Baby gulps bottle feeding
Tips for Bottle Fed Baby Gas
JanelMS, RD, LDN, CBS
Read time: 8 minutes
What should I know about handling infant gas in my bottle-fed baby?Understand that baby gas is unavoidable
Learn the many causes and symptoms of a gassy baby
Tips and tricks for baby gas relief
Gas is incredibly common in babies. Many health professionals consider it a result of baby’s immature digestive system. Gas bubbles create painful pressure that baby is not yet good at resolving on their own, and it’s often worse at night. In fact, you’ll hear a lot of rumbling and gurgling until your little one is able to handle the gas better, which generally happens around 3 or 4 months of age.
While swallowing air tends to be a common culprit of gas in babies, both causes and symptoms of gas discomfort vary from child to child. This sometimes makes it more challenging to find the right solution for your little one.
Common causes of gas discomfort in formula or bottle-fed babies:1, 2
Incorrect latch on the bottle nipple leading your baby to swallow too much air
Excessive crying that fills your baby’s belly with air
Constipation
Immature digestive tract is still learning to process breastmilk, and/or formula, gas, and stool effectively
Common symptoms of gas discomfort in formula or bottle-fed babies:
Excessive burping can indicate that your baby is swallowing too much air from bottle feeding or crying
Your baby may be crying, arching their back, drawing their legs up toward their tummy, or clenching their fists
Spitting up (while typically completely normal) can sometimes be a sign of gas build up in the stomach. Trapped gas bubbles can push some formula or breastmilk back up
Excessive flatulence (again, usually completely normal and a natural way to relieve the pressure of gas) can indicate your baby’s digestive tract is still maturing
Bloating or swollen abdomen can mean that gas is trapped in the intestines
Trouble sleeping is often a symptom, as well as a result, of the combined symptoms listed above – creating a vicious cycle!
While many believe that colic stems from gas, the true causes are harder to pinpoint. 3 Some research even points to infantile migraines as a cause.4 If your baby is crying for 3 hours per day, 3 days per week, and has been doing this for at least 3 weeks, check in with your baby’s pediatrician to chat about the possibility of colic.
3 Some research even points to infantile migraines as a cause.4 If your baby is crying for 3 hours per day, 3 days per week, and has been doing this for at least 3 weeks, check in with your baby’s pediatrician to chat about the possibility of colic.
Learn more about colic and what to do here: How Can I Manage My Baby’s Colic?
Not sure how to help your little one? Come chat with our team of registered dietitians, fellow moms, and lactation specialists, available from Monday – Friday 8 am – 6 pm (ET). Chat now!
Bottle feeding tips to help prevent gasWhat position should I bottle feed my baby in?Hold your baby more upright with only a slight recline. Hold the bottle mostly horizontal, tipped only just enough to keep milk in the nipple.5 This allows baby to draw milk out at the pace they prefer, rather than it flowing too fast and making them swallow more air.
You could also try an angled bottle that naturally allows air to vent out the back.
The best kind of bottle will have a soft nipple that contours along your baby’s mouth and lips thus preventing air from flowing along with the milk.
The milk should flow gradually and slowly so your baby has time to drink and swallow without gulping excessively.6 Many bottles and nipples are staged for different ages, so notice how fast your baby takes the bottle.7
Learn more: Choosing the Right Bottles and Nipples
How fast should baby eat from a bottle?Bottle-feeding should take as long as nursing does for infants – at least 20 minutes but no more than an hour. If your baby can chug down a bottle in 5 minutes, they are likely gulping too fast and taking in too much air. If this is the case, try a slower flow (lower level) nipple.
If your little one is still drinking too quickly, try paced bottle feeding. This aims to slow the feed down and allow baby to take control of the speed of the milk and take breaks. 8
8
Read more: Paced Bottle Feeding
Can formula cause gas?Some babies may have a food intolerance or allergy to an ingredient in the formula. If you also notice changes in baby’s stool, such as mucous or blood, chat with baby’s pediatrician about this possibility.
