Baby bringing up milk straight after feed
Reflux | Breastfeeding Challenges | Start for Life
Breastfeeding challenges
There may be times when breastfeeding is challenging. Never ignore any issues you may have – talk to your health visitor, midwife, GP or breastfeeding specialist as soon as possible, they will be able to help you sort it out quickly.
Here are some common breastfeeding issues, and tips on what to do.
- Colic
- Constipation
- Mastitis
- Milk supply
- Reflux
- Sore nipples
- Thrush
- Tongue-tie
Baby reflux
If your baby brings up milk, or is sick during or after feeding, this is known as reflux. Reflux, also called posseting or spitting up, is quite common and your baby should grow out of it, usually by the time they are 12 months old.
What causes baby reflux?
The muscle at the bottom of the food pipe acts as a kind of door into the stomach – so when food or milk travels down, the muscle opens allowing the food into the stomach.
However, while this muscle is still developing in the first year, it can open when it shouldn't (usually when your baby's tummy is full) allowing some food and stomach acid to travel back up again. Acid in the stomach is normal and a necessary part of the digestion process – it helps break down food.
In most babies, reflux is nothing to worry about as long as they are healthy and gaining weight as expected.
Baby reflux symptoms
- Constant or sudden crying when feeding.
- Bringing up milk during or after feeds (regularly).
- Frequent ear infections.
- Lots of hiccups or coughing.
- Refusing, gagging, or choking during feeds.
- Poor weight gain.
- Waking up at night a lot.
GORD
When reflux becomes painful and it happens frequently, this is known as 'gastro-oesophageal reflux disease' (GORD). GORD is more serious than mild, everyday reflux. The strong stomach acid can irritate and make the food pipe sore and inflamed, which is painful for your baby and may result in them needing medication.
The main signs and symptoms of GORD in your baby are:
- spitting up frequently
- abdominal pain
- feeding difficulties
- seeming unsettled and grizzly after a feed
These symptoms can lead to your baby not gaining weight, or even losing weight.
Silent reflux
Silent reflux can be confusing as there are no obvious signs or clues (such as spitting up). It's when the food travels back up the food pipe – but it's swallowed rather than spat out so is harder to identify. But your baby may display similar symptoms to those of regular reflux.
Breastfeeding Friend from Start for Life
The Breastfeeding Friend, a digital tool from Start for Life, has lots of useful information and expert advice to share with you – and because it's a digital tool, you can access it 24 / 7.
Breastfeeding tips for babies with reflux
- Feeding little and often (smaller feeds stop their tummy getting too full).
- Burping them requently during feeds – have a look at our guide to burping your baby for techniques.

- Try a different feeding position – check out our our guide to breastfeeding positions.
- Keep your baby upright, for at least an hour after feeding, this should help keep the milk down.
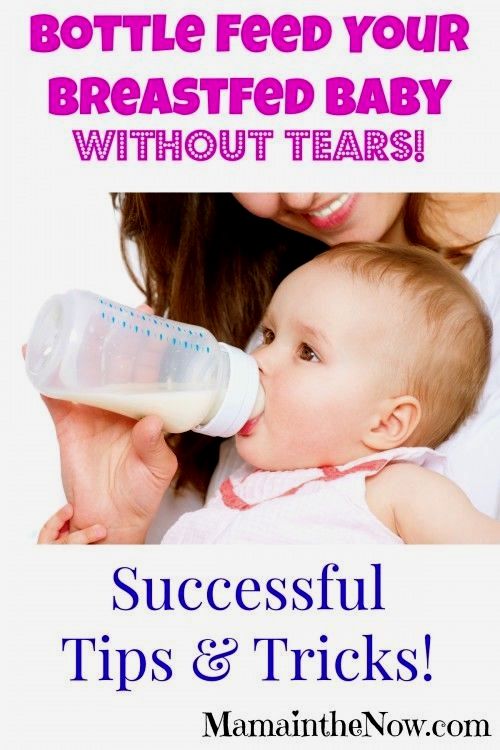
If you are mixed feeding (combining breastmilk and formula feeds), have a look at our advice on bottle feeding and reflux.
