How do i feed my baby cereal
How to Get Started – The Baby's Brew
I will always remember feeding each of my babies their first foods. After months of only breastfeeding and bottles, my husband and I couldn’t wait to introduce the next milestone to each of our babies. But with the first baby at least, there was also apprehension. Our pediatrician had recommended we start with a single-grain baby cereal such as rice cereal, but I didn’t know which one to get and I wanted to make sure I fed my baby the right way!
So to get you started off on the right food with baby feeding 101, I’ve put together this guide to giving your baby cereal for the first time. And it will only get more exciting as you introduce other foods to your little one.
Choosing a First Baby CerealBefore you actually feed your baby, you have to choose what you want to give them from the array of cereals and other options available.
Most parents reach for the rice cereal to give their baby as their first food. I know I did as a new mom! It’s an easy choice and one that doctors suggest due to its benefits. It's easy to such as its digest, won’t trigger an allergic reaction and is tolerated well by babies who’ve only been fed breastmilk or formula. It’s also iron-fortified, which babies need as their iron stores start to deplete around 6 months of age.
Though rice cereal has traditionally been suggested as the best first food for your baby, even many doctors may still give this recommendation, it has gotten a bit of a bad rap in recent years due to the arsenic that’s found in rice - causing parents to look at other options. (This article from Healthy Children explains how you can ensure rice cereal can be used in a healthy diet for your baby.)
If you do choose rice cereal, you’ll want to start introducing other solids to your baby shortly so that’s not all that they are getting, as recommended by the FDA.
Fortunately, if you want to skip the rice cereal completely, you can! There is no need to feel like this is the only first food for your baby. Many experts share that any iron-fortified single-grain baby cereal is a great choice, such as baby oatmeal or barley. You can even start with other pureed foods which we discuss later on in this article.
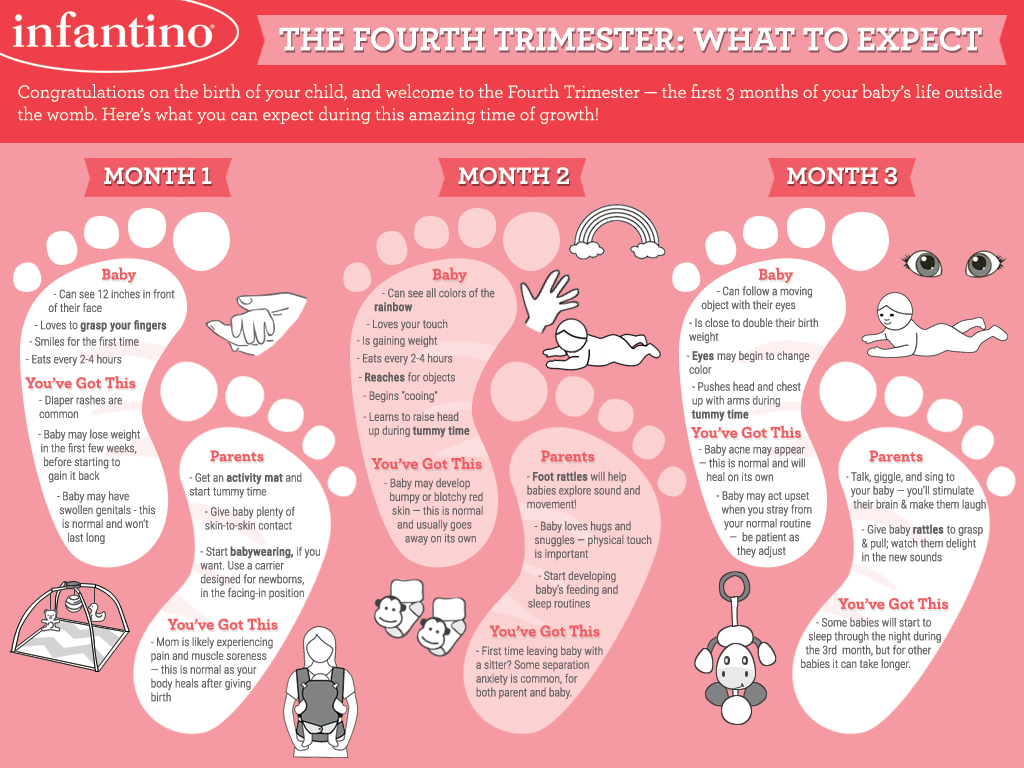
When to Start Feeding Your Baby CerealSeveral years ago the recommendation was that parents could feed their babies at four months if they showed readiness signs. But medical advice evolves and this is a guideline that medical experts have changed to give babies the healthiest start possible.
