Age for stage 1 baby foods
The 3 baby food stages: What foods and when
Making the leap from breast milk or formula to solids and then eventually to table food is an exciting time. But it’s also a little confusing because there isn’t a one-size-fits-all rule when it comes to baby food stages. While one child may happily take to pureed carrots at 6 months, another may purse their lips at anything but a breast or bottle until 8 months.
To simplify the whole process, here’s a general rule of thumb to keep in mind: Most foods are OK to give to babies in the first year, as long as they’re properly prepared. And if you’re concerned about food storage, read more from our experts on how long baby food lasts.
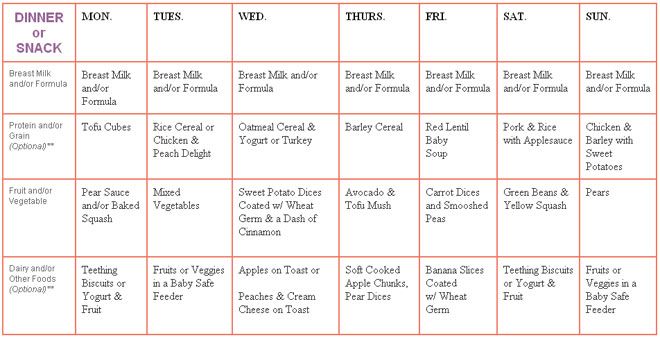
Here’s the quick lowdown on what to feed baby and when:
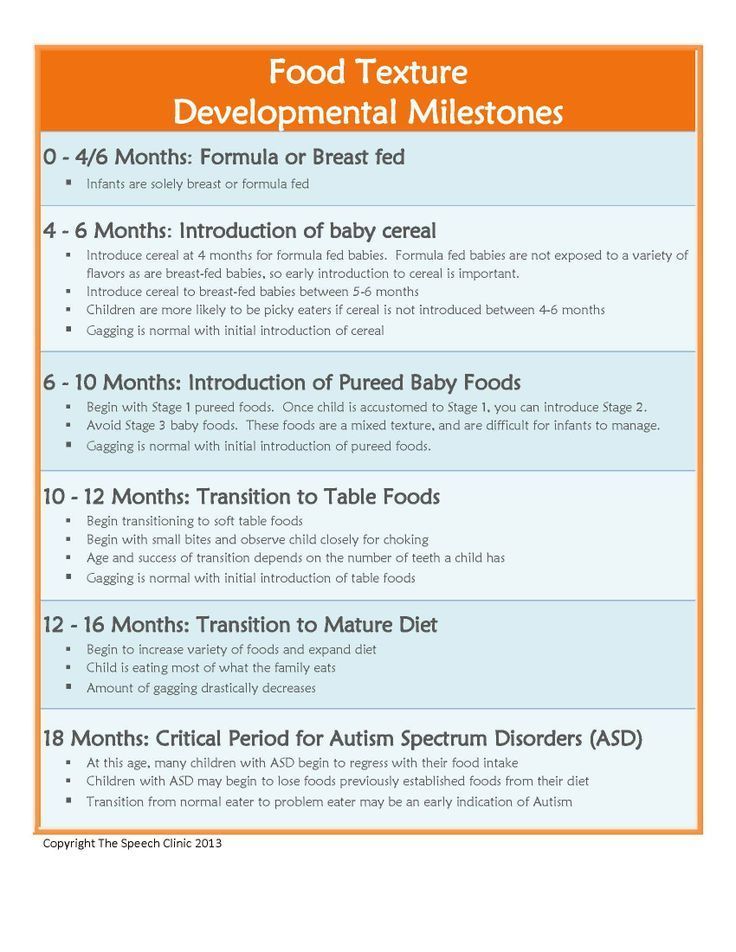
- Stage 1: Purees (4 to 6 months).
- Stage 2: Thicker consistency (6 to 9 months).
- Stage 3: Soft, chewable chunks (10 to 12 months).
“With the exception of raw or cooked honey, which shouldn’t be consumed until 12 months because of the risk of infantile botulism, babies can have any food that is texturally appropriate for their developmental feeding stage,” says Dr. Kristen Treegoob, a pediatrician at Children’s Hospital of Philadelphia.
In other words, it’s perfectly fine to give both a 6- and 12-month-old peas, but for the 6-month-old, they need to be pureed.
In the past, parents have been advised to start their baby with single-grain cereals, such as rice cereal, but the American Academy of Pediatrics (AAP) now says there’s “no medical evidence that introducing solid foods in any particular order has an advantage for your baby” — nutritionally or when it comes to long-term food preferences. (So, when your Aunt Joanne tells you that your baby will be a vegetable-hater for life if you start off with applesauce, she’s wrong.)
All of this said, there is a method to the messy madness that is the three stages of baby food. In order to make things less complicated — and more delicious — we tapped top experts and veteran parents to find out everything you need to know about feeding little ones at every stage (plus, we included a handy baby food stages chart). All you have to do now is serve the food and clean the high chair!
All you have to do now is serve the food and clean the high chair!
Stage 1 (4 to 6 months): What you need to know
The fun begins! Stage 1 baby food is typically for babies who are between the ages of 4 months and 6 months. But as with all things parenting-related, it’s important to keep in mind that each baby is different, and there’s no hard and fast rule for starting solids.
“While the AAP recommends exclusively breastfeeding from birth to age 6 months, it’s important to remember that not every baby is exclusively breastfed,” says Dr. Zulma Laracuente, a pediatrician in Alexandria, Louisiana. “Also, some babies show signs of readiness to start food earlier than others. You know your baby best.”
Solids that fall under the Stage 1 category are thin and smooth in texture — not much thicker than breast milk or formula — and contain a single ingredient. If you’re making your baby’s food at home, make sure it’s blended to an almost-watery puree.
“Stage 1 baby foods should have no chunks whatsoever,” says Jenifer Thompson, registered dietician and advanced practice dietician at Johns Hopkins in Baltimore. “Formula or breast milk can be added to the purees to make them thinner.”
“Formula or breast milk can be added to the purees to make them thinner.”
While there’s no specific food parents need to start with, many pediatricians recommend beginning with iron-rich foods, such as iron-fortified cereals or pureed meats.
“The reason we advise introducing solids at 6 months and starting with iron-containing foods is because iron stores that were built up during pregnancy are depleting, and iron is important for infants’ brain development,” says Dr. Melanie Custer, a pediatrician at Deaconess Clinic in Evansville, Indiana.
Custer also says that babies should “absolutely not” decrease their breast milk or formula when they first start off with solids.
