Baby food in bottle with formula
Introducing Solid Foods - When to Start Baby Food
In her new world of tastes and textures, how can you have a smooth transition?
There will come a point when you know it’s time to start building up your baby’s diet. For some moms who have only breastfed, this might mean incorporating baby formula as a supplementation option. If this is your plan, check out our Supplementing Basics guide.
The bigger change is when you begin introducing solid foods.This is a fun time for you and your baby, as many new tastes, textures, and flavors are now on her menu.The following information may help make the transition to solid foods go as smoothly as possible.
As always, talk to your healthcare professional before you begin any changes in your child’s diet.
Introducing solids: when and how do you begin?
According to the American Academy of Pediatrics, solid foods can be introduced when your baby is about 6 months old. This is the age when a baby learns to use her tongue to move food back to her throat and her mouth muscles are developed enough to let her swallow solid foods.
A helpful idea for making your baby’s first solid-food experience easier is to mix cereal with your breast milk or baby formula. In a bowl or cup, mix 4 to 5 tablespoons of breast milk—or a baby formula like Similac Pro-Advance®with 1 to 2 tablespoons of a single-grain cereal. You’ll want to warm it up, but always test the temperature before feeding.
These tips might help, too:
- To first get your baby to start on solid foods, try giving them to her at only one feeding each day. If she is not interested, try it again in a few days until she is.
- Choose a time of day that is the least stressful for you and when your baby isn’t extremely hungry. Many parents find midmorning or midafternoon an ideal time.
Stage 1 solids: baby’s first bites
When first feeding your little one solid foods, take baby steps by offering her only one new food at a time. She will let you know how much she wants to eat and what she likes and dislikes as you go along. It’s best to begin with single-ingredient foods and wait 3 to 5 days before adding each new food. This will help you confirm or dismiss any concern about allergies.
She will let you know how much she wants to eat and what she likes and dislikes as you go along. It’s best to begin with single-ingredient foods and wait 3 to 5 days before adding each new food. This will help you confirm or dismiss any concern about allergies.
Most pediatricians recommend starting your baby on a single-grain cereal or pureed meat, as they contain important nutrients. Once she’s comfortable with a first food, you can decide when you’re both ready to move on to other single-ingredient foods, such as a stage 1 jarred baby food.
You’ll know baby is ready for single-grain cereals once she’s about 6 months of age and can:
- Sit with support
- Hold her head up and turn away when full
- Take food from a spoon and learn to swallow
Start with a small amount of cereal and increase it gradually—even a teaspoonful is enough for some beginners. A good early start plan is 4 to 5 tablespoons of beast milk or Similac® formula mixed in a bowl with 1 to 2 tablespoons of rice cereal.
Suggestions for successful cereal feeding:
- During the first few feedings, babies usually respond best to a thinner consistency.
- Put a small amount of warm cereal on the tip of a rubber-coated spoon and place it in your baby's mouth. Don’t be surprised if at first the food comes right back out. Her instinct is to use the same mouth and tongue movements as she did when nursing or sucking from a bottle.
- As your baby transitions from a totally liquid diet of breast milk or formula, she might not swallow much at first.
- As she gets used to eating from a spoon, you can gradually increase the amount and consistency, offering two or three feedings a day.
Tips for introducing single-ingredient jarred foods to your baby
When introducing single-ingredient jarred baby foods, here are a few helpful hints to keep in mind:
- Introduce one new food at a time over the course of 3 to 5 days to watch out for food allergies
- Start with a small amount of food and increase gradually—even a teaspoonful is enough for some beginners
- Do not feed your baby directly from the jar, as bacteria from her saliva will deteriorate the food
- Only feed your baby when she’s sitting up
STAGE 2: combination foods add variety to mealtime
Now that your baby is eating single-ingredient foods regularly, she probably wants to try a combination of foods for added variety and flavor. Stage 2 baby foods are made with two or more ingredients and are roughly pureed or blended to be of a thicker consistency than stage 1. While stage 1 is mostly fruits and veggies, stage 2 foods might incorporate meat, grains, or legumes.
