How to regulate baby feeding
Tips for the First Year
Eat, sleep, pee, poop, repeat. Those are the highlights in a day of the life of a brand new baby.
And if you’re a new parent, it’s the eating part that may be the source of many of your questions and worries. How many ounces should your baby take? Do you wake a sleeping baby to eat? Why do they seem hungry all the time? When can your child start solids?
Questions abound — and, despite Grandma’s insistence, the answers have changed since you were a tot. It’s now recommended that newborns, even formula-fed ones, eat on demand (consider it good preparation for the teenage years) and that babies wait to start solid foods until they’re 4 to 6 months old.
On day one of life, your baby’s stomach is the size of a marble and can only hold 1 to 1.4 teaspoons of liquid at a time. As your baby gets older, their stomach stretches and grows.
It’s hard (or impossible, really) to know how much milk your baby is taking in while breastfeeding. But if you’re bottle feeding due to any number of valid reasons, it’s a bit easier to measure.
Here, from the American Academy of Pediatrics (AAP), a typical feeding schedule for bottle-fed babies.
| Age | Ounces per feeding | Solid foods |
|---|---|---|
| Up to 2 weeks of life | .5 oz. in the first days, then 1–3 oz. | No |
| 2 weeks to 2 months | 2–4 oz. | No |
| 2–4 months | 4-6 oz. | No |
| 4–6 months | 4–8 oz. | Possibly, if your baby can hold their head up and is at least 13 pounds. But you don’t need to introduce solid foods yet. |
| 6–12 months | 8 oz. | Yes. Start with soft foods, like one-grain cereals and pureed vegetables, meats, and fruits, progressing to mashed and well-chopped finger foods. Give your baby one new food at a time. Continue supplementing with breast or formula feedings. |
Every baby is unique — but one thing that’s pretty consistent is that breastfed babies eat more frequently than bottle-fed ones. That’s because breast milk is easily digested and empties from the stomach a lot quicker than formula.
Breastfed babies
There’s no rest for the weary. According to La Leche League International, you should begin nursing your baby within 1 hour of birth and provide about 8 to 12 feedings daily in the first few weeks of life (yeah, we’re exhausted for you).
At first, it’s important not to let your baby go more than 4 hours without feeding. You’ll likely need to wake them up if necessary, at least until breastfeeding is well established and they’re gaining weight appropriately.
As your baby grows and your milk supply amps up, your baby will be able to take in more milk in less time at one feeding. That’s when you might start to notice a more predictable pattern.
- 1 to 3 months: Your baby will feed 7 to 9 times per 24 hours.

- 3 months: Feedings take place 6 to 8 times in 24 hours.
- 6 months: Your baby will feed around 6 times a day.
- 12 months: Nursing may drop to about 4 times a day. The introduction of solids at about 6 months helps to fuel your baby’s additional nutritional needs.
Keep in mind that this pattern is just one example. Different babies have different paces and preferences, along with other factors that influence the frequency of feedings.
Bottle-fed babies
Like breastfed babies, bottle-fed newborns should eat on demand. On average, that’s about every 2 to 3 hours. A typical feeding schedule may look like this:
- Newborn: every 2 to 3 hours
- At 2 months: every 3 to 4 hours
- At 4 to 6 months: every 4 to 5 hours
- At 6+ months: every 4 to 5 hours
For both breastfed and bottle-fed babies
- Don’t give liquids other than formula or breast milk to babies under a year old. That includes juices and cow’s milk.
 They don’t provide the right (if any) nutrients and can be upsetting to your baby’s tummy. Water can be introduced around 6 months when you start offering a cup.
They don’t provide the right (if any) nutrients and can be upsetting to your baby’s tummy. Water can be introduced around 6 months when you start offering a cup. - Don’t add baby cereal to a bottle.
- It can create a choking hazard.
- A baby’s digestive system isn’t mature enough to handle cereal until about 4 to 6 months of age.
- You could overfeed your baby.
- Don’t give your baby any form of honey until after their first birthday. Honey can be dangerous for a baby, occasionally causing what’s called infant botulism.
- Do adjust your expectations based on your baby and their unique needs. Premature babies are likely to follow feeding patterns according to their adjusted age. If your baby has challenges like reflux or failure to thrive, you may need to work with your doctor on the appropriate feeding schedule and amount they should be eating.
Schedules are the holy grail of every parent. Your child will naturally start to fall into a feeding pattern as their tummy grows and they can take in more breast milk or formula at one sitting. This may begin to happen between 2 and 4 months of age.
