Baby feeding problems tongue
Tongue-tie in babies | Baby & toddler, Feeding articles & support
Tongue-tie (ankyloglossia) in babies can affect both breastfeeding and bottle-feeding. Here we explain about tongue-tie symptoms and treatment.
What is a tongue-tie (ankyloglossia)?
Most people have a frenulum – a piece of tissue under their tongue that stretches from the underside of the tongue to the floor of the mouth. Tongue-tie occurs if the frenulum either extends forwards towards the tip of the tongue, is attached close to the lower gum, or is short and tight so it interferes with normal tongue movement (Oakley, 2021).
What problems does tongue-tie cause for babies?
If a baby has a tongue-tie, they may not be able to extend or lift their tongue or move it from side to side. Some will be able to lift the sides, but not the tip (v-shaped tongue). Some will be unable to lift the posterior of the tongue (bowl-shaped tongue). In babies where they frenulum extends all the way to the tip, the tongue may look heart-shaped.
Tongue-tie can affect both breastfeeding and bottle-feeding. For some babies, the effects will be quite mild. For others, tongue-tie can make feeding extremely challenging or even impossible.
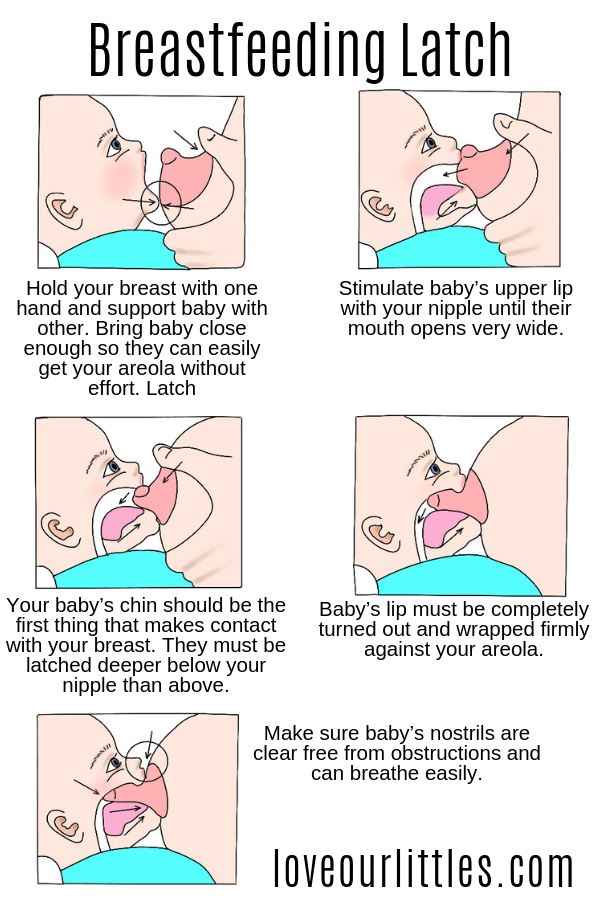
In order to breastfeed, a baby needs to be able to open their mouth wide, extend their tongue over their bottom lip and scoop the breast into their mouth. Then the tongue needs to massage the breast in a wave-like motion to remove milk from the breast (Oakley, 2021).
If your baby has a tongue-tie and you are breastfeeding, you might experience one or more of the following in your baby:
- difficulty in latching
- difficulty in maintaining a latch, with your baby frequently coming off the breast or slipping back to the nipple
- a shallow latch
- clamping down on the breast
- clicking noises while feeding
- unsettled behaviour during feeds
- frequent or long feeds
- poor weight gain or excessive early weight loss
- colic/wind/hiccups/reflux.
If you are breastfeeding your baby and they have tongue-tie, you might find your nipples are sore and appear squashed after a feed, often appearing ridged, lipstick-shaped, flattened or blanched. If your baby isn’t draining your breasts adequately, this can lead to engorgement, blocked ducts and mastitis. It can also have a negative effect on your milk supply. Feeds which are long or frequent can be very tiring (NHS, 2020; Oakley, 2021).
If you are bottle-feeding your baby, you might notice one or more of the following – your baby:
- is very slow to take a bottle
- chomps on the teat
- needs to be fed very often in order to get enough milk
- dribbles a lot during feeds
- tends to push the bottle teat out
- gags on feeds even when you slow the feed down
- can only manage a teat that has a very slow flow.
(Oakley, 2021)
How is tongue-tie diagnosed?
Can I tell if my baby has a tongue-tie?
If you look in your baby’s mouth, you might be able to see if they:
- are unable to extend their tongue fully
- have a tongue with a heart-shaped appearance at the tip
- have difficulty lifting their tongue or moving it from side to side.

(NHS, 2020)
Tongue-tie is not just about how your baby’s tongue looks. A tongue can look completely normal to an untrained eye yet still cause substantial problems with feeding (Young, 2011).
A tongue-tie is diagnosed by the baby’s tongue function too – what they can do with their tongue. It can only be diagnosed by a qualified tongue-tie practitioner (NHS, 2020).
Tongue-tie types
Tongue-ties can be described as anterior (where the frenulum extends towards the front of the tongue) or posterior (towards the back of the mouth).
Tongue-ties might also be described using a percentage or a number (type I, II, III and IV). This percentage or number describes how far along the underside of the tongue the frenulum comes. So 100%, or type I, would indicate that the frenulum comes all the way to the front of the tongue.
A posterior tongue-tie, which may be described as a 10% tongue-tie, can restrict tongue function just as much as an anterior one. That means these anatomical descriptions of how the tongue looks don't always relate to how severely a tongue-tie will affect tongue function and your baby's feeding (Oakley, 2021).
That means these anatomical descriptions of how the tongue looks don't always relate to how severely a tongue-tie will affect tongue function and your baby's feeding (Oakley, 2021).
Tongue-tie diagnosis
Some babies have a visible frenulum that doesn’t cause problems with feeding (UNICEF, no date). Tongue-tie shares many of the symptoms of other breastfeeding problems, so it’s not always easy to determine whether these problems are caused by a tongue-tie or something else.
A full feeding assessment should be done before or as part of a tongue-tie assessment (Oakley, 2021). If you and/or your baby are experiencing feeding difficulties, a feeding assessment and some breastfeeding support from a breastfeeding counsellor or trained breastfeeding professional is recommended. Support to improve your baby’s attachment to the breast may resolve the problem (UNICEF, no date).
A baby’s inability to open their mouth widely and extend their tongue may also be caused by tension around the mouth and neck, resulting from birth tensions or interventions during labour. This might be resolved by manual therapy, such as osteopathy or chiropractic from a registered practitioner (ATP, no date; Oakley, 2021).
This might be resolved by manual therapy, such as osteopathy or chiropractic from a registered practitioner (ATP, no date; Oakley, 2021).