Stage 2 baby foods are made with two or more ingredients and are roughly pureed or blended to be of a thicker consistency than stage 1. While stage 1 is mostly fruits and veggies, stage 2 foods might incorporate meat, grains, or legumes.
You’ll know if she’s ready for combination foods if she’s about 6 months old and:
- Sits well without support
- Keeps her head upright while sitting
- Eats a wide variety of single-ingredient foods
- Eats solid foods about 3 times a day
Introducing combination foods to your baby
The first step is to always check the ingredients of any food you seek to introduce. If your baby was sensitive to any single food, make sure it’s not a part of your food combinations. And:
- Introduce only one new ingredient at a time. Wait 3 to 5 days before introducing any other new foods to check for allergies.
- Maintain single foods in your baby's diet. Feed her a favorite single-grain cereal from time to time for variety.

- During her first year, include your breast milk or Similac® formula at each mealtime. It is a vital part of your baby's diet.
- Don’t worry if your baby refuses to eat, is fussy, or turns away. Try again later.
What if your baby seems to dislike some foods?
Your baby may make a face or literally turn her nose up at some foods you offer. This usually doesn’t mean she dislikes the food. She’ll simply need time to adjust to this new taste on her tongue.
To help, use any new food as her first bite of solids for a few days. The first day, she might make a face and spit the food out. The second day, she will usually swallow the first bite, but might refuse the second. Patiently continue this pattern and she’ll most likely develop a taste for any new food, including strong-tasting veggies.
Stage 3 baby food: nutrition by addition
Every baby is different; but, from about the age of 8 months, your baby should be ready for you to keep adding interesting new foods to her diet—foods with more complex tastes and textures. Almost anything goes at this stage as long as the food is in small pieces and/or cooked until very soft to make it easy to chew.
Almost anything goes at this stage as long as the food is in small pieces and/or cooked until very soft to make it easy to chew.
Here are a few basic signs for knowing if your baby is ready for complex tastes:
- She can pull up from a sitting to a standing position
- She can walk by holding onto furniture
- She wants to eat with her fingers
- She mashes food well with her gums or teeth
- She enjoys a variety of tastes and textures
Noticing a yellow tinge to your baby's skin?
Sometimes as you introduce colorful new foods to your little one’s diet, you may notice her skin taking on a yellow tinge. Check with your healthcare professional, but usually this is a harmless condition known as carotenemia. As little as 2 tablespoons of pureed carrots every day for 5 to 7 weeks can cause a baby’s skin color to change in this way. It will usually go away if you stop feeding carotene-rich foods such as carrots, sweet potatoes, and peaches for a few days.
Keep your nutritional guard up
As your growing baby’s diet continues to become more complex, make sure it’s also staying complete in its nutritional value. Toddler formulas like Go & Grow by Similac® can help balance your toddler’s diet as you begin to serve her table foods.
See our Balanced Toddler Nutrition page
Feeding your baby solid foods: what are the DOs and DON’Ts?
Talking is still months away, but your baby might be telling you things with her feeding signals. The following DOs and DON’Ts will help clue you in on baby’s mealtime needs and make the transition to solid foods as easy as possible for both of you.
When getting your baby started with solids…
DO remember that breast milk or Similac infant formula is still your baby's main source of nutrition for the first full year.
DON'T start solid foods earlier than about 4 months old, unless your healthcare professional tells you otherwise.
For mealtime success with your baby…
DO make sure your baby is hungry, but not overly so. A small "appetizer" of breast milk or Similac formula before feeding solids is recommended. Select a time of day that is the least stressful for you, and make sure you have plenty of time.
DO keep a sense of humor. Early feedings can be unproductive, challenging, and messy—but also entertaining.
To recognize signs of hunger and fullness in your baby…
DO learn your baby's signals. Feed her when you see she eagerly swallows every bite, follows the spoon with her eyes, and becomes impatient for more.
