Baby feeding recommendations
Feeding Guide for the First Year
Feeding Guide for the First Year | Johns Hopkins MedicineHealth
Reviewed By:
Tiffani Hays, M.S., R.D., L.N., Director of the Pediatric Clinical Nutrition Education & Practice
Making appropriate food choices for your baby during the first year of life is very important. More growth occurs during the first year than at any other time. It’s important to feed your baby a variety of healthy foods at the proper time. Starting good eating habits at this early stage will help set healthy eating patterns for life.
Recommended Feeding Guide for the First Year
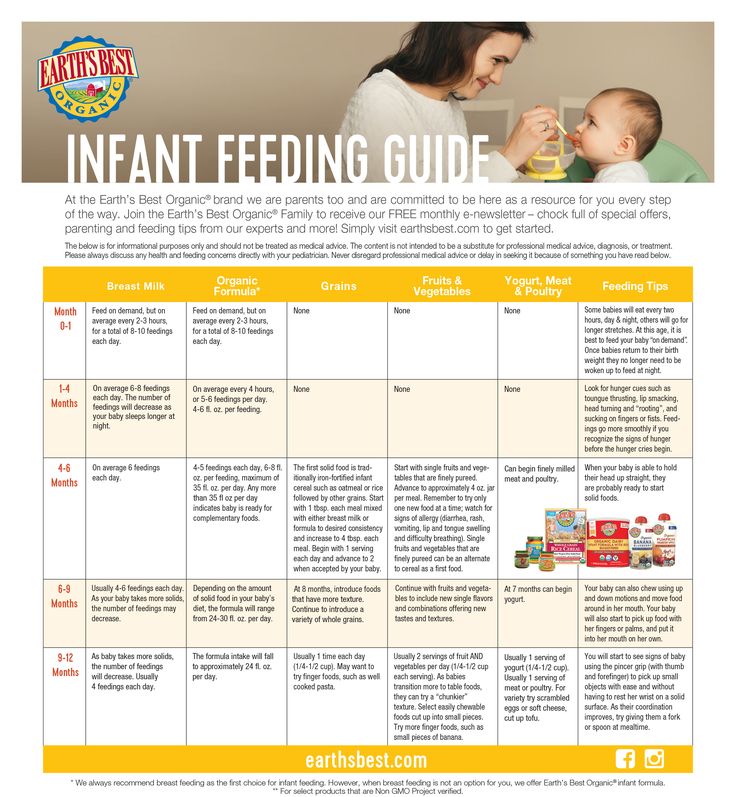
Breast milk and formula are designed to be the primary sources of nutrition throughout an infant’s first year of life. You should talk with your baby’s health care provider before starting solid foods. Solid foods should not begin before age 4 months because:
- Breast milk or formula provide your baby with all the nutrients that are needed.
- Your baby isn’t physically developed enough to eat solid food from a spoon.
- Feeding your baby solid food too early may result in poor feeding experiences and increased weight gain in both infancy and early childhood.
The American Academy of Pediatrics (AAP) recommends that all infants, children and adolescents take in enough vitamin D through supplements, formula or cow’s milk to prevent complications from deficiency of this vitamin. In November 2008, the AAP updated its recommendations for daily intake of vitamin D for infants, children, and adolescents who are healthy. It is now recommended that the minimum intake of vitamin D for these groups should be 400 IU per day, beginning soon after birth. Your baby’s health care provider can recommend the proper type and amount of vitamin D supplement.
Guide for Breast-feeding (Zero to 12 Months)
- In the early days after a baby’s birth, the mother should plan to breast-feed every two to three hours, including overnight. The mother should respond to the infant’s cues of hunger in a prompt and relaxed manner, providing a quiet and comfortable environment for both herself and the baby. Frustrated or distracted infants may have difficulties latching on.
- It is normal for infants to wake up overnight to feed for the first several months. If you have any concerns about overnight feeding, please discuss them with your health care provider.
- Alternate breasts to feed on, and allow the infant to completely empty the breast before switching to the other. This practice ensures the infant receives hindmilk, which is richer in nutrients.
- Follow your child’s feeding cues and resist forcing a schedule. Instead, rely on keeping track of wet diapers and your child’s growth to judge whether he or she is receiving enough breast milk.
 A mother’s milk changes as the infant grows, and feeding habits change as well in order to best meet a child’s needs. If you have any questions about whether your child is receiving enough breast milk, ask your health care provider.
A mother’s milk changes as the infant grows, and feeding habits change as well in order to best meet a child’s needs. If you have any questions about whether your child is receiving enough breast milk, ask your health care provider. - When not able to breast-feed, use a breast pump to extract milk and maintain milk supply. Pumped breast milk should be stored safely, using appropriate temperature guidelines. Pumped breast milk may be offered to infants in bottles, while responding to the same feeding cues to determine how much they take. Forcing bottles to be emptied may result in overfeeding and excess weight gain, even when feeding breast milk.
- With the proper support, a mother can meet the needs of most infants, even twins, so seek out help from your health care provider or lactation consultant for success.
Guide for Formula Feeding (Zero to 12 Months)
- When breast milk is not available, standard infant formula is an appropriate alternative for most healthy full term infants, but there are some differences between brands.
 Do not hesitate to ask your health care provider for a recommendation if you are unsure which formula to use.
Do not hesitate to ask your health care provider for a recommendation if you are unsure which formula to use. - Bottle-feeding should be interactive, with the caregiver holding both the bottle and the infant. Propping a bottle has been linked to an increased risk of ear infections and tooth decay.