“Infants still should receive 24 to 32 ounces of formula or breast milk each day,” she says. “Solids at this point are more of a snack, with baby eating about 3 to 4 tablespoons once or twice a day.”
How to tell your baby is ready for Stage 1
According to Treegoob, here are the signs your baby is prepared to start Stage 1 foods:
- They’re showing an interest in what family members are eating.

- They’re learning to open their mouths for a spoon.
- They’ve outgrown the involuntary habit of pushing food and spoons out of their mouth with their tongue.
- They have steady head control.
- They have the ability to move food from a spoon to their throat and swallow without choking.
Stage 2 (6 to 9 months): What you need to know
Time to mix it up! While Stage 2 solids are still basically mush, food has a little more texture at this point, as well as a few soft chunks.
“Stage 2 baby foods are thicker in consistency than Stage 1 purees, and many of the jars you find in stores have some small mashable bits in them,” says Treegoob. “These are great for infants who have done well with Stage 1 but who are not quite ready to chew. The typical age for Stage 2 is between 6 to 9 months.”
Treegoob also notes that the 7 to 9 month time frame is also when many babies begin modifying their breast milk or formula intake.
“As long as an infant’s weight remains on track and they’re drinking enough to stay hydrated, there isn’t a reason to worry if baby is showing interest in smaller or less frequent bottle or breastfeeds,” she says. “Infants typically take in somewhere between 24 to 32 ounces a day when they’re between 6 to 9 months.”
“Infants typically take in somewhere between 24 to 32 ounces a day when they’re between 6 to 9 months.”
Whether you’re making your little one’s food on your own or getting it pre-made at the store, you have a little more room to play once you hit Stage 2.
“In addition to being thicker in consistency, Stage 2 foods usually have multiple ingredients, including some spices,” says Custer. “At this point, baby is usually taking in more food than they were in Stage 1, so it’s important to make sure they’re being introduced to a wide variety of foods from different food groups.”
According to the AAP, babies should be eating about 4 ounces of solids — about one small jar of baby food — at each of their meals.
How to tell your baby is ready for Stage 2
Once your baby has consistently been eating Stage 1 foods, they’re likely ready for the next step. Here are other signs to look for, according to Thompson:
- Their oral skills are continuing to develop.
- They’re consistently taking food in and swallowing when you offer it (and not spitting it out).
Stage 3 (9 to 12 months): What you need to know
Now, the true culinary adventure begins — Stage 3 foods! While some babies will still happily have mom and dad spoon-feed them mashed food at this age, many babies will have what you’re having at this point — and they’ll do it themselves, thank you very much.
“As soon as we thought he was ready — at about 9 months — we started giving my son softer, cut-up versions of whatever we were having for dinner,” says mom of two Jennifer Reilly, of New York City. “There was more cleanup, but I actually got to sit down and eat my meal!”
Once babies hit the age range for Stage 3 foods, most have the oral and fine motor skills to self-feed.
“Between 8 to 12 months, babies develop the pincer grasp ability and should be able to pick up small pieces of finger foods with their finger and thumb and bring it to their mouth,” says Thompson.
Technically speaking, Stage 3 solids are thicker, more sophisticated versions of the baby food your little one has already been eating (think vegetable and beef pilaf or tender chicken and stars), but also, they’re not necessary for everyone.
“Stage 3 food is starting to have chunks mixed in, in order to prepare baby for table foods,” says Custer. “But some babies wind up skipping this stage altogether and go straight to soft table foods.”
While it’s perfectly fine to continue with Stage 3 foods up to your child’s first birthday, Treegoob advises letting your baby try their hand at “real food.” “Well-cooked veggies, ripe fruits, shredded meat, scrambled eggs, soft cheese and cooked pasta are all great options for babies this age,” she notes.
Between 9 months and 12 months is also when you’re likely to see a significant drop in how much breast milk or formula your baby is drinking.
“As babies continue to eat table foods, I’ve seen their breast milk or formula intake drop to as low as 16 to 20 ounces per day,” Treegoob says. “That said, some infants continue to show a heavy preference for breast milk or formula despite months of solid introduction. If you feel like your baby may be drinking excessive amounts of breast milk or formula, and they have no interest in food, I would recommend speaking with your pediatrician.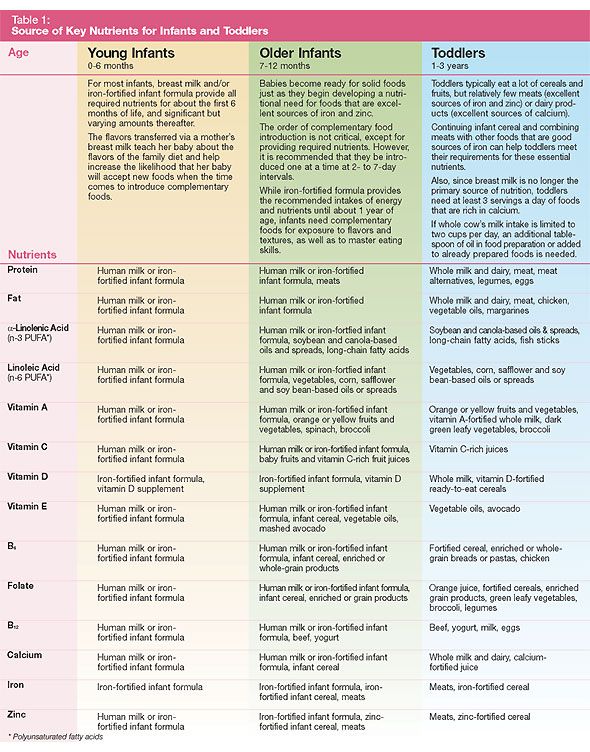 ”
”
How to tell your baby is ready for table food
Your child’s readiness to start table food will likely be more discernible than any other baby food stage. As long as they’re continuing to hone their oral skills, as well as their ability to pick food up and bring it to their mouth, you can count on them to let you know they’re ready for “big kid” food.
“My daughter looked like she was ready for pasta, eggs and basically anything we were eating shortly after she started solids,” says mom of two Julie Cortez of Brooklyn, New York. “We waited until about 8 months, when we knew she knew how to properly eat, and sure enough, she ate her whole plate on the first go! We completely skipped the Stage 3 jars of food.”
Follow these safe feeding must-knows
Even though your baby’s eating skills will continue to progress as they gain more experience, it’s important baby is always sitting upright, strapped in a high chair and never left unattended while eating. Also, make sure table food is always soft and cut into small pieces to avoid choking hazards. When first starting out with solids, be sure to wait a few days before giving them something new.
