Baby food poison symptoms
Food Poisoning (Infant/Toddler)
Food poisoning is illness that is passed along in food. It usually occurs 1 to 24 hours after eating food that has spoiled. It is often caused by toxins from bacteria in food that hasn't been cooked or refrigerated properly. Symptoms may include vomiting, diarrhea, and fever. These symptoms usually last 1 to 2 days. Antibiotics are usually not needed. But they may be used for some food poisoning caused by bacteria.
The main danger from this illness is dehydration. This is the loss of too much water and minerals from the body. When this occurs, your child's body fluids must be replaced. This can be done with oral rehydration solution. You can get oral rehydration solution at pharmacies and most grocery stores.
Home care
Follow all instructions given by your child’s healthcare provider.
If giving medicines to your child:
-
Don’t give over-the-counter diarrhea medicines unless your child’s provider tells you to.
These can make the illness last longer.
-
You can use acetaminophen or ibuprofen to control pain and fever. Or, you can use other medicine as prescribed.
-
Don’t give aspirin to anyone younger than age 18 who has a fever. This may cause liver damage and a life-threatening condition called Reye syndrome.
To prevent the spread of illness:
-
Remember that washing hands with soap and clean, running water or using alcohol-based sanitizer is the best way to prevent the spread of infection.
-
Wash your hands before and after caring for your sick child.
-
Clean the toilet or the diaper change area after each use. Dispose of soiled diapers in a sealed container.
-
Keep your child out of daycare until your child's provider says it's OK.
-
Teach your child to wash their hands after using the toilet and before meals. This is very important if your child is in daycare.
-
Wash your hands before and after preparing food. Keep in mind that people with diarrhea or vomiting should not prepare food for others.
-
Wash your hands and utensils after using cutting boards, countertops and knives that have been in contact with raw foods.
-
Wash and then peel fruits and vegetables.
-
Keep uncooked meats away from cooked and ready-to-eat foods.
-
Use a food thermometer when cooking.
 Cook poultry to at least 165°F (74°C). Cook ground meat (beef, veal, pork, lamb) to at least 160°F (71°C). Cook fresh beef, veal, lamb, and pork to at least 145°F (63°C).
Cook poultry to at least 165°F (74°C). Cook ground meat (beef, veal, pork, lamb) to at least 160°F (71°C). Cook fresh beef, veal, lamb, and pork to at least 145°F (63°C). -
Don’t serve raw or undercooked eggs (poached or sunny side up), poultry, meat, or unpasteurized milk or juices to your child.
Giving liquids and feeding
The main goal while treating vomiting or diarrhea is to prevent dehydration. This is done by giving your child small amounts of liquids often.
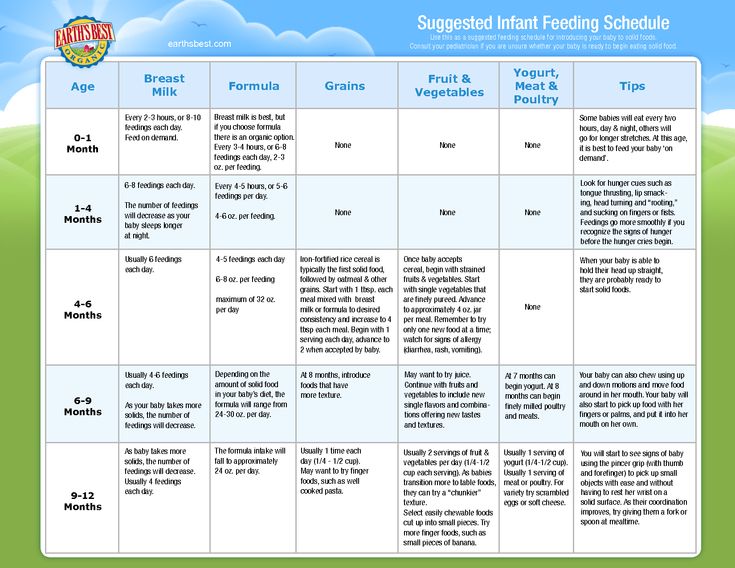
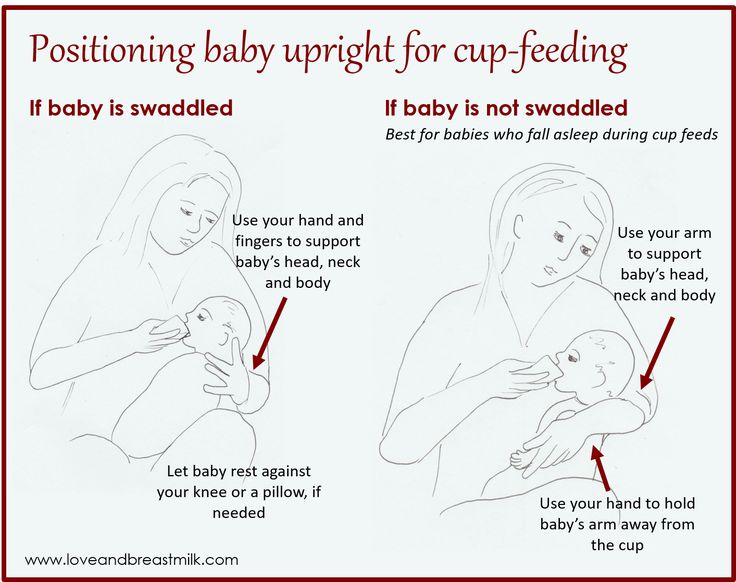
If your baby is breastfed:
-
For diarrhea: Keep breastfeeding. Feed your child more often than usual. If diarrhea is severe, give oral rehydration solution between feedings. As diarrhea decreases, stop giving oral rehydration solution and resume your normal breastfeeding schedule.

-
For vomiting: After 2 hours with no vomiting, restart breastfeeding. Spend half the usual feeding time on each breast every 1 to 2 hours. If your child vomits again, reduce feeding time to 5 minutes on 1 breast only, every 30 to 60 minutes. Switch to the other breast with each feeding. Some milk will be absorbed even when your child vomits. As vomiting stops, resume your regular breastfeeding schedule.
If your baby is bottle-fed:
-
Give small amounts of fluid at a time, especially if your child is vomiting. An ounce or 2 (30 to 60 mL) every 30 minutes may improve symptoms. Start with 1 teaspoon (5 mL) every 5 minutes and increase gradually as tolerated.
-
For diarrhea: Give full-strength formula or milk.
 If diarrhea is severe, give oral rehydration solution between feedings. If giving milk and the diarrhea is not getting better, stop giving milk. In some cases, milk can make diarrhea worse. Try soy or rice formula. Don't give apple juice, soda, or other sweetened drinks. Drinks with sugar can make diarrhea worse. If your child starts doing worse with food, go back to clear liquids.
If diarrhea is severe, give oral rehydration solution between feedings. If giving milk and the diarrhea is not getting better, stop giving milk. In some cases, milk can make diarrhea worse. Try soy or rice formula. Don't give apple juice, soda, or other sweetened drinks. Drinks with sugar can make diarrhea worse. If your child starts doing worse with food, go back to clear liquids. -
For vomiting: After 2 hours with no vomiting, try giving regular formula or milk. If at any time the child begins to vomit again, go back to small amounts of clear liquids. Begin with small amounts and increase the amount as tolerated.
-
If your child is doing well after 24 hours, resume a regular diet and feeding schedule.
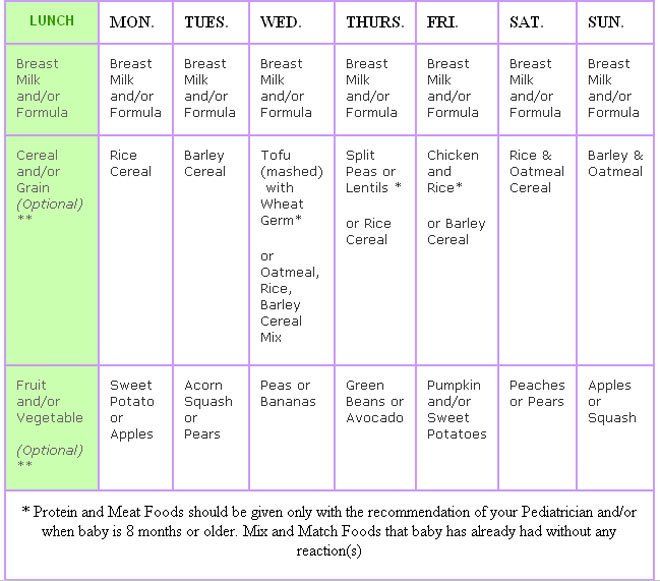
If your child is on solid food:
-
Keep in mind that liquids are more important than food right now.
 Give small amounts of liquids at a time, especially if the child is having stomach cramps or vomiting.
