Baby food bacterial contamination
Cronobacter Infection and Infants | Cronobacter Infection and Infants
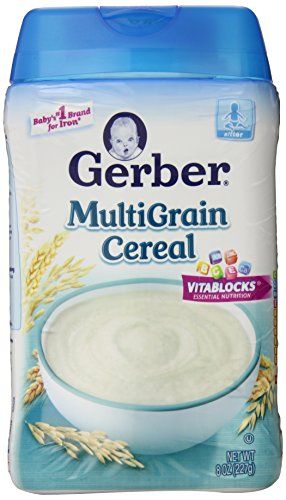
Cronobacter infections are often reported among infants who have been fed powdered infant formula.
Getting sick from Cronobacter does not happen often, but infections in infants can be deadly. Cronobacter infections in infants less than 12 months old are often linked to powdered infant formula. If your baby is fed with powdered infant formula, you can take steps to protect your baby from sickness.
Cronobacter sakazakii is a germ found naturally in the environment.
These germs can live in dry foods, such as:
- Powdered infant formula
- Powdered milk
- Herbal teas
- Starches
Rare but Serious Illness in Infants
Cronobacter infections are rare, but they can be deadly in newborns. Infections in infants usually occur in the first days or weeks of life. About two to four cases are reported to CDC every year, but this figure may not reflect the true number of illnesses. That’s because most hospitals and laboratories are not required to report Cronobacter infections to health departments.
Cronobacter germs can cause a dangerous blood infection (sepsis). They can also make the linings surrounding the brain and spinal cord swell (meningitis).
Infants who are more likely to get sick include:
- Infants 2 months and younger. These infants are most likely to develop meningitis if they get sick from Cronobacter.
- Infants born prematurely.
- Infants with weakened immune systems. Babies with this condition can’t fight germs as well because of illness or medical treatment, such as chemotherapy for cancer.
Cronobacter illness in infants will usually start with a fever and poor feeding, excessive crying, or very low energy. Some infants may also have seizures. You should take an infant with these symptoms to a medical provider as soon as possible.
Cronobacter infection can also be serious for:
- People 65 years and older.

- People who have immune systems weakened due to illnesses or conditions, such as HIV, organ transplants, or cancer.
Follow These Five Guidelines to Protect Your Baby From
CronobacterYou may want to take extra precautions if your baby is younger than 2 months old, was born prematurely, or has a weakened immune system:
Wash your hands with soap and water, especially before preparing bottles and feeding your baby.
1. Breastfeed if you can. Breastfeeding is one of the best things you can do for your baby’s health and development. Health officials and medical providers report very few cases of Cronobacter infection in infants fed only breast milk.
2. Clean, sanitize, and store feeding items such as baby bottles and breast pump parts safely. Help prevent germs from growing on these items and keep your baby’s milk safe. You can do this by carefully cleaning, sanitizing, and storing bottles and breast pump parts. Take apart bottles and breast pump equipment after use for thorough cleaning.
Take apart bottles and breast pump equipment after use for thorough cleaning.
3. Keep hands clean! Always wash your hands with soap and water for at least 20 seconds during key times:
- Before preparing and feeding bottles or food to your baby
- Before touching your baby’s mouth
- Before touching pacifiers or other things that go into your baby’s mouth
- After using the toilet or changing diapers
If soap and water are not available, use a hand sanitizer with at least 60% alcohol. Check the product label to be sure. Wash hands with soap and water as soon as possible after using hand sanitizer. Hand sanitizer with at least 60% alcohol kills Cronobacter. But hand sanitizer does not kill all types of germs. It may not work as well if hands are visibly greasy or dirty.
4. If you feed your baby with formula, consider using liquid formula when possible. Powdered infant formula is not sterile and might have germs in it. Using a liquid formula instead of powdered is especially important if your baby:
Using a liquid formula instead of powdered is especially important if your baby:
- Is less than 2 months old
- Was born prematurely, or
- Has a weakened immune system.
Liquid infant formula is made to be sterile (without germs). This means liquid formula should not make your baby sick with Cronobacter infection when you follow the instructions on the container.
You do not need to warm infant formula before feeding, but some people like to warm their baby’s bottle. If you do warm the bottle, never use a microwave. Microwaves heat milk and food unevenly, resulting in “hot spots” that can burn your baby’s mouth and throat.
- To warm a bottle, place it under warm running water. Keep the running water from getting into the bottle or on the nipple. Put a couple drops of infant formula on the inside of your wrist to make sure it is not too hot.
Keep all surfaces and feeding items clean when preparing infant formula. This includes all countertops, feeding items (nipples, caps, rings, valves), and objects that may enter the baby’s mouth, such as pacifiers and teethers.
This includes all countertops, feeding items (nipples, caps, rings, valves), and objects that may enter the baby’s mouth, such as pacifiers and teethers.
5. Prepare and store powdered infant formula safely. Make sure that your formula is not expired or recalled. The container should be in good condition with no dents, puffy ends, or rust spots. Keep powdered formula lids and scoops clean. Close containers of formula as soon as possible.
In most cases, it is safe to mix powdered infant formula following manufacturer’s instructions on the container. But, if your baby may be at higher risk, consider taking these extra steps to prepare your powdered formula with hot water (at least 158°F/70°C):
- Clean work surfaces, such as countertops and sinks, with soap and water, or use a disinfectant wipe or paper towel sprayed with cleaning product. Do not place feeding items directly in the sink, because germs in sinks or drains could contaminate these items.

- Wash hands with soap and water before preparing infant formula.
- Boil water and let it cool for about 5 minutes.
- Pour the water into a clean bottle or feeding cup.
- Add the exact amount of formula listed on the container.
- Carefully shake the capped bottle rather than stirring the mixture.
- If you plan to use the prepared formula right away, cool the formula to body temperature to ensure it is not too hot before feeding your baby. Run the prepared, capped bottle under cool water or place it into an ice bath. Do not let the cooling water get into the bottle or on the nipple.
- Before feeding the baby, test the formula’s temperature by putting a few drops on the inside of your wrist. It should feel warm, not hot.
Use prepared infant formula within 1 hour from start of feeding and within 2 hours of preparing it. If your baby does not finish the entire bottle of formula, throw away leftover formula.