If the breastfeeding professional (breastfeeding counsellor, midwife or health visitor) suspects your baby has a tongue-tie, they will refer you to a local tongue-tie practitioner. Tongue-tie practitioners will do a formal assessment of tongue-tie based on how the tongue functions as well as how it looks (e.g. the Hazelbaker Assessment Tool for Lingual Frenulum Function). Most midwives and health visitors are not tongue-tie practitioners so are unable to make a diagnosis of tongue-tie themselves.
Tongue-tie treatment
What is tongue-tie division?
Your baby could have a tongue-tie division, which can release their tongue so it can move more freely. This involves cutting the frenulum (NICE, 2005).
Tongue-tie division is a safe procedure that can improve the breastfeeding problems that tongue-tie causes (NICE, 2005).
Does tongue-tie division hurt?
Tongue-tie division procedures are very quick and simple and are thought to be almost painless (NICE, 2005).
Does tongue-tie division resolve feeding problems?
Most parents say their baby’s feeding improves after a tongue-tie division and many find it resolves the problem completely (Buryk et al, 2011; Berry et al, 2012). But a few babies do continue to have feeding difficulties even after a tongue-tie division.
Do I need to get my baby’s tongue-tie treated?
The decision on whether to have a tongue-tie divided is a personal one and different parents will make different decisions. Every tongue-tie is different too and the range of issues it causes can vary from very mild to severe. So how much the tongue-tie is affecting feeding and your life with your baby might influence your decision.
You might find it helpful to talk things through with an NCT breastfeeding counsellor too. They can help you explore your thoughts and feelings plus find ways of coping if you decide not to have the procedure done.
What else might help with feeding difficulties due to tongue-tie?
For some babies, it may be possible to improve feeding without having a tongue-tie division.
If babies are fed in a laid back position, they are more relaxed, can open their mouth wider and get a bigger mouthful of breast. But some babies are unable to extend their tongue enough to scoop the breast into their mouth, so this position doesn’t make feeding easier. A side-lying position or koala hold might also help.
Babies can also be helped by using an 'exaggerated latch'. This is where you hold your baby close to but below the breast, and use your forefinger to tilt your nipple upwards. That way, when your baby tips their head back and is brought into the breast, your nipple can be flipped towards the back of their mouth (Oakley, 2021).
Babies who are bottle-fed might find feeds easier if paced bottle feeding techniques are used. Occasionally, finger feeding can be a more comfortable option than using a bottle (Genna, 2013). A tongue-tie can make it difficult for babies to form a seal around the bottle teat. A high palate, often associated with a tongue-tie, can trigger the baby’s gag reflex. Shorter, wedge-shaped or flatter teats may be easier for babies with a tongue-tie to drink from (Oakley, 2021).
Shorter, wedge-shaped or flatter teats may be easier for babies with a tongue-tie to drink from (Oakley, 2021).
How can I find tongue-tie division services near me?
Only registered healthcare professionals who have received proper training in tongue-tie division should perform this procedure. In many areas, the NHS provides a tongue-tie division service. But provision varies across the country and parents in some areas have to travel long distances to reach a tongue-tie division service.
It can be even harder to find a tongue-tie division service when a baby is having problems bottle-feeding. Unfortunately, some areas might have no service available (Wise, 2015).
The National Institute for Health and Care Excellence – also known as NICE – supports considering tongue-tie division. Yet there is no common agreement among tongue-tie dividers on how to carry out the procedure or how far the membrane should be divided (NICE, 2005). This means the service different health professionals offer varies.
Online, you can see a directory of both NHS and private tongue-tie practitioners on the Association of Tongue-tie Practitioners (ATP) website.
What can I expect after my baby’s tongue-tie division?
Babies are often unsettled in the first day or two after a tongue-tie division and might need more cuddles and nurturing. After the procedure, you’ll probably see a white patch under your baby’s tongue; this takes 24 to 48 hours to heal but it won’t bother your baby (UNICEF, no date).
Do I need to do anything after the tongue-tie division?
Some tongue-tie practitioners recommend some tongue exercises or wound massage after a tongue-tie division. The exercises involve encouraging the baby to move their tongue through finger sucking and tongue-poking games. Massaging the wound with a clean finger may help prevent the tongue division knitting together and re-forming but there is no evidence to suggest that this is safe or effective (Oakley, 2021).
Will my baby’s feeding improve after their tongue-tie division?
Parents often expect that feeding will improve immediately after a tongue-tie division.
Feeding can be more difficult for the first day or two after a tongue-tie division because it takes time for your baby to adjust to their new, freely-moving tongue (Oakley, 2021).
Some babies might need further support even after a tongue-tie division. If things have not improved after a few days, you might find it helpful to get extra support to improve feeding – see below.
This page was last reviewed in March 2022.
Further information
Our support line offers practical and emotional support with feeding your baby and general enquiries for parents, members and volunteers: 0300 330 0700.
You might find attending one of our Early Days groups helpful as they give you the opportunity to explore different approaches to important parenting issues with a qualified group leader and other new parents in your area.
Make friends with other parents-to-be and new parents in your local area for support and friendship by seeing what NCT activities are happening nearby
Attending a Baby Cafe or other breastfeeding support drop-in can be a good way to access support with feeding your baby.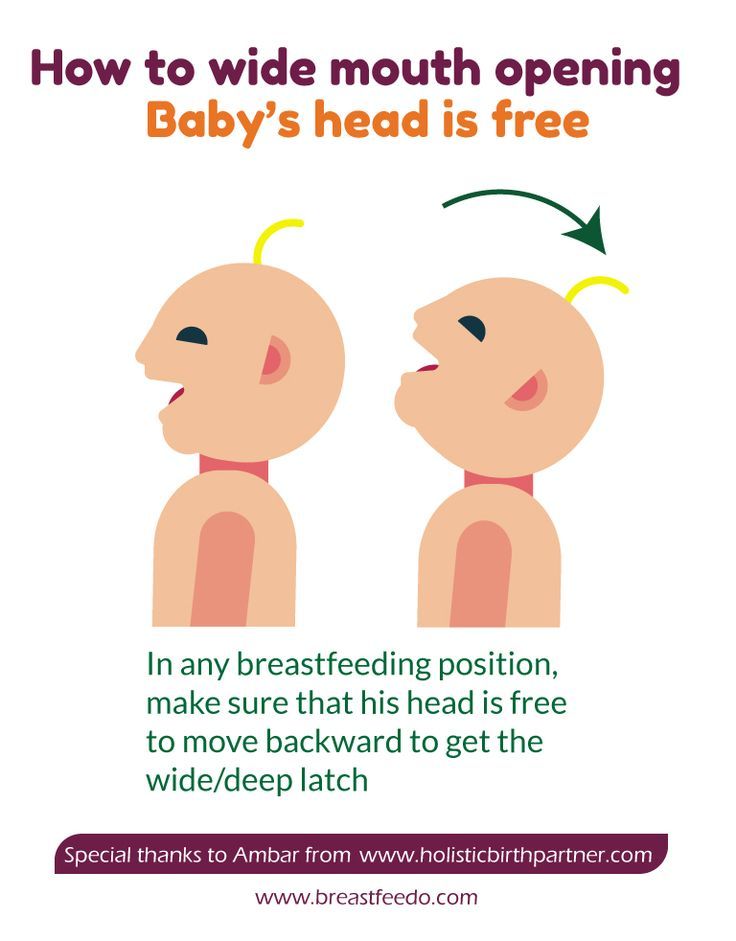 You may also find other parents there whose babies have had a tongue-tie.