Give small amounts of liquids at a time, especially if the child is having stomach cramps or vomiting. -
For diarrhea: If you're giving milk to your child and the diarrhea isn't going away, stop the milk. In some cases, milk can make diarrhea worse. If that happens, use oral rehydration solution instead. If diarrhea is severe, give oral rehydration solution between feedings. Sports drinks are not equivalent to oral rehydration solutions. They contain too much sugar and too few electrolytes.
-
For vomiting: Begin with oral rehydration solution at room temperature. Give 1 teaspoon (5 ml) every 5 minutes. Even if your child vomits, continue to give oral rehydration solution. Much of the liquid will be absorbed, despite the vomiting. After 2 hours with no vomiting, begin with small amounts of milk or formula and other fluids.
 Increase the amount as tolerated. Don't give your child plain water, milk, formula, or other liquids until vomiting stops. As vomiting decreases, try giving larger amounts of oral rehydration solution. Space this out with more time in between. Continue this until your child is making urine and is no longer thirsty (has no interest in drinking). After 4 hours with no vomiting, restart solid foods. After 24 hours with no vomiting, resume a normal diet.
Increase the amount as tolerated. Don't give your child plain water, milk, formula, or other liquids until vomiting stops. As vomiting decreases, try giving larger amounts of oral rehydration solution. Space this out with more time in between. Continue this until your child is making urine and is no longer thirsty (has no interest in drinking). After 4 hours with no vomiting, restart solid foods. After 24 hours with no vomiting, resume a normal diet. -
You can resume your child's normal diet over time as they feels better. Don’t force your child to eat, especially if they're having stomach pain or cramping. Don’t feed your child large amounts at a time, even if they're hungry. This can make your child feel worse. You can give your child more food over time if they can tolerate it. For a baby older than age 4 months, you can give cereal, mashed potatoes, applesauce, mashed bananas, or strained carrots during this time.
 For children age 1 or older, you can add crackers, white bread, rice, crackers, and other complex starches, lean meats, yogurt, fruits, and vegetables. Low-fat diets are easier to digest than high-fat diets.
For children age 1 or older, you can add crackers, white bread, rice, crackers, and other complex starches, lean meats, yogurt, fruits, and vegetables. Low-fat diets are easier to digest than high-fat diets. -
If the symptoms come back, go back to a simple diet or clear liquids.
Follow-up care
Follow up with your child’s healthcare provider, or as advised. If a stool sample was taken or cultures were done, call the provider for the results as instructed.
Call 911
Call 911 if your child has any of these symptoms:
When to seek medical advice
Call your child’s healthcare provider right away if any of these occur:
-
Abdominal pain that gets worse
-
Constant lower right abdominal pain
-
Repeated vomiting after the first 2 hours on liquids
-
Occasional vomiting for more than 24 hours
-
More than 8 diarrhea stools within 8 hours
-
Continued severe diarrhea for more than 24 hours
-
Blood or black material in vomit or stool
-
Reduced oral intake
-
Dark urine or no urine for 4 to 6 hours, no tears when crying, sunken eyes, or dry mouth
-
Fussiness or crying that can't be soothed
-
Unusual drowsiness
-
New rash
-
Diarrhea lasting more than 1 week
-
Fever (see Fever and children, below)
-
Symptoms get worse or your child has new symptoms
Fever and children
Use a digital thermometer to check your child’s temperature.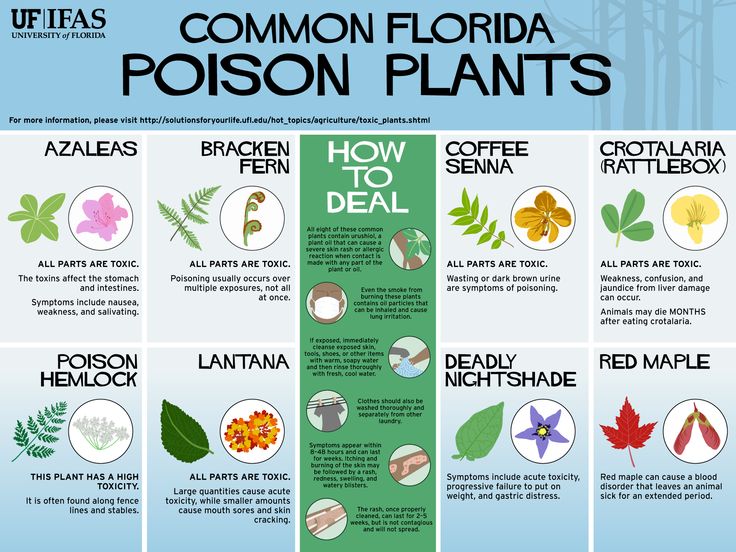 Don’t use a mercury thermometer. There are different kinds and uses of digital thermometers. They include:
Don’t use a mercury thermometer. There are different kinds and uses of digital thermometers. They include:
-
Rectal. For children younger than 3 years, a rectal temperature is the most accurate.
-
Forehead (temporal). This works for children age 3 months and older. If a child under 3 months old has signs of illness, this can be used for a first pass. The provider may want to confirm with a rectal temperature.
-
Ear (tympanic). Ear temperatures are accurate after 6 months of age, but not before.
-
Armpit (axillary). This is the least reliable but may be used for a first pass to check a child of any age with signs of illness.
 The provider may want to confirm with a rectal temperature.
The provider may want to confirm with a rectal temperature. -
Mouth (oral). Don’t use a thermometer in your child’s mouth until they are at least 4 years old.
Use the rectal thermometer with care. Follow the product maker’s directions for correct use. Insert it gently. Label it and make sure it’s not used in the mouth. It may pass on germs from the stool. If you don’t feel OK using a rectal thermometer, ask the healthcare provider what type to use instead. When you talk with any healthcare provider about your child’s fever, tell them which type you used.
Below are guidelines to know if your young child has a fever. Your child’s healthcare provider may give you different numbers for your child. Follow your provider’s specific instructions.
Fever readings for a baby under 3 months old:
Fever readings for a child age 3 months to 36 months (3 years):
-
Rectal, forehead, or ear: 102°F (38.
 9°C) or higher
9°C) or higher -
Armpit: 101°F (38.3°C) or higher
Call the healthcare provider in these cases:
-
Repeated temperature of 104°F (40°C) or higher in a child of any age
-
Fever of 100.4° (38°C) or higher in baby younger than 3 months
-
Fever that lasts more than 24 hours in a child under age 2
-
Fever that lasts for 3 days in a child age 2 or older
© 2000-2022 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.
Was this helpful?
Yes No
Tell us more.
Check all that apply.
Wrong topic—not what I was looking for.
It was hard to understand.
It didn't answer any of my questions.
I still don't know what to do next.
Other.
NEXT ▶
Last question: How confident are you filling out medical forms by yourself?
Not at all A little Somewhat Quite a bit Extremely
Thank You!
Food Poisoning (for Parents) - Nemours KidsHealth
What Is Food Poisoning?
Food poisoning is caused by bacteria and, sometimes, viruses or other germs.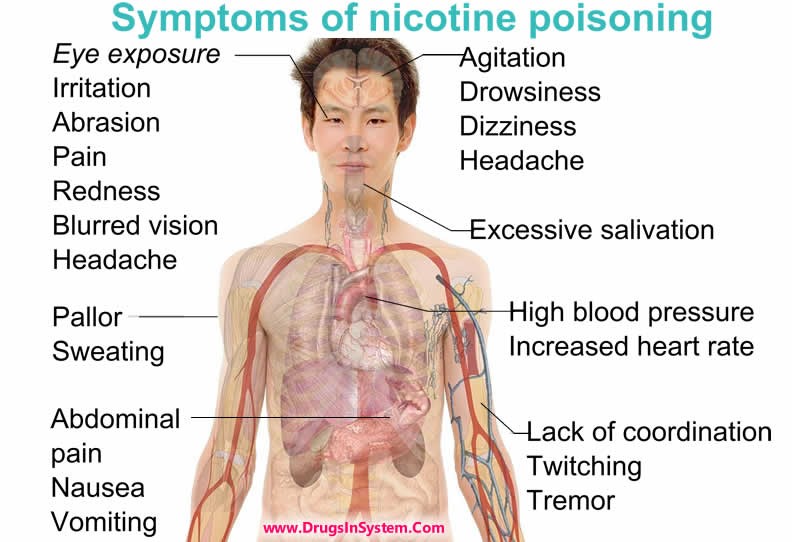 They can get into the food we eat or the liquids we drink. We can't taste, smell, or see these germs (at least not without a microscope). But even though they're tiny, they can have a powerful effect on the body.
They can get into the food we eat or the liquids we drink. We can't taste, smell, or see these germs (at least not without a microscope). But even though they're tiny, they can have a powerful effect on the body.
When germs that cause food poisoning get into our systems, they can release toxins. These toxins are poisons (the reason for the name "food poisoning"), and can cause diarrhea and vomiting.