It’s now suggested that it’s best to wait til closer to your baby’s ½ birthday to introduce solids, especially if he is breastfed. There’s really no reason to rush it!
But it’s not just age you want to pay attention to as we know that all babies develop at different rates.![]()
Here are signs to look for that will let you know your baby is ready for solid foods:
- able to sit up supported in a high chair
- has proper head control
- no more tongue thrust
- eager to take a spoon
- are interested in the food that you are eating
If your baby isn’t yet showing these signs, you’ll want to wait a bit longer before starting baby cereal or other solid foods. No need to worry - all babies are ready in their own time! Your baby will continue to get the nutrition they need from their breastmilk or formula so you don’t need to be concerned that they are missing out on important nutrients. If you do have concerns, it’s always best to talk to your pediatrician.
Can you give your baby cereal in a bottle?Even though your well-meaning grandma may suggest that you mix cereal into your baby’s bottle to help fill them up so they can sleep better, this practice is actually not safe according to the CDC. In fact, they share that it won’t help your baby sleep better anyway. This practice puts your baby at risk for choking or overfeeding and also may encourage parents to start solid foods long before they are ready.
In fact, they share that it won’t help your baby sleep better anyway. This practice puts your baby at risk for choking or overfeeding and also may encourage parents to start solid foods long before they are ready.
Instead, follow the guideline to not feed your baby solid foods until he or she is at least 5-6 months in age and watch for the other readiness signs mentioned above. At this point you can feed your baby with a spoon and introduce finger foods as they are ready.
RELATED: Starting Solid Foods With Your Baby
How to Introduce Cereal to Your BabyBreastmilk and formula will continue to be your baby’s primary source of nutrition until the age of one, but cereal is a great way to get them started with supplemental nutrition and transition them to solid foods. So how do you go about it?
Here are the steps to follow to give your baby her first single-grain cereal:
- Make sure they meet the recommended readiness signs. This will not only make for a safe feeding experience for your little guy or gal, but it will also be a lot more enjoyable for you.

- Plan to feed your little one after they’ve had a full feeding of breastmilk or formula. This way their tummy will mostly be full which means they’ll likely be happy to try a little cereal. (If you try to introduce solids to a hungry baby they will most likely be uncooperative!) Initially you’ll only feed your baby once per day, and it’s up to you when you want that time to be. We recommend choosing a time that your baby is usually in good spirits!
- Follow the directions on the label of your chosen baby cereal. You don’t need much to start! 1 tablespoon of cereal mixed with breastmilk or formula until it’s a runny consistency will be plenty for those first couple of feedings. If your baby is used to drinking warm milk or formula, you’ll want to use that same temperature of milk to mix with your baby’s food. (This is why we love the Baby’s Brew portable bottle warmer...you can choose your baby’s milk temperature with the push of a button!)
- Be sure your baby is sitting upright.
 Ideally this would be in a highchair, but they could also be sitting on your lap. You’ll want them to be wearing a bib as a lot your little one’s food won’t make it into their mouth initially.
Ideally this would be in a highchair, but they could also be sitting on your lap. You’ll want them to be wearing a bib as a lot your little one’s food won’t make it into their mouth initially. - Use an infant spoon to feed your baby. Do your best to get the spoon into their open mouth, but just know it’s going to be a bit messy at first as they get the hang of what’s going on. It won’t be long before they are opening wide at mealtime!
- Watch for cues from your baby that show that they are full (or are just are no longer interested). If your baby turns their head, is fussy or won’t open their mouth to eat, it’s time to be “all done!”
And that’s it! You can do another feeding the next day (or you can just do every other day) with the same type of cereal. Be sure to wait three - five days before introducing another food so you can keep an eye out for any allergic reactions. This is the recommendation given by the CDC.
After a couple weeks to a month of successfully feeding your baby once per day you can move to twice per day.
Some parents choose to start with a different food or may take baby cereal out of their little one’s diet altogether. Starting with other pureed foods instead is totally fine and may even work better for some babies. WebMD shares that both pureed vegetables or fruits are good starter foods and that there’s no rule saying that baby cereals must be first.
