Babies with reflux foods to avoid
Acid Reflux in Infants: Causes
Immature lower esophageal sphincter
The lower esophageal sphincter (LES) is a ring of muscle at the bottom of baby’s esophagus that opens to allow food into the stomach and closes to keep it there.
This muscle may not be fully matured in your baby, especially if they’re premature. When the LES opens, the contents of the stomach can flow back into the esophagus, causing baby to spit up or vomit. As you can imagine, it can cause discomfort.
This is very common and does not usually cause other symptoms. However, constant regurgitation from acid reflux can sometimes cause damage to the esophageal lining. This is much less common.
If spitting up is accompanied by other symptoms, it may then be called gastroesophageal reflux disease, or GERD.
Short or narrow esophagus
Refluxed stomach contents have a shorter distance to travel if the esophagus is shorter than normal. And if the esophagus is narrower than normal, the lining might more easily become irritated.
Diet
Changing the foods baby eats may help reduce the chances of acid reflux. And if you breastfeed, making changes to your diet might help your baby.
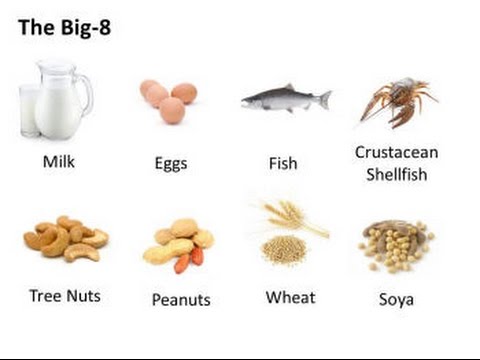
Some studies have shown that reducing intake of milk and eggs may help, though more research is needed to determine how much this affects the condition.
Certain foods may be causing acid reflux, depending on your infant’s age. For example, citrus fruits and tomato products increase acid production in the stomach.
Foods like chocolate, peppermint, and high fat foods can keep the LES open longer, causing the contents of the stomach to reflux.
Gastroparesis (delayed emptying of the stomach)
Gastroparesis is a disorder that causes the stomach to take longer to empty.
The stomach normally contracts to move food down into the small intestine for digestion. However, stomach muscles don’t work properly if there is damage to the vagus nerve because this nerve controls the movement of food from the stomach through the digestive tract.
In gastroparesis, the stomach contents remain in the stomach longer than they’re supposed to, encouraging reflux. It’s rare in healthy infants.
Hiatal hernia
A hiatal hernia is a condition in which part of the stomach sticks through an opening in the diaphragm. A small hiatal hernia doesn’t cause problems, but a larger one can cause acid reflux and heartburn.
Hiatal hernias are very common, especially in people over the age of 50, but they are rare in infants. However, the causes are unknown.
A hiatal hernia in children is usually congenital (present at birth) and may cause gastric acid to reflux from the stomach into the esophagus.
Position while feeding
Positioning — especially during and after feeding — is a frequently overlooked cause of acid reflux in infants.
A horizontal position makes it easier for the stomach contents to reflux into the esophagus. Simply keeping baby in an upright position while you’re feeding them and for 20 to 30 minutes afterward may reduce acid reflux.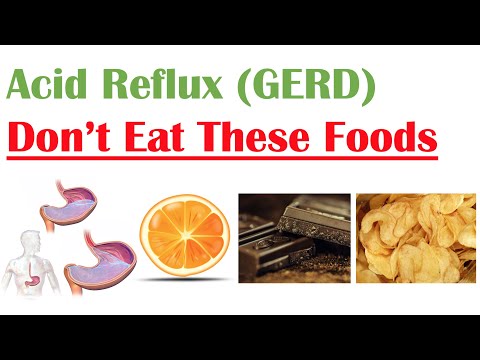
Sleep positioners and wedges, however, are not recommended while feeding or sleeping. These padded risers are intended to keep your baby’s head and body in one position, but are not recommended by the Food and Drug Administration due to the risk of sudden infant death syndrome (SIDS)
Angle of His
The angle at which the base of the esophagus joins the stomach is known as the “angle of His.” Differences in this angle may contribute to acid reflux.
This angle most likely affects the ability of the LES to keep the contents of the stomach from refluxing. If the angle is too sharp or too steep, it may make it difficult to keep the stomach contents down.
Overfeeding
Feeding your little one too much at once can cause acid reflux. Feeding your infant too frequently can also cause acid reflux. It’s more common for bottle-fed babies to overfeed than breastfed infants.
An oversupply of food can put too much pressure on the LES, which will cause your infant to spit up.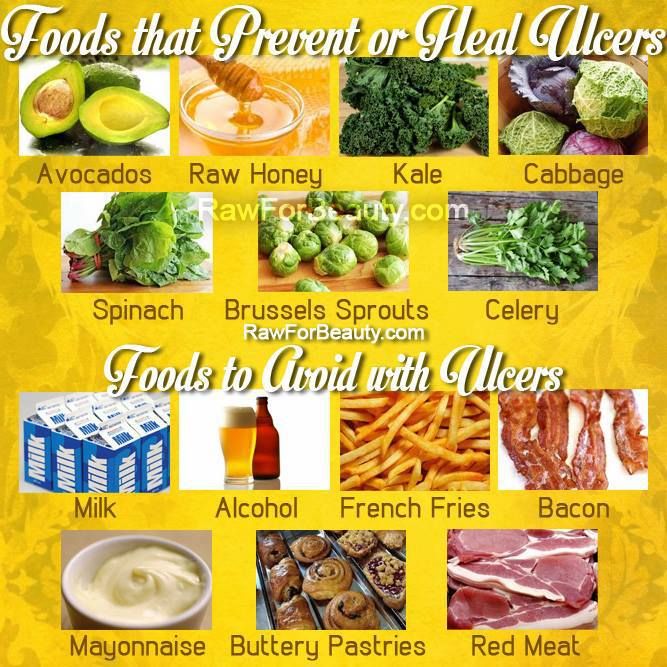 That unnecessary pressure is taken off the LES and reflux decreases when you feed baby less food more often.
That unnecessary pressure is taken off the LES and reflux decreases when you feed baby less food more often.
However, if your baby spits up often, but is otherwise happy and growing well, you may not need to change your feeding routine at all. Talk with your doctor if you have concerns that you are overfeeding your baby.
Your infant will usually grow out of acid reflux. However, call your child’s doctor immediately if you notice that your child:
- isn’t gaining weight
- has feeding difficulties
- is projectile vomiting
- has blood in their stool
- has pain signs such as arching of the back
- has unusual irritability
- has trouble sleeping
While it isn’t easy to determine the exact cause of acid reflux in infants, lifestyle and diet changes may help eliminate some of the factors.
If the acid reflux doesn’t go away with these changes and your baby has other symptoms, a doctor may want to perform tests to rule out a gastrointestinal disorder or other problems with the esophagus.
A Guide to Foods to Avoid for Acid Reflux While Breastfeeding
"The content below is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition."
Your baby is dealing with acid reflux after breastfeeding and will not stop crying.
Don’t worry, you can help avoid acid reflux episodes like these in the future.
