Baby irritable after feeding
How to Calm a Fussy Baby: Tips for Parents & Caregivers
Log in | Register
Ages & Stages
Ages & Stages
Here are ways you can try to comfort a crying baby. It may take a few tries, but with patience and practice you'll find out what works and what doesn't for your baby.
Swaddle your baby in a large, thin blanket (ask your nurse or child's doctor to show you how to do it correctly) to help them feel secure.
Hold your baby in your arms and place her body on their left side to help digestion or stomach for support. Gently rub their back. If your baby goes to sleep, remember to always lay her down in her crib on her back.
Turn on a calming sound.
Sounds that remind babies of being inside the womb may be calming, such as a white noise device, the humming sound of a fan, or the recording of a heartbeat.
Walk your baby in a body carrier or rock them. Calming motions remind babies of movements they felt in the womb.
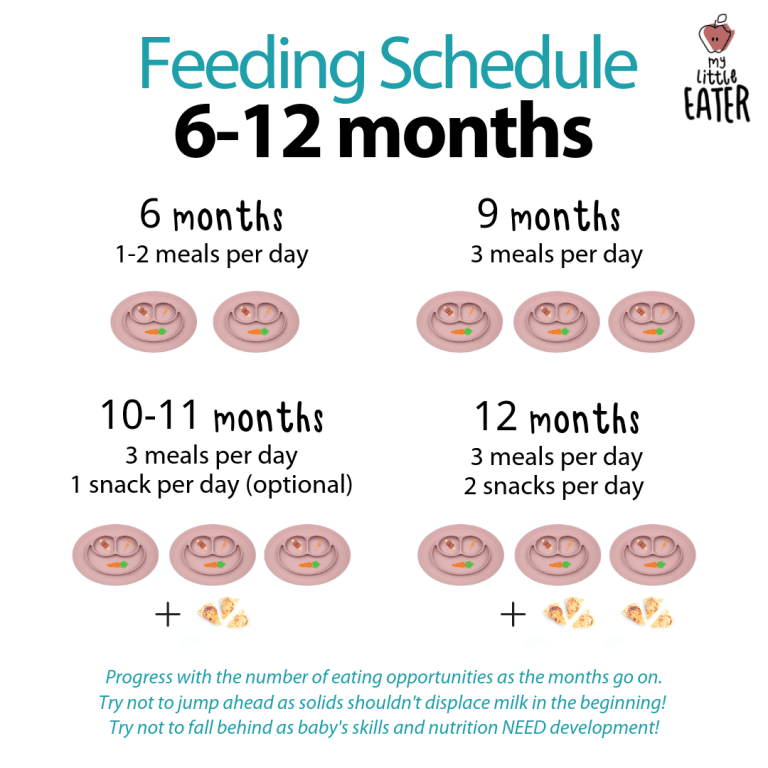
Avoid overfeeding your baby because this may also make them uncomfortable. Try to wait at least 2 to 2½ hours from the beginning of one feeding to the next.
If it is not yet time to feed your baby, offer the pacifier or help your baby find their thumb or finger. Many babies are calmed by sucking.