You may also find other parents there whose babies have had a tongue-tie.
Pictures of babies with tongue-tie can be found on Catherine Genna’s website.
The Baby Friendly Initiative, part of UNICEF, has a list of locations where tongue-tie can be divided within the UK, as does the Association of Tongue-Tie Practitioners.
Tongue-tie UK raises awareness about tongue-tie and lip-tie in the UK to help parents get information and support.
Feeding support and options to fix tongue-tie in babies | Pediatrics | Your Pregnancy Matters
×
What can we help you find?Refine your search: Find a Doctor Search Conditions & Treatments Find a Location
Appointment New Patient Appointment
or Call469-497-2500
MedBlog
Pediatrics; Your Pregnancy Matters
April 27, 2021
Pediatrics; Your Pregnancy Matters
Felicity Lenes-Voit, M. D. Otolaryngology
D. Otolaryngology
Tongue-tie might sound like an old wives' tale, but it's a real medical condition that affects 5 to 25 percent of newborns each year – a large range due to the many factors that can complicate getting a diagnosis.
But just because a baby has tissue under their tongue does not mean they will have feeding or speech implications. The functional contribution of the tissue is more important than whether there is extra tissue present. So, not all babies with a prominent frenulum are actually tongue-tied – and not all of them need intervention.
Babies with tongue-tie, or ankyloglossia, have extra tissue connecting their tongue to their floor of mouth which restricts the tongue motion.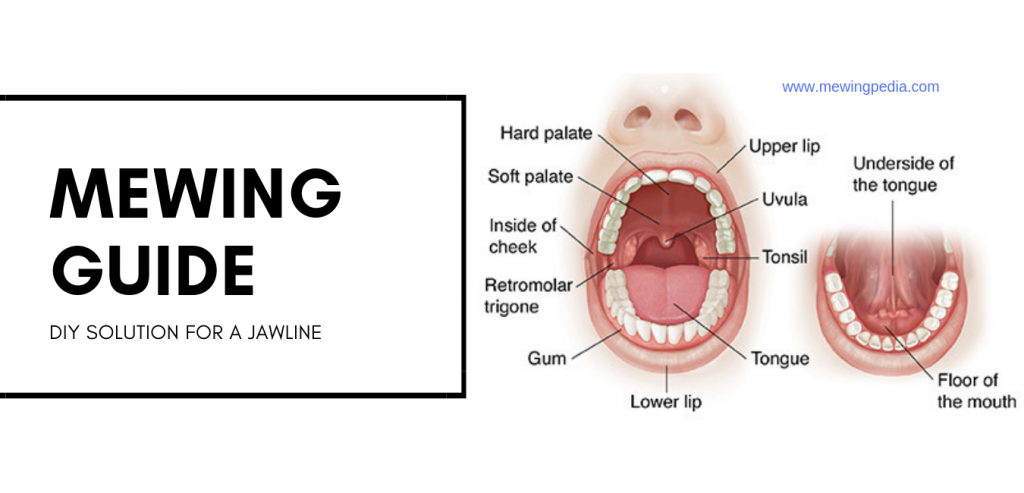 This can make it difficult for the baby to coordinate feeding.
This can make it difficult for the baby to coordinate feeding.
While there is no strong evidence that tongue-tie affects speech later in life, the condition can cause problems such as:
- Abnormal growth
- Frustration for parents and baby at feedings
- Reduced breastmilk supply
- Reflux
Most new parents can help their babies overcome feeding challenges with lactation support and non-invasive therapies. In some cases, an in-office procedure called frenotomy can help free the tongue to move more efficiently.
Since so many factors can complicate infant feeding, most babies need the combined expertise of specialists who are trained in different aspects of infant oral health.
UT Southwestern brings together pediatricians, lactation consultants, speech therapists, and otolaryngologists (ear, nose, and throat specialists) to help families overcome feeding challenges in the first few months after birth. All of these providers work together to make sure the baby gets the best, most appropriate, and most timely care.
Let's discuss how we diagnose tongue-tie, when a newborn might need a procedure right away, and what we can do to help your baby feed and grow better.
Ruling out other feeding issues
Learning to breast or bottle feed is expected to be a little challenging for babies and new parents. There are many areas where little adjustments can make a world of difference.
So, babies who struggle with feeding can receive support from several different providers. The progression often goes like this:
The first step is to discover the source of your baby's feeding problems, and our experts will work with you to do that.- Lactation consultant: All patients who deliver at UT Southwestern have access to lactation consultants in the weeks after delivery. These experts can troubleshoot positioning and latching issues that might be keeping the baby from effectively feeding.

- Pediatrician: Your baby's doctor is an excellent resource for investigating feeding and growth concerns. If they think your child may have tongue-tie, based on a physical exam, the pediatrician may treat your baby before you even leave the hospital or in an outpatient setting. Depending on their experience and your baby's need, the pediatrician may refer you to a speech therapist or an otolaryngologist.
- Speech therapists: These experts can recommend stretching exercises to help coordinate the tongue, jaw, and cheek muscles, essentially retraining the mouth to feed.
With tongue-tie and feeding issues, timing is everything. The earlier we detect feeding issues, the easier it will be to correct them. If the baby cannot latch, even with the support of a lactation consultant, and the baby has a severe tongue-tie, we may recommend frenotomy before the baby leaves the hospital.
Some babies simply have trouble latching right away, but with ongoing lactation support, they will improve. Your care team will work with you to determine the safest and most appropriate next steps for your newborn.
Your care team will work with you to determine the safest and most appropriate next steps for your newborn.
These windows of time are key to successful tongue-tie diagnosis and intervention:
1. Within two to four weeks after birth.
When the breast milk supply is first established, there can be a "grace period" in which the milk starts flowing with less stimulation from the baby, and the supply is not highly dependent on demand. Even if the new baby's mouth mechanics are not great at extracting milk right away, the baby can "lap it up" if there is an oversupply of milk or a very active letdown. However, this is not a substitute for good feeding mechanics.