DON'T continue feeding your baby if she turns her head away, refuses to open her mouth, or cries when you try feeding her.
To add new ingredients and foods…
DO wait 3 to 5 days to add each new food to your baby's diet so you can detect any allergic reaction your baby might have to a certain food. If your baby is fussy after eating a specific food, you can find help by troubleshooting the problem with our Tummy Trouble Tool.:max_bytes(150000):strip_icc()/BabyBrezzaReusableBabyFoodStoragePouches-7d8b5aa1852e4e67903b0380509f84e3.jpg)
DON'T season your baby’s food. Babies do not need added salt or sugar.
Baby feeding methods…
DO serve baby food from a small bowl. Feeding directly from a jar can encourage bacteria growth, and your baby's saliva can make the food watery.
DON'T put your baby to bed with a bottle. This can promote "baby-bottle mouth," a form of tooth decay.
DO gently stir and test the temperature of any food from the microwave before serving. Make sure the temperature is warm, not hot.
DON'T feed cereals or other solid foods through a bottle, unless your healthcare professional directs you to do so. Cereal in a bottle might cause your baby to gag or choke.
DON'T feed your baby in a reclining position because of the danger of gagging or choking.
Baby & toddler nutrition recommendations
Infant | Young Toddlers | Older Toddlers | Preschoolers | |
|---|---|---|---|---|
0-6 months | 6-12 months | 1-2 years | 2-3 years | 3-5 years |
Infant formula/breast milk |
|
|
| |
| Early solid food | Solid foods, milk, water | ||
|
| Toddler formula |
| |
|
|
| PediaSure | |
Join Similac® Rewards for up to $400* in benefits and support throughout your journey.
* Offers may vary.
Sign Up
Formula Feeding FAQs: Starting Solids and Milk (for Parents)
Whether you plan to formula feed your baby from the start, want to supplement your breast milk with formula, or are switching from breast milk to formula, you probably have questions.
Here are answers to some common questions about formula feeding.
When Can My Baby Try Solid Foods?
Doctors recommend waiting until your baby is about 6 months old to start solid foods. Some babies may be ready for solids sooner than 6 months, but wait until your baby is at least 4 months old.
Babies who are ready to eat solids foods:
- are interested in foods (for example, they may watch others eat, reach for food, and open their mouths when food is near)
- hold up their heads well, and sit up with little or no help
- don't push food of their mouth (which is a natural tongue reflex that disappears when babies are 4–6 months old)
- usually weigh twice their birth weight, or close to it
Talk to your doctor about the right time to start solid foods.
How Do I Introduce Solid Foods?
When the time is right, start with a single-grain, iron-fortified baby cereal. Start with 1 or 2 tablespoons of cereal mixed with breast milk, formula, or water. Feed your baby with a small baby spoon. Don’t add cereal to a baby's bottle unless your doctor recommends it.
When your baby gets the hang of eating the first food, introduce other foods from all food groups, such as puréed meats, fruits, vegetables, grains, beans, and yogurt. Wait a few days between introducing new foods to make sure your baby doesn't have an allergic reaction.
You can include foods that are more likely to cause allergies — such as peanuts, eggs, cow’s milk, seafood, nuts, wheat, and soy — among the foods you introduce to your infant. Waiting to start these foods does not prevent food allergies.
Talk to your doctor before giving foods that contain peanuts if your baby has severe eczema or an egg allergy, as these conditions make an allergy to peanuts more likely. Eating peanut-containing foods early on may lower a child’s chances of developing a peanut allergy. But your doctor will need to decide if you can give peanuts to your baby, and the safest way to do it. Usually, this requires allergy tests.
Eating peanut-containing foods early on may lower a child’s chances of developing a peanut allergy. But your doctor will need to decide if you can give peanuts to your baby, and the safest way to do it. Usually, this requires allergy tests.
Should We Avoid Some Foods?
Yes, don’t give your baby:
- foods with added sugars or no-calorie sweeteners
- high-sodium foods
- honey until after the first birthday. It can cause botulism in babies.
