Baby food gastric sleeve
Puréed Food Diet for Post-Bariatric Surgery Patients
COVID-19 Information
Read the Latest
Once you receive your surgeon's okay to progress to foods with a thicker consistency after your bariatric surgery, you can begin puréeing your foods.
Key Goals of the Puréed Food Diet (Phase 2B) After Bariatric Surgery
- Incorporate high protein foods into your diet, which helps your pouch heal.
- Women: 50–60 grams of protein
- Men: 60–70 grams of protein
- Start taking your chewable vitamin supplement with minerals.
- Drink plenty of fluids, 48–64 ounces per day.
Meal Plan for Phase 2B: Puréed Diet After Bariatric Surgery
- Consume three small meals each day.
- Protein supplements
- Gastric Bypass Patients: Begin using protein supplements after each meal to meet your daily protein requirements.
- Laparoscopic Adjustable Gastric Band Patients: Continue using protein supplements as you did in Phase 2A.
- Liquids between meals
- Wait at least 30 minutes after each meal. Then consume an 8 ounce protein supplement or shake, followed by 16 ounces of sugar free, clear liquids.
- Try to spread fluids out over a three-hour period.
- Stop drinking at least 30 minutes before mealtime.
Suggested Foods Ideas for Puréed Diet After Bariatric Surgery
Protein Sources
- Yogurt (plain or sugar free, low or nonfat, blended without fruit chunks)
- Strained cream soups (celery, potato, mushroom, or chicken made with skim milk)
- Skim milk with ½ scoop protein powder
- Protein supplements added to food or water for extra protein
- Mashed cottage cheese (low or nonfat, small curd)
- Ricotta cheese (low or nonfat)
- Scrambled eggs or egg substitute
- Puréed beef, chicken, or turkey
- Baby food meats
- White fish (cod, haddock, tilapia, orange roughy) mashed with a fork
- Canned chicken breast, mashed and moist
- Canned tuna fish in water, mashed
Grains/starches
- Cream of wheat or cream of rice
- Farina
- Grits
- Baby oatmeal
- Mashed potatoes/sweet potatoes
- Puréed winter squash
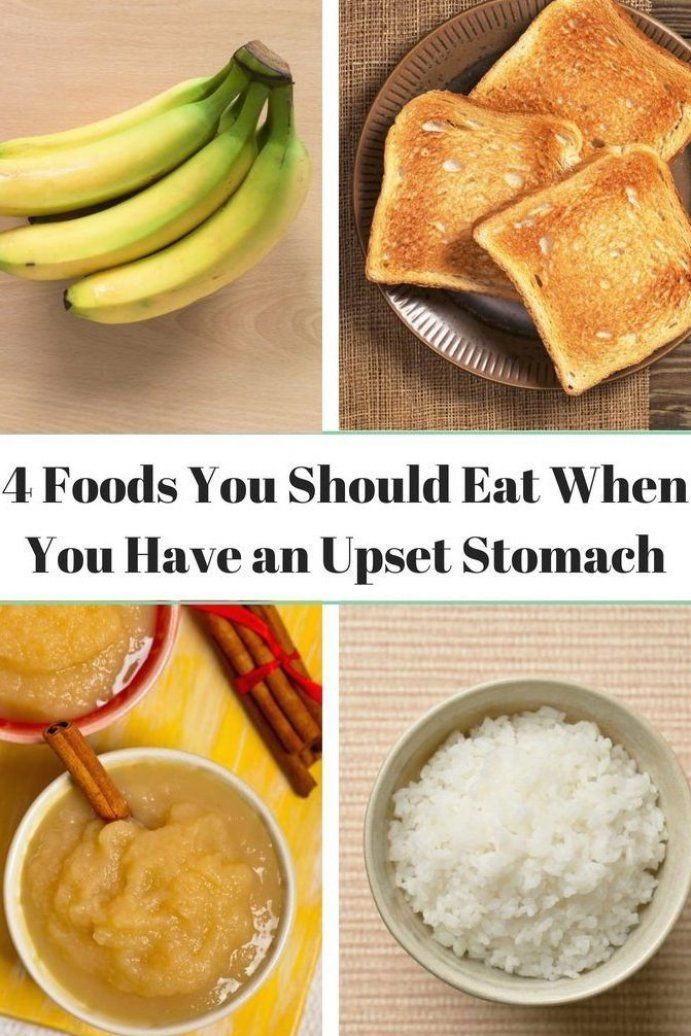
Fruits
- Diluted, 100% fruit juices (apple, grape, cranberry)
- Light juices sweetened with non-nutritive sweetener
- Applesauce
- Mashed bananas or mashed canned fruits in own juices
- Puréed peaches, apricots, pears, pineapples, melons
Vegetables
- Tomato juice
- Diet V-8 Splash® or V-8 Juice®
- Puréed spinach, carrots, summer squash or green beans
Avoid puréed broccoli, cauliflower, and other fibrous vegetables at this stage.