Some great first foods, if you want to skip the cereal route, include:
- Avocados
- Bananas
- Blended Red Meat (great source of iron)
- Squash
- Sweet Potatoes
- Pears
Just remember that these all need to be pureed and made into a runny consistency that’s easy for your baby to eat. Mixing with your baby’s warmed breastmilk or formula will help to bring this to a consistency that your baby can manage. You’ll also want to avoid giving your baby any of the top allergen foods such as the ones listed here unless you’ve been given different advice from your doctor. These are best introduced when your baby gets a little older.
These are best introduced when your baby gets a little older.
Still not sure which food to start with? It can be a bit overwhelming! This is a great conversation to have with your doctor before your baby turns 6 months and they can help guide you on what would be the best option. Whatever you choose, it is sure to be an exciting time for your family as your little guy or gal begins his journey of eating "real" food!
When, What, and How to Introduce Solid Foods | Nutrition
For more information about how to know if your baby is ready to starting eating foods, what first foods to offer, and what to expect, watch these videos from 1,000 Days.
The Dietary Guidelines for Americans and the American Academy of Pediatrics recommend children be introduced to foods other than breast milk or infant formula when they are about 6 months old. Introducing foods before 4 months old is not recommended. Every child is different. How do you know if your child is ready for foods other than breast milk or infant formula? You can look for these signs that your child is developmentally ready.
Your child:
- Sits up alone or with support.
- Is able to control head and neck.
- Opens the mouth when food is offered.
- Swallows food rather than pushes it back out onto the chin.
- Brings objects to the mouth.
- Tries to grasp small objects, such as toys or food.
- Transfers food from the front to the back of the tongue to swallow.
What Foods Should I Introduce to My Child First?
The American Academy of Pediatrics says that for most children, you do not need to give foods in a certain order. Your child can begin eating solid foods at about 6 months old. By the time he or she is 7 or 8 months old, your child can eat a variety of foods from different food groups. These foods include infant cereals, meat or other proteins, fruits, vegetables, grains, yogurts and cheeses, and more.
If your child is eating infant cereals, it is important to offer a variety of fortifiedalert icon infant cereals such as oat, barley, and multi-grain instead of only rice cereal. Only providing infant rice cereal is not recommended by the Food and Drug Administration because there is a risk for children to be exposed to arsenic. Visit the U.S. Food & Drug Administrationexternal icon to learn more.
Only providing infant rice cereal is not recommended by the Food and Drug Administration because there is a risk for children to be exposed to arsenic. Visit the U.S. Food & Drug Administrationexternal icon to learn more.
How Should I Introduce My Child to Foods?
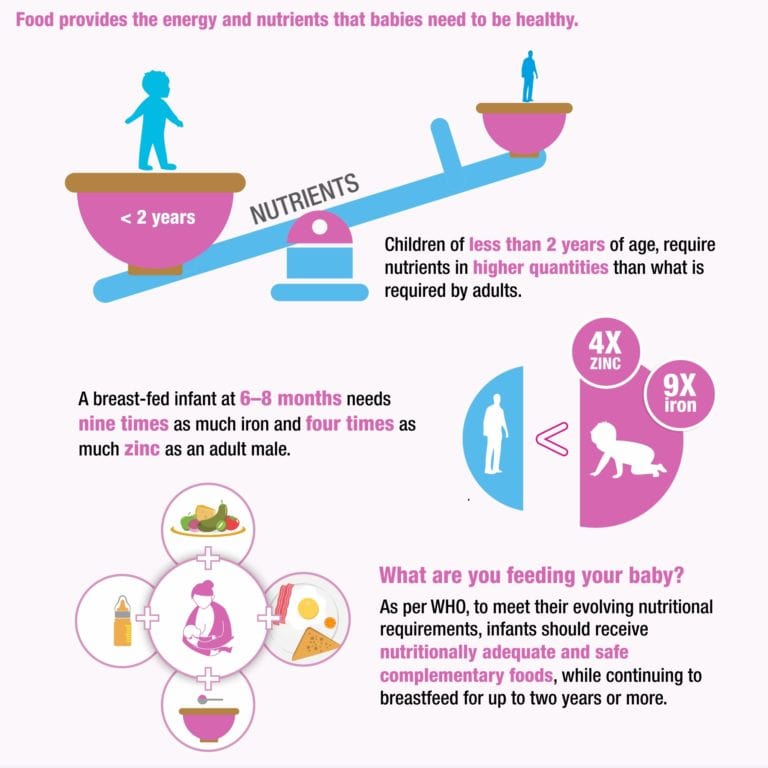
Your child needs certain vitamins and minerals to grow healthy and strong.