The main way to prevent acid reflux while breastfeeding is to avoid consuming foods that can cause acid reflux.
But what foods cause acid reflux in babies?
In this guide, we will break down all the foods to avoid for acid reflux while breastfeeding and show you how your nutrition can not only prevent acid reflux attacks but benefit your baby’s health even more.
Table of Contents
- How Can a Mother’s Diet Affect a Breastfed Baby?
- What Are Common Signs of Acid Reflux in Breastfed Babies?
- 7 Foods to Avoid When Breastfeeding a Baby With Reflux
- How Can I Soothe Acid Reflux in a Breastfed Baby? 2 Methods to Consider
- Start Treating Your Baby’s Acid Reflux With Holistic Nutrition Today
How Can a Mother’s Diet Affect a Breastfed Baby?
The female body does some miraculous things, and breastfeeding is no exception.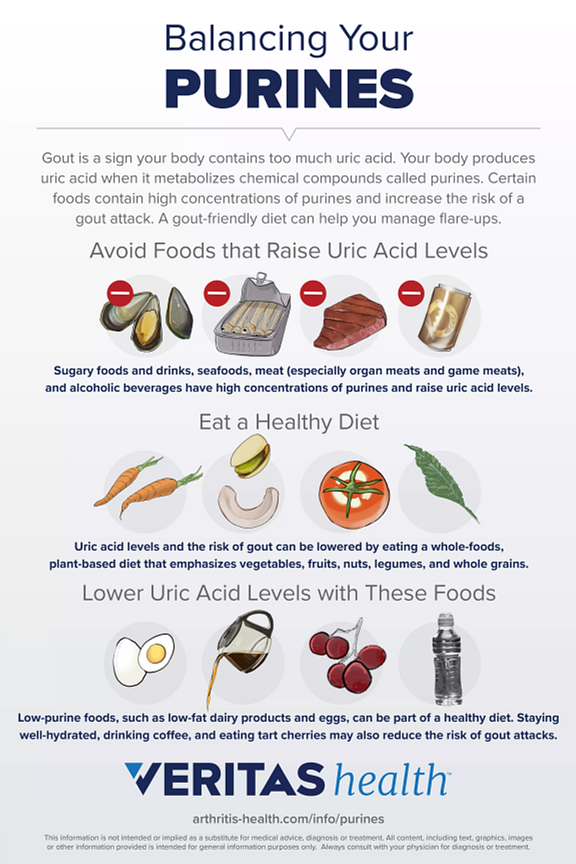
A mother’s diet is directly related to the diet of their breastfeeding baby, as what you eat can impact the nutrition, composition, and even taste of your breast milk.
You may be wondering, how long does it take for ingested foods to influence your breast milk?
The answer? It varies depending on the type of food you ingest.
Let’s take a look at some examples of time it takes for certain foods to influence your breast milk:
- Coffee: 15-60 minutes
- Garlic: 2 hours
- Carrots: 2-3 hours
- Mint 4-6 hours
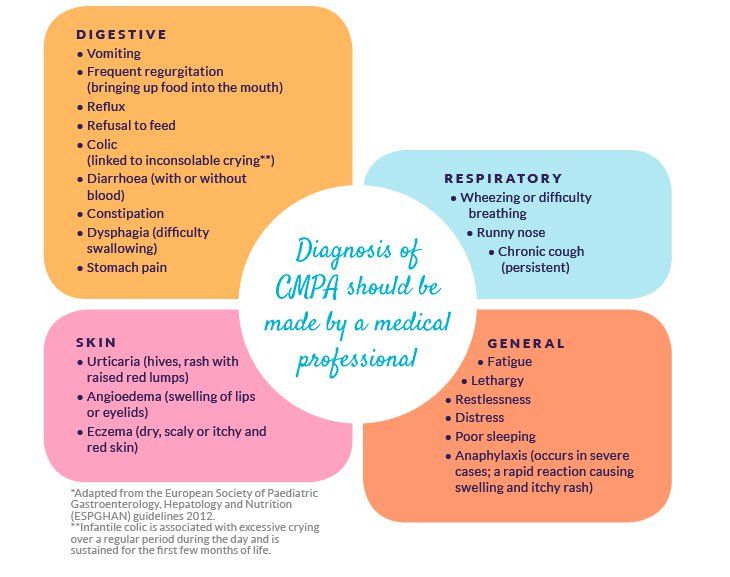
Some foods that influence your breast milk can affect your baby in different ways. For example, it’s possible for your child to have a food allergy in response to something you ate.
One of the most common reactions linked to a mother’s diet and breastfeeding is acid reflux .
What Are Common Signs of Acid Reflux in Breastfed Babies?
You probably already know that it’s common and normal for infants to spit up after a meal. You’ve cleaned it up dozens of times, likely.
You’ve cleaned it up dozens of times, likely.
This little phenomenon is known as gastroesophageal reflux (GER).
However, frequent vomiting, irritation, and a slew of other symptoms can hint to a more serious problem, known as gastroesophageal reflux disease (GERD), commonly known as acid reflux.
Common acid reflux symptoms to look out for include:
- Frequent vomiting and regurgitation
- Persistent coughing or wheezing
- Difficulty eating
- Irritability associated with feeding or following feedings
- Gassiness
7 Foods to Avoid When Breastfeeding a Baby With Reflux
It can seem overwhelming trying to figure out which foods to avoid when breastfeeding a baby with reflux, especially when you have an already fussy baby.
Below, we will discuss what foods cause reflux in breastfed babies. A good rule of thumb is that if certain foods cause acid reflux for you, they could also cause acid reflux for your baby.
#1: Fruit and Fruit Juice
Fruit and fruit juices with high acidity can trigger acid reflux in infants, causing discomfort.
Some acidic fruit and fruit juices you’ll want to avoid consuming are:
- Apples
- Oranges
- Lemons
- Other citrus fruits
#2: Tomatoes and Tomato Sauce
You may be surprised to hear that tomatoes and tomato-based sauces are included in this list of foods to avoid for acid reflux while breastfeeding.
While tomatoes can be an excellent source of vitamin C, which is an essential nutrient for healthy breastfeeding, they are also very acidic—
which can lead to a very gassy, uncomfortable, and irritable baby.
#3: Spicy Foods
Have you ever eaten a spicy meal only to get a dose of heartburn afterward? The same can happen to your baby when you breastfeed after eating spicy food.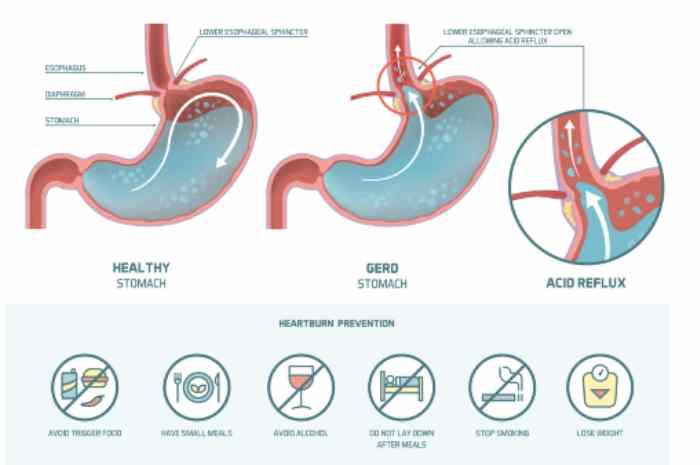
Spicy foods can irritate the lining of the stomach, which can trigger acid reflux.