Sample Menu for Phase 2B: Puréed Diet After Bariatric Surgery
Eat the protein portion of your meal first, and don't forget your liquids between meals (about 30 minutes after each meal).
Breakfast
- Protein: 2 tablespoons to ¼ cup scrambled eggs or egg substitute
- Starch: 2 tablespoons to ¼ cup cream of wheat
Lunch
- Protein: 2 tablespoons to ¼ cup mashed low fat cottage cheese
- Fruit: 2 tablespoons to ¼ cup puréed peaches in own juices
Dinner
- Protein: 2 tablespoons to ¼ cup baked skinless chicken breast (puréed) or mashed canned chicken breast
- Vegetable: 2 tablespoons to ¼ cup puréed carrots
Liquid meal- If you're having a liquid meal replacement, soup, or high protein shake:
- Drink 4 ounces (1/2 cup) over 20 to 30 minutes
- Try adding mashed, canned chicken or tuna to soup to increase protein content
- Blend if needed
Suggested Recipes
View Phase 2B: Puréed Food Diet suggested recipes for post-bariatric surgery.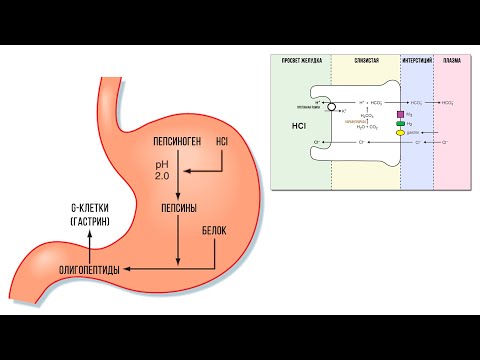
How to Purée Foods
Puréed food should be the consistency of baby food, “spoon thick.”
- Cut food into small pieces and place in blender or food processor
- Add liquid (broth, low calorie gravy or skim milk)
- Puréed until smooth
- Season food to taste
Tips and Ideas for Staying Hydrated
- Sip all fluids slowly to prevent nausea and vomiting
- Carry a water bottle with you everywhere
- Other liquids to help maintain hydration include decaffeinated coffee and tea, broth, and sugar free fruit juices with artificial sweeteners.
Next
As you receive regular checkups after your bariatric surgery, your bariatric surgeon will advise you when to advance to the next phase of your diet.
- Phase 3: Adaptive or Soft Food Diet
- Return to the overview of your diet after bariatric surgery
You Don't Need Baby Food After WLS |
Steph Wagner
January 20, 2016
Great news, right?!
If you’ve heard that you have to eat baby food after your Gastric Sleeve, Bypass, Band or Duodenal Switch surgery…I have great news for you.
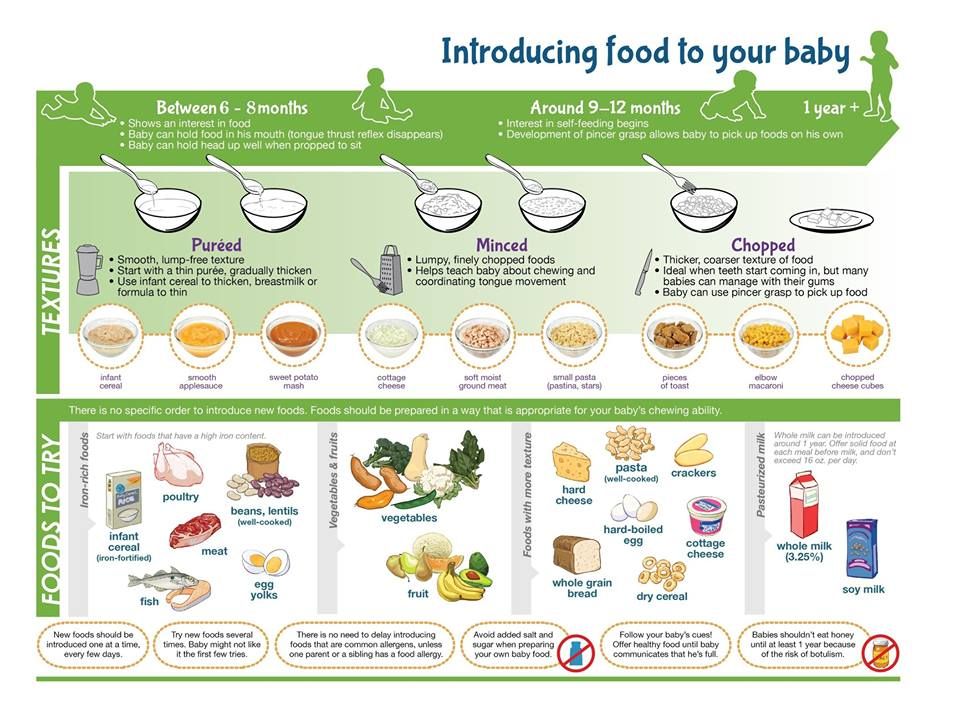
You may see a list of diet stages for after your surgery – Liquid, Pureed, Soft and Regular. Some programs will list baby food on their pureed diet.