It's normal for newborns to spend a few days learning to nurse or drink from a bottle, but if you're still struggling after visiting with a lactation consultant, the baby may need to visit a speech therapist. The therapist can recommend tongue and mouth stretches.
2. Don’t wait too long to see an ENT.
We generally do the office procedure until about 12 weeks old. It’s true that by 10-12 weeks the milk supply is much more supply and demand-based, but intervention earlier than this would still make things a lot easier on mom, and if mom and baby are still struggling at 10 weeks there have probably been some growth issues.
It’s true that by 10-12 weeks the milk supply is much more supply and demand-based, but intervention earlier than this would still make things a lot easier on mom, and if mom and baby are still struggling at 10 weeks there have probably been some growth issues.
What to expect at the otolaryngology visit
We will put together all the other specialists' recommendations and, after examining the baby and talking with you, create an overview of what is causing your baby's feeding problems.
For baby
We'll start by reviewing your baby's health history and feeding patterns:
- Was the baby a preemie?
- Any risk factors during pregnancy or delivery that may affect the milk supply?
- Do they suck, swallow, and breathe during feedings? Or do they tend to suck a long time without breaks to swallow (a sign they're not getting much milk)?
- Are they at risk for a condition that might affect muscle strength or coordination?
- Do they seem satisfied after eating?
- How long is a typical feeding session?
The otolaryngologist will check the baby's weight and how well they can suck on the doctor's gloved finger. We'll also check whether their tongue makes a massaging movement, which helps coax milk out of the breast or bottle. If the baby can move its tongue without restriction but is still having trouble feeding, frenotomy may not help. In those cases, we will refer you for more advanced speech or physical therapy.
We'll also check whether their tongue makes a massaging movement, which helps coax milk out of the breast or bottle. If the baby can move its tongue without restriction but is still having trouble feeding, frenotomy may not help. In those cases, we will refer you for more advanced speech or physical therapy.
For new parents
If you are breastfeeding, we'll also discuss your health history. Certain conditions, such as hypothyroidism or gestational diabetes – can decrease milk supply. We'll also discuss your stress level, your own eating and hydration routine, and whether you feel pain or discomfort while nursing.
Next steps
If the issue is related to your health, we may recommend diet or medication changes to increase your breastmilk supply. You may need to consider supplementing with formula if your health makes breastfeeding too difficult. This can be disappointing for some parents, but remember, a fed baby is a happy baby. Whether your child is breast or bottle fed is not a reflection on your parenting skills or love for your child.
If the baby does have tongue-tie and other therapies haven't solved the issue, we may recommend frenotomy. Also called "clipping," this outpatient procedure can potentially improve tongue mobility and feeding success.
How we perform frenotomy
There are two widely used techniques for performing frenotomy: cold steel and laser. UT Southwestern otolaryngologists use the cold steel technique because, despite its name, it is gentler, causes the infant less pain, and bears fewer risks of complications, such as cysts or scarring.
When possible, we do this procedure at 14 weeks or sooner. After that point, the baby will likely be stronger with greater head control, and the procedure carries more risks.
Frenotomy takes only a few minutes and starts with a sweet treat. We typically do not use oral numbing medications in infants younger than one. Oral numbing and pain medication can be overactive in babies and can cause complications such as decreased oxygen levels and cardiac toxicity.
To avoid that risk, we follow the American Academy of Otolaryngology–Head and Neck Surgery recommendations to feed the baby a sugary liquid mixture. The sweet taste stimulates the brain to release "feel-good" hormones that help curb the minimal pain of the procedure without increasing the risk of complications.
Then, we use a small retractor with a groove in it to gently elevate the tongue, exposing the frenulum. We make a small cut in the frenulum, taking care to avoid the salivary gland ducts on the floor of the mouth.
The incision will go from the front of the frenulum to the back of the tongue, and we will know we have released the tie by confirming a diamond-shaped release in the floor of the mouth.. Separating the tissue allows for maximum tongue mobility. However, we don't cut the tissue all the way back. Instead, the doctor will gently separate the tissue with their finger, avoiding the risk of cutting into the nerves on the floor of the mouth and bottom of the tongue.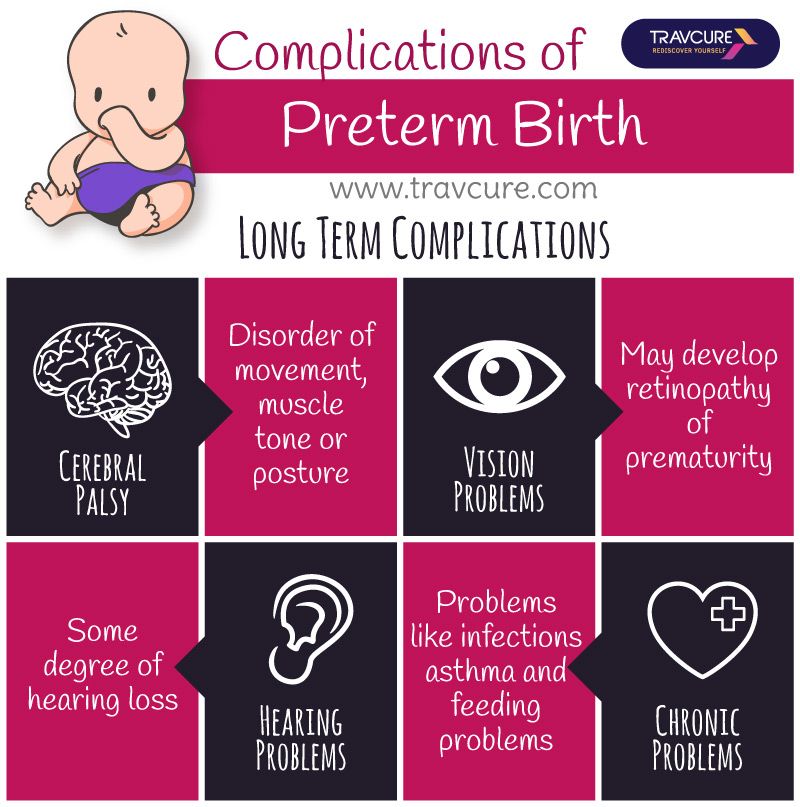
Then, the doctor will apply pressure to the incision to stop any bleeding. Next, the baby gets another dose of sweet liquid before we return them to you to feed. The suckling action of feeding comforts the baby and puts additional pressure on the incision site.
We'll observe the baby in the office for at least 15 minutes to ensure bleeding does not resume. While we wait, we'll go over a few exercises to do with the baby to minimize the development of scar tissue. It's best not to do these stretches at feedings – we don't want the baby to associate discomfort with eating, which can lead to further feeding challenges.