Now that your child is starting to eat food, be sure to choose foods that give your child all the vitamins and minerals they need.
Click here to learn more about some of these vitamins & minerals.
Let your child try one single-ingredient food at a time at first. This helps you see if your child has any problems with that food, such as food allergies. Wait 3 to 5 days between each new food. Before you know it, your child will be on his or her way to eating and enjoying lots of new foods.
Introduce potentially allergenic foods when other foods are introduced.
Potentially allergenic foods include cow’s milk products, eggs, fish, shellfish, tree nuts, peanuts, wheat, soy, and sesame.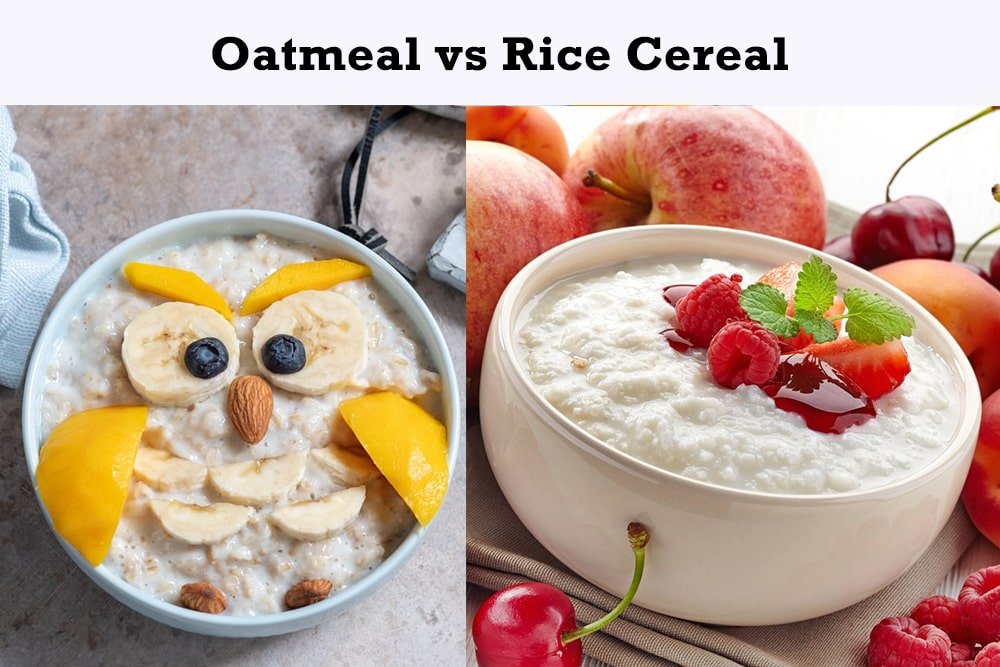 Drinking cow’s milk or fortified soy beverages is not recommended until your child is older than 12 months, but other cow’s milk products, such as yogurt, can be introduced before 12 months. If your child has severe eczema and/or egg allergy, talk with your child’s doctor or nurse about when and how to safely introduce foods with peanuts.
Drinking cow’s milk or fortified soy beverages is not recommended until your child is older than 12 months, but other cow’s milk products, such as yogurt, can be introduced before 12 months. If your child has severe eczema and/or egg allergy, talk with your child’s doctor or nurse about when and how to safely introduce foods with peanuts.
How Should I Prepare Food for My Child to Eat?
At first, it’s easier for your child to eat foods that are mashed, pureed, or strained and very smooth in texture. It can take time for your child to adjust to new food textures. Your child might cough, gag, or spit up. As your baby’s oral skills develop, thicker and lumpier foods can be introduced.
Some foods are potential choking hazards, so it is important to feed your child foods that are the right texture for his or her development. To help prevent choking, prepare foods that can be easily dissolved with saliva and do not require chewing. Feed small portions and encourage your baby to eat slowly. Always watch your child while he or she is eating.
Always watch your child while he or she is eating.
Here are some tips for preparing foods:
- Mix cereals and mashed cooked grains with breast milk, formula, or water to make it smooth and easy for your baby to swallow.