Every Bariatric Program is different in their diet progression. (Be sure to follow your own doctors recommendations, even if they differ from what I share on this site.) Your program may have a very similar structure to these four phases. Or it may only have three phases. Or it may have five or six phases. There are several different philosophies on the post-op diet, including how to progress yourself back to foods afterwards!
The Pureed Diet is sometimes included, and sometimes not included. I’ve worked for Bariatric Programs that used the Pureed Diet and some that haven’t. So what’s the deal?
Regardless of differences in the diets, the ultimate goal is all the same. To keep stress off your healing stomach. If you advance your diet too quickly, there is risk of irritating your stomach or even causing a stricture or blockage in your new stomach. You certainly don’t want to eat chicken breast right out of the gate for this reason!
You certainly don’t want to eat chicken breast right out of the gate for this reason!
If you do have a program that uses the Pureed Diet stage and it lists “baby food” as an option…you can skip it all together. If you just plain can’t stomach the idea of eating out of a jar of green beans, then don’t! I personally wouldn’t recommend it anyway (for lack of protein and for various other reasons) but if your program does include it, do not fret. It’s a guideline, it’s not a requirement.
The same goes for blending your meats (ick!!!) Some programs may list blended meats on the food list which may mean putting chicken thigh meat in a blender with a little bit of broth. Before you ask – nope. I’ve never tried it. No thanks.
Just because you are undergoing a weight-loss surgery and need to cautiously advance your diet, doesn’t mean you have to make it as miserable as possible. While you DO want to stick with only the phase you are supposed to be in, don’t feel like you must endure awful foods.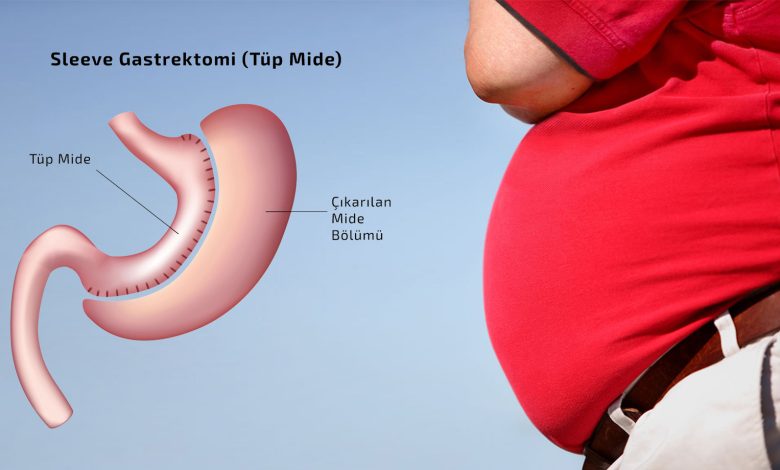 Get creative with your liquids and try soft mushy foods like tuna salad, cottage cheese, Greek yogurt and scrambled eggs. Yes…”real” foods that don’t require a blender or a jar opener! (Check out my blog post “The First Bite, When Your Liquid Diet is Finally Over“)
Get creative with your liquids and try soft mushy foods like tuna salad, cottage cheese, Greek yogurt and scrambled eggs. Yes…”real” foods that don’t require a blender or a jar opener! (Check out my blog post “The First Bite, When Your Liquid Diet is Finally Over“)
For the record, my personal recommendation to my own patients and clients is to follow a liquid diet for two weeks after surgery, then advance to a soft mushy protein phase for two weeks. After those first four weeks have gone successfully, patients are advanced back to a “regular” bariatric diet and can slowly begin incorporating more solid proteins. Again, do not replace your doctors recommendations with my own.
For more bariatric specific blog posts be sure to sign up for my email list! You may also consider becoming a Premier Access Member for meal plans, recipes, educational videos and more!
Click here to Subscribe to the Food Coach Me email list!
Enteral nutrition (tube feeding)
What is enteral nutrition?
Sometimes during treatment and recovery, children with cancer cannot get the calories and nutrients they need orally. Tube feeding, or enteral nutrition, provides nutrition in the form of a liquid or mixture given through a tube that is inserted into the stomach or intestines. Some medications may also be delivered through such a tube (probe).
Tube feeding, or enteral nutrition, provides nutrition in the form of a liquid or mixture given through a tube that is inserted into the stomach or intestines. Some medications may also be delivered through such a tube (probe).
Typically, the tube is inserted in two ways:
- Through the nose (non-surgical method)
- Through a small incision in the abdomen (surgical method)
Most commonly used are nasogastric tubes and gastrostomy tubes. But there are several types of enteral feeding tubes that differ in the method of insertion and location in the digestive tract.
Sometimes the patient is simply not able to eat enough calories or protein. There is no fault in this. It is important to help your child understand that nutritional support is not a punishment. Most children get used to the enteral feeding tube quickly. It is important that the child does not touch or pull the phone. Follow skin care instructions at the insertion site to avoid irritation or infection.