- Formula feeding should be in response to the infant’s needs and not based on a predetermined schedule. Look for cues of hunger and fullness to determine both when to feed and how much. The number of wet diapers per day and your child’s growth will reflect if he or she is getting enough formula. The chart below demonstrates common intakes for infants at various stages. However, ask your health care provider if you have any questions about how much formula your infant is taking.
- The amount of formula an infant takes will decrease as the baby increases intake of solid foods, but formula remains a significant source of calories, protein, calcium and vitamin D for the first year of life.

- Ask your health care provider before switching an infant less than 1 year of age from formula to cow’s milk or a cow’s milk alternative.
| Age | Amount of formula per feeding | Number of feedings per 24 hours |
|---|---|---|
| 1 month | 2 to 4 ounces | six to eight |
| 2 months | 5 to 6 ounces | five to six |
| 3 to 5 months | 6 to 7 ounces | five to six |
Complementary Feedings (After 6 Months of Age)
Beverages
- Offer only breast milk or formula in bottles until 1 year of age unless specifically advised by your health care provider.

- Begin offering breast milk and/or formula in a cup starting at 6 months of age. Infants should drink breast milk and/or formula for the first year of life.
- Fruit juice is not recommended under 1 year of age.
- When introducing juice, offer 100% pasteurized juice and limit it to 4–6 ounces per day. Do NOT place juice in a bottle.
- Avoid giving any sugar-sweetened beverages to infants.
Solid Foods
- Introduce solid foods when your infant is ready, at around 6 months of age depending on the infant’s development. Infants are ready to start eating solid foods when they can:
- sit up on their own or with a little support
- reach for and put things in their mouth
- open their mouth when seeing something coming
- keep food in their mouth rather than pushing it out onto the chin
- move food to the back of their mouth with their tongue
- turn their head away when they do not want something
- Prepare to introduce solid foods in a calm feeding environment where the infant is sitting upright and is appropriately supported and moderately hungry.

- Start with small amounts of solid food, feeding with a spoon or allowing finger feeding, then gradually increase the amount as the infant eats more and develops. Avoid offering breast milk or formula until after the solid-food experience has wound down.
- Expose infants to a wide variety of flavors and textures of healthy food. Don’t limit your baby’s food choices to the ones you like. Offering a range of foods early will pave the way for healthy eating habits.
- Maintain the division of responsibility when feeding.
- The caregiver is responsible for what to eat (offering appropriate variety and textures).
- The child is responsible for deciding whether to eat and how much.
- Avoid adding salt or sugar to make baby foods more appealing. Many babies and toddlers need to experience a new food multiple times before accepting it, and increased intakes of salt and sugar among children are associated with obesity in adults.

- Observe infants for any signs of intolerance when introducing a new food or texture, and discuss all concerns with your health care provider.
- Although convenient and safe, commercial baby foods are not required. Young children are more likely to eat foods they see others eating, so as long as they are observed to see how they handle new food in their mouths, baby-led weaning using table foods is an appropriate way to introduce solids.
- Avoid honey in any form during your child’s first year, as it can cause infant botulism. Address any concerns about developing food allergies with your health care provider.
- Don’t restrict fat and cholesterol in the diets of very young children, unless advised by your child’s health care provider. Children need calories, fat and cholesterol for the development of their brains and nervous systems, and for general growth.
Updated on July 26, 2019.
Related
-
Developmental Milestones: Babies and Toddlers
Well-Care Visits
-
Nutrition: Adolescent
Nutritional Deficiencies
-
Nutrition
Toddler Nutrition
Related Topics
How Often and How Much Should Your Baby Eat?
By: Sanjeev Jain, MD, FAAP
One of the most common questions new parents have is how often their baby should eat. The best answer is surprisingly simple: in general, babies should be fed whenever they seem hungry.
How do I know when my baby is hungry?
For babies born
prematurely or with certain medical conditions, scheduled feedings advised by your pediatrician are best. But for most healthy, full-term infants, parents can look to their baby rather than the clock for hunger cues. This is called feeding on demand, or
responsive feeding.
But for most healthy, full-term infants, parents can look to their baby rather than the clock for hunger cues. This is called feeding on demand, or
responsive feeding.
Hunger cues
A hungry baby often will cry. But it's best to watch for hunger cues before the baby starts crying, which is a late sign of hunger and can make it hard for them to settle down and eat.
Some other typical hunger cues in babies:
Licking lips
Sticking tongue out
Rooting (moving jaw and mouth or head in search of breast)
Putting his/her hand to mouth repeatedly
Opening her mouth
Fussiness
Sucking on everything around
It is important to realize, however, that every time your baby cries or sucks it is not necessarily because he or she is hungry. Babies suck not only for hunger, but also for comfort; it can be hard at first for parents to tell the difference. Sometimes, your baby just needs to be cuddled or changed.
Sometimes, your baby just needs to be cuddled or changed.
General guidelines for baby feeding
It is important to remember all babies are different―some like to snack more often, and others drink more at one time and go longer between feedings. However, most babies will drink more and go longer between feedings as they get bigger and their tummies can hold more milk:
Most newborns eat every 2 to 3 hours, or 8 to 12 times every 24 hours. Babies might only take in half ounce per feeding for the first day or two of life, but after that will usually drink 1 to 2 ounces at each feeding. This amount increases to 2 to 3 ounces by 2 weeks of age.
At about 2 months of age, babies usually take 4 to 5 ounces per feeding every 3 to 4 hours.
At 4 months, babies usually take 4 to 6 ounces per feeding.