Usually, doctors use "food poisoning" to describe an illness that comes on quickly after eating contaminated food. People often get diarrhea or start throwing up within a few hours after being infected. The good news is, food poisoning usually goes away quickly too. Most people recover in a couple of days with no lasting problems.
In a few cases, severe food poisoning can mean a visit to the doctor or hospital. When people need medical treatment for food poisoning, it's often because of dehydration. Getting dehydrated is the most common serious complication of food poisoning.
What Are the Signs & Symptoms of Food Poisoning?
How food poisoning shows up depends on the germ that caused it. Someone might start to feel sick within an hour or two of eating or drinking contaminated food or liquid. Other times, symptoms may not appear for a number of weeks. In most cases, symptoms will clear up within 1 to 10 days.
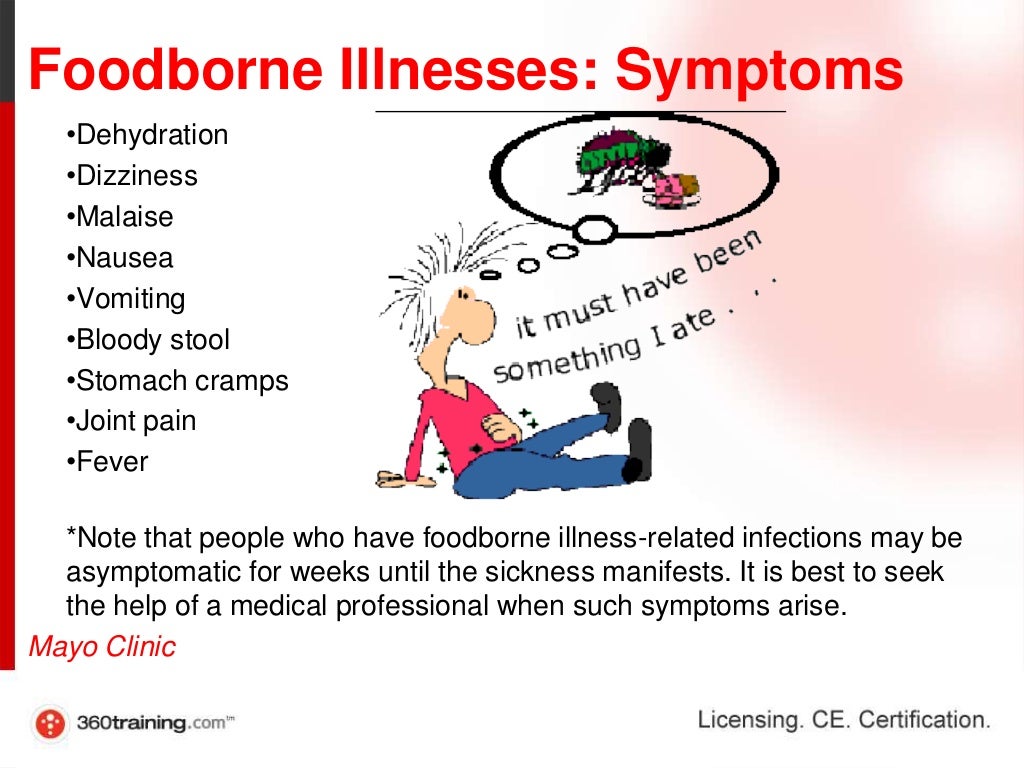
Signs that a child might have food poisoning include:
- nausea (feeling sick)
- belly pain and cramps
- vomiting
- diarrhea
- fever
- headache and overall weakness
In rare cases, food poisoning can make someone feel dizzy, have blurry vision, or notice tingling in the arms. In very rare cases, the weakness that sometimes goes along with food poisoning will cause trouble breathing.
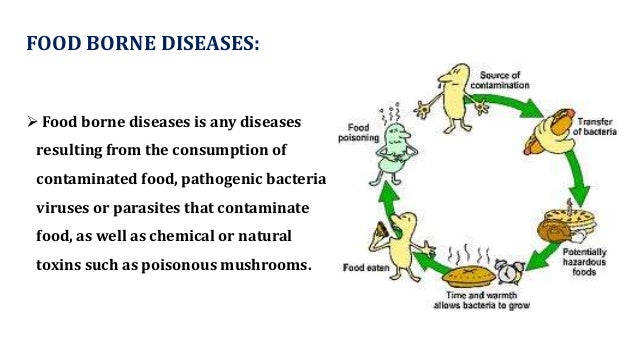
What Causes Food Poisoning?
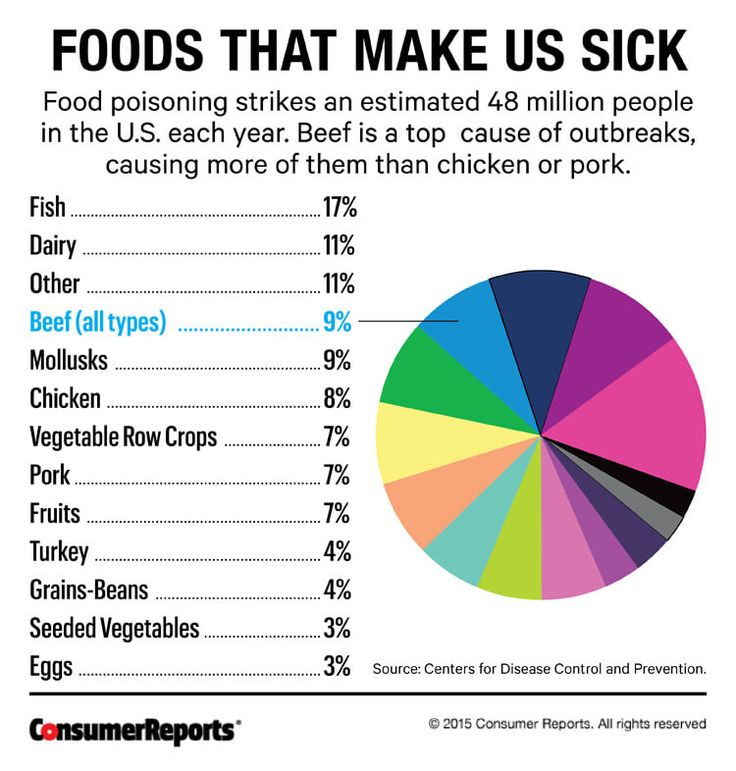
When people eat or drink something that's contaminated with germs, they can get sick with food poisoning. Often, people get food poisoning from animal-based foods — like meat, poultry, eggs, dairy products, and seafood. But unwashed fruits, vegetables, and other raw foods also can be contaminated and make people sick. Even water can cause food poisoning.
But unwashed fruits, vegetables, and other raw foods also can be contaminated and make people sick. Even water can cause food poisoning.
Foods and liquids can be contaminated at lots of different points during food preparation, storage, and handling. For example:
- Water that is used to grow food can become infected with animal or human feces (poop).
- Meat or poultry may come into contact with germs during processing or shipping.
- Bacteria can infect foods stored at the wrong temperature or kept too long.
- Cooks or other food handlers can contaminate foods if they don't wash their hands or they use unclean utensils or cutting boards.
People with health conditions (like chronic kidney disease) or weakened immune systems are more at risk of getting ill from food poisoning than people who are in good health.
What Germs Cause Food Poisoning?
Germs that often cause food poisoning include:
Salmonella.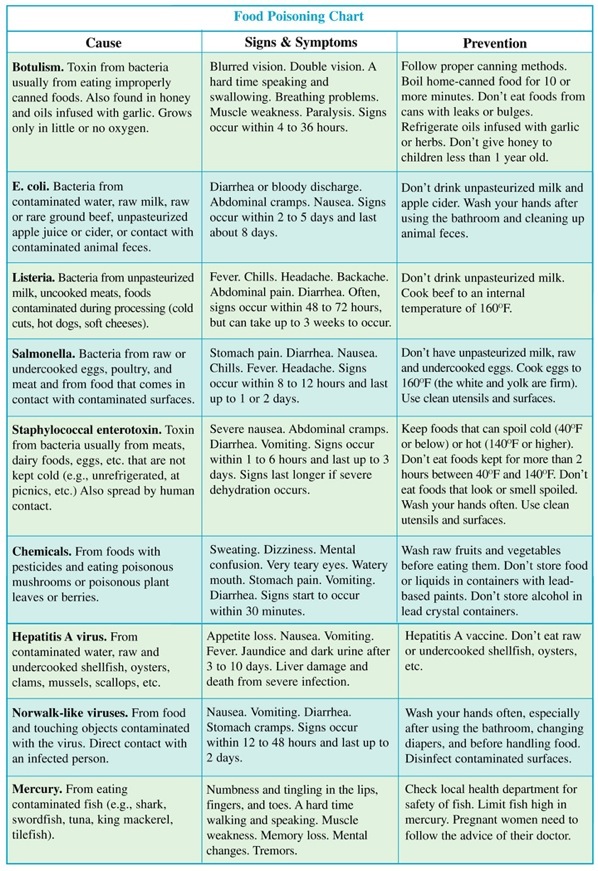 Salmonella bacteria are the leading cause of food poisoning in the United States. These bacteria usually get into foods when they come into contact with animal feces. The main causes of salmonella poisoning are eating dairy products, undercooked meat, and fresh produce that hasn't been washed well.