If you do not plan to start feeding your baby with the prepared formula right away, put it in the refrigerator immediately.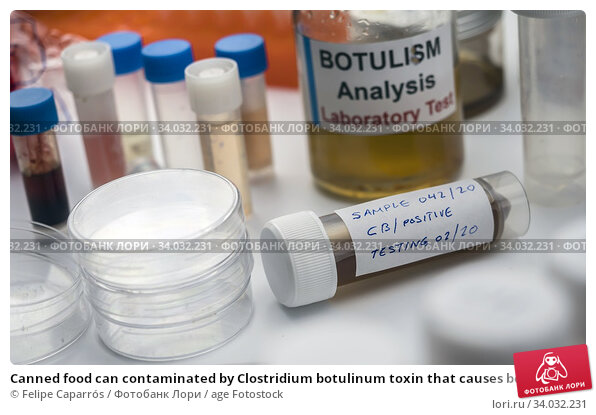 Use formula in the refrigerator within 24 hours. Throw out formula if you can’t remember how long you have kept it in the refrigerator. Do not feed it to your baby. For more information, visit CDC’s Infant Formula Preparation and Storage webpage.
Use formula in the refrigerator within 24 hours. Throw out formula if you can’t remember how long you have kept it in the refrigerator. Do not feed it to your baby. For more information, visit CDC’s Infant Formula Preparation and Storage webpage.
Baby formula recall spotlights rare, dangerous Cronobacter sakazakii bacteria
A recall of powdered baby formula from Abbott Laboratories is highlighting the danger of Cronobacter sakazakii, a bacterium that causes that causes rare but serious infections in infants.
Last month, the Food and Drug Administration announced it was investigating powdered formula linked to an Abbott facility in Sturgis, Michigan, following four reports that infants who had consumed it became seriously ill. Two of the infants have died. Abbott has issued a voluntary recall for some batches of its Similac, Alimentum and EleCare formulas.
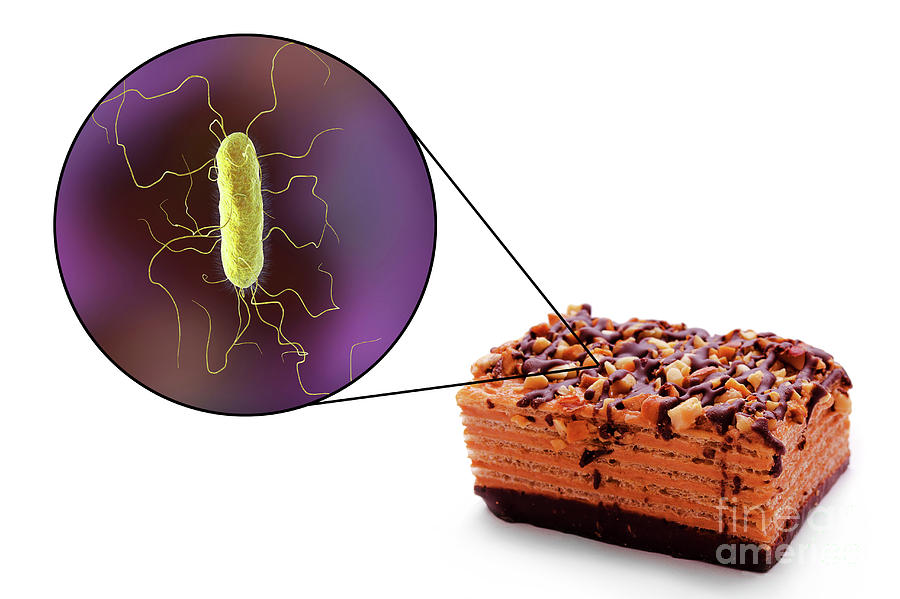
Cronobacter is found naturally in the environment and can live in dry foods, including powdered formulas, powdered milk and starches, according to the Centers for Disease Control and Prevention. It can affect people of all ages, but it is especially dangerous in infants.
It can affect people of all ages, but it is especially dangerous in infants.
Cronobacter is rare but serious
In addition to the four Cronobacter reports, the FDA also found one case of salmonella in an infant in connection with the Abbott facility. The agency has advised consumers to avoid Abbott powdered formula if the first two digits of the product code on the bottom of the package are 22 through 37; if the code includes K8, SH or Z2; or if the expiration date is April 1, 2022, or later.
Early signs of Cronobacter infection in babies under 1 year old are fever, crying, low energy and poor feeding habits. The bacterium can get into their bloodstreams and cause meningitis.
In older people, Cronobacter can enter the urinary tract or cause problems in cuts, scrapes or places where people have had surgery, according to the CDC.
The agency typically gets just two to four reports of Cronobacter in infants a year, although it notes that infection rates are not well understood because Minnesota is the only state that requires its Health Department to be notified of cases. In Minnesota, Cronobacter infections in infants under 1 year old must be reported within one working day. The four recent Cronobacter cases were reported in Minnesota, Ohio and Texas.
In Minnesota, Cronobacter infections in infants under 1 year old must be reported within one working day. The four recent Cronobacter cases were reported in Minnesota, Ohio and Texas.
Bill Marler, a Seattle-based food safety lawyer, said thorough reporting of food-borne illnesses is important because it is a way to "count people who are sick and to see what the common denominator is between them."
"The more people who have their illness reported, the more likely it is you’ll figure out what the problem is sooner, so then you can get the product off the market so less people get sick," Marler said.
How to protect your babyAbbott said in a statement that in its testing, no distributed product has tested positive for either Cronobacter or salmonella.
"Additionally, retained samples related to the three complaints for Cronobacter sakazakii tested negative for Cronobacter sakazakii," the company said. "And the retained sample related to the complaint for Salmonella Newport tested negative for Salmonella Newport. "
"
Marler said concerned parents can protect their children from possible Cronobacter exposure by practicing good hygiene habits, like keeping bottles clean.
The CDC recommends that powdered formula containers be stored properly, with clean lids and scoops. For babies born prematurely or those who have weakened immune systems, parents should heat water that gets mixed with the powder to 158 degrees Fahrenheit, then let the mixture cool.
