Baby food rash around mouth
My child has a rash around the mouth. Is it a food allergy?
Rashes around children’s mouths are common. They can happen when an irritant touches the skin or through the overuse of topical products. Certain foods may also trigger eczema flare-ups. In rare cases, a food allergy causes the rash.
When a rash appears around the mouth, it can be itchy or cause a burning sensation. The rash may appear red on light skin but be skin-colored on dark skin.
Several substances may trigger a rash, but it is often difficult to identify the cause. Parents and caregivers can help a child avoid possible triggers, including food allergens.
This article reviews the possible causes of skin rashes around the mouth and the treatment options.
The American College of Allergy, Asthma, & Immunology notes that food allergies can cause skin reactions and rashes when a person comes into contact with an allergen.
However, a rash around the mouth is more likely to have other causes, such as perioral dermatitis.
Food allergy symptoms can range from mild to severe and appear either immediately or some time after contact with the allergen. A severe food allergy can cause anaphylaxis, which can be life threatening.
Quick reactions develop within 1–2 hours of eating a food. To test what causes a quick reaction, doctors use skin prick tests. When the test is positive, it means that the child has developed immunoglobulin E (IgE) antibodies in response to the food. It is easier for doctors to determine the trigger for quick reactions than for delayed reactions.
Delayed reactions develop over 24–48 hours and are probably due to immune cells in the skin reacting to the food. These cells are called T cells. Skin prick tests are often negative in these cases, as IgE antibodies do not cause the reaction.
To identify the cause of a delayed reaction, doctors often recommend eliminating foods from the diet one by one and monitoring any symptoms. This can take a lot of time and persistence.
To discover more evidence-based information and resources for asthma & allergies, visit our dedicated hub.
Various factors can cause children to develop a rash around the mouth. These include:
Perioral dermatitis
Perioral dermatitis is a rash that appears around the mouth. On light skin, it may appear red or pink, resembling an acne breakout. On dark skin, it may be skin-colored. It can cause itchiness, stinging, and burning.
There are several potential causes in children, which can vary among individuals. These include:
- the long-term use of topical steroid creams
- prolonged use of inhaled prescription steroid sprays
- the overuse of heavy face creams or moisturizers
- skin irritants, such as soaps and other substances
- fluoride toothpaste
- acidic foods, such as tomatoes, strawberries, and citrus fruits, touching the skin
Learn more about perioral dermatitis and see some pictures.
Eczema
Eczema is an inflammatory skin condition that typically causes the following skin issues:
- itching
- a raised rash
- dry skin
- oozing or crusting
- swelling
- discoloration
Eczema can develop at any age and sometimes affects the area around the mouth.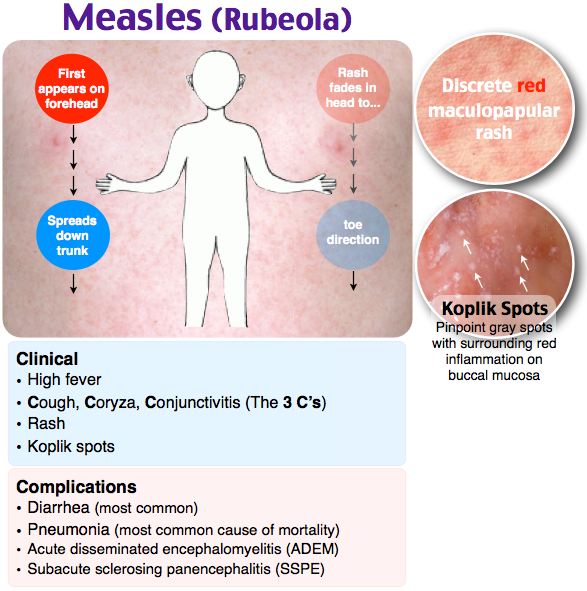 Certain foods, particularly acidic foods, may trigger an eczema flare-up, but they are not the underlying cause of eczema.
Certain foods, particularly acidic foods, may trigger an eczema flare-up, but they are not the underlying cause of eczema.
Learn more about eczema in children.
Certain foods can trigger a systemic reaction, including a rash around the mouth. The following food groups are the most common triggers of allergic reactions:
- shellfish
- soy
- peanuts
- cow’s milk
- tree nuts
- eggs
- wheat
- seafood
The following foods are acidic and may cause irritation if they come into contact with the skin:
- tomatoes and tomato sauces
- citrus fruits, such as oranges, lemons, and grapefruits
- strawberries
If a child regularly experiences a rash around the mouth, healthcare professionals may recommend that they undergo testing for food allergies.
Learn more about common foods that cause allergies.
It may not be possible to avoid a rash around the mouth, as the causes can vary. However, people can lower the likelihood of this symptom by:
- avoiding using topical steroid creams and heavy moisturizers around the mouth
- avoiding eating foods that can cause an allergic reaction
- limiting exposure to chemicals or other irritants
- wiping a child’s face gently with a damp face cloth after eating to avoid leaving traces of food on the skin
In some cases, the rash may resolve on its own. A child may only need to avoid exposing their skin to the irritant.
A child may only need to avoid exposing their skin to the irritant.
In other cases, a child may benefit from visiting a dermatologist, who may recommend:
- stopping using corticosteroids, including hydrocortisone cream, if applicable
- switching to fragrance-free, soap-free skin cleansers
- keeping the skin clean and applying fragrance-free moisturizer regularly
A dermatologist can help determine the best course of action and develop a personalized treatment plan for each child.
A parent or caregiver should consider contacting a doctor if a child regularly develops a rash around the mouth.
It is essential to seek emergency medical care if a child develops symptoms of anaphylaxis.
Anaphylaxis is a severe allergic reaction that can be life threatening. The symptoms develop suddenly and include:
- hives
- swelling of the face or mouth
- wheezing
- fast, shallow breathing
- a fast heart rate
- clammy skin
- anxiety or confusion
- dizziness
- vomiting
- blue or white lips
- fainting or loss of consciousness
If someone has these symptoms:
- Check whether they are carrying an epinephrine pen.
.jpg) If they are, follow the instructions on the side of the pen to use it.
If they are, follow the instructions on the side of the pen to use it. - Dial 911 or the number of the nearest emergency department.
- Lay the person down from a standing position. If they have vomited, turn them onto their side.
- Stay with them until the emergency services arrive.
Some people may need more than one epinephrine injection. If the symptoms do not improve in 5–15 minutes, or they come back, use a second pen if the person has one.
A rash around a child’s mouth may clear on its own, but it could require changes to the child’s diet or skin care routine. In some cases, a doctor may need to prescribe medication to help treat any underlying infections.
By avoiding triggers, a person should see improvements in their rash.
A rash around a child’s mouth can have various causes. Certain foods can sometimes trigger an immune response that leads to a rash and other symptoms. Severe allergic reactions can be life threatening.
Common causes of a rash around the mouth include reactions to a long-term topical steroid, the use of certain skin care products, or skin contact with highly acidic foods.
Once a person stops their exposure to the trigger, the rash should clear. Identifying triggers can take time and persistence.
My child has a rash around the mouth. Is it a food allergy?
Rashes around children’s mouths are common. They can happen when an irritant touches the skin or through the overuse of topical products. Certain foods may also trigger eczema flare-ups. In rare cases, a food allergy causes the rash.
When a rash appears around the mouth, it can be itchy or cause a burning sensation. The rash may appear red on light skin but be skin-colored on dark skin.
Several substances may trigger a rash, but it is often difficult to identify the cause. Parents and caregivers can help a child avoid possible triggers, including food allergens.
This article reviews the possible causes of skin rashes around the mouth and the treatment options.
The American College of Allergy, Asthma, & Immunology notes that food allergies can cause skin reactions and rashes when a person comes into contact with an allergen.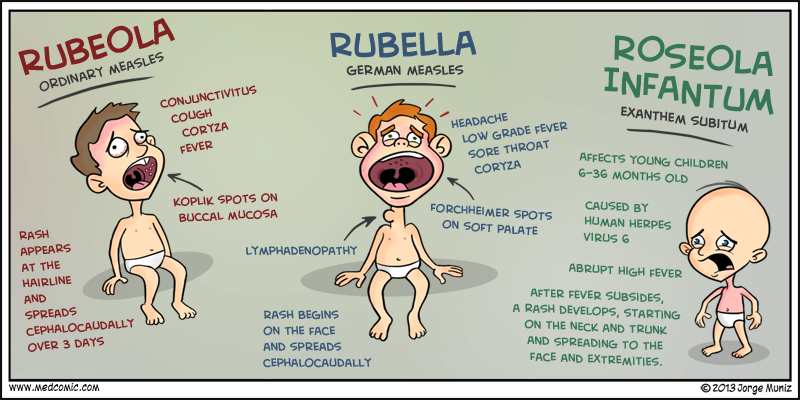
However, a rash around the mouth is more likely to have other causes, such as perioral dermatitis.
Food allergy symptoms can range from mild to severe and appear either immediately or some time after contact with the allergen. A severe food allergy can cause anaphylaxis, which can be life threatening.
Quick reactions develop within 1–2 hours of eating a food. To test what causes a quick reaction, doctors use skin prick tests. When the test is positive, it means that the child has developed immunoglobulin E (IgE) antibodies in response to the food. It is easier for doctors to determine the trigger for quick reactions than for delayed reactions.
Delayed reactions develop over 24–48 hours and are probably due to immune cells in the skin reacting to the food. These cells are called T cells. Skin prick tests are often negative in these cases, as IgE antibodies do not cause the reaction.
To identify the cause of a delayed reaction, doctors often recommend eliminating foods from the diet one by one and monitoring any symptoms. This can take a lot of time and persistence.
This can take a lot of time and persistence.
To discover more evidence-based information and resources for asthma & allergies, visit our dedicated hub.
Various factors can cause children to develop a rash around the mouth. These include:
Perioral dermatitis
Perioral dermatitis is a rash that appears around the mouth. On light skin, it may appear red or pink, resembling an acne breakout. On dark skin, it may be skin-colored. It can cause itchiness, stinging, and burning.
There are several potential causes in children, which can vary among individuals. These include:
- the long-term use of topical steroid creams
- prolonged use of inhaled prescription steroid sprays
- the overuse of heavy face creams or moisturizers
- skin irritants, such as soaps and other substances
- fluoride toothpaste
- acidic foods, such as tomatoes, strawberries, and citrus fruits, touching the skin
Learn more about perioral dermatitis and see some pictures.
Eczema
Eczema is an inflammatory skin condition that typically causes the following skin issues:
- itching
- a raised rash
- dry skin
- oozing or crusting
- swelling
- discoloration
Eczema can develop at any age and sometimes affects the area around the mouth. Certain foods, particularly acidic foods, may trigger an eczema flare-up, but they are not the underlying cause of eczema.
Learn more about eczema in children.
Certain foods can trigger a systemic reaction, including a rash around the mouth. The following food groups are the most common triggers of allergic reactions:
- shellfish
- soy
- peanuts
- cow’s milk
- tree nuts
- eggs
- wheat
- seafood
The following foods are acidic and may cause irritation if they come into contact with the skin:
- tomatoes and tomato sauces
- citrus fruits, such as oranges, lemons, and grapefruits
- strawberries
If a child regularly experiences a rash around the mouth, healthcare professionals may recommend that they undergo testing for food allergies.
Learn more about common foods that cause allergies.
It may not be possible to avoid a rash around the mouth, as the causes can vary. However, people can lower the likelihood of this symptom by:
- avoiding using topical steroid creams and heavy moisturizers around the mouth
- avoiding eating foods that can cause an allergic reaction
- limiting exposure to chemicals or other irritants
- wiping a child’s face gently with a damp face cloth after eating to avoid leaving traces of food on the skin
In some cases, the rash may resolve on its own. A child may only need to avoid exposing their skin to the irritant.
In other cases, a child may benefit from visiting a dermatologist, who may recommend:
- stopping using corticosteroids, including hydrocortisone cream, if applicable
- switching to fragrance-free, soap-free skin cleansers
- keeping the skin clean and applying fragrance-free moisturizer regularly
A dermatologist can help determine the best course of action and develop a personalized treatment plan for each child.
A parent or caregiver should consider contacting a doctor if a child regularly develops a rash around the mouth.
It is essential to seek emergency medical care if a child develops symptoms of anaphylaxis.
Anaphylaxis is a severe allergic reaction that can be life threatening. The symptoms develop suddenly and include:
- hives
- swelling of the face or mouth
- wheezing
- fast, shallow breathing
- a fast heart rate
- clammy skin
- anxiety or confusion
- dizziness
- vomiting
- blue or white lips
- fainting or loss of consciousness
If someone has these symptoms:
- Check whether they are carrying an epinephrine pen. If they are, follow the instructions on the side of the pen to use it.
- Dial 911 or the number of the nearest emergency department.
- Lay the person down from a standing position. If they have vomited, turn them onto their side.
- Stay with them until the emergency services arrive.
Some people may need more than one epinephrine injection. If the symptoms do not improve in 5–15 minutes, or they come back, use a second pen if the person has one.
A rash around a child’s mouth may clear on its own, but it could require changes to the child’s diet or skin care routine. In some cases, a doctor may need to prescribe medication to help treat any underlying infections.
By avoiding triggers, a person should see improvements in their rash.
A rash around a child’s mouth can have various causes. Certain foods can sometimes trigger an immune response that leads to a rash and other symptoms. Severe allergic reactions can be life threatening.
Common causes of a rash around the mouth include reactions to a long-term topical steroid, the use of certain skin care products, or skin contact with highly acidic foods.
Once a person stops their exposure to the trigger, the rash should clear. Identifying triggers can take time and persistence.
Take care of your baby's skin
Please wait
All products
Cosmetics
Food additives
Mom and children
for the RT cavity
hygiene
9000 nine0031The skin of babies and children is much more fragile and sensitive than adults. Many mothers are wondering how to properly care for their skin. child to be as healthy as possible. To keep skin healthy baby and protect the skin from irritants, parents should be vigilant and careful in choosing care products. nine0003
There is a difference between the needs of the skin of a newborn baby, baby up to 3 years and a child from 3 to 10-12 years. As a general rule, children and infants should not use hygiene products and skin care products intended for for adults.
What are the features skin of babies and children?
“Skin like a baby” is an expression commonly used when talking about about soft and velvety skin, but this is not entirely true. At birth, the baby's skin is already fully formed, but it is thinner and more vulnerable, than an adult, and is not able to effectively perform its barrier function. A few weeks after birth, the baby's skin stops producing sebum, and the sebaceous glands in the skin are not activated until adolescence. Thus, the hydrolipidic layer becomes thinner, and therefore less its barrier function becomes effective. As a result, the skin becomes drier and more susceptible to pathogens and allergens. nine0003
At birth, the baby's skin is already fully formed, but it is thinner and more vulnerable, than an adult, and is not able to effectively perform its barrier function. A few weeks after birth, the baby's skin stops producing sebum, and the sebaceous glands in the skin are not activated until adolescence. Thus, the hydrolipidic layer becomes thinner, and therefore less its barrier function becomes effective. As a result, the skin becomes drier and more susceptible to pathogens and allergens. nine0003
The skin of babies and toddlers is highly absorbent, so all products applied to children's skin, are absorbed and enter the bloodstream faster than adults. Therefore, for the hygiene of the child's skin, it is important to use gentle products, which guarantee very good tolerability and have a high level safety while meeting strict production requirements.
Baby skin and atopic dermatitis
Various external irritants such as wind, cold, hard water and heating, weaken the skin of the child, make it more dry and reactive. With atopic dermatitis the child's skin is very dry and rough, sometimes with red spots. Leather becomes itchy, the child's sleep is disturbed. nine0003
With atopic dermatitis the child's skin is very dry and rough, sometimes with red spots. Leather becomes itchy, the child's sleep is disturbed. nine0003
Atopic dermatitis is a very common type of dermatosis that can start in the second or third month of life and in most cases disappears after some years. Atopic skin suffers from increased permeability of the horny layer due to lipid deficiency and therefore ceases to properly perform a barrier function. This causes inflammation and an outbreak of atopic dermatitis, most often accompanied by severe itching.
When scratching the affected areas, wounds are formed that are harmful skin. Children's skin becomes more permeable to allergens. atopic dermatitis occurs in two successive phases - exacerbation (spots, itching, risk of infection) and remission (symptoms improve but skin remains dry and itchy). There are 3 main types of environmental allergens that are more common cause acute inflammatory reactions in total:
Aeroallergens: dust mites, pollen, mold and fungal spores, wool cats and dogs
Food allergens
Contact allergens: nickel, fragrances
Skin irritation around the mouth
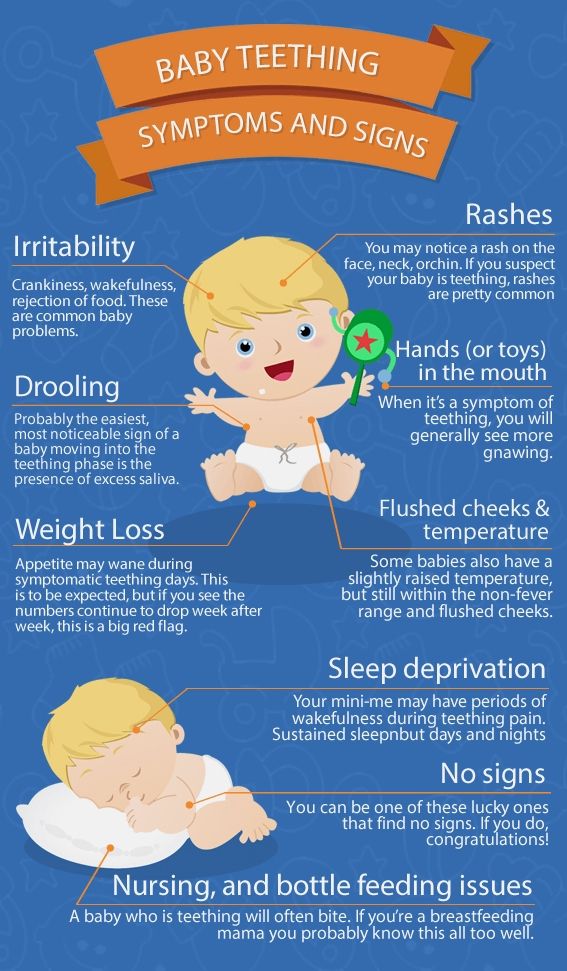
Irritation around the mouth is characterized by redness, small pimples, dryness and roughness. Perioral dermatitis occurs around the mouth under the influence of profuse salivation, with prolonged use of a pacifier, thumb sucking, or during teething teeth. The enzyme amylase, which is found in saliva, increases irritation. In winter, perioral dermatitis is aggravated by cold and wind. nine0003
Perioral dermatitis occurs around the mouth under the influence of profuse salivation, with prolonged use of a pacifier, thumb sucking, or during teething teeth. The enzyme amylase, which is found in saliva, increases irritation. In winter, perioral dermatitis is aggravated by cold and wind. nine0003
How to care for the skin of babies and children?
1. Daily attention
Pay attention to risk areas: face, skin around the mouth, the area under the diaper and all the folds on the skin.
· Always consult your pharmacist or pediatrician when choosing your care products.
Avoid wool and synthetics when choosing tight clothing.
Make sure that the air in the room where the baby, not too dry, and the air temperature does not exceed 20 ° C.
2. Hygiene
Use a mild hygiene product, do not containing soap that protects the skin child and does not irritate the skin and eyes. When bathing a child, make sure that the temperature of the water in the bath was not higher than 35 ° C, as heat increases dryness skin.
Dry skin thoroughly and gently after bathing baby with a soft towel, paying special attention to the folds.
Then apply moisturizer to baby's delicate skin cream with very high tolerance. nine0003
To cleanse the skin of a child's face, you can use cotton pads and soap-free hygiene products such as micellar water. This help to avoid contact with the city hard water, which can irritate the skin.
3. Care
The skin of babies and children is very delicate, so it is important to learn how to properly protect it from external stimuli. Use moisturizing and nourishing creams or milks with a high level of safety and portability. nine0003
If the child has normal skin, daily Apply a moisturizing milk that nourishes and protects the skin.
If your skin tends to be dry, choose extra nourishing creams that restore the barrier function of the skin, prevent itching and provide instant comfort.
BIODERMA ABCDerm - baby and baby skin care
special cleaning and care products. To support and restore the natural physiological balance of the delicate skin of babies, BIODERMA has created a line of 9 products0046 ABCDerm , suitable for infants from birth (excluding preterm infants) children).
To support and restore the natural physiological balance of the delicate skin of babies, BIODERMA has created a line of 9 products0046 ABCDerm , suitable for infants from birth (excluding preterm infants) children).
To wash the body, face and hair of a child, use ABCDerm Gel Moussant - gentle cleansing gel, without soap, which maintains the integrity of the skin barrier. In addition, it forms a light foam for a pleasant bathing baby.
To moisturize the skin use ABCDerm Hydratant - gentle moisturizer milk that creates a protective layer and strengthens the natural skin barrier, and also limits factors that cause irritation. nine0003
For daily cleansing use micellar water ABCDerm h3O or micellar wipes ABCDerm h3O Lingettes which are very convenient and practical when you the baby is away from home. Extra gentle micellar water supports natural balance, soothes and softens the skin.
Cream for irritated skin around the mouth ABCDerm Peri-oral blocks the irritating effect of saliva, soothes the skin, reduces redness, limits bacterial growth and protects the skin. nine0003
The ABCDERM line meets the following dermatological requirements: safety (reducing the risk of allergies thanks to carefully selected ingredients), effectiveness (carefully selected safe ingredients in optimal dosages with proven dermatological efficacy), tolerability (minimum amount components to guarantee portability and comfort) and control (obligatory control at each stage of production up to before the sale). nine0003
BIODERMA ABCDERM moisturizing milk for children, 200 ml
1
Item in stock
€15. 99
99
BIODERMA ABCDERM baby wet wipes h3O, 60 pcs. nine0003
0
Item in stock
€9.99
Feel good
Beauty
Diseases, symptoms and treatment
Holiday preparation
Free consultations
News AZETA
Login
Continue shopping
Vai esat pārliecināti, ka vēlaties veikt šo darbību?
Parental leaflet on viral diseases
Parental leaflet. nine0218
nine0218
Measles is a viral infection with a very high susceptibility. If a person has not had measles or has not been vaccinated against this infection, then after contact with the patient, infection occurs in almost 100% of cases. The measles virus is highly volatile. The virus can spread through ventilation pipes and elevator shafts - at the same time, children living on different floors of the house get sick.
The period from contact with a person with measles to the appearance of the first signs of the disease lasts from 7 to 14 days. nine0003
The disease begins with a severe headache, weakness, fever up to 40 degrees C. A little later, a runny nose, cough and almost complete lack of appetite join these symptoms.
Very characteristic of measles is the appearance of conjunctivitis - inflammation of the mucous membrane of the eyes, which is manifested by photophobia, lacrimation, sharp redness of the eyes, and subsequently - the appearance of purulent discharge.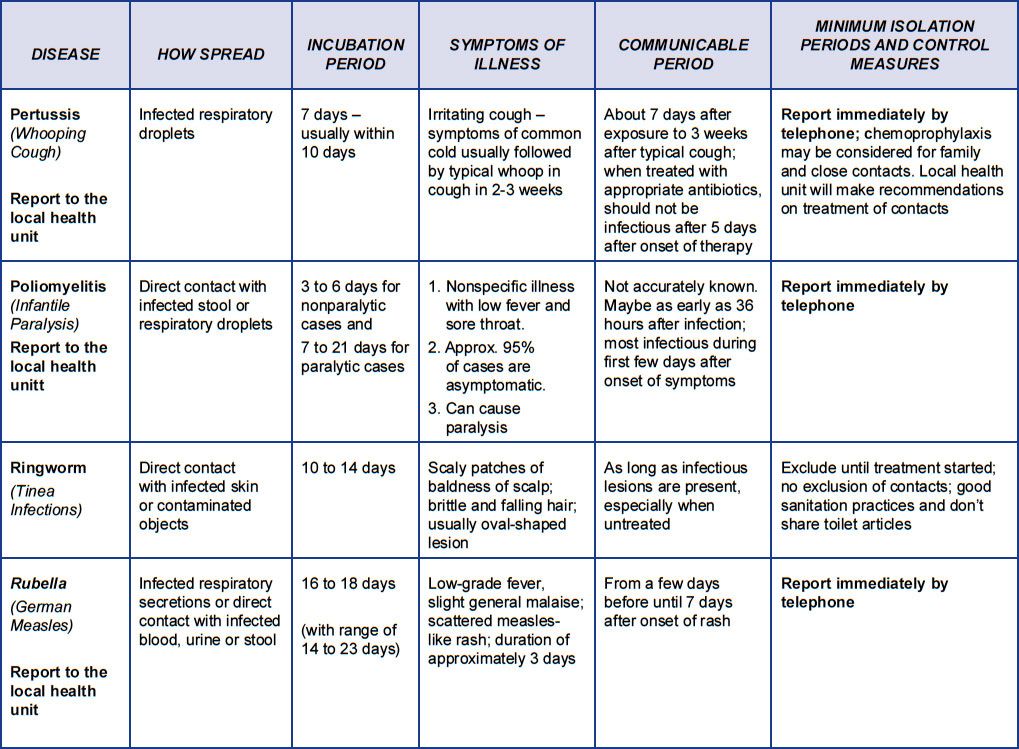 These symptoms last 2 to 4 days.
These symptoms last 2 to 4 days.
Rash appears on the 4th day of illness , which looks like small red spots of various sizes (from 1 to 3 mm in diameter), with a tendency to merge. The rash occurs on the face and head (it is especially characteristic of its appearance behind the ears) and spreads throughout the body for 3-4 days. It is very characteristic of measles that the rash leaves behind pigmentation (dark spots that persist for several days), which disappears in the same sequence as the rash appears.
Measles can be quite serious complications . These include inflammation of the lungs (pneumonia), inflammation of the middle ear (otitis media), and sometimes such a formidable complication as encephalitis (inflammation of the brain).
It must be remembered that after suffering from measles for a sufficiently long period of time (up to 2 months) there is a suppression of immunity, so the child can get sick with some cold or viral disease, so you need to protect him from excessive stress, if possible from contact with sick children. nine0003
nine0003
After measles, lifelong immunity develops. All those who have had measles become immune to this infection.
The only reliable protection against the disease is vaccination against measles, which is included in the National Immunization Schedule.
Parent's note.
Rubella is an airborne viral infection. As a rule, children who stay in a water room for a long time with a child who is a source of infection get sick. Rubella in its manifestations is very similar to measles, but it is much easier. nine0003
The period from contact to the appearance of the first signs of illness lasts from 14 to 21 days.
Rubella begins with an increase in the occipital lymph nodes and an increase in body temperature up to 38 degrees C. A runny nose, and sometimes a cough, joins a little later. A rash appears 2 to 3 days after the onset of the disease. Rubella is characterized by a pink, punctate rash that begins with a rash on the face and spreads throughout the body. Rubella rash, unlike measles, never merges, there may be a slight itch. The period of rashes can be from several hours, during which there is no trace of the rash, up to 2 days. nine0003
Rubella rash, unlike measles, never merges, there may be a slight itch. The period of rashes can be from several hours, during which there is no trace of the rash, up to 2 days. nine0003
The treatment of rubella is to relieve the main symptoms - the fight against fever, if any, the treatment of the common cold, expectorants.
Complications from rubella are rare.
After rubella, immunity also develops, re-infection is extremely rare, but can occur.
It is therefore very important to get vaccinated against rubella, which, like the measles vaccine, is included in the National Immunization Schedule. nine0218
Information for parents.
Mumps (mumps) is a childhood viral infection characterized by acute inflammation in the salivary glands.
Infection occurs by airborne droplets. Susceptibility to this disease is about 50-60% (that is, 50-60% of those who were in contact and who were not ill and not vaccinated get sick).
It can take 11 to 23 days from contact with a sick mumps to the onset of illness. nine0003
Mumps begins with an increase in body temperature up to 39 degrees C and severe pain in or under the ear, aggravated by swallowing or chewing. At the same time, salivation increases. Swelling quickly grows in the area of the upper part of the neck and cheeks, touching this place causes severe pain in the child. Unpleasant symptoms disappear within three to four days: body temperature decreases, swelling decreases, pain disappears.
However, quite often mumps ends inflammation in the glandular organs , such as the pancreas (pancreatitis), gonads. Past pancreatitis in some cases leads to diabetes mellitus . Inflammation of the gonads (testicles) is more common in boys. This significantly complicates the course of the disease, and in some cases may result in infertility. In especially severe cases, mumps can be complicated by viral meningitis (inflammation of the meninges), which is severe. nine0003
nine0003
After a disease, a strong immunity is formed, but complications can lead to disability.
The only reliable protection against the disease is vaccination against mumps, which is included in the National Immunization Schedule.
Parent's note.
Varicella (chickenpox) is a common childhood infection. Mostly young children or preschoolers are ill. Susceptibility to the causative agent of chickenpox (the virus that causes chickenpox refers to herpes viruses) is also quite high. About 80% of contact persons who have not been ill before develop chickenpox. nine0003
14 to 21 days pass from the moment of contact with a patient with chickenpox until the first signs of the disease appear.
The disease begins with a rash. Usually it is one or two reddish spots, similar to a mosquito bite. These elements of the rash can be located on any part of the body, but most often they first appear on the stomach or face. Usually the rash spreads very quickly - new elements appear every few minutes or hours. Reddish spots, which at first look like mosquito bites, the next day take the form of bubbles filled with transparent contents. These blisters are very itchy. The rash spreads throughout the body, to the limbs, to the scalp. In severe cases, there are elements of the rash on the mucous membranes - in the mouth, nose, on the conjunctiva of the sclera, genitals, intestines. By the end of the first day of the disease, the general state of health worsens, the body temperature rises (up to 40 degrees C and above). The severity of the condition depends on the number of lesions. If there are elements of the rash on the mucous membranes of the pharynx, nose and on the conjunctiva of the sclera, then pharyngitis, rhinitis and conjunctivitis develop due to the addition of a bacterial infection. Bubbles open in a day or two with the formation of sores, which are covered with crusts. Headache, feeling unwell, fever persist until new rashes appear.
Usually the rash spreads very quickly - new elements appear every few minutes or hours. Reddish spots, which at first look like mosquito bites, the next day take the form of bubbles filled with transparent contents. These blisters are very itchy. The rash spreads throughout the body, to the limbs, to the scalp. In severe cases, there are elements of the rash on the mucous membranes - in the mouth, nose, on the conjunctiva of the sclera, genitals, intestines. By the end of the first day of the disease, the general state of health worsens, the body temperature rises (up to 40 degrees C and above). The severity of the condition depends on the number of lesions. If there are elements of the rash on the mucous membranes of the pharynx, nose and on the conjunctiva of the sclera, then pharyngitis, rhinitis and conjunctivitis develop due to the addition of a bacterial infection. Bubbles open in a day or two with the formation of sores, which are covered with crusts. Headache, feeling unwell, fever persist until new rashes appear. This usually happens within 3 to 5 days. Within 5-7 days after the last sprinkling, the rash disappears. nine0003
This usually happens within 3 to 5 days. Within 5-7 days after the last sprinkling, the rash disappears. nine0003
Treatment of chickenpox is to reduce itching, intoxication and prevent bacterial complications. The elements of the rash must be lubricated with antiseptic solutions (as a rule, this is an aqueous solution of brilliant green or manganese). Treatment with coloring antiseptics prevents bacterial infection of rashes, allows you to track the dynamics of the appearance of rashes. It is necessary to monitor the hygiene of the mouth and nose, eyes - you can rinse your mouth with a solution of calendula, the mucous membranes of the nose and mouth also need to be treated with antiseptic solutions. nine0003
Complications of chickenpox include myocarditis - inflammation of the heart muscle, meningitis and meningoencephalitis (inflammation of the meninges, brain matter), inflammation of the kidneys (nephritis). Fortunately, these complications are quite rare. After chickenpox, as well as after all childhood infections, immunity develops. Re-infection happens, but very rarely.
After chickenpox, as well as after all childhood infections, immunity develops. Re-infection happens, but very rarely.
Reminder for parents.
Scarlet fever is the only childhood infection caused not by viruses but by bacteria (group A streptococcus). This is an acute disease transmitted by airborne droplets. Infection through household items (toys, dishes) is also possible. Children of early and preschool age are ill. The most dangerous in terms of infection are patients in the first two to three days of the disease. nine0003
Scarlet fever begins very acutely with fever up to 39 degrees C, vomiting, headache. The most characteristic symptom of scarlet fever is tonsillitis, in which the mucous membrane of the throat has a bright red color, swelling is pronounced. The patient notes a sharp pain when swallowing. There may be a whitish coating on the tongue and tonsils. The tongue subsequently acquires a very characteristic appearance ( “crimson ”) - bright pink and coarsely granular.
The tongue subsequently acquires a very characteristic appearance ( “crimson ”) - bright pink and coarsely granular.
By the end of the first beginning of the second day of illness, 9 appears0217 the second characteristic symptom of scarlet fever is a rash. It appears immediately on several parts of the body, most densely located in the folds (elbow, inguinal). Its distinguishing feature is that the bright red punctate scarlatinal rash is located on a red background, which gives the impression of a general confluent redness. When pressed against the skin, a white line remains . The rash may be spread over the entire body, but there is always a clean (white) area of skin between the upper lip and nose, and also the chin. Itching is much less pronounced than with chicken pox. nine0003 Rash lasts up to 2 to 5 days. The manifestations of sore throat persist a little longer (up to 7-9 days). Scarlet fever is usually treated with antibiotics , since the causative agent of scarlet fever is a microbe that can be eliminated with antibiotics and strict adherence to bed rest . Almost exclusively children suffer from scarlet fever because with age a person acquires resistance to streptococci. Those who have been ill also acquire strong immunity. Information for parents. Whooping cough is an acute infectious disease characterized by a long course. The hallmark of the disease is a spasmodic cough. The mechanism of transmission of infection is airborne. From the moment of contact with a whooping cough patient until the first signs of the disease appear, 3 to 15 days pass. Whooping cough feature is a gradual increase in cough within 2 to 3 weeks after its onset. Typical signs of whooping cough: Whooping cough is often complicated by bronchitis, otitis media, pneumonia, rectal prolapse, umbilical and inguinal hernias. After having had whooping cough for a long time (several months), coughing fits may return, especially if the child catches a cold or during physical exertion. nine0003 The only reliable prevention against whooping cough is vaccination with DTP, a vaccine that is included in the National Immunization Schedule. Parents' fears about the harmful effects of the vaccine are unfounded. The quality of the DTP vaccine is not inferior in its properties to vaccines produced in other countries. Memo for parents. Acute intestinal infections is a large group of diseases that occur with more or less similar symptoms, but can be caused by a huge number of pathogens: bacteria, viruses, protozoa. nine0003 In summer, the number of intestinal infections in children inevitably increases. Firstly, , in summer a large amount of raw vegetables, fruits and berries are consumed, on the unwashed surface of which a huge number of microbes, including potentially dangerous ones, live. Secondly, , children spend a lot of time outdoors in summer, and not always even their parents remember that eating with clean hands is a mandatory rule . The third reason : in the summer, getting into food (dairy products, meat, fish, broths), some pathogens multiply at a tremendous speed and quickly reach the amount that successfully breaks through the protective barriers of the gastrointestinal tract. From the moment the pathogen enters the gastrointestinal tract to the onset of the disease, it can take from several hours to 7 days. The disease begins with fever, malaise, weakness, lethargy. Appetite is sharply reduced, nausea, vomiting quickly joins. Also very important is the local treatment of angina and detoxification (removal of toxins from the body that are formed during the vital activity of microorganisms - for this they give plenty of drink). Vitamins, antipyretics are shown. Scarlet fever also has enough serious complications . Before the use of antibiotics, scarlet fever often resulted in the development of rheumatism with the formation of acquired heart defects or kidney disease. Currently, subject to well-prescribed treatment and careful adherence to recommendations, such complications are rare.
Also very important is the local treatment of angina and detoxification (removal of toxins from the body that are formed during the vital activity of microorganisms - for this they give plenty of drink). Vitamins, antipyretics are shown. Scarlet fever also has enough serious complications . Before the use of antibiotics, scarlet fever often resulted in the development of rheumatism with the formation of acquired heart defects or kidney disease. Currently, subject to well-prescribed treatment and careful adherence to recommendations, such complications are rare.  A feature of whooping cough is the high susceptibility of children to it, starting from the first days of life.
A feature of whooping cough is the high susceptibility of children to it, starting from the first days of life.

 There are several reasons for this.
There are several reasons for this.  The chair is liquid, frequent with impurities. The consequence of fluid loss is dryness of the mucous membranes and skin, facial features are sharpened, the child loses weight, urinates little. Painful facial expression. If your child has the above signs of illness, call the doctor immediately. nine0217 Self-medication is not allowed
The chair is liquid, frequent with impurities. The consequence of fluid loss is dryness of the mucous membranes and skin, facial features are sharpened, the child loses weight, urinates little. Painful facial expression. If your child has the above signs of illness, call the doctor immediately. nine0217 Self-medication is not allowed
Prevention of intestinal infections requires strict adherence to general hygiene measures in the home, when preparing food and during meals.
In the summer, all foodstuffs should be protected from flies. Ready food should be stored in the refrigerator: at a low temperature, even if microbes get into the food, they will not be able to multiply. The disease can also be caused by illegibility when buying products that are eaten without heat treatment - from the hands, outside the markets, where they do not pass sanitary control. When swimming in open water, in no case should water be swallowed. If you eat on the beach, wipe your hands with at least special wet wipes.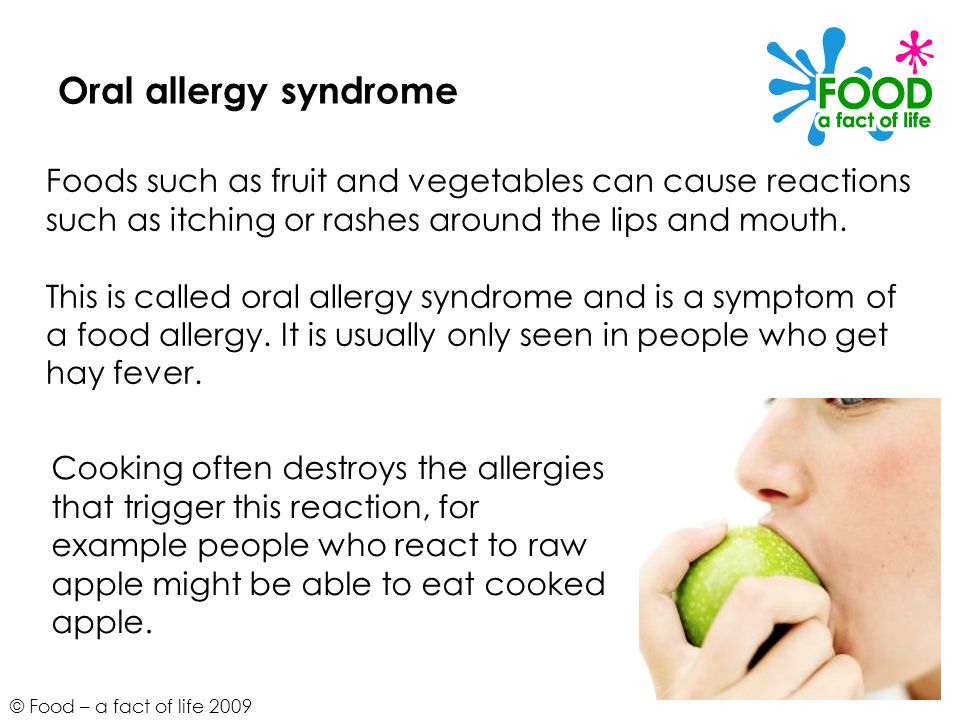 nine0003
nine0003
And remember that parental example is the best way to teach a child.
Parent Guide .
Tuberculosis is a chronic infectious disease caused by Mycobacterium human tuberculosis, affecting mostly the respiratory organs, as well as all organs and systems of the body.
The source of infection for is people with tuberculosis. The most common is the air way of infection. Transmission factors are nasopharyngeal mucus, sputum and dust containing bacteria. nine0003
Reproduction of tuberculosis bacteria in the child's body leads to significant functional disorders with symptoms of intoxication: irritability appears or, conversely, lethargy, fatigue, headache, sweating. With a long course of the disease, the child loses weight, the skin becomes pale, and there is a tendency to inflammatory diseases. For children, a reaction from the lymph nodes is typical: they increase in size, become dense.