At 6 months, babies may be taking up to 8 ounces every 4 to 5 hours.

Most babies will increase the amount of formula they drink by an average of 1 ounce each month before leveling off at about 7 to 8 ounces per feeding. Solid foods should be started at about 6 months old.
Concerns about overfeeding or underfeeding your baby
Too full?
Babies are usually pretty good at eating the right amount, but they can sometimes take in more than they need. Infants who are bottle feeding may be more likely to overfeed, because drinking from a bottle may take less effort than breastfeeding.
Overfed babies can have stomach pains, gas, spit up or vomit and be at higher risk for obesity later in life. It's better to offer less, since you can always give more if your baby wants it. This also gives babies time to realize when they're full.
If you are concerned your baby wants to eat
all the time―even when he or she is full―talk with your pediatrician.
Pacifiers may be used after feeding to help sooth healthy-weight babies who like to suck for comfort, rather than nutrition. For babies who are breastfed, it's best to wait to offer pacifiers until around 3 to 4 weeks of age, when breastfeeding is well-established.
For babies who are breastfed, it's best to wait to offer pacifiers until around 3 to 4 weeks of age, when breastfeeding is well-established.
Trouble gaining weight?
Most babies will double their birth weight by 5 months of age and triple their birth weight by their first birthday. If your baby is having trouble gaining weight, don't wait too long between feeding―even if it means waking your baby. Be sure to talk with your pediatrician about how often and how much to feed your baby.
How do I know if my baby is getting enough to eat?
Daily diapers
A newborn's diaper is a good indicator of whether he or she is getting enough to eat. In the first few days after birth, a baby should have 2 to 3 wet diapers each day. After the first 4 to 5 days, a baby should have at least 5 to 6 wet diapers a day. Stool frequency is more variable and depends whether your baby is breastfed or formula fed.
Growth charts
During regular health check-ups, your pediatrician will check your baby's weight and plot it on a
growth chart. Your baby's progress on the growth chart is one way to tell whether or not they are getting enough food. Babies who stay in healthy growth percentile ranges are
probably getting a healthy amount of food during feedings.
Your baby's progress on the growth chart is one way to tell whether or not they are getting enough food. Babies who stay in healthy growth percentile ranges are
probably getting a healthy amount of food during feedings.
Remember
Talk with your pediatrician if you have any questions or concerns about your baby getting the right amount to eat.
More information:
- Making Sure Your Baby is Getting Enough Milk
- Amount and Schedule of Formula Feedings
- Is Your Baby Hungry or Full? Responsive Feeding Explained (Video)
- Remedies for Spitty Babies
- Ask the Pediatrician: With the baby formula shortage, what should I do if I can't find any?
- Ask the Pediatrician: How should we feed our baby if we're running low on money?
-
Airplane Choo Choo: A Feeding Guide for Children (National Dairy Council)
About Dr. Jain:
Sanjeev Jain, MD, FAAP, is a Clinical Associate Professor of General Pediatrics and Adolescent Medicine at the University of Wisconsin School of Medicine and Public Health. Within the American Academy of Pediatrics, he is a member of the Section on International Child Health and the Wisconsin State Chapter.
Within the American Academy of Pediatrics, he is a member of the Section on International Child Health and the Wisconsin State Chapter.
The information contained on this Web site should not be used as a substitute for the medical care and advice of your pediatrician. There may be variations in treatment that your pediatrician may recommend based on individual facts and circumstances.
WHO | Supplementary feeding
In cases where breast milk is no longer sufficient to meet the nutritional needs of the infant, supplementary food should be included in the child's diet. The transition from exclusive breastfeeding to food consumed in the family, which is called supplementary feeding, usually occurs between 6 and 18-24 months of age, which is a very vulnerable stage. This is when the onset of malnutrition in many infants is a significant factor in the high prevalence of malnutrition among children under five years of age worldwide.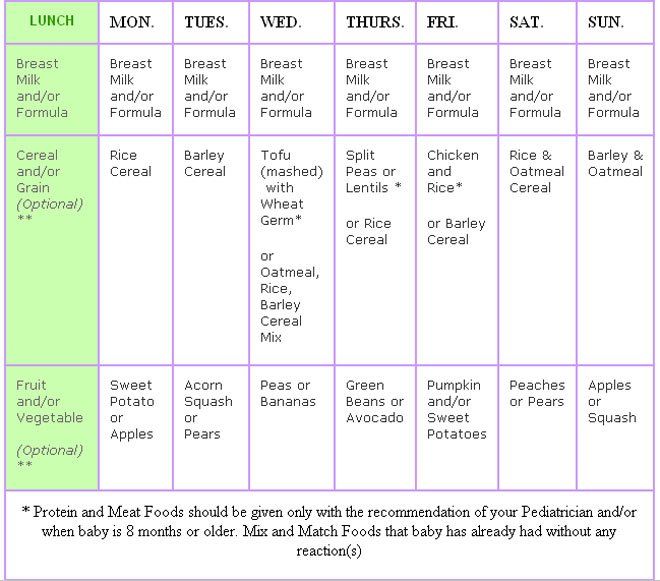 WHO estimates that 2 out of 25 children in low-income countries are stunted.
WHO estimates that 2 out of 25 children in low-income countries are stunted.
WHO/J. Muriel
Complementary feeding should be timely, which means that all infants should begin to receive nutrition in addition to breast milk from 6 months. It must be adequate, which means that complementary foods should be given in the quantity, frequency, sequence, and variety of foods to meet the nutritional needs of the growing baby while breastfeeding continues. Food should be prepared and served in a safe manner, that is, care should be taken to minimize the risk of pathogen contamination. And they should be fed in an appropriate way, which means that their texture should be appropriate for the age of the child and that flexible feeding is applied, following the principles of psycho-social care.