This may begin to happen between 2 and 4 months of age.
For now, though, focus on learning your baby’s hunger cues, such as:
- rooting around your chest, looking for a nipple.
- putting their fist in their mouth
- smacking or licking their lips
- fussing that can escalate quickly (don’t wait until your baby’s hangry to feed them)
Once your baby is a few months old, you may be able to introduce a sleep/feed schedule that works for you.
Let’s say, for example, your 4-month-old wakes every 5 hours for a feeding. That means if you feed at 9 p.m., your baby wakes around 2 a.m. But if you wake and feed the baby at 11 p.m., just before you go to bed, they may not rouse until 4 a.m., giving you a decent chunk of nighttime winks.
In general, if your baby seems hungry, feed them. Your baby will naturally eat more frequently during growth spurts, which typically occur around 3 weeks, 3 months, and 6 months of age.
Some babies will also “cluster feed,” meaning they’ll feed more frequently during certain periods and less at others. For example, your baby may cluster feed during the late afternoon and evening and then sleep longer at night (yay!). This is more common in breastfed babies than bottle fed babies.
For example, your baby may cluster feed during the late afternoon and evening and then sleep longer at night (yay!). This is more common in breastfed babies than bottle fed babies.
Worried about overfeeding? While this isn’t really possible to do with an exclusively breastfed baby, you can overfeed a baby who’s taking a bottle — especially if they’re sucking on the bottle for comfort. Follow their hunger cues, but talk to your pediatrician if you’re worried your little one may be overeating.
Your baby is probably ready for solids if they’re 4 to 6 months old and:
- have good head control
- seem interested in what you’re eating
- reach for food
- weigh 13 or more pounds
Which food to start with? The AAP now says it doesn’t really matter much in what order you introduce foods. The only real rule: Stick with one food for 3 to 5 days before offering another. If there’s an allergic reaction (rash, diarrhea, vomiting are common first signs), you’ll know which food is causing it.
As your baby grows, move from pureed baby food to ones that have more texture (for example, mashed banana, scrambled egg, or well-cooked, chopped pasta). This generally happens around 8 to 10 months of age.
Your supermarket offers a variety of baby food products, but if you want to make your own, keep it sugar and salt free. Additionally, at this stage, don’t feed your baby anything that could be a choking hazard, including:
- hard foods, such as popcorn or nuts
- hard, fresh fruits, like apples; cook to soften or chop into very small pieces
- any meat that isn’t well cooked and very well chopped (this includes hot dogs)
- cheese cubes
- peanut butter (though talk to your pediatrician about this one — and the benefits of introducing diluted peanut butter before the age of 1)
As your baby nears their first birthday, they should be eating a variety of foods and taking in about 4 ounces of solids at each meal. Continue to offer breast milk or formula. By 8 months, babies are drinking about 30 ounces a day.
By 8 months, babies are drinking about 30 ounces a day.
Oh yeah, and buy some stock in a company that makes stain-fighting laundry detergent. It’ll pay for college.
Babies aren’t cookie cutter. Some will gain weight easily, while others will have problems. Things that can affect a baby’s weight gain include:
- having a birth defect like a cleft lip or palate, which creates problems feeding
- having a milk protein intolerance
- being premature
- being fed with a bottle versus the breast
A 2012 study of more than 1,800 babies found that the infants who were fed with a bottle — regardless of whether the bottle contained breast milk or formula — gained more weight in the first year than babies who nursed exclusively.
Your baby’s doctor is the best one to advise you on a healthy weight range for your baby.
How, when, and what to feed a baby are top worries of every parent — but there’s good news: Most babies are pretty good judges of when they’re hungry and when they’re full — and they’ll let you know it.
You just need to present them with the right choices at the right time and pay attention to their cues. If you have any questions or concerns, your pediatrician is there to help you along the way.
Tips for the First Year
Eat, sleep, pee, poop, repeat. Those are the highlights in a day of the life of a brand new baby.
And if you’re a new parent, it’s the eating part that may be the source of many of your questions and worries. How many ounces should your baby take? Do you wake a sleeping baby to eat? Why do they seem hungry all the time? When can your child start solids?
Questions abound — and, despite Grandma’s insistence, the answers have changed since you were a tot. It’s now recommended that newborns, even formula-fed ones, eat on demand (consider it good preparation for the teenage years) and that babies wait to start solid foods until they’re 4 to 6 months old.