"This is a good reminder for parents to use good methods when feeding their kids infant formula," Marler said.
Minyvonne Burke
Minyvonne Burke is a senior breaking news reporter for NBC News.
Botulism
Botulism- Popular Topics
- Air pollution
- Coronavirus disease (COVID-19)
- Hepatitis
- Data and statistics »
- News bulletin
- The facts are clear
- Publications
- Find Country »
- A
- B
- C
- D
- E
- e
- ё 9000
- x
- C
- h
- Sh
9000 WHO in countries » - Reporting
- Regions »
- Africa
- America
- Southeast Asia
- Europe
- Eastern Mediterranean
- Western Pacific
- Media Center
- Press releases
- Statements
- Media messages
- Comments
- Reporting
- Online Q&A
- Developments
- Photo reports
- Questions and answers
- Update
- Emergencies "
- News "
- Disease Outbreak News
- WHO Data »
- Dashboards »
- COVID-19 Monitoring Dashboard
- Basic moments "
- About WHO »
- CEO
- About WHO
- WHO activities
- Where does WHO work?
- Governing Bodies »
- World Health Assembly
- Executive committee
- Main page/
- Media Center /
- Newsletters/
- Read more/
- Botulism
\n
\nThe spores produced by Clostridium botulinum are resistant to high temperatures and are widely distributed in the environment. In the absence of oxygen, these spores germinate, develop, and begin to release toxins. There are 7 different forms of botulinum toxin - types A - G. Four of them (types A, B, E and in rare cases F) cause human botulism. Types C, D, and E cause disease in mammals, birds, and fish.
In the absence of oxygen, these spores germinate, develop, and begin to release toxins. There are 7 different forms of botulinum toxin - types A - G. Four of them (types A, B, E and in rare cases F) cause human botulism. Types C, D, and E cause disease in mammals, birds, and fish.
\n
\nBotulinum toxins enter the body through the consumption of foods that have not been properly processed, in which bacteria or spores survive and produce toxins. The main cause of human botulism is food intoxication, but it can be caused by intestinal infection in infants, wound infections, and inhalation.
\n
Symptoms of foodborne botulism
\n
\nBotulinum toxins are neurotoxic and therefore affect the nervous system. Foodborne botulism is characterized by descending flaccid paralysis, which can lead to respiratory failure.
\n
\nEarly symptoms are extreme fatigue, weakness, and dizziness, usually followed by blurred vision, dry mouth, and difficulty swallowing and speaking. Vomiting, diarrhea, constipation, and bloating may also occur. As the disease progresses, weakness in the neck and arms may occur, after which the respiratory muscles and muscles of the lower body are affected. The temperature does not rise and loss of consciousness does not occur.
Vomiting, diarrhea, constipation, and bloating may also occur. As the disease progresses, weakness in the neck and arms may occur, after which the respiratory muscles and muscles of the lower body are affected. The temperature does not rise and loss of consciousness does not occur.
\n
\nThe cause of these symptoms is not the bacterium itself, but the toxin it produces. Symptoms usually appear 12–36 hours (minimum 4 hours and maximum 8 days) after exposure. The incidence of botulism is low, but the mortality rate is high unless a correct diagnosis is made promptly and treatment provided promptly (early antitoxin and intensive mechanical ventilation). The disease can be fatal in 5-10% of cases.
\n
Exposure and transmission
\n
Foodborne botulism
\n
\nC. botulinum is an anaerobic bacterium, which means that it can only grow in the absence of oxygen. Foodborne botulism occurs when the bacteria C. botulinum grows and produces toxins in foods before they are consumed. C. botulinum produces spores that are widely distributed in the environment, including soil, as well as river and sea water.
Foodborne botulism occurs when the bacteria C. botulinum grows and produces toxins in foods before they are consumed. C. botulinum produces spores that are widely distributed in the environment, including soil, as well as river and sea water.
\n
\nBacterial growth and toxin production occur in products with low oxygen content and at a certain combination of storage temperature and preservation parameters. This occurs most often in lightly preserved foods, as well as in foods that have not been properly processed, canned or bottled at home. In an acidic environment (pH less than 4.6), C. botulinum does not grow, and therefore no toxin is produced in acidic foods (however, low pH levels do not destroy previously produced toxins). Low storage temperatures are also used in combination with certain levels of salt and/or acidity to prevent bacterial growth and toxin production.
\n
\nBotulinum toxin is found in a wide range of foods, including low acid canned vegetables such as green beans, spinach, mushrooms, and beets; fish such as canned tuna, fermented, salted and smoked fish; and meat products such as ham and sausages. Food varies from country to country and reflects local dietary habits and food preservation practices. Sometimes botulinum toxins are found in industrial products.
Food varies from country to country and reflects local dietary habits and food preservation practices. Sometimes botulinum toxins are found in industrial products.
\n
\nAlthough C. botulinum spores are resistant to high temperatures, the toxin produced by bacteria that develop from spores under anaerobic conditions is destroyed by boiling (for example, at an internal temperature of >85C for five or more minutes). Therefore, the most common cause of human botulism is ready-to-eat foods in packages with a low oxygen content.
\n
\nTo determine the cause and prevent further cases, samples of the food involved in suspected cases should be obtained immediately, placed in appropriate sealed containers, and sent to laboratories.
\n
Infant botulism
\n
\nInfant botulism occurs mainly in infants under 6 months of age. Unlike foodborne botulism, which is caused by the consumption of already produced toxins in food (see point a above), infantile botulism occurs when children ingest C. botulinum spores, which develop into bacteria that colonize the intestines and release toxins. For most adults and children over 6 months of age, this does not happen because the natural defense mechanisms of the intestine that develop later prevent spores from germinating and bacteria from growing.
Unlike foodborne botulism, which is caused by the consumption of already produced toxins in food (see point a above), infantile botulism occurs when children ingest C. botulinum spores, which develop into bacteria that colonize the intestines and release toxins. For most adults and children over 6 months of age, this does not happen because the natural defense mechanisms of the intestine that develop later prevent spores from germinating and bacteria from growing.