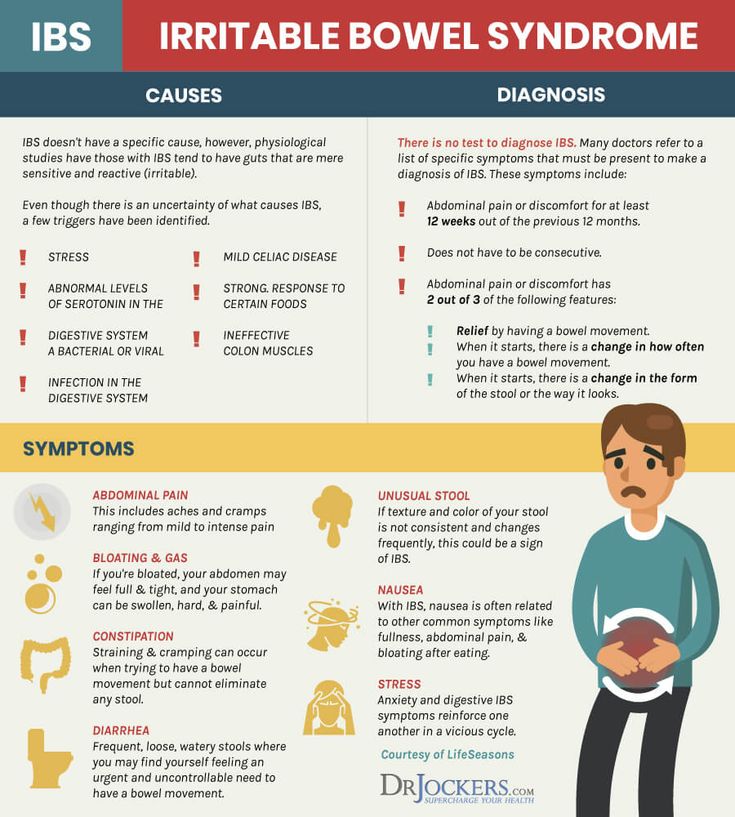
If food sensitivity is the cause of discomfort, a change in diet may help.
For breastfed babies: Moms may try changing their own diet. See if your baby gets less fussy if you cut down on milk products or caffeine. If there is no difference after making the dietary changes, resume your usual diet. Avoiding spicy or gassy foods like onions or cabbage has worked for some moms, but this has not been scientifically proven.
For bottle-fed babies: Ask your child's doctor if you should try a different formula. This has been shown to be helpful for some babies.
Keep a diary of when your baby is awake, asleep, eating, and crying. Write down how long it takes your baby to eat or if your baby cries the most after eating. Talk with your child's doctor about these behaviors to see if their crying is related to sleeping or eating.
Limit each daytime nap to no longer than 3 hours a day.
 Keep your baby calm and quiet when you feed or change themr during the night by avoiding bright lights and noises, such as the TV.
Keep your baby calm and quiet when you feed or change themr during the night by avoiding bright lights and noises, such as the TV.
Checklist for what your baby may need:
Here are some other reasons why your baby may cry and tips on what you can try to meet that need. If your baby is…
Hungry. Keep track of feeding times and look for early signs of hunger, such as lip-smacking or moving fists to his mouth.
Cold or hot. Dress your baby in about the same layers of clothing that you are wearing to be comfortable.
Wet or soiled. Check the diaper. In the first few months, babies wet and soil their diapers a lot.
Spitting up or vomiting a lot. Some babies have symptoms from gastroesophageal reflux (GER), and the fussiness can be confused with colic.
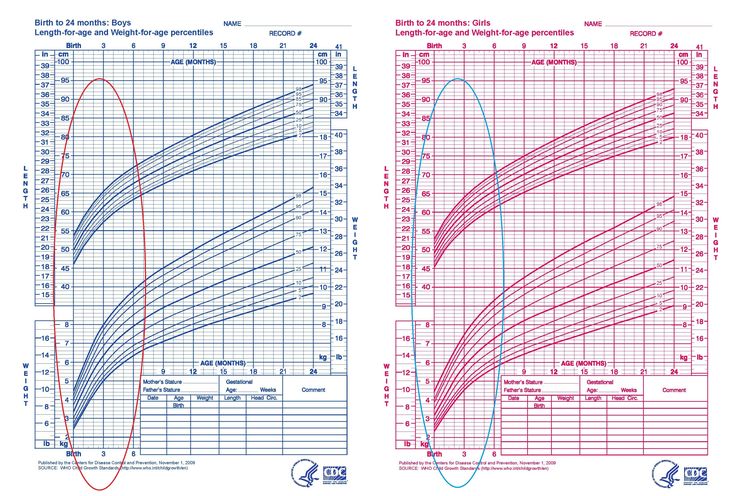
 Contact your child's doctor if your baby is fussy after feeding, has excessive spitting or vomiting, and is losing or not gaining weight.
Contact your child's doctor if your baby is fussy after feeding, has excessive spitting or vomiting, and is losing or not gaining weight. Sick (has a fever or other illness). Check your baby's temperature. If your baby is younger than 2 months and has a fever, call your child's doctor right away. See Fever and Your Baby for more information.
