Common food sensitivities in breastfed babies
Allergies & Food Intolerances - La Leche League GB
Babies can be unsettled for many reasons and it can sometimes take time and effort to work out the cause. Our page The Unhappy Breastfed Baby can help you determine whether your baby’s behaviour is due to something other than an allergy.
But when you have ruled out most of the obvious causes and your baby is still, unhappy, colicky, experiencing dry and itchy skin or passing mucousy stools you may wonder whether they could be reacting to something in their diet or environment, or something in your own diet.
Certain medical conditions can have symptoms similar to those of an allergic reaction. It may be wise to rule these out before deciding whether a baby’s symptoms are due to an allergy or food intolerance.
A baby’s immune system is immature at birth.
Colostrum, or early milk, is rich in antibodies, particularly secretory IgA (SIgA), which provide a protective coating inside a baby’s intestines1. Mature breastmilk continues to provide protection, helping to prevent potential allergens from reaching a baby’s blood.
Exclusive breastfeeding generally helps to protect against allergy but it may still occur.
If any immediate family member ( siblings or parents) has an allergy eczema, hay fever or asthma, it makes it more likely that the baby could develop allergies2.
Food intolerance
A food intolerance does not involve an allergic reaction but can cause similar symptoms. It occurs when a baby has difficulty digesting a particular food. You may not need to stop giving your baby a food to which he is intolerant—reducing the amount may be enough.
Food allergy
A food allergy occurs when a baby has an immune response to specific foods. There are two types of food allergy reactions; immediate and delayed. A baby can have either or both3.
Immediate reactions are also called IgE-mediated alllergies. This is because the baby’s immune system creates specific IgE antibodies to a certain food. If a baby is given the specific food they are allergic to, the IgE antibodies will recognise it and cause the rapid release of chemicals, including histamine, that trigger inflammation and allergic symptoms. Symptoms appear within minutes, or up to 2 hours after eating the food responsible3.
If a baby is given the specific food they are allergic to, the IgE antibodies will recognise it and cause the rapid release of chemicals, including histamine, that trigger inflammation and allergic symptoms. Symptoms appear within minutes, or up to 2 hours after eating the food responsible3.
Delayed reactions are called non-IgE mediated allergies because they are not controlled by IgE. Instead it is believed such reactions are regulated by immune cells. Symptoms appear 4-72 hours after eating the food3.
It is wise to see your GP or health visitor if your baby is showing signs of allergy, but some symptoms are more worrying than others. Seek immediate medical help if your baby has signs of an anaphylactic reaction: sudden onset of breathing difficulties, swelling, or collapse, with or without a rash, after physical contact or eating a particular food.
Allergy symptoms
Food allergy symptoms occur in several different body systems; the tummy, airways and skin. An Allergic baby will usually have symptoms in more than one body system, but need not experience all the symptoms to indicate allergy. Many of the following allergy symptoms can also occur in normally developing children for other reasons.
An Allergic baby will usually have symptoms in more than one body system, but need not experience all the symptoms to indicate allergy. Many of the following allergy symptoms can also occur in normally developing children for other reasons.
| IgE mediated symptoms3 | Non-IgE mediated symptoms3 | |
|---|---|---|
| Time | Immediate: within minutes or up to 2 hours | Delayed: within 4–72 hours |
| When nursing | Baby hungry for the breast but pulls away after a minute or two, arching the back and screaming* | |
| Skin | Itching Inflammation** Hives/nettle rash Swelling, usually around the lips, face and eyes | Itching Inflammation** Eczema (dermatitis) |
| Tummy | Itchy mouth Nausea Colicky tummy pain*** Vomiting Diarrhoea | Reflux Loose or frequent poos Blood or mucus in poo Tummy pain Infantile colic*** Food refusal or aversion Constipation Inflammation in the nappy area** |
| Airways | Cough, chest tightness, wheeze, noisy breathing, trouble breathing Itchy nose, sneezing, runny nose, nasal congestion, conjunctivitis | Cough, chest tightness, wheeze, noisy breathing, trouble breathing |
| Other | Anaphylaxis: sudden onset of breathing difficulties, swelling, or collapse with or without a rash | Reduced growth, along with one or more tummy symptoms above Lethargy |
*This may also be caused by a fast let-down. See Too Much Milk and Oversupply for See Too Much Milk and Oversupply formore information if you think that this may apply to you. **Inflammation appears red on lighter skin, and darker brown, purple or grey on darker skin. ***Colic is defined as repeated episodes of excessive and inconsolable crying in an infant that otherwise appears to be healthy and thriving. | ||
Environmental triggers
An irritant is something that causes damage to the skin. Eczema (also known as dermatitis) and dry skin rashes can be caused by mild irritants such as bubble bath, baby wipes, skin cream, fabric conditioner or laundry detergent4. Many mothers find avoiding unnecessary products or using a different product improves things. Reading packaging can help avoid problems with common irritants such as lanolin and perfumes. Use fragrance-free products whenever possible. Be aware that herbals can also be allergenic and irritant – being natural does not necessarily mean a product is any less irritating. Hay fever symptoms and other ear, nose and throat symptoms can be caused by spring and summer pollens and other airborne allergens such as dust.
Hay fever symptoms and other ear, nose and throat symptoms can be caused by spring and summer pollens and other airborne allergens such as dust.
Identifying the problem food
If your baby is having only your milk
Food allergens in the mother’s diet can pass through into the breastmilk so a breastfed baby can have an allergic response or intolerance to something in the mother’s diet.
