Baby goes stiff when feeding
Hypertonia in babies: What to do if your baby stiffens their body
Babies sometimes stiffen their legs and arms or tighten up their body when you pick them up or they get excited or frustrated. Often this type of stiffening is no big deal.
Children might also stiffen up their bottoms when they're having a bowel movement, especially if the stool is hard. And colic can make babies pull in and tighten their arms and legs, tense their abdomen, and clench their fists.
Your baby may also be discovering new ways to use their muscles. Some older babies stiffen up to resist doing something they dislike, such as getting a diaper change or being put into their car seat.
All of these situations are perfectly normal. But in other cases, a baby stiffening their body or arms and legs can indicate a problem.
What is hypertonia?
Hypertonia is a condition that makes a baby's muscles stiff and hard to move. It happens because of damage to areas of the brain and spinal cord that control muscle movements.
While babies need to contract their muscles to move their bodies and sit upright, muscles that are continually contracted are less flexible. Often hypertonia affects a baby's arm, leg, and neck muscles.
Children with hypertonia move in different ways because they often have a limited range of motion at their joints. They may have trouble walking, balancing, and letting go of objects they've grabbed.
There are two types of hypertonia:
- Spastic hypertonia is muscle spasms and exaggerated reflexes that increase when a baby moves.
- Dystonic hypertonia is when muscle tone stays the same whether the baby is moving or still.
Advertisement | page continues below
Doctors will move a baby's arms and legs in different directions at various speeds to figure out which type of hypertonia they have.
Symptoms of hypertonia in babies
Muscle stiffness is the main symptom of hypertonia. Where that stiffness occurs and how severe it is can vary based on the cause.
In general, a child with hypertonia might:
- Have trouble moving their joints, especially joints in the arms, legs, or neck
- Have less range of motion
- Lose their balance and fall often
- Feel pain or soreness in their muscles
- Jerk or twitch their arms or legs
In severe hypertonia, the joint can freeze in place. Doctors call this a contracture. Babies with contractures may not be able to move the affected body part much, or at all.
Causes of hypertonia in babies
When a baby wants to move, signals from their nervous system (brain and spinal cord) travel to their nerves, which direct their muscles to contract or relax. An injury to the brain or spinal cord can prevent those signals from reaching the nerves.
In hypertonia, the baby's muscles don't get the signal to relax. They stay contracted.
Possible causes of hypertonia in babies include:
- A lack of oxygen during birth
- Head injury
- Brain tumor
- Exposure to a chemical that affects the brain
- Problems that happened when the brain developed in the womb
Other reasons why your baby may stiffen their body
Hypertonia isn't the only possible reason for a baby to stiffen their body. A few other medical conditions also cause this symptom.
A few other medical conditions also cause this symptom.
Infantile spasm. These rare seizures look like a sudden stiffening of the baby's arms, legs, or head, which may also jut forward. Infantile spasms often start when a baby is 4 to 7 months old. Each spasm lasts just a second or two, and babies can have up to 100 of them per day. Treatment with medication is important to prevent serious complications like epilepsy, developmental delay, and intellectual disability.
Cerebral palsy. This group of brain disorders affects a baby's muscle control. Cerebral palsy has a few types. Some cause uncontrollable movements. Others lead to poor balance. The most common type is spastic cerebral palsy, which causes muscle stiffness.
Seizures and epilepsy. Epilepsy is a brain disorder in which nerve cells fire in an abnormal pattern, leading to seizures. During a seizure, a baby's arms and legs might jerk, twitch, or stiffen. An electroencephalogram and other tests can help your doctor determine whether your baby is having seizures.
When to call the doctor if your baby stiffens their body
The occasional stiffening of an arm or leg probably isn't anything to worry about. But if it happens often, you'll want to seek help.
Whenever you have a question or concern about your baby's development, it's wise to call the doctor. In the unlikely event that stiffness does signal a condition like cerebral palsy or epilepsy, getting it checked out can start you on the path to a diagnosis and treatment.
Babies have lots of strange behaviors that can look concerning but are normal, like throwing themselves backward when they're upset. But if your child does have a problem or developmental delay, you'll want to get help and support ASAP.
High Muscle Tone - Breastfeeding Support
If a baby has high muscle tone (hypertonia) you may notice he seems to arch his back and hold himself very stiffly. A baby with this type of muscle tension may need to work harder at breastfeeding and expend more energy. You might find he is quite fussy at the breast and breastfeeding isn’t very comfortable for you, with no obvious explanation. This article discusses how high muscle tone can affect breastfeeding and shares ideas that may help a tense baby to relax and breastfeed more comfortably.
You might find he is quite fussy at the breast and breastfeeding isn’t very comfortable for you, with no obvious explanation. This article discusses how high muscle tone can affect breastfeeding and shares ideas that may help a tense baby to relax and breastfeed more comfortably.
Find an IBCLC
Search for a breastfeeding expert near you
What causes high muscle tone in babies?
The position of a baby in the uterus, invasive birthing practices, pain or neurological disorders can all affect muscle tone. Babies who are very hungry can also have high muscle tone, including newborn babies or older babies who are very underweight. Contact your health professional for further information if you have any concerns. This article is not intended to be a substitute for advice from your health professionals.
High muscle tone and breastfeeding
Feeding difficulties that may be explained by high muscle tone and are described in Breastfeeding Answers Made Simple, 2010 include:
- A tight jaw—baby may be unable to open his mouth wide enough to take the breast properly.
- Clamping—baby may clamp down on the breast.
- Restricted tongue movements causing bunching, humping or retraction of the tongue.
- A tendency for baby to gag during feeding.
- Feeding pain and nipple damage for the breastfeeding mother
Feeding difficulties such as these can also have other causes however, for example an underweight or hungry baby may demonstrate body tension that can include tongue retraction. Or a baby may clamp down on the breast if they are struggling with a fast flow of milk or are in a shallow latch (the way baby attaches to the breast). In order to rule out positioning, latch or low weight gain as causes of either painful feeds or body tension/high muscle tone in your baby, include a lactation consultant in your health care team to ensure all aspects of breastfeeding are fully assessed.
Ideas to help with muscle relaxation
If your baby still seems tense once hunger or a poor latch have been ruled out, ideas that can help with muscle relaxation include:
- Skin-to-skin contact for several hours each day.

- A quiet environment so as not to over stimulate your baby.
- Swinging your baby in a blanket to calm him. Lie baby on a blanket or sheet, then using two adults hold the ends of the blanket and gently swing baby from side to side 1.
- Supervised tummy time—tummy time on a parent is most comfortable for a young baby e.g. with the mother leaning back in a reclining or laid back position. See the link from The American Occupational Therapy Association (AOTA) for safety guidance and precautions for tummy time.
- Physical therapy or cranial work may be helpful—see Does Cranial Therapy Work? or Cranial Osteopathy or Craniosacral Therapy for my Baby.