When first starting out with solids, be sure to wait a few days before giving them something new.
“This allows for observation for any adverse reaction or intolerance to the new food,” Thompson says.
And finally, be sure to give your baby a wide range of healthy food in order to expose them to a variety of tastes and textures — and don’t be discouraged if they don’t take to a specific food at first.
“If baby refuses a food or makes a strange face when eating, this may simply mean that it is a new food and unfamiliar to them,” Thompson says. “Try again. It may take 10 to 20 exposures of a new food before they accept it.”
Here’s more on every baby food stage:
- Stage 1 baby food.
- Stage 2 baby food.
- Stage 3 baby food.
When is a child ready to start solids?
Diving into the world of solid food with your baby is a messy, adorable milestone that, let’s be honest, sometimes feels a little confusing. While some little ones happily slurp down baby cereal at 6 months, others won’t go near a mashed carrot until they’re hitting the 9-month mark — what gives?
The truth is, while solid food exposes babies to new tastes and textures, it’s not even necessary in the very beginning (yes, really).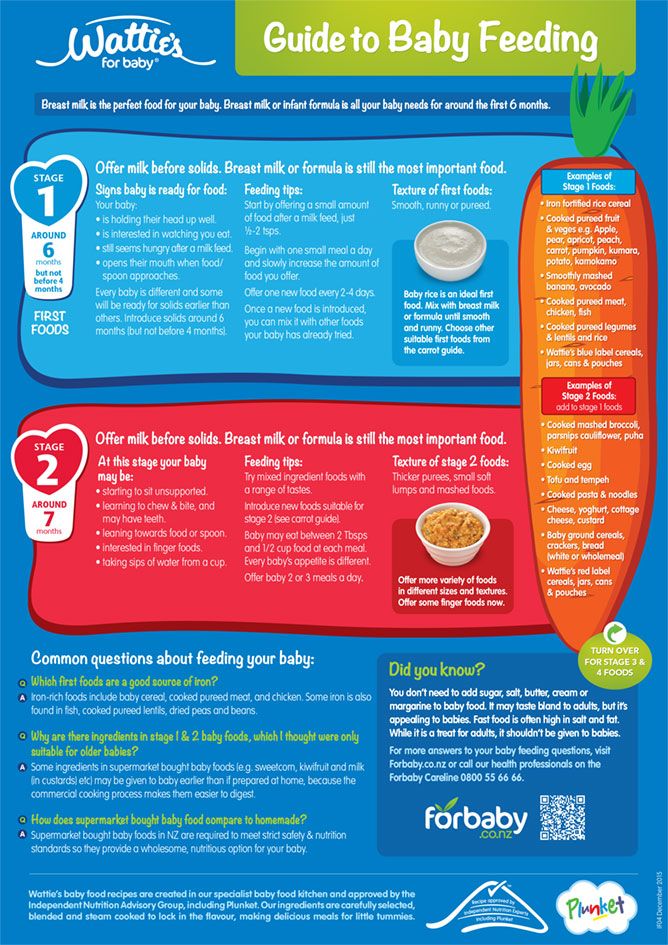
“While the general recommendation for starting solids is between 4 and 6 months old, solids at this point are more about introducing baby to new tastes and developing oral motor function,” says Dr. Melanie Custer, a pediatrician at Deaconess Clinic in Evansville, Indiana. “Breast milk or formula should continue to be the primary source of nutrition through 12 months.”
Of course, when your baby is eyeballing your bowl of oatmeal every morning, it’s only natural to start wondering when to start baby food. Here, experts and veteran parents weigh in on the dos and don’ts of starting solids, a.k.a. Stage 1 baby foods. Ready the bibs!
What is Stage 1 baby food?
Stage 1 baby foods are single-ingredient foods that are very thin in consistency. You can either buy them at the store or make them yourself, as long as they’re a smooth puree with zero chunks and include just one ingredient so you’re introducing your baby to one new food at a time.
And remember, every child is different and develops at their own individual pace. Check with your child’s doctor for baby food recommendations during the first year.
Check with your child’s doctor for baby food recommendations during the first year.
When to start Stage 1 baby food
According to Custer, the reason it’s recommended that full-term babies wait until 6 months to try solids is because they’re losing iron stores that were built during pregnancy, and iron is important for infants’ brain development.
“Growing babies need all the nutrients they can get — and breast milk and formula are both far superior to solids when it comes to nutrients, including iron,” says Jenifer Thompson, an advanced practice dietician at Johns Hopkins in Baltimore. “It’s important to remember that solid foods are also called complementary foods because their intention is to complement the breast milk and/or formula baby is drinking.”
Thompson also notes that offering solids too early on — prior to 4 months — has been associated with excessive weight gain and adiposity (excess fat) in preschool and older ages.
Signs baby is ready to start solid food
Knowing your baby is ready for Stage 1 foods goes beyond celebrating their half-year birthday.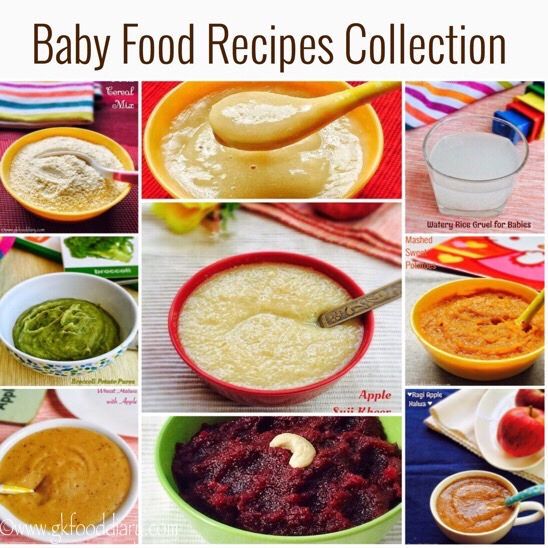 It’s important to look out for developmental and social signals, as well.
It’s important to look out for developmental and social signals, as well.
“One of the biggest indicators that your baby is ready for solid foods is that they’re showing an interest in what other family members are eating,” says Dr. Kristen Treegoob, a pediatrician at Children’s Hospital of Philadelphia.
If you notice baby staring at your food and opening their mouth or leaning forward if food is ever offered, these are signs that solid foods have piquéd your baby’s interest, according to Thompson.
“I knew my son was ready for solids when, at 7 months, he started staring — like, really staring — at all of our food during dinner,” says mom of two Erin Henderson, of Waltham, Massachusetts. “It reached a point where we felt bad eating in front of him!”