Consider:
- Are you taking any laxatives, medicines, vitamins, iron tablets or other supplements?
- Do you drink lots of caffeinated drinks? Coffee, cola, tea and some pain relievers, cold remedies, weight control aids and diuretics contain caffeine. Chocolate contains a substance called theobromine that can have a similar effect to caffeine if you eat a lot.
- Have you recently eaten a new food or any particular food in large amounts?
- Are there any foods that you don’t like but have decided to eat during pregnancy or breastfeeding because you think they will be good for you and your baby?
- Are there foods that you crave? What foods do you snack on when you have a bad day?
Depending on how sensitive your baby is, removing or cutting down on the offending items in your diet may well solve the problem.
If your baby is also having infant formula or solids
The majority of babies don’t need anything other than mother’s milk before about six months — no infant formula, drinks or solids. Babies who have started solids can be sensitive to certain common foods until they are a little older.
Consider:
- Could your baby be reacting to the drinks or solid foods he is having?
- Is he on any medication or vitamin supplements?
- Could he be receiving other drinks such as infant formula or juice, or solid food, from anyone else without your knowledge?
- Infant formula or follow-on formula is usually cow’s milk-based and a common, avoidable cause of allergy. Babies do not need follow-on formula at all.
Removing the offending food from your baby’s diet for now should solve the problem; they may be able to tolerate it in a few months time. If you think your baby may be reacting to a prescribed medication that they have to take, speak to your doctor, who may be able to prescribe an alternative.
Common problem foods
5Common problem foods which may be eaten by a baby or a breastfeeding mother include:
- Milk and other dairy products such as butter, yoghurt, cheese, whey, casein, caseinate, lactose
- Egg
- Peanut
- Soy
- Wheat
- Fish
- Sesame seeds (in tahini and hummus)
- Lupin/lentils (including chickpeas which are in hummus)
- Shellfish; crustaceans (e.g. crab, lobster, crayfish, shrimp, prawn), molluscs (e.g. mussels, oysters, squid)
- Fenugreek is closely related to peanuts
- Tree nuts (almonds, hazelnuts, walnuts, cashews, etc.)
- Celery and celeriac
- Mustard
Common foods that can be involved in intolerance or irritation but not usually allergy:
- Sulphur dioxide and sulphites, benzoates, glutamate, salicylates, dietary amines
- Citrus fruits, strawberries, tomatoes
- Certain additives, artificial colourings, flavourings and preservatives
These can turn up in the most unexpected places so do check everything consumed including drinks and medicines. For example, some juice drinks contain milk, and wine can contain milk, egg or sulphites.
For example, some juice drinks contain milk, and wine can contain milk, egg or sulphites.
Cutting out suspected foods
If your baby is exclusively breastfed, you may need to follow an elimination – reintroduction diet. It can help to keep a food and symptom diary.
When eliminating major food groups take care to ensure you continue to eat a healthy and balanced diet. Your GP may be able to refer you to a dietician if you wish.
Only cut out one food at a time and allow 2–4 weeks to see if your baby’s symptoms improve. If there is no improvement in this time, then the food is unlikely to be the culprit and can be reintroduced3. Consider cutting out a different food.
If symptoms do improve, reintroduce the food slowly to confirm the food allergy. However, if your baby has previously experienced a severe or immediate reaction, ask your GP for specialist support before reintroducing the food.
Note: Usually a cow’s milk protein allergy (CMPA) predicts an allergy to other animal milks (e. g. goat or sheep milk), and in some cases soya. If you plan to cut out dairy you may wish to cut out other animal milks and soya at the same time, then reintroduce them each individually.
g. goat or sheep milk), and in some cases soya. If you plan to cut out dairy you may wish to cut out other animal milks and soya at the same time, then reintroduce them each individually.
Seek immediate medical help if your baby has shown anaphylactic signs, such as a rapidly developing rash, breathing difficulties, or swelling.
A note on eczema
Elimination – reintroduction diets should not be done due to the presence of eczema alone.
Some children who have a food allergy do have eczema, but most children who have eczema do not have a food allergy. If the only symptom is eczema it is unlikely to be caused by a food allergy. It is worth noting that frequently eating a particular food may mean a baby learns to tolerate it. If the food is stopped, for example during an elimination diet, there is a risk that tolerance may stop and an IgE mediated allergy (including possible anaphylaxis) can form. If you think your baby’s eczema is due to a food allergy it is best to speak with your GP about allergy testing or to get referred to an allergy specialist6.
Introducing solid foods
Human milk contains tiny traces of whatever foods a mother herself has been eating. This is the ideal way to prepare a baby gently for the eventual introduction of solids. The best foods for your baby are usually healthy foods selected from your diet. Solids can be introduced when your baby can sit up (with or without support) and starts reaching out for the food on your plate. For more information, see Starting Solid Food.
If your baby is under the care of a paediatrician for allergies, talk to your specialist team about how to introduce specific allergenic foods.
Body tolerance levels can change
Being allergic or intolerant to something means that your body is sensitised to it, but the symptoms you display may vary in each particular instance; sometimes you may not display any symptoms. Your body’s allergen tolerance level changes based on many factors including stress and your general health, so its ability to react to immune threats also varies. If your immune system is affected by more stressors than usual, you may show symptoms of an allergy/intolerance more readily.