Specific ideas to help breastfeeding
- Skin-to-skin contact before a breastfeed.

- Try laid back or natural positions for breastfeeding. Lie your baby on his tummy (prone) on your abdomen to help to reduce his body extension and encourage his tongue to relax forward with the help of gravity. Conversely rugby hold may be helpful for some babies.
- Use the colic hold before a feed. Drape your baby over your forearm with their tummy facing down and their arms hanging freely, see picture.
- In some situations a well fitted nipple shield can be used as a suck training tool.
- Try the charm hold before a breastfeed, this is a variation of the colic hold (see sub-heading below) and is particularly useful for babies who are not extending their tongues.
- Finger-feeding—either with baby in a tummy down (prone) position or with your baby held in the crook of your arm can be used as a training exercise before a breastfeed, see What is Finger Feeding? for further information.
The Charm Hold
The charm hold is a version of the colic hold where the baby also sucks a parent’s clean finger in a tummy down position. This can also be used as a position for a finger feeding exercise as above. Baby can be lying on a parent’s lap as in the description below:
Excerpt from
Helping a Mother with a Baby Who Is Reluctant to Nurse, Leaven, LLLI, 1999
Lay the baby across his parent’s lap face down toward the floor with his hips flexed (bent). The parent supports the baby’s forehead with the heel of the hand and extends a clean index finger with smoothly trimmed fingernail for the baby to suck until the tight tongue relaxes and comes forward to snuggle around the finger. It may take several minutes for this to happen. It is called the Charm hold because it “works like a charm.” As soon as the baby’s tongue relaxes, he can be gently turned right-side-up and immediately offered the breast.
Alternatively the baby could be supported tummy down, astride a parents arm as in the colic hold. If baby’s chest is supported by the parent’s hand, rather than their elbow, the free hand can reach baby’s mouth for suck training with the heel of the hand supporting baby’s forehead2.
If baby’s chest is supported by the parent’s hand, rather than their elbow, the free hand can reach baby’s mouth for suck training with the heel of the hand supporting baby’s forehead2.
High muscle tone due to food allergy (or pain)
In her book Breastfeeding Works! Even With Allergies, Robyn Noble describes how food allergy related gut pain (or other causes of infant pain) can cause problems breastfeeding. Some babies may seem to be unable to latch or have sucking problems, or be very fussy and restless at the breast resisting the usual breastfeeding holds. When they are in pain, babies can hold a lot of tension in their jaw and clamp down on the breast causing painful sore or damaged nipples, creasing of the nipples and repeated cases of mastitis. Noble calls this the hypertonic bite response and says it can explain nipple damage even when outwardly the baby seems well latched. The author’s tips to help manage hypertonic bite response due to food allergy or intolerance include:
Noble calls this the hypertonic bite response and says it can explain nipple damage even when outwardly the baby seems well latched. The author’s tips to help manage hypertonic bite response due to food allergy or intolerance include:
- Hold the breast firmly during a breastfeed to push more breast tissue towards the baby’s top lip
- Work to resolve baby’s pain through an exclusion diet for the breastfeeding mother (cows’ milk products are a common culprit)
For more information on food allergies and intolerances and how they could affect a breastfed baby see Milk Allergy in Babies and the book Breastfeeding Works! Even With Allergies by Robyn Noble (2015).
Infant torticollis
If your baby has more difficulty turning his head to one side than to the other, or holds his head to one side and prefers feeding in certain breastfeeding positions, he may have torticollis i.e. one of the muscles in the neck is very tight on one side3.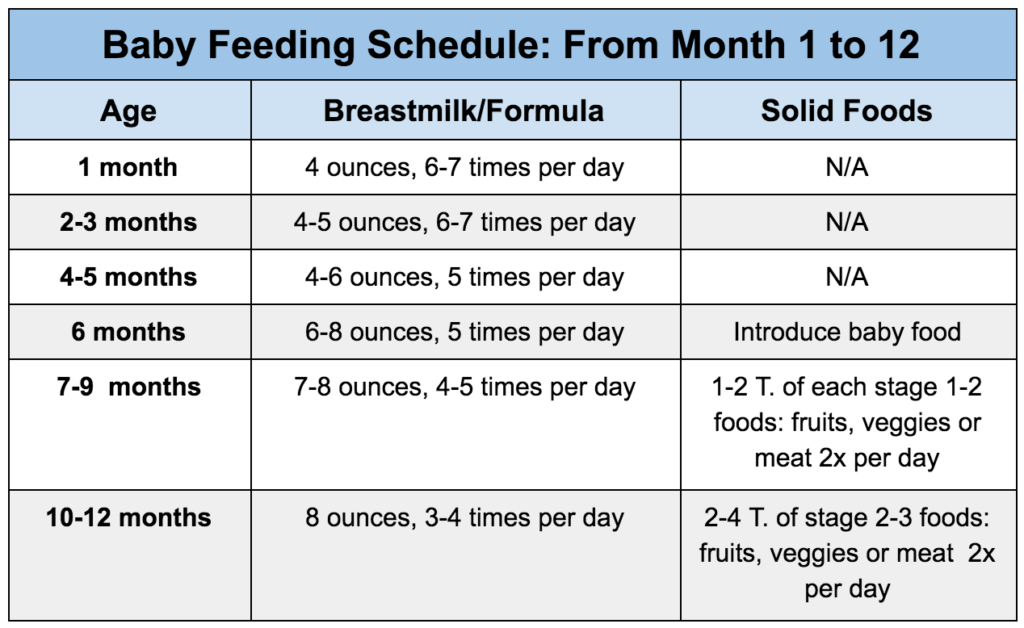 This may have been caused by your baby’s positioning in the womb or after a traumatic birth and can be diagnosed by your health care professional.
This may have been caused by your baby’s positioning in the womb or after a traumatic birth and can be diagnosed by your health care professional.
Alison Hazelbaker has recorded a presentation on the ways torticollis can affect breastfeeding.
Recorded Webinar
Infant Torticollis: A New Threat to Lactation, ILCA Webinar, Alison K. Hazelbaker, PhD, IBCLC, FILCA, CST, RCST
Hazelbaker indicates that torticollis may cause specific behaviours during a breastfeed including: jaw clenching, arm cycling, nipple compression, Vasospasm Symptoms including blanching or a white stripe on the nipple, exquisite pain, irritation to nerves, difficulty latching on one side, a shallow latch, retracted tongue, and the baby’s head may keep turning away from the breast. Hazelbaker notes that excess use of any kind of rigid seat or car seat can make the symptoms worse and that tummy time or physical therapy can be helpful. There is further helpful information in the presentation.
Tongue exercises for high muscle tone?