When to see the GP
If your baby has difficulty feeding or refuses to feed, regularly brings milk back up and seems uncomfortable after a feed, talk to your pharmacist, GP, or health visitor. They'll be able to give you practical advice on how to ease the symptoms and manage it – they may also need to rule out other causes (such as cow's milk allergy).
It might be helpful to keep a record of when your baby feeds, with details of how often and how much your baby brings the food back up, and how often your baby cries or seems distressed. This will help your health visitor or GP decide if your baby needs treatment.
My Baby Is Bringing Up Milk!
It’s not uncommon for many babies to bring up a little milk at the end of a feed.
However, some babies bring up a lot more than that – sometimes, it could be at every other feed, or you may find that this is happening at every feed! If this is happening to your baby, it can be a little disconcerting.
However, if your baby is generally well and not unduly uncomfortable with this, then it’s very likely to be a typical kind of reflux.
It’s important to know that your baby’s digestive system is quite immature for at least six months, so it is easy for milk to backtrack up from the stomach into the esophagus (this is the tube that connects the stomach with your baby’s mouth).
If this happens to your baby, please recognize that this type of reflux is perfectly normal.
However, some babies bring up milk for other reasons, for example, if you have a fast let-down of milk.
In this situation, you may find that your baby will do the initial fast sucks to call the milk down, then the milk will come shooting down, and this flow can be very fast!
Your baby is likely to start coughing and spluttering and sucking in air.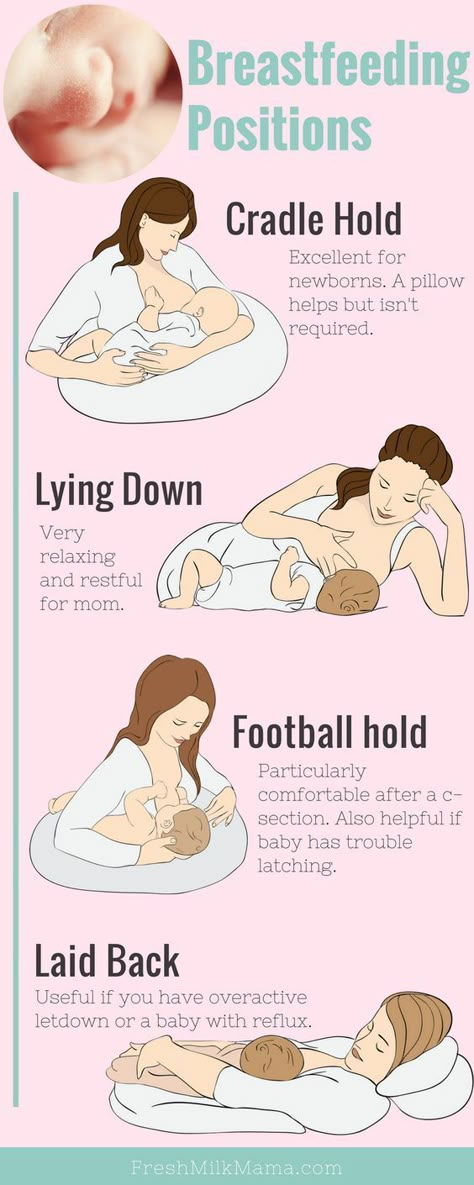 When babies suck in the air, they will often bring up milk as a consequence.
When babies suck in the air, they will often bring up milk as a consequence.
It’s also possible that your baby is bringing up milk because your breasts are engorged, which means that they are becoming full and possibly painful.
There is also a medical condition called pyloric stenosis where your baby may have projectile vomiting, usually occurring in newborns between three to five weeks.
With this condition, a very forceful amount of milk may come out of your newborn’s mouth at least once per day, so a doctor must make a diagnosis because pyloric stenosis is a serious condition that requires surgery.
So apart from pyloric stenosis, if your doctor is suspecting GERD, then he’s likely to start your baby on a course of medication to settle the symptoms, or may suggest some further tests.