Listen now: Treating Tongue-Tie (backtableENT)
Existing patients may also schedule an appointment using MyChart.
More Options
A few closing thoughts
Moms and dads often blame themselves when feeding doesn't take off right away. But feeding problems are multifactorial, and most concerns can be resolved with expert support – no procedure required.
Seeking help when you need it is the best way to prevent long-term growth problems and reduce your frustration. Your pediatrician, Ob/Gyn provider, and lactation consultants will work with you to identify and overcome feeding challenges in your baby's first few months of life.
Our infant feeding team has the expertise to determine what's causing your baby's feeding issues. And if your child needs lactation support, speech therapy, or surgery, we'll guide you through the process and answer your questions every step of the way.
To discuss infant feeding concerns, call 469-497-2500 or request an appointment online.
Dr. Shivani Patel, a maternal-fetal medicine specialist at UT Southwestern, explains the advantages of exclusive pumping and why some women prefer it over breastfeeding.
Learn more
Back and Spine; Brain; Orthopaedics and Rehab; Pediatrics
- Benjamin Greenberg, M.
 D.
D.
January 26, 2023
Pediatrics; Your Pregnancy Matters
- Jessica Morse, M.D.
December 6, 2022
Eyes and Vision; Pediatrics
- Jessica Thayer, M.
 D.
D.
November 29, 2022
Cancer; Eyes and Vision; Pediatrics
- J. William Harbour, M.D.
September 21, 2022
Pediatrics; Women's Health
- Nirupama DeSilva, M.
 D.
D. - Jason Jarin, M.D.
August 31, 2022
Pediatrics; Your Pregnancy Matters
- Becky Ennis, M.D.
July 19, 2022
Pediatrics
- Tanya Martinez-Fernandez, M.
 D.
D.
July 13, 2022
ENT; Pediatrics
- Kenneth Lee, M.D., Ph.D.
June 23, 2022
Pediatrics; Your Pregnancy Matters
- Jamie Morgan, M.
 D.
D.
June 14, 2022
More Articles
Solutions to six breastfeeding problems in the first week
Are you having difficulty breastfeeding your newborn baby? Read on for expert advice on tackling the main challenges of the first week of breastfeeding.
Share this information
Cathy Garbin, child health nurse, midwife and lactation consultant:
Cathy, a mother of two, was a research fellow at the renowned Human Lactation Research Institute, founded by Peter Hartmann, for seven years, providing support to breastfeeding mothers in clinics and at home. Today, she still works as a family counselor, and also conducts seminars for attending physicians and speaks at international conferences.
Breastfeeding is not always easy, so if
you are having difficulty, know that you are not alone.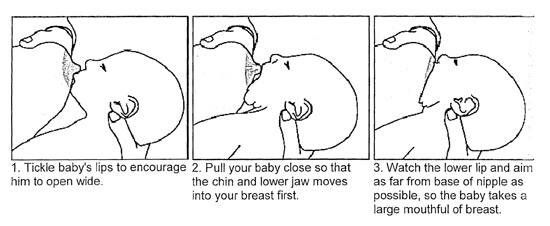 A US study found that out of 500 new mothers surveyed, 92% experienced breastfeeding problems by the third day. 1 Fortunately, most early breastfeeding problems are easy to resolve. Below you can read recommendations for solving the main problems that mothers often face in the first week of feeding.
A US study found that out of 500 new mothers surveyed, 92% experienced breastfeeding problems by the third day. 1 Fortunately, most early breastfeeding problems are easy to resolve. Below you can read recommendations for solving the main problems that mothers often face in the first week of feeding.
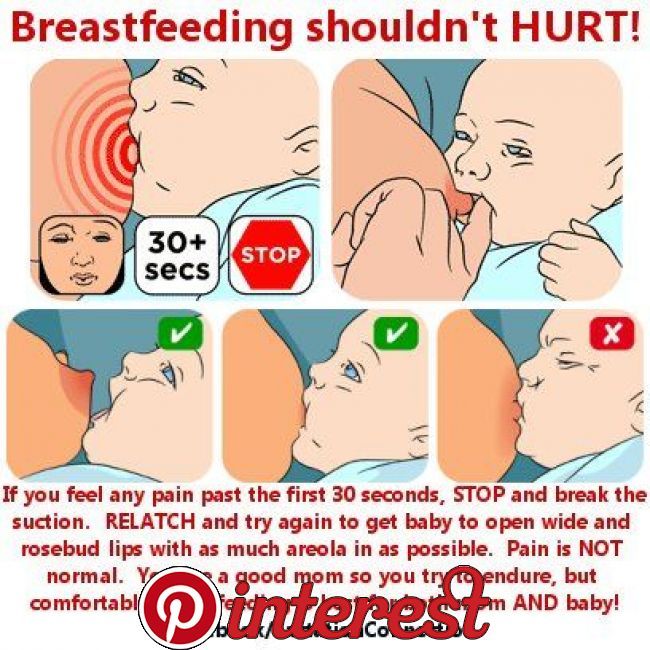
Problem #1. Breastfeeding hurts!
Pain during feeding is usually associated with tenderness or inflammation of the nipples, especially when milk "comes" on the second to fourth day after birth. 2 The baby will beg for a breast every couple of hours, and this can quickly aggravate the problem: some mothers' nipples crack, bleed, or blister. This is, of course, very annoying.
Solutions 3
- Check how the baby latch on. An incorrect latch is one of the most common causes of pain during breastfeeding. A newborn baby should take most of the lower half of the areola (dark skin around the nipple) into his mouth, and your nipple should rest against his palate, supported from below by the tongue.

- Contact a lactation consultant or healthcare professional to make sure your baby's mouth and torso are properly positioned during feeding and there are no other latch-on problems. The doctor may also examine the baby's mouth for physical abnormalities.
- Try other feeding positions. Reclining, cross cradle, underarm, or lying positions can relieve pressure on the most painful areas of your breasts.
- Gently wipe soaked nipples with water-soaked cotton swabs after each feed to remove milk residues that can cause infection.
- Air dry nipples or blot with a clean, soft muslin or flannel cloth to prevent bacterial growth in a humid environment. Use disposable or reusable bra pads to absorb leaking milk and remember to change them regularly.
- Soften your nipples. An ultra-pure lanolin treatment will help relieve inflammation and dry skin. You can also apply a few drops of your own breast milk to your nipples.
 In both cases, you do not have to wash your breasts before the next feeding. You can also apply refrigerated hydrogel pads* to your nipples. They soothe the nipples and help relieve pain during feeding, as well as speed up healing.
In both cases, you do not have to wash your breasts before the next feeding. You can also apply refrigerated hydrogel pads* to your nipples. They soothe the nipples and help relieve pain during feeding, as well as speed up healing. - Protect your nipples. Nipple shields* protect the sore area from rubbing against clothing.