Other signs your baby may be ready for solids, according to Custer and Thompson, include:
- They can sit up with little to no support.
- They can hold their head up without being wobbly.
- Their tongue thrust reflex has disappeared.
 “Before introducing solids, it’s important to make sure your baby can open their mouth for a spoon and accept food off of it, rather than pushing it away with their tongue, which is an involuntary habit until about 4 months,” says Custer.
“Before introducing solids, it’s important to make sure your baby can open their mouth for a spoon and accept food off of it, rather than pushing it away with their tongue, which is an involuntary habit until about 4 months,” says Custer.
What Stage 1 baby food to start with
According to Thompson, it’s recommended that early solid foods provide a source of iron, protein and zinc. But remember, you’re complementing your baby’s diet, not revamping it, so it’s OK to get a little creative and go with your gut.
“There is no medical evidence that solid foods must be introduced in any particular order, or that vegetables must be introduced before fruits to ensure that they don’t have a preference for sweets and will it not lead to a dislike of vegetables,” says Thompson.
And once you get going, continue to mix it up.
“There is no one-size-fits-all for solid food introduction, and we typically recommend parents introduce a variety of tastes, colors and food groups in the first few months,” says Treegoob. “That said, the American Academy of Pediatrics recommends that breastfed infants first begin with iron-rich foods, which include iron-fortified infant cereals and iron-rich pureed meats. Formula-fed infants typically get enough iron through formula, so they may have a little more flexibility at first.”
“That said, the American Academy of Pediatrics recommends that breastfed infants first begin with iron-rich foods, which include iron-fortified infant cereals and iron-rich pureed meats. Formula-fed infants typically get enough iron through formula, so they may have a little more flexibility at first.”
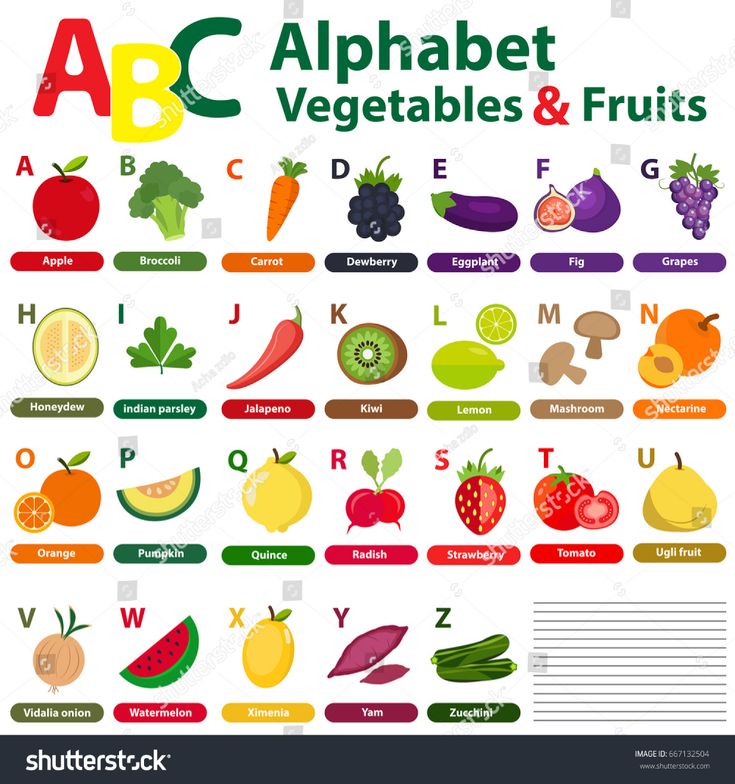
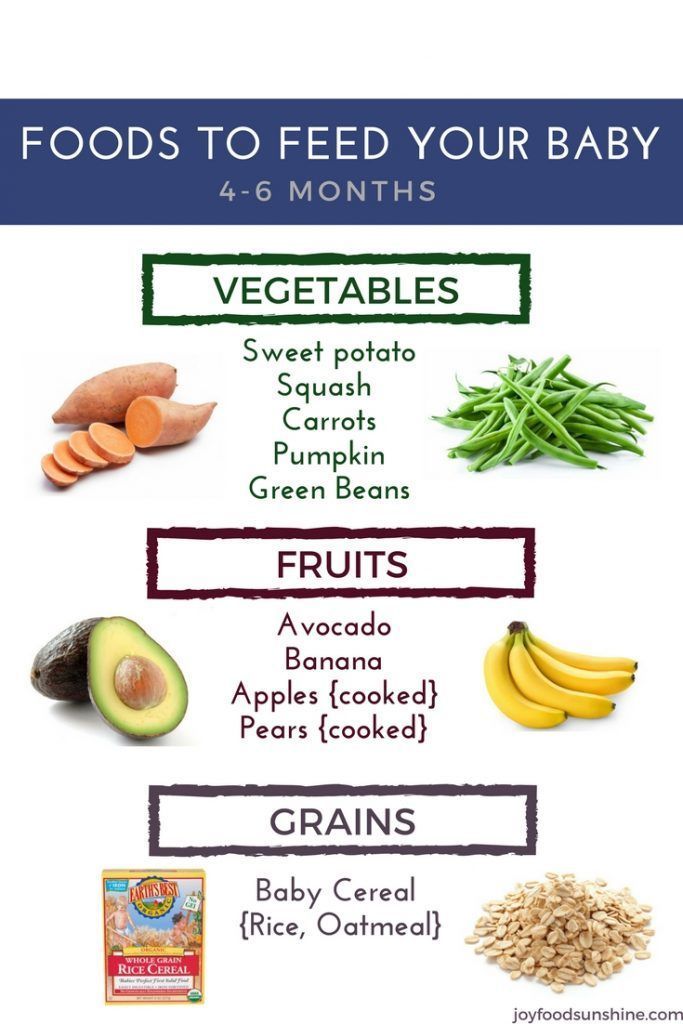
Here’s a list of first foods to try (make sure all are pureed to very thin consistency):
- Bananas.
- Avocados.
- Sweet potatoes.
- Carrots.
- Pureed meats, such as chicken and turkey.
- Butternut squash.
- Peaches.
- Applesauce.
- Grains, such as barley, oats, wheat and rice.
Custer does note that infants should not eat raw or cooked honey until 12 months, as it might contain spores that can cause infantile botulism, a serious illness that can hamper an infant’s ability to move, eat and breathe. For more tips on food storage, our experts weigh in on how long baby food lasts.
How to start Stage 1 foods safely
When your baby first starts experimenting with solids, keep in mind it’s a gradual process, and you’re still a ways off from three solid meals per day. In the beginning, it’s best to think of solids as more of a snack than a meal.