Because we know that babies often feel so much more comfortable when they’re upright, it’s a good idea to feed your baby in vertical positions too.
Consider that your baby can feed in all positions, so consider what would be the most comfortable for you and your baby.
If your baby’s head is higher than the rest of his body, this can help him to feel more comfortable.
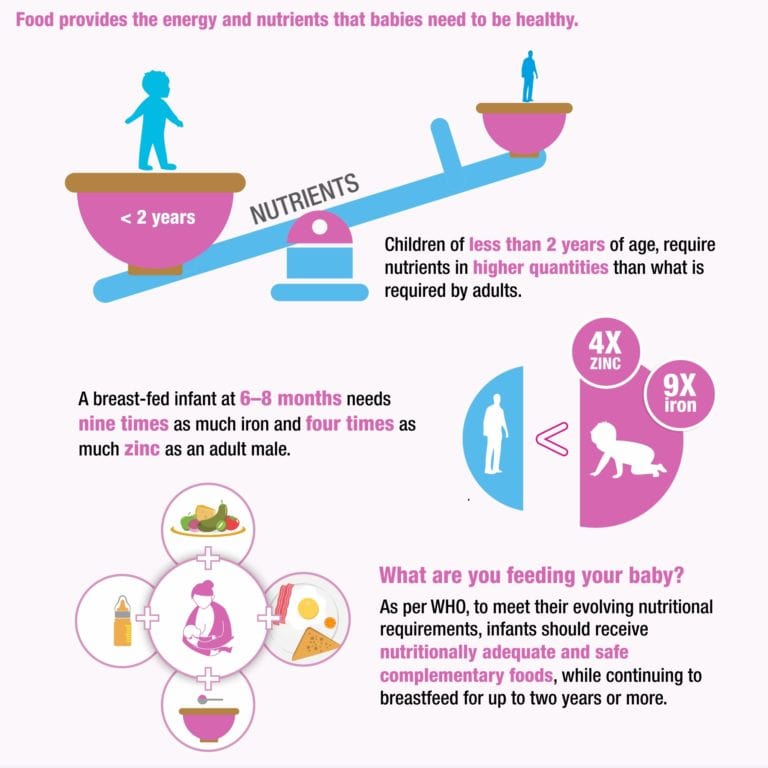
Your baby is also likely to benefit from short, frequent feeds because breastmilk is very digestible.
It will go through his system very fast. Also, those frequent feeds mean that milk won’t sit around in the stomach for too long and then be able to backtrack.
Even if the milk does backtrack up the esophagus, it is less irritating than formula milk is.
Also, watch out for your baby’s feeding cues and determine which strategies work best to ease your baby’s symptoms.
Do bear in mind that not all babies will lose weight in this situation. Many will happily follow their growth charts according to their normal centiles.
Some babies WILL lose weight, however, and your doctor will need to monitor the situation.
Also, note that the medications doctors give to babies for this condition can sometimes take two to four weeks to take effect.
Be assured that if your baby HAS been diagnosed with GERD, and started medication, over the next few weeks and months, and also as you begin to introduce solids around six months of age, you will generally see an improvement.
Do seek out skilled support from a health professional who understands about GERD and seek help from your family members who can offer support to you during this difficult time.
Solving five breastfeeding problems after the first month
Expert advice on solving the top five breastfeeding problems that may arise after the first month.
Share this information
Cathy Garbin, child health nurse, midwife and lactation consultant:
Cathy, a mother of two, was a research fellow at the renowned Human Lactation Research Institute, founded by Peter Hartmann, for seven years, providing support to breastfeeding mothers in clinics and at home. Today, she still works as a family counselor, and also conducts seminars for attending physicians and speaks at international conferences.
You and your baby have already fully established the process of breastfeeding and know what and how to do. It seems that all difficulties are left behind. However, some more surprises await you. The following are suggestions for dealing with breastfeeding problems that may arise later.
However, some more surprises await you. The following are suggestions for dealing with breastfeeding problems that may arise later.