#4: Caffeine
While your daily cup of coffee isn’t enough to cause problems for your infant, experts advise breastfeeding mothers to not consume more than 750mL of caffeine per day (the equivalent of 5 cups of coffee).
If your infant takes in too much caffeine from your breast milk, they can experience acid reflux as well as other caffeine stimulation symptoms, such as irritability.
#5: Foods High in Fat
It is best to only consume foods with high fat content in moderation while breastfeeding.
Breastfeeding your baby after consuming foods high in fat can cause the lower esophageal sphincter (LES) to stay open longer, which causes the contents of the stomach to reflux.
#6: Seafood with High Mercury Levels
While seafood can be a great source of protein and omega-3 fatty acids that are wonderful building blocks for proper nutrition, some seafood can do more harm than good.
Avoid consuming seafood that is high in mercury. The mercury from these foods can find its way into your breast milk supply. Excessive amounts of mercury in breast milk can have adverse effects on your baby’s developing nervous system.
Some kinds of seafood that are high in mercury include:
- Swordfish
- King mackerel
- Tilefish
#7: Alcohol
No level of alcohol in breastmilk is considered safe for your child to consume.
However, this doesn’t mean that you can’t enjoy a glass of wine every once in a while.
When it comes to breastfeeding and consuming alcohol, you have two options to ensure your child’s safety:
- Pump before consuming alcohol. If you plan on enjoying an alcoholic beverage, you can pump breast milk before drinking alcohol so you have a clean supply to feed your baby later.
- Wait it out.
 If you drink alcohol, wait for it to completely clear your breast milk before breastfeeding. Depending on your body weight, you’ll want to wait at least 2-3 hours after consuming:
If you drink alcohol, wait for it to completely clear your breast milk before breastfeeding. Depending on your body weight, you’ll want to wait at least 2-3 hours after consuming:
- 12 oz. of 5% beer
- 5 oz. of 11% wine
- 1.5 oz. of 40% liquor
How Can I Soothe Acid Reflux in a Breastfed Baby? 2 Methods to Consider
Neither your heart nor sanity can put up with your baby crying in discomfort for hours due to acid reflux, but it can be difficult to know exactly how to help soothe acid reflux in a breastfed baby or avoid it altogether for that matter.
After all, motherhood doesn’t come with an instruction manual.
There are two ways you can handle acid reflux in babies:
- Treat the symptoms of acid reflux to soothe your baby’s discomfort.
- Treat the root of the cause and avoid acid reflux altogether
#1: Help Baby’s Physical Discomfort
There are a number of ways that you can decrease your baby’s discomfort caused by acid reflux.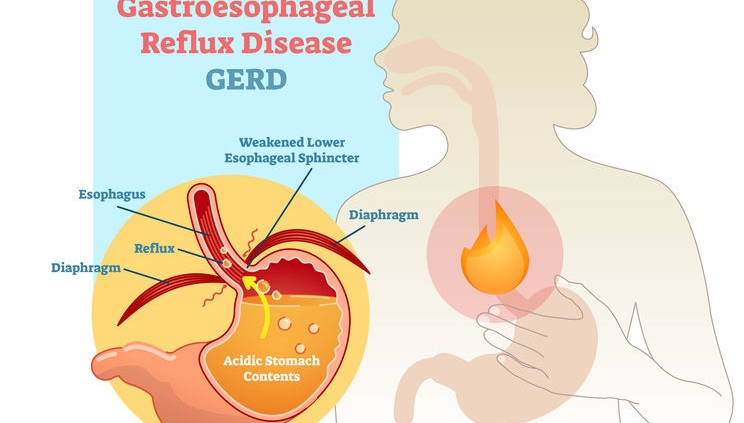
If your baby is dealing with acid reflux, you can try to treat their symptoms by:
- Doing smaller, more frequent feeds
- Feeding your baby upright
- Thickening breast milk
- Burping your baby more frequently
Try Smaller, More Frequent Feedings
When your baby’s stomach is too full, they are at greater risk of having acid reflux after feedings.
Feeding your baby more frequently in small amounts can help avoid irritating acid reflux symptoms.
This is because a less-full stomach decreases the amount of pressure put on the lower esophageal sphincter, which is a muscle that prevents food from going back into the esophagus from the stomach.
The lower esophageal sphincter takes about a year to strengthen,
which is why babies spit up often.
Feed Your Baby Upright
Feeding your baby in an upright position can help reduce the risk of acid reflux in babies.
Additionally, keeping your baby upright for at least 30 minutes after feeding is also believed to have the same acid reflux prevention effect.
Thicken Breast Milk
With your doctor’s approval, you can thicken your breast milk by adding a small amount of infant rice cereal. Thickening the breast milk can help lessen spit-ups and acid reflux symptoms.
Thickening your breast milk may help reduce the risk of your baby’s stomach contents sloshing up into the esophagus. Always consult your doctor before trying this alternative.
Burp Your Baby More Frequently
It’s important to burp your baby often—both during and after feedings.
Frequently burping your baby can help reduce acid reflux symptoms. Anytime your baby pulls off the nipple during breastfeeding, be sure to give them a little burp.
#2: Acid Reflux in Babies: Mother’s Diet Can Help with Holistic Nutrition
Now that we have discussed how to treat acid reflux symptoms , let’s talk about a better option— preventing acid reflux episodes before they happen.
Holistic nutrition is an excellent tool to help avoid acid reflux in infants caused by breastfeeding.
You may be wondering, “what is holistic nutrition and how is it related to foods to avoid for acid reflux while breastfeeding?”.
Holistic nutrition is based on the idea that your nutrition is related to all aspects of your health.
Holistic nutrition is a lifestyle that involves eating healthy foods that are:
- Whole
- Un-refined
- Un-processed
- Organic
- Locally grown
Let’s talk about how holistic nutrition benefits both the breastfeeding mother and child.
How Does Holistic Nutrition Benefit the Breastfeeding Mother and Baby?
Holistic nutrition focuses on providing your body with nutrient-dense foods that will only have a positive impact on your health.
If your diet is not having a positive impact on your health, chances are that it is not positively impacting the health of your breastfed baby either.:max_bytes(150000):strip_icc()/what-can-i-eat-if-i-have-a-peptic-ulcer-1742154-01-ec37a34d14c44195999f8d44372f820b.png?resize=1060%2C707&ssl=1)
Think about it: if certain foods give you acid reflux, why wouldn’t your baby be susceptible to the same kind of reaction by consuming that food composition through your breast milk?
Holistic nutrition involves eliminating refined and processed foods, which are known to cause acid reflux.
By not consuming these foods or strictly limiting the consumption, you are stopping the problem at the source instead of simply treating symptoms.
However, healthy and whole foods can also be culprits of acid reflux attacks.