Salmonella bacteria are the leading cause of food poisoning in the United States. These bacteria usually get into foods when they come into contact with animal feces. The main causes of salmonella poisoning are eating dairy products, undercooked meat, and fresh produce that hasn't been washed well.
E. coli (Escherichia coli). E. coli bacteria usually get into food or water when they come into contact with animal feces. Eating undercooked ground beef is the most common cause of E. coli poisoning in the United States.
Listeria. These bacteria are mostly found in unpasteurized dairy products, smoked seafood, and processed meats like hot dogs and lunchmeats. Listeria bacteria also can contaminate fruits and vegetables, although that's less common.
Campylobacter. These bacteria most commonly infect meat, poultry, and unpasteurized milk. Campylobacter also can contaminate water. As with other kinds of bacteria, these usually get into foods through contact with infected animal feces.
Campylobacter also can contaminate water. As with other kinds of bacteria, these usually get into foods through contact with infected animal feces.
Staphylococcus aureus. These bacteria (which can be found in meats, prepared salads, and foods made with contaminated dairy products) spread through hand contact, sneezing, or coughing. That means that people who prepare or handle food can spread the infection.
Shigella. Shigella bacteria can infect seafood or raw fruits and vegetables. Most of the time these bacteria spread when people who prepare or handle food don't wash their hands properly after using the bathroom. Sometimes, an infection causes blood in the stool (poop).
Hepatitis A. People mostly get this virus from eating raw shellfish or foods that have been handled by someone who is infected. It can be hard to know the source of an infection because people may not get sick for 15 to 50 days afterward.
Norovirus. Norovirus infections spread easily from person to person, especially in crowded settings, like daycares and schools.
Some of these, including Listeria and E. coli, can cause potentially dangerous heart, kidney, and bleeding problems.
When Should I Call the Doctor?
Most cases of food poisoning don't need medical attention, but some do. The most common serious problem from food poisoning is dehydration. A child who is healthy is unlikely to get dehydrated as long as he or she drinks enough liquids to replace what's lost through throwing up or diarrhea.
Call the doctor if your child has any of these symptoms:
- vomiting that lasts for more than 12 hours
- diarrhea with a fever higher than 101°F (38.3°C)
- severe belly pain that doesn't go away after a bowel movement
- bloody feces (diarrhea or regular poop) or bloody vomit
- bowel movements that are black or maroon
- a racing or pounding heart
It's important to watch for signs of dehydration, which include:
- extreme thirst
- making little or no urine (pee)
- dizziness
- sunken eyes
- lightheadedness or weakness
If your family recently been to a foreign country and your child starts having diarrhea or other stomach problems, call your doctor.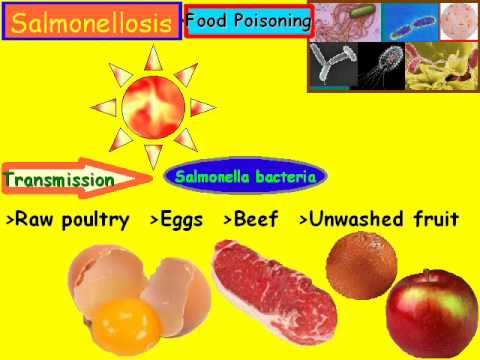
Food poisoning (especially dehydration) can be more serious for people with weakened immune systems or health conditions. If your child has a health condition (such as kidney problems or sickle cell disease), call your doctor right away. Pregnant women also should let their doctors know if they get food poisoning as some germs can affect the unborn child.
How Is Food Poisoning Diagnosed?
A doctor will ask about what your child ate most recently and when symptoms began. The doctor will do an exam, and might take a sample of blood, stool, or pee and send it to a lab for analysis. This will help the doctor find out what's causing the illness.
How Is Food Poisoning Treated?
Usually, food poisoning runs its course and kids get better on their own. Occasionally, though, doctors prescribe antibiotics to treat more severe types of bacterial food poisoning. A child with severe dehydration may need to be treated in a hospital with intravenous (IV) fluids.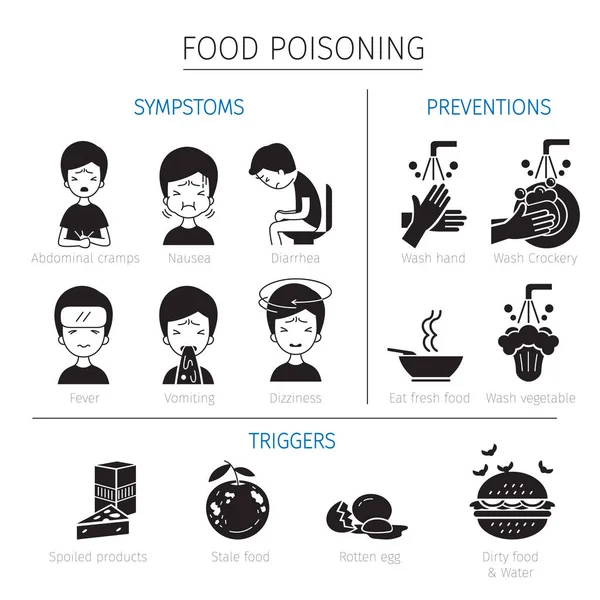
At-Home Care
Food poisoning usually goes away on its own in a few days. To help your child feel better in the meantime, make sure he or she:
- Gets plenty of rest.
- Drinks liquids to protect against dehydration. Electrolyte solutions work, but anything except milk or caffeinated beverages will do.
- Takes small, frequent sips to make it easier to keep the fluids down.
- Avoids solid foods and dairy products until any diarrhea has stopped.
Do not give over-the-counter anti-diarrhea medicines. These can make the symptoms of food poisoning last longer. When diarrhea and vomiting have stopped, offer your child small, bland, low-fat meals for a few days to prevent further stomach upset.
If symptoms become serious or you see signs of dehydration, call your doctor.
How Can We Prevent Food Poisoning?
Follow these tips to help protect your family from food poisoning:
- Teach everyone in your family to wash their hands well and often, especially after using the bathroom, before touching food, and after touching raw food.
 Use soap and warm water and scrub for at least 15 seconds.
Use soap and warm water and scrub for at least 15 seconds. - Clean all utensils, cutting boards, and surfaces that you use to prepare food with hot, soapy water.
- Don't serve unpasteurized milk or food that contains unpasteurized milk.
- Wash all raw vegetables and fruits that you can't peel yourself.
- Keep raw foods (especially meat, poultry, and seafood) away from other foods until they're cooked.
- Use perishable food or any food with an expiration date as soon as possible.
- Cook all food from animal sources to a safe internal temperature. For ground beef and pork, this means at least 160°F (71°C). For solid cuts of meat, the safe temperature is 145°F (63°C). For chicken and turkey (ground and whole), it's at least 165°F (74°C). Cook chicken eggs until the yolk is firm. Fish generally is safe to eat once it reaches a temperature of 145°F (63°C).
- Refrigerate leftovers quickly, preferably in containers with lids that snap tightly shut.
- Defrost foods in the refrigerator, a microwave, or cold water. Food should never be thawed at room temperature.
- If food is past its expiration date, tastes funny, or smells strange, throw it out.
- If you're pregnant, avoid all raw or undercooked meat or seafood, smoked seafood, raw eggs and products that might contain raw eggs, soft cheeses, unpasteurized milk and juice, patés, prepared salads, luncheon meats, and hot dogs.
- Don't drink water from streams or untreated wells.
If someone in your family gets food poisoning, tell your local health department. Officials there might be able to find the cause and stop an outbreak that could affect others.
Reviewed by: Ryan J. Brogan, DO
Date reviewed: April 2022
Treatment of food poisoning in a child
Food poisoning is an acute infectious-toxic pathology. It occurs when eating poor-quality products that contain pathogens, toxic substances and poisons.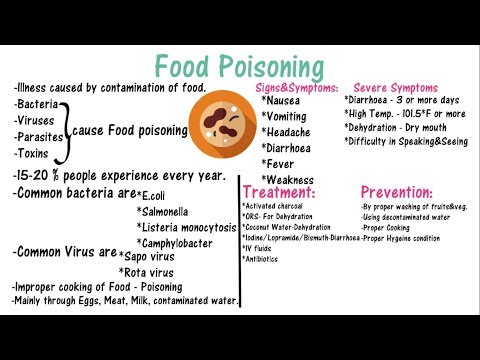 The main manifestations are diarrhea, vomiting, fever, signs of dehydration and severe intoxication. The task of treatment is to quickly stop the symptoms of poisoning, replenish fluid deficiency, and prevent the development of complications.