Formula may cause gas if a lot of bubbles or foam formed when shaking the powder and water together.9 This will cause baby to swallow more air. Let the bottle sit in the fridge until all bubbles have dispersed.
Most formulas can be prepared up to 24 hours in advance and kept in individual bottles in the refrigerator, allowing for plenty of time for the bubbles to reduce!
Learn more: How to Prep Formula
What else can I do to prevent gas when bottle feeding?Burp baby during and after a feedingTake a break after every ounce or two to burp your baby in the middle of a feeding, as they may have swallowed too much air. Burp after the feed as well.
Pediatricians recommend burping your baby while they are in a seated position, with their head supported by the cradle of your hand. You can also burp your baby in the typical position – upright and over your shoulder.10
Be patient while burping because it may take some time for the gas bubbles to surface. You can always try laying baby down for a moment or two to let the bubbles re-settle and then lifting baby up and trying again. If your little one doesn’t burp after a few minutes, it’s ok to move on.
Use tummy timeTummy time isn’t just for your baby’s core and neck strength – the gentle pressure of lying on their belly can help push out the trapped gas.11 Wait at least 30 minutes after a feeding to allow your baby’s belly to settle before starting tummy time.
Or try a more advanced move – use both hands and a lot of guided support to lay your baby tummy down on a large beach or exercise ball and gently roll baby on the ball in a circular motion.
The football hold – try carrying your baby face down with her body resting on your forearm, the front of baby’s diaper area in your hand with baby’s chin cradled in your elbow. Carrying your little one in this face-down position will place the same gentle pressure on her belly that is achieved during tummy time. While in the football hold, you can also gently tap your baby’s back or give a gentle bounce with your arm to give gravity a helping hand.
The colic curl position – Place your baby’s head and back against your chest and encircle your arms under their bottom. Then, move your arms up gently to curl baby into a ball. Or, try reversing this position by placing your baby’s feet against your chest as you hold them.12
The tummy tuck position – Place a rolled-up cloth diaper or a warm (not hot) water bottle enclosed in a cloth diaper under your baby’s tummy. To further relax a tense tummy, lay your baby stomach-down on a cushion with legs dangling over the edge while rubbing baby’s back. Turn baby’s head to the side so their breathing isn’t obstructed.
To further relax a tense tummy, lay your baby stomach-down on a cushion with legs dangling over the edge while rubbing baby’s back. Turn baby’s head to the side so their breathing isn’t obstructed.
While your baby is lying on their back, gently rub their tummy in a clockwise motion, pulling your hands down the curve of the belly. Massaging in a clockwise direction helps to move gas along as that is the route the intestinal tract follows. You can use some baby-safe lotion or oil if baby’s torso is not covered in clothing.13
Bicycle baby’s legsBicycling your baby’s legs in a circular motion can help to move the intestines and release gas trapped lower in the abdominal track. With your baby lying on their back, take their legs in your hands and cycle them slowly back and forth as if they were riding on a bike. Take a break every now and then to press both baby’s knees gently into their own tummy for some extra pressure.
Simethicone breaks down bubbles of gas trapped in the stomach and intestines. It is not absorbed by the body and therefore considered quite safe for babies.9
In clinical trials, simethicone drops were effective in reducing the total amount of gas passed, but not more effective than a placebo when the study focused on baby’s total crying time and the severity of colic-like episodes.14, 15
Wait it out!For most babies, the number one most effective treatment for gas is time. Remember that babies are likely to be gassy no matter what because their digestive system is still immature. If you cannot find an apparent cause for your baby’s gassiness, they probably just need a little more time to mature.
Let’s Chat!We know parenting often means sleepless nights, stressful days, and countless questions and confusion, and we want to support you in your feeding journey and beyond.
Our Happy Baby Experts are a team of lactation consultants and registered dietitians certified in infant and maternal nutrition – and they’re all moms, too, which means they’ve been there and seen that. They’re here to help on our free, live chat platform Monday through Friday, from 8am–6pm ET. Chat Now!