A nasogastric tube is inserted into the stomach or small intestine through the nose and throat.
Enteral feeding tube types
Enteral feeding tube connects to the stomach or small intestine. The location depends on how the patient tolerates the formula and how well their body is able to digest the nutrients. If possible, they try to place the probe in the stomach so that digestion occurs naturally.
There are 5 types of enteral feeding tubes:
Nasogastric Tube . A nasogastric tube is inserted into the stomach through the nose. It passes through the throat, esophagus and into the stomach.
Nasojejunal Probe . A nasojejunal tube is similar to a nasogastric tube but passes through the entire stomach into the small intestine.
Gastrostomy Tube (Gastrostomy Probe) . A gastrostomy tube is inserted through a small incision in the skin. The probe in this case passes through the wall of the abdominal cavity directly into the stomach.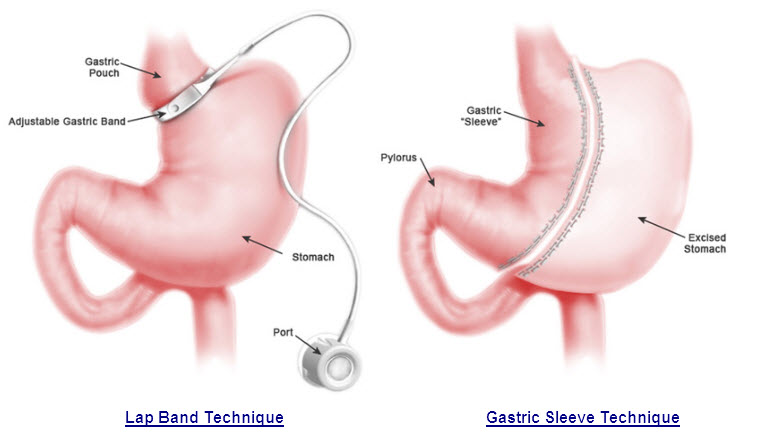
Gastrojejunostomy tube (gastrojejunostomy probe) . The gastrojejunostomy tube is inserted into the stomach like a gastrostomy tube, but passes through the stomach into the small intestine.
Jejunostomy Probe . A jejunostomy tube is inserted through a small incision in the skin and passed through the abdominal wall into the small intestine.
Nasal tubes, including nasogastric and nasojejunal tubes, are generally used for short-term enteral feeding, usually not more than 6 weeks. The probe comes out of the nostril and is attached to the skin with adhesive tape. Nasogastric and nasojejunal tubes have a number of advantages, such as a low risk of infection and a simple insertion procedure. However, the probe must be attached to the face, and this worries some children. Other children may have problems with the nasogastric tube due to chemotherapy, which irritates the skin and mucous membranes.
Surgical insertion tubes - gastrostomy tube, gastrojejunostomy tube and jejunostomy tube - are used for longer periods of time or if a nasal tube cannot be placed in the child. The opening in the abdominal wall through which the probe is inserted is called the stoma. A long tube or a "button" (low profile) probe may be visible on the patient's body. After healing, the stoma is usually pain free and the child can perform most daily activities.
The opening in the abdominal wall through which the probe is inserted is called the stoma. A long tube or a "button" (low profile) probe may be visible on the patient's body. After healing, the stoma is usually pain free and the child can perform most daily activities.
-
Insertion of nasogastric and nasojejunal tubes
-
Gastrostomy, gastrojejunostomy and jejunostomy insertion
After healing, the stoma usually does not hurt. The child can perform most daily activities.
Side effects of enteral nutrition
The most common side effects of enteral nutrition are nausea, vomiting, stomach cramps, diarrhoea, constipation and bloating.
There may be other side effects:
- Infection and irritation at the insertion site
- Probe misaligned or falling out
- Lung ingestion of formula
Most side effects can be avoided by following the care and nutrition instructions.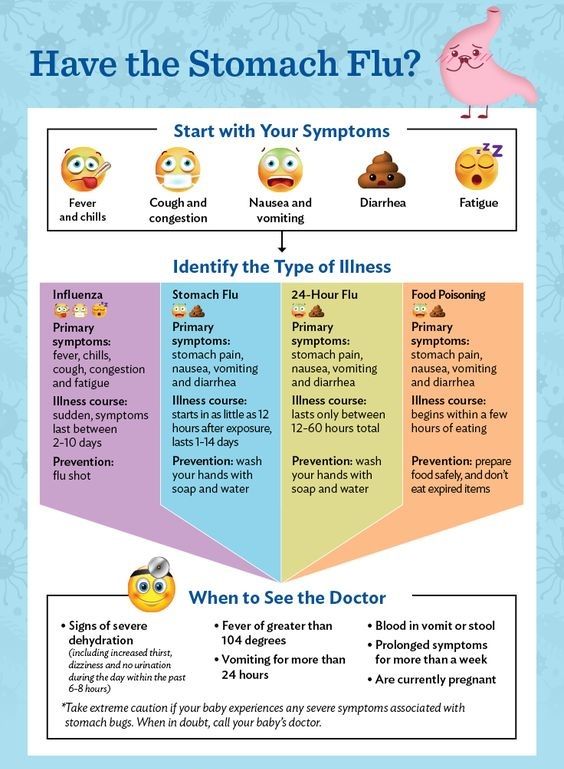
Feeding babies with tubes in place
It is the responsibility of the nutritionist to provide the baby with all the necessary nutrients. In children with cancer, an enteral feeding tube is often used in addition to what the child can eat normally. However, some patients have to enter all the nutrients through a tube.