The main manifestations are diarrhea, vomiting, fever, signs of dehydration and severe intoxication. The task of treatment is to quickly stop the symptoms of poisoning, replenish fluid deficiency, and prevent the development of complications.
Class
Food poisoning is referred to as toxic infection or intoxication. Pathology develops after the use of low-quality food, water, plant, chemical or medicinal toxic substances.
There are two types of food poisoning in children:
- Infectious. The causative agents are microbes and their toxic waste products.
- Non-infectious. Caused by toxic substances of plant, animal origin, toxic impurities.
The asymptomatic or latent stage of food poisoning begins from the moment the toxins enter the body until the first symptoms appear. The duration depends on the individual characteristics and age of the child, the amount and rate of absorption of poisons. This stage is most favorable for therapy, since toxic substances have not yet penetrated into the blood.
The toxicogenic stage begins with the appearance of the first symptoms of poisoning and lasts until bacteria and poisons are completely eliminated from the body. This period is characterized by the manifestation of all symptoms of poisoning. In order for the treatment to be effective, it is necessary to identify toxins and accelerate the process of elimination.
At the last stage of convalescence, the disturbed functions of the organs of the digestive, excretory, and immune systems are restored.
Causes
Food poisoning is one of the most common problems in pediatrics. In children, intoxication is more severe than in adults. This is due to the characteristics of the child's body: low acidity of gastric juice, incompletely formed intestinal microflora, rapid absorption of poisons and the spread of toxins throughout the body.
The main causative agents of food poisoning in children are staphylococci, proteus, klebsiella, enterotoxigenic strains of E.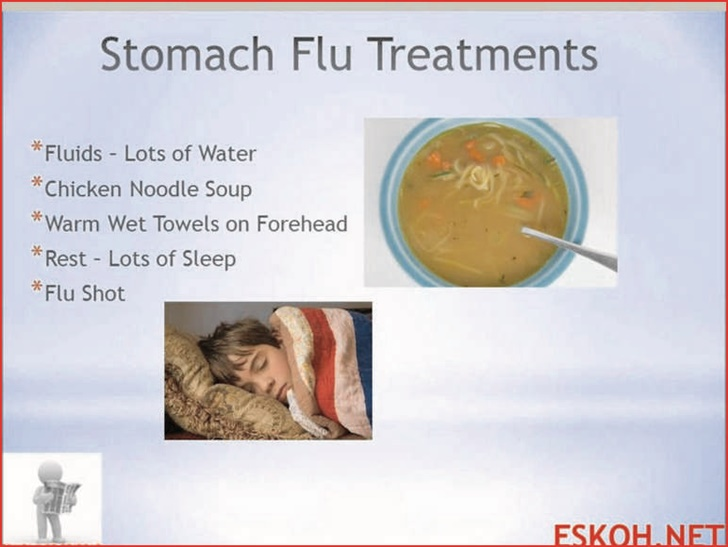 coli, clostridia. Pathogens enter the body only with food, in which they multiply, release toxins.
coli, clostridia. Pathogens enter the body only with food, in which they multiply, release toxins.
Causes of violation of food quality:
- non-compliance with sanitary and hygienic standards;
- violation of the rules for storage, preparation and sale of food products;
- contamination of food by people with intestinal infections, purulent pathologies - tonsillitis, furunculosis, panaritium, mastitis, streptoderma;
- contamination of soil and plants by animal feces.
Spoiled products may have an unpleasant taste, smell, uncharacteristic texture, but often organoleptic indicators remain within the normal range.
Non-infectious poisoning - a consequence of accidental consumption of poisonous berries or plants, mushrooms. Intoxication can occur after eating agricultural products that are contaminated with poisonous fungicides, insecticides.
Which products are classified as potentially hazardous?
In children, food poisoning often occurs after drinking unboiled water, missing milk or dairy products.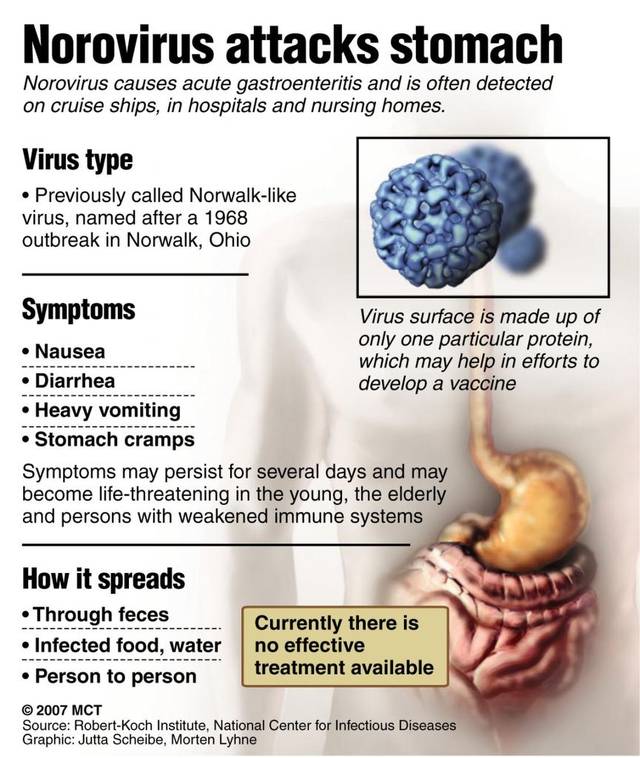
Dangerous products include:
- eggs;
- cream confectionery;
- fish and seafood;
- sausages;
- meat, vegetable preserves;
- mushrooms.
Food poisoning is most often diagnosed in summer and autumn. During this period, the conditions for the reproduction of microbial pathogens are the most favorable.
Symptoms of food poisoning in a child
Despite the variety of toxic infections, clinical manifestations are largely similar. The latent stage lasts an average of 2-6 hours, sometimes no more than 30 minutes or more than a day. Signs of poisoning are manifested by symptoms of gastroenteritis, intoxication, dehydration.
Poisoning always begins acutely - nausea, repeated vomiting with particles of undigested food. The child complains of abdominal pain, watery stools, mucous membranes, green impurities, blood streaks. Bowel emptying occurs up to 5-10 times a day.
Simultaneously with dyspeptic disorders, the temperature rises to 38–39 degrees. Signs of intoxication quickly increase: refusal to eat, headache and muscle pain. Symptoms of dehydration appear: the skin is pale and dry, facial features are sharpened, the number of urination decreases, the mucous membranes dry out. In infants, the fontanel sinks. With food poisoning, convulsions often occur, acidosis develops.
Signs of intoxication quickly increase: refusal to eat, headache and muscle pain. Symptoms of dehydration appear: the skin is pale and dry, facial features are sharpened, the number of urination decreases, the mucous membranes dry out. In infants, the fontanel sinks. With food poisoning, convulsions often occur, acidosis develops.
In most cases, signs of poisoning gradually disappear after 2-3 days, but weakness and abdominal pain may persist for several weeks.
Severe forms of food poisoning are predominantly observed in young children with weakened immunity. The risk of developing complications against the background of intoxication increases with prematurity, malnutrition and dysbacteriosis in history.
If a child is poisoned by poisonous plants, berries, lesions of the central nervous system are observed:
- retardation of reactions;
- euphoria;
- hallucinations;
- impaired speech, vision;
- convulsions.
If the cardiovascular system is damaged by toxins, the heart rate speeds up or slows down, blood pressure decreases.
Mushroom poisoning is very dangerous for children. After eating a pale toadstool, indomitable vomiting, cholera-like diarrhea with impurities of blood in the feces begins. Other symptoms are intestinal colic, respiratory disorders, convulsions. Toxins adversely affect the liver, which leads to the development of toxic hepatitis. AT 90% of cases are fatal due to acute liver failure.
Signs of fly agaric poisoning are increased salivation, shortness of breath, severe vomiting, convulsions, bronchospasm, hallucinations, nystagmus or strabismus. But the mortality rate is less than 1%.
Botulism develops when poor-quality canned food is consumed. The toxin affects the nervous system, which manifests itself in the form of paralysis and paresis. Poisoning in children can cause the development of acute respiratory failure, heart rhythm disturbances. The first symptoms appear after 4-6 hours. Worries about pain in the epigastric region, nausea, vomiting, diarrhea. Sometimes there are problems with vision. When the respiratory system is affected, shortness of breath begins, the skin in the region of the nasolabial triangle turns blue, and arrhythmia develops.
When the respiratory system is affected, shortness of breath begins, the skin in the region of the nasolabial triangle turns blue, and arrhythmia develops.
First aid for child poisoning
Act immediately. First aid rules:
- In case of poisoning with mushrooms, berries, medicines, induce vomiting.
- Gastric lavage with clean water to remove toxins from the intestines. Babies should not do the washing themselves, as the child can inhale the vomit. Instead, you can do a cleansing enema. The volume of water for gastric lavage - 16 ml / kg for children 3-6 years old, over 7 years old - 14 ml / kg.