- Be patient. The inflammation usually resolves after a few days as your body adjusts to breastfeeding and your baby learns to suckle.
- Seek medical attention, if pain during feeding does not go away after a few days. Constant inflammation of the nipples may indicate an infection that requires prompt treatment.
Problem #2. Baby doesn't latch on properly
Some newborns do not latch on properly right away. Maybe both of you just need more time to learn how to breastfeed, or maybe the baby was born prematurely, feels unwell after a difficult birth, or mom has flat or inverted nipples.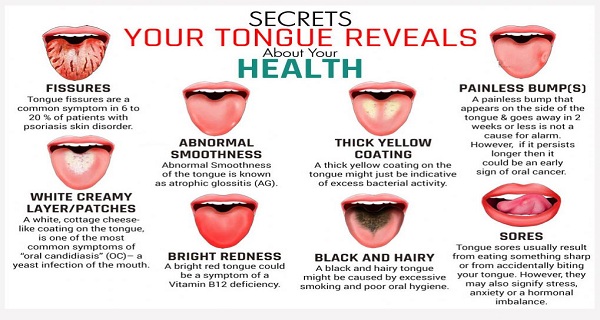
Solutions
- Contact a lactation consultant or healthcare professional who can help identify the cause of the problem and suggest solutions.
- Flat or inverted nipples must be pulled out. Nipple formers* fit comfortably in the bra and apply gentle pressure to the nipples to help them come out for easier feeding.
- Try different positions and ways to support your newborn. The baby needs to feel supported. He must be comfortable and breathe freely in order to suckle properly. Do not hold the child by the head and do not put pressure on it. Lean back and let your child take the lead. This stimulates his natural reflexes and helps him find and latch on to his breasts. 4
- When feeding, try to find the optimal position. Instead of putting your baby on and off, stressing both of you, try to position him in a way that is easy and comfortable for him.
 Hold the torso and legs of the baby close to you, support him by the shoulders and hold him firmly so that he feels safe. Let the baby's head rest freely on your arm so that he can tilt it back slightly and breathe freely. The chin should be pressed against your chest. If these small adjustments don't make feeding more comfortable for your baby, seek help from a lactation consultant or healthcare professional.
Hold the torso and legs of the baby close to you, support him by the shoulders and hold him firmly so that he feels safe. Let the baby's head rest freely on your arm so that he can tilt it back slightly and breathe freely. The chin should be pressed against your chest. If these small adjustments don't make feeding more comfortable for your baby, seek help from a lactation consultant or healthcare professional. - Use nursing pads. If your baby is having difficulty latch-on, a lactation consultant or healthcare professional may suggest trying nursing pads*. A nipple with an overlay is more convenient to take in the mouth, so it is larger and more rigid. Do not use nursing pads for a long time.
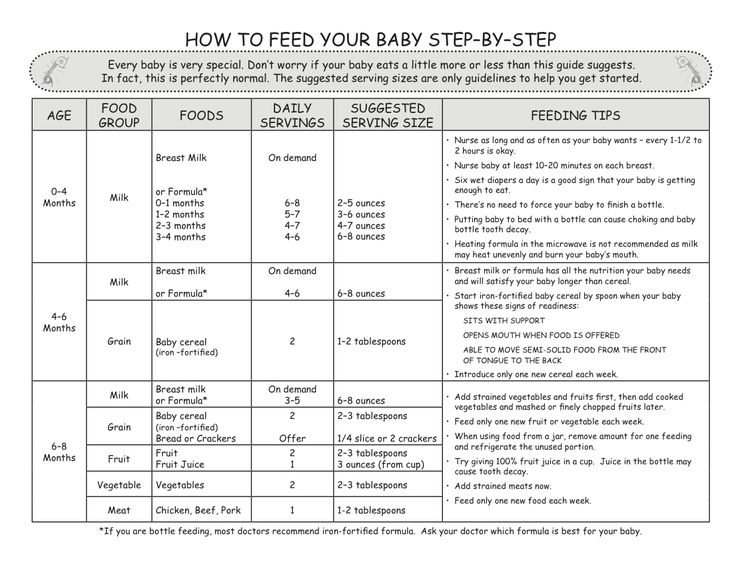
Problem #3. Not enough breast milk
You will produce little breast milk at the very beginning, as the hormonal changes that trigger milk production occur slowly and do not end until the second or fourth day after birth. 2 You may be worried that your baby is not getting enough milk, but in the early days his stomach is still too small and feedings are frequent, so don't worry. The only things to worry about these days are excessive weight loss, too few wet and soiled diapers, or signs of dehydration in the baby. For more information on how often a newborn should urinate and void, see Breastfeeding Newborns: What to Expect in the First Week.
The only things to worry about these days are excessive weight loss, too few wet and soiled diapers, or signs of dehydration in the baby. For more information on how often a newborn should urinate and void, see Breastfeeding Newborns: What to Expect in the First Week.
Solutions
- Contact a Lactation Consultant or your healthcare provider who can determine if you have problems with milk production. The sooner you do this, the better.
- Feed your baby on demand, not on a schedule. In the first week after birth, your baby will ask to breastfeed every two to three hours (or more often!), both day and night. Such frequent feeding helps to establish the production of breast milk.
- Take care of yourself. It's not always easy with a newborn, but try to rest whenever you can, eat right, and accept any help around the house or with older children that your loved ones can give you to fully focus on breastfeeding.
- Try expressing milk. If a baby is feeding frequently but not gaining any weight, a lactation consultant or doctor may recommend pumping to increase breast milk production. If milk is not coming out at all, you can try the Medela Symphony Dual Electric Clinical Breast Pump**. It features an Initiate program that mimics a baby's natural sucking rhythm for the first few days.
Problem #4. Breast full and heavy
Your breasts will become fuller and heavier as milk comes in.