The adequacy of complementary foods (adequacy is a shorthand for timely, adequate, safe and appropriate) depends not only on the availability of a variety of foods in the family, but also on the feeding methods used by caregivers. Feeding young children requires active care and stimulation, where the caregiver responds to the child's signals of hunger and encourages the child to eat. Such feeding is also referred to as active or flexible feeding.
Feeding young children requires active care and stimulation, where the caregiver responds to the child's signals of hunger and encourages the child to eat. Such feeding is also referred to as active or flexible feeding.
WHO recommends that infants be given complementary foods from 6 months in addition to breast milk, initially 2-3 times a day at 6-8 months of age, increasing to 3-4 times a day at 9-11 months, and at 12-24 months additionally include 1-2 times a day additional nutritious food, if desired.
Inappropriate feeding practices are often a more important determinant of inadequate food intake than family food availability. WHO has developed a protocol for tailoring feeding recommendations to allow program managers to find out local feeding practices, common feeding problems and suitable complementary foods. The protocol builds on existing information and suggests that improved feeding recommendations be tested in families. WHO recommends using this protocol to develop interventions to improve complementary nutrition and include it in the process of adapting the Integrated Management of Childhood Illness strategy.
Research has shown that caregivers need skilled support to feed their infants properly. Guidelines on appropriate feeding are included in the Early Childhood Feeding Advisory, Guidelines and First-Level Health Workers Training Course on Integrated Management of Childhood Illness. WHO has produced a guide, Supplementary Feeding: Family Table Food for Breastfed Children, which provides more detailed guidance for health care workers on how to support supplementary feeding.
The WHO Global Consultation on Supplementary Feeding, 10-13 December 2001, resulted in updated recommendations on good feeding practices and guidance for program managers on their implementation. Background material prepared for these consultations is published in the Special Supplement to Food and Nutrition Bulletin 24(1) 2003 and supplements the WHO/UNICEF publication Supplementary Feeding of Young Children in Developing Countries: A Review of Current Scientific Knowledge, 1998, WHO/NUT/98.1. The Pan American Health Organization Guidelines on Complementary Feeding for Breastfed Children (2003) summarize the current scientific evidence on supplementary feeding and are intended to guide policy and programmatic action at the global, national and local levels, and The Guidelines for Feeding Non-Breastfeeding Children 6-24 Months of Age (2005) provide guidance on feeding children who are not breastfed.
Based on new knowledge, WHO, in collaboration with partners, has developed updated indicators for infant and young child feeding, including supplementary feeding. As a result, three publications have been produced: definitions, measurement and country profiles.
Publications
- Feeding newborns and young children: publications
Related links
- Promoting adequate feeding for infants and young children
- Exclusive breastfeeding
- Global Strategy for Infant and Young Child Nutrition
- World Health Organization recommendations for infant nutrition
Breastfeeding a newborn | What to Expect in the First Week
The first week of a baby's life is a wonderful but hectic time, especially if you haven't breastfed before. Our breastfeeding tips will help you settle in as quickly as possible
Share this information
The first time after giving birth, mothers are often confused. The body is still recovering, and you are already starting to get to know your newborn baby. The emotional state during this period can be unstable, especially between the second and fifth days, when many women have milk 1 and at the same time postpartum depression begins 2 . In addition, people around often expect (and demand) that a woman come to her senses as soon as possible and become a “super mom”. But the best thing to do this first week is just to be with your baby and get breastfeeding going.
The body is still recovering, and you are already starting to get to know your newborn baby. The emotional state during this period can be unstable, especially between the second and fifth days, when many women have milk 1 and at the same time postpartum depression begins 2 . In addition, people around often expect (and demand) that a woman come to her senses as soon as possible and become a “super mom”. But the best thing to do this first week is just to be with your baby and get breastfeeding going.
When should I start breastfeeding my newborn?
Try to breastfeed your baby within the first hour after birth. When the baby latch onto the breast and begins sucking rhythmically, it stimulates the mammary gland cells and starts milk production. 1 It is not for nothing that this time is called the “magic hour”!
“Ideally, the baby should be placed on the mother's stomach immediately after birth so that it can immediately attach to the breast. He won't necessarily eat, but he should be able to,” explains Cathy Garbin, an internationally recognized expert on breastfeeding.
He won't necessarily eat, but he should be able to,” explains Cathy Garbin, an internationally recognized expert on breastfeeding.
“Hold your baby and let him find the breast on his own and put the nipple in his mouth. This is called the breast-seeking reflex. On the Internet you can watch videos that show what this process looks like. If the baby does not latch onto the nipple on its own, the midwife will help to properly attach it to the breast. But for starters, it’s good to give the baby the opportunity to do it on their own. In this case, the optimal position for the mother is reclining. ”
Don't spend that special first hour of your baby's life weighing and swaddling—or at least wait until he's suckling for the first time. Enjoy hugs and close skin-to-skin contact. This promotes the production of oxytocin, the hormone of love, in you and your baby, and oxytocin plays a key role in the supply of the first breast milk - colostrum. 3
“As soon as the obstetricians were convinced that our son was healthy, the three of us — me, my husband and our baby — were left to give us the opportunity to get to know each other. It was a very special hour - an hour of awkwardness, turbulent emotions and bliss. During this time, I breastfed my son twice, ”recalls Ellie, a mother of two from the UK.