\n
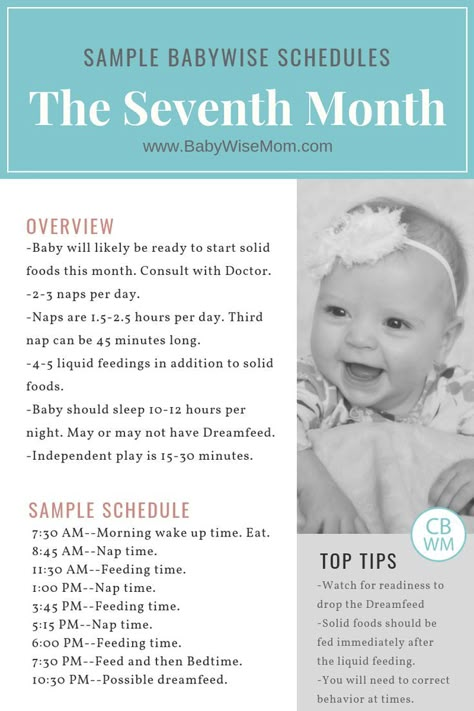
\nClinical symptoms in infants include constipation, loss of appetite, weakness, altered crying, and marked loss of head control. There are several possible sources of infant botulism infection, but a number of cases have been associated with honey contaminated with spores. Therefore, parents and caregivers should not give honey to children under 1 year of age.
\n
Wound botulism
\n
\nWound botulism rarely develops when spores enter an open wound and are able to multiply under anaerobic conditions. Symptoms are similar to foodborne botulism but may take up to two weeks to appear. This form of the disease is associated with substance abuse, in particular heroin injections.
Symptoms are similar to foodborne botulism but may take up to two weeks to appear. This form of the disease is associated with substance abuse, in particular heroin injections.
\n
Botulism due to inhalation
\n
\nBotulism rarely results from inhalation. Such incidents do not occur naturally, but are associated, for example, with accidental or deliberate events (such as bioterrorism) that result in the release of toxins in aerosols. The clinical picture of inhaled botulism is similar to that of foodborne botulism. The median lethal dose in humans is estimated at 2 nanograms of botulinum toxin per kilogram of body weight, which is about 3 times higher than that of foodborne botulism.
\n
\nSymptoms appear 1-3 days after exposure to toxins, or longer for lower levels of intoxication. Symptoms develop in the same way as in foodborne botulism, and the final stage is muscle paralysis and respiratory failure.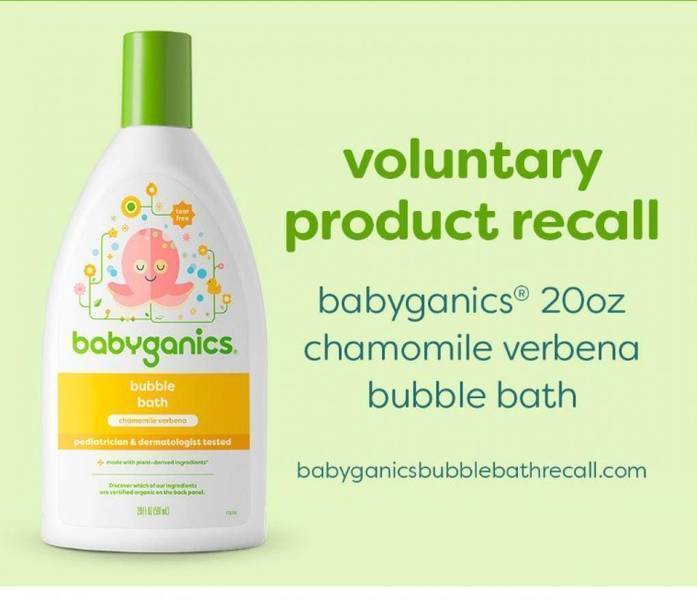
\n
\nIf aerosol exposure to a toxin is suspected, additional exposure to the patient and others must be prevented. The patient's clothing should be removed and stored in plastic bags until thoroughly laundered in soapy water. The patient should take a shower and be disinfected immediately.
\n
Other types of intoxication
\n
\nTheoretically, botulism can be transmitted through water by ingestion of a toxin previously produced. However, given the fact that water treatment (such as boiling or disinfecting with 0.1% hypochlorite) destroys the toxin, this risk is considered low.
\n
\nBotulism of undetermined origin is usually reported in adults in cases where the source of foodborne or wound botulism has not been identified. These cases are comparable to childhood botulism and may occur when the normal intestinal flora is altered as a result of surgery or antibiotic therapy.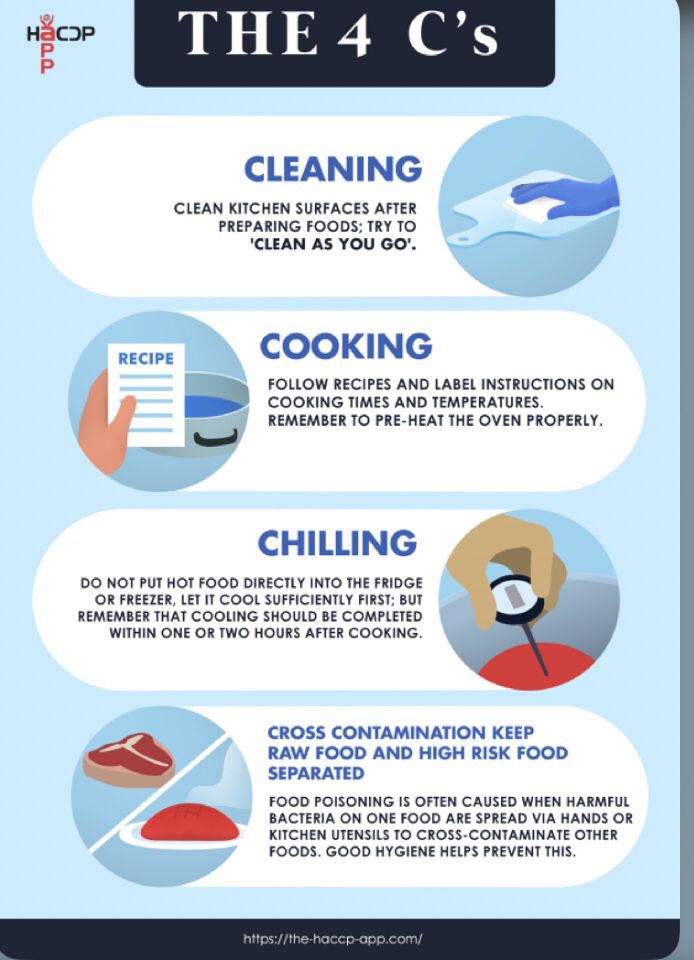
\n
\nAdverse reactions to a pure toxin used in medical and/or cosmetic applications among patients have been reported, see Botox section below for more information.