If your immune system is affected by more stressors than usual, you may show symptoms of an allergy/intolerance more readily.
Seek support
It can be quite an effort to be an allergy detective with a fussy baby on your hands, so seek information and support. The good news is that small changes to your diet could make a big difference to a baby with a food allergy or intolerance.
An LLL Leader can help you determine the most likely cause of your baby’s symptoms. Local LLL groups are great for practical and moral support and you may find others there who have had similar experiences. Your GP or health visitor can help diagnose food allergy and refer you to specialist services for testing and advice.
Did you know?
- If a baby reacts when their mother drinks milk or has dairy products, this is a sensitivity to cow’s milk protein, not lactose intolerance.
- Most infant formulas contain cow’s milk, often referred to as whey based or casein based.
- Soya, the basis of some infant formulas, is also a common allergen.

- Infant formula may contain fish oils and vegetable oils (e.g. palm, rapeseed, coconut, sunflower).
- Medicines and supplements can contain other ingredients that are potentially allergenic.
- If you or a member of your immediate family has an allergy or intolerance, your baby is more likely to have one too1.
FAQs
Q. Do I have to give up breastfeeding if my baby is allergic to something in my milk?
A. No; eliminating the offending food from your diet will remove the allergen from your breast milk enabling you to continue breastfeeding if you wish to. See section Cutting out suspected food.
Q. Will my baby outgrow his food allergy?
A. Possibly; some children do, some do not. Children are most likely to grow out of cows’ milk, egg and soy allergies.
Q. I thought I was not meant to feed my baby egg/peanut/etc. until they were over 1 year old?
A. This was old advice. Recent research shows introducing allergenic foods from around 6 months old may help the baby to learn to tolerate the food. Introducing the food later can make it more likely that the baby will develop an allergy to the food.
Recent research shows introducing allergenic foods from around 6 months old may help the baby to learn to tolerate the food. Introducing the food later can make it more likely that the baby will develop an allergy to the food.
Q. What’s the difference between cow’s milk protein allergy (CMPA) and lactose intolerance?
A. True lactose intolerance (reduced capacity to digest lactose) is very rare in babies and is diagnosed within days of birth. Temporary lactose intolerance or lactose overload (too much lactose for the baby to digest) can cause tummy symptoms similar to an allergy. Lactose is produced in the breast, regardless of the mother’s diet. Seek support if you suspect your baby has symptoms of lactose overload. CMPA is an immune reaction and can cause symptoms in many body systems. Breastfeeding mothers of children with CMPA generally need to exclude all cow’s milk protein from their diet – including milk, cheese, yogurt etc. See section Cutting out suspected food.
Q. Should I avoid eating a food my baby is allergic to if I become pregnant again?
A. No; as long as you are not allergic to it and it is not one the foods you usually need to avoid in pregnancy (such as undercooked meat) eating a particular food in pregnancy has no effect on the development of allergy.
Q. Is my baby allergic to a food because I ate it whilst pregnant?
A. No; eating a particular food in pregnancy has no effect on the development of allergy.
Q. If I have another baby will it develop allergies too?
A. Possibly; if you have a sibling with allergies you are more likely to be genetically predisposed to develop allergies. However, having an older sibling decreases the risk of developing allergy.
Written by Sue Cardus, Robyn Halliday and mothers of La Leche League Great Britain
Endnotes
- Andreas, N., Kampmann, B., Le-Doare, K. Human Breast Milk: A review on its composition and bioactivity.
 Early Human Development, 2015; 91 (11): 629-635.
Early Human Development, 2015; 91 (11): 629-635. - Muraro, A et al. EACCI Food Allergy and Anaphylaxis Guidelines. Primary prevention of food allergy. Allergy, 2014;69(5):590-601.
- NICE Guideline [CG116]. Food allergy in under 19s: assessment and diagnosis, 23rd February 2011, https://www.nice.org.uk/guidance/cg116 (accessed 26th Jul 2020).
- NHS. Contact dermatitis, https://www.nhs.uk/conditions/contact-dermatitis/causes/ (accessed 26th Jul 2020).
- Muraro, A et al. EAACI Food Allergy and Anaphylaxis Guidelines. Diagnosis and management of food allergy. Allergy, 2014; 69 (8): 1008-25.
- Young, M. Editorial: Elimination Diets in Eczema—A Cautionary Tale. JACI: In Practice, 2016; https://www.jaci-inpractice.org/article/S2213-2198(15)00573-5/pdf
Further Reading
The Womanly Art of Breastfeeding. LLLI. London: Pinter & Martin, 2010.
BREASTFEEDING ANSWERS – A GUIDE
FOR HELPING FAMILIES: SECOND EDITION. . Mohrbacher, N. Nancy Mohrbacher Solutions inc., 2020.
. Mohrbacher, N. Nancy Mohrbacher Solutions inc., 2020.
MILK MATTERS: INFANT FEEDING AND IMMUNE DISORDER. Minchin, M. Geelong: Alma Publications, 2015.
BREASTFEEDING WORKS! EVEN WITH ALLERGIES. Noble, R. Brisbane: Complete Publishing, 2017.
Amazing milk
Is My Baby Getting Enough Milk?
My Baby Won’t Breastfeed
Rhythms and Routines
Safer Sleep & the Breastfed Baby
Starting Solid Food
Toddlers and Food
The Unhappy Breastfed Baby
Too Much milk
Thrush and Breastfeeding
Online information:
LLLGB website
Unicef Research on Allergies
NICE Guideline [CG116]. Food allergy in under
19s: Assessment and Diagnosis
GP Infant Feeding Network: Cow’s Milk Allergy
National Eczema Society
Anaphylaxis Campaign
CMPA Support
You can buy this information in printed form from our shop.