In the beginning, it’s best to think of solids as more of a snack than a meal.
“Babies will often start with just a bite or two at first and advance to three to four tablespoons at a time,” says Custer. “When they’re first starting off around 6 months, they can have solids one or two times a day.”
“Foods should be offered one at a time when babies are starting off with solids,” says Thompson. “Then, wait between three to four days before introducing a new one, so you can properly identify an adverse reaction or intolerance.”
Here are a few more tips for feeding your baby:
- Make sure they’re sitting in an upright position, such as in a highchair, to prevent the risk of choking.
- Add a little breast milk or formula to their food. “At first, foods should be just slightly thicker than breast milk or formula to allow the infant to get used to eating,” Custer says. “Foods can get thicker as their eating skills are mastered.”
- Always feed your baby with a spoon.
 “Unless you’ve been advised by your pediatrician, never put solid foods, including infant cereal, in bottles with or without milk,” says Treegoob.
“Unless you’ve been advised by your pediatrician, never put solid foods, including infant cereal, in bottles with or without milk,” says Treegoob. - Give baby breast milk or formula first. “Both of my babies were more open to trying solid foods in the beginning when they were happy and relaxed,” says mom of two Darcy McConnell of Garwood, New Jersey. “That was always after they had their bottle.”
Also, be patient. Starting solids is a learning curve for everyone.
“If your baby turns their head away, spits out food or pushes you away with their hands when you try to feed them solid food, then they are not quite ready,” says Treegoob. “Try again in a few days.”
How baby-led weaning works
A less conventional way to start your baby on real food is baby-led weaning, which forgoes what’s thought of as Stage 1 baby food altogether, as well as a spoon.
“The baby-led weaning approach to introducing solid foods recommends that purees and traditional baby foods be omitted, and to start with finger foods, as well as self-feeding right from the beginning,” says Thompson.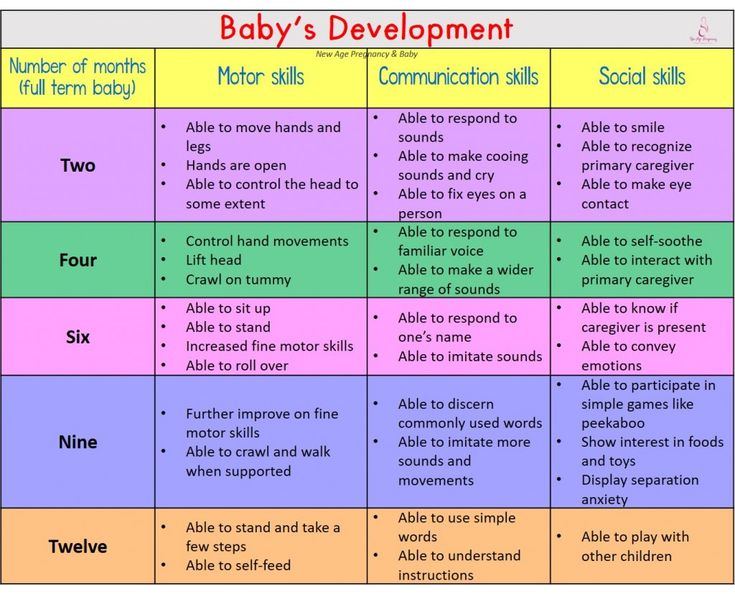 “This method may be preferred for some, but should always be discussed with a pediatrician since a possible concern of this method is the risk of choking, which could be minimized with appropriate food choices.”
“This method may be preferred for some, but should always be discussed with a pediatrician since a possible concern of this method is the risk of choking, which could be minimized with appropriate food choices.”
Proponents of baby-led weaning believe that letting baby pick, choose and explore food on their own will help with appetite control overall (possibly reducing the risk of obesity later in life), as well as promote a taste for a wider range of foods. All of this said, research on baby-led weaning is still fairly scant, so it’s important to discuss it with your pediatrician if you choose to take this approach.
Ready for the next stages?
- Stage 2 baby food
- Stage 3 baby food
🎖▷ Why you don't have to worry about weight gain with Lamictal
psychology
8,268 2 min read
If you're worried that taking Lamictal (lamotrigine) may cause weight gain, there's good news. It probably won't affect your weight much.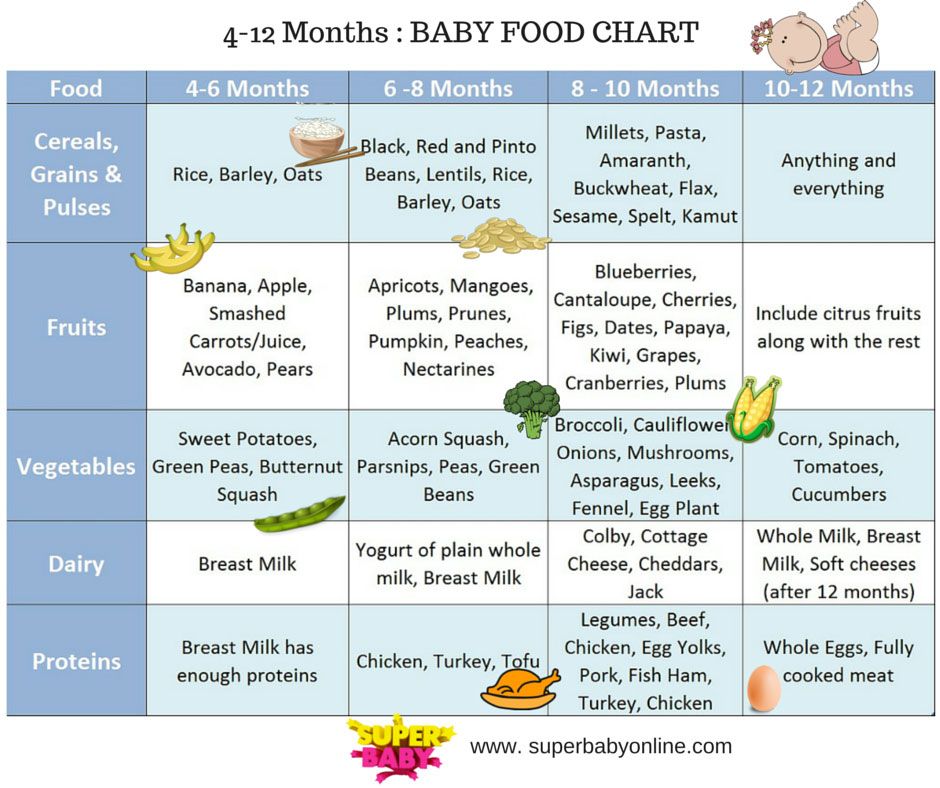 If anything, you're more likely to lose weight due to Lamictal than gain weight, but either way, the changes are likely to be pretty small.