On day one of life, your baby’s stomach is the size of a marble and can only hold 1 to 1. 4 teaspoons of liquid at a time. As your baby gets older, their stomach stretches and grows.
4 teaspoons of liquid at a time. As your baby gets older, their stomach stretches and grows.
It’s hard (or impossible, really) to know how much milk your baby is taking in while breastfeeding. But if you’re bottle feeding due to any number of valid reasons, it’s a bit easier to measure.
Here, from the American Academy of Pediatrics (AAP), a typical feeding schedule for bottle-fed babies.
| Age | Ounces per feeding | Solid foods |
|---|---|---|
| Up to 2 weeks of life | .5 oz. in the first days, then 1–3 oz. | No |
| 2 weeks to 2 months | 2–4 oz. | No |
| 2–4 months | 4-6 oz. | No |
| 4–6 months | 4–8 oz. | Possibly, if your baby can hold their head up and is at least 13 pounds. But you don’t need to introduce solid foods yet. |
| 6–12 months | 8 oz. | Yes. Start with soft foods, like one-grain cereals and pureed vegetables, meats, and fruits, progressing to mashed and well-chopped finger foods. Give your baby one new food at a time. Continue supplementing with breast or formula feedings. Give your baby one new food at a time. Continue supplementing with breast or formula feedings. |
Every baby is unique — but one thing that’s pretty consistent is that breastfed babies eat more frequently than bottle-fed ones. That’s because breast milk is easily digested and empties from the stomach a lot quicker than formula.
Breastfed babies
There’s no rest for the weary. According to La Leche League International, you should begin nursing your baby within 1 hour of birth and provide about 8 to 12 feedings daily in the first few weeks of life (yeah, we’re exhausted for you).
At first, it’s important not to let your baby go more than 4 hours without feeding. You’ll likely need to wake them up if necessary, at least until breastfeeding is well established and they’re gaining weight appropriately.
As your baby grows and your milk supply amps up, your baby will be able to take in more milk in less time at one feeding. That’s when you might start to notice a more predictable pattern.
- 1 to 3 months: Your baby will feed 7 to 9 times per 24 hours.
- 3 months: Feedings take place 6 to 8 times in 24 hours.
- 6 months: Your baby will feed around 6 times a day.
- 12 months: Nursing may drop to about 4 times a day. The introduction of solids at about 6 months helps to fuel your baby’s additional nutritional needs.
Keep in mind that this pattern is just one example. Different babies have different paces and preferences, along with other factors that influence the frequency of feedings.
Bottle-fed babies
Like breastfed babies, bottle-fed newborns should eat on demand. On average, that’s about every 2 to 3 hours. A typical feeding schedule may look like this:
- Newborn: every 2 to 3 hours
- At 2 months: every 3 to 4 hours
- At 4 to 6 months: every 4 to 5 hours
- At 6+ months: every 4 to 5 hours
For both breastfed and bottle-fed babies
- Don’t give liquids other than formula or breast milk to babies under a year old.
 That includes juices and cow’s milk. They don’t provide the right (if any) nutrients and can be upsetting to your baby’s tummy. Water can be introduced around 6 months when you start offering a cup.
That includes juices and cow’s milk. They don’t provide the right (if any) nutrients and can be upsetting to your baby’s tummy. Water can be introduced around 6 months when you start offering a cup. - Don’t add baby cereal to a bottle.
- It can create a choking hazard.
- A baby’s digestive system isn’t mature enough to handle cereal until about 4 to 6 months of age.
- You could overfeed your baby.
- Don’t give your baby any form of honey until after their first birthday. Honey can be dangerous for a baby, occasionally causing what’s called infant botulism.
- Do adjust your expectations based on your baby and their unique needs. Premature babies are likely to follow feeding patterns according to their adjusted age. If your baby has challenges like reflux or failure to thrive, you may need to work with your doctor on the appropriate feeding schedule and amount they should be eating.
Schedules are the holy grail of every parent. Your child will naturally start to fall into a feeding pattern as their tummy grows and they can take in more breast milk or formula at one sitting. This may begin to happen between 2 and 4 months of age.
This may begin to happen between 2 and 4 months of age.
For now, though, focus on learning your baby’s hunger cues, such as:
- rooting around your chest, looking for a nipple.
- putting their fist in their mouth
- smacking or licking their lips
- fussing that can escalate quickly (don’t wait until your baby’s hangry to feed them)
Once your baby is a few months old, you may be able to introduce a sleep/feed schedule that works for you.