It was a very special hour - an hour of awkwardness, turbulent emotions and bliss. During this time, I breastfed my son twice, ”recalls Ellie, a mother of two from the UK.
Did you know that breastfeeding helps to recover after childbirth? This is because oxytocin stimulates uterine contractions. In the first hours after childbirth, this contributes to the natural release of the placenta and reduces blood loss. 4
What if the birth did not go according to plan?
If you had a caesarean section or other complications during childbirth,
You can still establish skin-to-skin contact with your baby and breastfeed him in the first hours after birth.
“If you can't hold your baby, have your partner do it for you and make skin-to-skin contact with the baby. This will give the baby a sense of security, care and warmth so that he can hold on until you recover, ”Katie advises.
If the baby is unable to breastfeed, it is advisable to start expressing milk as early as possible and do so as often as possible until the baby is able to feed on its own. “While breastfeeding in the first hours after birth lays an excellent foundation for the future, it is not so important,” Cathy reassures. “It is much more important to start lactation so that in the future, if necessary, you can start breastfeeding.”
“While breastfeeding in the first hours after birth lays an excellent foundation for the future, it is not so important,” Cathy reassures. “It is much more important to start lactation so that in the future, if necessary, you can start breastfeeding.”
To start milk production, you can express milk manually or use a breast pump that can be given to you at the hospital. 5 And with expressed precious colostrum, you can feed your baby. This is especially important if the baby was born premature or weak, since breast milk is extremely healthy.
If a baby was born prematurely or has a medical condition and cannot be breastfed immediately, this is no reason not to continue breastfeeding. “I have worked with many new mothers who were unable to breastfeed their baby for the first six weeks due to preterm labor or other reasons. Nevertheless, all of them later successfully switched to breastfeeding,” says Kathy.
Does the baby latch on correctly?
Correct breastfeeding is a prerequisite for successful breastfeeding 6 , as it determines how effectively the baby will suckle milk, and therefore grow and develop. Latching on the breast incorrectly can cause sore or damaged nipples, so don't hesitate to ask your doctor to check that your baby is properly attached to the breast, even if you are told that everything is fine and you do not see obvious problems - especially while you are in the hospital.
Latching on the breast incorrectly can cause sore or damaged nipples, so don't hesitate to ask your doctor to check that your baby is properly attached to the breast, even if you are told that everything is fine and you do not see obvious problems - especially while you are in the hospital.
“While I was in the hospital, I called the doctor at every feed and asked me to check if I was breastfeeding correctly,” says Emma, mother of two from Australia. - There were several cases when it seemed to me that everything seemed to be right, but it was painful to feed, and the doctor helped me take the baby off the breast and attach it correctly. By the time I was discharged, I had already learned to do it confidently.”
When applying to the breast, point the nipple towards the palate. This will allow the baby to take the nipple and part of the areola under it into their mouth. It will be easier for him to suck if he has both the nipple and part of the areola around in his mouth. 6
6
“When a baby latch on properly, it doesn't cause discomfort and it causes a pulling sensation, not pain,” Cathy explains. - The baby's mouth is wide open, the lower lip may be slightly turned outward, and the upper one lies comfortably on the chest. The body language of the child indicates that he is comfortable. There isn't much milk at this early stage, so you probably won't notice your baby swallowing, but he will suckle a lot and nurse frequently."
How often should a newborn be fed?
The frequency and duration of breastfeeding in the first week can vary greatly. “The first 24 hours of life are completely different for different children. Someone sleeps a lot (after all, childbirth is tiring!), And someone often eats, says Katie. - Such a variety greatly confuses young mothers. Everyone gives different advice, so it's important to remember that every mother and child is different."
“Colostrum is thicker than mature breast milk and is produced in smaller amounts, but has many benefits. When the baby eats colostrum, he learns to suck, swallow and breathe until milk begins to flow in more volume, ”explains Cathy.
When the baby eats colostrum, he learns to suck, swallow and breathe until milk begins to flow in more volume, ”explains Cathy.
Milk usually arrives on the second or fourth day after delivery. Until this time, the baby is applied to the breast 8-12 times a day (and sometimes more often!), including at night. 7 Feeding may last 10-15 minutes at this stage, or 45 minutes or even an hour, as the baby is just beginning to develop the muscles and coordination needed to suckle effectively.
“At first, the intensity of feeding is very high, often higher than many people realize, and this is shocking to most new mothers,” says Cathy. - Sometimes mom has no time to go to the toilet, take a shower and have a snack. It usually comes as a surprise."
Camille, a mother from Australia, experienced this. “The first week, Frankie ate every two hours, day and night, and each time it took half an hour to an hour to feed,” she recalls. “My husband and I were completely exhausted!”
Do I need to feed my newborn on a schedule?
The good news is that frequent feeding promotes lactation and stimulates milk production.![]() 7 The more your baby eats, the more milk you will have. Therefore, forget about feeding your newborn on a schedule - this way he will have less chance of feeding. Try to feed your baby when he signals that he is hungry 8 :
7 The more your baby eats, the more milk you will have. Therefore, forget about feeding your newborn on a schedule - this way he will have less chance of feeding. Try to feed your baby when he signals that he is hungry 8 :
- tossing and turning in his sleep;
- opens eyes;
- turns his head if he feels a touch on his cheek;
- sticks out tongue;
- groans;
- licks lips;
- sucks fingers;
- is naughty;
- whimpers;
- is crying.