If anything, you're more likely to lose weight due to Lamictal than gain weight, but either way, the changes are likely to be pretty small.
The effect of Lamictal on weight has been little studied, and various clinical trials have found minimal effect. In fact, some researchers even considered the drug as a possible remedy for obesity and as a remedy for overeating. This information should be reassuring for people with bipolar disorder, as many of the medications used to treat this condition can cause weight gain. nine0003
Lamictal findings and weight gain or loss
Lamictal is an anticonvulsant that can be used to treat seizures such as epilepsy. It is also used as a mood stabilizer for bipolar disorder.
In the first clinical trials with the drug, 5 percent of adults with epilepsy lost weight while taking Lamictal, while 1 to 5 percent of patients with bipolar I disorder gained weight while taking the drug. The researchers do not disclose how much weight patients have gained or lost.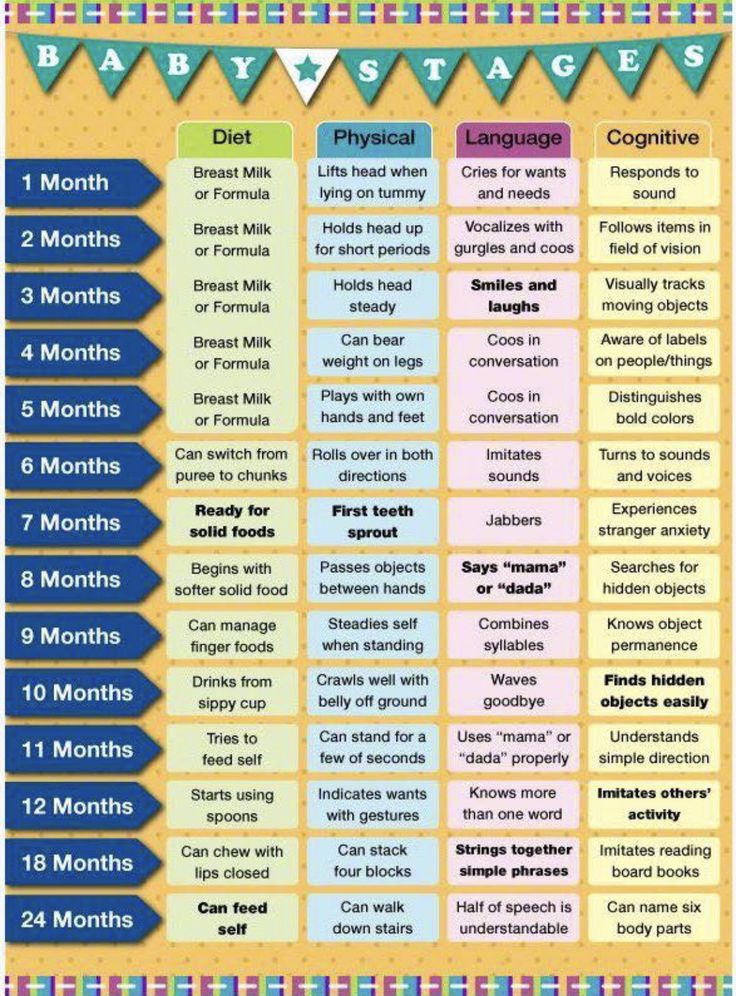 nine0008 Meanwhile, a 2006 study comparing the effects on weight of Lamictal, lithium, and placebo found that some Lamictal-treated patients gained weight, some lost weight, and most remained about the same weight. Weight changes are usually not many pounds anyway. Obese patients taking Lamictal lost an average of four pounds, while the weight of non-obese patients remained virtually unchanged.
nine0008 Meanwhile, a 2006 study comparing the effects on weight of Lamictal, lithium, and placebo found that some Lamictal-treated patients gained weight, some lost weight, and most remained about the same weight. Weight changes are usually not many pounds anyway. Obese patients taking Lamictal lost an average of four pounds, while the weight of non-obese patients remained virtually unchanged.
Relationship between weight gain and other bipolar drugs
Weight gain from medications used to treat bipolar disorder is unfortunately quite common. Some mood stabilizers commonly used for bipolar disorder, especially lithium and Depakote (valproate), carry a high risk of weight gain.
In addition, the atypical antipsychotics Clozaril (clozapine) and Zyprexa (olanzapine) tend to cause significant weight gain in people who take them. Finally, some antidepressants, notably Paxil (paroxetine) and Remeron (mirtazapine), have been associated with weight gain. nine0008 Therefore, if you are already overweight, you and your psychiatrist may want to consider additional weight gain when determining your bipolar medication regimen. Based on this, Lamictal may be a good choice.
Based on this, Lamictal may be a good choice.
Lamictal as a possible treatment for obesity
Lamictal has also been studied as a possible treatment for obesity in people without epilepsy or bipolar disorder.
In a small clinical study of 40 people conducted in 2006, researchers randomly assigned participants to receive either lamictal or placebo for up to 26 weeks. Each participant in the study had a body mass index (BMI) between 30 and 40, placing them in the obese group to the level of severe obesity. Those who took Lamictal lost an average of just over 10 pounds. Those who took the placebo lost about 7 pounds in the meantime, so while those who took Lamictal lost more weight, they didn't lose all that much more. nine0008 Another study in 2009 looked at Lamictal as a remedy for overeating. This study involved 51 people with the condition that 26 of them received Lamictal, and 25 - placebo.
Those who took Lamictal lost more weight than those who took placebo (about 2. 5 pounds vs. about one third of a pound) and did have significant improvements in blood sugar and cholesterol lab test results. However, Lamictal did not appear to affect other aspects of the eating disorder when compared to placebo. nine0003
5 pounds vs. about one third of a pound) and did have significant improvements in blood sugar and cholesterol lab test results. However, Lamictal did not appear to affect other aspects of the eating disorder when compared to placebo. nine0003
Tags
LamictalworryYou don't need weight about Why increase
how to choose the right one and which milk formula is best for the baby?