Copyright LLLGB 2020
Is your Baby Reacting to Breastmilk?
Read time: 8 minutes
What should I know about an allergy or intolerance in my breastfed baby?Learn the difference between an allergy and a food intolerance or sensitivity
Know the signs and symptoms of food allergy or intolerance in breastfed infants
Learn which foods are the most common allergens or culprits in food intolerances
How to manage your food intake to help alleviate your baby’s symptoms
Breastmilk is incredible – it offers a complete form of nutrition for infants, and offers a range of benefits for health, growth, immunity, and development. 1 The nutrients in your breastmilk come directly from what’s circulating in your blood, meaning that the nutrients and compounds you absorb from the food you eat are then passed along to your baby.
1 The nutrients in your breastmilk come directly from what’s circulating in your blood, meaning that the nutrients and compounds you absorb from the food you eat are then passed along to your baby.
While being truly allergic or reacting to something in mom’s milk is rare in babies, a small percentage of mothers do notice a difference in their babies’ symptoms or behavior after eating certain foods.
What’s the difference between an allergy and an intolerance or sensitivity?Sometimes these terms are used interchangeably, but an allergy and an intolerance/sensitivity are very different. According to the American Academy of Allergy Asthma and Immunology (AAAI), an allergy is when the immune system reacts to a food, whereas an intolerance happens during digestion.2 Allergies generally have more severe symptoms, often causing skin reactions or difficulty breathing. Food intolerances occur when we have difficulty digesting a food, which often result in gastro-intestinal symptoms.
With an allergy, the culprit food often needs to be taken out of the diet completely to avoid symptoms. Food intolerances however may allow for a small amount of the offending food to be eaten without any reactions. This is the ‘threshold’ amount: the lowest amount of the food you can eat without having symptoms.
Read more: Major Allergens: While Pregnancy and Breastfeeding
Which foods might cause an allergic reaction?In general, food allergens include cow’s milk, soy, eggs, peanuts, wheat, tree nuts, fish, and shellfish.3 In children, the most common allergens are peanuts, milk, tree nuts, and shellfish.4, 5
What are the symptoms of a food allergy in babies?
Food allergies affect about 7.6% of children in the United States.4
The most common symptoms of an allergy in breastfed infants are eczema (a scaly, red skin rash) and bloody stool (with no other signs of illness). You might also see hives, wheezing or other breathing problems, nasal congestion, swelling of a body part (tongue, lips, face), throat tightness, pale skin, vomiting or diarrhea. 6
6
If you notice any of these symptoms, be sure to call baby’s pediatrician right away. While you can likely manage most food allergies in your breastfed infant by changing your diet, there are some cases in which using a hypoallergenic formula may be required.
Here are some tips for Managing Gas in Breastfed Babies
Which foods might cause a food intolerance or sensitivity reaction?You may have heard that eating foods that make you gassy will also cause gastrointestinal distress for your baby, or that eating foods like onion, garlic and cruciferous vegetables will cause colic. While there is no significant data to support such an association, there are some mothers who do notice certain foods make their babies fussier than usual. This may be a food intolerance or sensitivity.
There is a much wider variety of foods that may trigger a reaction when it comes to food intolerances; but it’s important to note that food sensitivities in babies are much less common than food allergies.
Foods that may cause reactions include: Fructose, lactose and other FODMAPs (easily fermented carbohydrates found in a variety of foods), wheat, histamine (often found in processed meats, cheeses, and some produce), and food additives.7
What are the symptoms of a food intolerance in babies?
The most common symptom of a food sensitivity in babies is a change in their bowel habits. Extra gas, bloating, diarrhea or constipation, fussy after eating, mucous in the stool, or crying excessively may indicated baby is not doing well with a food you’re eating.
Note that if your little one has excessive crying that continues on a daily basis and lasts for long periods, that may indicate colic rather than food sensitivity.8 Talk with your pediatrician about this possibility, if eliminating various foods has no effect on your child’s symptoms.
Read: Managing Colic in Babies
What can I do if my baby is reacting to something in my diet?The ultimate goal is figuring out which food is affecting your baby. An elimination diet can help identify which food may be causing the allergy or food sensitivity.9 This means removing possible allergens from your diet for 2 to 3 weeks each while you continue breastfeeding.
An elimination diet can help identify which food may be causing the allergy or food sensitivity.9 This means removing possible allergens from your diet for 2 to 3 weeks each while you continue breastfeeding.
There are two ways to go about an elimination diet:
Take out one potential allergen or intolerant at a time: If there is one food strongly suspected as the culprit, you can choose to take out just that one food. Watch to see if your baby’s symptoms subside. Should baby’s symptoms get better, keep that food out of your diet. If baby’s symptoms remain the same over the course of 3 weeks, you can begin eating that food again and then eliminate a different allergen.
Take out all potential allergens or intolerants at once: If you are unsure which food is causing the problems, all allergens or possible culprit foods can be taken out for the 2 to 3 weeks and then added back in one at a time.
For a possible food intolerance or sensitivity, add one food back in over the course of 3 days – this is the challenge period. The first day eat a small amount, the second day eat a medium amount, the third day eat a larger amount. Doing it this way shows you if baby has a threshold. Sometimes you can eat a small amount of an offending food without it bothering your little one.