\n
Botox
\n
\nThe C. botulinum bacterium is used to produce Botox, a pharmaceutical drug used primarily for clinical and cosmetic injections. Botox uses purified and highly diluted botulinum neurotoxin type A. Treatments are performed in healthcare settings according to the needs of the patient and are generally well tolerated, although adverse reactions have been observed in rare cases.
\n
Diagnosis and treatment
\n
\nDiagnosis is usually based on clinical history and clinical examination followed by laboratory confirmation, including demonstration of the presence of botulinum toxin in serum, stool, or food, or culture of C. botulinum in specimens stool, wound fluid or food. Botulism is sometimes misdiagnosed as it is often mistaken for a stroke, Guillain-Barré syndrome, or myasthenia gravis.
botulinum in specimens stool, wound fluid or food. Botulism is sometimes misdiagnosed as it is often mistaken for a stroke, Guillain-Barré syndrome, or myasthenia gravis.
\n
\nAfter a clinical diagnosis is made, the antitoxin should be administered as soon as possible. Early administration of antitoxin effectively reduces mortality rates. In the case of severe botulism, supportive care is required, in particular mechanical ventilation, which may be required for several weeks and even months. Antibiotics are not required (except in cases of wound botulism). There is a vaccine against botulism, but it is rarely used because its efficacy has not been fully evaluated and adverse reactions have been reported.
\n
Prevention
\n
\nProphylaxis of foodborne botulism is based on good food preparation practices, particularly during cooking/sterilization, and hygiene.
\n
\nFood botulism can be prevented by inactivating the bacterium and its spores in heat-sterilized (eg, autoclave) or canned foods, or by inhibiting bacterial growth and toxin production in other foods. Vegetative forms of the bacterium can be killed by boiling, but spores can remain viable even when boiled for several hours. However, spores can be destroyed by heat treatment at very high temperatures, such as industrial canning
\n
\nIndustrial heat pasteurization (including vacuum-packed and hot-smoked pasteurized foods) may not be sufficient to kill all spores and therefore the safety of these foods must be based on preventing bacterial growth and toxin production. Low temperatures, combined with the salt content and/or acidic environment, inhibit bacterial growth and toxin production.
\n
\nThe WHO Five Essentials for Safer Eating serves as the basis for educational programs to train food handlers and preparers and to educate their consumers.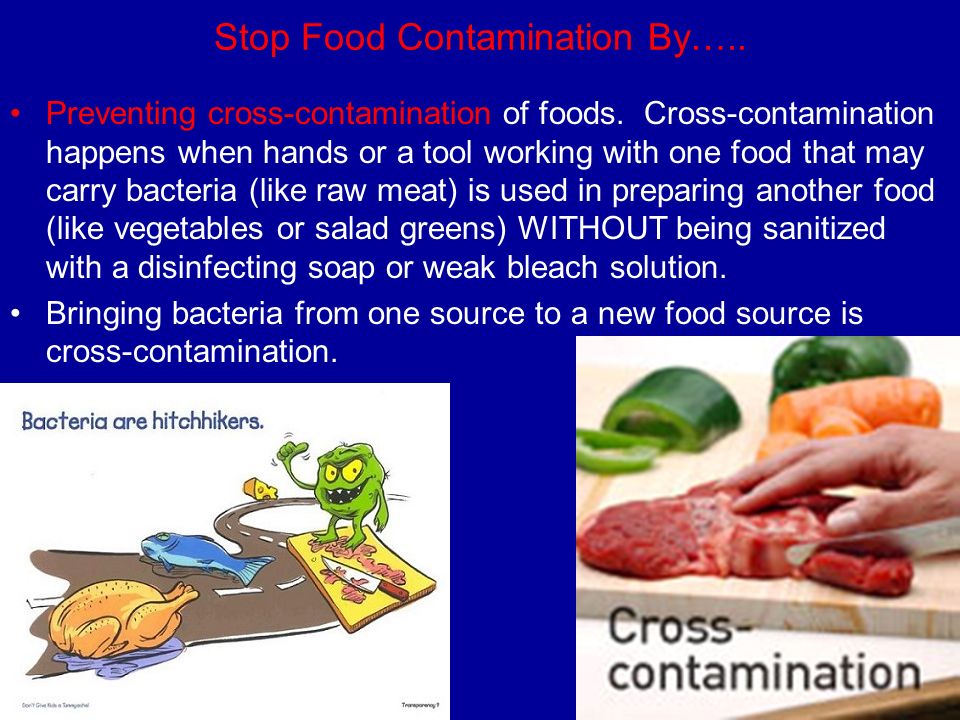 They are especially important in preventing food poisoning.
They are especially important in preventing food poisoning.
\n
\nThese five principles are:
\n
- \n
- keep clean; \n
- separate raw from cooked; \n
- thoroughly heat treat; \n
- store food at a safe temperature; \n
- use clean water and clean food raw materials. \n
\n
WHO activities
\n
\nOutbreaks of botulism are rare, but they are public health emergencies that require rapid recognition to identify the source of infection, determine the type of outbreak (natural, accidental or potentially intentional), preventing other cases of illness and effectively treating affected patients. The success of treatment is highly dependent on early diagnosis and prompt administration of botulinum antitoxin.