Problem #1. I need to be away from my baby
Whether it's social events, travel or medical treatment, at some point you may need to be away from your baby for a while.
Solutions
- Express milk so that someone else can feed the baby. Now that breastfeeding is established, you can express and store your breast milk in the refrigerator or freezer. Try different options to find the most convenient time for pumping in your daily routine. Some mothers manage to pump more breast milk in the morning when the baby wakes up after a long night's sleep. For others, it's best to express 60 minutes after feeding. Remember that everyone is different. Don't be discouraged if you don't get enough milk the first time: it's possible that you'll be able to express enough for one feeding in just two or three pumpings.
 As with feeding, it may take time for your body to adjust to pumping.
As with feeding, it may take time for your body to adjust to pumping. - Take your breast pump with you, if you plan to skip a feed. Even if you leave your baby with expressed milk, but will be absent for more than two hours, you will need to empty your breast. Pump at the same frequency as you would breastfeed your baby. This will support milk production and prevent discomfort. Express milk regularly throughout the day without waiting for your breasts to overflow. 1 Most electronic breast pumps are battery operated, so you don't have to find an outlet nearby.
Problem #2. How to continue breastfeeding after returning to work?
You will likely have to leave your baby more often and for longer when you go to work, so it's especially important to find ways to continue breastfeeding and pumping that work for both of you. As mentioned above, you can build up a supply of breastmilk before you go to work and then pump regularly to support milk production, prevent discomfort, and make sure your baby has enough pumped milk the next day. Many companies now provide dedicated pumping rooms, and modern breast pumps work efficiently and reliably. If you have a regular work schedule or work part-time, you can still breastfeed your baby before and after work and at night.
Many companies now provide dedicated pumping rooms, and modern breast pumps work efficiently and reliably. If you have a regular work schedule or work part-time, you can still breastfeed your baby before and after work and at night.
Solutions
- Express as often as you would feed your baby. This will help maintain milk production and prevent discomfort, as well as reduce the risk of clogged milk ducts, mastitis and breast swelling. 1
- Try double pumping. Double pumping not only takes half the time, but also produces an average of 18% more milk than pumping from each breast in sequence. Milk is more nutritious and has a higher fat content. 2
- Assemble and bring to work the set, which includes a breast pump, milk storage bags and, if desired, a bustier top for hands-free pumping. You will also need a cooler bag to carry your expressed milk.
- Know your rights.
 In many countries, the law allows women to express and safely store breast milk at work. Discuss these options with your employer before returning to work. This will get you both ready.
In many countries, the law allows women to express and safely store breast milk at work. Discuss these options with your employer before returning to work. This will get you both ready.
Problem #3. It seems to me that the baby suckles only for pleasure
Sometimes you may feel that the baby takes your breast in order to calm down, and not to eat. However, do not forget that breastfeeding is not only nutrition, it is also comfort for your baby. "Soothing suckling" (when the baby suckles but does not eat milk) helps the baby to calm down and relax. Remember that a sudden increase in the frequency or duration of feedings may indicate insufficient milk production. However, if the baby continues to gain weight and you use enough diapers a day, this is unlikely.
Solution
- Be patient. The baby needs your care - listen to his needs and support him. Usually, the period of soothing suckling does not last too long, but it allows the child to feel your love and protection - and this is the best thing you can give him.

Problem #4. I want to switch from mixed to exclusive breastfeeding
Breastfeeding is so good for you and your baby that it's worth trying to fight for it. However, if you have rarely fed lately, your milk production may have been reduced. If your baby has only been mixed-fed for a couple of weeks, you will most likely be able to restore enough milk. Contact a lactation consultant or medical specialist who will help you and give you the necessary advice. This is a very individual process that depends on many factors. In any case, do not despair, because every drop of your milk is important for the child.
Solutions 1.3
- Increase milk production. Try to put the baby to the breast more often, because the more milk the baby consumes, the more milk is produced. You can also express milk additionally. As mentioned earlier, double pumping in particular helps increase milk production.
- Be in physical contact with your baby as much as possible.