Read more about the experts that help write our content!
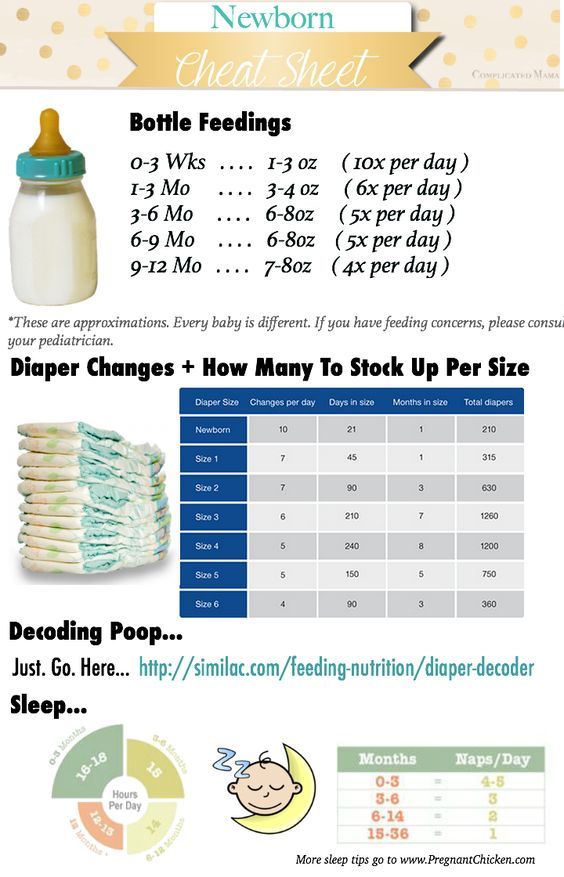
For more on this topic, check out the following articlesHow Much Formula does my Baby Need?
How Do I Manage Gas In My Breastfed Baby?
Should I Switch Baby Formulas?
Bottle-feeding problems and solutions | From Tiny Tot to Toddler
Babies can sometimes have trouble feeding. Usually, the problem is temporary. The first thing to do is observe your baby. Try to get a feel for her temperament as well as her feeding and sleeping routine.
Your baby sleeps a lot
If your baby sleeps a lot, you probably wonder whether you should wake her to feed. Knowing what’s best isn’t always easy. You can follow her routine and let her sleep if she
Knowing what’s best isn’t always easy. You can follow her routine and let her sleep if she
- Wakes up on her own to feed
- Is an active and effective feeder
- Pees at least 6 times and passes at least 3 stools a day
- Is calm and seems satisfied after feeding
- Has regained her birth weight and continues to put on weight
In this case, there is nothing to worry about. Babies each have their own routine that develops over time.
You may need to wake your baby up to feed her if she sleeps a lot.
Photo: Marie-Ève Bolduc
Some babies sleep so much they may skip some feedings, especially during the first 2 to 3 weeks. This means they will have a hard time getting all the milk they need. If your baby sleeps a lot and doesn’t show the signs described above, you need to stimulate her to drink more.
What to do?
- Keep an eye out for signs that she’s sleeping lightly (she’s moving, making sucking motions, or moving her eyes beneath her eyelids) when it will be easier to wake her up.

- Stimulate her: talk to her, massage her back, legs, arms, etc.
- Leave her in an undershirt or diaper: babies drink less when they are warm.
- See a professional if you’re worried or see no improvement after a few days.
Your baby drinks very slowly
Babies can’t always suck effectively at the start. This is more common among babies who were born a few weeks prematurely (between 35 and 37 weeks of pregnancy). Even full-term babies may need a few days or weeks to get the hang of things. This situation usually improves with time. Be patient: your baby is learning. Some babies, however, will continue to drink slowly even as they get older.
What to do?
- Change to a faster nipple.
- Stimulate your baby as she feeds by rubbing her feet and tickling her back and sides.