- Taking enterosorbents - these drugs collect toxins in the intestinal lumen, remove them with feces.
- More to drink. You need to drink in small portions, but often. You can give your child water with a weak saline solution, weak tea, mineral water without gas.
- Call a doctor.
Timely first aid will help to avoid the development of complications of poisoning.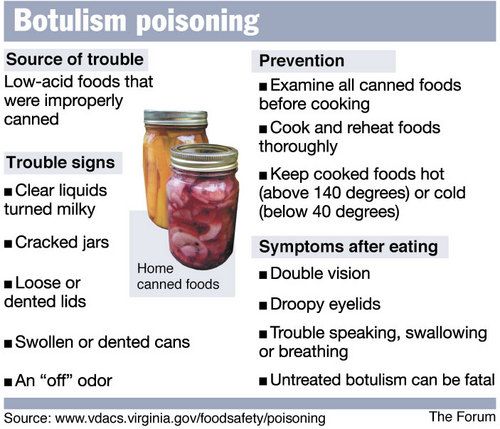
In case of poisoning, children should not:
- give painkillers, drugs, drugs for vomiting and diarrhea;
- apply hot or cold compresses to the abdomen;
- use soda to induce vomiting, potassium permanganate to wash the stomach;
- give milk and dairy products.
Diagnosis of food poisoning in a child
Diagnosis of food poisoning in a child can be done by a pediatrician or an infectious disease specialist. The examination begins with the collection of anamnesis, examination of the patient.
Specific diagnostic tests are prescribed to isolate the pathogen. Biomaterial - feces and vomit, gastric lavage, the remains of contaminated food. With a generalized form of infection, a blood culture is prescribed. Auxiliary methods - RIF, PCR, ELISA. Additionally, you may need to consult a neurologist, gastroenterologist, surgeon.
Be sure to carry out differential diagnosis to exclude acute gastritis, cholecystitis, pancreatitis, giardiasis, acute intestinal infection, inflammation of the appendix, meningitis. A blood test is prescribed to rule out a viral, bacterial infection, a stool test to detect infections caused by pathological bacteria.
A blood test is prescribed to rule out a viral, bacterial infection, a stool test to detect infections caused by pathological bacteria.
How to treat
Treatment of poisoning in a child begins with the elimination of signs of dehydration. Apply oral, parenteral rehydration therapy.
Auxiliaries:
- enzymes;
- sorbents;
- prebiotics to restore the balance of intestinal microflora;
- antimicrobials are necessary for severe toxic infection.
In case of toadstool poisoning, emergency hemosorption is performed to cleanse the blood of toxins.
Diet for child poisoning
It is best not to feed the child for 12-24 hours after poisoning. When vomiting stops, a sparing diet is indicated. Breastfed babies under one year of age need to skip a few feedings.
How to feed a child after poisoning:
- liquid porridge - rice, buckwheat, cooked in a mixture of equal amounts of water and milk;
- slimy soups;
- crackers;
- kefir;
- compotes;
- after a few days - vegetable puree, children's cottage cheese or kefir, yogurt without additives;
- gradually introduce meat and fish soufflé into the menu.

List of prohibited products - pastries, whole milk, black bread, fresh white bread. You can not give your child pasta, chocolate, ice cream, chips, sweet carbonated drinks, wheat and barley porridge. From vegetables, cucumbers, tomatoes, cabbage are contraindicated.
The duration of the diet is 14 days.
Possible consequences of food poisoning in a child
Complications occur in case of severe poisoning, lack of correct and timely therapy.
Possible effects:
- dysbacteriosis;
- renal and hepatic insufficiency;
- disturbances in the functioning of the nervous and immune systems;
- chronic diseases of the gastrointestinal tract.
Prognosis and prevention
Poisoning in a child of mild and moderate severity ends in complete recovery.
Methods of prevention:
- properly store food, observe the temperature regime and other storage conditions;
- observe the rules of heat treatment, children should absolutely not be given raw fish, poorly fried meat;
- drink only boiled, purified water, do not swallow water when swimming in reservoirs;
- wash hands, vegetables and fruits thoroughly;
- store medicines, chemicals out of the reach of children;
- to tell children about poisonous mushrooms, berries, plants, the dangers of their use.

People who work in the kitchen in children's institutions should have regular medical check-ups. In the presence of pustular skin pathologies, respiratory diseases, signs of an intestinal infection, the worker is not allowed into the catering unit.
Treatment of food poisoning in Moscow
Food poisoning in a child is a dangerous condition, you should not self-medicate, you should immediately consult a doctor. Call our clinic, describe the symptoms, the patient's condition, the possible cause of the poisoning. The administrator of the "Miracle Doctor" center will write you to the doctor in the near future.
Q&A
Why is acute poisoning dangerous for a child?
Fever, vomiting more often 3–5 times, diarrhea in a child is a reason to immediately call an ambulance.
Poisoning in a child at any age leads to a breakdown of the immune system. Dehydration is very dangerous for babies. In children under 4 years of age with profuse vomiting and loose stools, the critical phase of dehydration can occur within a few hours.
How to give water to a baby if he vomits very often?
Even if the vomiting is severe and persistent, the child must be given water. The consequences of dehydration are extremely dangerous for the child's body. You need to water the child in small portions - 1 tsp each. every 5 minutes. Water should not be cold, so as not to cause spasm and vomiting. The optimal temperature is a few degrees above body temperature.
Food poisoning in a child. What is Food Poisoning in a Child?
IMPORTANT
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
Food poisoning in a child is an acute infectious-toxic lesion that occurs as a result of eating poor-quality products containing pathogens and their toxins, plant or other poisons.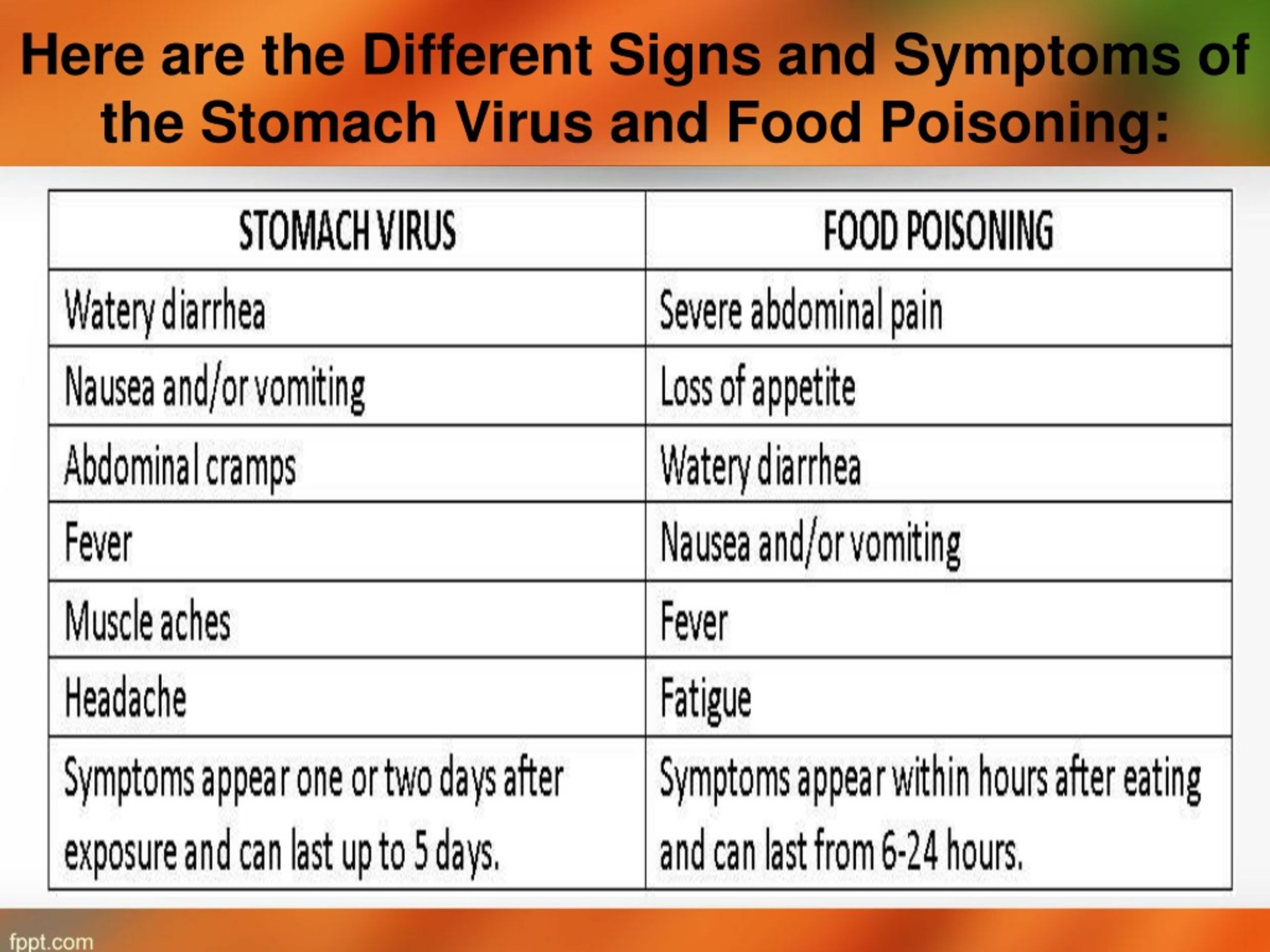 Food poisoning in a child is manifested by diarrhea, vomiting, fever, intoxication, dehydration. Diagnosis of food poisoning in children involves the clarification of the epidemiological history; identification of a pathogen or toxin in blood, feces, vomit, food samples. Treatment of food poisoning in children requires immediate gastric lavage or cleansing enema, enterosorbents, rehydration.