The patient is prescribed a mixture containing:
- Calories
- Fluid
- Carbohydrates
- Fats
- Protein
- Vitamins and minerals
Standard formulas are suitable for many patients. For babies, it is preferable to use breast milk. Some children need special formulas that take into account their characteristics: the presence of allergies, diabetes or digestive problems.
It is very important for family members to work closely with a nutritionist. Nutritional needs may change due to changes in the child's health or side effects such as vomiting or diarrhea.
Types of enteral feeding
There are three types of enteral feeding - bolus, continuous and gravity.
Bolus feeding - large doses of the mixture are given to the patient by tube several times a day. This species is closest to the usual diet.
Continuous feed - Electronic pump delivers small doses of formula for several hours. Some children may need continuous feeding to reduce nausea and vomiting.
Gravity Feeding - A bag of formula is placed on the IV stand and a predetermined amount of formula is dripped through the tube at a slow rate. The duration of such nutrition depends on the needs of the patient.
Enteral feeding at home
Children can go home with a feeding tube. The doctors will ensure that family members know how to feed and care for the probe. Family members need to pay attention to the following issues:
- Weight gain or loss
- Vomiting or diarrhea
- Dehydration
- Infection
Formulas, Consumables, and Equipment Required:
- Formula: Most enteral formulas are sold ready-made.
 Some are available as a powder or liquid to mix with water.
Some are available as a powder or liquid to mix with water. - Syringe
- Adapter tube (if the child has a button tube for long-term enteral nutrition)
- Pump (with continuous power)
- Feeding formula bag with tubing (for continuous feeding)
- IV Stand (gravity fed)
General tips for enteral feeding at home:
- Always wash your hands with soap and water before feeding your baby.
- Make sure the baby's head is above the stomach.
- Throw away any ready-made or homemade formulas that have been opened and kept in the refrigerator for 24 hours or more.
- Store mixed formulations in the refrigerator and discard after 24 hours.
- Ready-to-use formulas do not need to be refrigerated.
- Do not empty the syringe completely during feeding.
- Wash the syringe (and transfer tube, if used) with warm water and dishwashing detergent after each use.
- Watch for signs of nausea, vomiting, bloating or irritability while feeding.
 If you notice these signs, stop feeding and contact your doctor immediately.
If you notice these signs, stop feeding and contact your doctor immediately. - Check the skin around the injection site for signs of irritation or infection.
-
Modified November 2018
Gastric sleeve - PROMED CLINIC
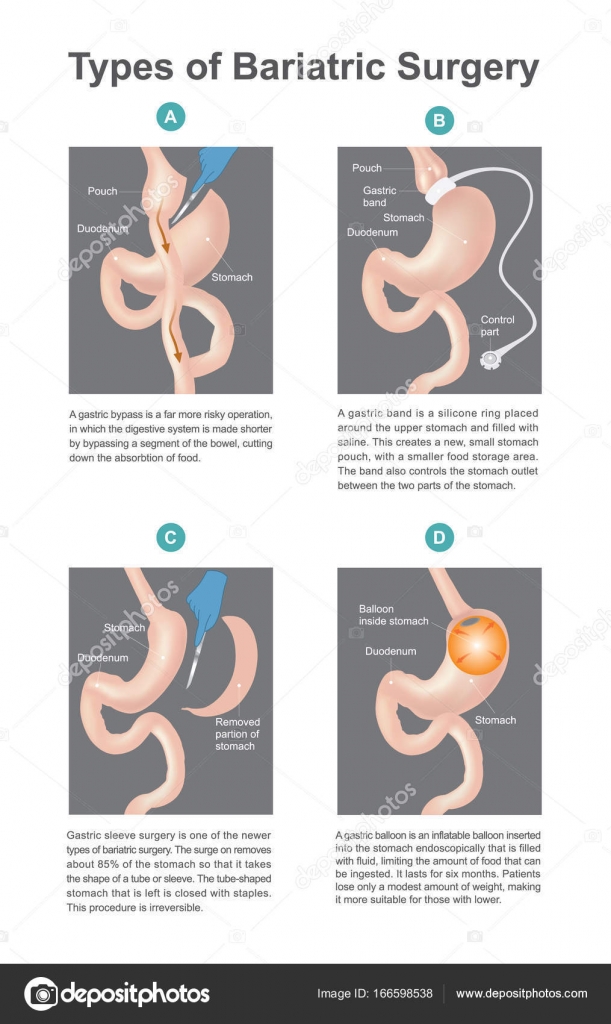
Gastric sleeve surgery, which is the most widely used technique in obesity surgery, aims to prevent problems with hunger and excess weight by reducing the volume of the stomach. The reason it is called a "tubular stomach" is because the stomach pouch is surgically converted into a tube. Sleeve gastrectomy surgery is also called gastric reduction surgery.