If your breastfeeding child is experiencing acid reflux and you are unable to pinpoint what food is causing it, using the elimination diet can help uncover which foods are resulting in episodes of acid reflux in your child.
Start Treating Your Baby’s Acid Reflux With Holistic Nutrition Today
Holistic nutrition goes beyond simply what foods to avoid for acid reflux while breastfeeding.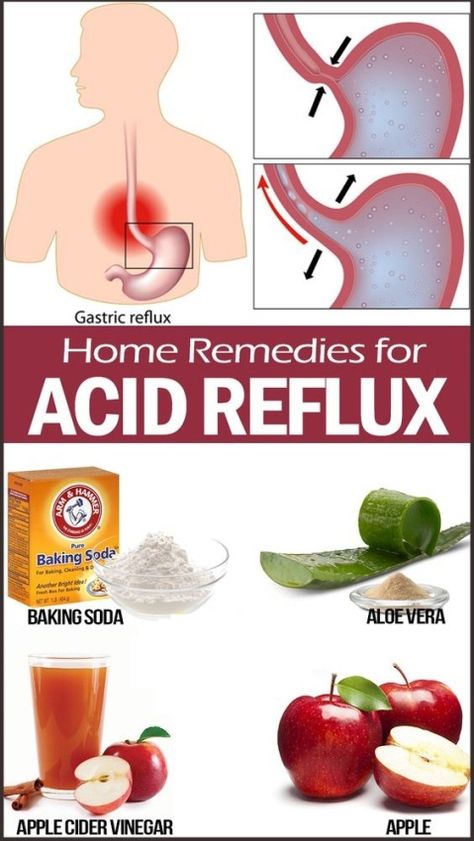
Not only does holistic nutrition help avoid acid reflux episodes for you and your breastfeeding child, but it provides both of you with the best nutrition possible for optimal health.
Learn more about how holistic nutrition can benefit you and your child today by scheduling a free consultation.
Proper nutrition for GERD - Clinic on Leninsky
The key to solving many problems with the gastrointestinal tract is proper nutrition. Gastroenterologist at the Clinic on Leninsky Katerina Chesskaya tells what you can and should eat for those who suffer from reflux disease.
What is GERD?
Gastroesophageal reflux disease (GERD) is a chronic relapsing disease in which there is a spontaneous, regularly repeated reflux of stomach contents into the esophagus. As a result, the lower esophagus is affected. The reflux of stomach contents into the esophagus is considered normal if it occurs occasionally and is not accompanied by negative factors.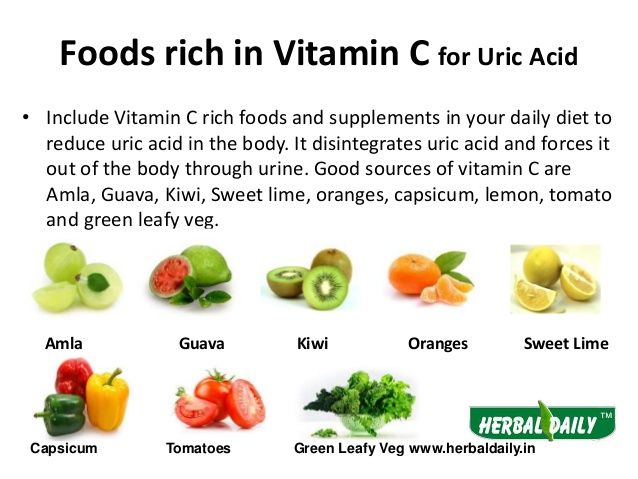 The disease is evidenced by the frequent recurrence of casting and inflammatory processes of the gastrointestinal tract.
The disease is evidenced by the frequent recurrence of casting and inflammatory processes of the gastrointestinal tract.
GERD is usually manifested by belching and heartburn after eating or bending forward, and also at night. Another indication of the presence of GERD is pain behind the sternum, extending to the interscapular region, lower jaw, and the left half of the chest. There are also signs of GERD that are not directly related to the esophagus - a cough, shortness of breath, often occurring when lying down, hoarseness, dry throat, rapid satiety, and bloating. The cause of chronic inflammatory diseases of the nasopharynx (pharyngitis, laryngitis, sinusitis, tonsillitis) in 30% of cases is GERD. It has been proven that against the background of GERD there is a risk of developing obstructive pulmonary diseases, including bronchial asthma.
Proper nutrition for GERD
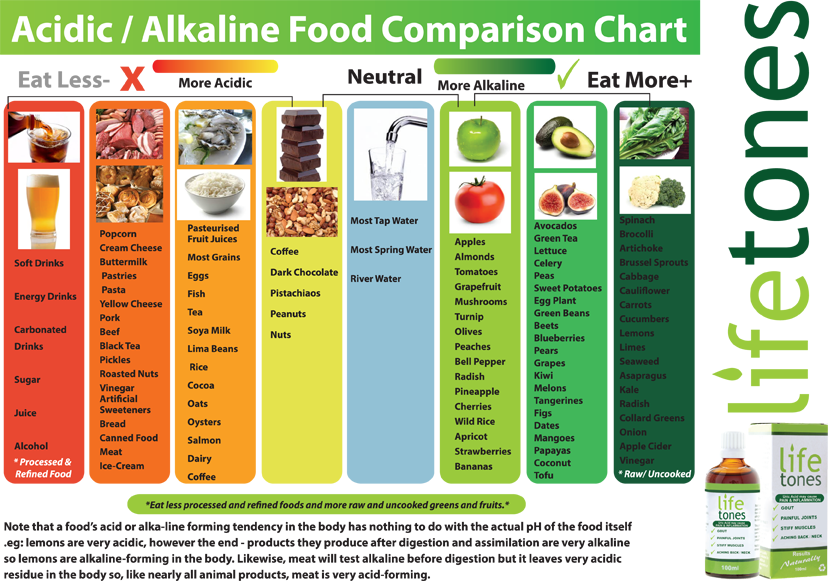
As in the case of many other diseases of the gastrointestinal tract, the main principle of the treatment of GERD is proper nutrition. There are foods that relax the lower esophageal sphincter, which leads to the reflux of acidic stomach contents into the esophagus, that is, reflux. These include; strong tea, coffee, chocolate, citrus fruits, tomatoes, bitters (garlic, onion), fresh mint. As well as fatty varieties of fish, meat and products that cause gas formation: muffins, hot pastries, legumes, brown bread, cakes, pastries, grapes, cucumbers, carbonated drinks. Alcohol and smoking also reduce the tone of the lower esophageal sphincter.
There are foods that relax the lower esophageal sphincter, which leads to the reflux of acidic stomach contents into the esophagus, that is, reflux. These include; strong tea, coffee, chocolate, citrus fruits, tomatoes, bitters (garlic, onion), fresh mint. As well as fatty varieties of fish, meat and products that cause gas formation: muffins, hot pastries, legumes, brown bread, cakes, pastries, grapes, cucumbers, carbonated drinks. Alcohol and smoking also reduce the tone of the lower esophageal sphincter.
Here is a list of foods to consider when planning your menu for the day.