For further information on suck training or tongue exercises see your breastfeeding specialist or refer to Chapter 12 “Neurological Issues and Breastfeeding” in Supporting Sucking Skills In Breastfeeding Infants 2017 by Cathy Watson-Genna. The chapter includes:
The chapter includes:
- Tongue exercises that may help with high muscle tone
- How to relax a tight jaw
- The value of finger feeding for some situations
Contacting your health professional and IBCLC lactation consultant will help you identify whether any of these exercises are appropriate in your situation. Tongue exercises are best shown by someone familiar with their use and application. It may be that trying different breastfeeding positions for your newborn or some different latching tips are all that are needed.
Tongue-tie?
Some symptoms such as not being able to open the jaw very wide, having a heightened gag reflex or pinching the nipple during breastfeeding can also be caused by poor tongue function due to a tight, short frenulum. You can check your baby’s tongue function with your IBCLC lactation consultant or tongue-te practitioner and see Is My Baby Tongue-Tied?
There are several ways to help relax a baby who has high muscle tone and there are specific exercises and techniques that can help a tense baby breastfeed.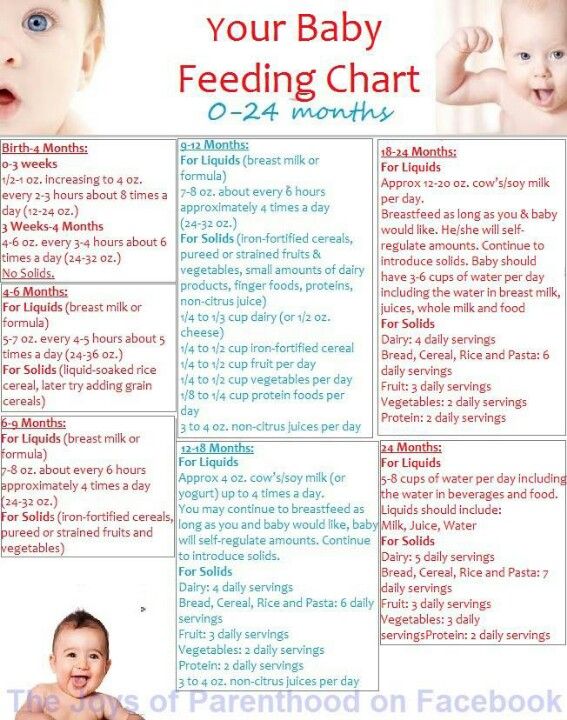 Babies who are underweight or in pain can also be tense, so it is important to rule out hunger or a physical pain as a cause of high muscle tone. Your health professional team will help you if you have any concerns that your baby has high muscle tone and your IBCLC lactation consultant will be a valuable member of the team if positioning, latch or low weight gain are causes of your baby’s body tension.
Babies who are underweight or in pain can also be tense, so it is important to rule out hunger or a physical pain as a cause of high muscle tone. Your health professional team will help you if you have any concerns that your baby has high muscle tone and your IBCLC lactation consultant will be a valuable member of the team if positioning, latch or low weight gain are causes of your baby’s body tension.
Footnotes & References
-
Breastfeeding Answers Made Simple, 2010, p.307
-
Cathy Watson-Genna, Supporting Sucking Skills In Breastfeeding Infants, 3e, 2017
-
For more information see Torticollis and Preferential Head Turn from Southampton NHS Foundation Trust
"Here and now" in contact between mother and child //Psychological newspaper
I would like to share a little experience of psychotherapy with several young mothers who have recently given birth to their first child and are faced with the problems and complexities of their new situation.
The events described refer to that recent time, when the consultation of a psychologist and work with a psychotherapist seemed to many to be something unusual and exotic. A more familiar and traditionally safe way to solve their problems was to discuss with friends, acquaintances, more experienced mothers. nine0003
It is hardly possible to imagine anything more in keeping with complete good contact than the interaction between mother and infant. All possible sides are included in the communication process: the child feels the mother and responds to her with his whole body, voice. Their relationship is direct, they are addressed to the very depths of each person's personality, this is a real meeting of two personalities, two "I". Feeding, feeding a child is an ideal situation for deep, genuine contact, knowledge of each other. But in reality...
A woman who decides to have a baby today is quite realistically threatened to be buried under a mountain of various problems: find, buy the necessary things, feed, heal, teach, educate - in short, become everything for her child. In very few cases, a woman manages to share her responsibility for the child with someone else (her mother, husband, doctor, teacher, etc.). Usually new requirements are added by other people. The doctor, visiting a sick child, asks the question: “Why are you treating him so badly?” The teacher, dissatisfied with the success of the child, may ask: “Why are you teaching him so badly?” nine0003
In very few cases, a woman manages to share her responsibility for the child with someone else (her mother, husband, doctor, teacher, etc.). Usually new requirements are added by other people. The doctor, visiting a sick child, asks the question: “Why are you treating him so badly?” The teacher, dissatisfied with the success of the child, may ask: “Why are you teaching him so badly?” nine0003
In such a situation, the mother takes full responsibility for the future of the child, his health, his success, his character. She tries to fulfill all her duties, to provide the best opportunities for her unborn child, and deprives herself of the opportunity to be "here and now" with the child. She is in "his future", with his tomorrow's problems, and, for example, even when she feeds her child, she is not so much in contact with him, but immersed in creating good health for him in the future. Focusing on the future problems and difficulties of the child, diligently peering into the tasks that have not yet arisen at this particular moment, the mother does not see her child as he is at this moment, which means that she cannot turn to him as a subject and only manipulates him. I think that here is an important point of many disorders in the development of the child's contact with the outside world. The child gains experience of being an object for others and does not gain experience of being a subject. nine0003
I think that here is an important point of many disorders in the development of the child's contact with the outside world. The child gains experience of being an object for others and does not gain experience of being a subject. nine0003
In such a situation, one can hardly overestimate the support that a psychologist or psychotherapist can provide to the mother. To some extent, the paradox of life was that most of the young mothers turned to me for psychological help, not because I have some professional competence, relevant university training, etc., but because in their eyes I was an “experienced mother » five children. And my existence also confirmed that many problems could actually be solved. This largely determined the nature of our “work”: it did not take the form of traditional psychotherapeutic sessions, but began as an “exchange of maternal experience” and only then did the actual psychotherapeutic request arise. nine0003
Usually the beginning was connected with some kind of medical or domestic issue related to feeding or the peculiarities of the child's regimen, and already from them we moved on to a discussion of psychological problems proper.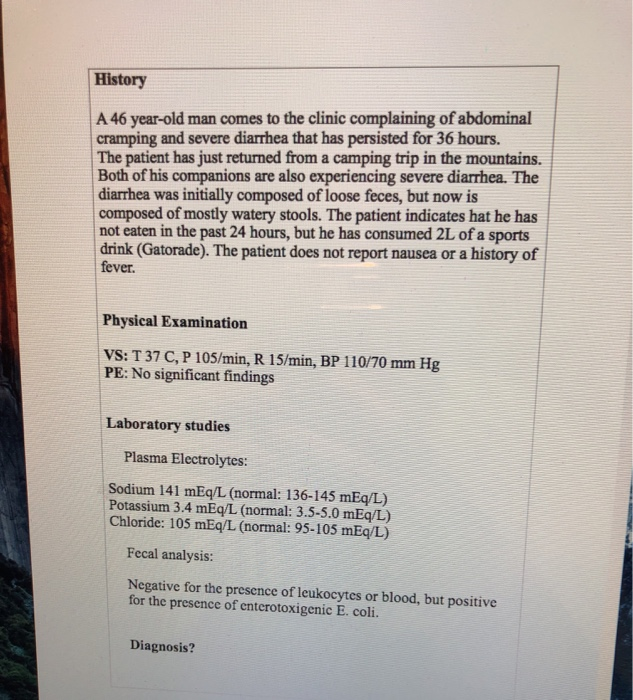