- unpasteurized juice, milk, yogurt, or cheese
- regular cow's milk or soy beverages instead of breast milk or formula before 12 months. It’s OK to offer pasteurized yogurt and cheese.
- foods that may cause choking, such as hot dogs, raw carrots, grapes, popcorn, and nuts
Always supervise your child when eating. Make sure your child is sitting up in high chair or other safe place.
When Can My Baby Have Cow's Milk?
Before their first birthday, babies still need the nutrients in breast milk or formula. But after that, they’re ready to switch to cow's milk.
But after that, they’re ready to switch to cow's milk.
Most kids under age 2 should drink whole milk. If a toddler is overweight or there is a family history of obesity, high cholesterol, or heart problems, your doctor might recommend switching to reduced fat (2%) milk.
If your child can’t drink cow’s milk, choose an unsweetened soy beverage fortified with calcium and vitamin D. Other milk alternatives, like almond, oat, rice, or coconut milk, have less protein and may not be fortified.
How Do We Switch to Cow’s Milk?
You can switch your baby from formula to whole milk by replace bottles of formula with bottles — or sippy cups — of milk. By 1 year old, your baby should be eating a variety of solid foods and drinking about 16 to 24 ounces (480–720 milliliters) of milk per day.
When Can I Start Giving My Baby Water and Other Drinks?
In their first 6 months, healthy babies drinking enough formula usually don't need extra water. Once your baby is eating solid foods, you can offer a small amount of water between feedings, up to 4–8 ounces a day.
Water that has fluoride helps prevent tooth decay. If your water does not have fluoride, talk to your doctor or dentist about fluoride drops.
Do not give juice to babies younger than 12 months. After your child’s first birthday, limit 100% fruit juice to no more than 4 ounces a day. Always serve juice in a cup, not in a bottle. Don’t give your child sugar-sweetened beverages, including soda, juice drinks, sports drinks, and flavored milks.
Reviewed by: Mary L. Gavin, MD
Date reviewed: November 2021
How to warm up infant formula
— Polina Alexandrovna, is it possible to warm up infant formula — what do doctors and manufacturers say?
- General recommendations do not prohibit heating the mixture. Another question is how and why to do it. Mixtures that are sold ready-made are naturally heated. Dry mixtures must be diluted with water of the required temperature, and the need for heating in this case is lost.
— And if the situation forces you to prepare the mixture in advance, what should mom do?
- It is theoretically possible to heat infant formula that has been diluted in water and not used for a certain time.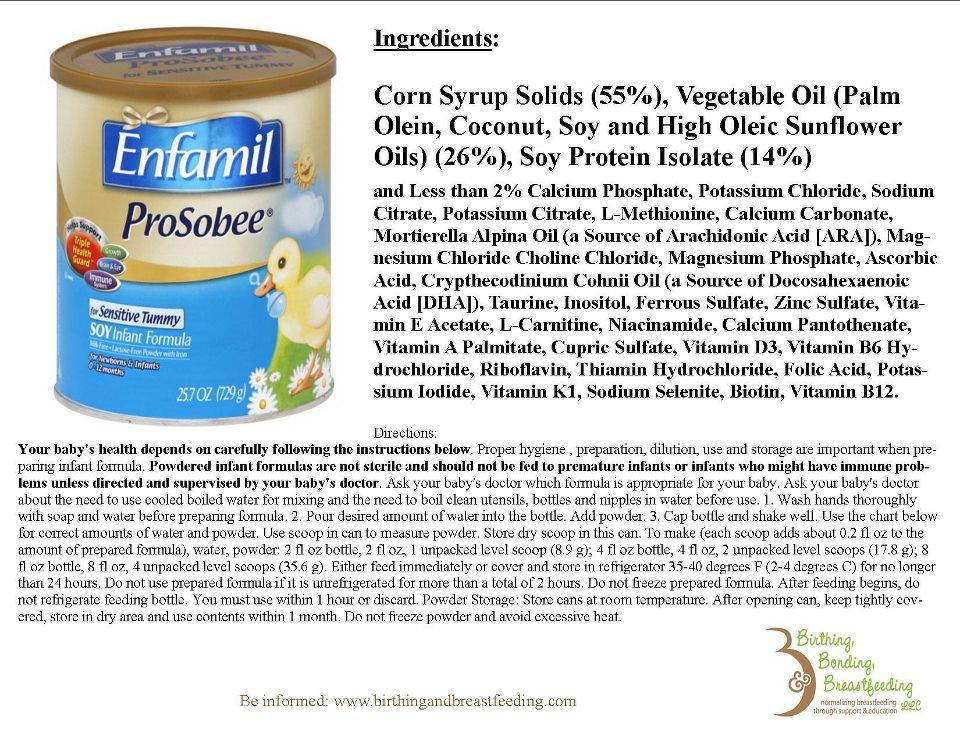 But this moment must be avoided. Fresh meals can be prepared just before the baby is fed, using separate containers with a powder dispenser and a thermos of water hot enough to cool down to the right temperature by the time the formula is diluted. When traveling by car, it makes sense to use mobile water bottle warmers, they are often powered by a car cigarette lighter.