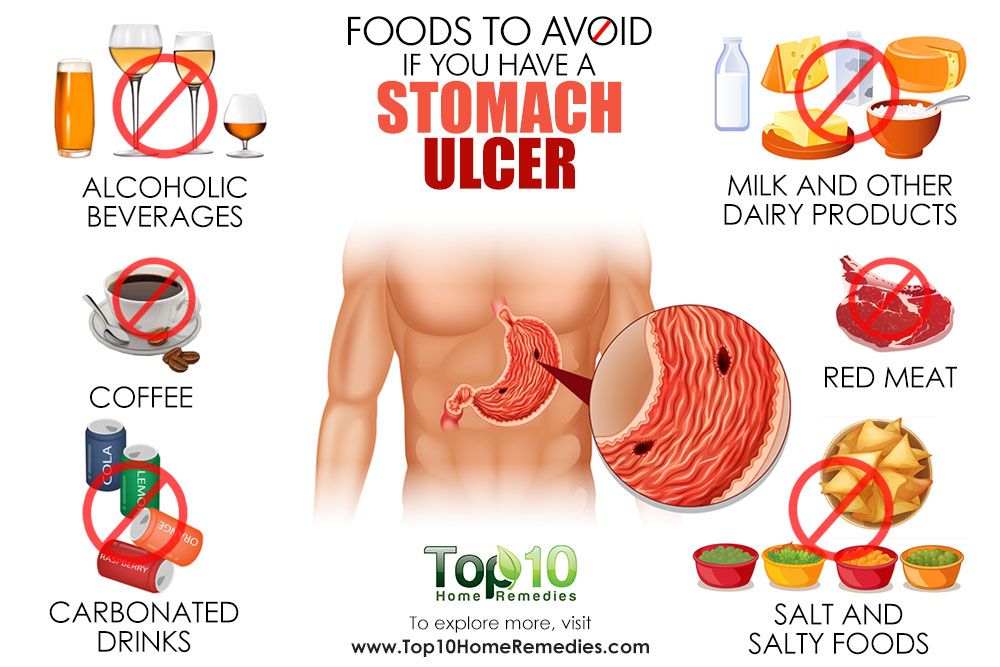
Delete:
1. Bread: fresh rye bread, tarts and pancakes.
2. Meat: stewed and fried meat dishes from fatty meat, poultry.
3. Fish: fatty fish, fried, smoked, salty dishes.
4. Vegetables: white cabbage, turnip, rutabaga, radish, sorrel, spinach, onion, cucumbers, salted, pickled and pickled vegetables, mushrooms.
5. Fruit: Raw, sour, unripe fruit, dried fruit puree.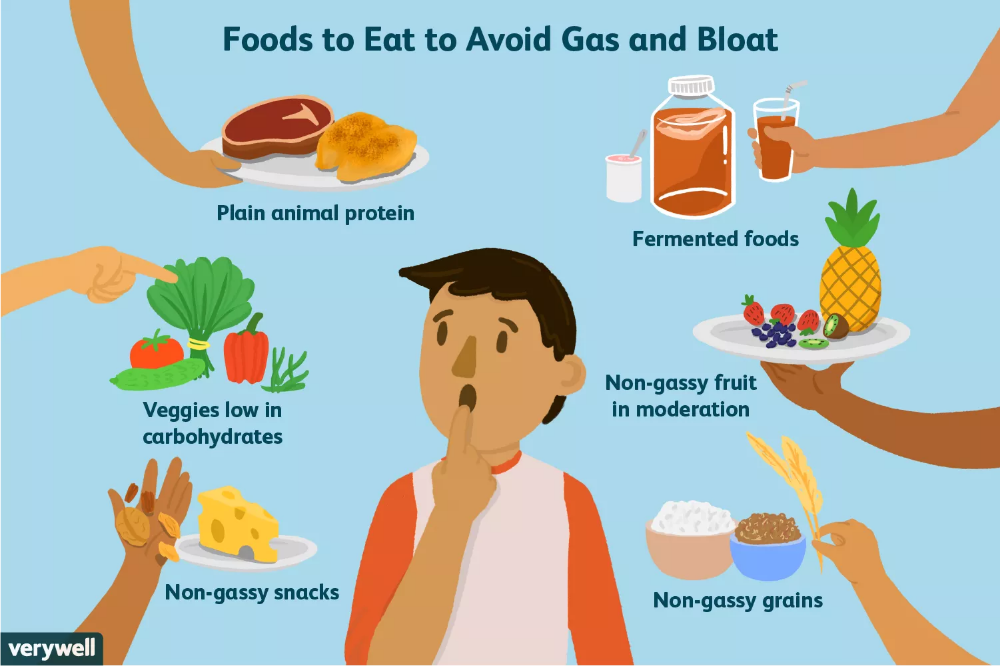
6. Cereals: millet, pearl barley, barley and corn grits, legumes.
7. High acidity dairy products, spicy and salty cheeses.
8. Sweet: halva, chocolate, ice cream, cakes.
9. Drinks: sour, carbonated, fruit drinks, strong tea, coffee and alcohol.
Recommended:
1. Bread: from wheat flour of the first or highest grade, yesterday, dry, uncomfortable baking.
2. Meat: Beef, veal, chicken, rabbit, turkey, all in the form of cutlets, meatballs, soufflés, mashed potatoes and quenelles.
3. Fish: boiled river fish - zander, pike, perch, any low-fat varieties.
4. Vegetables: carrots, cauliflower, potatoes, beets, squash and squash.
5. Fruits: Sweet berries, ripe fruits. Preferably mashed or baked.
6. Cereals: oatmeal, semolina, buckwheat (mashed), rice porridge, on the water with the addition of milk, boiled vermicelli.
7. Dairy products: milk, lean cheese and low-fat sour cream. Cottage cheese dishes made from pureed cottage cheese, for example, cheesecakes, casseroles.
8. Sweet: jam, marshmallows, honey, marshmallow, cream and milk puddings.
9. Drinks: weak tea or cocoa with milk, sweet juices and decoctions.
It is also important to adhere to the diet:
— Fractional meals in small amounts and often up to 5-6 times a day.
- Do not lie down immediately after eating, the last meal is 2-3 hours before bedtime.
- Do not work in a slope, exclude the "gardener" pose.
- Do not wear tight belts and limit abdominal exercise.
- Obese people need to normalize body weight.
Remember that only a gastroenterologist can make a diagnosis of GERD (however, like any disease), to accurately determine the patient's condition. At the appointment, the doctor, together with the patient, will find the cause of the disease, outline a treatment plan and further supportive therapy in order to avoid relapses.
At the Clinic on Leninsky, an appointment is being made:
- pediatric gastroenterologist Natalya Medvedeva;
- gastroenterologist Ekaterina Chesskaya.
You can make an appointment with a gastroenterologist at the Clinic on Leninsky
by calling +7 (495) 668-09-86 .
Moscow, Leninsky prospect, building 67, building 2
Tel. .-Fri. 7:30–20:00 Sat-Sun 9:00–18:00
Treatment and prevention of gastroesophageal reflux disease
Treatment and prevention of gastroesophageal reflux disease (GERD)
Gastroesophageal reflux disease (GERD) common, but rarely detected and therefore untreated since GERD usually responds well to treatment.