Let’s say, for example, your 4-month-old wakes every 5 hours for a feeding. That means if you feed at 9 p.m., your baby wakes around 2 a.m. But if you wake and feed the baby at 11 p.m., just before you go to bed, they may not rouse until 4 a.m., giving you a decent chunk of nighttime winks.
In general, if your baby seems hungry, feed them. Your baby will naturally eat more frequently during growth spurts, which typically occur around 3 weeks, 3 months, and 6 months of age.
Some babies will also “cluster feed,” meaning they’ll feed more frequently during certain periods and less at others. For example, your baby may cluster feed during the late afternoon and evening and then sleep longer at night (yay!). This is more common in breastfed babies than bottle fed babies.
For example, your baby may cluster feed during the late afternoon and evening and then sleep longer at night (yay!). This is more common in breastfed babies than bottle fed babies.
Worried about overfeeding? While this isn’t really possible to do with an exclusively breastfed baby, you can overfeed a baby who’s taking a bottle — especially if they’re sucking on the bottle for comfort. Follow their hunger cues, but talk to your pediatrician if you’re worried your little one may be overeating.
Your baby is probably ready for solids if they’re 4 to 6 months old and:
- have good head control
- seem interested in what you’re eating
- reach for food
- weigh 13 or more pounds
Which food to start with? The AAP now says it doesn’t really matter much in what order you introduce foods. The only real rule: Stick with one food for 3 to 5 days before offering another. If there’s an allergic reaction (rash, diarrhea, vomiting are common first signs), you’ll know which food is causing it.
As your baby grows, move from pureed baby food to ones that have more texture (for example, mashed banana, scrambled egg, or well-cooked, chopped pasta). This generally happens around 8 to 10 months of age.
Your supermarket offers a variety of baby food products, but if you want to make your own, keep it sugar and salt free. Additionally, at this stage, don’t feed your baby anything that could be a choking hazard, including:
- hard foods, such as popcorn or nuts
- hard, fresh fruits, like apples; cook to soften or chop into very small pieces
- any meat that isn’t well cooked and very well chopped (this includes hot dogs)
- cheese cubes
- peanut butter (though talk to your pediatrician about this one — and the benefits of introducing diluted peanut butter before the age of 1)
As your baby nears their first birthday, they should be eating a variety of foods and taking in about 4 ounces of solids at each meal. Continue to offer breast milk or formula. By 8 months, babies are drinking about 30 ounces a day.
By 8 months, babies are drinking about 30 ounces a day.
Oh yeah, and buy some stock in a company that makes stain-fighting laundry detergent. It’ll pay for college.
Babies aren’t cookie cutter. Some will gain weight easily, while others will have problems. Things that can affect a baby’s weight gain include:
- having a birth defect like a cleft lip or palate, which creates problems feeding
- having a milk protein intolerance
- being premature
- being fed with a bottle versus the breast
A 2012 study of more than 1,800 babies found that the infants who were fed with a bottle — regardless of whether the bottle contained breast milk or formula — gained more weight in the first year than babies who nursed exclusively.
Your baby’s doctor is the best one to advise you on a healthy weight range for your baby.
How, when, and what to feed a baby are top worries of every parent — but there’s good news: Most babies are pretty good judges of when they’re hungry and when they’re full — and they’ll let you know it.
You just need to present them with the right choices at the right time and pay attention to their cues. If you have any questions or concerns, your pediatrician is there to help you along the way.
Various breastfeeding positions
Try different breastfeeding positions to find the one that works best for you and your baby. You can see the options in our selection of photos
Share this information
There is no right or wrong way to hold the baby while
feeding, and mom and baby are sure to find their favorite position.
It is important that both you and your child feel comfortable. 1.2 It's good to learn a few different breastfeeding positions and techniques because life's circumstances often require us to be flexible, especially as your baby gets older and you start to leave the house more often.
Whatever position you choose to breastfeed your baby, remember a few simple rules.
- Prepare everything you need before feeding, including drinks, food, mobile phone, TV remote control, book or magazine. And do not forget to go to the toilet - the feeding process can take a long time!
- Make sure your baby is comfortable. Whichever position you choose, it's important to keep your baby strong, level, and provide good support for their head, neck, and spine.
- You should also be comfortable. Don't stress. If necessary, use pillows of different sizes or rolls of towels to support your back or arms.
- Make sure your baby is latching on correctly. Proper grip is the key to comfort when breastfeeding.