Overstimulated. Try ways to calm your baby mentioned above.
Bored. Quietly sing or hum a song to your baby. Go for a walk.
Why parents & caregivers need breaks from crying babies:
If you have tried to calm your crying baby but nothing seems to work, you may need to take a moment for yourself. Crying can be tough to handle, especially if you're physically tired and mentally exhausted.
Take a deep breath and count to 10.
Place your baby in a safe place, such as crib or playpen without blankets and stuffed animals; leave the room; and let your baby cry alone for about 10 to 15 minutes.
While your baby is in a safe place, consider some actions that may help calm you down.
Listen to music for a few minutes.
Call a friend or family member for emotional support.
Do simple household chores, such as vacuuming or washing the dishes.
If you have not calmed after 10 to 15 minutes, check on your baby but do not pick up your baby until you feel you have calmed down.
When you have calmed down, go back and pick up your baby. If your baby is still crying, retry soothing measures.
Call your child's doctor. There may be a medical reason why your baby is crying.
Try to be patient. Keeping your baby safe is the most important thing you can do. It is normal to feel upset, frustrated, or even angry, but it is important to keep your behavior under control. Remember, it is never safe to shake, throw, hit, slam, or jerk any child—and it never solves the problem!
More information:
- Responding to Your Baby's Cries
- Colic Relief Tips for Parents
- A Parent's Guide To Safe Sleep
- Remedies for Spitty Babies
- Abusive Head Trauma: How to Protect Your Baby
- Last Updated
- 3/21/2022
- Source
- Crying and Your Baby: How to Calm a Fussy or Colicky Baby (Copyright © 2016 American Academy of Pediatrics)
The information contained on this Web site should not be used as a substitute for the medical care and advice of your pediatrician.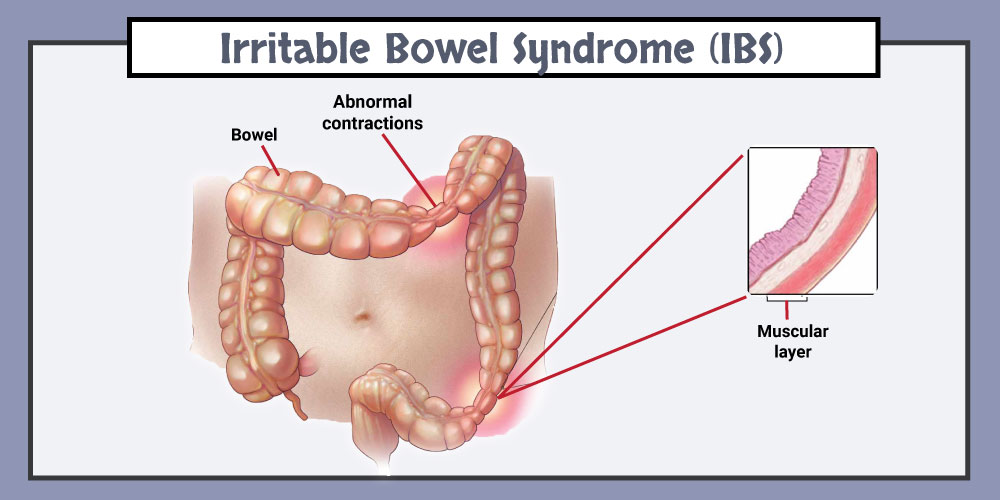 There may be variations in treatment that your pediatrician may recommend based on individual facts and circumstances.
There may be variations in treatment that your pediatrician may recommend based on individual facts and circumstances.
Baby Cries After Feeding: What Should I Do?
Medically reviewed by Karen Gill, M.D. — By Chaunie Brusie on October 3, 2018
My daughter, the “crier”
My second daughter was what my oldest fondly referred to as a “crier.” Or, in other words, she cried. A lot. The crying with my baby girl seemed to intensify after every single feeding and particularly at night.
It was those hellish hours between darkness and dawn when my husband and I would take turns walking around the house with her in our arms, praying and, mostly in my case, sobbing because we couldn’t console our baby.