\n
\nWHO's role in responding to outbreaks of botulism that may be of international concern is: ensure rapid local detection of disease outbreaks and an effective international response. WHO's main tool for surveillance, coordination and response is the International Food Safety Authorities Network (INFOSAN), which links the national authorities of Member States responsible for managing food safety events. This network is jointly managed by FAO and WHO. \n
WHO's main tool for surveillance, coordination and response is the International Food Safety Authorities Network (INFOSAN), which links the national authorities of Member States responsible for managing food safety events. This network is jointly managed by FAO and WHO. \n

\n
","datePublished":"2018-01-10T10:22:00.0000000+00:00","image":"https://www.who.int/images/ default-source/departments/food-safety/preserved-food.jpg?sfvrsn=fab6deb7_3","publisher":{"@type":"Organization","name":"World Health Organization: WHO","logo" :{"@type":"ImageObject","url":"https://www.who.int/Images/SchemaOrg/schemaOrgLogo.jpg","width":250,"height":60}}," dateModified":"2018-01-10T10:22:00.0000000+00:00","mainEntityOfPage":"https://www.who.int/ru/news-room/fact-sheets/detail/botulism"," @context":"http://schema.org","@type":"Article"};
Key Facts
- Clostridium botulinum is a bacterium that produces dangerous toxins (botulinum toxins) in low oxygen conditions.
- Botulinum toxins are among the most powerful lethal substances known today.
- Botulinum toxins block nerve function and can lead to respiratory and muscle paralysis.
- Human botulism may refer to food botulism, infant botulism, wound botulism, and inhalation botulism or other types of intoxication.

- Foodborne botulism, caused by the consumption of improperly processed foods, is a rare but potentially fatal disease if not diagnosed promptly and treated with an antitoxin.
- Home-canned or fermented foods are one of the main sources of foodborne botulism and special precautions must be taken when preparing them.
Overview
Foodborne botulism is a severe, potentially fatal, but relatively rare disease. This is an intoxication usually caused by the consumption of highly active neurotoxins, botulinum toxins, produced in contaminated foods. Botulism is not transmitted from person to person.
The spores produced by Clostridium botulinum are resistant to high temperatures and are widely distributed in the environment. In the absence of oxygen, these spores germinate, develop, and begin to release toxins. There are 7 different forms of botulinum toxin - types A - G. Four of them (types A, B, E and in rare cases F) cause human botulism. Types C, D, and E cause disease in mammals, birds, and fish.
Types C, D, and E cause disease in mammals, birds, and fish.
Botulinum toxins enter the body through the consumption of foods that have not been properly processed, in which bacteria or spores survive and produce toxins. The main cause of human botulism is food intoxication, but it can be caused by intestinal infection in infants, wound infections, and inhalation.
Symptoms of foodborne botulism
Botulinum toxins are neurotoxic and therefore affect the nervous system. Foodborne botulism is characterized by descending flaccid paralysis, which can lead to respiratory failure.
Early symptoms are extreme fatigue, weakness, and dizziness, which are usually followed by blurred vision, dry mouth, and difficulty swallowing and speaking. Vomiting, diarrhea, constipation, and bloating may also occur. As the disease progresses, weakness in the neck and arms may occur, after which the respiratory muscles and muscles of the lower body are affected. The temperature does not rise and loss of consciousness does not occur.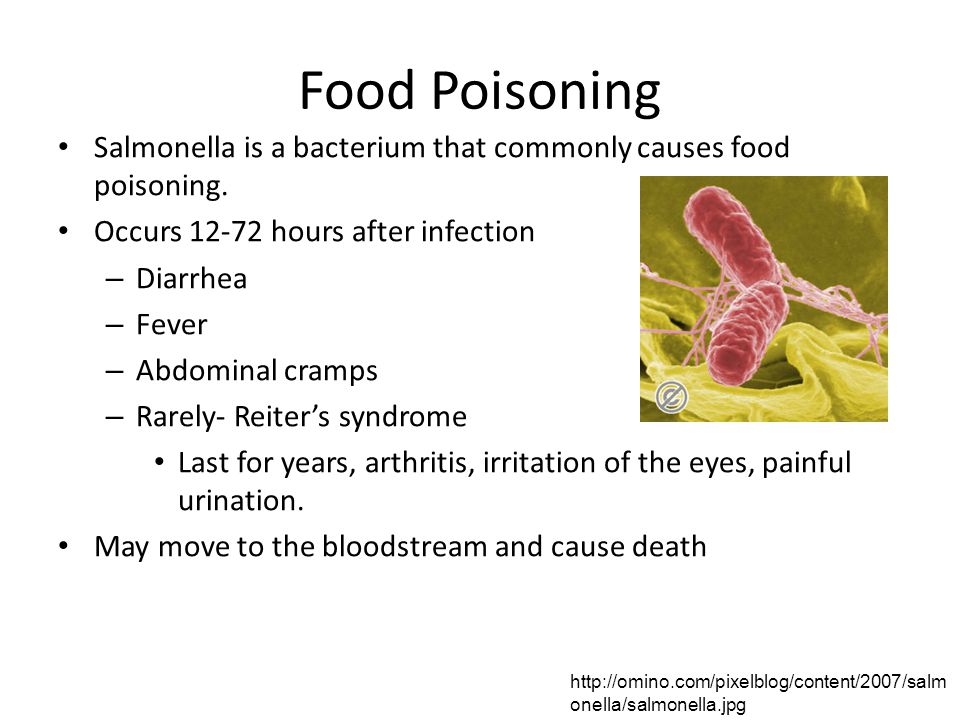
The cause of these symptoms is not the bacterium itself, but the toxin it produces. Symptoms usually appear 12–36 hours (minimum 4 hours and maximum 8 days) after exposure. The incidence of botulism is low, but the mortality rate is high unless a correct diagnosis is made promptly and treatment provided promptly (early antitoxin and intensive mechanical ventilation). The disease can be fatal in 5-10% of cases.
Exposure and transmission
Foodborne botulism
C. botulinum is an anaerobic bacterium, which means that it can only grow in the absence of oxygen. Foodborne botulism occurs when the bacteria C. botulinum grows and produces toxins in foods before they are consumed. C. botulinum produces spores that are widely distributed in the environment, including soil, as well as river and sea water.
Bacterial growth and toxin production occurs in products with low oxygen content and under a certain combination of storage temperature and preservation parameters. This occurs most often in lightly preserved foods, as well as in foods that have not been properly processed, canned or bottled at home. In an acidic environment (pH less than 4.6), C. botulinum does not grow, and therefore no toxin is produced in acidic foods (however, low pH levels do not destroy previously produced toxins). Low storage temperatures are also used in combination with certain levels of salt and/or acidity to prevent bacterial growth and toxin production.