Gastric sleeve surgery, which is the most widely used method in obesity surgery, aims to prevent problems with hunger and excess weight by reducing the volume of the stomach. The reason it is called a "tubular stomach" is because the stomach pouch is surgically converted into a tube. Sleeve gastrectomy surgery is also called gastric reduction surgery.
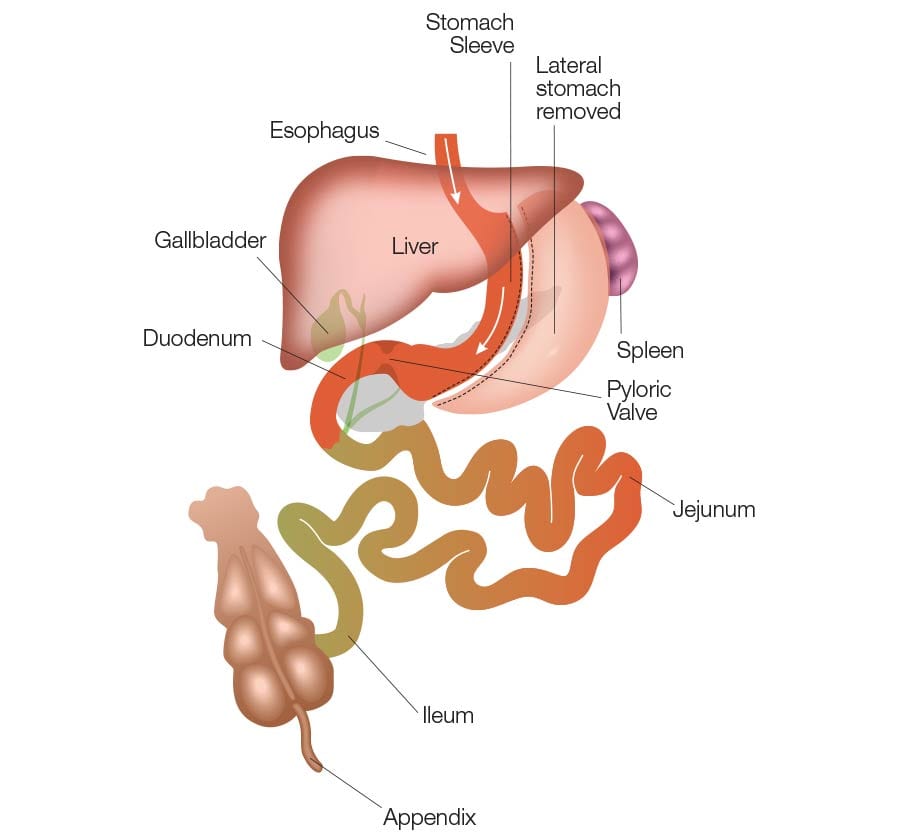
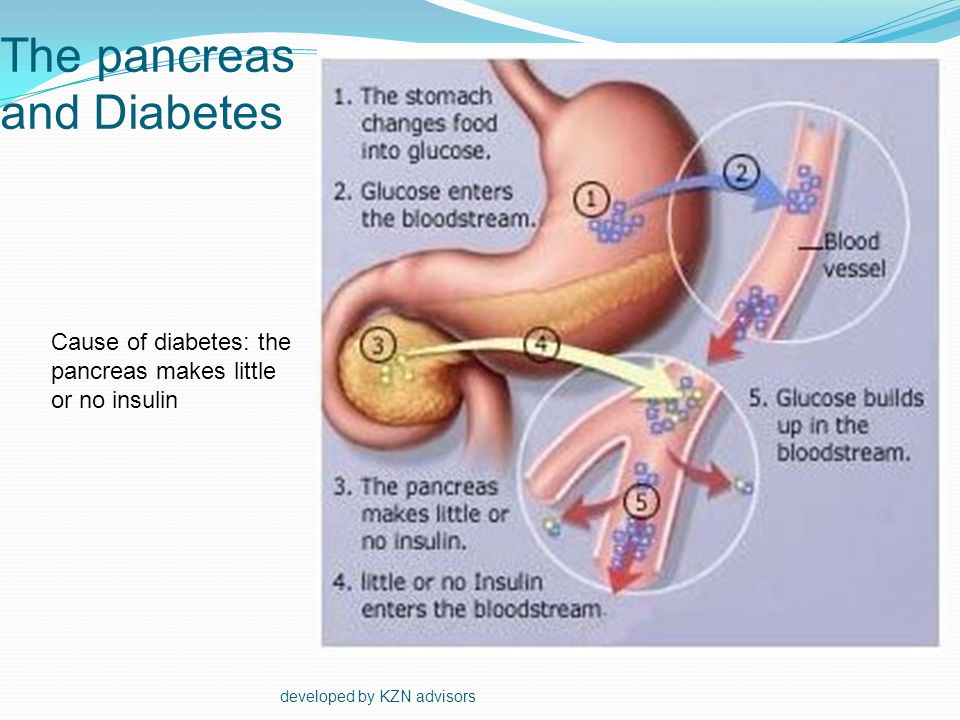
WHAT IS GASTRIC TUBE SURGERY (SLEEVE GASTRECTOMY)?
