reports fussiness, counsel parent about importance of responding with an array of strategies, not just feeding.
- If parent reports sleeping problems, counsel about bedtime routines, healthy sleep practices, and realistic sleep expectations based upon baby's age.
- Let parents know that it is important that it will get better.
- Encourage parents to make feeding time responsive and pleasant for them and their baby.
-
- It can be difficult when a parent and baby are not getting enough sleep.
 Can you tell me how this is going for you?
Can you tell me how this is going for you? - It can be difficult when a baby cries a lot. How is it going with your baby? Would you like to talk about some ways to soothe your baby that don’t involve feeding?
- Can you tell me about what feeding time is like for you and your baby?
- Tell me how your family and friends (spouse, grandparents, etc) are supporting you with feeding your baby.
- How would you describe your baby? Is she content, fussy, sleepy, etc?
- It can be difficult when a parent and baby are not getting enough sleep.
-
HALF Message(s):
Some parents (and grandparents!) worry that young babies aren’t getting enough to eat. But there’s no need to worry — babies under age 6 months get everything they need from breast milk or formula.HALF Resources:
For realistic parent derived strategies for bottle feeding refer parents to the following sections on healthychildren.org/growinghealthyAlso take advantage of the HealthyGrowth app to create personalized patient education for your patient.

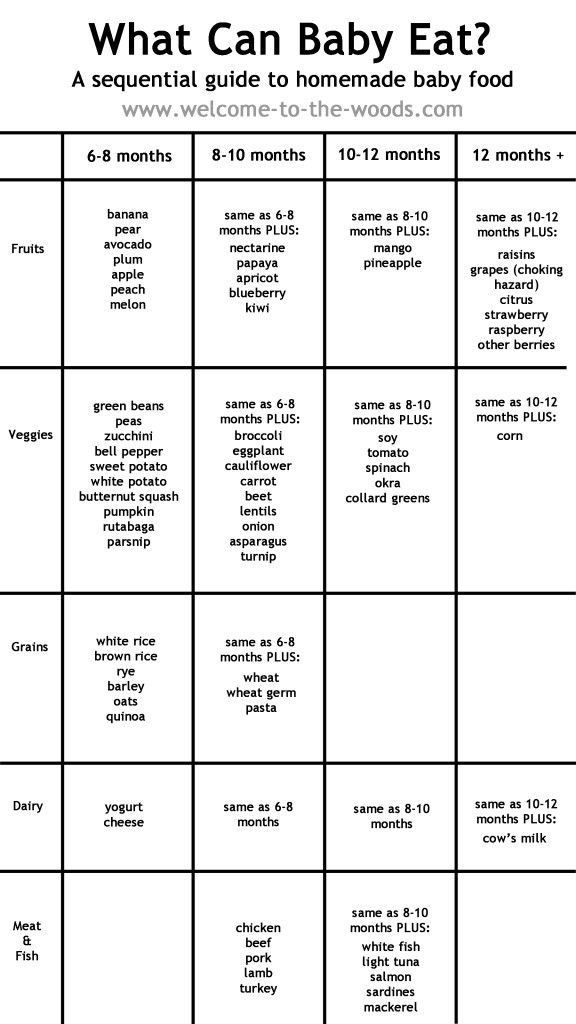
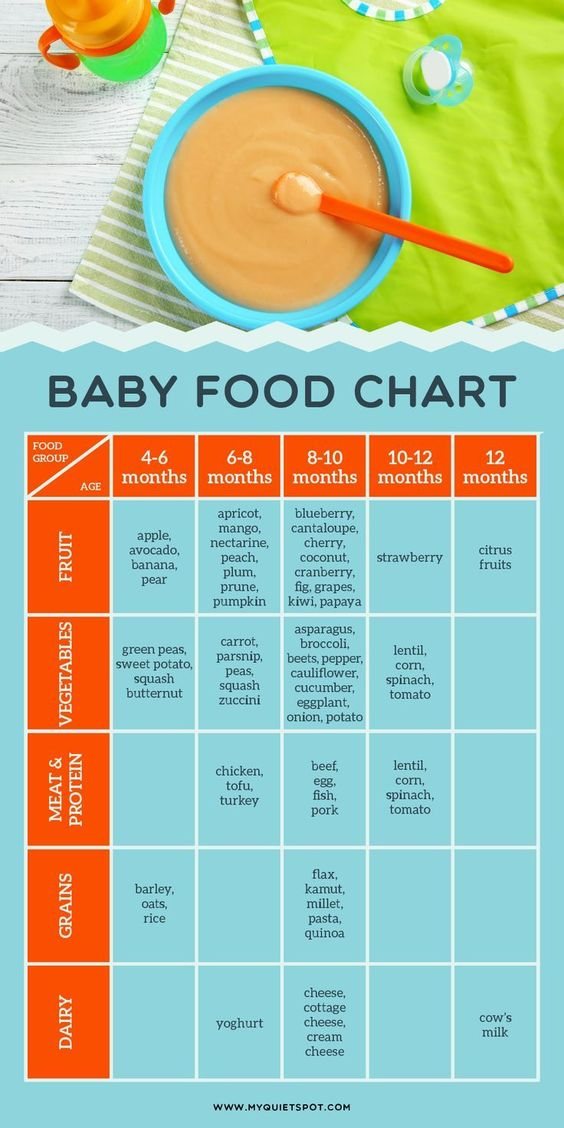
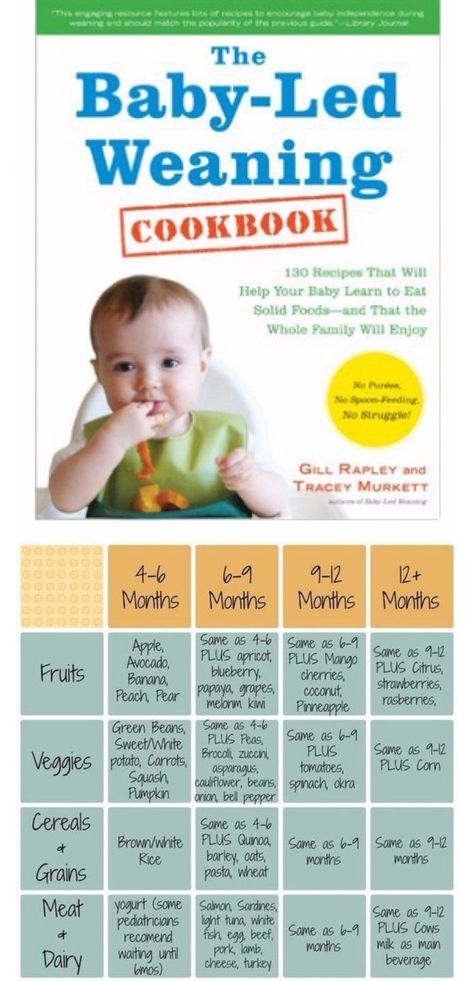
Food Introduction
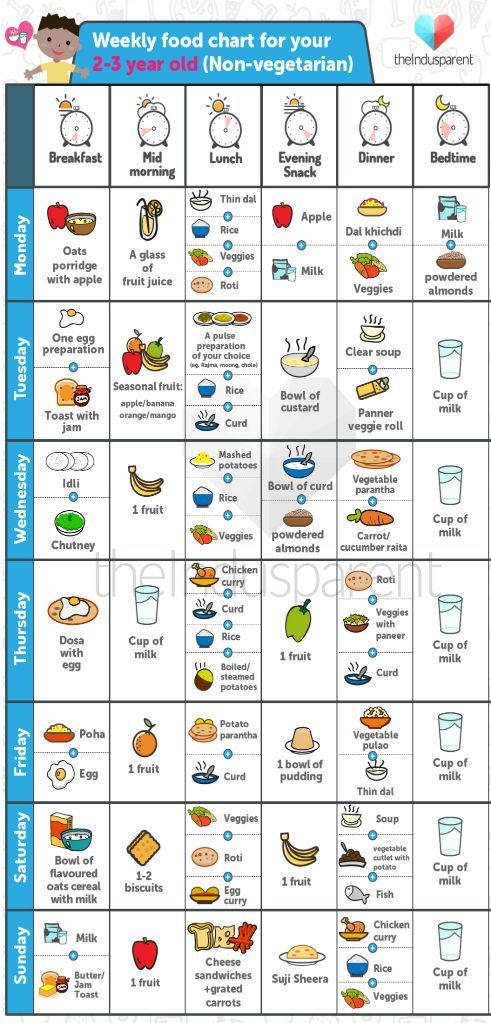
- Introduce solid foods around 6 months of age
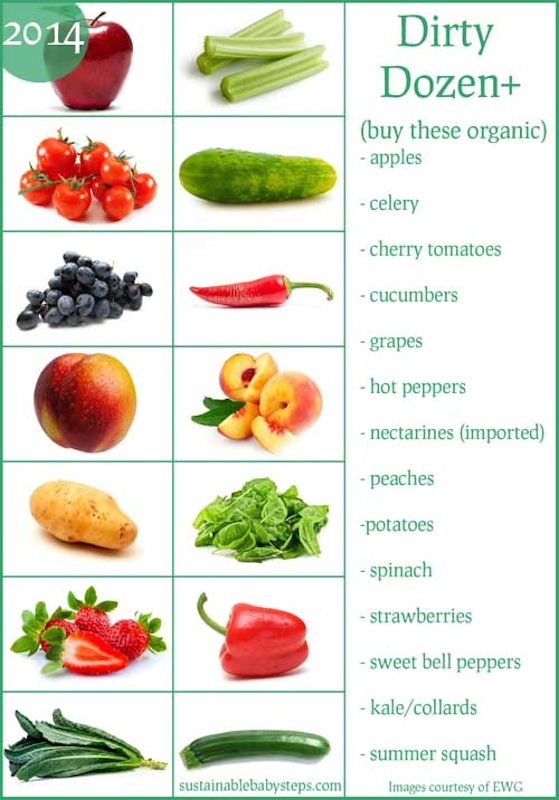
- Expose baby to a wide variety of healthy foods
- Also offer a variety of textures
-
- A substantial number of families introduce complementary solid foods around 3-4 months, especially if the infant is perceived as fussy.