Talking about their feelings, young mothers talked about their confusion, lack of self-confidence (“I can’t do everything right at all” - while it is assumed that there is such an absolutely correct way in the world. “I always do not have enough time, to do laundry, take a walk with the child, I can neither read nor meet friends, I don’t see anyone, because I don’t have enough time all the time”). They complained of difficulties in making a decision and uncertainty about its correctness (“I don’t understand where to start, I start doing one thing, then I quit it, take on others and so on without end”, “yesterday I gave my baby for the first since kefir, it was probably wrong, I won’t do it again”), to my lack of independence in communicating with the child. nine0003
It could be seen that in this case, the mother was not in contact with her child, but was absorbed in her fears, expectations, her duties. The feeling of separation from the child, of being fenced off from him, a misunderstanding of his desires, his condition was not always realized by mothers, but it manifested itself in words, gestures, and looks.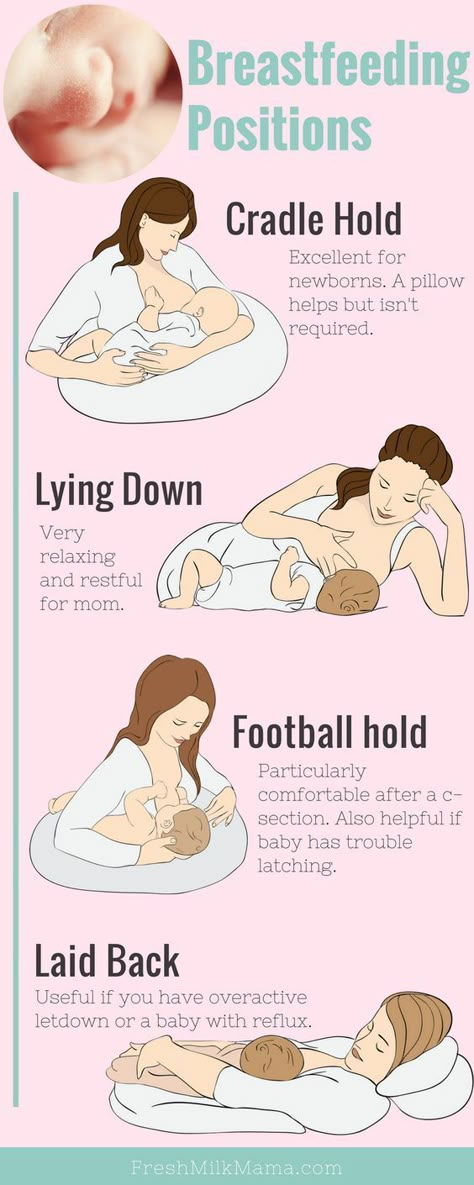 Sometimes there was irritation with the child, anger from not understanding his behavior, especially screaming or crying, and, consequently, the inability to help him, correct something. One mother told me: “I can’t understand what he needs, what he wants. I'm afraid something is wrong with him." Another mother spoke of her daughter like this: “When a girl cries, I get very scared, I just can’t guess what is happening to her. We just cry together." On another occasion, the same mother said: “When she cries and screams, I get so angry that I want to throw her or hit her; I know I'm a very bad mother." nine0003
Sometimes there was irritation with the child, anger from not understanding his behavior, especially screaming or crying, and, consequently, the inability to help him, correct something. One mother told me: “I can’t understand what he needs, what he wants. I'm afraid something is wrong with him." Another mother spoke of her daughter like this: “When a girl cries, I get very scared, I just can’t guess what is happening to her. We just cry together." On another occasion, the same mother said: “When she cries and screams, I get so angry that I want to throw her or hit her; I know I'm a very bad mother." nine0003
At the first steps of our work, it turned out that it was impossible for young mothers who found themselves in the role of patients to remain with their feelings for the child, with their fears and aggression, and they began to “drown out” them with frantic economic and educational activity. At the same time, they constantly did something with the baby, but only by manipulating him, and this led to growing disappointment: “I try to calm him down,” one mother said about her son, “I change my pants, feed him, but nothing helps, I I feel terribly tired, disappointed, I am a very bad mother. nine0003
nine0003
Most of our meetings took place at home, so that I could directly observe the interaction of mother and child during feeding, dressing, in free communication. It was evident how mother and baby touched each other, how free or constrained were the movements of the mother, the consistency of their postures, their tension during this communication. It could be noted that the movements of the mothers were very constrained and tense. They were not free and direct, did not correspond to the feelings of the mother herself or the state of the child, but were dictated by some special tasks: to dress the child (and not to warm him), to feed the child (and not to satisfy his hunger). This was also manifested in the answers to my question: “What do you want to do now?” - "Dress". Sometimes the mother did not even look at her child, at his face, into his eyes while she was feeding him or changing his clothes. Being near, I felt this tension and stiffness of the hands and the whole body of the mother, and I had a clear desire to stop the flow of these actions. nine0003
nine0003
Then I asked my mother to stop, to stop fussing, despite the abundance of different things, to give myself time to just be with the child. This was the first step in the actual therapeutic work. At the first moment, surprise appeared on the face: how is it possible to take it and stop? Then the surprise was replaced by confusion: "I don't know what I want to do with the child." There was a consciousness that at the moment of interaction with the child she was out of real contact with him, she was not with him "here and now", but with the experience of her failure or her obligations. nine0003
During communication, the mother was in contact "not with her child, but with someone else who had to prove their worth and competence." And her actions were not caused by a real situation, but by some picture of a “good mother” in her mind and a picture of a “prosperous future” for her child. Continuing to do something with the child, this mother tried to help him by doing the “correct” manipulations, but the baby did not stop screaming, he continued to openly suffer. Mom began to feel fear, despair, these feelings completely filled her, and suddenly she felt that she really wanted to "throw him away and run away." She said that she would like to “close her eyes and plug her ears, she would like to go somewhere far away, but she feels that the baby is chained to her, and she cannot leave him, give him up, she must stay with him, but does not want to watch him cry, hear his voice. She stood near the door from the room, but did not go out, took a step towards the child and came back. She didn't want to touch him, but when she did, it was with force, with great tension. She hugged the child with such force, as if she wanted to pinch him. nine0003
Mom began to feel fear, despair, these feelings completely filled her, and suddenly she felt that she really wanted to "throw him away and run away." She said that she would like to “close her eyes and plug her ears, she would like to go somewhere far away, but she feels that the baby is chained to her, and she cannot leave him, give him up, she must stay with him, but does not want to watch him cry, hear his voice. She stood near the door from the room, but did not go out, took a step towards the child and came back. She didn't want to touch him, but when she did, it was with force, with great tension. She hugged the child with such force, as if she wanted to pinch him. nine0003
At this point, I pointed out to her that her child was strong enough and tough enough to go without her for a while, and that I was quite sure that nothing bad would happen to him if she allowed herself to stay in another room for a while and leave him alone in the bed. After some hesitation, she decided to try and put her crying and loudly screaming baby in the crib, went to the door and said that somehow nothing prevented her from leaving the room. I asked her to come back as soon as she feels she really wants to be with her child. A few minutes later she returned to the room much calmer and smiling shyly. She looked at her son and began to touch him, stroke him. Now it was soft movements, filled with her feelings, and not the obligation to be a "good mother". As soon as the mother was able to get in touch with her feelings, her feelings for the child, she no longer needed to restrain and limit herself. Her hands became freer, they could not only hold the child, but also feel his body, his movements, his tension. nine0003
I asked her to come back as soon as she feels she really wants to be with her child. A few minutes later she returned to the room much calmer and smiling shyly. She looked at her son and began to touch him, stroke him. Now it was soft movements, filled with her feelings, and not the obligation to be a "good mother". As soon as the mother was able to get in touch with her feelings, her feelings for the child, she no longer needed to restrain and limit herself. Her hands became freer, they could not only hold the child, but also feel his body, his movements, his tension. nine0003
I offered to take the child in my arms and feel his whole body with my hands, palms, fingers. Mom gently and gradually began to change her position, becoming an increasingly comfortable environment for the child. She began to follow his movements, his desire for her and away from her. Their movements resembled a game or a special dance. They looked at each other, smiled at each other, forming a single circle. Suddenly, the mother laughed and said that, it turns out, it is very easy to understand your child. She said: “I feel him well, I understand that he wants to be with me, this is clear to me.” But some time later, the baby began to turn his head and mom immediately guessed that he was looking for her breasts, he was hungry. Just a few hours ago, she spoke of her son: “He screams and turns his head in all directions. I don't understand what he wants! Now she said: “He wants to eat!” At that moment, she no longer felt angry at her child, the meaning of his cry and his movements was clear to her. nine0003
Suddenly, the mother laughed and said that, it turns out, it is very easy to understand your child. She said: “I feel him well, I understand that he wants to be with me, this is clear to me.” But some time later, the baby began to turn his head and mom immediately guessed that he was looking for her breasts, he was hungry. Just a few hours ago, she spoke of her son: “He screams and turns his head in all directions. I don't understand what he wants! Now she said: “He wants to eat!” At that moment, she no longer felt angry at her child, the meaning of his cry and his movements was clear to her. nine0003
It turned out to be important for the mother to feel the body of her child - his arms, legs, back, stomach, neck. This made it possible to feel and understand the meaning of the child's gestures and postures, to distinguish between pain and hunger, to realize the differences in his feelings and desires. This helped to treat the child as an integral creature with a soul and consciousness, and made it possible to establish contact with him.
I tried to support young mothers in their actions with the child, in an effort not to be afraid to touch him, move him in order to feel his response. There was a change from the situation “SHOULD - SHOULD NOT, POSSIBLE - SHOULD NOT” to a situation of free contact with each other, from taking on and diligently fulfilling the role of a “good mother” in general to being a “bad mother” to your child. Now they were discovering for themselves the possibility of contact with their child, the opportunity for a new experience, for being a “happy mother”. nine0003
Somewhat later, when we discussed the changes that were taking place in themselves and in their relationship with the children, I said that it was a kind of psychotherapy. In response, one of the mothers said: “It was as if my eyes were opened,” and the other was surprised: “I did everything myself!” It seems to me that this is a very good result: the experience of contact with the child really became her personal experience.
In general, these stories developed as follows: at first, mother and child were out of contact, mother was closed from the child by her fear or anger. During our work, they united in contact into a single figure, they merged in their feelings and movements. In conclusion, they again found themselves separated at some distance, but not as flat roles, but as three-dimensional figures, as separate personalities with their own inner world. nine0003
The peculiarity of these situations was also that the mother, acting as a patient, acted simultaneously as a therapist in relation to her child, providing awareness of the need, the possibility of active actions for her child and satisfaction of the need for closeness, security, love.
Source: Kedrova N.B. "Here and now" in mother-child contact // Moscow Journal of Psychotherapy. 1994. No. 3.
nine0000 Breastfeeding in the first month: what to expectNot sure how to establish lactation and increase milk production? If you need help, support, or just want to know what to expect, read our first month breastfeeding advice
Share this information
The first weeks of breastfeeding are a very stressful period. If at times you feel like you can't handle it, know that you are not alone. Feeding your baby all day long is completely natural and helps produce breast milk, but can be quite tiring at times. Be patient, think about yourself and remember: after the first month, when milk production stabilizes, it will become easier. nine0003
If at times you feel like you can't handle it, know that you are not alone. Feeding your baby all day long is completely natural and helps produce breast milk, but can be quite tiring at times. Be patient, think about yourself and remember: after the first month, when milk production stabilizes, it will become easier. nine0003
How often should a baby be breastfed?
Babies are born with a small stomach that grows rapidly with increasing milk production: in the first week it is no larger than an apricot, and after two weeks it is already the size of a large chicken egg. 1.2 Let the child eat as much as he wants and when he wants. This will help him quickly regain the weight lost after birth and grow and develop further.
“Be prepared to feed every two to three hours throughout the day. At night, the intervals between feedings can be longer: three to four or even five hours, says Cathy Garbin, a recognized international expert on breastfeeding. Some eat quickly and are satiated in 15 minutes, while others take an entire hour to feed. Do not compare your breastfeeding regimen with that of other mothers - it is very likely that there will be nothing in common between them. nine0003
Do not compare your breastfeeding regimen with that of other mothers - it is very likely that there will be nothing in common between them. nine0003
At each feed, give your baby a full meal from one breast and then offer a second one, but don't worry if the baby doesn't take it. When the baby is full, he lets go of his chest and at the same time looks relaxed and satisfied - so much so that he can immediately fall asleep. The next time you feed, start on the other breast. You can monitor the order of the mammary glands during feeding using a special application.