- Mash or puree vegetables, fruits and other foods until they are smooth.
- Hard fruits and vegetables, like apples and carrots, usually need to be cooked so they can be easily mashed or pureed.
- Cook food until it is soft enough to easily mash with a fork.
- Remove all fat, skin, and bones from poultry, meat, and fish, before cooking.
- Remove seeds and hard pits from fruit, and then cut the fruit into small pieces.
- Cut soft food into small pieces or thin slices.
- Cut cylindrical foods like hot dogs, sausage and string cheese into short thin strips instead of round pieces that could get stuck in the airway.
- Cut small spherical foods like grapes, cherries, berries and tomatoes into small pieces.

- Cook and finely grind or mash whole-grain kernels of wheat, barley, rice, and other grains.
Learn more about potential choking hazards and how to prevent your child from choking.
Top of Page
Antibiotics and breastfeeding | Mamovediya
Of course, during breastfeeding, a nursing mother should avoid taking medications, and even more so antibiotics. But, there are situations when a nursing mother needs antibiotic treatment.
In this case, the question arises, is it possible to breastfeed the baby?
Most pediatricians are of the opinion that it is possible, but the main condition for this should be the compatibility of antibiotics with breastfeeding.
How do you know if your antibiotics are compatible with breastfeeding?
Dr. Hale has developed a guide to help you determine if certain medications are compatible with breastfeeding. Also, the compatibility of a specific drug with breastfeeding can be found in the WHO guide, the online guide E-lactancia and Lactmed.
In most cases, with the right choice of antibiotics, a nursing mother is allowed to breastfeed. When prescribing antibiotics to a nursing mother, the doctor needs to opt for those drugs that will bring the least negative effect on the child's body.
All penicillin and cephalosporin antibiotics have been shown to be acceptable during breastfeeding. That is why, when a doctor prescribes antibiotics to a woman who is breastfeeding, the safety of the drug for the child should be taken into account.
Scientists and physicians have established that only 1-2% of the drugs that the mother takes enter the milk of a nursing mother. Based on this, the likelihood that antibiotics during breastfeeding will harm the baby is quite small, but still it exists. You need to be especially careful with a baby under the age of six months, who is exclusively breastfed.
In order to minimize the side effects of antibiotics for a nursing mother and baby, as well as to avoid negative reactions on the part of the baby's body, the doctor may recommend taking probiotics along with taking antibiotics. Thanks to the intake of probiotics, it is possible to protect the intestinal microflora of the mother and child.
Thanks to the intake of probiotics, it is possible to protect the intestinal microflora of the mother and child.
Today, almost all modern antibiotics in the form of tablets and capsules are safe for breastfeeding. But antibiotics in injections are considered more dangerous for the baby.
The danger of some antibiotics for a child is that these drugs can accumulate in the baby's blood due to the immaturity of their excretory system, as well as a rather weak cleaning ability of the child's blood.
Of course, a nursing mother can take antibiotics only after a doctor's appointment and if there are strict indications for this. Before taking an antibiotic, you must carefully read the instructions for use of the drug.
In the event that the instructions indicate that this antibiotic is possible for a child of the same age as your baby, then such a drug can also be used by a nursing mother.
Taking antibiotics by a nursing mother is best done during feeding or immediately after breastfeeding the baby, because in this way it is possible to avoid the period of maximum concentration in the blood and reduce the negative effect of the drug on the baby.
In the event that the mother's health requires taking antibiotics that are harmful to the baby, then it is better to temporarily interrupt breastfeeding, but at the same time it is necessary to maintain lactation and express regularly.
After taking antibiotics that are dangerous for the baby, breastfeeding can be resumed only one day after the end of the drug.
The most dangerous consequences of taking antibiotics by a nursing mother are the following: the risk of gastrointestinal bleeding in the child, the risk of toxic damage to the bone marrow, growth retardation.
In any case, when taking antibiotics during breastfeeding, there should be regular and careful monitoring of the baby's condition, since the baby may develop diarrhea, a rash on the skin, allergic reactions, increased salivation.
If any negative reaction occurs from the body of the baby, it should be immediately shown to the pediatrician.

The most important thing that a nursing mother should remember when taking antibiotics is that it is necessary to strictly observe the prescribed dosage of the drug, never reduce the dose and not stop taking the drug on her own, even if the symptoms of the disease have noticeably decreased.