- If your baby does not latch on well or you experience pain while feeding, contact a lactation consultant for help. The specialist will also be able to show you how to hold your baby more comfortably.
1. Relaxed feeding or reclining position
The relaxed feeding position, also known as biological feeding, 1 is often the first position for most mothers.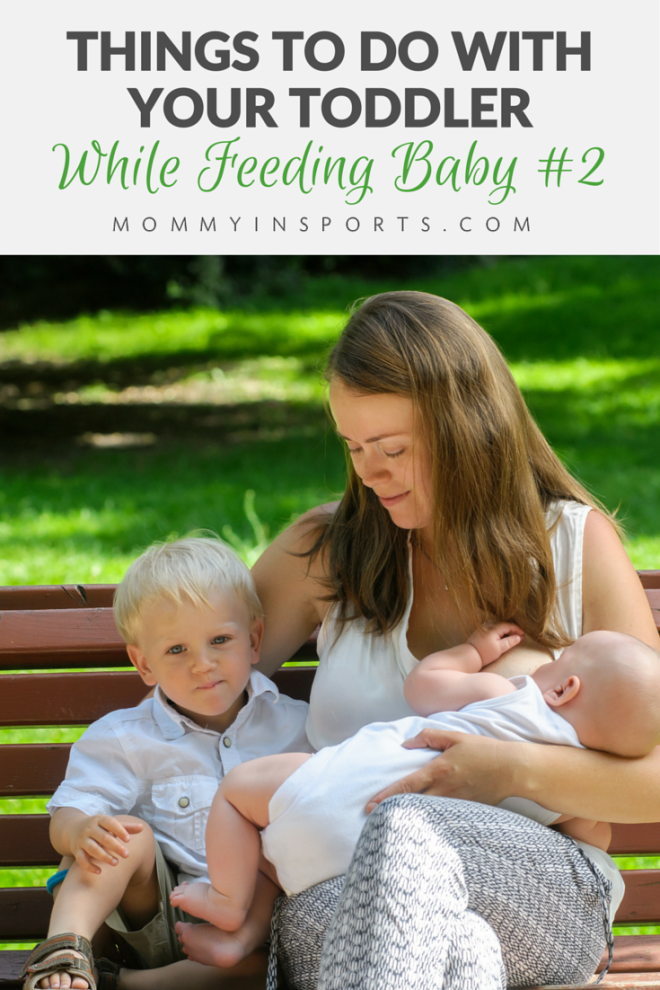 If, immediately after birth, the baby is placed on the mother’s chest or stomach, normally, he instinctively reaches for the breast and tries to grab the nipple. This phenomenon is known as the breast seeking reflex. Skin-to-skin contact stimulates the infant's feeding instinct, and gravity helps him to latch onto the breast and maintain balance.
If, immediately after birth, the baby is placed on the mother’s chest or stomach, normally, he instinctively reaches for the breast and tries to grab the nipple. This phenomenon is known as the breast seeking reflex. Skin-to-skin contact stimulates the infant's feeding instinct, and gravity helps him to latch onto the breast and maintain balance.
But it's not just newborns that can be fed in the reclining position - this position is great for babies of all ages. It can be especially helpful if your baby does not latch well in other positions or does not like to be touched during feeding, and also if you have too much milk flow or too large breasts. Isabelle, a mother from the UK, shares her experience: “I had large breasts, and the baby was born small - 2.7 kg, so it was not easy to find a comfortable position at first. After a few weeks, it became clear that there was no “correct” posture for me. As a result, I most often fed lying down, putting the baby on my chest. ”
It is more convenient to feed not lying flat on your back, but half-sitting, leaning on pillows. So you will have a back support and you will be able to watch the baby during feeding.
So you will have a back support and you will be able to watch the baby during feeding.
2. Cradle position
This is the classic
first thought of breastfeeding. Mom sits straight
, and the baby lies on her side on her arm, pressing his stomach against her stomach. 3 Although this is a very popular position, it is not always easy to master with newborns because it gives the baby less support. Try putting a pillow under your back, and put a special breastfeeding pillow on your knees and lean on it with your hands. So you can more reliably support the child, without overstraining your back and shoulders. Just make sure that the baby does not lie too high on the pillow for feeding. The breast should remain at a natural level so that the baby can grab it without effort, otherwise sore nipples cannot be avoided.
“I breastfed in the cradle position because it suited me perfectly! It was comfortable and I loved just sitting and looking at my little one,” recalls Rachel, a mother of two from Italy.