WHO recommends that mothers exclusively breastfeed their babies until the age of six months. Despite the obvious health benefits of breast milk, many of them, for various reasons, cannot get it or do not get it enough. And then the mother has to study all the information about the features of infant formula, their composition and differences from each other. nine0034
Infant formula has been developed and improved over the years to be like breast milk. We will find out what kind of infant formula is available and how to choose an infant formula.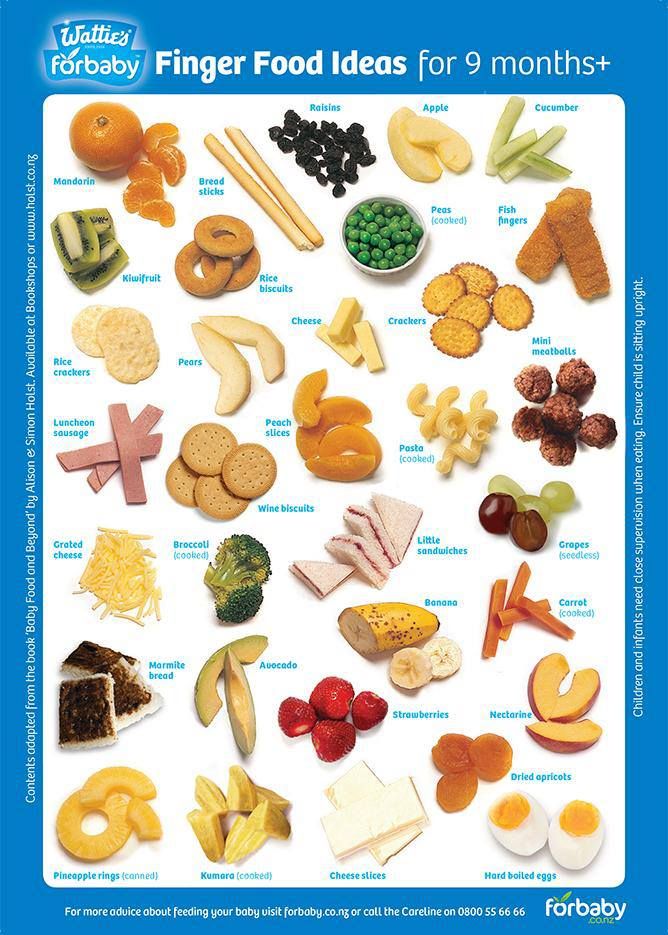
The national program provides for the possibility of mixed and artificial feeding with adapted milk mixtures. They are made from animal milk, which is modified in such a way that the components of the mixture, as a result, repeat the composition and properties of breast milk and correspond to the physiological needs of children in infancy and early childhood[1]. nine0003
Types of infant milk formulas:
- standard or basic;
- therapeutic and prophylactic;
- medical.
Which infant formula is best? The answer depends primarily on the state of health of a particular child. It is important to remember that some children are not suitable for regular formulas, they need to eat formulas of specialized formulas: they are introduced to eliminate the symptoms of lactose intolerance, treat allergies to cow's milk proteins, reduce or stop spitting up, get rid of constipation and other problems. nine0003
All mixtures are given as prescribed by a physician.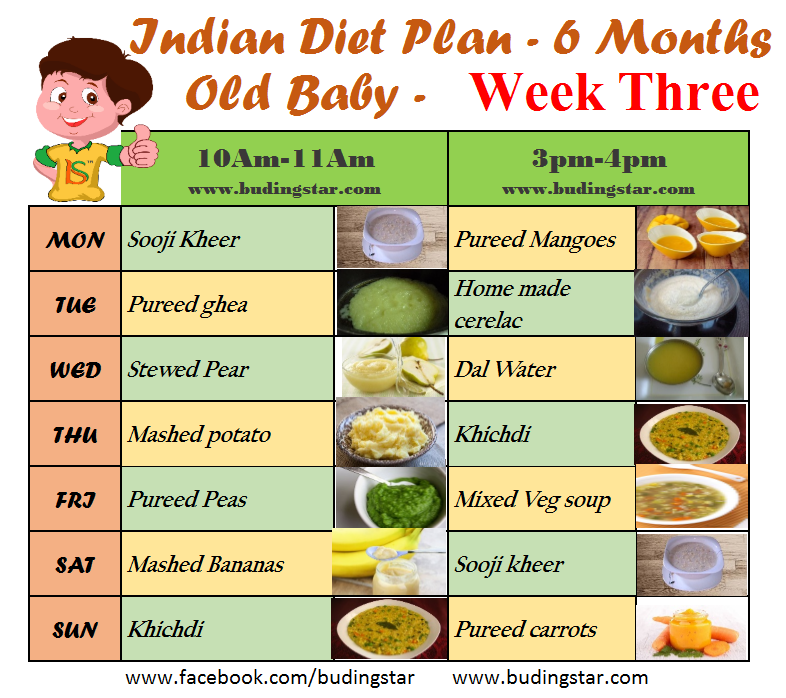 Despite this, parents should themselves understand the composition and features of artificial nutrition in order to clearly know which set of components the baby needs and better understand the recommendations of a specialist.
Despite this, parents should themselves understand the composition and features of artificial nutrition in order to clearly know which set of components the baby needs and better understand the recommendations of a specialist.
This is important
The first rule when choosing infant formula is to work with your pediatrician to find out what your baby needs and find out if the formula is right for him. The best infant formula is the one on which the baby gains weight normally and also feels good during and after feeding. nine0034
Types of infant formulas by age
Formulas are selected not only according to their purpose, but also according to age. According to the numbers indicated on the jars (packs), which are called stages, you can determine the stage of feeding:
- 1st stage (initial, or starting, mixtures) - from 0 to 6 months;
- 2nd stage (subsequent mixtures) - from six months to 12 months;
- Stage 3 (milk drinks) - from one to three years.
It is worth noting that this is not the only possible classification. For example, among milk formulas there are universal "from 0 to 12 months", designed to feed a child throughout the first year of his life, and mixtures labeled "PRE" for premature babies. nine0003
Age-appropriate formulas are formulated to meet the nutritional needs of newborns, infants and toddlers and their ability to digest and absorb food. Mixtures vary greatly in the amount of proteins, fats, carbohydrates and minerals. And the transition to the mixture of the next step should be timely, because a lack of nutrients or, conversely, an “overload” with them can lead to health problems for the baby.