Antibiotics can be taken while breastfeeding, but it is very important to use medicines under the supervision of a doctor, follow the dosage and not self-medicate.
Various breastfeeding positions
Try different breastfeeding positions to find the one that works best for you and your baby. You can see the options in our selection of photos
Share this information
There is no right or wrong way to hold the baby while feeding
, and mom and baby are sure to find their favorite position.
It is important that both you and your child feel comfortable. 1.2 It's good to learn a few different breastfeeding positions and techniques because life's circumstances often require us to be flexible, especially as your baby gets older and you start to leave the house more often.
Whatever position you choose to breastfeed your baby, remember a few simple rules.
- Prepare everything you need before feeding, including drinks, food, mobile phone, TV remote control, book or magazine. And do not forget to go to the toilet - the feeding process can take a long time!
- Make sure your baby is comfortable. Whichever position you choose, it's important to keep your baby strong, level, and provide good support for their head, neck, and spine.
- You should also be comfortable. Don't stress. If necessary, use pillows of different sizes or rolls of towels to support your back or arms.
- Make sure your baby is latching on correctly. Proper grip is the key to comfort when breastfeeding.
- If your baby does not latch on well or you experience pain while feeding, contact a lactation consultant for help. The specialist will also be able to show you how to hold your baby more comfortably.
1. Relaxed feeding or reclining position
The relaxed feeding position, also known as biological feeding, 1 is often the first position for most mothers.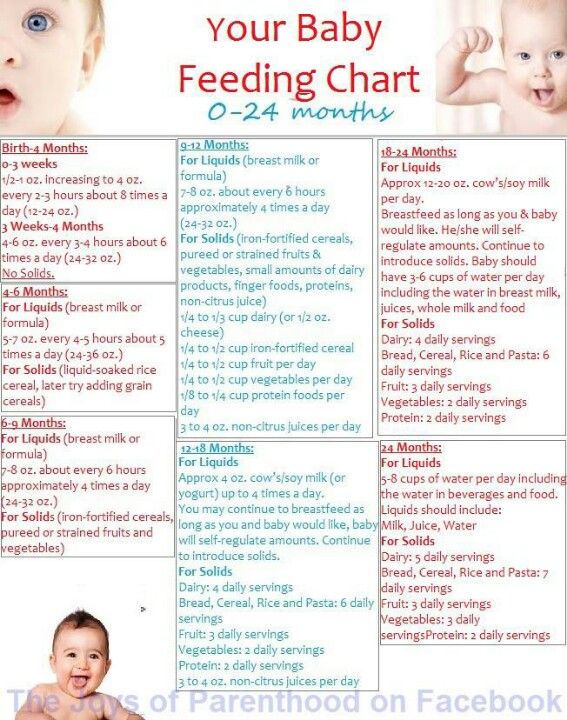 If, immediately after birth, the baby is placed on the mother’s chest or stomach, normally, he instinctively reaches for the breast and tries to grab the nipple. This phenomenon is known as the breast seeking reflex. Skin-to-skin contact stimulates the infant's feeding instinct, and gravity helps him to latch onto the breast and maintain balance.
If, immediately after birth, the baby is placed on the mother’s chest or stomach, normally, he instinctively reaches for the breast and tries to grab the nipple. This phenomenon is known as the breast seeking reflex. Skin-to-skin contact stimulates the infant's feeding instinct, and gravity helps him to latch onto the breast and maintain balance.
But it's not just newborns that can be fed in the reclining position - this position is great for babies of all ages. It can be especially helpful if your baby does not latch well in other positions or does not like to be touched during feeding, and also if you have too much milk flow or too large breasts. Isabelle, a mother from the UK, shares her experience: “I had large breasts, and the baby was born small - 2.7 kg, so it was not easy to find a comfortable position at first. After a few weeks, it became clear that there was no “correct” posture for me. As a result, I most often fed lying down, putting the baby on my chest. ”
It is more convenient to feed not lying flat on your back, but half-sitting, leaning on pillows. So you will have a back support and you will be able to watch the baby during feeding.
So you will have a back support and you will be able to watch the baby during feeding.