The first day eat a small amount, the second day eat a medium amount, the third day eat a larger amount. Doing it this way shows you if baby has a threshold. Sometimes you can eat a small amount of an offending food without it bothering your little one.
Remember that for a food allergy, it is likely the food must be taken out completely from your diet.
If your baby shows symptoms during any of the challenge days, stop the challenge and take the food back out of your diet. Don’t trial a new food until all your baby’s symptoms are gone. If there are no symptoms during the challenge period, you can eventually eat this food again! For now, take it back out of the diet after its 3 day challenge and wait to add it back in after you’ve challenged all culprit foods.10
Keep a good log of the foods you’ve challenged, symptoms, and amounts you’ve eaten!
You can continue breastfeeding despite the symptoms as long as your baby continues to grow and put on weight during this process.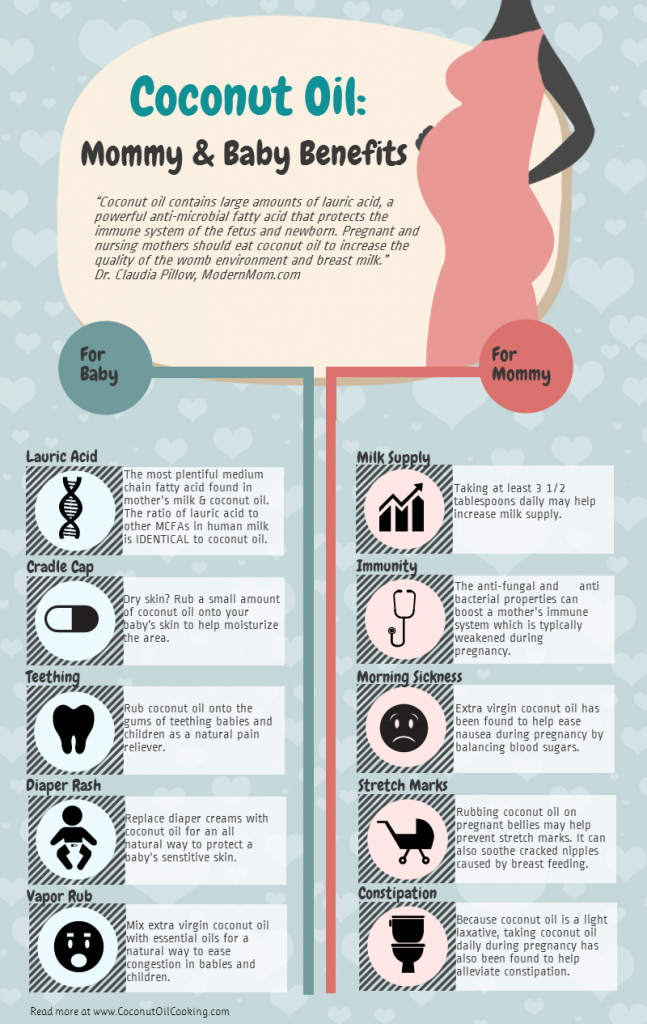
If you plan on trying an elimination diet, especially a multi-food elimination, be sure to work with a registered dietitian. This will help ensure you are still getting all the nutrition you and your baby need as well as help navigate hidden sources of allergens. Foods like milk, soy, and corn can hide in all sorts of pesky places.
Our Happy Baby Experts are dietitians and infant feeding specialists, they can help you meet your breastfeeding goals while keeping both you and baby happy and healthy. Chat with them now!
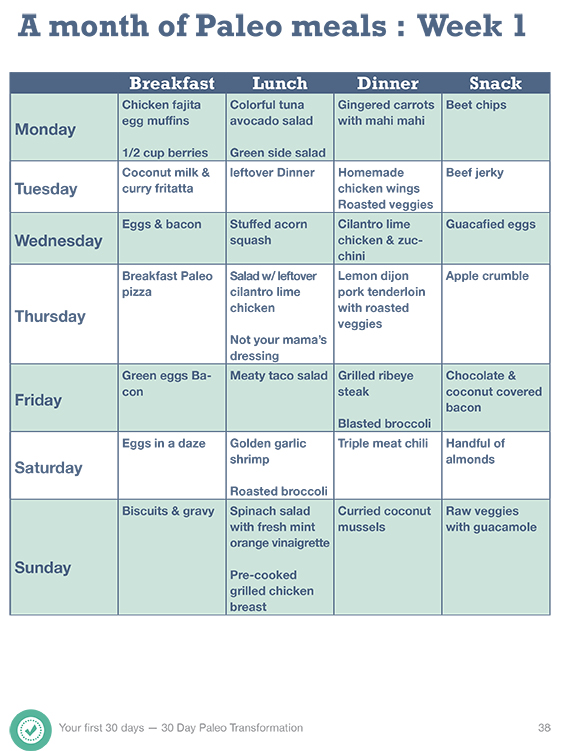
Trying to figure out what to eat while also taking out all allergens? Check out this Meal Plan for Allergen Free Eating.
Does breastfeeding help protect against allergies?While more research is needed, some studies have indicated that breastfeeding exclusively for at least four months may help to reduce the risk and severity of food allergies, even in families with a history of them.11, 12
So if your little one does show an intolerance or allergy early, know that it may resolve on its own before they turn one and that continued breastfeeding may help to safeguard against allergies later on.