I didn’t know it then in my sleep-deprived state, but my daughter’s crying after feedings wasn’t that uncommon. In combination with her frequent spitting up, it was pretty much a classic textbook case of colic.
Colic
Colic, in technical terms, simply means a “crying, fussy baby that doctors can’t figure out.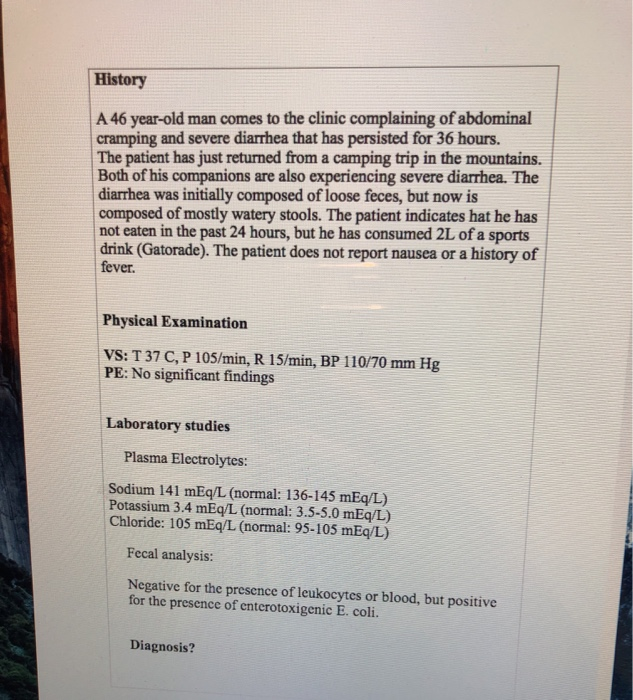 ”
”
OK, so that’s not really the definition, but in essence, that’s what it boils down to. The British Medical Journal (BMJ) lists one criterion for colic: A baby that cries for at least three hours a day, three or more days a week, and is under 3 months old. Check, check, and check.
There isn’t one single known cause of colic. Even the actual clinical incidence of colic, estimated by BMJ to be around 20 percent of all babies, can be tricky.
Acid reflux
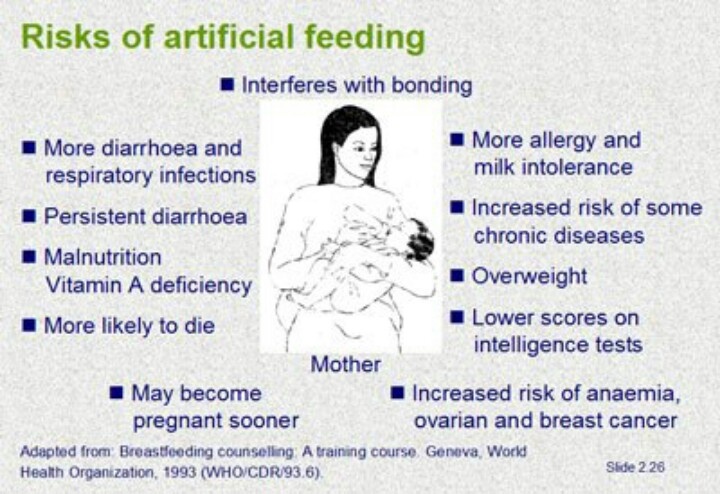
One of those causes of crying after feeding and spitting up in babies is actually acid reflux. This condition is known as gastroesophageal reflux disease (GERD) if it also causes significant symptoms such as poor weight gain.
When my “crier” daughter was 5, she frequently complained of her stomach hurting and as a result, had to undergo a series of testing with a gastroenterologist, a doctor that specializes in the GI system.
At our first appointment, the very first question he asked me was if she had colic as a baby and if she spit up a lot, to both of which I practically shouted, “Yes! How did you know?!”
He explained that acid reflux or GERD can manifest as symptoms similar to colic in babies, stomach pain in school-aged children, and later as actual heartburn pain in adolescents.
While many infants spit up, fewer have actual GERD, which can be caused by an underdeveloped flap between the esophagus and stomach or a higher-than-normal production of stomach acid.