But this moment must be avoided. Fresh meals can be prepared just before the baby is fed, using separate containers with a powder dispenser and a thermos of water hot enough to cool down to the right temperature by the time the formula is diluted. When traveling by car, it makes sense to use mobile water bottle warmers, they are often powered by a car cigarette lighter.
— Is it true that some mixtures can be heated while others cannot?
— It is possible and necessary to warm up ready-made liquid mixtures, which are sold in Tetra Pak packages. In another way, it is simply impossible, the child will not eat a cold mixture. On dry milk mixtures there are no markings with contraindications for warming up. However, it is illogical to dilute the mixture with cold water and then heat it up - it is initially poorly bred in cold water. It is better to dilute the dry mixture with water at the temperature recommended by the manufacturer.
— Can infant formula be heated in the microwave?
- Microwave does not destroy any elements of the mixture. But there are pitfalls that are not immediately noticeable. In the microwave, the mixture heats up unevenly, and very hot spots can form locally. Accordingly, if the temperature rises excessively, proteins can coagulate or certain nutrients can be destroyed. No one can guarantee what will happen in a particular microwave oven - they all have different capacities and configurations.
But there are pitfalls that are not immediately noticeable. In the microwave, the mixture heats up unevenly, and very hot spots can form locally. Accordingly, if the temperature rises excessively, proteins can coagulate or certain nutrients can be destroyed. No one can guarantee what will happen in a particular microwave oven - they all have different capacities and configurations.
— Then what is the best way to warm up infant formula?
— In order to be sure that the mixture is heated correctly, a water bath should ideally be used. Even in the instructions of the manufacturers of ready-to-use liquid mixtures, heating is recommended in a water bath.
— Polina Aleksandrovna, is it possible to reheat infant formula?
- Reheating is not recommended. If the prepared mixture was heated and it cooled down again, it is better to dilute a fresh portion.
Read also
- answers to other frequently asked questions about blends
- How long does reconstituted infant formula keep in the refrigerator?
- It is not recommended to store the mixture in cooked form: diluted - fed the child. Yes, there are extreme situations when it is impossible otherwise: there was no mixture at hand, this was the last portion ... But storing the diluted mixture at room temperature is prohibited, and even in the refrigerator they keep it - at the peril and risk of parents - no more than 1 -2 hours. And obviously it is not necessary to store the diluted mixture more than the child can consume at a time. A mixture that the child has not finished eating should not be stored under any circumstances.
Yes, there are extreme situations when it is impossible otherwise: there was no mixture at hand, this was the last portion ... But storing the diluted mixture at room temperature is prohibited, and even in the refrigerator they keep it - at the peril and risk of parents - no more than 1 -2 hours. And obviously it is not necessary to store the diluted mixture more than the child can consume at a time. A mixture that the child has not finished eating should not be stored under any circumstances.