Why does the child always ask for a breast?
The first month is usually the hardest time to breastfeed. But do not think that because the baby is constantly hungry and asks for a breast almost every 45 minutes, then you do not have enough milk. nine0003
In the first month, the baby needs to eat frequently to start and stimulate the mother's milk production. It lays the foundation for a stable milk supply in the future. 3
3
In addition, we must not forget that the child needs almost constant contact with the mother. The bright light and noise of the surrounding world at first frighten the baby, and only by clinging to his mother, he can calm down.
Sarah, mother of three from the UK, confirms: “Crying is not always a sign of hunger. Sometimes my kids just wanted me to be around and begged for breasts to calm them down. Use a sling. Place the cradle next to the bed. Don't look at the clock. Take advantage of every opportunity to relax. Forget about cleaning. Let those around you take care of you. And not three days, but six weeks at least! Hug your baby, enjoy the comfort - and trust your body." nine0003
Do I need to feed my baby on a schedule?
Your baby is still too young for a strict daily routine, so
forget about breastfeeding schedules and focus on his needs.
“Volumes have been written about how to feed a baby on a schedule, but babies don't read or understand books,” Cathy says.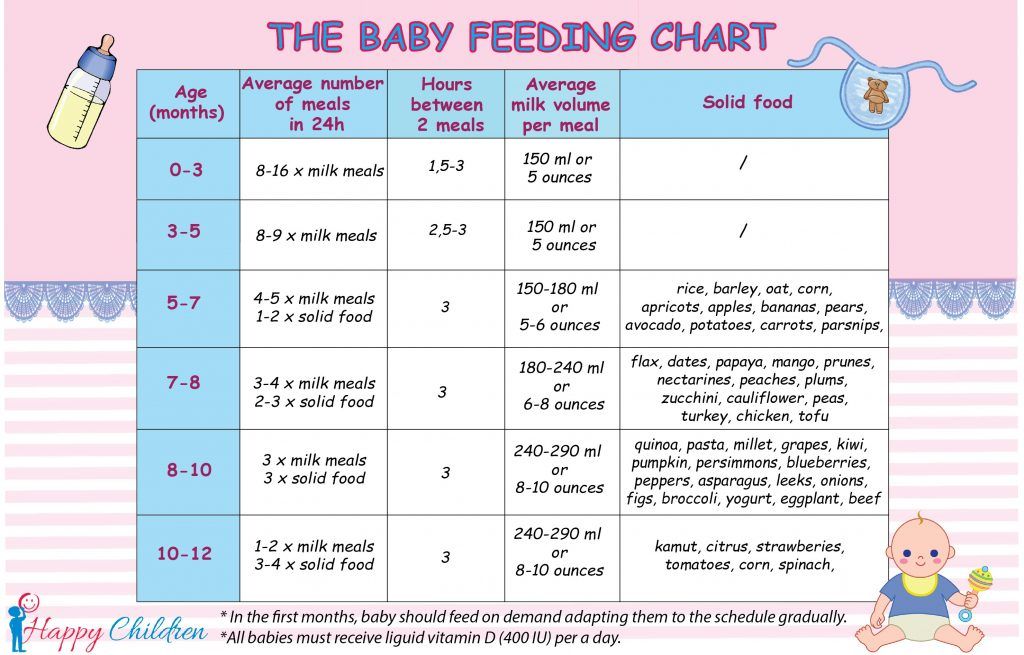 - All children are different. Some people can eat on a schedule, but most can't. Most often, over time, the child develops his own schedule.
- All children are different. Some people can eat on a schedule, but most can't. Most often, over time, the child develops his own schedule.
Some mothers report that their babies are fine with scheduled feedings, but they are probably just the few babies who would eat every four hours anyway. Adults rarely eat and drink the same foods at the same time of day - so why do we expect this from toddlers?
Offer your baby the breast at the first sign of hunger. Crying is already the last stage, so be attentive to early signs: the baby licks his lips, opens his mouth, sucks his fist, turns his head with his mouth open - looking for the breast. nine0061 4
What is a “milk flush”?
At the beginning of each feed, a hungry baby actively suckles the nipple,
thereby stimulating the milk flow reflex - the movement of milk through the milk ducts. 5
“Nipple stimulation triggers the release of the hormone oxytocin,” Cathy explains. “Oxytocin circulates throughout the body and causes the muscles around the milk glands to contract and the milk ducts to dilate. This stimulates the flow of milk. nine0003
This stimulates the flow of milk. nine0003
If the flushing reflex fails, milk will not come out. This is a hormonal response, and under stress it may not work at all or work poorly. Therefore, it is so important that you feel comfortable and calm when feeding.
“Studies show that each mother has a different rhythm of hot flashes during one feed,” Kathy continues, “Oxytocin is a short-acting hormone, it breaks down in just 30-40 seconds after formation. Milk begins to flow, the baby eats, the effect of oxytocin ends, but then a new rush of milk occurs, the baby continues to suckle the breast, and this process is repeated cyclically. That is why, during feeding, the child periodically stops and rests - this is how nature intended. nine0003
The flow of milk may be accompanied by a strong sensation of movement or tingling in the chest, although 21% of mothers, according to surveys, do not feel anything at all. 5 Cathy explains: “Many women only feel the first rush of milk. If you do not feel hot flashes, do not worry: since the child eats normally, most likely, you simply do not understand that they are.
If you do not feel hot flashes, do not worry: since the child eats normally, most likely, you simply do not understand that they are.
How can you tell if your baby is getting enough milk?
Since it is impossible to track how much milk a baby eats while breastfeeding, mothers sometimes worry that the baby is malnourished. Trust your child and your body. nine0003
After a rush of milk, the baby usually begins to suckle more slowly. Some mothers clearly hear how the baby swallows, others do not notice it. But one way or another, the child himself will show when he is full - just watch carefully. Many babies make two or three approaches to the breast at one feeding. 6
“When a child has eaten, it is noticeable almost immediately: a kind of “milk intoxication” sets in. The baby is relaxed and makes it clear with his whole body that he is completely full, says Katie, “Diapers are another great way to assess whether the baby is getting enough milk. During this period, a breastfed baby should have at least five wet diapers a day and at least two portions of soft yellow stool, and often more. ” nine0003
” nine0003
From one month until weaning at six months of age, a baby's stool (if exclusively breastfed) should look the same every day: yellow, grainy, loose, and watery.
When is the child's birth weight restored?
Most newborns lose weight in the first few days of life. This is normal and should not be cause for concern. As a rule, weight is reduced by 5-7%, although some may lose up to 10%. One way or another, by 10–14 days, almost all newborns regain their birth weight. In the first three to four months, the minimum expected weight gain is an average of 150 grams per week. But one week the child may gain weight faster, and the next slower, so it is necessary that the attending physician monitor the health and growth of the baby constantly. nine0061 7.8
At the slightest doubt or signs of dehydration, such as
dark urine, no stool for more than 24 hours, retraction of the fontanel (soft spot on the head), yellowing of the skin, drowsiness, lethargy, lack of appetite (ability to four to six hours without feeding), you should immediately consult a doctor. 7
7
What is "cluster feeding"?
When a baby asks for a breast very often for several hours, this is called cluster feeding. nine0061 6 The peak often occurs in the evening between 18:00 and 22:00, when many babies are especially restless and need close contact with their mother. Most often, mothers complain about this in the period from two to nine weeks after childbirth. This is perfectly normal and common behavior as long as the baby is otherwise healthy, eating well, gaining weight normally, and appears content throughout the day. 9
Cluster feeding can be caused by a sharp jump in the development of the body - during this period the baby especially needs love, comfort and a sense of security. The growing brain of a child is so excited that it can be difficult for him to turn off, or it just scares the baby. nine0061 9 If a child is overworked, it is often difficult for him or her to calm down on his own and the help of adults is needed.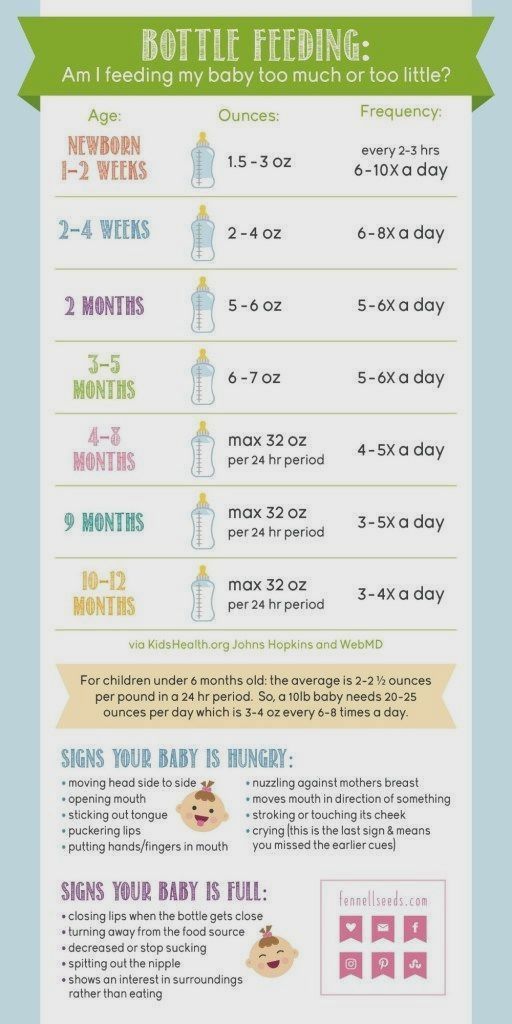 And breastfeeding is the best way to calm the baby, because breast milk is not only food, but also pain reliever and a source of happiness hormones. 10
And breastfeeding is the best way to calm the baby, because breast milk is not only food, but also pain reliever and a source of happiness hormones. 10
“No one told me about cluster feeding, so for the first 10 days I just went crazy with worry - I was sure that my milk was not enough for the baby,” recalls Camille, a mother from Australia, “It was a very difficult period . I was advised to pump and supplement until I finally contacted the Australian Breastfeeding Association. There they explained to me what was happening: it turned out that it was not about milk at all. nine0003
Remember, this is temporary. Try to prepare dinner for yourself in the afternoon, when the baby is fast asleep, so that in the evening, when he begins to often breastfeed, you have the opportunity to quickly warm up the food and have a snack. If you are not alone, arrange to carry and rock the baby in turns so that you have the opportunity to rest. If you have no one to turn to for help and you feel that your strength is leaving you, put the baby in the crib and rest for a few minutes, and then pick it up again.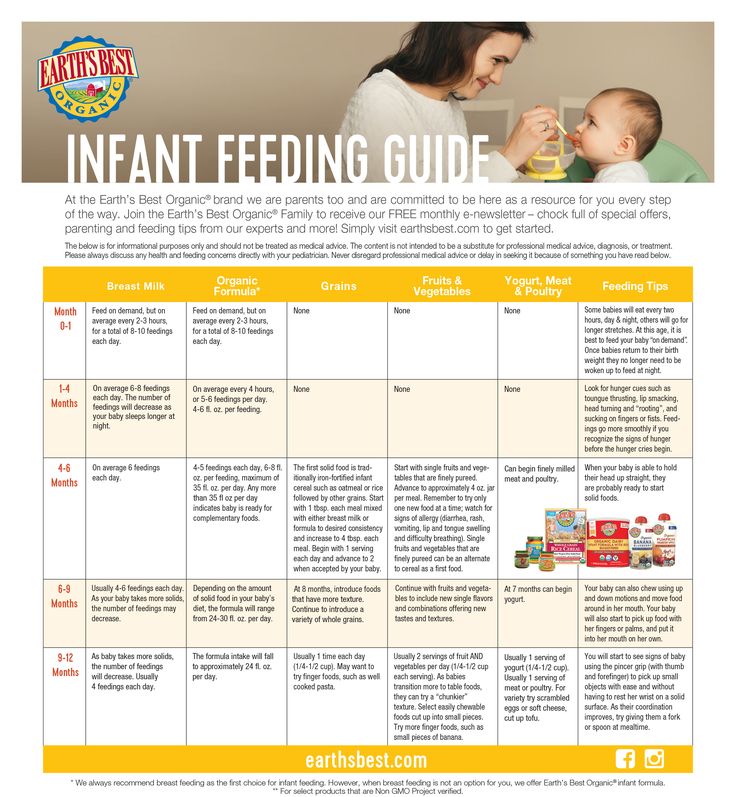 nine0003
nine0003
Ask your partner, family and friends to help you with household chores, cooking and caring for older children if you have any. If possible, hire an au pair. Get as much rest as possible, eat well and drink plenty of water.