- Formula fed infants are at more risk for early introduction of solids.
- Introduction to solids prior to 4 months is associated with increased weight gain and adiposity, both in infancy and early childhood.
- Research indicates that it is important to expose children to a wide variety of flavors and textures.
- Many babies and toddlers need to be exposed to foods multiple times before accepting them.
- Babies and toddlers are more likely to eat foods they see their peers and parents eating.
-
- Other family members and friends were influencers and provided false evidence that introducing solids helped calm fussy babies.
- Parental frustration and desire for happy babies were big motivators to introduce solids.
- Parents cited the concern about wasting food.
- Many parents assumed once their child rejected a food that it meant their child did not like that food.
- Concept of offering a food 10-15 times before acceptance was confusing.
-
- If parent reports fussiness and/or sleeping problems, counsel about the importance of appropriate complimentary food introduction. Share potential calming and soothing strategies for infants, as well as coping strategies for parents.
- Encourage parents to wait until around 6 months to introduce solids.
- Remind parents that this is a very important time and the kinds of foods your baby eats now help him to enjoy healthy foods later.
- Counsel about the importance of introducing a wide variety of foods, especially vegetables and fruits. As the infant grows, it is important to expose the baby to variety of textures.
- Explain that sometimes it takes a baby 10-15 tries over time before they will actually accept a new food.
- Explain that this 10-15 tries is over a period of months and to not get discouraged.
- To address concerns about waste, discuss strategies that limit wasted food, such as not feeding directly from a jar but removing a small serving from a jar to a different container.
- You can reassure parents that it is okay if the infant doesn’t like something the first time, and it is important to keep offering it.
-
- Tell me how your family and friends (spouse, grandparents, etc) are supporting you with feeding your baby.
- How would you describe your baby? Is she content, fussy, sleepy, etc?
Well Visit 2 and 4:
- Can you tell me a little about your plans to introduce your baby to solid foods?
6 month visit:
- It is wonderful that your baby is ready to embark or beginning to eat solid food.
 It is an exciting milestone! Do you have any concerns or questions
It is an exciting milestone! Do you have any concerns or questions - Tell me a little bit about your experiences so far.
- Can you tell me about your feeding experiences so far? Are you having fun? Do you have any concerns?
- Can you describe what foods your baby likes and dislikes?
- What do you do when your baby seems to dislike or not try a new food?
- How do you introduce new foods to your baby?
-
HALF Message(s):
Lots of parents are excited to start their babies on solid foods. Others are nervous. Starting to eat solid foods (like baby cereal and baby food) is an important part of your baby’s development. Did you know that babies who start eating solid food too early are more likely to be overweight or obese in childhood and adulthood? This is one more important reason to wait until your baby is really ready before giving him solid foods.HALF Resources:
- For realistic parent derived strategies for solid food introduction refer parents to the following sections on healthychildren.
 org/growinghealthy
org/growinghealthy - Quick Tips: Keep Your Child Healthy widget. Simply select Starting Solid Foods to generate the results.
- Food and Feeding Infants.
Also take advantage of the HealthyGrowth app to create personalized patient education for your patient.
HALF Message(s):
Introducing your baby to new foods can be both fun and frustrating. Some parents worry about wasting food and money if their babies don’t like a lot of foods at first. Good news: a new eater only needs 1-2 tablespoons of each food and will gradually increase to 3-4 tablespoons as she gets older. By getting your baby used to lots of different foods, you’ll help him build a healthy diet for life. - For realistic parent derived strategies for solid food introduction refer parents to the following sections on healthychildren.
Healthy Snacking
- After 9 months, offer 2-3 healthy and nutritious snacks per day
- Maintain fruit and vegetable consumption after finger foods are introduced
-
- Almost all older infants snack regularly, but the quality of the snacks is variable.

- The most common snack foods are often finger foods such as cereal, cookies, crackers, and French fries.
- Eating at regular intervals helps to foster self-regulation and reduces overeating.
- At 9 months, there is a considerable drop in fruit and veggie consumption, and an increase in non-nutritive finger and snack foods.
- Almost all older infants snack regularly, but the quality of the snacks is variable.
-
- Many parents (especially grandparents) seem to associate snack time with “treat” time.
- Parents generally were positive about introduction of finger foods but many opted for prepackaged foods that were portable and not choking hazards.
-
- Counsel on appropriate feeding recommendations and the importance of regular healthy and nutritious meals and snacks.
- When discussing routines, mention the importance of planning for regular and healthy snacks.
- Explain that snacks are an opportunity to provide critical nutrients babies need.
- Counsel that snack and meal times should be supervised and ideally occur seated at a table, not in transit (i.e. stroller or car seat).
- By 9 months, counsel on the importance of maintaining fruits and veggies as part of the baby's diet.
- Discuss strategies to use healthy finger foods as snack foods, rather than just prepackaged snack items.
- Snacks are an important part of the baby's nutrition. Suggest that parents offer a fruit and/or veggie for at least one snack every day.
- Discuss potential choking hazards and strategies to offer healthy foods in bite size portions.
-
- What kinds of foods do you offer your child for snacks?
- What kinds of foods does your child want for snacks?
- What part do snacks play in your eating plan for your child?
- How do you feel about snacks as treats or rewards?
- How often does he have snacks? What other kinds of foods do you offer?
- How does your child respond to being offered fruits? Vegetables?
- What do you do if your child refuses to eat fruits and/or vegetables?
- What kind of snacks does your child get in child care? What about when they are staying with grandparents or with other family members?
-
HALF Message(s):
Have fun with finger foods. Let your baby try feeding herself. Offer healthy snacks 2-3 times per day.
Let your baby try feeding herself. Offer healthy snacks 2-3 times per day. HALF Resources:
- For realistic parent derived strategies on healthy snacking and finger foods refer parents to the following sections on healthychildren.org/growinghealthy
- Quick Tips: Keep Your Child Healthy widget. Simply select Healthy Snack and Routines and Schedules to generate the results.
- Food and Feeding Infants.
Also take advantage of the HealthyGrowth app to create personalized patient education for your patient.
Foster Self-feeding
- Babies are encouraged to use spoons and fingers to feed themselves
- Babies are encouraged to drink from a cup starting at 6 months of age
- Parents recognize hunger and satiety cues
-
- Babies have an innate ability to self-regulate their food.

- Responsive feeding helps foster self-regulation.
- Babies have an innate ability to self-regulate their food.
-
- Parents identified time and cleanliness as the two big barriers to self-feeding.
- Wasting food is another concern.
-
- Discuss responsive feeding, hunger and satiety cues with parents.
- Encourage parents to foster babies self-feeding by using fingers, spoons, and cups. Explain that using their hands and trying to use a spoon are important parts of how a baby learns to self-feed and regulate how much they eat.
- Acknowledge that self-feeding can sometimes be messy and take a bit longer. Strategize with parents about setting certain meals and snacks aside for their child to hone these skills, and remind parents when they opt to feed their child to be aware of fullness cues.
-
- How is your baby doing with a spoon?
- Can you describe how you go about encouraging your baby to feed herself?
- What is it like at mealtimes when your baby feeds herself? How do you feel about it, and how does your baby feel about it?
- What would be helpful to you and your baby to encourage self feeding?