 As in the first days after childbirth, close physical contact with the baby promotes the production of the hormone oxytocin, which in turn triggers milk production. It will also make both of you feel more calm and relaxed.
As in the first days after childbirth, close physical contact with the baby promotes the production of the hormone oxytocin, which in turn triggers milk production. It will also make both of you feel more calm and relaxed. - Reduce the number of formula feedings gradually. Resist the urge to stop supplementing with formula right away. If you gave your baby formula after each breastfeed, start giving it every other time until milk production rises. Keep a close eye on the number of soiled diapers and weight gain during this transition period. It is likely that at first the child will ask for the breast more often, and this is absolutely normal.
- Speak with a lactation consultant or healthcare professional. He will be able to help you and strengthen your confidence that your baby gets everything he needs.
Problem #5. My child has lost interest in the breast
If your child, who always ate with appetite, suddenly began to refuse the breast for no apparent reason, this is a false refusal, the so-called "strike". You may assume that he is ready to switch to solid foods, or that he does not like your milk anymore, but this is most likely not the case. It's just that the child develops vision, and now he is more distracted by the world around him. Or maybe something frightened the child during feeding, or he reacts to a violation of the regimen, perhaps he has a stuffy nose or teething. What you take for lack of interest may actually mean that your baby has simply learned to breastfeed more effectively and therefore takes less time to suckle.
You may assume that he is ready to switch to solid foods, or that he does not like your milk anymore, but this is most likely not the case. It's just that the child develops vision, and now he is more distracted by the world around him. Or maybe something frightened the child during feeding, or he reacts to a violation of the regimen, perhaps he has a stuffy nose or teething. What you take for lack of interest may actually mean that your baby has simply learned to breastfeed more effectively and therefore takes less time to suckle.
Solutions
- Be patient. False rejection is usually temporary and goes away after a few days. To provide the baby with the necessary nutrition during this period, give him expressed milk.
- Find a quieter feeding area with as few distractions as possible. Baby is more likely to eat better if he can relax and focus on his chest.
- Check in which position you feed.
 The baby may refuse to breastfeed if he is uncomfortable or unable to move his head to breathe during feeding.
The baby may refuse to breastfeed if he is uncomfortable or unable to move his head to breathe during feeding. - Express milk to keep it flowing . You can try feeding your baby with expressed breast milk using the Medela Calma smart pacifier.
- Do not start formula or solid foods. Supplementing with formula can lead to reduced milk production and will only make matters worse. If your baby is regularly fed with expressed milk and is growing well, and the number of soiled diapers is normal, try not to worry. If the baby is less than six months old, you should not give him solid food: his digestive system is not yet strong and may not be ready for such a load.
- Do not force-feed. Try to relax and be in skin-to-skin contact with your baby as much as possible, hug him and often offer the breast so that he can take it on his own. The release of oxytocin that body contact triggers will also help you pump.
 4
4
Related content: Breastfeeding: what to expect after the first month
Literature
1 Kent JC et al. Principles for maintaining or increasing breast milk production. J Obstet , Gynecol , & Neonatal Nurs . 2012;41(1):114-121. - Kent J.S. et al., "Principles for Maintaining and Increasing Breast Milk Production". G Obstet Ginecol Neoneutal Nurs. 2012;41(1):114-121.
2 Prime DK et al. Simultaneous breast expression in breastfeeding women is more efficacious than sequential breast expression. Breast Med . 2012;7(6):442-447. - Prime D.K. et al., “During the breastfeeding period, pumping both breasts simultaneously is more productive than sequential pumping.” Brest Med (Breastfeeding Medicine). 2012;7(6):442-447.
3 Amir L. Breastfeeding managing ‘supply’ difficulties. Aust fam physician . 2006;35(9):686. - Amir L., "Breastfeeding: Problems of 'Supply'. Aust Fam Physical. 2006;35(9):686.
Aust fam physician . 2006;35(9):686. - Amir L., "Breastfeeding: Problems of 'Supply'. Aust Fam Physical. 2006;35(9):686.