Bring your baby in for a checkup. You’ll want to rule out any other causes for her symptoms, check baby’s growth and weight gain, and make sure baby is not losing excessive blood if your little one experiencing bloody stool. Your doctor can also discuss the possibility of confirming the presence of an allergy with a skin prick test.
If your child is diagnosed with a food allergy, remember to ask about reintroducing the food later. Most kids will grow out of food allergies, sometimes by their first birthday.
Keep a food and symptom journalWe know it’s hard to find time to eat in those first few months, let alone write down what made it into your mouth, but tracking your intake alongside your baby’s symptoms is a good way to shed light on any possible reactions.
Just remember that foods we eat remain in our bodies for long periods of time. So while a journal can be helpful to pinpoint the onset of symptoms when you first eat the offending food, know that your baby’s symptoms can persist for several days or up to 2 weeks, even if you don’t eat that particular food again.
So while a journal can be helpful to pinpoint the onset of symptoms when you first eat the offending food, know that your baby’s symptoms can persist for several days or up to 2 weeks, even if you don’t eat that particular food again.
If you notice an adverse reaction in your baby after you eat certain foods, try removing that food from your diet and watch for improvement.
Start with cow’s milk. The most frequent allergic reaction in breastfed babies is a milk protein allergy.5 Remember, it takes time for your body to be completely free of the offending food, so make sure you’ve removed all sources of the food for at least two weeks.
Seek supportChanging your diet can be hard. Finding a registered dietitian who can help make adjustments to your diet will help take some stress out of this process. Additionally, may lactation consultants are familiar with helping make these adjustments as well and also ensuring baby is getting what they need.
We know parenting often means sleepless nights, stressful days, and countless questions and confusion, and we want to support you in your feeding journey and beyond.
Our Happy Baby Experts are a team of lactation consultants and registered dietitians certified in infant and maternal nutrition – and they’re all moms, too, which means they’ve been there and seen that. They’re here to help on our free, live chat platform Monday through Friday, from 8am–6pm ET. Chat Now!
Read more about the experts that help write our content!
For more on this topic, check out the following articles:
How to Deal with Nursing Strikes while Breastfeeding
How much Should I Eat while Breastfeeding?
How do I Manage Gas in my Breastfeed Baby?
Which Foods Should You Avoid While Breastfeeding?
Food allergy in young children
- Main
- All about allergies
- Allergy in children
- Food allergies in young children - treat or outgrow?
Contents
How food allergies develop in babies
Food allergies in a child is a problem that can make significant adjustments to everyday life. This problem affects up to 6% of children under 2 years of age, according to the American Academy of Allergy, Asthma and Immunology (AAAAI). And at the age of 3 years, food allergies, according to WHO, already suffer up to 8% of children.
This problem affects up to 6% of children under 2 years of age, according to the American Academy of Allergy, Asthma and Immunology (AAAAI). And at the age of 3 years, food allergies, according to WHO, already suffer up to 8% of children.
However, among children under 5 years of age, the incidence of allergies is decreasing and is about 5%. This is due to the fact that some types of children's food allergies disappear on their own over time.
For example, up to 90% of children outgrow cow's milk and egg allergies. On the other hand, only 10-20% of children get rid of peanut allergy as they grow older. Food reactions to nuts, fish, or seafood are also likely to persist into adulthood.
To find out if the child has outgrown the allergy, it will be necessary to periodically undergo appropriate testing.
But, even if the baby outgrows one allergy, in the future the disease can "return" with such allergic conditions as asthma or hay fever. This phenomenon is called allergic or atopic march.
This phenomenon is called allergic or atopic march.
In addition, according to scientists, some factors may increase the likelihood of allergic reactions.
For example, one of the hypotheses is hygiene, based on the fact that a significant increase in the number of allergic diseases is observed in developed countries, where hygiene is better and there are relatively fewer infections.
The use of antibiotics in infancy may also be associated with an increased risk of subsequent development of allergies. This assumption is based on the notion that antibiotics deplete the normal gastrointestinal bacterial flora that would normally suppress the Th3 response.
Along with this, scientists believe that some factors may, on the contrary, reduce the risk of developing allergies in a child .
So, according to the results of research, food allergies in children occur less often if the baby remains exclusively breastfed for at least the first six months of his life.
The intake of probiotics by breastfeeding mothers or babies as a supplement to infant formula can also help reduce the risk of developing allergies.
In addition, early gradual exposure to allergens such as peanuts also prevents further allergies to them.
But new foods should be introduced into the baby's diet in turn: one at a time and with an interval of two or three days, or even less often. In this case, any reaction should be recorded, and, if necessary, reported to the doctor.
You also need to know that food reaction, as a rule, does not appear at the first acquaintance with the allergen. In most cases, the reaction is preceded by a sensitization process - it is formed by the preliminary exposure to the allergen. It occurs directly or through breast milk.
Causes of food allergies in children
Whether a child develops a food allergy to a particular food depends on many factors.
First, a baby is more likely to develop this problem if the family has a family history or other allergic conditions such as asthma, hay fever or eczema.
The tendency to develop allergies to food and inhalant allergens is mainly genetically determined. The chance of developing a food allergy in a child whose parents do not have a history of allergies is 20%. If one of the parents has an allergy, the chances increase to 30-50%. If both parents suffer from allergies, then with a probability of 60% - 80% the child will also have this problem.
The connection between food allergies and eczema is also quite strong.