GERD is treated gradually. The doctor will help you choose the right course of treatment. If the disease is mild, it will be enough for the patient to follow a certain diet, give up certain activities, and sometimes take over-the-counter medications.
In cases where the symptoms are more persistent (daily heartburn, symptoms that come on at night), prescription medication may be required.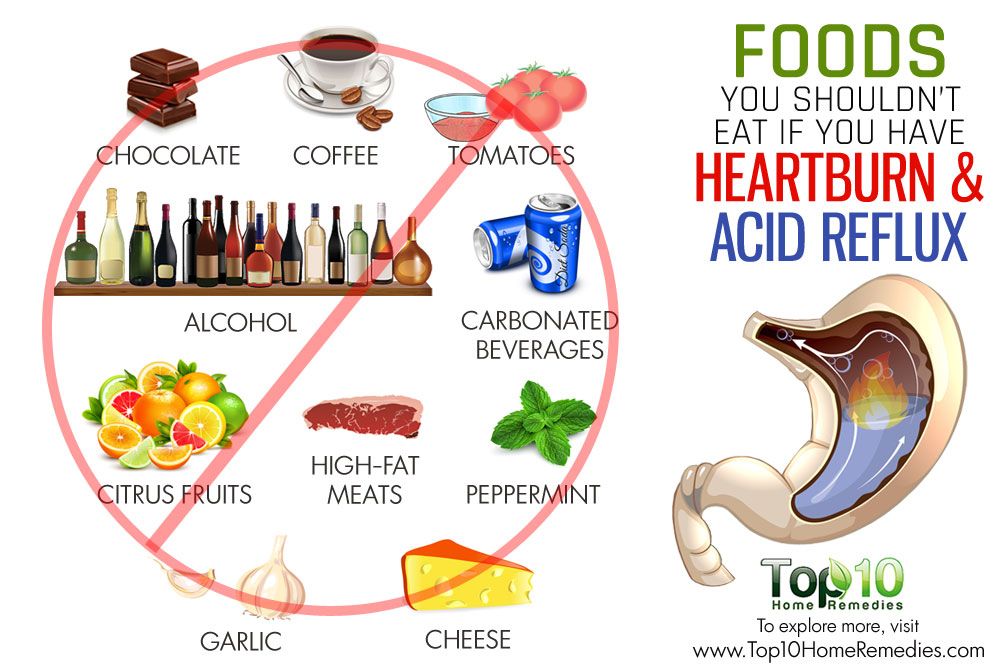 Surgery is a reasonable alternative to permanent medication, especially if the disease is acquired at an early age.
Surgery is a reasonable alternative to permanent medication, especially if the disease is acquired at an early age.
Surgery is also recommended if medication does not help. However, today there is a new generation of drugs that can effectively control gastroesophageal reflux.
If symptoms are still uncomfortable after taking strong drugs, GERD is most likely not the cause. Most gastroenterologists and surgeons do not recommend surgery in such cases, since the symptoms still continue to disturb after it.
Lifestyle changes
Gastroesophageal reflux treatment begins with lifestyle changes. First you need to understand what affects the occurrence of symptoms.
If you have symptoms of GERD, use the following tips:
- Avoid foods and drinks that stimulate the lower esophageal sphincter to relax, such as foods flavored with mint, chocolate, and alcohol.
- Lose weight if you are overweight.
 Being overweight and obese contributes to GERD because being overweight increases pressure on the stomach and lower esophageal sphincter, causing acidic stomach acid to reflux into the esophagus and irritate the esophageal mucosa.
Being overweight and obese contributes to GERD because being overweight increases pressure on the stomach and lower esophageal sphincter, causing acidic stomach acid to reflux into the esophagus and irritate the esophageal mucosa.
- Do not lie down for at least two or three hours after eating. After eating it is good to take a walk. This not only prevents the onset of GERD symptoms, but also burns extra calories.
- Avoid foods that trigger GERD symptoms. Do not eat fatty or fried foods, creamy sauces, mayonnaise or ice cream. Other foods that may exacerbate symptoms include coffee, tea, sodas, tomatoes, and citrus fruits.
- Stop smoking. Smoking disrupts the digestive system and, according to some studies, relaxes the lower esophageal sphincter. Smoking also reduces the amount of bicarbonate in saliva and reduces its ability to protect the esophagus from stomach acid.
 Some types of nicotine replacement therapy (nicotine patch, nicotine gum) can cause indigestion, stomach pain, and vomiting. Talk to your doctor about possible side effects of these products before use.
Some types of nicotine replacement therapy (nicotine patch, nicotine gum) can cause indigestion, stomach pain, and vomiting. Talk to your doctor about possible side effects of these products before use.
- Do not wear clothes that put pressure on your belly, such as tight belts, tight jeans, and elastic waistbands that put pressure on your stomach and lower esophageal sphincter.
- Raise the head of the bed 15 to 20 cm or use a wedge pillow to force acid into the stomach by gravity.
- Do not bend over after eating. If you need to pick something up from the floor, it's better to squat on half-bent knees and try not to bend at the waist. Do not engage in sports and physical labor after eating.
- Check your medications. Some medications can make symptoms worse. These drugs include theophylline, calcium channel blockers, alpha and beta blockers, anticholinergics that may be present in drugs used to treat Parkinson's disease, asthma, and some over-the-counter cold and cough medicines.
 If you think a drug you are taking is affecting your symptoms, talk to your doctor about alternatives. Do not interrupt the prescribed treatment without consulting a doctor.
If you think a drug you are taking is affecting your symptoms, talk to your doctor about alternatives. Do not interrupt the prescribed treatment without consulting a doctor.
Medication for gastroesophageal reflux
Your doctor may prescribe medication for GERD. Because GERD is often a chronic condition, you will need to take medication for the rest of your life. In some cases, long-term treatment is not required.
Be patient, it takes time to find the right drug and dosage. If the symptoms do not go away even after taking the drugs, or if they reappear immediately after completing the course, consult your doctor. If GERD symptoms appear during pregnancy, contact your obstetrician before starting medication.
The following is information about drugs commonly prescribed to treat GERD:
Over-the-counter antacids
These drugs help with mild and rare symptoms. Their action is to neutralize the acidic gastric juice. Antacids are usually fast-acting and can be taken as needed. Because they do not last long, they do not prevent heartburn and are less effective for symptoms that often occur.
Antacids are usually fast-acting and can be taken as needed. Because they do not last long, they do not prevent heartburn and are less effective for symptoms that often occur.
Most antacids contain calcium carbonate (Maalox) or magnesium hydroxide. Sodium bicarbonate, or baking soda, helps with heartburn and indigestion. It should be mixed with at least 120 ml of water and taken one to two hours after meals so as not to overload a full stomach. Talk to your doctor about the need for this treatment. Do not use this method for more than two weeks and use it only in extreme cases, since soda can lead to metabolic disorders (pH) and the formation of erosions in the esophagus and stomach. Before using it on children under 12 years of age, consult a doctor.