Food poisoning in a child is manifested by diarrhea, vomiting, fever, intoxication, dehydration. Diagnosis of food poisoning in children involves the clarification of the epidemiological history; identification of a pathogen or toxin in blood, feces, vomit, food samples. Treatment of food poisoning in children requires immediate gastric lavage or cleansing enema, enterosorbents, rehydration.
- Classification
- Causes
- Symptoms of food poisoning in a child
- Diagnosis of food poisoning in a child
- Treatment of food poisoning in a child
- Prognosis and prevention of food poisoning in a child
- Prices for treatment
General
Food poisoning in a child is food poisoning or intoxication associated with the consumption of infected food, water, or toxic (plant, chemical, medicinal) substances. Food poisoning in children occupies a leading place in the range of infectious pathology and toxicology of childhood and represents a serious problem in practical pediatrics.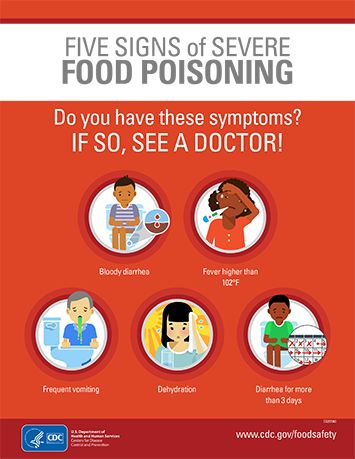
Food poisoning in a child is much more severe than in adults, which is explained by the characteristics of the child's body: low acidity of gastric juice, incomplete formation of intestinal microflora, faster absorption of the poison and its distribution throughout the body, relatively low detoxification capacity of the liver and filtration function of the kidneys, etc. Often the same products that do not cause any signs of poisoning in an adult cause food poisoning in a child.
Food poisoning in a child
Classification
A child may have the following types of food poisoning:
In the clinical course of food poisoning in a child, 3 stages are distinguished:
- Latent (asymptomatic) - lasts from the moment the toxin/poison is taken until the first symptoms of food poisoning appear in the child.
 The duration of the latent period depends on the age and individual characteristics of the child, the amount of a toxic substance that has entered the body with food, and the rate of its absorption. The latent stage of food poisoning is the most favorable "window" for the treatment of a child, when the poison has not yet entered the bloodstream and has not exerted its toxic effect. First aid in this case is gastric lavage and the intake of enterosorbents.
The duration of the latent period depends on the age and individual characteristics of the child, the amount of a toxic substance that has entered the body with food, and the rate of its absorption. The latent stage of food poisoning is the most favorable "window" for the treatment of a child, when the poison has not yet entered the bloodstream and has not exerted its toxic effect. First aid in this case is gastric lavage and the intake of enterosorbents. - Toxicogenic - lasts from the appearance of the first signs of poisoning to the elimination of bacteria and poison from the body. The toxicogenic period is manifested by the developed symptoms of food poisoning in a child, characteristic of this toxic infection or poison. This stage requires identification of bacteria and poison, their removal (gastric lavage, cleansing enema, forced diuresis), detoxification, etc.
- Stage of convalescence - restoration of impaired functions (digestive, excretory, immune, etc.).
Causes
Infectious food poisoning in a child (food poisoning) can be caused by staphylococcus aureus, proteus, klebsiella, clostridia, citrobacter, enterotoxigenic strains of Escherichia coli, etc. These pathogens enter the body exclusively with food, in which they first multiply and produce toxins. Contamination of food and the accumulation of toxins are favored by non-compliance with sanitary and hygienic standards in the process of storing, preparing and selling food. At the same time, the products may look like poor quality (unpleasant smell, taste, changed color, texture) or have normal organoleptic qualities.
These pathogens enter the body exclusively with food, in which they first multiply and produce toxins. Contamination of food and the accumulation of toxins are favored by non-compliance with sanitary and hygienic standards in the process of storing, preparing and selling food. At the same time, the products may look like poor quality (unpleasant smell, taste, changed color, texture) or have normal organoleptic qualities.
Microbial sources that seed food can be persons suffering from intestinal infections, purulent diseases (tonsillitis, furunculosis, streptoderma, felons, mastitis, etc.), as well as animals that pollute water, soil, plants and other environmental objects with their feces. Food poisoning in a child can be caused by drinking unboiled water, contaminated milk and dairy products, eggs, cream confectionery, fish and seafood, sausages, meat (beef, pork, chicken, etc.), home-made canned food, etc.
Food poisoning in children can occur as sporadic, familial or mass outbreaks. They are characterized by an increase in the incidence in the summer-autumn period, when there are favorable conditions for the reproduction of microbial pathogens and the accumulation of toxins.
They are characterized by an increase in the incidence in the summer-autumn period, when there are favorable conditions for the reproduction of microbial pathogens and the accumulation of toxins.
Non-infectious food poisoning is usually associated with the child's accidental consumption of poisonous berries (nightshade, wolfberry, black elderberry, crow's eye, etc.), plants (hemlock, henbane, poisonous milestone, dope, etc.), mushrooms (pale toadstool, fly agaric, false chanterelles or honey mushrooms). Food poisoning in a child can occur when eating agricultural products contaminated with toxic chemical impurities (fungicides, insecticides, inorganic compounds).
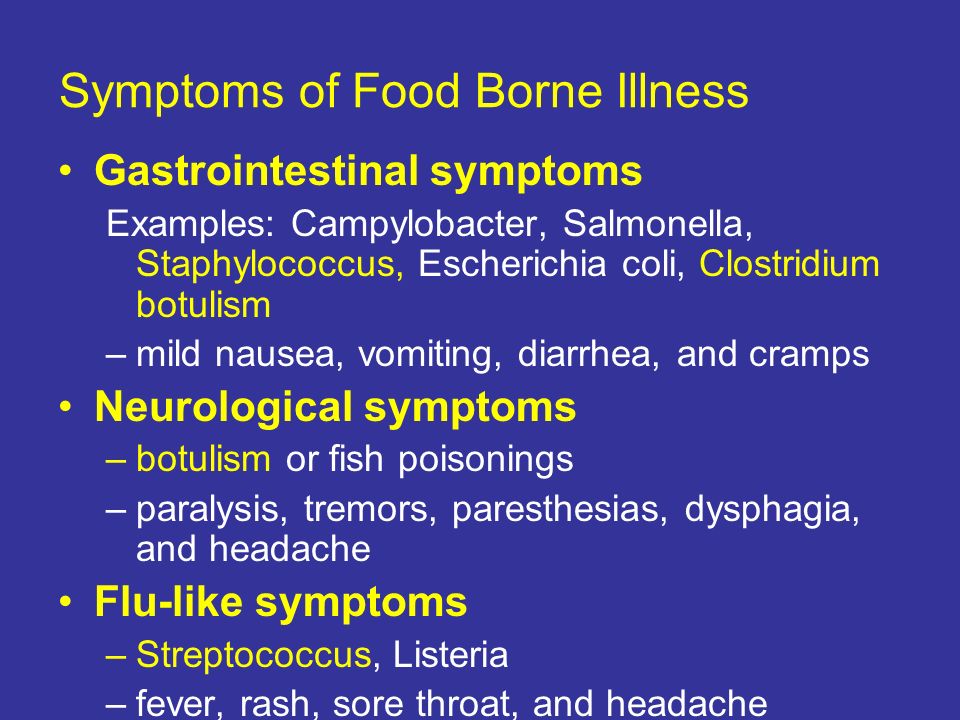
Symptoms of food poisoning in a child
The clinical picture of food poisoning in a child with various toxic infections is very similar. Usually the latent stage lasts 2-6 hours; sometimes shortened to 30 minutes. or lengthens up to 24 hours. Food poisoning in a child is manifested by signs of gastroenteritis, general infectious symptoms, intoxication, dehydration.
The disease begins acutely, with nausea, repeated vomiting of food eaten, abdominal pain (mainly in the stomach area), watery diarrhea with impurities of greens, mucus, streaks of blood. The frequency of stool reaches 5-10 times a day.