This occurs most often in lightly preserved foods, as well as in foods that have not been properly processed, canned or bottled at home. In an acidic environment (pH less than 4.6), C. botulinum does not grow, and therefore no toxin is produced in acidic foods (however, low pH levels do not destroy previously produced toxins). Low storage temperatures are also used in combination with certain levels of salt and/or acidity to prevent bacterial growth and toxin production.
Botulinum toxin has been found in a wide range of foods, including low-acid canned vegetables such as green beans, spinach, mushrooms, and beets; fish such as canned tuna, fermented, salted and smoked fish; and meat products such as ham and sausages. Food varies from country to country and reflects local dietary habits and food preservation practices. Sometimes botulinum toxins are found in industrial products.
Although C. botulinum spores are heat tolerant, the toxin produced by bacteria that develop from spores under anaerobic conditions is destroyed by boiling (eg, internal temperature >85C for five minutes or more).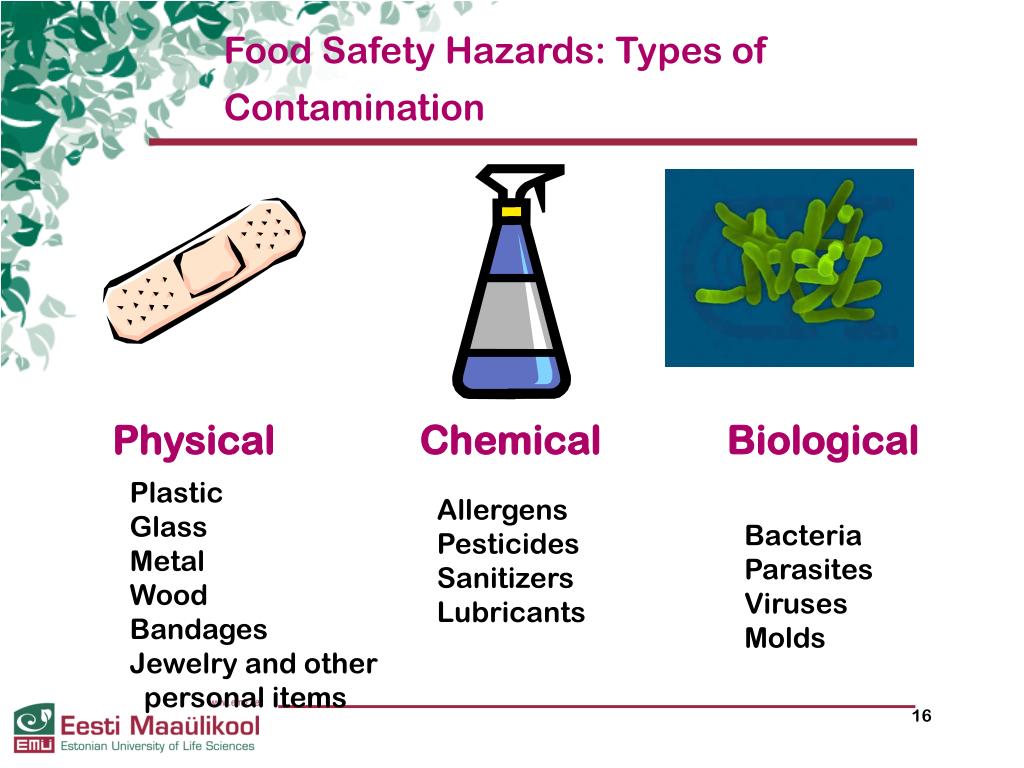 Therefore, the most common cause of human botulism is ready-to-eat foods in packages with a low oxygen content.
Therefore, the most common cause of human botulism is ready-to-eat foods in packages with a low oxygen content.
In order to determine the cause and prevent further cases of illness, samples of the products involved in suspected cases should be obtained immediately, placed in appropriate sealed containers and sent to laboratories.
Infant botulism
Infant botulism develops mainly in children under the age of 6 months. Unlike foodborne botulism, which is caused by the consumption of already produced toxins in food (see point a above), infantile botulism occurs when children ingest C. botulinum spores, which develop into bacteria that colonize the intestines and release toxins. For most adults and children over 6 months of age, this does not happen because the natural defense mechanisms of the intestine that develop later prevent spores from germinating and bacteria from growing.
Clinical symptoms in infants include constipation, loss of appetite, weakness, altered crying, and marked loss of head control. There are several possible sources of infant botulism infection, but a number of cases have been associated with honey contaminated with spores. Therefore, parents and caregivers should not give honey to children under 1 year of age.
There are several possible sources of infant botulism infection, but a number of cases have been associated with honey contaminated with spores. Therefore, parents and caregivers should not give honey to children under 1 year of age.
Wound botulism
Wound botulism rarely develops when spores enter an open wound and are able to reproduce under anaerobic conditions. Symptoms are similar to foodborne botulism but may take up to two weeks to appear. This form of the disease is associated with substance abuse, in particular heroin injections.
Inhalation botulism
Botulism rarely develops as a result of inhalation. Such incidents do not occur naturally, but are associated, for example, with accidental or deliberate events (such as bioterrorism) that result in the release of toxins in aerosols. The clinical picture of inhaled botulism is similar to that of foodborne botulism. The median lethal dose in humans is estimated at 2 nanograms of botulinum toxin per kilogram of body weight, which is about 3 times higher than that of foodborne botulism.
Symptoms appear 1–3 days after the inhalation of toxins, or after a longer period of time in the case of lower levels of intoxication. Symptoms develop in the same way as in foodborne botulism, and the final stage is muscle paralysis and respiratory failure.
If exposure to a toxin by inhalation of aerosols is suspected, additional exposure to the patient and others must be prevented. The patient's clothing should be removed and stored in plastic bags until thoroughly laundered in soapy water. The patient should take a shower and be disinfected immediately.
Other types of intoxication
Theoretically, botulism can be transmitted through water by ingestion of a toxin previously produced. However, given the fact that water treatment (such as boiling or disinfecting with 0.1% hypochlorite) destroys the toxin, this risk is considered low.