Another type of antacid contains alginate or alginic acid (eg Gaviscon). The advantage of such an antacid is that it does not allow fluid to seep back into the esophagus.
Antacids can interfere with the body's ability to absorb other drugs, so if you are taking other drugs, check with your doctor before taking antacids.
Ideally, you should take antacids at least 2-4 hours after taking other drugs to minimize the chance of them not being absorbed. People with high blood pressure should avoid taking high sodium antacids (Gaviscon).
Finally, antacids are not a reliable treatment for erosive esophagitis, a disease that must be treated with other drugs.
Hydrochloric acid suppressants
These drugs reduce the amount of acid produced by the stomach and are available both with and without a prescription. Usually, the same drugs are dispensed on prescription, but in a larger dosage. They may help those who are not helped by antacids. Most patients get better if they take drugs that suppress the production of hydrochloric acid and make lifestyle changes.
The mechanism of action distinguishes between two groups of such drugs:
-Blocks H 2 -gistamine reticators
-Proton pump inhibitors
Most likely, the doctor recommends taking the drug within a few weeks in a standard dose, and then if it is not possible to achieve the desired effect, prescribe a drug with a higher dosage.
Traditional h3 blockers include:
- nizatidine (Axid AR Axid AR)
- famotidine (Pepcid AS Pepcid AC)
- cimetidine (Tagamet HB Tagamet HB)
- ranitidine 75 (Zantac 75)
Pepcid Complete is a combination of famotidine, calcium carbonate and magnesium hydroxide found in antacids.
Conventional proton pump inhibitors include:
- lansoprazole (Prevacid)
- omeprazole (Prilosec, Prilosec)
- rabeprazole (AcipHex, AcipHex, Pariet)
- pantoprazole (Protonix Protonix, Nolpaza Nolpaza)
- esomeprazole (Nexium) , Nexium)
- omeprazole + sodium bicarbonate ("Zegeride" Zegerid)
- dexlansoprazole ("Dexilant" Dexilant)
Proton pump inhibitors (PPI) also reduce acidity, but are more powerful than h3- blockers. Proton pump inhibitors are most commonly prescribed to treat heartburn and acid reflux.
These drugs block the secretion of acid from the cells of the gastric mucosa and significantly reduce the amount of stomach acid.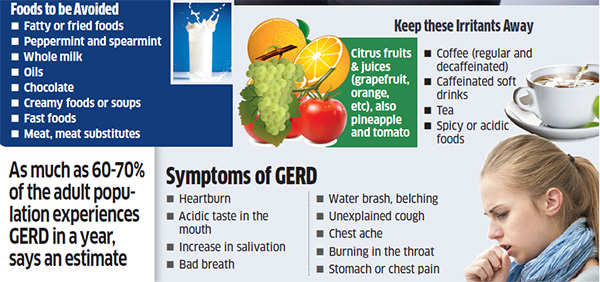 They don't work as fast as antacids, but they can relieve reflux symptoms for hours.
They don't work as fast as antacids, but they can relieve reflux symptoms for hours.
PPIs are also used to treat inflammation of the esophagus (esophagitis) and erosions of the esophagus. Studies have shown that the majority of patients with esophagitis who took these drugs recovered after 6-8 weeks. It is likely that your doctor will re-evaluate your health after 8 weeks of taking proton pump inhibitors and, according to the results, reduce the dosage or stop treatment. If symptoms do not return within three months, you will only need to take medication occasionally. People with liver disease should consult their doctor before taking these drugs.
Prokinetics
Prokinetics e.g. They also increase the contractions of the esophagus and stomach to some extent, so that the stomach is emptied more quickly. These drugs may be used as an adjunctive treatment for people with GERD.
GERD surgery
Surgery is an alternative to conservative treatment of GERD. Surgery is most commonly performed on young patients (because they would otherwise require long-term treatment) with typical GERD symptoms (heartburn and belching) who are helped by medication but are looking for an alternative to daily medication.
Surgery is most commonly performed on young patients (because they would otherwise require long-term treatment) with typical GERD symptoms (heartburn and belching) who are helped by medication but are looking for an alternative to daily medication.
Patients with atypical symptoms or patients who are not responding to medical treatment should only have surgery if there is no doubt about the diagnosis of GERD and the relationship between symptoms and reflux is confirmed by research.
Fundoplication is used in most cases. During this operation, the upper part of the stomach is wrapped around the lower esophageal sphincter, which increases its tone. These days, minimally invasive (laparoscopic) techniques are commonly used instead of traditional "open" surgery. One of the benefits of a fundoplication is that the hiatal hernia can also be repaired during the operation.
Surgery is not always effective and some patients still need to take medication after surgery.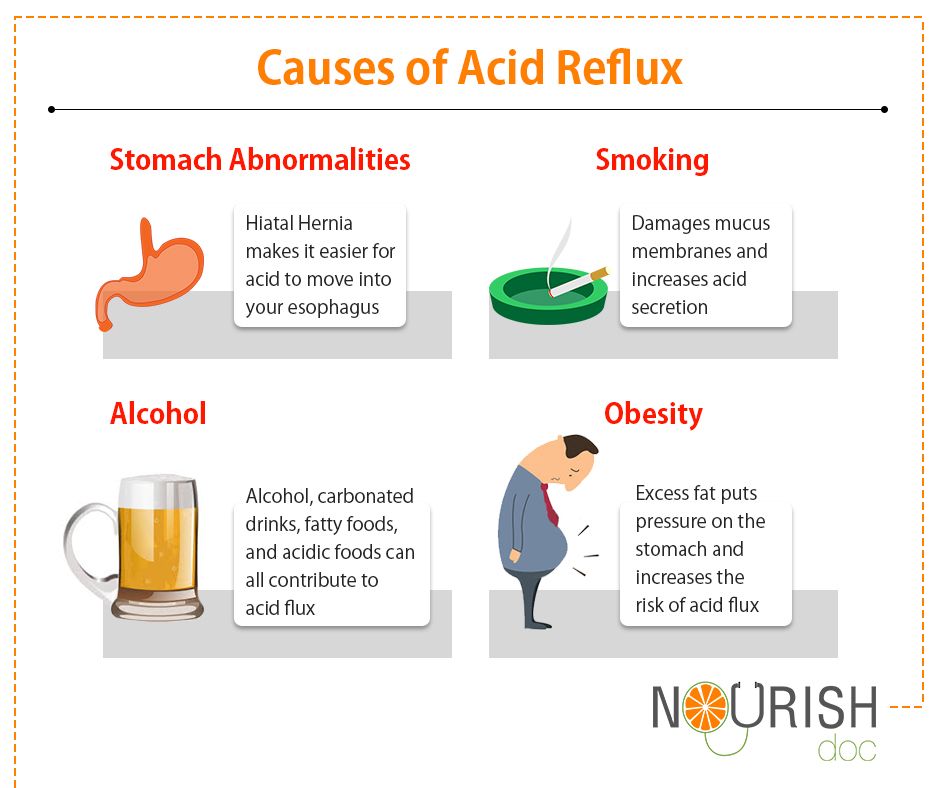 The results of this surgery are usually positive, but complications can still occur, such as difficulty swallowing, bloating and gas, difficult recovery after surgery, and diarrhea that occurs due to damage to the nerve endings that are adjacent to the stomach and intestines.
The results of this surgery are usually positive, but complications can still occur, such as difficulty swallowing, bloating and gas, difficult recovery after surgery, and diarrhea that occurs due to damage to the nerve endings that are adjacent to the stomach and intestines.
Prevention of GERD
First of all, you need to pay attention to lifestyle and avoid situations that can trigger the onset of the disease.
Remember that GERD happens when stomach acid backs up into the esophagus, which connects the throat to the stomach.
To keep the lower esophageal sphincter functioning properly, follow these guidelines:
Avoid bending over or other physical exercises that increase pressure on the abdominal cavity. Don't exercise on a full stomach.
Do not wear clothes that are tight around the waist, such as elastic waistbands and belts, which can increase pressure on the stomach.
Do not lie down in the field of food.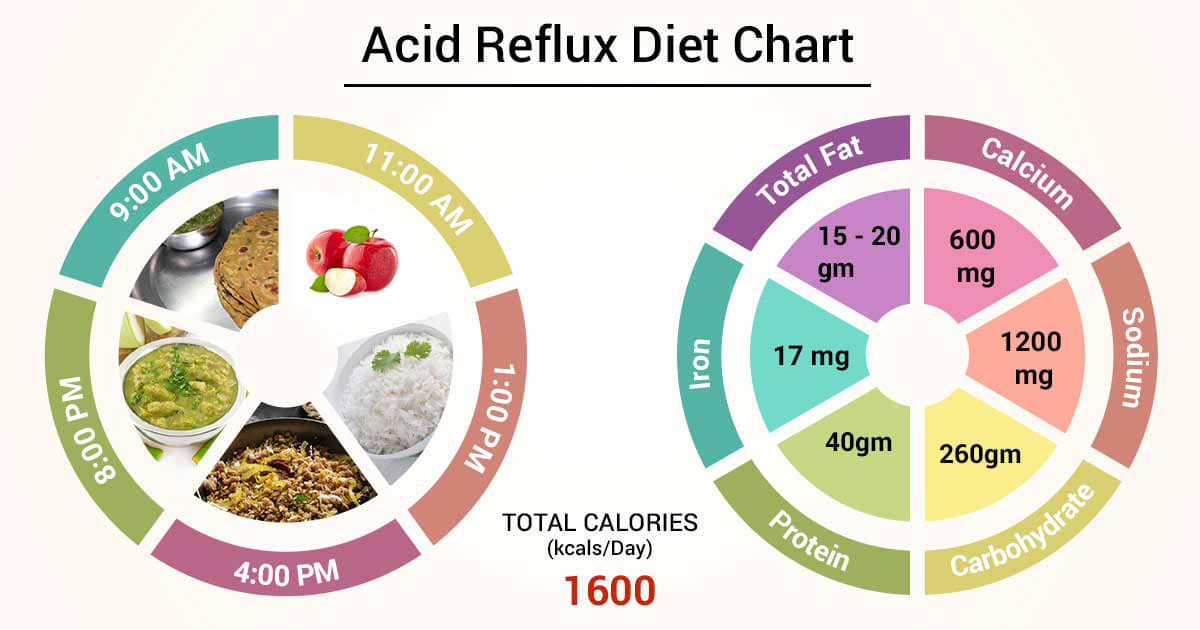 If you lie on your back after a large meal, it will be easier for the contents of the stomach to pass into the esophagus. For a similar reason, don't eat before bed. The head of the bed should rise 15-20cm so that gravity keeps the acid in the stomach where it should be while you sleep.
If you lie on your back after a large meal, it will be easier for the contents of the stomach to pass into the esophagus. For a similar reason, don't eat before bed. The head of the bed should rise 15-20cm so that gravity keeps the acid in the stomach where it should be while you sleep.
Do not overeat. Due to the fact that there is a large amount of food in the stomach, pressure on the lower esophageal sphincter increases, as a result of which it opens.
To keep your lower esophageal sphincter and esophagus functioning properly, follow these tips:
Quit smoking and avoid products containing tobacco. Smoking relaxes the lower esophageal sphincter, reduces the amount of acid-neutralizing saliva in the mouth and throat, and damages the esophagus.
Avoid foods that aggravate symptoms, such as tomato sauces, mints, citrus fruits, onions, coffee, fried foods, and carbonated drinks.
Do not drink alcoholic beverages.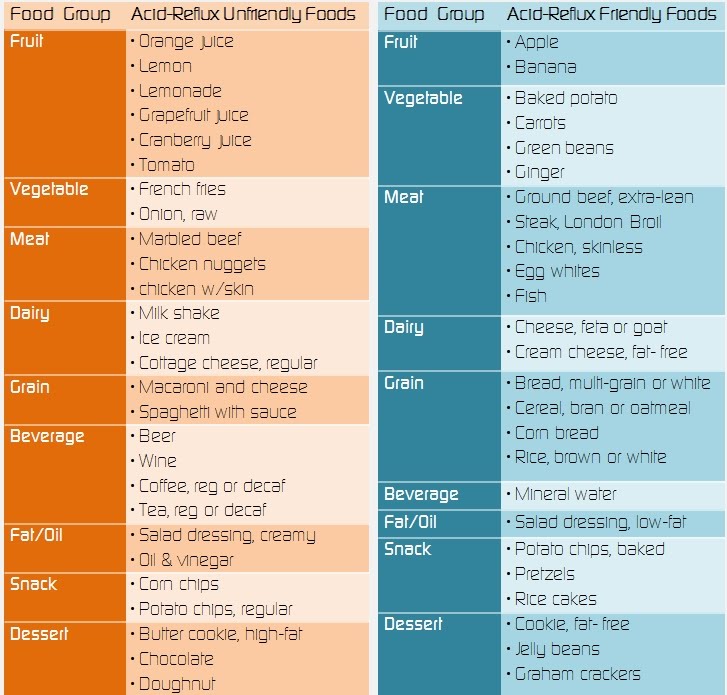 Alcohol causes the lower esophageal sphincter to relax, and the esophagus may begin to contract unevenly, causing acid to reflux into the esophagus and cause heartburn.
Alcohol causes the lower esophageal sphincter to relax, and the esophagus may begin to contract unevenly, causing acid to reflux into the esophagus and cause heartburn.
Check your medications. Some medications can make symptoms worse. Do not interrupt the prescribed treatment without consulting your doctor. Drugs that have this effect include asthma and emphysema drugs (such as theophylline), anticholinergics for Parkinson's disease and asthma, sometimes found in over-the-counter drugs, some calcium channel blockers, alpha blockers, and beta-blockers to treat heart disease or high blood pressure, some drugs that affect the nervous system, iron supplements.
While some drugs exacerbate GERD symptoms, others can cause drug-induced esophagitis, a condition that causes the same symptoms as GERD but is not due to reflux. Drug esophagitis happens when a pill is swallowed but does not reach the stomach because it sticks to the wall of the esophagus. Because of this, the mucous membrane of the esophagus is corroded, chest pain, esophageal ulcers and pain during swallowing occur.