Almost simultaneously with the phenomena of gastroenteritis, the body temperature rises to 38-39 ° C. The intoxication syndrome is rapidly growing, characterized by lethargy, refusal to eat, headache and muscle pain. Fluid loss with vomiting and stool leads to dehydration: facial features are sharpened, the skin becomes pale and dry to the touch. A child with food poisoning may have convulsions, oligo-, anuria, hemodynamic disorders, acidosis.
The course of food poisoning is short; in most cases, symptoms regress after 2–3 days, although weakness and abdominal pain may persist for longer. Severe forms of food poisoning can be observed in young children, debilitated individuals with a concomitant background (prematurity, malnutrition, dysbacteriosis, etc.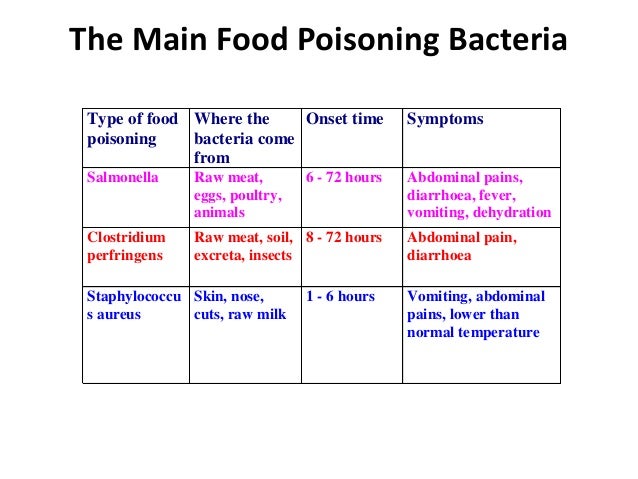 ). In severe cases, the child may develop necrotic enteritis, infectious-toxic or hypovolemic shock, endocarditis, sepsis.
). In severe cases, the child may develop necrotic enteritis, infectious-toxic or hypovolemic shock, endocarditis, sepsis.
In case of food poisoning by poisonous plants in a child, the central nervous system is often affected, which can be manifested by lethargy, euphoria, hallucinations, visual impairment, speech disorders, convulsions, coma. With a toxic effect on the cardiovascular system, tachycardia or bradycardia, arrhythmia, and arterial hypotension occur. Most plants mainly affect the gastrointestinal tract, which makes food poisoning in a child less dangerous.
Food poisoning of a child with mushrooms always occurs through the fault of adults who allow the use of unknown or dubious "gifts of the forest" in food. Poisoning with a pale toadstool is accompanied by indomitable vomiting, intestinal colic, cholera-like diarrhea mixed with blood, convulsions, and respiratory distress. The action of the poison leads to the development of toxic hepatitis, and in 90% of cases - to death due to acute liver failure.
In case of fly agaric poisoning, increased salivation, vomiting, shortness of breath, bronchospasm, hallucinations, and convulsions occur. The mortality rate for fly agaric poisoning is 1%. The clinical picture, diagnosis and treatment of botulism can be found here.
Diagnosis of food poisoning in a child
Food poisoning in a child can usually be diagnosed by a pediatrician or pediatric infectious disease specialist. The diagnosis of food poisoning in a child is facilitated by the clarification of the epidemiological history, a typical clinical picture, an indication of group cases of poisoning of persons who consumed the same food.
Specific diagnostic tests include the isolation of the pathogen from bacteriological culture of feces, vomit, gastric lavage, and the remains of an infected product. In case of suspicion of a generalized form of infection, a blood culture is performed. During mass outbreaks of food poisoning in children's groups, kitchen workers are subject to examination, from whom swabs are taken from their hands, from the nasopharynx, and rectum.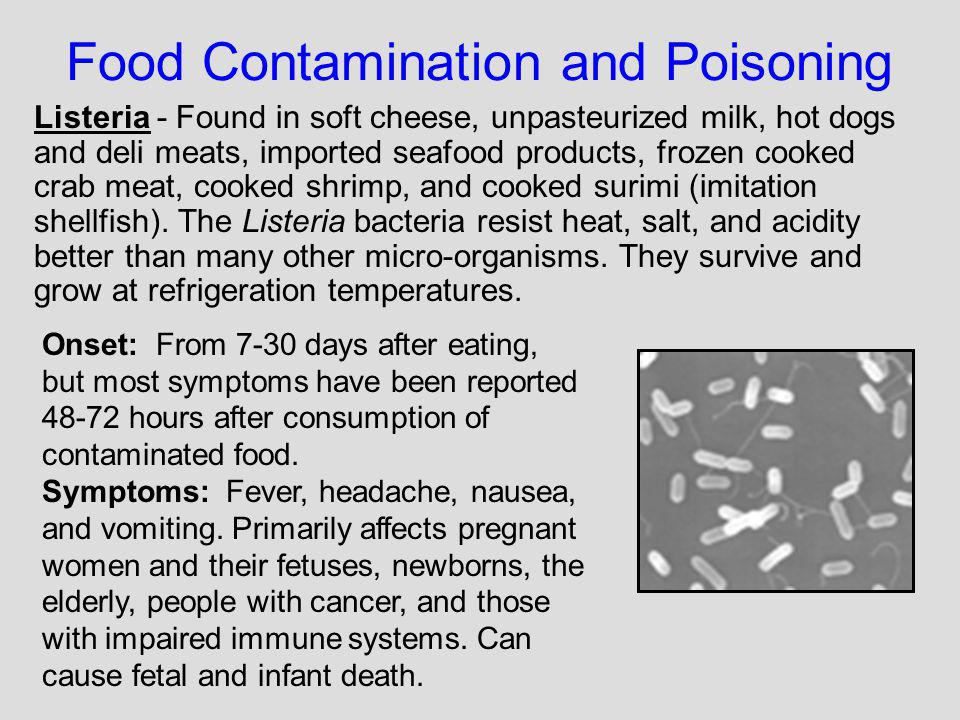 Express methods for detecting the pathogen (RIF, ELISA, PCR) are of secondary importance.
Express methods for detecting the pathogen (RIF, ELISA, PCR) are of secondary importance.
In some cases, a child with food poisoning may need to consult a pediatric neurologist, pediatric gastroenterologist, pediatric surgeon. Differential diagnosis of food poisoning is carried out with acute gastritis, acute appendicitis, cholecystitis, pancreatitis, giardiasis, acute intestinal infection, meningitis in a child.
Treatment of food poisoning in a child
Emergency assistance in establishing the fact of food poisoning in a child consists in washing the stomach to clean water and administering a cleansing enema to remove toxins from the gastrointestinal tract. For the same purpose, the appointment of enterosorbents (activated carbon, combined preparations) is indicated.
To eliminate dehydration, oral rehydration (sweet tea, saline solutions) is necessary for moderate forms - parenteral rehydration therapy with saline solutions./stomach-flu-symptoms-770657-86-310db9fd0f1543e289250a64c8384d58.png) In case of food poisoning, the child is prescribed replacement therapy with polyenzymatic preparations with pancreatin. Antimicrobial therapy for a child with food poisoning is carried out only for severe toxic infections under the supervision of a doctor.
In case of food poisoning, the child is prescribed replacement therapy with polyenzymatic preparations with pancreatin. Antimicrobial therapy for a child with food poisoning is carried out only for severe toxic infections under the supervision of a doctor.
It is advisable to abstain from eating for 12-24 hours. After the cessation of vomiting, a sparing diet is recommended to the child (liquid cereals, mucous soups, crackers, compotes, kefir).
In case of poisoning with a pale toadstool, a child needs an emergency extracorporeal hemocorrection (hemosorption).
Prediction and prevention of food poisoning in a child
Food poisoning in a child that occurs in mild or moderate severity usually ends in a complete recovery. The consequences of food poisoning in a child can be various dysfunctions of organs and systems. So, the outcome of food poisoning is often dysbacteriosis, and mushroom poisoning - kidney and liver failure. With severe food poisoning, a child may develop severe multiple organ failure, requiring intensive care. With toxic infections, the lethality is low (about 1%), which cannot be said about mushroom poisoning.
With severe food poisoning, a child may develop severe multiple organ failure, requiring intensive care. With toxic infections, the lethality is low (about 1%), which cannot be said about mushroom poisoning.
Prevention of food poisoning in a child dictates the need for proper storage and adequate heat treatment of food products, drinking only boiled water, thorough washing of hands and food under running water. Regular hygienic examination of persons working in children's kitchens and in public catering is necessary; preventing workers with pustular skin diseases (pyoderma), respiratory tract infections, intestinal infections from entering the catering unit.
It is necessary to acquaint children with poisonous plants and mushrooms, and strictly forbid them to eat unknown berries, fruits, seeds, etc.
You can share your medical history, what helped you in the treatment of food poisoning in a child.
Sources
- In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests.