Baby fussy after feeding formula
Infant Formula - familydoctor.org
Breast milk is the best source of nutrition for your baby. However, some women are unable to or choose not to breastfeed. In these cases, baby formulas are an option. Infant formulas are specially made to meet babies’ nutritional needs. If you plan to use formula, here are some important tips to make it work for you and your baby.
Path to improved health
Your family doctor will probably recommend a formula made from cow’s milk. Some formulas are iron fortified. This means they have extra iron in them. Some formulas have little or no iron at all. Most doctors recommend using an iron-fortified formula.
Some formulas are made from soy milk instead of cow’s milk. If your baby seems to be allergic to formula made from cow’s milk, your doctor may suggest using a soy milk formula.
If you’re not breastfeeding, use infant formula during the first year of your baby’s life. Regular cow’s milk and regular soy milk are not the same as infant formula made from cow’s milk or from soy milk. Regular cow’s milk and regular soy milk do not contain all the nutrients that your baby needs to grow and develop. Babies younger than one who drink regular cow’s milk or regular soy milk are at risk for problems associated with low iron.
How much infant formula
Your doctor will give you an idea of how much to feed your baby when you first start using formula. Most babies need 2.5 ounces of formula per pound of body weight each day. This means that an eight-pound baby may drink about 20 ounces of formula a day. However, this is just an estimate. It is important to pay attention to your baby’s cues. Other than crying, signs that your baby may be hungry include smacking their lips, sucking and rooting (turning their head toward your hand when you touch their face).
Feed your baby as often as they want to be fed. It could be more in the beginning. This may be 8 to 12 times a day. Your baby may want to be fed less often as they grow and can take more formula at each feeding. How often your baby wants to eat will change as they go through growth spurts. Growth spurts typically occur at about 2 and 6 weeks of age. It can happen again at about 3 and 6 months of age.
How often your baby wants to eat will change as they go through growth spurts. Growth spurts typically occur at about 2 and 6 weeks of age. It can happen again at about 3 and 6 months of age.
Your baby is probably getting enough formula if they:
- Act satisfied after each feeding
- Gain weight regularly after the first 3 to 7 days following birth (Your baby may lose a little weight during the first week after being born.)
- Have about 6 to 8 wet diapers a day
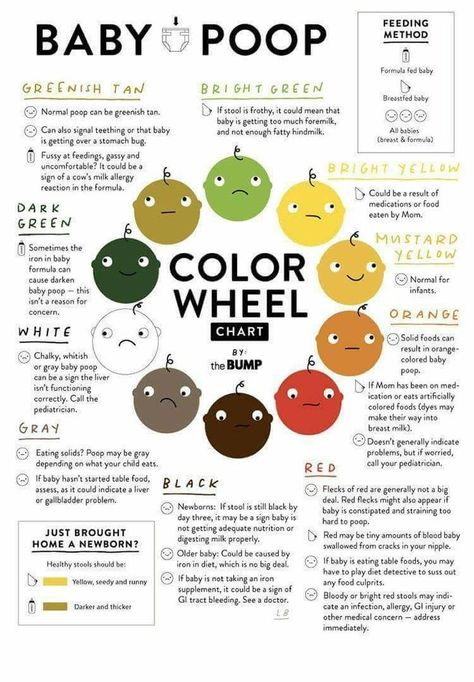
- Have about 2 to 5 or more stools a day at first (This will fall to 2 or fewer stools a day as your baby grows. Your baby’s stools will be runny when you start formula.)
Baby formula is sold in several forms:
- Ready-to-use:This is the most expensive kind of formula, but no mixing is necessary.
- Concentrated liquid:This is a less expensive formula. You mix the liquid formula with an equal part of water.
- Powder:This is the least expensive formula.
 You mix one level scoop of powdered formula with two ounces of water and stir well.
You mix one level scoop of powdered formula with two ounces of water and stir well.
Most times, you can feed your baby a bottle without warming it first. It is okay for the formula to be cool or room temperature. If your baby seems to prefer warm formula, you can put the filled bottle in a container of warm water and let it stand for a few minutes. Test the warmth of the formula by putting a few drops on your wrist before giving the bottle to your baby.
Things to consider
The most important thing to know when giving your baby formula is to follow the directions on the formula container. Measure carefully and never add extra water to the formula. You also should wash your hands before preparing the formula.
If you use well water or if there are problems with the water in your town, boil the water first. You also can use bottled water. If you boil the water, let it cool off before mixing it with the formula. Always use a clean cup to measure the water.
Sometimes it may be necessary to change the kind of formula you give your baby. If your baby is always fussy, needs more iron, or has certain food allergies, your doctor may suggest changing your baby’s formula to a different kind. Some of the signs that your baby is intolerant to the type of formula you’re feeding them are:
If your baby is always fussy, needs more iron, or has certain food allergies, your doctor may suggest changing your baby’s formula to a different kind. Some of the signs that your baby is intolerant to the type of formula you’re feeding them are:
- Excessive crying or fussiness after a feeding
- Extra gas
- Very loose, watery stools (This is not always related to formulas. If you are concerned about your baby’s stool habits, the color, or consistency, talk with your doctor before changing your baby’s formula.)
- Dry, red, and scaly skin
- Extreme fatigue or weakness
- Forceful vomiting
Never give your baby hot formula. Check the temperature of the formula by placing a few drops on your skin to be sure it isn’t too hot before feeding it to your baby. The formula should only be lukewarm. Never heat bottles in the microwave. Microwaves heat foods and liquids unevenly. This can cause hot spots in the formula that can burn your baby.
Sterilize (clean) bottles and nipples before you use them for the first time. You can do this by putting them in boiling water for five minutes. After that first time, you probably don’t need to sterilize them again. Instead, wash bottles, nipples and caps in hot, soapy water. Rinse them carefully to remove any soap residue. You can also run them through the dishwasher, which kills more germs than washing by hand.
You can do this by putting them in boiling water for five minutes. After that first time, you probably don’t need to sterilize them again. Instead, wash bottles, nipples and caps in hot, soapy water. Rinse them carefully to remove any soap residue. You can also run them through the dishwasher, which kills more germs than washing by hand.
Questions to ask your doctor
- How long should I try to breastfeed before starting formula?
- Can formula help minimize food and other allergies?
- Should I be concerned about formula recalls?
- Is it okay to give my child formula after the age of 1?
Resources
Centers for Disease Control and Prevention: How Much and How Often to Feed Infant Formula
U.S. Food & Drug Administration: Questions & Answers for Consumers Concerning Infant Formula
U.S. National Library of Medicine, Medline Plus: Infant Formulas Overview
Copyright © American Academy of Family Physicians
This information provides a general overview and may not apply to everyone. Talk to your family doctor to find out if this information applies to you and to get more information on this subject.
Talk to your family doctor to find out if this information applies to you and to get more information on this subject.
Baby Cries After Feeding: What Should I Do?
Medically reviewed by Karen Gill, M.D. — By Chaunie Brusie on October 3, 2018
My daughter, the “crier”
My second daughter was what my oldest fondly referred to as a “crier.” Or, in other words, she cried. A lot. The crying with my baby girl seemed to intensify after every single feeding and particularly at night.
It was those hellish hours between darkness and dawn when my husband and I would take turns walking around the house with her in our arms, praying and, mostly in my case, sobbing because we couldn’t console our baby.
I didn’t know it then in my sleep-deprived state, but my daughter’s crying after feedings wasn’t that uncommon. In combination with her frequent spitting up, it was pretty much a classic textbook case of colic.
Colic
Colic, in technical terms, simply means a “crying, fussy baby that doctors can’t figure out. ”
”
OK, so that’s not really the definition, but in essence, that’s what it boils down to. The British Medical Journal (BMJ) lists one criterion for colic: A baby that cries for at least three hours a day, three or more days a week, and is under 3 months old. Check, check, and check.
There isn’t one single known cause of colic. Even the actual clinical incidence of colic, estimated by BMJ to be around 20 percent of all babies, can be tricky.
Acid reflux
One of those causes of crying after feeding and spitting up in babies is actually acid reflux. This condition is known as gastroesophageal reflux disease (GERD) if it also causes significant symptoms such as poor weight gain.
When my “crier” daughter was 5, she frequently complained of her stomach hurting and as a result, had to undergo a series of testing with a gastroenterologist, a doctor that specializes in the GI system.
At our first appointment, the very first question he asked me was if she had colic as a baby and if she spit up a lot, to both of which I practically shouted, “Yes! How did you know?!”
He explained that acid reflux or GERD can manifest as symptoms similar to colic in babies, stomach pain in school-aged children, and later as actual heartburn pain in adolescents.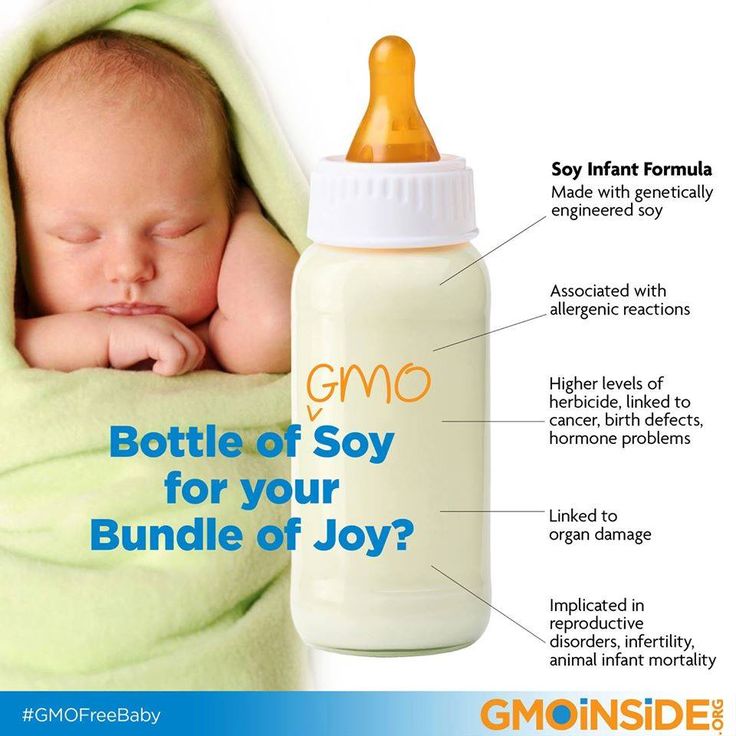
While many infants spit up, fewer have actual GERD, which can be caused by an underdeveloped flap between the esophagus and stomach or a higher-than-normal production of stomach acid.
In most cases, a diagnosis of infant reflux is simply based on your baby’s symptoms. If your doctor suspects a severe case however, there are several different tests that actually diagnose infant reflux.
Testing can involve taking a biopsy of your baby’s intestine or using a special type of X-ray to visualize any affected areas of obstruction.
Food sensitivities and allergies
Some babies, especially breastfed babies, may be allergic to certain food particles that their mothers are eating.
The Academy of Breastfeeding Medicine notes that the most common offender is cow’s milk protein in the mother’s milk, but even a true allergy is very rare. Only about 0.5 to 1 percent of exclusively breastfed babies are thought to be allergic to cow’s milk protein.
The other most common culprits, according to the ABM, are egg, corn, and soy, in that order.
If your baby is displaying symptoms of extreme irritability after feedings and has other symptoms, such as bloody stools (poop), you should speak with your healthcare provider about getting them tested for allergies.
Aside from a true allergy, there’s also been some evidence that following a low allergen diet while breastfeeding (essentially avoiding those top allergy foods, such as dairy, eggs, and corn) may be beneficial for infants with colic.
Strict elimination diets can have their own risks, so speak with your doctor before significantly changing your diet.
In our situation, I found that dairy, caffeine, and certain seeded fruit exacerbated my daughter’s crying and spitting up. By eliminating those foods and substances from my diet, I was able to help lessen her discomfort.
If you have a baby with colic, you might want to try anything at all to help ease your baby’s crying. If you’re curious to see if your diet has any effect, you can start by logging your food in a food journal and writing down your baby’s reactions after each meal.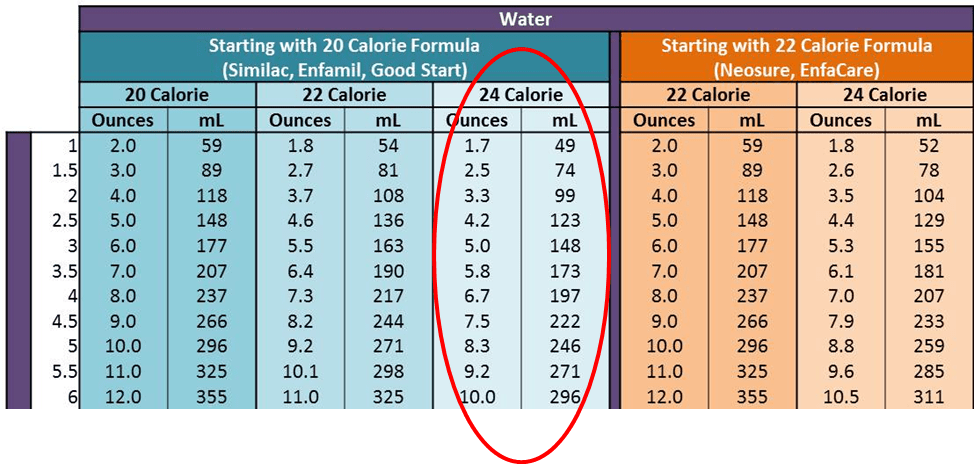
Next, you can eliminate one food at a time and see if reducing your intake of certain foods seems to make a difference in your baby’s behavior. If you hit on one you feel helps your baby to cry less, this does not mean they will not be able to eat that food in the future.
Just be sure to keep in mind that a true allergy is rare. Also, be sure to monitor for any additional symptoms, such as blood in your baby’s poop.
Gas
If your baby is crying a lot after every feeding, it may simply be a buildup of air swallowed while eating. It’s thought that bottle-fed babes in particular may be more prone to swallowing a lot of air during a feeding. This can trap gas in their stomachs and be uncomfortable.
In general, breastfed babies swallow less air while eating simply due to the way they eat. But every baby is different and even breastfed babies may need to be burped after a feeding.
Trying keeping your baby upright after a feeding and burping gently from the bottom of their back and up through the shoulders to work the gas bubbles up and out. Also check out this illustrated guide to burping a sleeping baby.
Also check out this illustrated guide to burping a sleeping baby.
Formula
If your baby is formula-fed, swapping out the formula you use may be a simple solution to a crying baby after feedings. Every formula is a little bit different and certain brands make formulas for more sensitive baby tummies.
If you decide to try this, talk to your baby’s pediatrician about whether an elemental formula would be a good choice to try for a week. If you try one different brand and you see no change in your baby’s fussiness, continuing to try different brands is unlikely to help.
Takeaway
Colic, along with a few other common conditions, might be the culprit if you too have a “crier” on your hands.
If your baby doesn’t find relief after dietary changes or additional burping, then make an appointment to see their doctor.
Share on Pinterest
Chaunie Brusie, BSN, is a registered nurse with experience in labor and delivery, critical care, and long-term care nursing. She lives in Michigan with her husband and four young children, and is the author of the book “Tiny Blue Lines.”
She lives in Michigan with her husband and four young children, and is the author of the book “Tiny Blue Lines.”
Last medically reviewed on October 3, 2018
- Parenthood
- Baby
- 06 Months
How we reviewed this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- ABM clinical protocol #24: Allergic proctocolitis in the exclusively breastfed infant. (2011). DOI:
10.1089/bfm.2011.9977 - Harrel MC, et al. (2015). Is there a correlation between maternal diet in breastfeeding mothers and infantile colic? DOI:
10.1097/01.EBP.0000541032.94135.ca - Mayo Clinic Staff. (2018). Infant reflux.
mayoclinic. org/diseases-conditions/infant-acid-reflux/diagnosis-treatment/drc-20351412
org/diseases-conditions/infant-acid-reflux/diagnosis-treatment/drc-20351412 - Rosen LD, et al. (2007). Complementary, holistic, and integrative medicine.
pedsinreview.aappublications.org/content/28/10/381 - Saavedra MA, et al. (2003). Infantile colic incidence and associated risk factors: A cohort study. .
ncbi.nlm.nih.gov/pubmed/14502331 - Sung V, et al. (2014). Treating infant colic with the probiotic Lactobacillus reuteri: Double blind, placebo controlled randomised trial. DOI:
10.1136/bmj.g2107 - Symptoms & causes of GER and GERD in infants. (2015).
niddk.nih.gov/health-information/digestive-diseases/acid-reflux-ger-gerd-infants/symptoms-causes
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Current Version
Oct 3, 2018
Written By
Chaunie Brusie
Edited By
Nizam Khan (TechSpace)
Medically Reviewed By
Karen Richardson Gill, MD
Share this article
why the baby cries while feeding
While the baby is quite a baby, crying is the only way of his communication with his mother and the outside world. If the baby is restless during feeding, he will let you know that he is uncomfortable. We will analyze what can cause baby crying in such a situation.
If the baby is restless during feeding, he will let you know that he is uncomfortable. We will analyze what can cause baby crying in such a situation.
Dry milk drink "Baby milk" Valio Baby 3 NutriValio for feeding children over 12 months Read more
As a rule, the causes of a baby’s tears at the breast or bottle with a mixture are physiological, and there may be several of them.
Abdominal pain
Most likely, the child is worried about colic (they can start from 2-4 weeks of age and usually end by 3 months). Unpleasant sensations are associated with the fact that the infant has an insufficiently developed intestinal microflora and it is difficult for the digestive system to cope with the task assigned to it. Children's crying during colic is accompanied by arching the back and pulling the legs to the stomach - the pain from the formation of gases in the intestines is always acute. To alleviate the condition of the crumbs, it is useful for a nursing mother to drink teas with fennel, cumin or anise. If your baby is formula-fed, choose formula carefully. Valio Baby baby food is as close as possible to the composition of breast milk and contains the GOS prebiotic, which is necessary for the health of the child's digestive system. The cause of colic is also the wrong feeding technique and, as a result, the capture of excess air by the baby.
To alleviate the condition of the crumbs, it is useful for a nursing mother to drink teas with fennel, cumin or anise. If your baby is formula-fed, choose formula carefully. Valio Baby baby food is as close as possible to the composition of breast milk and contains the GOS prebiotic, which is necessary for the health of the child's digestive system. The cause of colic is also the wrong feeding technique and, as a result, the capture of excess air by the baby.
#PROMO_BLOCK#
Earache
Children under one year old often suffer from otitis media, this is due to the anatomical features of the structure of the nasopharynx in babies in the first months of life. A baby may cry during feeding because swallowing causes a sharp pain in his ears. Very carefully touch the tragus of the baby's auricles - if he cries, then you need to see a doctor.
Headache
It is no secret that many neurological disorders are accompanied by headaches. It becomes especially strong when swallowing. If the baby is constantly crying during feeding, be sure to make an appointment with a pediatric neurologist.
It becomes especially strong when swallowing. If the baby is constantly crying during feeding, be sure to make an appointment with a pediatric neurologist.
Inflammation of the oral mucosa
Crying during feeding may signal that the baby is experiencing discomfort in the mouth or throat. Its cause is most often thrush or pharyngitis. These diseases require treatment under the supervision of a pediatrician.
Lack or excess of breast milk
The lactation of a nursing woman is affected by a considerable number of factors - the psychological state, fatigue, stress, malnutrition and its lack, improper organization of breastfeeding. The baby may cry because he does not have enough milk. Whether the food shortage is really critical is easy to check using the wet diaper method. By the way, the crying of a baby may also indicate that there is too much milk - the stream is too strong and the baby simply chokes.
Unusual taste of breast milk
If a mother ate, for example, something spicy on the eve of feeding, this will certainly affect the taste of milk. The baby, of course, will cry. This cause of children's "grief" is the most easily eliminated - be attentive to your menu and do not upset your beloved baby.
The baby, of course, will cry. This cause of children's "grief" is the most easily eliminated - be attentive to your menu and do not upset your beloved baby.
In addition to the reasons described, the reason for children's tears during feeding can be erupting teeth and inflammation of the gums, as well as nasal congestion with allergies and SARS. Be attentive to your baby. If all is well, the baby should not cry while feeding.
3.4 35
Power supplyShare:
Oksana Ivargizova
Medical Institute. Pavlova, specialization - pediatrics
Author: Reetta Tikanmäki
Palm oil in baby food
Infant milk formulas are made from cow's milk. However, in terms of fat composition, it differs significantly from that of the mother.
However, in terms of fat composition, it differs significantly from that of the mother.
Read
Author: Ivargizova Oksana
How to choose milk formula for a baby
Breast milk is the best food for a newborn baby. It contains all the necessary nutritional components that fully meet the needs of the child and are necessary for his healthy and harmonious development.
Read
Show all
Why does a baby cry - an article in the newspaper of the EMS Clinic Na Zdorovye
— The easiest answer to the question about sedatives is definitely: no. Parents should not use painkillers, sedatives, herbal “bye-bye”-fees and other means to calm the baby. In any case, until it was recommended by a neurologist after a comprehensive examination. Giving a sedative to an infant is like hiding your head under a pillow when the alarm goes off: it won't stop time and you'll be late for work anyway.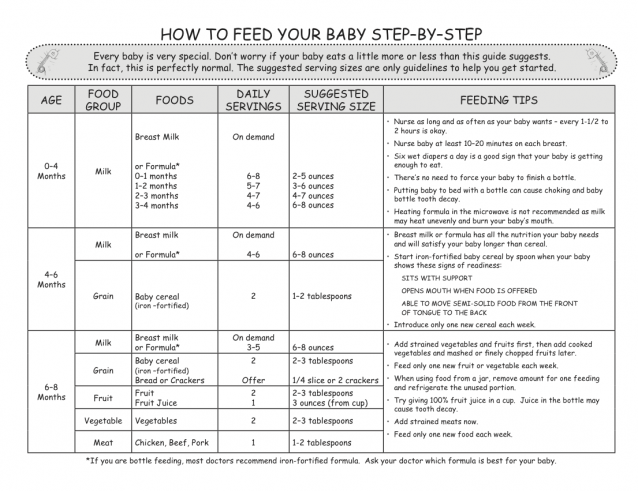 You need to try to understand your baby, make sure that his most basic needs are met, and only then proceed to the exclusion of more complex and rare problems.
You need to try to understand your baby, make sure that his most basic needs are met, and only then proceed to the exclusion of more complex and rare problems.
Try to remain calm and act only in the interests of the child
Up to three weeks of age, the most common cause of constant crying of a child is banal malnutrition. A common mistake of parents is the desire to stick to the schedule when breastfeeding in the first month of a child's life. A baby can suck out 150 ml of milk in three minutes, or maybe 20 ml in an hour, and a nursing mother is not able to understand how much has been eaten by the sensations of "emptying the breast". With free feeding in the first month, record the dynamics of the baby's weight gain. When feeding on a schedule, conduct a series of control feedings with measurement of body weight before and after feeding, so you can make sure that the amount of one feeding is sufficient. If the baby's crying stops instantly as soon as you give the breast, this is absolutely normal.
What to do if the baby cries even after you have changed the diaper, tried to feed, picked up? If this happens often and the mother does not succeed in calming the child for more than an hour, you should consult a doctor. It is not always obvious to parents, especially good ones, in what order to seek medical help: should I call an ambulance or go to see my pediatrician in a couple of days, or maybe it’s better to grab the child and the CHI policy and rush to the nearest city hospital? Try to remain calm and act only in the interests of the child. Here are some tips to help you.
- If the baby is crying and cannot be calmed for more than two hours, call emergency services. Pre-measure the baby's temperature, check for rashes on the baby's body, and remember if there was a stool within the last 12 hours. Also make sure you have enough breast milk for a single feed. Report this information to the emergency services
- If a child often worries , sleep is short, but there is no monotonous crying-crying for more than two hours, then this can be dealt with on your own, and then with the help of a doctor at a clinic appointment or by calling him at home.
 The better prepared you are for your consultation, the more productive it will be. Things to do before the consultation:
The better prepared you are for your consultation, the more productive it will be. Things to do before the consultation:
- Determine breastfeeding volume by three to four checkweighs before and after feeding
- See if there is a connection between baby crying and feeding. When does the child worry and cry - immediately after eating, during feeding, an hour later, etc.?
- Recall the circumstances in which anxiety and frequent crying appeared: vaccination, errors in the mother's diet, starting to use or changing formula?
- Note accompanying symptoms and their relationship to crying: regurgitation, constipation, frequent stools, flatulence, appearance or increase of skin rash
- Assess the change in stool frequency and consistency
- Observe if restlessness and crying persist after stool or flatulence
- Find out if there is an effect when placing a gas tube or a glycerin suppository.
The task of a pediatrician when complaining of frequent and prolonged crying of a child is to determine why the child is crying, whether he has any disorders (including digestive disorders) and what kind they are - functional, that is, this is a conditionally normal condition associated with the growth and development of the body or a reaction to changes in external (primarily nutritional) factors, or it is a pathology that must be suspected, diagnosed and treated.