In most cases, a diagnosis of infant reflux is simply based on your baby’s symptoms. If your doctor suspects a severe case however, there are several different tests that actually diagnose infant reflux.
Testing can involve taking a biopsy of your baby’s intestine or using a special type of X-ray to visualize any affected areas of obstruction.
Food sensitivities and allergies
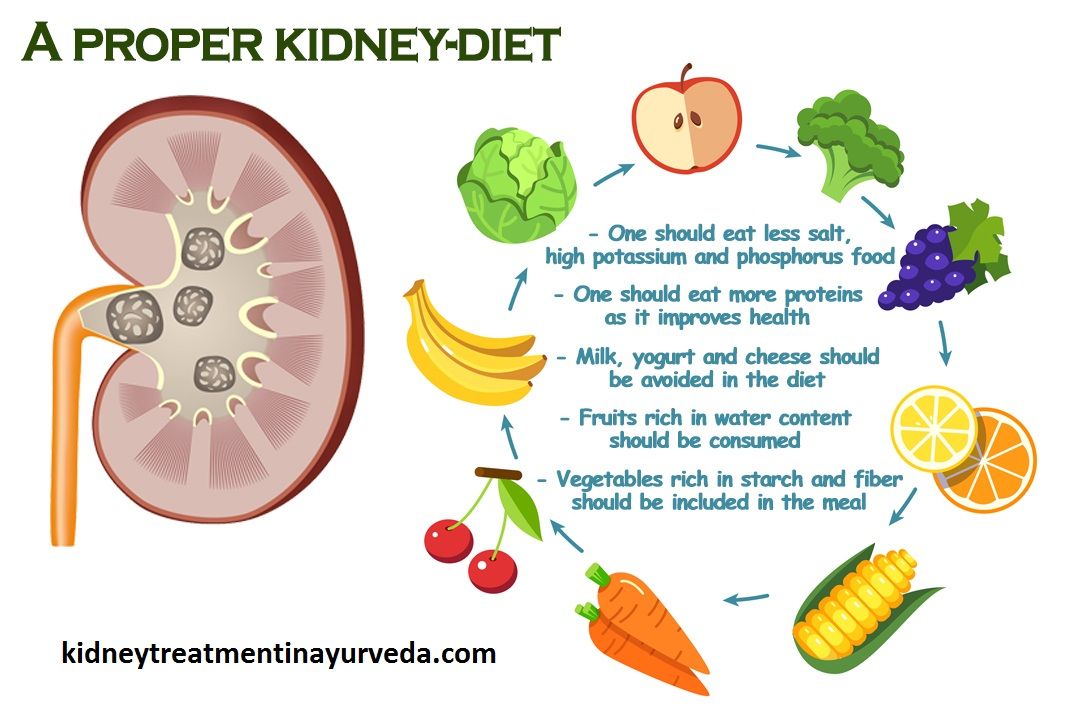
Some babies, especially breastfed babies, may be allergic to certain food particles that their mothers are eating.
The Academy of Breastfeeding Medicine notes that the most common offender is cow’s milk protein in the mother’s milk, but even a true allergy is very rare. Only about 0.5 to 1 percent of exclusively breastfed babies are thought to be allergic to cow’s milk protein.
The other most common culprits, according to the ABM, are egg, corn, and soy, in that order.
If your baby is displaying symptoms of extreme irritability after feedings and has other symptoms, such as bloody stools (poop), you should speak with your healthcare provider about getting them tested for allergies.
Aside from a true allergy, there’s also been some evidence that following a low allergen diet while breastfeeding (essentially avoiding those top allergy foods, such as dairy, eggs, and corn) may be beneficial for infants with colic.
Strict elimination diets can have their own risks, so speak with your doctor before significantly changing your diet.
In our situation, I found that dairy, caffeine, and certain seeded fruit exacerbated my daughter’s crying and spitting up. By eliminating those foods and substances from my diet, I was able to help lessen her discomfort.
If you have a baby with colic, you might want to try anything at all to help ease your baby’s crying. If you’re curious to see if your diet has any effect, you can start by logging your food in a food journal and writing down your baby’s reactions after each meal.