Crying is the last sign of hunger, so if in doubt, just offer your baby the breast. If he bursts into tears, it will be more difficult to feed him, especially at first, when both of you are just learning how to do it. As your baby grows, he will likely eat less frequently and take less time to feed, so breastfeeding will seem more predictable.
Does breastfeeding hurt?
You may have heard that breastfeeding is not painful at all, but in fact, in the first days, many new mothers experience discomfort. And this is not at all surprising, given that the nipples are not used to such frequent and strong sucking.
And this is not at all surprising, given that the nipples are not used to such frequent and strong sucking.
“Breastfeeding can be uncomfortable for the first couple of days – your body and your baby are just getting used to it. If a baby eats for too long and does not latch well, the sensations are almost the same as from unworn new shoes, Cathy compares. Just as tight shoes can rub your feet, improper suckling can damage your nipples. Prevention is always better than cure, so if the pain persists after a few days of feeding, contact a lactation consultant or healthcare professional.”
Maria, a mother from Canada, agrees: “Although my son seemed to latch onto the breast well, he damaged his nipples while feeding, and I was in pain. As it turned out, the reason was a shortened frenulum of the tongue. The breastfeeding specialists at our city clinic have been of great help in diagnosis and treatment.”
In addition, you may experience period cramps during the first few days after breastfeeding, especially if this is not your first baby.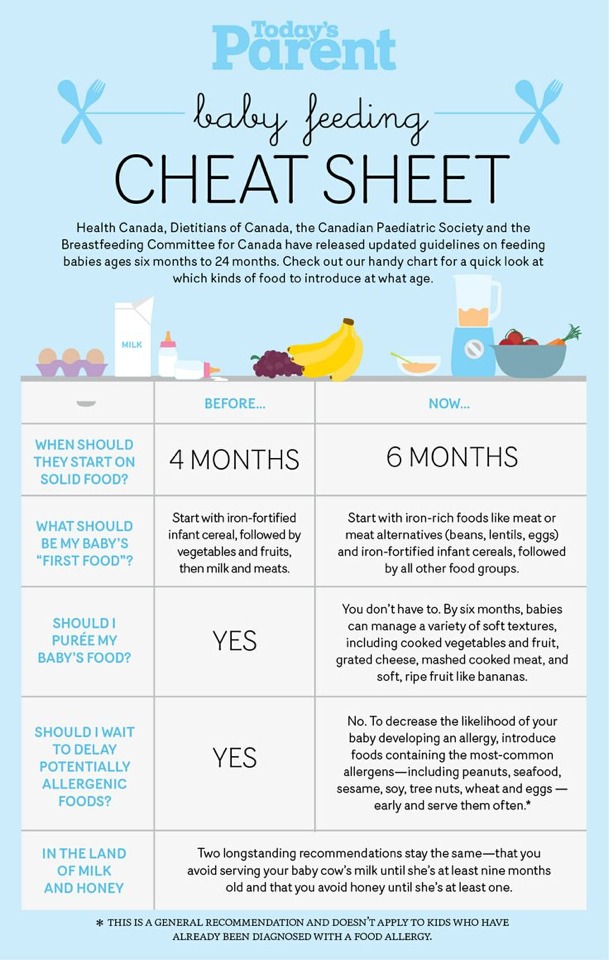 This is the so-called postpartum pain. The fact is that oxytocin, which is released during breastfeeding, contributes to further contraction of the uterus to restore its normal size. 4
This is the so-called postpartum pain. The fact is that oxytocin, which is released during breastfeeding, contributes to further contraction of the uterus to restore its normal size. 4
When milk arrives, the breasts usually become fuller, firmer and larger than before delivery. In some women, the breasts swell, harden and become very sensitive - swelling of the mammary glands occurs. 10 Frequent breastfeeding relieves these symptoms. For more breast care tips, read our article What is Breast Swelling?
How often does a newborn urinate and defecate?
What goes into the body must go back out. Colostrum
has a laxative effect, helping to eliminate meconium - the original feces. It looks a little scary - black and sticky, like tar. 11 But don't worry, it won't always be like this. Breastfed babies usually have a slightly sweet smell of stool.
How many times a day you will need to change diapers and how the contents should look like, see below.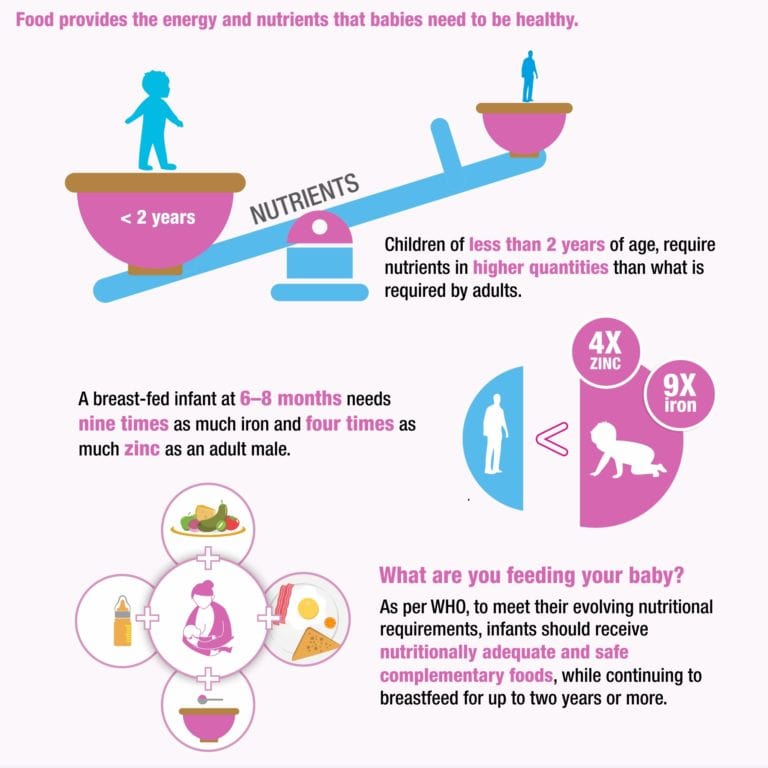
Day one
- Frequency: once or more.