If the baby suckles well and often, this should not cause any problems. However, in some women, the breasts become so full that they become hard and painful. This condition, called breast swelling, can cause discomfort. The swollen chest seems to be “burning”, now all the activity of your body is concentrated in it, resembling a busy traffic at rush hour. Fortunately, this condition usually resolves within 24 to 48 hours. However, due to the swelling of the mammary glands, the nipples can become flat and the baby may have difficulty latch-on.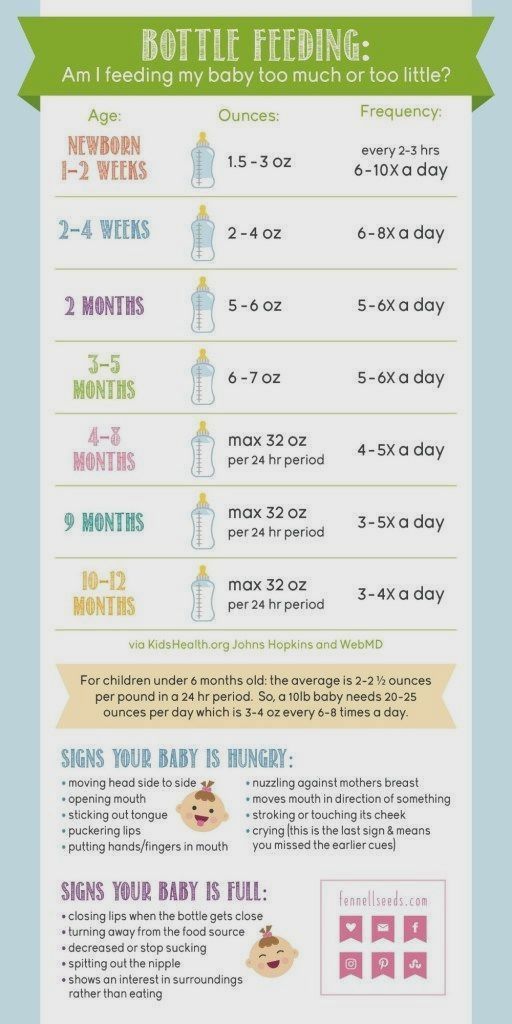 5
5
Solutions
- Feed your baby often. Try to breastfeed at least 8-12 times a day. This is the main way to alleviate this condition. For more tips and tricks, see the article on Breast Swelling. 6.7
- Call your healthcare provider, if symptoms persist for more than 48 hours, you have a fever, or your baby is unable to breastfeed due to swelling.
Problem #5. Milk is leaking
Breast leakage is very common in the early days of breastfeeding when milk production begins. Milk may leak from one breast while you are feeding the other, when you sleep on your stomach, or when something accidentally triggers the milk flow reflex, such as when you hear a baby crying in a store. The leakage usually stops after about six weeks.
Solutions
- Protect clothes from stains will help disposable or reusable bra pads to be used day and night.

- Don't waste precious drops! Breast milk collection pads* fit inside the bra and allow you to collect any leaking milk. This is a very useful thing when there is too much milk and the pads are not absorbing well, or when one breast is leaking while you are feeding the other. If you want to save the collected milk, use only the milk collected at the feeding. Place it in a sterile container and refrigerate immediately if you are not supplementing with it right away. Collected milk must be used within 24 hours. The breast milk collection sleeves should not be worn for more than two to three hours at a time.
Problem #6. There seems to be too much milk
Sometimes when milk comes in, too much is produced! In the first few weeks there may be an overabundance of milk, but usually everything returns to normal soon. 7 Up to this point, the breasts may be heavy and sore almost all the time, even immediately after a feed, and a lot of milk may leak. A strong flush can cause a baby to cough or choke, vomit immediately after a feed, have tummy discomfort, or have hard, frothy, greenish stools. These are all signs that you are having too much milk, but the problem may resolve itself as your breasts get used to the new function.
A strong flush can cause a baby to cough or choke, vomit immediately after a feed, have tummy discomfort, or have hard, frothy, greenish stools. These are all signs that you are having too much milk, but the problem may resolve itself as your breasts get used to the new function.
Solutions
- Express some milk by hand at the beginning of each feed to ease the force of the flush.
- Try to feed while leaning back: this will help your baby control the flow of milk. The cradle position is also good: hold the baby obliquely by the shoulders so that the head can lean back slightly while on your arm. The torso of the baby will be located diagonally on you.
- Be kind and patient. Let your baby rest and absorb milk both during and after feeding. Don't move your baby too much or too fast, as this can make him nauseous. As the baby grows, he will learn to better cope with the rush of milk, which is likely to weaken anyway.
- Use the towel or swaddle to soak up spilled milk if the baby can't handle the flush, and place the breast milk collection pad on the other breast to catch any spilled milk.
- Contact a lactation consultant or doctor if problems persist after a few weeks . He will examine you and may suggest one-sided feedings or hourly breast changes (“breast duty”) to reduce your milk supply.
Related materials: Difficulties in breastfeeding in the next few weeks and problems with breastfeeding after the first month
Literature
1 Wagner EA et al. Breastfeeding concerns at 3 and 7 days postpartum and feeding status at 2 months. Pediatrics . 2013: peds -2013. - Wagner I.A. et al., "Breastfeeding Problems at Days 3 and 7 of a Child's Life and Type of Feeding at 2 Months". Pediatrix (Pediatrics). 2013:e865–e875.
2 Pang WW, Hartmann PE. Initiation of human lactation: secretory differentiation and secretory activation. J Mammary Gland Biol Neoplasia 2007;12(4):211-221. - Pang, W.W., Hartmann, P.I., "Lactation initiation in the lactating mother: secretory differentiation and secretory activation." G Mammary Gland Biol Neoplasia. 2007;12(4):211-221.
Initiation of human lactation: secretory differentiation and secretory activation. J Mammary Gland Biol Neoplasia 2007;12(4):211-221. - Pang, W.W., Hartmann, P.I., "Lactation initiation in the lactating mother: secretory differentiation and secretory activation." G Mammary Gland Biol Neoplasia. 2007;12(4):211-221.
3 Cadwell K. Latching - On and Suckling of the Healthy Term Neonate: Breastfeeding Assessment. J Midwifery & Women ’ s 2007;52(6):638-642. — Cadwell, K., "Latching and sucking in healthy newborns: evaluation of breastfeeding." F Midwifery Women Health. 2007;52(6):638-642.
4 Colson SD et al. Optimal positions for the release of primitive neonatal reflexes stimulating breastfeeding. Early Hum Dev . 2008;84(7):441-449. - Colson S.D. et al., "Optimal Positions for Provoking Primitive Innate Reflexes to Induce Breastfeeding." Airlie Hume Dev. 2008;84(7):441-449.
2008;84(7):441-449. - Colson S.D. et al., "Optimal Positions for Provoking Primitive Innate Reflexes to Induce Breastfeeding." Airlie Hume Dev. 2008;84(7):441-449.
5 Jacobs A et al. S3-guidelines for the treatment of inflammatory breast disease during the lactation period. Geburtshilfe Frauenheilkd. 2013;73(12):1202-1208. - Jacobs A. et al., "Recommendations S -3 for the treatment of inflammatory diseases of the breast during breastfeeding. Geburtskhilfe und Frauenheilkünde. . ABM Clinical Protocol# 4: Mastitis , Revised MARCH 2014. Breastfeed : 5): 5) H., Academy of Breastfeeding Protocol Committee, AVM Clinical Protocol #4: Mastitis, March 2014 edition of Brestfeed Med (Breastfeeding Medicine). 2014;9(5):239-243.