Next, you can eliminate one food at a time and see if reducing your intake of certain foods seems to make a difference in your baby’s behavior. If you hit on one you feel helps your baby to cry less, this does not mean they will not be able to eat that food in the future.
Just be sure to keep in mind that a true allergy is rare. Also, be sure to monitor for any additional symptoms, such as blood in your baby’s poop.
Gas
If your baby is crying a lot after every feeding, it may simply be a buildup of air swallowed while eating. It’s thought that bottle-fed babes in particular may be more prone to swallowing a lot of air during a feeding. This can trap gas in their stomachs and be uncomfortable.
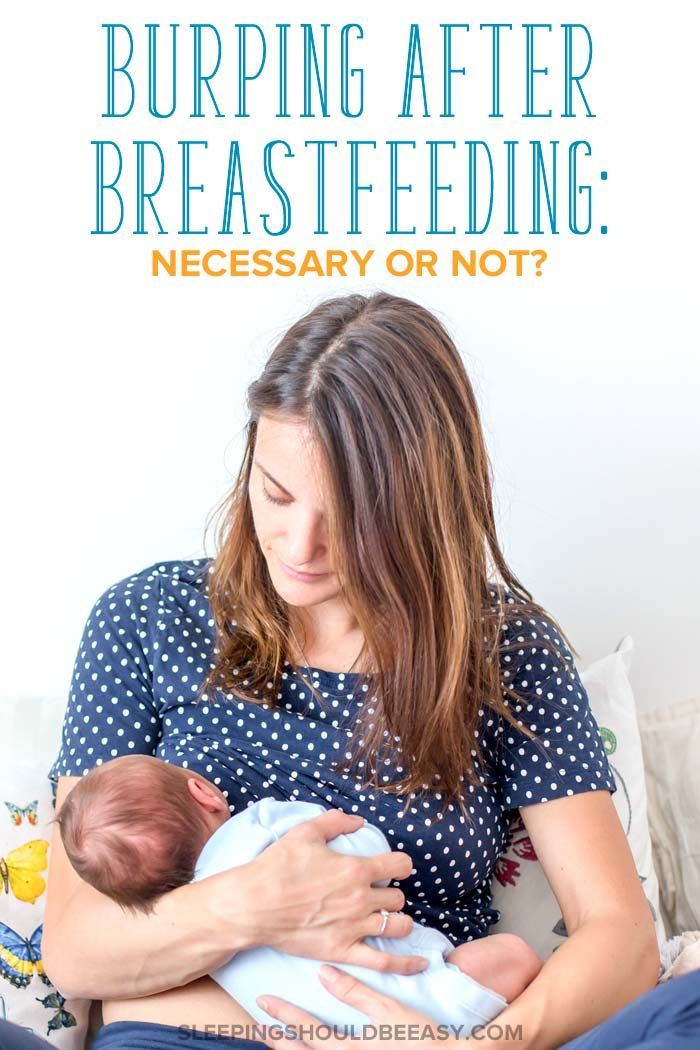
In general, breastfed babies swallow less air while eating simply due to the way they eat. But every baby is different and even breastfed babies may need to be burped after a feeding.