- Run your finger under her chin and across her cheeks to stimulate her.
- Change her diaper or change her position for a few minutes.
Your baby often chokes while drinking
If the nipple you are using flows too quickly and your baby has too much milk in her mouth, she may choke (i. e., she swallows noisily, coughs and spits up a little milk).
e., she swallows noisily, coughs and spits up a little milk).
What to do?
- Change to a slower nipple.
- Take short feeding breaks.
- Avoid laying your baby on her back during feeding since milk will flow into her mouth even when she’s not sucking. Try to feed her in a near-sitting position so that the bottle is tilted only slightly downward (just enough for the nipple to fill with milk and not air). Your baby will then be able to drink at her own pace.
Your baby regurgitates a lot
As long as your baby is happy and putting on weight, regurgitation (“spitting up”) is generally nothing to worry about (see Regurgitation).
Some babies drink very fast, and their stomachs expand too quickly. This makes it easier for them to regurgitate, especially if they are very active and start moving around right after feeding.
If milk is coming out of the bottle too quickly, your baby will drink too much just to satisfy her need to suck. If she regurgitates a lot, the nipple on the bottle may be too fast.
If she regurgitates a lot, the nipple on the bottle may be too fast.
What to do?
If your baby is in good spirits and gaining weight, there’s nothing to worry about. You don’t need to do anything.
If regurgitation seems to be bothering her, watch her drink. If necessary, try these strategies:
- Change to a slower nipple.
- Take short feeding breaks.
- Try to burp her more.
- Avoid laying your baby on her back during feeding. Try to feed her in a near–sitting position so that milk will flow into her mouth more slowly.
- Try to keep activity to a minimum right after feeding.
It’s best to see a doctor if your baby
- Seems to be in pain
- Projectile vomits several times a day
- Wets fewer diapers
- Isn’t putting on enough weight
Your baby refuses the bottle
Your baby normally breastfeeds, and you want to bottle‑feed her? If she has trouble bottle-feeding or refuses to altogether, see the tips on Combining breast and bottle.
Baby won't take the bottle | Philips Avent
search support iconSearch Keywords
Home ›› What to do when your baby refuses a bottle
↑ top
any problems. If your breastfed baby refuses a bottle, don't worry. This is a common occurrence in many babies who are used to breastfeeding. Obviously, this can create certain difficulties for moms, especially if you need to return to work in the near future.
3 Philips Avent products to help you bottle feed:
So why is your baby refusing to bottle and crying? There are many ways to quickly and easily teach a breastfed baby to a bottle. Here are important tips on what to do when your baby refuses a bottle.
Is the baby refusing the bottle? Take a step back
If your baby cries while bottle feeding, the first thing to do is to start over and rethink your feeding approach and technique. Try the following steps when bottle feeding your baby: [1]
Try the following steps when bottle feeding your baby: [1]
- Lift and tilt your baby's head forward. Before inserting the pacifier into the baby's mouth, make sure that the baby's head is raised and tilted over his body to avoid choking: so that the baby does not choke and have the opportunity to burp during bottle feeding.
- Insert the pacifier. Bring the pacifier to the baby's lips and gently guide it into the baby's mouth. In no case do not try to press the nipple on the baby's lips and try to push it into his mouth. After touching the pacifier to the baby's lips, wait for the baby to open his mouth and take the pacifier.
- Hold the bottle at an angle. Tilt the bottle at an angle so that the nipple is only half full. So the child can eat at his own pace.
- Let the baby burp during and after feeding. It can be useful for a child to burp not only after feeding, but also approximately in the middle of the process. This will help reduce gas or tummy discomfort that your baby may experience from swallowing too much air.

- Stop in time, do not overfeed the baby. If the baby begins to turn his head away from the bottle or closes his mouth, then he is full and you need to stop feeding.
- Perhaps the flow of milk from the nipple to the baby is weak or, on the contrary, too fast, so he is naughty and refuses the bottle. Try changing the nipple to a nipple with a different flow.