4 Moberg KU, Prime DK. Oxytocin effects in mothers and infants during breastfeeding. Infant . 2013;9(6):201-206. - Moberg KW, Prime DK, "The effects of oxytocin on mother and child during breastfeeding." Infant. 2013;9(6):201-206.
Feeding expressed milk | breastfeeding
When can I start breastfeeding my baby with expressed breast milk? How to do it right? Is it worth worrying that the child will confuse the pacifier with the breast? In this article we will answer your questions.
Share this information
When can I start breastfeeding my baby?
If your baby is healthy and breastfeeding well, there is no need to give him expressed milk. For the first four weeks, you work together to start and increase milk production, and your baby also learns to suckle properly at the breast. There is not enough scientific evidence on this yet, 1 but there is an opinion that bottle feeding in the first month may negatively affect the process of establishing breastfeeding.
There is not enough scientific evidence on this yet, 1 but there is an opinion that bottle feeding in the first month may negatively affect the process of establishing breastfeeding.
However, if the newborn is unable to latch on or suckle for some reason, start expressing milk as soon as possible after birth. Read more about this in our articles on coping with problems in the first week, breastfeeding premature babies and babies with special needs, and seeking help from your healthcare provider.
How to feed your baby with expressed breast milk?
There are many expert feeding solutions that allow you to give your baby expressed milk in a variety of ways, depending on your and your baby's needs.
For example, the innovative Calma smart pacifier only lets milk through when the baby creates a vacuum by suckling. This means that when feeding from a bottle, he will make the same movements with his tongue and jaws as when sucking at the breast. 2.3 The Calma Smart Soother was developed with input from breastfeeding experts at the University of Western Australia. When using this pacifier, the baby can suck, swallow, pause and breathe in the same way as when breastfeeding. 4 Preservation of natural sucking skills allows the baby to easily transition from breast to bottle and back.
2.3 The Calma Smart Soother was developed with input from breastfeeding experts at the University of Western Australia. When using this pacifier, the baby can suck, swallow, pause and breathe in the same way as when breastfeeding. 4 Preservation of natural sucking skills allows the baby to easily transition from breast to bottle and back.
In addition, Medela also offers regular bottle teats* in two versions that produce milk at different rates. All Medela* nipples can be placed directly on bottles used for expressing milk, minimizing the risk of spillage.
If you need to feed your baby with expressed milk, but you do not want to bottle feed him until he is learning to breastfeed, you can use a sippy cup* for temporary feeding. The baby will be able to drink milk from such a mug, but you should be careful not to spill the milk. For the first time, it is advisable to feed the child from a drinking cup under the supervision of the attending physician in order to learn how to do it correctly.
If your baby needs to be supplemented with expressed milk in addition to regular breastfeeding, the Supplementary Feeding System (SNS)* can be used. It is equipped with a thin, flexible capillary that can be clipped close to the nipple to give your baby expressed milk while breastfeeding. Thanks to this, the baby suckles the breast for longer, thereby developing sucking skills and stimulating the production of milk from the mother. This can be helpful when there is a shortage of breast milk, as well as when feeding adopted or surrogate children.
If the baby is unable to breastfeed because he is too weak or has a congenital disease, you can use the Special Needs Cup*, which releases milk with gentle pressure, making it suitable for feeding these babies.
How to teach a child to bottle feed?
If breastfeeding is going well and you decide to start bottle feeding your baby with expressed breast milk, follow these guidelines.
Start early and take your time
Don't wait until the first day of work or the first time you leave the house to start bottle feeding your baby. Start accustoming your baby to small portions of expressed milk a couple of weeks before the desired date, calmly and without haste. Gradually build up to one full serving of pumped milk from a bottle.
Start accustoming your baby to small portions of expressed milk a couple of weeks before the desired date, calmly and without haste. Gradually build up to one full serving of pumped milk from a bottle.
Choose a time
Ideally, at the first bottle feeding, the baby should be hungry, but not too hungry - in this state, he is as relaxed as possible.
Let others feed
Your baby is used to feeding from your breast, so when you offer him a bottle it can be confusing. The process can go faster if the first time the baby is bottle-fed by someone else while you are not in the room, so that your sight and smell do not embarrass the baby.