- What are the requirements for the reconstituted bottle?
- Sterile - the main requirement: the bottle must contain a mixture that the child has not yet consumed. The dishes must be hermetically sealed, excluding contact with air and the environment.
It is not recommended to store diluted infant formula, so there is no special need to warm up dry milk formula. If it is not possible to feed the baby at home, then it is better to take a thermos of hot water and a container of dry formula with you and dilute a portion of the mixture just before feeding the baby.
* Breast milk is the best food for babies. WHO recommends exclusive breastfeeding for the first 6 months of a child's life and continued breastfeeding after complementary foods are introduced until the age of 2 years. Before introducing new products into the baby's diet, you should consult with a specialist. The material is for informational purposes and cannot replace the advice of a healthcare professional. For feeding children from birth. The product is certified.
How to store milk formula correctly? — Bellakt
Proper storage of milk formula largely determines its quality and, as a result, ensures the baby's nutritional safety. Strictly adhere to the manufacturer's recommendations when storing dry and diluted mixtures.
Baby dry mixes "Bellakt" are produced in cardboard boxes with foil bags. Therefore, closed dry mixes are recommended to be stored in a dry, cool place within the expiration date indicated on the package.
Never use expired meals!
Keep the opened package in a dry, dark, cool place at a temperature not higher than +25ºС and air humidity not higher than 85%. Avoid exposure to direct sunlight.
The best place for storage is a closed kitchen cabinet away from the stove. Do not store the mixture in the refrigerator as the high humidity may cause it to clump.
After opening the inner pouch, keep the product tightly closed and out of the reach of children.
Use the contents of an opened package within 20 days.
Even if you still have formula after this period, do not feed it to your baby. The mixture is packed by the manufacturer in a vacuum environment. After opening the package, the substances that make up the mixture interact with atmospheric oxygen, resulting in a change in their physical and chemical properties. For an adult, such changes may not be noticeable, but the baby's body reacts sharply to all changes in its familiar environment.
The mixture is packed by the manufacturer in a vacuum environment. After opening the package, the substances that make up the mixture interact with atmospheric oxygen, resulting in a change in their physical and chemical properties. For an adult, such changes may not be noticeable, but the baby's body reacts sharply to all changes in its familiar environment.
In addition to the mixture itself, it is important to properly store all the accessories necessary for its preparation - spoons, nipples, bottles. It is optimal to take a special container for them or store them in a sterilizer.
Remember that only clean, dry hands should be used to measure and dilute the mixture. Otherwise, there is an increased risk of pathogenic organisms entering the dry diet, for which a nutrient-rich mixture is a favorable environment for reproduction and growth. How to store the finished product?
How to store the finished product?
Can formula milk be stored and if so, for how long?
This question often comes to the manufacturer from parents.
The mixture is recommended to be prepared immediately before use and it is not recommended to use the remains of the mixture for subsequent feeding.
But this possibility is not always available.
The European Society of Pediatric Gastroenterology, Hepatology and Nutrition (ESPGHAN) issued recommendations in 2004 according to which reconstituted dry formula can be stored in a sealed bottle at room temperature for no more than 4 hours. In the refrigerator at temperatures up to +4°C, the finished mixture can be stored for 30 hours.
But this is only if the bottle is tightly closed with a sterilized cap, and the baby did not eat from the bottle.
If the child even drank a little from the bottle, it cannot be stored, because the risk of developing pathogenic microorganisms increases.
One of the options for safe feeding a child outside the home (on a long walk, on the road, in a clinic, etc.) is to take water and dry formula separately. Pour the required amount of formula for one feeding into a sterilized bottle and close tightly. Pour boiled water heated to +50°C into a thermos. When the baby is hungry, dilute the mixture.
Councils on Children's Mixing:
- use the mixture only within the expiration date indicated on the package;
- store the opened mixture for no more than 20 days;
- store the mixture in a dry, dark, cool place in an airtight container.