- Colour: greenish black.
- Texture: sticky like tar.
Second day
- Frequency: twice or more.
- Colour: dark greenish brown.
- Texture: less sticky.
Day three
- Frequency: twice or more.
- Colour: greenish brown to brownish yellow.
- Texture: non-sticky.
Fourth day and then the entire first month
- Frequency: twice or more.
- Color: yellow (feces should turn yellow no later than by the end of the fourth day).
- Texture: grainy (like mustard with grains interspersed). Leaky and watery.
The baby's urine should be light yellow. On average, babies urinate once a day for the first two days. Starting around the third day, the number of wet diapers increases to three, and from the fifth day onwards, diapers have to be changed five times a day or more often. In addition, during the first few days, the weight of wet diapers increases. 11
In addition, during the first few days, the weight of wet diapers increases. 11
Is the baby getting enough breast milk?
Since very little milk is produced at first,
You may feel that your baby is not getting enough milk. But if you feed your baby on demand, you will produce exactly as much milk as he needs. If you want to keep the process under control, be guided by the frequency of diaper changes above. If your baby soils less diapers, check with your doctor.
“For the first three or four weeks, most babies just eat and sleep. If the child is worried and constantly asks for a breast, you should consult with your doctor, ”Katie recommends.
Sometimes the baby may vomit after feeding. If the vomit is the color of milk, this is not a cause for concern. But if there are orange, red, green, brown or black blotches in it, or the child vomits with a "fountain", consult a doctor. You should also consult a doctor if the baby has a high temperature, the fontanel (soft spot on the head) has sunk, blood is found in the stool, and also if the weight recorded at birth has not recovered within two weeks.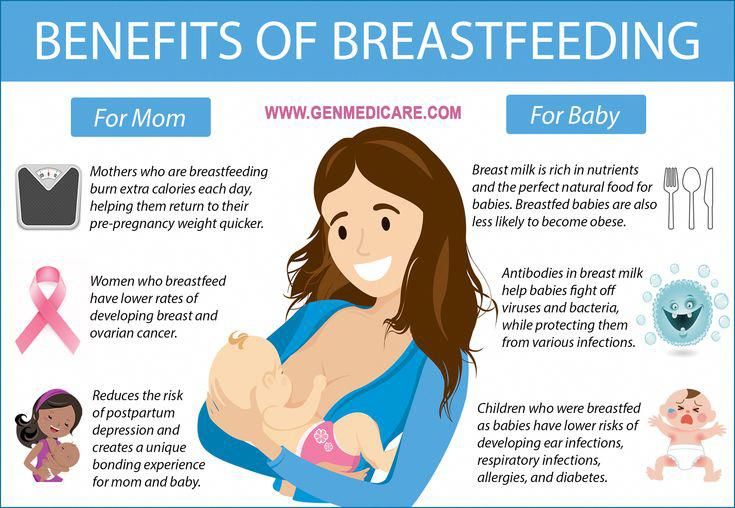 11
11
But if there are no frightening symptoms and the baby is growing at a normal pace, it means that he has enough milk. Soon you will both get used to breastfeeding and establish a more stable routine.
For the next step in breastfeeding, see Breastfeeding the First Month: What to Expect.
Literature
1 Pang WW, Hartmann PE. Initiation of human lactation: secretory differentiation and secretory activation. J Mammary Gland Biol Neoplasia 2007;12(4):211-221. - Pang, W.W., Hartmann, P.I., "Lactation initiation in the lactating mother: secretory differentiation and secretory activation." G Mammary Gland Biol Neoplasia. 2007;12(4):211-221.
2 Shashi R et al. Postpartum psychiatric disorders: Early diagnosis and management. Indian J Psychiatry . 2015; 57( Suppl 2): S 216– S 221. - Shashi R. et al., Postnatal mental disorders: early diagnosis and treatment. Indian J Saikiatri. 2015; 57(App 2):S216-S221.
2015; 57( Suppl 2): S 216– S 221. - Shashi R. et al., Postnatal mental disorders: early diagnosis and treatment. Indian J Saikiatri. 2015; 57(App 2):S216-S221.
3 Moberg KU, Prime DK. Oxytocin effects in mothers and infants during breastfeeding. Infant . 2013;9(6):201-206. - Moberg K, Prime DK, "The effects of oxytocin on mother and child during breastfeeding." Infant. 2013;9(6):201-206.