7 Academy of Breastfeeding Medicine Protocol Committee. ABM clinical protocol # 20: Engorgement.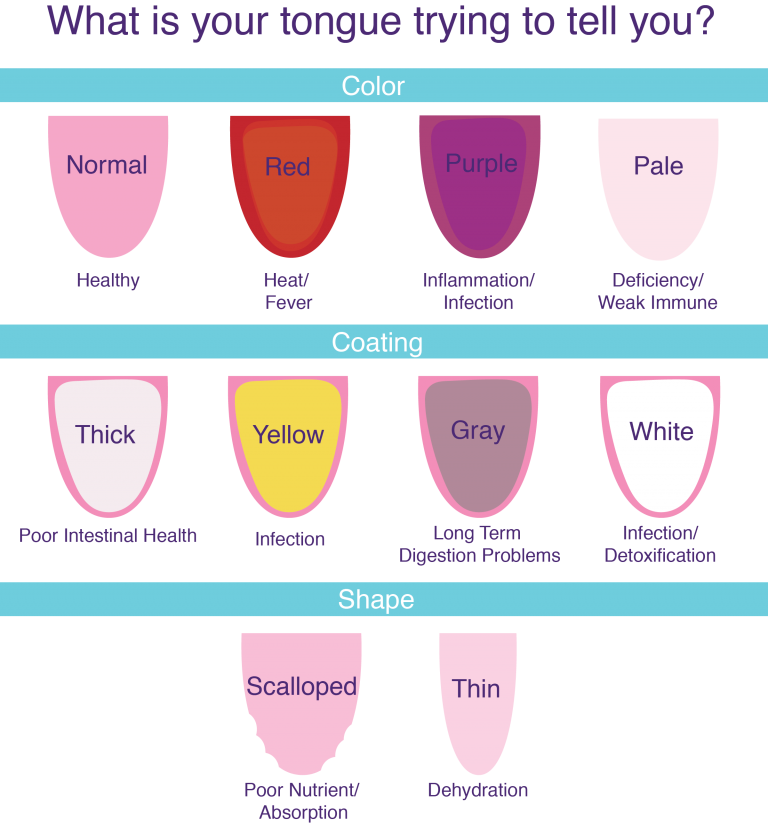 Breastfeed Med . 2009;4(2):111-113. - Protocol Committee of the Academy of Breastfeeding Medicine, "AVM Clinical Protocol No. 20: Engorgement, Revision 2016". Brestfeed Med (Breastfeeding Medicine). 2009;4(2):111-113.
Breastfeed Med . 2009;4(2):111-113. - Protocol Committee of the Academy of Breastfeeding Medicine, "AVM Clinical Protocol No. 20: Engorgement, Revision 2016". Brestfeed Med (Breastfeeding Medicine). 2009;4(2):111-113.
Read instructions before use. Consult a specialist about possible contraindications.
* RU No. ФСЗ 2010/07352 dated 07/19/10
** RU No. ФСЗ 2010/06525 dated 17/03/2021
Comprehension of language movement in infants 2
Sept. 2021
This resource is intended for healthcare professionals
Researchers have used ultrasound video for the first time to see differences in tongue movements between breastfed infants and adults when swallowing.
The tongue is an active muscle and a marvel of coordination. When we drink, the tongue prepares for swallowing by collecting liquid in the mouth, taking the shape of a bowl. It then quickly pushes the liquid back where it is swallowed, while still allowing us to continue breathing.
When we eat, the tongue works by holding food in the mouth, moving it with saliva and turning it into a lump, which is then pushed back for swallowing. Both adults and infants use a peristaltic type of movement when swallowing.
Language training before birth
Teaching our tongue to do all this work begins in the womb. Before birth, the tongue begins to work by swallowing the amniotic fluid. After the birth of a child, the tongue plays a key role - it helps to squeeze milk out of the mother's breasts, working in conjunction with the jaws and lips.
When the baby is suckled to the mother's breast, the nipple and areola are retracted into the mouth so that the nipple reaches the junction of the hard and soft palate. After the baby has sucked well, the tongue begins to work, rhythmically squeezing the nipple with peristaltic movements that squeeze the milk from the mammary gland into the back of the throat, where it is swallowed. Babies naturally coordinate sucking, swallowing, and breathing.
Bottle feeding
This process changes slightly when the baby is bottle fed. The stiffness of the artificial material does not allow the nipple to stretch and take the shape of the baby's mouth. Peristaltic movements of the tongue are difficult and milk can flow almost without effort on the part of the child.
Parents should remember that during breastfeeding, babies make an effort to get milk. When bottle-feeding, milk often flows very easily and babies can drink the same amount of milk much faster (compared to breastfeeding). This may seem like a good way to save time, but as with many other things in life, slower is often better. If you choose a bottle that works more like a breast, with a slower flow, it allows the baby to stop and pause, the baby enjoys comfortable feeding, and the corresponding satiety signals are developed more slowly.
Research task
Usually everything goes smoothly. But from time to time, babies have difficulty swallowing. This may be due to various problems and they are not always easy to learn and understand.
This may be due to various problems and they are not always easy to learn and understand.
At the beginning of the atomic era, diagnostics were carried out using X-ray cinematography (filming of X-ray images). For the first time in history, people could see the amazing internal processes in the mouth and observe how the tongue helps to swallow. When concerns arose about the effects of radiation on technicians and patients, the practice was discontinued. Currently, video recording using ultrasound and MRI is often used. However, even with the use of less invasive methods or technologies, scientists still have to find ways to study babies while breastfeeding that do not affect their actions.
Tongue Movement Study
The 2020 study "Quantification of Tongue Movement During Feeding in Infants and Swallowing in Adults" shows certain patterns. The scientists used ultrasound video to study tongue movements.
“We observed the most organized and rhythmic tongue movements in infants who were exclusively breastfed, less mobility in those who had conditions that interfere with normal feeding, such as tongue tie, and more “disorganized movements with bottle feeding than breastfeeding,” the researchers report. “This highlights the key role of tongue movements in breast or bottle sucking.”
Disorganized movements with bottle feeding than with breastfeeding,” researchers report. “This highlights the key role of tongue movements in breast or bottle sucking.” They could also observe differences in tongue mobility before and after treatment in infants with tongue and lip frenulum. And for the first time, pictures of a baby with torticollis during breastfeeding and bottle feeding were obtained. The results showed "slightly less rhythmic sucking than usual during breastfeeding and irregular sucking during bottle feeding."
Although this study was limited, the use of ultrasound video was effective in obtaining objective information about tongue movements. As more scientists use this technique, we'll get more information about how language works and we'll be able to get more accurate information about natural feeding and how to deal with it.
Share this article:
Similar articles
Are you not a healthcare professional?
References
Genna CW, Saperstein Y, Siegel SA, Laine AF, Elad D.