-
HALF Message(s):
Let your baby try feeding herself as soon as she’s ready — usually around 8 or 9 months old.
HALF Resources:
- For realistic parent derived strategies on self-feeding refer parents to the following sections on healthychildren.org/growinghealthy
- Food and Feeding Infants
Healthy Drinks
- Babies should drink breastmilk or formula for the first year of life
- Try to avoid introducing juice until child is a toddler. If juice is introduced, wait until 6-9 months and limit consumption to 4-6 ounces
- Avoid introduction of sugar-sweetened beverage
-
- Almost 80% of babies 6-9 months drink juice regularly.
- Children who consume such fruit juices have higher energy intakes.
-
- In general, parents thought 100% juice was a healthy choice.
- Parents thought that the oral health angle was impactful when discussing risks of sugared beverages.
- Some parents mentioned elimination issues as a reason to or not use juice drink.
- Other family members and eating out were two factors parents identified as contributing to the introduction of juice or other sugar sweetened beverages
.
- In general, parents thought 100% juice was a healthy choice.
-
- Remind parents that breastmilk, formula and water are the best beverage choices at this time. Suggest that water is a great choice for practicing drinking from a cup and encourage families to foster use of cups over bottles and sippy cups.
- If they want to introduce juice, help parents understand what a 4-6 ounce serving looks like, and that this is the amount for one day.
-
- Does your child drink juice? How much do you offer?
- How do you feel about your child drinking sugar sweetened beverages like soda, sports drinks, and juice?
- What beverages does your family drink at meals and between meals? What about when eating out?
- When you eat out, what beverages does your child drink?
- What beverages does your child drink at child care? With other friends and family members?
-
HALF Message(s):
Breast milk and formula are the best choices for your baby. When it’s time for him to start using a cup (around 6 to 9 months), give him breast milk, formula, or water.
When it’s time for him to start using a cup (around 6 to 9 months), give him breast milk, formula, or water. HALF Resources:
- For realistic parent derived strategies on healthy drinking refer parents to the following sections on healthychildren.org/growinghealthy
- Quick Tips: Keep Your Child Healthy widget. Simply select Bottle Feeding and Healthy Snacks to generate the results.
- Food and Feeding Infants
Also take advantage of the HealthyGrowth app to create personalized patient education for your patient.
Last Updated
07/06/2021
Source
American Academy of Pediatrics
When, What, and How to Introduce Solid Foods | Nutrition
For more information about how to know if your baby is ready to starting eating foods, what first foods to offer, and what to expect, watch these videos from 1,000 Days.
The Dietary Guidelines for Americans and the American Academy of Pediatrics recommend children be introduced to foods other than breast milk or infant formula when they are about 6 months old.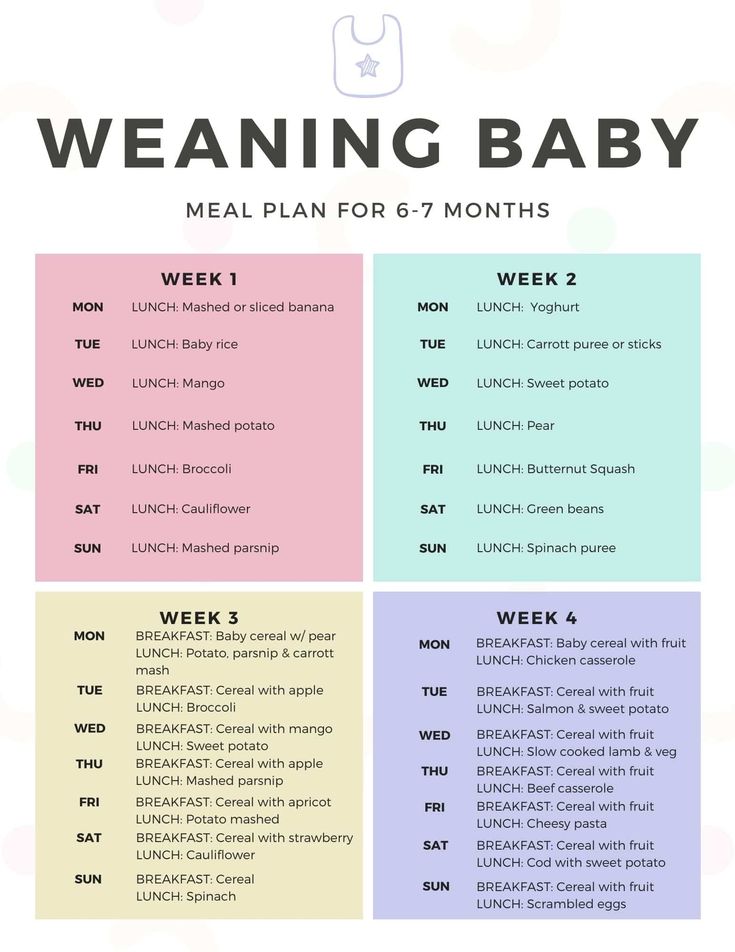 Introducing foods before 4 months old is not recommended. Every child is different. How do you know if your child is ready for foods other than breast milk or infant formula? You can look for these signs that your child is developmentally ready.
Introducing foods before 4 months old is not recommended. Every child is different. How do you know if your child is ready for foods other than breast milk or infant formula? You can look for these signs that your child is developmentally ready.
Your child:
- Sits up alone or with support.
- Is able to control head and neck.
- Opens the mouth when food is offered.
- Swallows food rather than pushes it back out onto the chin.
- Brings objects to the mouth.
- Tries to grasp small objects, such as toys or food.
- Transfers food from the front to the back of the tongue to swallow.
What Foods Should I Introduce to My Child First?
The American Academy of Pediatrics says that for most children, you do not need to give foods in a certain order. Your child can begin eating solid foods at about 6 months old. By the time he or she is 7 or 8 months old, your child can eat a variety of foods from different food groups. These foods include infant cereals, meat or other proteins, fruits, vegetables, grains, yogurts and cheeses, and more.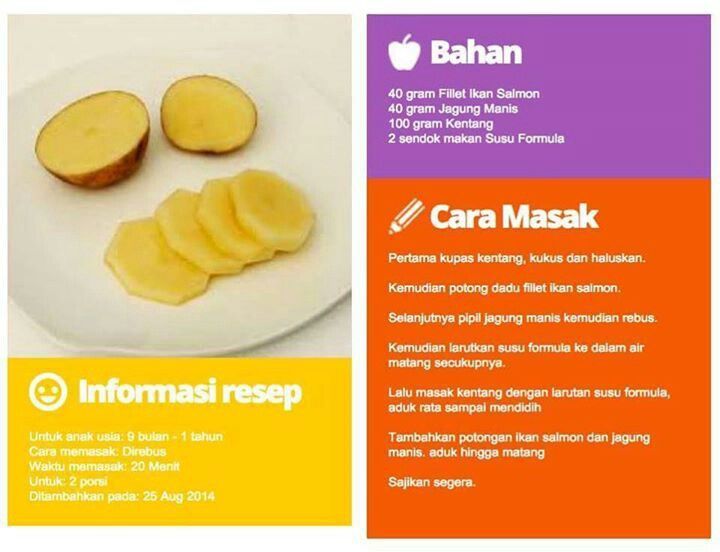
If your child is eating infant cereals, it is important to offer a variety of fortifiedalert icon infant cereals such as oat, barley, and multi-grain instead of only rice cereal. Only providing infant rice cereal is not recommended by the Food and Drug Administration because there is a risk for children to be exposed to arsenic. Visit the U.S. Food & Drug Administrationexternal icon to learn more.
How Should I Introduce My Child to Foods?
Your child needs certain vitamins and minerals to grow healthy and strong.
Now that your child is starting to eat food, be sure to choose foods that give your child all the vitamins and minerals they need.
Click here to learn more about some of these vitamins & minerals.
Let your child try one single-ingredient food at a time at first. This helps you see if your child has any problems with that food, such as food allergies. Wait 3 to 5 days between each new food. Before you know it, your child will be on his or her way to eating and enjoying lots of new foods.
Introduce potentially allergenic foods when other foods are introduced.
Potentially allergenic foods include cow’s milk products, eggs, fish, shellfish, tree nuts, peanuts, wheat, soy, and sesame. Drinking cow’s milk or fortified soy beverages is not recommended until your child is older than 12 months, but other cow’s milk products, such as yogurt, can be introduced before 12 months. If your child has severe eczema and/or egg allergy, talk with your child’s doctor or nurse about when and how to safely introduce foods with peanuts.
How Should I Prepare Food for My Child to Eat?
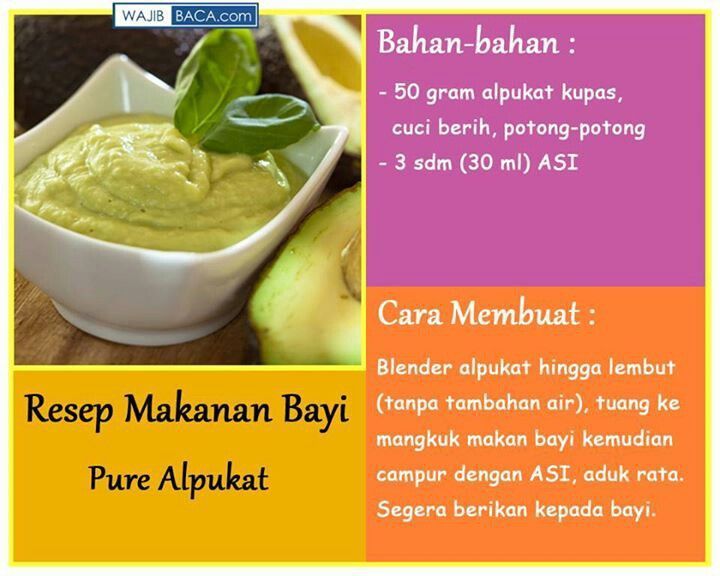
At first, it’s easier for your child to eat foods that are mashed, pureed, or strained and very smooth in texture. It can take time for your child to adjust to new food textures. Your child might cough, gag, or spit up. As your baby’s oral skills develop, thicker and lumpier foods can be introduced.
Some foods are potential choking hazards, so it is important to feed your child foods that are the right texture for his or her development. To help prevent choking, prepare foods that can be easily dissolved with saliva and do not require chewing. Feed small portions and encourage your baby to eat slowly. Always watch your child while he or she is eating.
To help prevent choking, prepare foods that can be easily dissolved with saliva and do not require chewing. Feed small portions and encourage your baby to eat slowly. Always watch your child while he or she is eating.
Here are some tips for preparing foods:
- Mix cereals and mashed cooked grains with breast milk, formula, or water to make it smooth and easy for your baby to swallow.
- Mash or puree vegetables, fruits and other foods until they are smooth.
- Hard fruits and vegetables, like apples and carrots, usually need to be cooked so they can be easily mashed or pureed.
- Cook food until it is soft enough to easily mash with a fork.
- Remove all fat, skin, and bones from poultry, meat, and fish, before cooking.
- Remove seeds and hard pits from fruit, and then cut the fruit into small pieces.
- Cut soft food into small pieces or thin slices.
- Cut cylindrical foods like hot dogs, sausage and string cheese into short thin strips instead of round pieces that could get stuck in the airway.
- Cut small spherical foods like grapes, cherries, berries and tomatoes into small pieces.
- Cook and finely grind or mash whole-grain kernels of wheat, barley, rice, and other grains.
Learn more about potential choking hazards and how to prevent your child from choking.
Top of Page
Drinks in children's nutrition | Safronova A.I., Pyrieva E.A., Georgieva O.V.
Introduction
Early childhood is a critical period for the formation of eating behavior, which can have a significant impact on the prevention of nutrition-associated chronic diseases. Drinks are an integral part of the diet of children of any age category. In childhood, special attention is paid to drinks, which is due to the risk of receiving an excess amount of simple carbohydrates with them and, as a result, increased addiction to sweet foods.
According to [1], the drinking regimen of modern children is not considered optimal. Most children consume insufficient amounts of drinking water, which is often replaced by sweet drinks, both home-made and industrial production (compotes, fruit drinks, nectars, etc.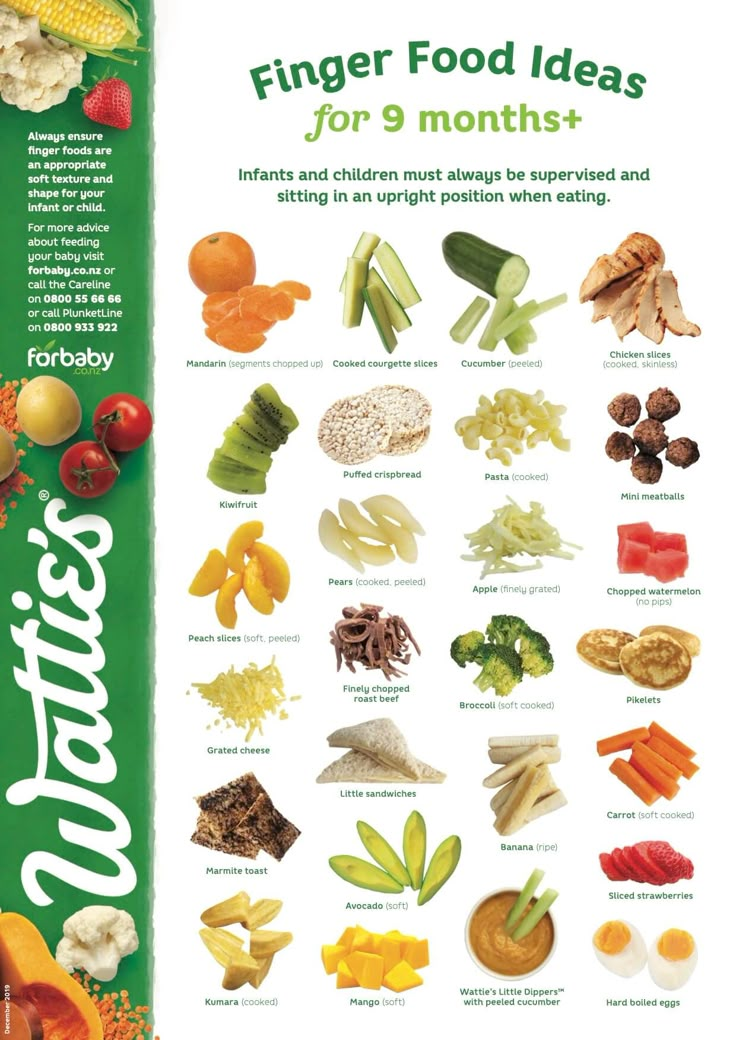 ), which leads to an excess intake of sugar into the body and an increase in the calorie content of the diet as a whole. Epidemiological studies [2, 3] have shown that the consumption of sugary drinks affects the development of overweight and may be associated with a wide spread of metabolic and cardiovascular diseases.
), which leads to an excess intake of sugar into the body and an increase in the calorie content of the diet as a whole. Epidemiological studies [2, 3] have shown that the consumption of sugary drinks affects the development of overweight and may be associated with a wide spread of metabolic and cardiovascular diseases.
Sugar-containing drinks in children's diet
Observations [4, 5] show that the consumption of added sugar in the daily diet of children aged 2–9 years is 14% of the daily requirement, with most of the sugars coming from sugar-containing drinks. According to WHO recommendations [6], the safe level of intake of added sugars in the diet of children over 2 years of age and adults should not exceed 10% of the daily calorie intake. Currently, the prospects for its further reduction to 5% of the daily calorie intake are being evaluated. The safe amount of added sugars in the diet of children under 2 years of age has not yet been regulated and is actively discussed. According to researchers [7], the amount of such sugars should have established limits, namely, no more than 10% of the daily caloric intake of the diet of this age group.
According to researchers [7], the amount of such sugars should have established limits, namely, no more than 10% of the daily caloric intake of the diet of this age group.
Due to the worsening pandemic of childhood obesity, the American Academy of Pediatrics does not recommend the use of sugar-sweetened beverages for children under 5 years of age [8]. Despite this, practice shows that 25% of children aged 1 to 2 years and 45% of children aged 2–4 years in the United States regularly consume sugar-containing drinks [9]. A high level of consumption of these drinks was also noted among adolescents, and it differs depending on the level of economic development of the country. In countries with a level
Above average 57% of adolescents use carbonated soft drinks at least once a day, in lower middle income countries this figure is 39% and in low income countries 44% [10]. The great popularity of sugar-containing drinks is largely due to aggressive advertising, affordability (relative to 100% natural juice), as well as incorrect marketing policies using illustrations similar to natural juices on packaging (including images of fruits), information about nutritional value (for example, "no artificial flavors"). e7ators", "all natural"), which misleads consumers.
e7ators", "all natural"), which misleads consumers.
Among the sugar-containing drinks used in baby food, there are carbonated drinks, sweetened "fruit" teas, juice drinks. The sugar content in sweet carbonated drinks is much higher than in traditional ones [11]. With one serving of a sweet carbonated drink (200 ml), a child gets more than half of the recommended daily amount of sugar. The comparative content of carbohydrates in various drinks is presented in Table 1.
Natural juices in baby food
Juices are among the products recommended for use in baby food starting from the introduction of complementary foods and contain only natural carbohydrates.
In accordance with TR TS 023/2011 "Technical Regulations for Juice Products from Fruits and Vegetables", juice is understood as "a product obtained by physical impact from good-quality, ripe, fresh fruits and (or) vegetables and in which the characteristic features of juice from fruits and (or) vegetables of the same name, nutritional value, physicochemical and organoleptic properties" [12]. Thus, in the characteristics of juices, the terms "juice with sugar" or "juice without sugar" are unacceptable. When sugar is added to fruit juice, the product is referred to as nectar or drink. At the same time, the proportion of the fruity part in nectars is 25–50%, and in juice drinks it is 10–25% [12].
Thus, in the characteristics of juices, the terms "juice with sugar" or "juice without sugar" are unacceptable. When sugar is added to fruit juice, the product is referred to as nectar or drink. At the same time, the proportion of the fruity part in nectars is 25–50%, and in juice drinks it is 10–25% [12].
For many years, juices have been included in the diet of infants primarily as a complementary food product. This is due, first of all, to the easy perception of juices by children due to the liquid consistency familiar to infants, similar to mother's milk, as well as the sweet taste, which children are addicted to from birth. In addition, juices allow you to expand the range of nutrients entering the body, primarily due to various natural sugars, minerals, in particular potassium, iron, dietary fiber, as well as organic acids and polyphenols.
The effect of drinking 100% fruit juices and drinks with added sugars varies significantly. A recent meta-analysis [13] showed that increasing the consumption of sugary drinks to more than 250 ml per day leads to a 13% increase in the risk of developing diabetes, while the same amount of fruit juice only increases the risk by 7%. This may be due to the presence of polyphenols in juices, which have a protective effect on the development of type 2 diabetes, despite the high content of natural sugars.
This may be due to the presence of polyphenols in juices, which have a protective effect on the development of type 2 diabetes, despite the high content of natural sugars.
Polyphenols contained in juices are associated with their antioxidant activity, which, according to numerous studies [12, 14], can lead to anti-inflammatory, antitumor and hypotensive effects, as well as a beneficial effect on the cardiovascular, genitourinary, endocrine systems, gastrointestinal intestinal tract and other organs. It has been shown [15] that citrus fruit flavonoids have a neuroprotective effect, which has been evaluated in some degenerative diseases of the nervous system, in particular in Alzheimer's disease. In addition, fruit juices have a lower glycemic index (e.g. apple juice - 36, orange - 50) compared to sugary carbonated drinks, which have a glycemic index close to 70.
The carbohydrate composition of fruit juices varies significantly in terms of the content of natural sugars. Carbohydrates are found in juices in the form of mono- and disaccharides, as well as some polysaccharides (pectin, starch, dextrins), which are present in juices with pulp and unclarified juices. So, in apples and pears and, accordingly, in juices from them, fructose predominates. Stone fruits tend to have a slightly higher glucose content than fructose. Cherry and juice products from it contain mainly glucose and fructose, and in approximately equal amounts, which may vary slightly. Peaches, apricots and plums contain more sucrose. In most berries and citrus fruits, the ratio of glucose to fructose is approximately 1:1, with a possible predominance of fructose. And banana, pineapple, mango, tangerines contain more sucrose (Table 2) [16].
Carbohydrates are found in juices in the form of mono- and disaccharides, as well as some polysaccharides (pectin, starch, dextrins), which are present in juices with pulp and unclarified juices. So, in apples and pears and, accordingly, in juices from them, fructose predominates. Stone fruits tend to have a slightly higher glucose content than fructose. Cherry and juice products from it contain mainly glucose and fructose, and in approximately equal amounts, which may vary slightly. Peaches, apricots and plums contain more sucrose. In most berries and citrus fruits, the ratio of glucose to fructose is approximately 1:1, with a possible predominance of fructose. And banana, pineapple, mango, tangerines contain more sucrose (Table 2) [16].
Another important component of juices are organic acids (malic, citric, etc.) (Table 3).
In pome fruits, as well as cherries and plums, malic acid dominates, the content of which is 50–90% of the total acid content. Apricots and peaches contain malic and citric acids in approximately equal amounts. The main acid in berries, as well as in citrus, tropical and subtropical fruits, is citric acid, followed by malic acid. Tartaric acid, along with malic acid, is the main one only in grapes.
Apricots and peaches contain malic and citric acids in approximately equal amounts. The main acid in berries, as well as in citrus, tropical and subtropical fruits, is citric acid, followed by malic acid. Tartaric acid, along with malic acid, is the main one only in grapes.
The high content of organic acids in juices predetermines their high acidity, which can cause irritation of the immature intestinal and stomach mucosa and provoke dyspeptic disorders (diarrhea, regurgitation, etc.). In this regard, the titratable acidity of juices intended for baby food is strictly regulated and should not exceed 0.8% (in terms of malic acid). The exception is citrus juices, for which the titratable acidity is limited to 1.2% (in terms of citric acid).
Juice products 8 have a rather high content of potassium, the level of which varies depending on the type of juice (see Table 3) [11, 13].
Sterilized clarified fruit juice drinks in baby food
The range of juices for baby food and juice products with their inclusion is constantly expanding. Recently, a new class of juice products has appeared on the baby food market for young children - sterilized clarified fruit juice-containing drinks. For their production, as a rule, a wide range of concentrated fruit and berry juices and specially prepared drinking water are used. A distinctive feature of the new type of product is the content of fruit juice (not less than 50% and, as a rule, not more than 70%), as well as the production without the addition of sugars, organic acids, stabilizers, dyes, flavors.
Recently, a new class of juice products has appeared on the baby food market for young children - sterilized clarified fruit juice-containing drinks. For their production, as a rule, a wide range of concentrated fruit and berry juices and specially prepared drinking water are used. A distinctive feature of the new type of product is the content of fruit juice (not less than 50% and, as a rule, not more than 70%), as well as the production without the addition of sugars, organic acids, stabilizers, dyes, flavors.
The line of sterilized fruit clarified juice-containing drinks developed by PROGRESS JSC for feeding children over 12 months old, produced under the FrutoNyanya trademark, includes a diverse assortment. Reconstituted fruit juice drinks are made on the basis of concentrated fruit (apple, pear, cherry, etc.) with the addition of berry (raspberry, rosehip, blackcurrant, etc.) juices. The entire line is enriched with inulin, minerals (iron and calcium), vitamins (E, A, D 3 ), which increases the nutritional value of juices.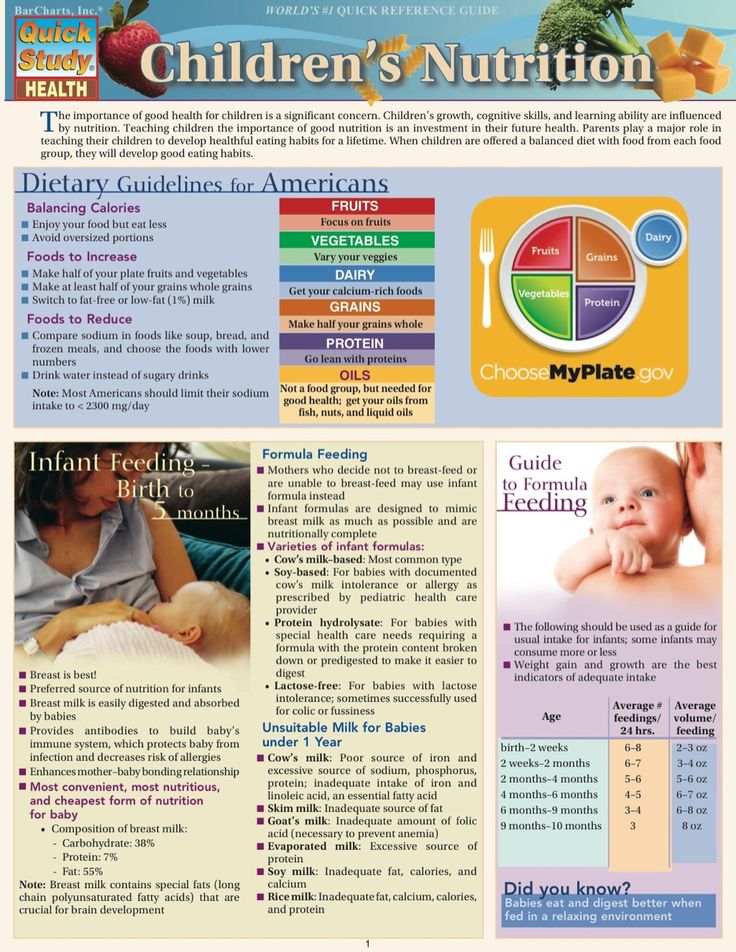 A study [17] of the nutritional value of direct-pressed fruit juice with pulp, in particular the FrutoNyanya trademark, conducted at the Federal State Budgetary Scientific Institution of the Federal Research Center for Nutrition and Biotechnology, showed that a portion of direct-pressed juice (100 ml) is able to meet the needs of a young child in potassium by 17 .2-42.5% of the recommended consumption rate (RIA), in copper - by 6.8-10.4% of the RDA, in chromium - by 9-18% of the RDA, in dietary fibers - by 15-17, 5% of RNP.