Sleeve gastrectomy, also known as gastric reduction surgery, is the process of reducing the stomach in the form of a tube.
 The stomach, which has a curved structure, is cut laparoscopically, that is, by a closed surgical method, the excess is removed and given the appearance of a cylindrical tube. In the stomach, the capacity of which is reduced, the level of appetite decreases at the same rate. For this reason, rapid saturation is achieved and weight loss is observed.
The stomach, which has a curved structure, is cut laparoscopically, that is, by a closed surgical method, the excess is removed and given the appearance of a cylindrical tube. In the stomach, the capacity of which is reduced, the level of appetite decreases at the same rate. For this reason, rapid saturation is achieved and weight loss is observed. BENEFITS OF GASTRIC PIPE SURGERY
Since the laparoscopic procedure is used for sleeve gastrectomy, which is an operation to reduce the stomach, the recovery process is faster than other methods. It is often preferred because it has the lowest risk of obesity surgery. Contrary to popular belief, it is administered very simply without adding any foreign bodies to the stomach.
Due to the decrease in appetite after surgery, effective weight loss occurs. It is faster and healthier than other weight loss methods, and the digestive system does not get worse.
HOW IS THE STOMACH REDUCED?
The gastric reduction process is applied by opening holes with a diameter of only a few millimeters.
 For this procedure, it is not necessary to make a very large incision in the wall of the stomach. This situation also affects the healing process, an easier operation is performed.
For this procedure, it is not necessary to make a very large incision in the wall of the stomach. This situation also affects the healing process, an easier operation is performed. The procedure uses thin cameras and instruments. It is injected through drilled millimeter holes with these instruments and cameras. Approximately 70-80% of the stomach is excised. The operation, which is performed under general anesthesia, takes from 60 to 90 minutes. After stomach reduction surgery, appetite is controlled and weight loss is achieved.
CAUSES OF LOSS OF APPEALS AFTER SURGERY
Ghrelin is a hormone that is secreted in the stomach and causes hunger. During stomach reduction surgery, the part of the stomach that secretes this hormone is removed. Thus, the feeling of hunger after the operation is significantly reduced. At the same time, as the size of the stomach decreases, saturation occurs very quickly. This is how the weight loss process begins after surgery. Even if people want to, they cannot consume large portions of food, they cannot take in too much liquid.
 For this reason, it is necessary to draw up a balanced program of eating and drinking with small portions.
For this reason, it is necessary to draw up a balanced program of eating and drinking with small portions. WHO IS THE OPERATION FOR?
Gastric reduction surgery performed by Promed Clinic specialists is usually preferred not for aesthetic reasons, but to eliminate life-threatening health problems. However, after the operation, a person loses a lot of weight, and this can satisfy people. After a sleeve gastrectomy, people may also ask for a tummy tuck or similar surgery, and this can be discussed with a specialist at a later date.
Like other types of surgery, sleeve gastrectomy can be performed on people between the ages of 18 and 65. It is usually applied to people who are diagnosed with severe obesity (morbid obesity) and whose body mass index is greater than 40. In addition, it may be preferred for type 2 diabetes, metabolic disorders, sleep apnea.
WHAT IS GASTRIC TUBE SURGERY (SLEEVE GASTRECTOMY)?
Sleeve gastrectomy, also known as gastric reduction surgery, is the process of reducing the stomach in the form of a tube.
 The stomach, which has a curved structure, is cut laparoscopically, that is, by a closed surgical method, the excess is removed and given the appearance of a cylindrical tube. In the stomach, the capacity of which is reduced, the level of appetite decreases at the same rate. For this reason, rapid saturation is achieved and weight loss is observed.
The stomach, which has a curved structure, is cut laparoscopically, that is, by a closed surgical method, the excess is removed and given the appearance of a cylindrical tube. In the stomach, the capacity of which is reduced, the level of appetite decreases at the same rate. For this reason, rapid saturation is achieved and weight loss is observed. BENEFITS OF GASTRIC TUBING SURGERY
Since the laparoscopic procedure is used for sleeve gastrectomy, which is a stomach reduction surgery, the recovery process is faster than other methods. It is often preferred because it has the lowest risk of obesity surgery. Contrary to popular belief, it is administered very simply without adding any foreign bodies to the stomach.
Due to the decrease in appetite after surgery, effective weight loss occurs. It is faster and healthier than other weight loss methods, and the digestive system does not get worse.
HOW IS THE STOMACH REDUCED?
The gastric reduction process is applied by opening holes with a diameter of only a few millimeters.
 For this procedure, it is not necessary to make a very large incision in the wall of the stomach. This situation also affects the healing process, an easier operation is performed.
For this procedure, it is not necessary to make a very large incision in the wall of the stomach. This situation also affects the healing process, an easier operation is performed. The procedure uses thin cameras and instruments. It is injected through drilled millimeter holes with these instruments and cameras. Approximately 70-80% of the stomach is excised. The operation, which is performed under general anesthesia, takes from 60 to 90 minutes. After stomach reduction surgery, appetite is controlled and weight loss is achieved.
CAUSES OF LOSS OF APPEALS AFTER SURGERY
Ghrelin is a hormone that is secreted in the stomach and causes hunger. During stomach reduction surgery, the part of the stomach that secretes this hormone is removed. Thus, the feeling of hunger after the operation is significantly reduced. At the same time, as the size of the stomach decreases, saturation occurs very quickly. This is how the weight loss process begins after surgery. Even if people want to, they cannot consume large portions of food, they cannot take in too much liquid.
 For this reason, it is necessary to draw up a balanced program of eating and drinking with small portions.
For this reason, it is necessary to draw up a balanced program of eating and drinking with small portions. WHO IS THE OPERATION FOR?
Gastric reduction surgery performed by Promed Clinic specialists is usually preferred not for aesthetic reasons, but to eliminate life-threatening health problems. However, after the operation, a person loses a lot of weight, and this can satisfy people. After a sleeve gastrectomy, people may also ask for a tummy tuck or similar surgery, and this can be discussed with a specialist at a later date.
Like other types of surgery, sleeve gastrectomy can be performed on people between the ages of 18 and 65. It is usually applied to people who are diagnosed with severe obesity (morbid obesity) and whose body mass index is greater than 40. In addition, it may be preferred for type 2 diabetes, metabolic disorders, sleep apnea.
Frequently Asked Questions
With mesotherapy, which stimulates the hair roots, dormant hair follicles can begin to develop and grow. Thus, the hair grows, and it can be said that new hair grows. However, hair that has completely fallen out due to genetic factors and no longer grows can only be treated with hair transplantation. This process is used for faster growth and strengthening of hair after transplantation.
Thus, the hair grows, and it can be said that new hair grows. However, hair that has completely fallen out due to genetic factors and no longer grows can only be treated with hair transplantation. This process is used for faster growth and strengthening of hair after transplantation.
People who have done this process with their hair begin to look forward to the results with curiosity. Because it is a nutritional supplement that penetrates deep into the cells, the results are difficult to see immediately, but gradually they begin to appear. The effect appears in the first 4 weeks after the procedure. Clear results are seen in an average of 6 months. The effect of the procedure lasts for 12-18 months.
Hair mesotherapy, applied at intervals of 1-4 weeks, can be applied in an average of 4 or 6 sessions. For some people, this may rarely be preferred as a single session.
Every cell in the body needs nutrients such as vitamins, minerals and amino acids. So we feed every day.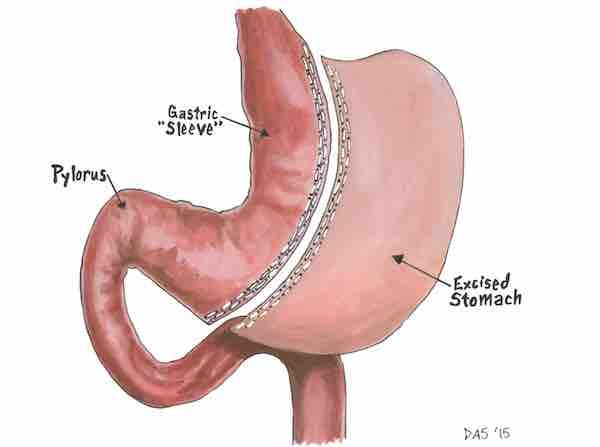 It is possible to have healthy hair because the nutritional needs of the scalp are met directly in the mesotherapy treatments applied to the hair. Since the subcutaneous tissues in which the application is made are nourished, the hair follicles also become healthier. Thus, hair loss can be prevented.
It is possible to have healthy hair because the nutritional needs of the scalp are met directly in the mesotherapy treatments applied to the hair. Since the subcutaneous tissues in which the application is made are nourished, the hair follicles also become healthier. Thus, hair loss can be prevented.
It can be used by anyone aged 18 to 65 who wants their hair to be nourished from the inside, from the roots. This is especially preferable for severe hair loss and unwillingness to aggravate this situation. Effective results can be seen with any type of hair, regardless of male or female.
This is done to nourish the roots and blood reaching the roots in people with severe hair loss or weak hair strands. Thus, the hair looks brighter, thicker and more vibrant. When used after hair transplantation, it accelerates root splicing and develops follicles.
It is applied by injecting vitamins, minerals and growth aids into the scalp. The content transferred to the cells is very nutritious.