Maintain optimal temperature
Your baby will be more willing to eat expressed milk if the temperature is around 37°C, close to body temperature.
Dip the nipple in milk
Try dipping the nipple in expressed milk before offering it to your baby. This way it will taste and smell like your breast milk. Lightly touch the baby's upper lip with the nipple to open the mouth.
This way it will taste and smell like your breast milk. Lightly touch the baby's upper lip with the nipple to open the mouth.
Choose the right position for bottle feeding
Feed your baby on demand and keep him reclining during feeding. Never bottle feed your baby when he is lying or sitting, otherwise he may choke. Listen to the wishes of the child - take as many pauses as he needs. You can even try to shift it from one hand to another during feeding.
Be patient
Don't worry if your baby doesn't take the bottle right away - it may take several tries. If he pushes the bottle away or starts crying, calm him down, wait a few minutes and try again. If he still doesn't want to bottle feed, wait a few more minutes and breastfeed him as usual. Repeat the bottle experiment at a different time of day.
How much expressed milk should I give my baby?
All children are different. Research shows that between the ages of one and six months, a baby can consume between 50 and 230 ml of milk per feeding. To start, prepare about 60 ml and observe how much your baby needs - more or less. You will soon realize how much milk he usually eats. Just never force him to finish the cooked portion.
To start, prepare about 60 ml and observe how much your baby needs - more or less. You will soon realize how much milk he usually eats. Just never force him to finish the cooked portion.
How can I keep my baby safe when bottle feeding?
Always clean and sterilize the pump and bottles according to the manufacturer's instructions. Wash your hands before expressing, pouring milk, and feeding your baby. Follow our instructions for safely storing and thawing your expressed milk.
If breastmilk needs to be warmed, place the bottle or bag in a bowl of warm water or a heater or under running water at a maximum of 37°C. Never heat breast milk in the microwave or on the stove.
Will the baby be able to transition from breast to bottle?
Some mothers worry that if they start bottle feeding too early, the baby will get used to the artificial nipple and not want to breastfeed. Others, on the contrary, are worried that if the child is not immediately accustomed to the bottle, then he will no longer eat from it.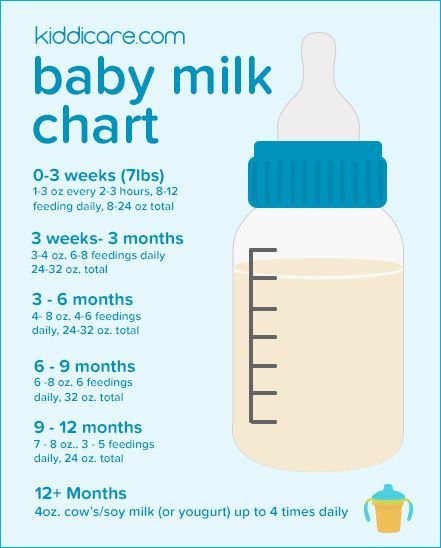 In general, in these cases, they say that the child confuses the nipple with the breast.
In general, in these cases, they say that the child confuses the nipple with the breast.
Experts disagree on whether such confusion is a problem. 1 Without a doubt, it is easier for a baby to suckle milk from a regular bottle with a nipple, which does not require a vacuum, than from the breast, since the milk flows faster, also under the influence of gravity. And some babies really have clear preferences: only the breast or only the nipple. However, many babies are comfortable suckling both the breast and the pacifier.
If you are unable to feed your baby with expressed breast milk, seek help from a lactation consultant or specialist.
Literature
1 Zimmerman E, Thompson K. Clarifying nipple confusion. J. Perinatol. 2015;35(11):895-899. - Zimmerman I., Thompson K., "On the issue of breastfeeding." J Perinatol (Journal of Perinatology). 2015;35(11):895-899.
2 Geddes DT et al. Tongue movement and intra-oral vacuum of term infants during breastfeeding and feeding from an experimental teat that released milk under vacuum only.