Other tips if your baby refuses the bottle
If you've followed the steps above and your baby still refuses the bottle, don't worry. There are other ways to help bottle feed your baby. Here are some simple tricks you can add to your bottle feeding process. [2]
1. Remind your child about mom.
Sometimes a child can be fed by someone other than his mother - dad, grandmother or, for example, a nanny. If your baby fusses while bottle feeding, try wrapping the bottle in something that smells like mommy, like a piece of clothing or some fabric. This will make it easier to feed the baby when the mother is not around.
This will make it easier to feed the baby when the mother is not around.
2. Try to maintain skin contact while bottle feeding.
Some babies need contact with their mother, so try bottle feeding while leaning against you. However, some babies are better at bottle feeding when they are in the exact opposite position than when they are breastfed. For example, there is a position with bent legs. Lay the child on your bent knees, facing you, pointing the child's legs towards your stomach. During feeding, the baby will be able to look at you and contact you in this way. If your baby refuses a bottle, experiment to see which works best.
3. Move while feeding.
Sometimes all it takes to get your baby to take the bottle is a little wiggle or walk. The next time your baby starts crying while bottle feeding, try moving around a little rhythmically to calm him down.
4. Try changing the milk temperature.
Try changing the milk temperature.
If the baby still does not want to take the bottle, check if the milk in the bottle is too hot or too cold. Before feeding, put some warm breast milk on the inside of your wrist to check the temperature. Milk should be warm, but if it seemed hot to you, just place the bottle for a short while under a stream of cold water.
Choosing the right bottle for your baby If you plan to combine bottle feeding with breastfeeding, it is advisable to choose bottles with a nipple that will have a wide base as the bottle will grip closer to the breast. Also pay attention to the fact that the nipple is firm and flexible, the child must make an effort to drink from the bottle, as well as from the breast. Give preference to nipples with an anti-colic valve that vents air out of the bottle.
Natural bottle allows you to combine breast and bottle feeding. 83.3% of babies switch from a Natural bottle to breastfeeding and back. *
*
If you choose a bottle for artificial feeding, traditional bottles are fine, but it is desirable that the nipple is made of a hypoallergenic material, such as silicone, has an anti-colic valve and did not stick together when bottle fed. In case your baby spit up often, then use special bottles with anti-colic and anti-reflux valve, which reduces the risk of spitting up and colic.
Bottle with unique AirFree valve reduces the risk of colic, gas and spitting up. With this bottle, you can feed your baby in an upright or semi-upright position to reduce spitting up. Due to the fact that the nipple is filled with milk and not air during feeding, the baby does not swallow air, which means that feeding will be more comfortable.
Both bottles are indispensable if you want to breastfeed, bottle feed or just bottle feed your baby.
“My baby refuses to breastfeed but bottle feeds – help!”
Sometimes a baby gets used to bottle feeding and refuses to breastfeed. Therefore, it is important to use bottles that are suitable for combining breastfeeding with bottle feeding. If, nevertheless, you are faced with the fact that the child refuses to take the breast, try using silicone nipple covers to make the transition from the bottle to the breast and back more imperceptible.
Therefore, it is important to use bottles that are suitable for combining breastfeeding with bottle feeding. If, nevertheless, you are faced with the fact that the child refuses to take the breast, try using silicone nipple covers to make the transition from the bottle to the breast and back more imperceptible.
Remember that if you want to combine breastfeeding and bottle feeding, it is worth waiting at least a month before offering a bottle, so that you are lactating and have time to get used to each other and develop a breastfeeding regimen.
Breastfeed and bottle feed your baby with pleasure
Remember that it takes a while for your baby to get used to bottle feeding. This is completely normal. If you have to go to work, be sure to set aside enough time to bottle train your baby beforehand.
Remember that every child is different, so what works for one may not work for another. With a little time and patience, you will find out what works best for your baby when he refuses a bottle.
You will identify your child's unique needs. However, if your baby still refuses the bottle after all the steps above, check with your pediatrician.