A study [17] of the nutritional value of direct-pressed fruit juice with pulp, in particular the FrutoNyanya trademark, conducted at the Federal State Budgetary Scientific Institution of the Federal Research Center for Nutrition and Biotechnology, showed that a portion of direct-pressed juice (100 ml) is able to meet the needs of a young child in potassium by 17 .2-42.5% of the recommended consumption rate (RIA), in copper - by 6.8-10.4% of the RDA, in chromium - by 9-18% of the RDA, in dietary fibers - by 15-17, 5% of RNP.
Enrichment of fruit juice drinks with inulin (0.45 g per 100 ml) ensures the satisfaction of the daily physiological needs of children older than 12 months. in dietary fiber by 4.5% when consuming 100 ml of the drink. The inclusion of vitamins and minerals in these drinks will ensure that the physiological needs of children older than 12 months are satisfied when consuming 100 ml of the drink. in vitamin D by 10%, in vitamins A, E, C, iron and calcium - by 15% [18].
Juice restrictions in childhood
In accordance with domestic recommendations [19], juices should not be included in the diet of children before 8 months of age. life. According to the recommendations of the American Academy of Pediatrics (AAP) (2016) [2] and ESPGHAN (2017) [20], it is not recommended to introduce juices into the diet of children under 12 months of age. life.
It is necessary to control the amount of juice in the diet of children, regardless of age. A meta-analysis [21], published in 2017, indicates that juices can have a negative impact on health when their daily intake is exceeded by more than 200 ml / day in children of the 2nd half of life and more than 300 ml / day by children older than one year. Data on the effect on the increase in body mass index (BMI) of various types of juices in children are contradictory. Some studies [22] have found an increase in BMI as a result of daily juice consumption in children under the age of 6 years f2.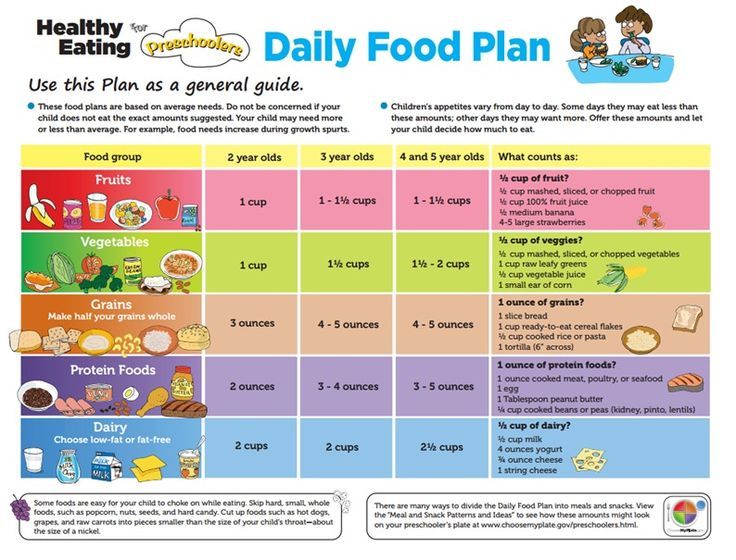 In other studies [23], this hypothesis was not confirmed. At the same time, most researchers [13, 20] agree that randomized controlled trials are required to assess the impact of juice consumption on children's health, including the impact on BMI and obesity development, including depending on the type of juice. Until then, it is recommended to limit the amount of juice consumed by children of all age groups [24]. Table 4 shows modern Russian [1] and American [2] recommendations for the amount of juice in the diet of children, depending on their age.
In other studies [23], this hypothesis was not confirmed. At the same time, most researchers [13, 20] agree that randomized controlled trials are required to assess the impact of juice consumption on children's health, including the impact on BMI and obesity development, including depending on the type of juice. Until then, it is recommended to limit the amount of juice consumed by children of all age groups [24]. Table 4 shows modern Russian [1] and American [2] recommendations for the amount of juice in the diet of children, depending on their age.
All experts [1, 7, 17] point out the importance of using commercially produced products in the organization of nutrition for young children, which have guaranteed safety and a stable ingredient and chemical composition, are characterized by the high quality of the raw materials used, optimal consistency, and the possibility of enrichment with limited nutrients.
Adding any food additives (dyes, stabilizers) and flavorings to juices and juice products for baby food is prohibited both in our country [1] and abroad [2].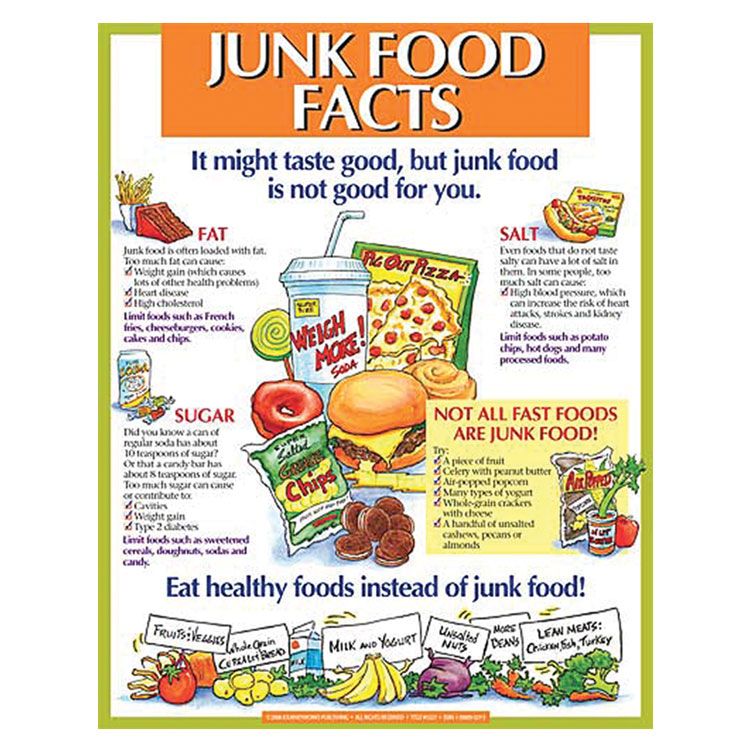 The only exceptions are some additives, such as natural fruit flavors obtained by a special technology in the manufacture of concentrated juices, as well as citric and ascorbic acids [1, 2].
The only exceptions are some additives, such as natural fruit flavors obtained by a special technology in the manufacture of concentrated juices, as well as citric and ascorbic acids [1, 2].
The quality and safety of juices are regulated by the requirements of the technical regulations of the EEC: "On food safety" (TR TS 021/2011) [25], "Technical regulations for juice products from fruits and vegetables" (TR TS 023/2011) [26], and See also "Unified sanitary-epidemiological and hygienic requirements for goods subject to sanitary-epidemiological supervision (control)" [27].
Conclusion
When using fruit juices in baby food, the following rules should be followed: do not offer the child juices between meals, as entertainment, or, on the contrary, in order to calm him down. The use of any juice-containing drinks, as well as juices, including those offered for baby food, should be regulated taking into account the amount of juice component in their composition, recommendations for the amount of juice in baby food should serve as a guide for this.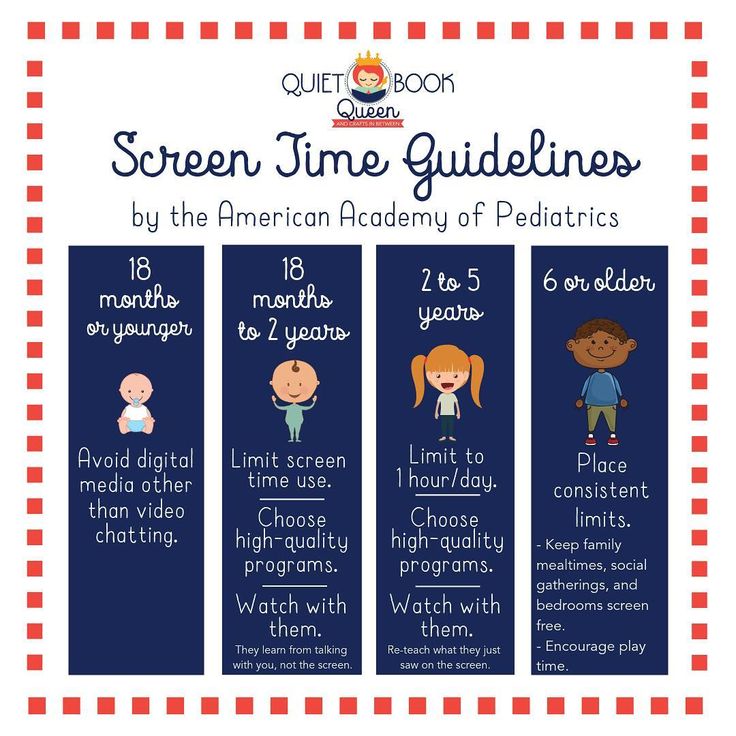 Large randomized trials are needed to reach a consensus on the maximum allowable sugar content, the number of drinks consumed per day, and the age of children when the use of juices and juice-containing drinks is acceptable.