Atopic children have a genetic predisposition to produce immunoglobulin E (IgE) antibodies to various food and inhalant allergens to which they are exposed. Further influence of IgE, which is fixed on mast cells, leads to the release of chemical mediators that cause both an immediate reaction and a delayed reaction.
Atopic dermatitis (AD), IgE-mediated food allergy, asthma and allergic rhinitis are often interrelated. They may coexist, or as one condition improves, the other may evolve into the already mentioned “allergic march. ”
Babies who develop severe eczema before three months of age are more likely to have food allergies. Simply put, the earlier the baby has eczema, and the greater the birth weight, the more likely it is that the baby will develop a food allergy.
approximately 90% of all food allergies are caused by the following eight products:
· Milk
A common food allergy in infants and young children is a reaction to milk, eggs, peanuts and nuts such as hazelnuts, walnuts and almonds.
According to statistics, 1.6-7% of children are allergic to cow's milk, and about 2% of children under the age of three are allergic to eggs and peanuts.
Peanuts, tree nuts, fish and shellfish cause the most serious reactions.
Due to cow's milk protein allergy, infants may develop allergy to formula fed or supplemented. Also, formula-fed babies may develop an allergy to soy.
Food allergy symptoms in young children
Most food allergies are of the immediate type. In this case, food allergy in a child appears immediately - most often within 15 minutes after eating, or within 2 hours.
The main symptoms of an immediate food allergy are:
urticaria (most commonly around the mouth, nose and eyes, but this rash can spread all over the body)
mild swelling of the lips, eyes and face
runny or stuffy nose, sneezing, watery eyes
itchy mouth and throat irritation
nausea, vomiting and diarrhoea.
If a child has a severe reaction, wheezing, breathing problems, swelling of the throat and tongue, and a sudden drop in blood pressure may occur. Such a severe reaction is called anaphylaxis, and its extreme, severe manifestation, is anaphylactic shock . This is a particularly life-threatening condition that is most commonly caused by foods such as peanuts, nuts, fish, and seafood. At the first sign of anaphylaxis, you should immediately seek medical help and inject epinephrine.
However, sometimes an allergy does not make itself felt immediately, but after a delay
Therefore, the problem is more difficult to notice. But this type of reaction is becoming more common. First of all, a delayed reaction is typical for products such as milk and soy. Such an allergy has several other manifestations.
The main signs of delayed or non-IgE mediated food allergy in a child are:
reflux
colic
diarrhea
constipation
blood or mucus in stool
poor weight gain and short stature
moderate to severe eczema, common in children with milk allergy
Is it possible to cure a food allergy in a child
The answer to this question is ambiguous. On the one hand, today there are no official cures for food allergies for children. On the other hand, as mentioned at the beginning, a child may very likely outgrow an allergy to certain foods.
Until then, the best option would be abstaining from the allergen and periodically undergoing special tests to diagnose food allergies.
Children with mild allergies, for example to eggs, can sometimes eat foods containing baked eggs. If your child has a severe allergy to, for example, nuts, they may need to be avoided in any form or amount. More precisely, this can be determined by a molecular allergy test.
In milder cases of allergy, children are prescribed antihistamine drops to relieve general allergy symptoms.
Antihistamines may be used to treat symptoms of an allergic reaction such as hives, runny nose, or stomach pain. Topical ointments may be effective in treating skin manifestations. But when a child has a severe reaction in the form of anaphylaxis, such symptomatic treatment does not work. Therefore, it is necessary to inject adrenaline. The latter is available as auto-injectors.
In any case, consultation with an allergist is indispensable. Moreover, sometimes another problem can be hidden behind the symptoms of an allergy. For example, it may be intolerance to milk proteins or lactose milk sugar. Usually, food intolerance in children is manifested by indigestion and can last for several weeks.
sources of information:
1. https://www.hopkinsmedicine.org/health/conditions-and-diseases/food-allergies-in-children?amp=true
/www.nhs.uk/conditions/pregnancy-and-baby/food-allergies-in-babies-and-young-children/
3. https://www.ncbi.nlm.nih.gov/pmc/articles /PMC2805592/
4. https://www.healthychildren.org/English/healthy-living/nutrition/Pages/Food-Allergies-in-Children.aspx
5. https://pubmed.ncbi.nlm. http://nih.gov/27276868/
6. https://www.webmd.com/parenting/baby/introducing-new-foods
7. https://www.babycentre.co.uk/a555826/food-allergies-in-babies
8. https://www.parents.com/health/allergies/food/all-about-food-allergies-in-babies/
9. https://kidshealth.org/en/parents/food-allergies. html
Subscribe to new articles about allergies and their treatment!
I give JSC "Farmak" consent to the processing of my personal data (with the full text of the consent I have read and accept)
Food allergies, food intolerances and pseudo-allergies: what are the signs and causes
Views: 33914 Published: / Updated:
- Allergy
General
There are various reasons why food can make you feel bad, the most well-known being food allergies and food intolerances. What both allergies have in common is that they involve the immune system. However, there are some differences in how the immune system implements its response and what changes this results in.
Immunoglobulins are specific proteins produced in response to antigens. The main function of immunoglobulins is the binding and removal of dangerous antigens: bacteria, viruses, allergens. Immunoglobulins are also known as antibodies. There are five main types of antibodies (Ig): A, G, M, E, and D. B-lymphocytes, a special type of white blood cell, produce antibodies by switching from one type to another. B-lymphocytes are part of the adaptive immune system.