Articles and tips from Philips Avent
References:
*O.L. Lukoyanova, T.E. Borovik, I.A. Belyaeva, G.V. Yatsyk; NTsZD RAMS; 1st Moscow State Medical University THEM. Sechenova, "The use of modern technological methods to maintain successful breastfeeding", RF, 10/02/2012 3 llli.org - The Baby Who Doesn't Nurse
llli.org - Introducing a Bottle to a Breastfed Baby
Baby+ app
Download the app and track your child's development and growth with trackers and save those special moments forever.
Download app:
You are leaving the Philips Healthcare (“Philips”) official website. Any links to third party websites that may be included on this site are provided solely as a convenience to you. Philips makes no warranties regarding any third party websites or the information they contain.
I understand
You are about to visit a Philips global content page
Continue
You are about to visit the Philips USA website.
I understand
How to bottle train a baby. Bottle feeding
Even if your baby is breastfed and you don't need to feed or supplement with formula, you still need to introduce your baby to the bottle. It will be needed when the baby needs to be given water, herbal tea for colic, or medication. Be prepared for the fact that acquaintance with a new thing may not go very smoothly.
Spring water Valio still, 1.5 l Read more
There are several reasons why a baby won't take a bottle.
Baby does not want to eat or drink
It simply doesn't occur to many anxious parents that the child is simply not hungry or thirsty at the moment. Do not forget also that the needs of a little person change - at 2 months the baby is not at all interested in the bottle, and at six months, after active games, he will drink from it with great pleasure.
Do not forget also that the needs of a little person change - at 2 months the baby is not at all interested in the bottle, and at six months, after active games, he will drink from it with great pleasure.
Uncomfortable temperature fluid
The child is very sensitive to hot or cold drinks. He is used to mother's milk. This means that water, tea or medicine should be heated to a comfortable 36-37 degrees.
Dislike the pacifier
What the baby does not like in one or another nipple - the shape, the rate of fluid intake, the density of the material - is almost impossible to guess. All that's left is to experiment. Offer different types (fortunately, there are a lot of them on sale now - silicone, latex, standard round, flat and orthodontic), something your baby will definitely "taste". Often the baby refuses the bottle because the nipple is cool. Before feeding, it can be dipped in warm water. But if the baby is teething, it is better to cool the nipple on the contrary - it will soothe the tooth in the gums.
Child does not like formula or drink
You can experiment with the mixture and offer the baby something new. Try Valio Baby® - they are as close as possible to the composition of breast milk and, unlike many other mixtures, they are made not from powdered, but from fresh cow's milk. It, in turn, is thoroughly tested and exceeds the standards of the European Union and the requirements for premium milk in Russia.
#PROMO_BLOCK#
How to teach your baby to bottle feed
Get to know the bottle gradually
First, just let the baby examine, touch the bottle. Let it be somewhere nearby more often and become a familiar subject for him. Feed/drink from it once a day at first, then offer more frequently.
Simulate breastfeeding
Often a child refuses a bottle because of an uncomfortable position. Hold the baby as if you were breastfeeding him. Place the nipple at the level of your nipple. Be calm and relaxed.
Be calm and relaxed.
Choose the right time
Giving a bottle to a well-fed child is a pointless exercise. However, if the baby is very hungry, the innovation will also not be to his liking. He will be naughty and demand his mother's breasts, and not a rubber nipple.
Ask for help
Sometimes it is easier for a baby to accept a bottle from the hands of a grandmother, nanny or dad. When there is no mother's breast in sight, which means asking for it is pointless.
Be very patient and unobtrusive
Move the pacifier over the baby's lips - it is likely that he will take it himself, following his instinct. If this does not happen, carefully insert the pacifier into the baby's mouth. Make sure he grabs her well. In the future, even when the baby is used to the bottle, do not leave him unattended - the baby may choke.
3.14 21
Power supplyShare:
Author: Reetta Tikanmäki
Palm oil in baby food
Infant milk formulas are made from cow's milk.