“My daughter slept a lot during the day, but from 23:00 to 5:00 the cluster feeding period began, which was very tiring,” recalls Jenal, a mother from the USA, “My husband tried his best to make life easier for me - washed, cleaned, cooked, changed diapers, let me sleep at every opportunity and never tired of assuring me that we were doing well. nine0003
If you are concerned about the frequency of breastfeeding, it is worth contacting a specialist. “Check with a lactation consultant or doctor to see if this is indicative of any problems,” recommends Cathy. “Resist the temptation to supplement your baby with formula (unless recommended by your doctor) until you find the cause. It may not be a matter of limited milk production at all - it may be that the child is inefficiently sucking it.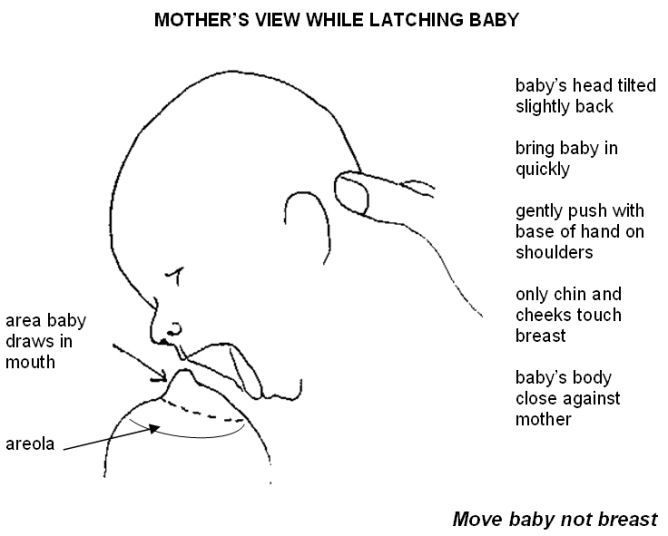
When will breastfeeding become easier? nine0059
This early stage is very special and does not last long. Although sometimes it seems that there will be no end to it, rest assured: it will get easier soon! By the end of the first month, breast milk production will stabilize, and the baby will become stronger and learn to suckle better. 2.3 Any problems with latch on by this time will most likely be resolved and the body will be able to produce milk more efficiently so inflammation and leakage of milk will start to subside.
“The first four to six weeks are the hardest, but then things start to get better,” Cathy assures. It just needs to be experienced!” nine0003
The longer breastfeeding continues, the more benefits it brings, from saving on formula and improving sleep quality 11-13 to boosting your baby's immune system 14 and reducing your risk of certain cancers. 15
“When you feel like you're on your limit, try to go from feed to feed and day to day,” advises Hannah, a UK mom. “I was sure I wouldn’t make it to eight weeks. And now I have been breastfeeding for almost 17 weeks, and I dare say it is very easy.” nine0003
“I was sure I wouldn’t make it to eight weeks. And now I have been breastfeeding for almost 17 weeks, and I dare say it is very easy.” nine0003
Read the resource Breastfeeding beyond the first month: what to expect
Literature
1 Naveed M et al. An autopsy study of relationship between perinatal stomach capacity and birth weight. Indian J Gastroenterol .1992;11(4):156-158. - Navid M. et al., Association between prenatal gastric volume and birth weight. Autopsy. Indian J Gastroenterol. 1992;11(4):156-158.
2 Neville MC et al. Studies in human lactation: milk volumes in lactating women during the onset of lactation and full lactation . Am J Clinl Nutr . 1988;48(6):1375-1386. at the beginning and at the peak of lactation." Am F Clean Nutr. 1988;48(6):1375-1386.
3 Kent JC et al. Principles for maintaining or increasing breast milk production. J 2012;41(1):114-121. - Kent J.S. et al., "Principles for Maintaining and Increasing Milk Production". J Obstet Ginecol Neoneutal Nurs. 2012;41(1):114-121. nine0046
Principles for maintaining or increasing breast milk production. J 2012;41(1):114-121. - Kent J.S. et al., "Principles for Maintaining and Increasing Milk Production". J Obstet Ginecol Neoneutal Nurs. 2012;41(1):114-121. nine0046
4 Australian Breastfeeding Feeding cues ; 2017 Sep [ cited 2018 Feb ]. - Australian Breastfeeding Association [Internet], Feed Ready Signals; September 2017 [cited February 2018]
5 Kent JC et al. Response of breasts to different stimulation patterns of an electric breast pump. J Human Lact . 2003;19(2):179-186. - Kent J.S. et al., Breast Response to Different Types of Electric Breast Pump Stimulation. J Human Lact (Journal of the International Association of Lactation Consultants). 2003;19(2):179-186.
2003;19(2):179-186.
6) Kent JC et al . Volume and frequency of breastfeedings and fat content of breast milk throughout the day. Pediatrics. 2006;117(3): e 387-395. - Kent J.S. et al., "Amount and frequency of breastfeeding and fat content of breast milk during the day." Pediatrix (Pediatrics). 2006;117(3):e387-95.
7 Lawrence RA, Lawrence RM. Breastfeeding: A guide for the medical profession. 7th ed. Maryland Heights MO, USA: Elsevier Mosby; 2010. 1128 p . - Lawrence R.A., Lawrence R.M., "Breastfeeding: A guide for healthcare professionals." Seventh edition. Publisher Maryland Heights , Missouri, USA: Elsevier Mosby; 2010. P. 1128.
8 World Health Organization. [Internet]. Child growth standards; 2018 [cited 2018 Feb] - World Health Organization. [Internet]. Child Growth Standards 2018 [cited February 2018]. nine0046
[Internet]. Child Growth Standards 2018 [cited February 2018]. nine0046
9 Australian Breastfeeding Association . [ Internet ]. Cluster feeding and fussing babies ; Dec 2017 [ cited 2018 Feb ] - Australian Breastfeeding Association [Internet], Cluster Feeding and Screaming Babies; December 2017 [cited February 2018]. nine0046
10 Moberg KU, Prime DK. Oxytocin effects in mothers and infants during breastfeeding. Infant . 2013;9(6):201-206.- Moberg K, Prime DK, "Oxytocin effects on mother and child during breastfeeding". Infant. 2013;9(6):201-206.
11 U.S. Department of Health & Human Services [Internet]. Surgeon General Breastfeeding factsheet; 2011 Jan 20 [cited 2017 Feb] - Department of Health and Human Services [Internet], "Breastfeeding Facts from the Chief Medical Officer", Jan 20, 2011 [cited Feb 2017]
12 Kendall-Tackett K et al. The effect of feeding method on sleep duration, maternal well-being, and postpartum depression. clinical lactation. 2011;1;2(2):22-26. - Kendall-Tuckett, K. et al., "Influence of feeding pattern on sleep duration, maternal well-being and the development of postpartum depression." Clinical Lactation. 2011;2(2):22-26.
The effect of feeding method on sleep duration, maternal well-being, and postpartum depression. clinical lactation. 2011;1;2(2):22-26. - Kendall-Tuckett, K. et al., "Influence of feeding pattern on sleep duration, maternal well-being and the development of postpartum depression." Clinical Lactation. 2011;2(2):22-26.
13 Brown A, Harries V. Infant sleep and night feeding patterns during later infancy: Association with breastfeeding frequency, daytime complementary food intake, and infant weight. Breast Med . 2015;10(5):246-252. - Brown A., Harris W., "Night feedings and infant sleep in the first year of life and their association with feeding frequency, daytime supplementation, and infant weight." Brest Med (Breastfeeding Medicine). 2015;10(5):246-252.
14 Hassiotou F et al. Maternal and infant infections stimulate a rapid leukocyte response in breastmilk.