2. Cradle position
This is the classic position that comes to mind first when
it comes to breastfeeding. Mom sits straight
, and the baby lies on her side on her arm, pressing his stomach against her stomach. 3 Although this is a very popular position, it is not always easy to master with newborns because it gives the baby less support. Try putting a pillow under your back, and put a special breastfeeding pillow on your knees and lean on it with your hands. So you can more reliably support the child, without overstraining your back and shoulders. Just make sure that the baby does not lie too high on the pillow for feeding. The breast should remain at a natural level so that the baby can grab it without effort, otherwise sore nipples cannot be avoided.
“I breastfed in the cradle position because it suited me perfectly! It was comfortable and I loved just sitting and looking at my little one,” recalls Rachel, a mother of two from Italy.
3. Cross Cradle
This breastfeeding position looks almost exactly like the cradle, but the baby is on the other arm. 3 This gives baby support around the neck and shoulders so he can tilt his head to latch on. This position is great for breastfeeding newborns and small babies, as well as for babies who do not latch well. Since the baby lies completely on the other hand, it becomes easier to control his position and you can adjust the chest with your free hand.
Julie, a UK mother of two, finds this position very practical: “I usually breastfeed my youngest in the cross cradle position. So I have a free second hand, and I can take care of an older baby at the same time. ”
Do not hold the baby's head at first, otherwise you may inadvertently press his chin against his chest. Because of this, the child will not be able to take the breast deeply, because the nipple will rest against the base of the tongue, and not against the palate, which will lead to inflammation of the nipples. As the child grows, this position becomes more comfortable, and he can rest his head on your palm (as shown in the photo above).
As the child grows, this position becomes more comfortable, and he can rest his head on your palm (as shown in the photo above).
4. Underarm breastfeeding
In this position, also known as the “ball grip”, the mother is seated with the baby lying along her arm at the side, legs towards the back of a chair (or any other seat). 3 Another comfortable position for newborn breastfeeding, you can give your baby good support, full control of the position and a good view of his face. And the baby feels safe in close contact with the mother's body. This position is especially good for those who have had a caesarean section or a premature birth, as well as mothers of twins and women with large breasts.
“When I breastfed my first daughter, I had very large K-sized breasts—twice the size of her head,” recalls Amy, an Australian mother of two. - I put rolls of towels under each breast, because they were very heavy, and fed my daughter in a pose from under the arm, but only sitting straighter so as not to crush her. This position was also convenient because I had a caesarean section and could not put the baby on my stomach.”
This position was also convenient because I had a caesarean section and could not put the baby on my stomach.”
5. Side-lying position
The side-lying position is ideal for a relaxed
nighttime feeding in bed or on the couch. If you had a
caesarean section or ruptures during childbirth, this position may be more comfortable than sitting down. 3 In this position, mother and baby lie side by side, tummy to tummy.
“It was difficult for me to sit during endless night feedings, firstly because of the caesarean section, and secondly because of lack of sleep,” recalls Francesca, a mother from the UK. “And then I discovered that you can feed your baby lying on your side and rest at the same time.”
“Because of the short tongue frenulum, Maisie could only properly latch on to her breasts while lying on her side. The lactation consultant showed me how it's done. In this position, the flow of milk was optimal for my daughter, and it was easier for her to keep the nipple in her mouth. As she got older, she became much better at grabbing her breasts in normal positions,” says Sarah, mother of two from Australia.
As she got older, she became much better at grabbing her breasts in normal positions,” says Sarah, mother of two from Australia.
6. Relaxed breastfeeding after caesarean section
If you can't find a comfortable position for breastfeeding after caesarean section, 3 try to hold the baby on the shoulder while reclining - this does not stress the postoperative suture and allows you to breastfeed the baby comfortably. You can also try side feeding.
7. Upright breastfeeding or “koala pose”
When breastfeeding in an upright position or “koala pose”, the baby sits with a straight back and head up on the mother's hip. 4 This position can be tried even with a newborn if it is well supported, but it is especially convenient for feeding an older child who can already sit up by himself. The upright sitting position, or “koala pose,” is great for toddlers who suffer from reflux or ear infections and feel better sitting. In addition, this pose may be suitable for children with a shortened frenulum of the tongue or reduced muscle tone.
“When my daughter got a little older, I would often feed her in an upright position, which was more comfortable for both of us, and I could still hold her close,” recalls Peggy, a mother from Switzerland. “Besides, it was possible to discreetly breastfeed her in public places.”
8. Overhanging position
In this position, the baby lies on his back, and the mother bends over him
on all fours so that the nipple falls directly into his mouth. 4 According to some mothers, this breastfeeding position is good to use from time to time for mastitis, when touching the breast is especially unpleasant. Some say that this breastfeeding position helps with blockage of the milk ducts, although there is no scientific evidence for this yet. You can also feed in the “overhanging” position while sitting, kneeling over the baby on a bed or sofa, as well as reclining on your stomach with support on your elbows. Pillows of various sizes that you can lean on will help you avoid back and shoulder strain.
“I have breastfed several times in the 'overhang' position for clogged milk ducts when no other means of dissolving the blockage worked. And this pose seems to have helped. I think it's because of gravity, and also because the breasts were at a completely different angle than with normal feeding, and my daughter sucked her differently, ”says Ellie, a mother of two from the UK.
Feeding in the "overhanging" position is unlikely to be practiced regularly, but in some cases this position may be useful.
“I used to breastfeed in the overhang position when my baby was having trouble latch-on,” says Lorna, mother of two in the UK. - This, of course, is not the most convenient way, but then I was ready for anything, if only he could capture the chest. We succeeded and have been breastfeeding for eight months now!”
9. Feeding a baby in a sling or “on the fly”
Breastfeeding in a sling takes some practice, but it can be used to go out of the house, look after older children or even do a little household chores.
The sling is also useful if the baby does not like to lie down or is often attached to the breast. Lindsey, a mother of two in the US, notes: “I used the carrier frequently for both of my children. When we were out, I tied the sarong around my neck and covered the carrier with it. Under such a cape, the baby can eat as much as he wants until he falls asleep.
This breastfeeding position is best when the baby is already good at breastfeeding and can hold his head up by himself. Any slings are suitable for breastfeeding, including elastic and rings, as well as carrying bags. Whatever option you choose, the main thing is that you can always see the face of the child, and his chin does not rest against his chest.
10. Double hand-held breastfeeding
Double hand-held breastfeeding (or “double-ball grab”) is great for mothers of twins—you can breastfeed both at the same time, with your arms relatively free. 4 When feeding in this position, it is advisable to use a special pillow for breastfeeding twins, especially at first. It will provide extra support and help keep both babies in the correct position, as well as reduce the burden on the abdomen if you had a caesarean section. In addition, the hands are freer, and if necessary, you can deal with one child without interfering with the second.
It will provide extra support and help keep both babies in the correct position, as well as reduce the burden on the abdomen if you had a caesarean section. In addition, the hands are freer, and if necessary, you can deal with one child without interfering with the second.
“My twins were born very tiny and had to be fed every two hours at any time of the day or night. Very soon it became clear: if I want to do anything besides feeding, I need to feed them both at the same time, - says Emma, mother of two children from the UK. “I breastfed them two by hand using a breastfeeding pillow.”
Other good positions for breastfeeding twins are two criss-cross cradles, one baby in the cradle and the other close at hand, reclining feeding, or sitting upright (one baby on one side, the other on the other).
11. Feeding in the “breast support” or “dancer's hand” position
muscle tone (which is typical for premature babies, children suffering from various diseases or Down syndrome), try supporting his head and your chest at the same time. 4 Grab your chest with your palm underneath so that your thumb is on one side and all the others are on the other. Move your hand slightly forward so that your thumb and forefinger form a "U" just in front of your chest. With the other three fingers, continue to support the chest. With your thumb and forefinger, hold the baby's head while feeding so that his chin rests on the part of the palm between them, your thumb gently holds the baby on one cheek, and your index finger on the other. So the baby gets excellent support, and you can control his position and see if he is holding his breast.
4 Grab your chest with your palm underneath so that your thumb is on one side and all the others are on the other. Move your hand slightly forward so that your thumb and forefinger form a "U" just in front of your chest. With the other three fingers, continue to support the chest. With your thumb and forefinger, hold the baby's head while feeding so that his chin rests on the part of the palm between them, your thumb gently holds the baby on one cheek, and your index finger on the other. So the baby gets excellent support, and you can control his position and see if he is holding his breast.
Literature
1 Colson SD et al. Optimal positions for the release of primitive neonatal reflexes stimulating breastfeeding. Early Hum Dev . 2008;84(7):441-449. - Colson S.D. et al., "Optimal Positions for Provoking Primitive Innate Reflexes to Induce Breastfeeding." Early Hume Dev. 2008;84(7):441-449.
2 UNICEF UK BFHI [ Internet ].