Botulism of undetermined origin is commonly reported in adults when no source of foodborne or wound botulism has been identified. These cases are comparable to childhood botulism and may occur when the normal intestinal flora is altered as a result of surgery or antibiotic therapy.
These cases are comparable to childhood botulism and may occur when the normal intestinal flora is altered as a result of surgery or antibiotic therapy.
Adverse reactions to a pure toxin used in medical and/or cosmetic applications among patients have been reported, see Botox section below for more information.
Botox
The bacterium C. botulinum is used to produce Botox, a pharmaceutical drug used primarily for injections for clinical and cosmetic purposes. Botox uses purified and highly diluted botulinum neurotoxin type A. Treatments are performed in healthcare settings according to the needs of the patient and are generally well tolerated, although adverse reactions have been observed in rare cases.
Diagnosis and treatment
Diagnosis is usually based on the clinical history and clinical examination followed by laboratory confirmation, including demonstration of the presence of botulinum toxin in serum, stool, or food, or culture of C. botulinum in stool, wound fluid, or food samples. Botulism is sometimes misdiagnosed as it is often mistaken for a stroke, Guillain-Barré syndrome, or myasthenia gravis.
Botulism is sometimes misdiagnosed as it is often mistaken for a stroke, Guillain-Barré syndrome, or myasthenia gravis.
Once a clinical diagnosis has been made, the antitoxin should be administered as soon as possible. Early administration of antitoxin effectively reduces mortality rates. In the case of severe botulism, supportive care is required, in particular mechanical ventilation, which may be required for several weeks and even months. Antibiotics are not required (except in cases of wound botulism). There is a vaccine against botulism, but it is rarely used because its efficacy has not been fully evaluated and adverse reactions have been reported.
Prevention
Prevention of foodborne botulism is based on good food preparation practices, particularly during cooking/sterilization, and hygiene.
Foodborne botulism can be prevented by inactivating the bacterium and its spores in heat-sterilized (eg, autoclaved) or canned foods, or by inhibiting bacterial growth and toxin production in other foods. Vegetative forms of the bacterium can be killed by boiling, but spores can remain viable even when boiled for several hours. However, spores can be destroyed by heat treatment at very high temperatures, such as industrial canning
Vegetative forms of the bacterium can be killed by boiling, but spores can remain viable even when boiled for several hours. However, spores can be destroyed by heat treatment at very high temperatures, such as industrial canning
Industrial heat pasteurization (including vacuum-packed and hot-smoked pasteurized products) may not be sufficient to kill all spores and therefore the safety of these products must be based on the prevention of bacterial growth and toxin production. Low temperatures, combined with the salt content and/or acidic environment, inhibit bacterial growth and toxin production.
The WHO Five Essentials for Safer Food serves as the basis for educational programs to train food handlers and preparers and to educate their consumers. They are especially important in preventing food poisoning.
These are the following five principles:
- keep clean;
- separate raw from cooked;
- conduct thorough heat treatment;
- store food at a safe temperature;
- Use clean water and clean food raw materials.

WHO activities
Outbreaks of botulism are rare, but they are public health emergencies that require rapid recognition to identify the source of infection, determine the type of outbreak (whether natural, accidental or potentially intentional), prevent other cases, and effectively treat affected patients. The success of treatment is highly dependent on early diagnosis and prompt administration of botulinum antitoxin.
WHO's role in responding to outbreaks of botulism that may be of international concern is:
- Surveillance and detection: WHO supports the strengthening of national surveillance and international alert systems to ensure rapid detection of disease outbreaks on the ground and an effective international response . WHO's main tool for surveillance, coordination and response is the International Food Safety Authorities Network (INFOSAN), which links the national authorities of Member States responsible for managing food safety events.
 This network is jointly managed by FAO and WHO.
This network is jointly managed by FAO and WHO. - Risk assessment: WHO's response is based on a risk assessment methodology that includes identifying the type of outbreak - whether it is natural, accidental, or possibly deliberate. WHO also provides scientific assessments as the basis for international food safety standards, guidelines and recommendations developed by the Codex Alimentarius Commission.
- Source isolation: WHO is coordinating with national and local authorities to contain the further spread of disease outbreaks.
- Assistance: WHO coordinates international agencies, experts, national laboratories, airlines and commercial organizations to mobilize the equipment, supplies and supplies needed for the response, including the supply and administration of botulinum antitoxin.
Israel to increase stocks of infant formula after acute US shortage
Vestiveb
17.566
3. 537
537
3.495
This decision has been made following a thorough analysis of the impact of the crisis in the United States in the first quarter of 2022. Then there was an acute shortage of mixtures in the country after a suspicion of bacterial contamination of products was revealed at the largest enterprise of the American manufacturer Similac.
So far, the Materna brand, which has over 50% of the Israeli market in the baby food sector, has been the only supplier of the state reserve for these products.
Subscribe to the Vesti telegram channel
Now, taking into account the conclusions after the crisis in the United States, for the first time a special contract will be signed with the Israeli concern Teva, which imports nutrition brand Nutrilon. Thus, the state minimizes the risks of dependence on a single large manufacturer.
In the case of a single supplier, there is a serious threat to the emergency stock. If production is jeopardized for any reason, the reserves may be affected as well. In an emergency - from an earthquake to a war - the state runs the risk of being left without the necessary amount of strategic reserves.
If production is jeopardized for any reason, the reserves may be affected as well. In an emergency - from an earthquake to a war - the state runs the risk of being left without the necessary amount of strategic reserves.
In Israel, the state reserves are administered by the National Emergency Management, which is subordinate to the Ministry of Defense. It deals, among other things, with the accumulation and storage of the necessary amount of basic foodstuffs and commodities such as wheat, sugar, butter, baby food, animal feed, medicines and much more.
Government contracted suppliers are required to keep approximately 2-3 months' worth of stock in their own warehouses and renew as needed.
One of the main problems of the US crisis is the concentration of the baby food market.
Abbott, maker of Similac blends, controls about 50% of the US market, so plant closures and supply disruptions due to the coronavirus pandemic have led to shortages so severe that US Presidential intervention has been required.-unitednaturals-050820.jpg)