3. Cross Cradle
This breastfeeding position looks almost the same as Cradle, but the baby is on the other arm. 3 This gives your baby support around the neck and shoulders so he can tilt his head to latch on. This position is great for breastfeeding newborns and small babies, as well as for babies who do not latch well. Since the baby lies completely on the other hand, it becomes easier to control his position and you can adjust the chest with your free hand.
Julie, a UK mother of two, finds this position very practical: “I usually breastfeed my youngest in the cross cradle position. So I have a free second hand, and I can take care of an older baby at the same time. ”
Do not hold the baby's head at first, otherwise you may inadvertently press his chin against his chest. Because of this, the child will not be able to take the breast deeply, because the nipple will rest against the base of the tongue, and not against the palate, which will lead to inflammation of the nipples. As the child grows, this position becomes more comfortable, and he can rest his head on your palm (as shown in the photo above).
As the child grows, this position becomes more comfortable, and he can rest his head on your palm (as shown in the photo above).
4. Underarm breastfeeding
In this position, also known as the “ball grip”, the mother sits with the baby lying along her arm at the side, legs towards the back of the chair (or any other seat). 3 Another comfortable position for newborn breastfeeding, you can give your baby good support, full control of his position and a good view of his face. And the baby feels safe in close contact with the mother's body. This position is especially good for those who have had a caesarean section or a premature birth, as well as mothers of twins and women with large breasts.
“When I breastfed my first daughter, I had very large K-sized breasts—twice the size of her head,” recalls Amy, an Australian mother of two. - I put rolls of towels under each breast, because they were very heavy, and fed my daughter in a pose from under the arm, but only sitting straighter so as not to crush her. This position was also convenient because I had a caesarean section and could not put the baby on my stomach.”
This position was also convenient because I had a caesarean section and could not put the baby on my stomach.”
5. Side-lying position
The side-lying position is ideal for a relaxed
nighttime feeding in bed or on the couch. If you had a
caesarean section or ruptures during childbirth, this position may be more comfortable than sitting down. 3 In this position, mother and baby lie side by side, tummy to tummy.
“It was difficult for me to sit during endless night feedings, firstly because of the caesarean section, and secondly because of lack of sleep,” recalls Francesca, a mother from the UK. “And then I discovered that you can feed your baby lying on your side and rest at the same time.”
“Because of the short tongue frenulum, Maisie could only properly latch on to her breasts while lying on her side. The lactation consultant showed me how it's done. In this position, the flow of milk was optimal for my daughter, and it was easier for her to keep the nipple in her mouth. As she got older, she became much better at grabbing her breasts in normal positions,” says Sarah, mother of two from Australia.
As she got older, she became much better at grabbing her breasts in normal positions,” says Sarah, mother of two from Australia.
6. Relaxed breastfeeding after caesarean section
If you can't find a comfortable position for breastfeeding after caesarean section, 3 try holding the baby on your shoulder in a reclining position – this does not stress the postoperative suture and allows you to breastfeed your baby comfortably. You can also try side feeding.
7. Sitting upright breastfeeding or “koala pose”
When breastfeeding in an upright position or “koala pose”, the baby sits with a straight back and a raised head on the mother's hip. 4 This position can be tried even with a newborn if it is well supported, but it is especially convenient for feeding a grown child who can already sit up by himself. The upright sitting position, or “koala pose,” is great for toddlers who suffer from reflux or ear infections and feel better sitting. In addition, this pose may be suitable for children with a shortened frenulum of the tongue or reduced muscle tone.
In addition, this pose may be suitable for children with a shortened frenulum of the tongue or reduced muscle tone.
“When my daughter got a little older, I would often feed her in an upright position, which was more comfortable for both of us, and I could still hold her close,” recalls Peggy, a mother from Switzerland. “Besides, it was possible to discreetly breastfeed her in public places.”
8. Overhanging position
In this position, the baby lies on his back, and the mother bends over him
on all fours so that the nipple falls directly into his mouth. 4 Some moms say this breastfeeding position is good to use occasionally for mastitis, when touching the breasts is especially unpleasant. Some say that this breastfeeding position helps with blockage of the milk ducts, although there is no scientific evidence for this yet. You can also feed in the “overhanging” position while sitting, kneeling over the baby on a bed or sofa, as well as reclining on your stomach with support on your elbows.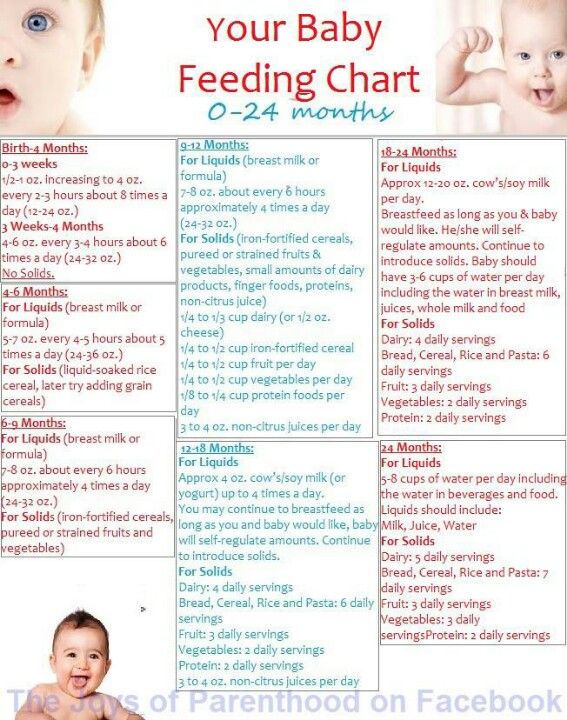 Pillows of various sizes that you can lean on will help you avoid back and shoulder strain.
Pillows of various sizes that you can lean on will help you avoid back and shoulder strain.
“I have breastfed several times in the 'overhang' position for clogged milk ducts when no other means of dissolving the blockage worked. And this pose seems to have helped. I think it's because of gravity, and also because the breasts were at a completely different angle than with normal feeding, and my daughter sucked her differently, ”says Ellie, a mother of two from the UK.
Feeding in the "overhanging" position is unlikely to be practiced regularly, but in some cases this position may be useful.
“I used to breastfeed in the overhang position when my baby was having trouble latch-on,” says Lorna, mother of two in the UK. - This, of course, is not the most convenient way, but then I was ready for anything, if only he could capture the chest. We succeeded and have been breastfeeding for eight months now!”
9. Breastfeeding in a sling or in a sling
Breastfeeding in a sling takes some practice, but it can be used to go out, look after older children, or even do a little household chores.
The sling is also useful if the baby does not like to lie down or is often attached to the breast. Lindsey, a mother of two in the US, notes: “I used the carrier frequently for both of my children. When we were out, I tied the sarong around my neck and covered the carrier with it. Under such a cape, the baby can eat as much as he wants until he falls asleep.
This breastfeeding position is best when the baby is already good at breastfeeding and can hold his head up by himself. Any slings are suitable for breastfeeding, including elastic and rings, as well as carrying bags. Whatever option you choose, the main thing is that you can always see the face of the child, and his chin does not rest against his chest.
10. Double hand-held breastfeeding
Double hand-held breastfeeding (or “double-ball grab”) is great for mothers of twins—you can breastfeed both at the same time and keep your arms relatively free. 4 When feeding in this position, it is advisable to use a special pillow for breastfeeding twins, especially at first. It will provide extra support and help keep both babies in the correct position, as well as reduce the burden on the abdomen if you had a caesarean section. In addition, the hands are freer, and if necessary, you can deal with one child without interfering with the second.
It will provide extra support and help keep both babies in the correct position, as well as reduce the burden on the abdomen if you had a caesarean section. In addition, the hands are freer, and if necessary, you can deal with one child without interfering with the second.
“My twins were born very tiny and had to be fed every two hours at any time of the day or night. Very soon it became clear: if I want to do anything besides feeding, I need to feed them both at the same time, - says Emma, mother of two children from the UK. “I breastfed them two by hand using a breastfeeding pillow.”
Other good positions for breastfeeding twins are two criss-cross cradles, one baby in the cradle and the other close at hand, reclining feeding, or sitting upright (one baby on one side, the other on the other).
11. Breastfeeding in the "hand-supported" or "dancer's hand" position
muscle tone (which is typical for premature babies, children suffering from various diseases or Down syndrome), try supporting his head and your chest at the same time. 4 Grasp your chest with your palm underneath so that your thumb is on one side and all the others are on the other. Move your hand slightly forward so that your thumb and forefinger form a "U" just in front of your chest. With the other three fingers, continue to support the chest. With your thumb and forefinger, hold the baby's head while feeding so that his chin rests on the part of the palm between them, your thumb gently holds the baby on one cheek, and your index finger on the other. So the baby gets excellent support, and you can control his position and see if he is holding his breast.
4 Grasp your chest with your palm underneath so that your thumb is on one side and all the others are on the other. Move your hand slightly forward so that your thumb and forefinger form a "U" just in front of your chest. With the other three fingers, continue to support the chest. With your thumb and forefinger, hold the baby's head while feeding so that his chin rests on the part of the palm between them, your thumb gently holds the baby on one cheek, and your index finger on the other. So the baby gets excellent support, and you can control his position and see if he is holding his breast.
Literature
1 Colson SD et al. Optimal positions for the release of primitive neonatal reflexes stimulating breastfeeding. Early Hum Dev . 2008;84(7):441-449. - Colson S.D. et al., "Optimal Positions for Provoking Primitive Innate Reflexes to Induce Breastfeeding." Early Hume Dev. 2008;84(7):441-449.
2 UNICEF UK BFHI [ Internet ]. Off to the best start ; 2015 [ cited 2018 Feb ]. - UNICEF UK, Baby-Friendly Hospital Initiative, Start the Best You Can [Internet]. 2015 [cited February 2018].
Off to the best start ; 2015 [ cited 2018 Feb ]. - UNICEF UK, Baby-Friendly Hospital Initiative, Start the Best You Can [Internet]. 2015 [cited February 2018].
3 Cadwell K. Latching - On and Suckling of the Healthy Term Neonate: Breastfeeding Assessment. J Midwifery & Women's Health. 2007;52(6):638-642. — Cadwell, K., "Latching and sucking in healthy newborns: evaluation of breastfeeding." F Midwifery Women Health. 2007;52(6):638-642.
4 Wambach K, Riordan J, editors. Breastfeeding and human lactation. Jones & Bartlett Learning ; 2014. 966 p . - Wambach K., Riordan J., "Breastfeeding and female lactation". Burlington, MA: Publishing House Jones & Bartlett Learning ; 2014. Pp. 966.
Pp. 966.
15 breastfeeding rules
15 breastfeeding rules
(based on WHO-UNICEF recommendations)
years of life.
Successful breastfeeding requires the following rules:
- Early breastfeeding within the first hour after birth.
- Eliminate pre-breastfeeding from a bottle or other means to avoid unwanted imprinting and not set the baby on any other feeding than breastfeeding.
- Joint maintenance of mother and child in one room.
- The correct position of the baby at the breast , which allows the mother to avoid many problems and complications with the breast. This should be taught to the mother in the maternity hospital or later with the help of a specialist and learn this on purpose.
- Feeding on demand . It is necessary to apply it to the chest for any reason, giving the opportunity to suckle the breast when he wants and how much he wants.
 This is very important not only for the saturation of the child, but also for his feeling of comfort and security. There is nothing wrong with the fact that the baby once again attaches to the breast. There is no harm in this, only gain.
This is very important not only for the saturation of the child, but also for his feeling of comfort and security. There is nothing wrong with the fact that the baby once again attaches to the breast. There is no harm in this, only gain. - The duration of feeding is regulated by the child . You should not tear the baby from the breast before he releases the nipple.
- Night feedings of the baby provide stable lactation and protect the woman from milk stagnation, the next pregnancy. In addition, night milk is considered the most complete.
- No additional soldering or introduction of any liquids . If the child is thirsty, it should be applied to the breast more often.
- No teats or bottle feeding . If necessary, supplementation should be given only from a cup, from a spoon or from a pipette.
- Don't transfer your baby to the second breast before he has suckled the first breast .
 If the mother rushes to offer the baby a second breast, he will not get enough late milk rich in fats. In addition, it can lead to stagnation of milk.
If the mother rushes to offer the baby a second breast, he will not get enough late milk rich in fats. In addition, it can lead to stagnation of milk. - Avoid washing nipples before and after feeding . Frequent breast washing removes the protective layer of fat from the areola and nipple, leading to cracking. The chest should be washed no more than once a day during a hygienic shower. If a woman takes a shower less often, then in this case it should be wiped before feeding with a damp cloth without using soap.
- Refusal of frequent control weighings of the child . This procedure does not provide objective information about the nutritional value of the infant. It only irritates the mother, leads to a decrease in lactation and unreasonable introduction of supplementary feeding. Objective figures are given by weighing 1-2 times a week.
- Exclusion of extra milk expression . With properly organized breastfeeding, milk is produced exactly as much as the baby needs, so there is no need to express after each feeding.