4 Sobhy SI, Mohame NA. The effect of early initiation of breast feeding on the amount of vaginal blood loss during the fourth stage of labor. J Egypt Public Health Assoc . 2004;79(1-2):1-12. - Sobhi SI, Moham NA, "Early initiation of breastfeeding and its effect on vaginal bleeding in the fourth stage of labor." F Egyptian Public Health Assoc.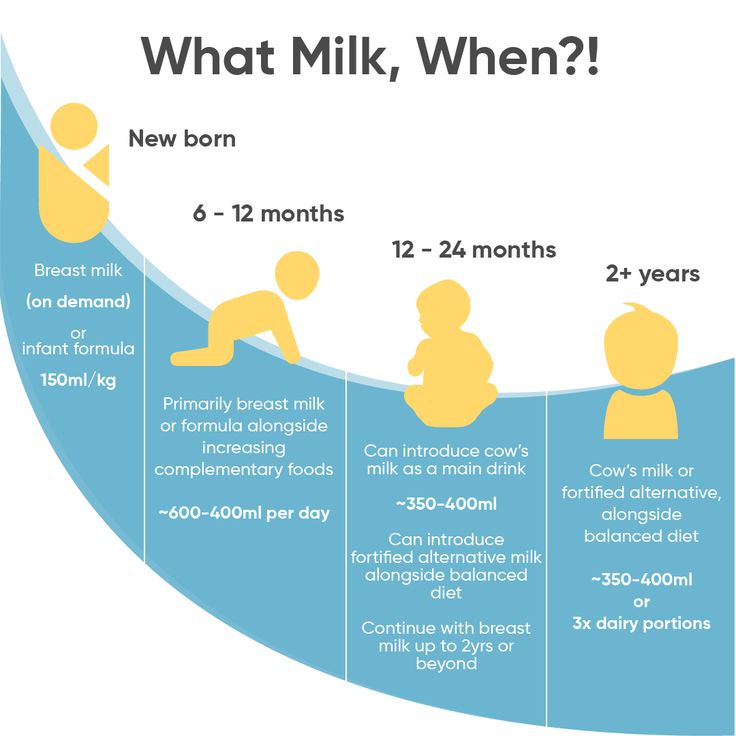 2004;79(1-2):1-2.
2004;79(1-2):1-2.
5 Meier PP et al. Which breast pump for which mother: an evidence-based approach to individualizing breast pump technology. J Perinatol . 2016;36(7):493. - Meyer P.P. et al., Breastpump Selection: A Scientific Approach to Customizing Pumping Technology. J Perinatol (Journal of Perinatology). 2016;36(7):493-499.
6 Cadwell K. Latching - On and Suckling of the Healthy Term Neonate: Breastfeeding Assessment. J Midwifery & Women ’ s Health . 2007;52(6):638-642. — Cadwell, K., "Latching and sucking in healthy newborns: evaluation of breastfeeding." F Midwifery Women Health. 2007;52(6):638-642.
7 Kent JC et al. Principles for maintaining or increasing breast milk production. J Obstet , Gynecol , & Neonatal Nurs .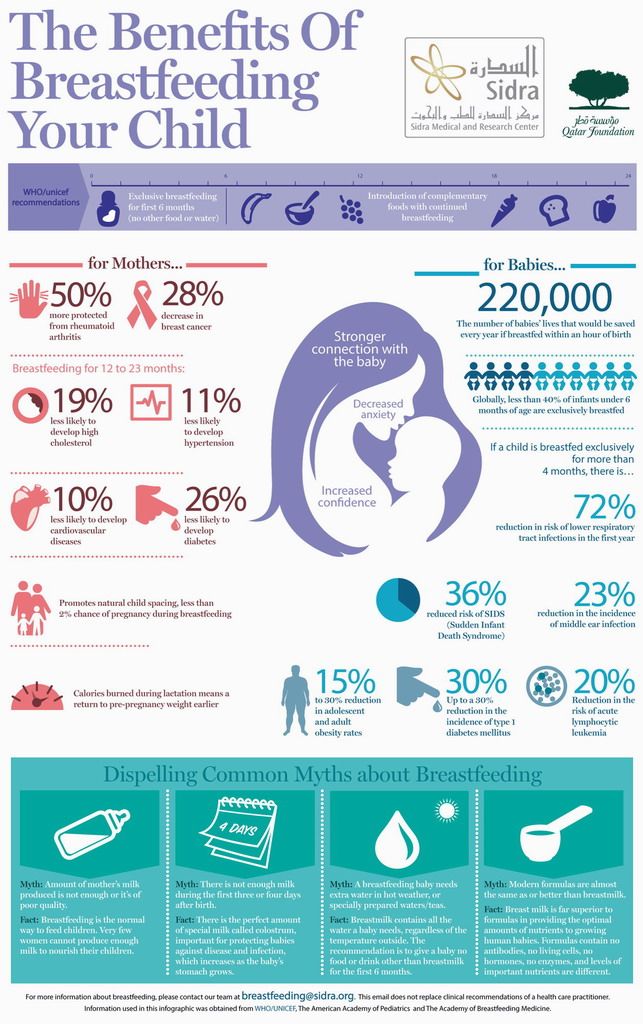 2012;41(1):114-121. - Kent J.S. et al., "Principles for Maintaining and Increasing Milk Production". J Obstet Ginecol Neoneutal Nurs. 2012;41(1):114-121.
2012;41(1):114-121. - Kent J.S. et al., "Principles for Maintaining and Increasing Milk Production". J Obstet Ginecol Neoneutal Nurs. 2012;41(1):114-121.
8 Australian Breastfeeding Association [ Internet ]. Feeding cues ; 2017 Sep [ cited 2018 Feb ]. - Australian Breastfeeding Association [Internet], Feed Ready Signals; September 2017 [cited February 2018]
9 Jacobs A et al. S3-guidelines for the treatment of inflammatory breast disease during the lactation period. Geburtshilfe Frauenheilkd . 2013;73(12):1202-1208. - Jacobs, A. et al., Guidelines S -3 for the management of inflammatory breast disease during breastfeeding. Geburtskhilfe und Frauenheilkünde. 2013;73(12):1202-1208.