Immunoglobulins realize the secondary immune response.
Classic IgE food allergy
A classic allergy occurs when the immune system produces specific IgE antibodies. Subclass E antibodies result in an immediate allergic reaction.
A typical example of an allergic type of reaction is a food allergy to peanuts. When a person with an allergy consumes peanuts for the first time, B-lymphocytes are exposed to peanut allergens. B cells begin to produce IgE antibodies to fight the "infection" of the peanut. For the body, peanuts are poison, not food.
IgE antibodies are created specifically to protect the body from peanuts, therefore they are called specific. Peanut IgE antibodies bind to allergens and attach to mast cells. Mast cells are a type of white blood cell that contain histamine and other markers of inflammation. The inflammatory response is designed to protect the body by limiting the action of the allergen.
In mast cells, IgE antibodies wait until the next interaction with peanuts. When a person repeatedly consumes peanuts, IgE antibodies signal mast cells to release histamine and other compounds. Histamine and other compounds cause allergy symptoms such as itching and inflammation, and swelling.
Allergy symptoms appear within seconds or minutes after contact with the allergen: itching, rash, watery eyes, severe swelling, difficulty breathing or anaphylactic shock in severe cases.
Symptoms may be seasonal, as in allergies due to pollen or mold, or year-round, as in food allergies. Allergy symptoms can range from mild to severe. Allergic reactions are especially dangerous for children, since their immune system is not fully formed until 8-12 years of age.
The total IgE test is performed as a first level test for allergies. Elevated values indicate an allergic nature of the disease or parasitic infections. The next step is the determination of specific IgE. These tests are needed to confirm the allergic nature of the disease. If a person is suspected of being allergic to several food components, it is recommended to undergo a full allergological examination.
Food intolerance
A food intolerance is an adverse reaction to a food without an antigen-antibody response. Food intolerance is a collective term that combines various conditions, but in which the same manifestations are observed as with classical allergies.
Food intolerance has symptoms similar to allergic reactions, but delayed in time. Its symptoms may appear immediately or 1-3 days after the trigger meal. Therefore, the connection food ↔️ reaction is not always so noticeable.
The immune system does not take part in the development of food intolerance. Food intolerance reactions are not an independent disease, but only mask the problem of a deeper order. Only a doctor can figure out the reasons.
The difficulty in diagnosing food intolerance lies in the delayed symptoms of the disease and the lack of specificity. Symptoms may appear immediately or three days or more after eating the trigger food.
Clinical manifestations range from headaches and nausea to depression, anxiety and hyperactivity, or fatigue, bloating or mood changes after eating. Dark circles under the eyes, not associated with sleep and wakefulness, also indicate a negative reaction of the liver to food, especially in children. Most people live with these symptoms sometimes for years.
Adults are more likely to develop food intolerances than children. As a rule, people with pathology of the gastrointestinal tract, metabolic disorders, smokers constitute a risk group for food intolerance.
Determining which food triggers which symptoms is difficult due to delayed reactions. The IgG test helps to localize and limit the list of triggers.
Not all food intolerances are related to the immune system. Therefore, it is not always inappropriate to link IgG to food intolerance in general.
The most common cause of food intolerance is enzyme deficiency. In children, the lack of enzymes is the result of the immaturity of enzyme systems, in adults - the pathology of the pancreas, inflammatory bowel diseases, autoimmune conditions.
Deficiency of certain gastrointestinal enzymes leads to adverse reactions such as flatulence.
Flatulence symptoms:
- diarrhea;
- swelling;
- skin rash;
- headaches;
- nausea;
- fatigue;
- abdominal pain;
- runny nose.
Celiac disease and lactase deficiency - two bright states of food intolerance.
Celiac disease and lactase deficiency are the most striking conditions in which a certain relationship between consumed products and the frequency of side effects has been revealed.
Celiac disease or celiac disease is an autoimmune disease in which the immune system attacks its own tissues. However, this is not an allergy. Reactions caused by gluten affect the villi of the intestinal wall, which leads to their atrophy.
In lactase deficiency, there is a deficiency of the enzyme lactase, which breaks down milk sugar. This enzyme is active in young children, as they are predominantly breastfed. In adults, enzyme activity is reduced and this is considered the norm. Due to the fact that the activity of the enzyme is reduced, side effects occur, the degree of which varies from mild to severe. Intolerance occurs due to malabsorption and is associated with the intake of a regular glass of milk.
Elimination diet leads to better well-being.
Other groups of substances that cause abdominal discomfort are tyramine and sulfites. Tyramine-containing foods can cause migraines, and in people taking MAO drugs, cause a sharp rise in blood pressure. Sulfites are used as preservatives, so they are ubiquitous. Sulfites can cause asthma attacks or symptoms such as: abdominal pain, diarrhea, nausea, vomiting, wheezing, hives, swelling.
Pseudoallergic reactions
This type of reaction has similar manifestations as an allergy, but differs in other mechanisms of formation.
Pseudo-allergic reactions can be explained by the activation of inflammatory or anaphylactic mechanisms not associated with antigen-specific immune reactions. These reactions can be induced by the following agents: direct mast cell activators, complement activators, and non-steroidal anti-inflammatory drugs. These substances in the human body can cause a number of physiological and pathological reactions, leading to the appearance of symptoms of pseudo-allergic reactions, such as nausea, dermatitis, hypotension, anaphylactic shock.