This is important
The second rule in choosing a formula is to focus on a specific age group: you can not give formula 2 formula until six months or a year and a half, you cannot replace formula with regular milk. After a year, you should also not rush to introduce whole milk: it has few vitamins, minerals, but a lot of protein and fat, and this can cause digestive disorders. From formula 3 formula, a one-year-old baby will receive a significant portion of the daily requirement of nutrients in a form suitable for his small tummy. nine0034
From formula 3 formula, a one-year-old baby will receive a significant portion of the daily requirement of nutrients in a form suitable for his small tummy. nine0034
Types of infant formula in the form
There are two types: liquid and dry. Ready-made infant formulas in liquid form are not widely used in Russia. Powdered infant formula is the most popular. Not only are they economical, their free-flowing texture allows you to measure the exact amount of powder your child needs according to their age. This is a convenient option for both supplementary feeding and full artificial feeding. You just need to follow the recommendations of the doctor regarding the volume of servings, and the manufacturer's instructions for diluting the mixture in water. If you add powder in excess of the norm or, conversely, less, this will lead to a change in the concentration of nutrients, which can even be harmful to the health of the baby. nine0003
What is contained in infant formula and how they differ in composition
As a rule, infant formula contains four groups of components: protein, carbohydrate, fat, vitamin and mineral.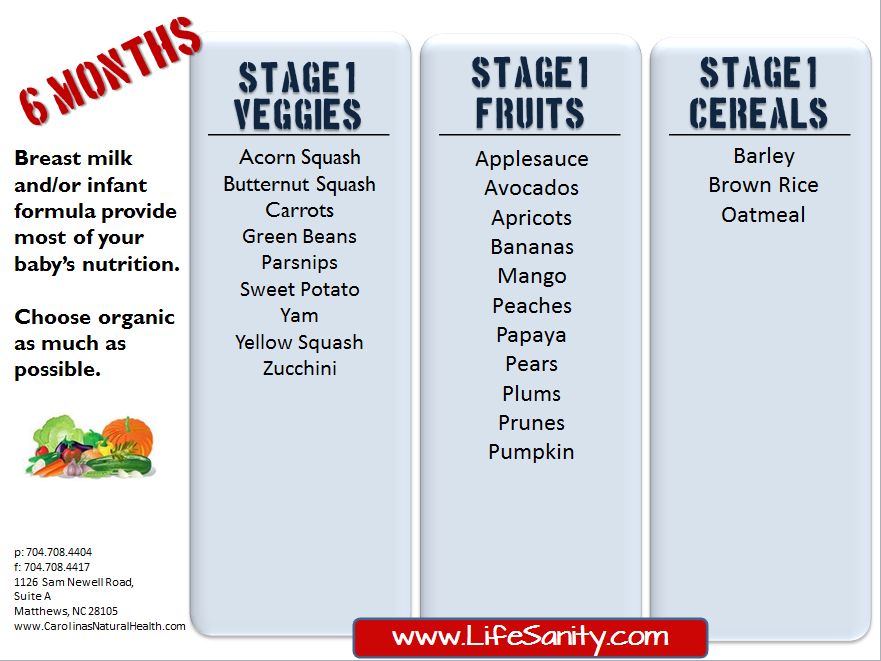 What then distinguishes one product from another? They differ in the degree of similarity of the composition with breast milk and in the number of basic and the presence of additional functional components that have a beneficial effect on child development.
What then distinguishes one product from another? They differ in the degree of similarity of the composition with breast milk and in the number of basic and the presence of additional functional components that have a beneficial effect on child development.
Proteins. Mature breast milk contains about 60% whey protein and 40% casein [2] . In many initial formulas, similar proportions - so the protein is easier to digest. Whey protein in the stomach forms a soft clot that resembles cottage cheese in texture. It is faster and easier to ferment and digest than casein, which takes much longer to digest. In subsequent mixtures, the ratio of proteins of the whey fraction to the casein fraction of 50:50 will be optimal.
Notes
For better digestion of milk protein, demineralized whey is added to some mixtures. This increases the amount of whey protein and the quality of the protein component. And at the same time, thanks to this, the growth of all body tissues, good weight and healthy kidneys of the baby are ensured. nine0034
nine0034
Fats serve as an energy reserve for the whole organism. Breast milk fats consist of saturated and unsaturated fatty acids, including linoleic and α-linolenic acids - they should be a mandatory component of dry infant formula. Docosahexaenoic acid (DHA) and arachidonic acid (ARA), which are found in breast milk, are used to further fortify formulas. They are important for the development of mental and visual functions.
To form the fat component of the mixture, vegetable oils are mainly used: sunflower, palm, coconut, soybean, corn and other raw materials. nine0003
Interesting
In modern baby food production there is a tendency to use milk lipids instead of palm oil in formulas as a source of useful essential fatty acids, including the “correct” palmitic acid. Such a fatty composition makes the stool softer in artificial children.
Carbohydrates. Most formulas contain lactose (milk sugar, the main source of carbohydrates in breast milk) as the carbohydrate component, which aids in the absorption of macronutrients. There is also a combination of lactose and maltodextrin (it contains a smaller proportion), due to which the baby gets a longer feeling of fullness after consuming the mixture. Also important is the presence in mixtures of prebiotic oligosaccharides (POS) characteristic of mother's milk: together with bifidobacteria, they help resist the growth of harmful bacteria and stimulate the intestines and immune system of a formula-fed baby. nine0003
There is also a combination of lactose and maltodextrin (it contains a smaller proportion), due to which the baby gets a longer feeling of fullness after consuming the mixture. Also important is the presence in mixtures of prebiotic oligosaccharides (POS) characteristic of mother's milk: together with bifidobacteria, they help resist the growth of harmful bacteria and stimulate the intestines and immune system of a formula-fed baby. nine0003
Vitamins and minerals are contained in a certain concentration and ratio. However, due to the reduced digestibility of vitamins from the mixture, they are added to the formula in larger quantities when compared with mother's milk [3].
In infancy and early life, it is especially important that children receive adequate amounts of vitamin D (prevention of rickets), iron (reduces anemia), calcium (strengthens bones and teeth), iodine (involved in intellectual development) and B vitamins (immunity support factor and protection against neurological disorders, sleep disorders, tremors). nine0003
nine0003
Permissible levels of all nutrients in infant formula are regulated by the Technical Regulations of the Customs Union "On the Safety of Milk and Dairy Products" (TR CU 033/2013)[4].
This is important
The third rule in choosing a mixture is to thoroughly study the composition. In addition to essential nutrients, some formulas are fortified with functional ingredients that enhance their quality and benefits, including improving digestion and immunity, developing cognitive functions and developing vision in newborns and infants. nine0034
Cow vs goat milk
As for the basis for milk formula, cow milk is more often used than goat milk. Despite the apparent simplicity of choosing the type of milk, its good tolerance is of great importance. This means clear skin without rashes and redness, no colic, no profuse regurgitation and mucus in the stool, as well as excellent appetite and weight gain in the child.
For information
Some children have a poor digestive system for milk protein, but they still accept goat's milk well.