Large randomized trials are needed to reach a consensus on the maximum allowable sugar content, the number of drinks consumed per day, and the age of children when the use of juices and juice-containing drinks is acceptable.
Gratitude
The editors would like to thank PROGRESS JSC for their assistance in the technical editing of this publication.
Acknowledgments
Editorial Board is grateful to JSC "PROGRESS" for the assistance in technical edition of this publication.
Information about authors:
Safronova Adilya Ilgizovna - Ph.D. 109240, Russia, Moscow, Ustyinsky proezd, 2/14; ORCID ID 0000-0002-6023-8737.
Pyreva Ekaterina Anatolyevna - Ph.D. 109240, Russia, Moscow, Ustyinsky proezd, 2/14; ORCID iD 0000-0002-9110-6753.
Georgieva Olga Valentinovna - Ph.D., Senior Researcher, Laboratory of Age-Related Nutrition, Federal State Budgetary Institution of Science, Federal Research Center for Nutrition and Biotechnology; 109240, Russia, Moscow, Ustyinsky proezd, 2/14; ORCID iD 0000-0002-1157-8751.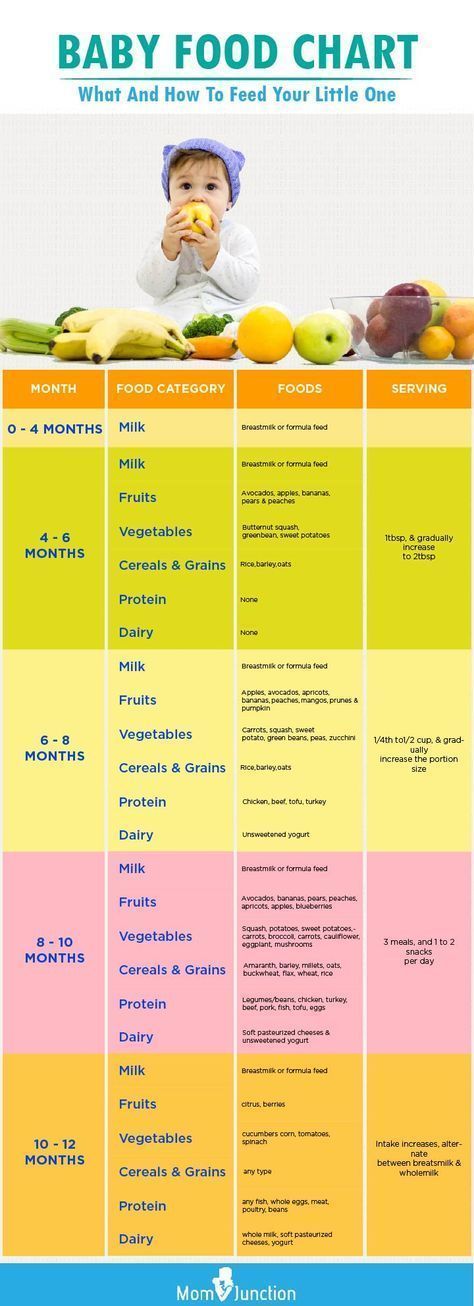
Contact information: Pyrieva Ekaterina Anatolyevna, e-mail: [email protected].
Financial transparency: none of the authors has a financial interest in the submitted materials or methods.
No conflict of interest.
Article received on 04.12.2021.
Received after review on December 28, 2021.
Accepted for publication 01/27/2022.
About the authors:
Adilya I. Safronova - C. Sc. (Med.), leading researcher of the Laboratory of Age-related Nutrition, Federal Research
Center for Nutrition & Biotechnology; 2/14, Ust'inskiy pass., Moscow, 109240, Russian Federation; ORCID ID 0000-0002-6023-8737.
Ekaterina A. Pyr'eva - C. Sc. (Med.), Head of the Laboratory of Age-related Nutrition, Federal Research Center for Nutrition & Biotechnology; 2/14, Ust'inskiy pass., Moscow, 109240, Russian Federation; ORCID iD 0000-0002-9110-6753.
Olga V. Georgieva - C. Sc. (Tech.), senior researcher of the Laboratory of Age-related Nutrition, Federal Research Center for Nutrition & Biotechnology; 2/14, Ust'inskiy pass., Moscow, 109240, Russian Federation; ORCID iD 0000-0002-1157-8751.
Contact information: Ekaterina A. Pyr'eva, e-mail: [email protected].
Financial Disclosure: no authors have a financial or property interest in any material or method mentioned.
There is no conflict of interest.
Received 12/04/2021.
Revised 12/28/2021.
Accepted 01/27/2022.
Complementary foods - introduction of fruit puree, fruits and juices into the baby's diet
Historically, fruit juice was recommended by pediatricians as a source of vitamin C, calcium, and other vitamins. The juice is delicious, sweet, children drink it with pleasure, and suddenly it turned out that there are potential risks: the high sugar content in the juice increases calorie intake, overweight and the risk of caries. More recently, about twenty years ago, doctors recommended the introduction of complementary foods, starting with juices and fruits. But now the situation has changed. Children's nutritionists believe that the optimal time for the introduction of juices is 1 year after the child gets used to the main complementary foods: vegetables, cereals, meat, fish, fruits. At the same time, you can find recommendations to give juices from 6 months or after 3 years. Carbohydrates, which are abundant in juice, change the child's appetite, but to get the required amount of vitamins, you need to drink a lot of it, about 1 liter! In addition, they do not give a feeling of satiety and the child may be prone to overeating.
More recently, about twenty years ago, doctors recommended the introduction of complementary foods, starting with juices and fruits. But now the situation has changed. Children's nutritionists believe that the optimal time for the introduction of juices is 1 year after the child gets used to the main complementary foods: vegetables, cereals, meat, fish, fruits. At the same time, you can find recommendations to give juices from 6 months or after 3 years. Carbohydrates, which are abundant in juice, change the child's appetite, but to get the required amount of vitamins, you need to drink a lot of it, about 1 liter! In addition, they do not give a feeling of satiety and the child may be prone to overeating.
Administering fruit juice American Academy of Pediatrics recommendations: download
- Optimal to completely avoid the use of juice in infants under 6 months;
- AAP and the American Academy of Pediatric Dentistry guidelines state that juice should be offered to babies in a cup, not a bottle, and that babies should not go to bed with a bottle in their mouth.

- They concluded that long-term exposure to the sugar contained in the juice on the teeth is the main factor influencing dental caries.
- After 1 year, fruit juice can be used as part of a meal or snack. It should not be drunk like water during the day or used as a means to calm an upset child.
- Do not give juices if the child has diarrhea, oral rehydration solutions only.
- The development of perioral rash in some children after feeding freshly squeezed citrus juice is most likely due to the chemical irritant effect of the acid.
- Diarrhea and other gastrointestinal symptoms that some children experience are most commonly associated with carbohydrate malabsorption.
- Although fruit allergy can develop at an early age, this is rare.
Baby food - fresh juices
Freshly squeezed juices are not recommended for children under one year of age. But there is no strict ban. Juice until the year is not useful, unlike children older than one year .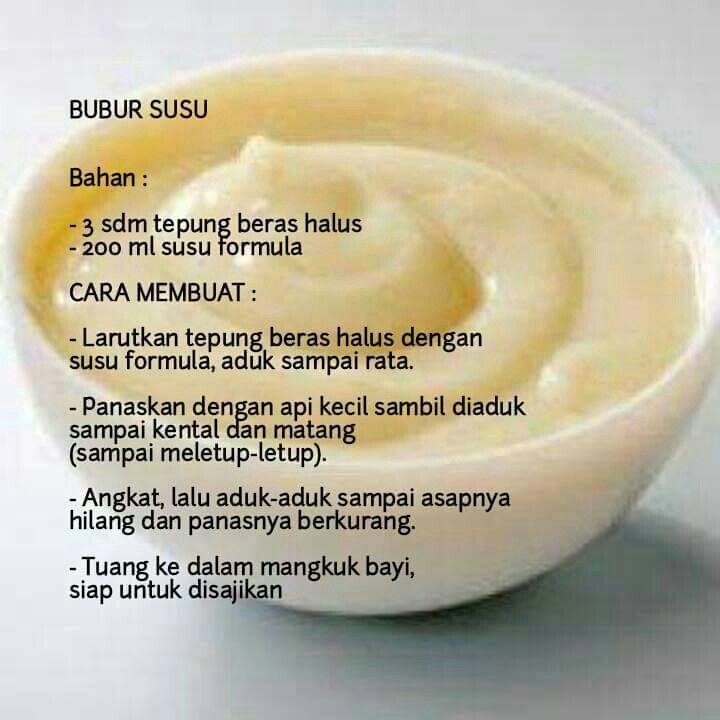 It contains a lot of fruit acid, which can lead to increased peristalsis and intestinal walls, pain, and digestive disorders. Dilute with water in a ratio of 1:1. And remember, fresh juice retains its maximum amount of vitamins in the first half hour, so do not store juice for later. With a later introduction of juice, their better tolerance is noted. This is due to the maturation of the mucosa of the gastrointestinal tract and its readiness for the absorption of juice. But even with this, the child may experience pain and bloating, regurgitation, and stool disorders. This is due to the presence of organic acids in juices, which have an irritating effect on the gastrointestinal tract.
It contains a lot of fruit acid, which can lead to increased peristalsis and intestinal walls, pain, and digestive disorders. Dilute with water in a ratio of 1:1. And remember, fresh juice retains its maximum amount of vitamins in the first half hour, so do not store juice for later. With a later introduction of juice, their better tolerance is noted. This is due to the maturation of the mucosa of the gastrointestinal tract and its readiness for the absorption of juice. But even with this, the child may experience pain and bloating, regurgitation, and stool disorders. This is due to the presence of organic acids in juices, which have an irritating effect on the gastrointestinal tract.
How do I start adding juice to my baby?
First, a teaspoonful (about 5 ml) between feedings, observing the baby's reaction. For children under 3 years old, juices are recommended to be diluted with boiled or baby water in a ratio of 1:2. Freshly squeezed juices - up to 7-8 years. The amount of juice: from 1 year to 1.5 years - up to 100 ml, should not be exceeded. At 2 years - 200 ml.
The amount of juice: from 1 year to 1.5 years - up to 100 ml, should not be exceeded. At 2 years - 200 ml.
At first it is better to give the juice of green apples or pears. Juice from plums, apricots, peaches - it is better to give at an older age, they have a slight laxative effect.
Then you can give a mixture of juices from 2 or 3 fruits. You can give a mixture of cherry, cherry, currant, raspberry juice, orange juice, pineapple, mango, grapefruit and mixtures thereof. It is better to give grape juice from 5-6 years old, there are a lot of carbohydrates.
It must be remembered that:
- Apple, carrot and pear juice - strengthen
- Plum, pumpkin, apricot, peach - weakening
This can be used if there are digestive problems.
If we choose industrial juices - carefully read what is written on the label, there should be no artificial additives, dyes and preservatives. Do not use opened packages. Should I give industrial juices for baby food? Why not? They are made from high quality, proven, specially selected raw materials, production is strictly controlled, they have balanced compositions and optimal taste. Until the age of 3, buy juices for your child only marked “baby food” on the package.
Do not use opened packages. Should I give industrial juices for baby food? Why not? They are made from high quality, proven, specially selected raw materials, production is strictly controlled, they have balanced compositions and optimal taste. Until the age of 3, buy juices for your child only marked “baby food” on the package.
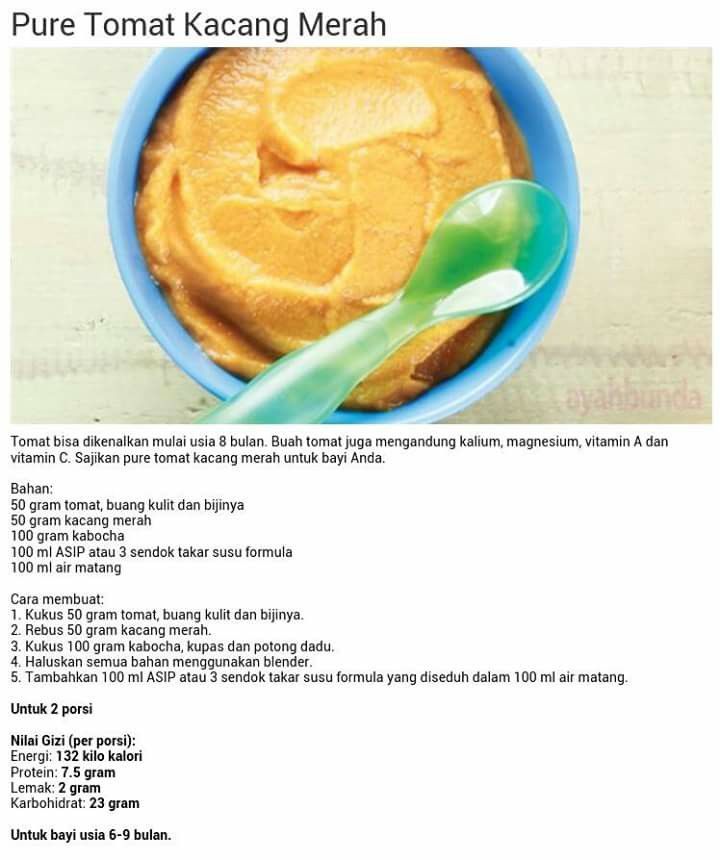
Introduction of fruit and fruit puree - European recommendations
If your young child has already tasted vegetables and accepted them, it's time for fruit. The season is always for them, but the best is in autumn, when the most delicious apples, pears and plums appear. Fresh fruits from all over the world are available in stores all year round, but it's worth starting with seasonal, locally grown ones. And these are: apricots, raspberries, apples, pears, plums. They contain not only vitamins, dietary fiber, but also minerals, including valuable microelements, which should be present in the child during the expansion of the diet.
Fruit is usually recommended from 6-7 months of age. Complementary foods often begin with fruit or vegetable purees. But it is better to start with vegetables. Fruit puree tastes better, is sweeter, and the child may then eat vegetables worse. But vegetable puree will not affect the baby's desire to eat fruit dishes. Therefore, more often pediatricians are advised to give fruit dishes after the introduction of vegetables and cereals. Start complementary foods with fruits in the form of mashed apples or bananas or pears. Then you can add fruits that grow in your area of \u200b\u200bresidence. Then you can include fruit and fruit and vegetable mixtures.
Fashionable but exotic fruits or with strong flavors - strawberries, mangoes, kiwis, currants - are best introduced later. But there is no strict ban.
Fruit puree should be started with 1 teaspoon in the morning, increasing to 100 g over 2 weeks.
Homemade or factory made? As you wish, subject to the basic hygiene rules of cooking. If you have time, make your own fruit puree. Plums, apricots, banana can be mashed in a mortar or blender. Grate apples and pears on a fine plastic grater. For the first time, the apple can be boiled, then it will be soft. Pour the prunes with boiling water and leave for 15 minutes. Do not add sugar!
If you have time, make your own fruit puree. Plums, apricots, banana can be mashed in a mortar or blender. Grate apples and pears on a fine plastic grater. For the first time, the apple can be boiled, then it will be soft. Pour the prunes with boiling water and leave for 15 minutes. Do not add sugar!
Homemade fruit puree - don't forget about hygiene
Pour boiling water over a grater, preferably a plastic one or a blender, wash and peel the fruit.
Gradually make the fruit puree coarser.
Start with liquid puree, at 8 months to finely ground puree, at 10 months of age. - puree from larger particles.
When the child has 6-8 teeth, you can give pieces of fruit and he will eat them on his own.
Properties of various fruit purees
- Banana puree is a good source of trace elements: magnesium and potassium, calcium, iron and phosphorus.
 Bananas rarely cause allergic reactions
Bananas rarely cause allergic reactions - Prune puree can act as a mild laxative that increases intestinal motility. Contains potassium, vitamins B1 (thiamine), B2 (riboflavin).
- Blueberry puree contains tannin - tannin, contains pectin, which has a disinfectant and anti-inflammatory effect, contains a large amount of provitamin A - beta-carotene, which is good for vision, manganese. In addition, blueberries are low allergenic. Apricots are an excellent source of potassium, carotene, vitamin C and pectin.
Tips from the Nyankovskih Healthy Child University
- Fruits are sweet and can be used instead of sweets.
- Fruits should be introduced into the child's diet as the second food group after vegetables. They can be given quite early, when the baby is four months old (between 17 and 26 weeks of age).
- Initially it can be a mousse (or puree from a jar) and then an apple scraper with a spoon.