Trying keeping your baby upright after a feeding and burping gently from the bottom of their back and up through the shoulders to work the gas bubbles up and out.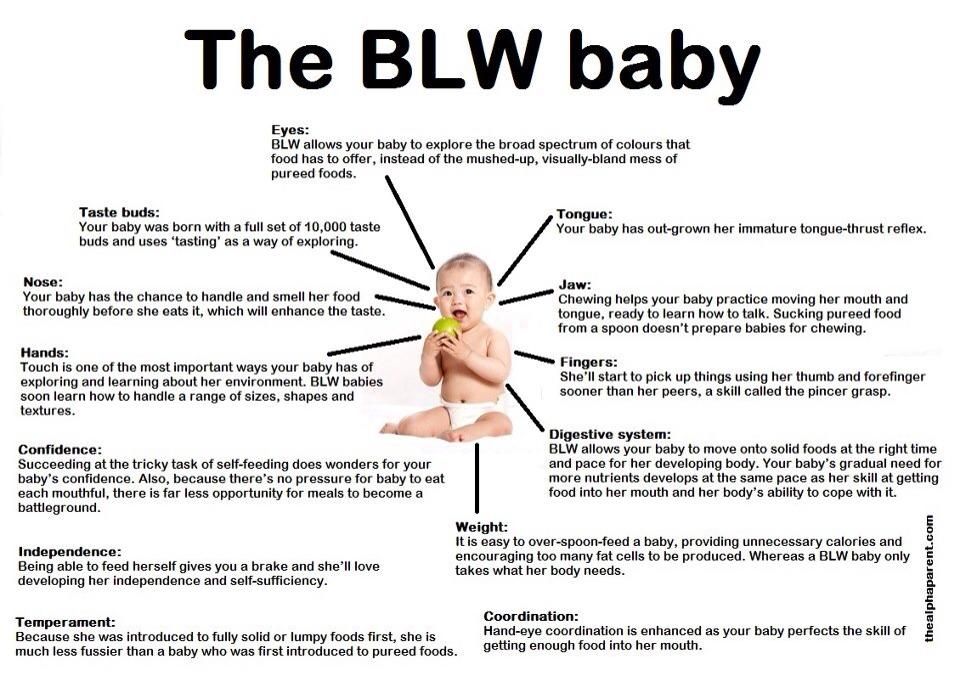 Also check out this illustrated guide to burping a sleeping baby.
Also check out this illustrated guide to burping a sleeping baby.
Formula
If your baby is formula-fed, swapping out the formula you use may be a simple solution to a crying baby after feedings. Every formula is a little bit different and certain brands make formulas for more sensitive baby tummies.
If you decide to try this, talk to your baby’s pediatrician about whether an elemental formula would be a good choice to try for a week. If you try one different brand and you see no change in your baby’s fussiness, continuing to try different brands is unlikely to help.
Takeaway
Colic, along with a few other common conditions, might be the culprit if you too have a “crier” on your hands.
If your baby doesn’t find relief after dietary changes or additional burping, then make an appointment to see their doctor.
Share on Pinterest
Chaunie Brusie, BSN, is a registered nurse with experience in labor and delivery, critical care, and long-term care nursing.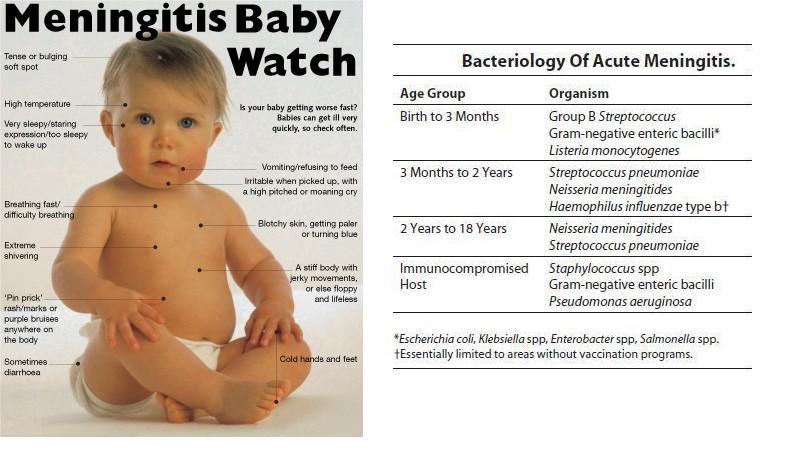 She lives in Michigan with her husband and four young children, and is the author of the book “Tiny Blue Lines.”
She lives in Michigan with her husband and four young children, and is the author of the book “Tiny Blue Lines.”
Last medically reviewed on October 3, 2018
- Parenthood
- Baby
- 06 Months
How we reviewed this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- ABM clinical protocol #24: Allergic proctocolitis in the exclusively breastfed infant. (2011). DOI:
10.1089/bfm.2011.9977 - Harrel MC, et al. (2015). Is there a correlation between maternal diet in breastfeeding mothers and infantile colic? DOI:
10.1097/01.EBP.0000541032.94135.ca - Mayo Clinic Staff. (2018). Infant reflux.
mayoclinic. org/diseases-conditions/infant-acid-reflux/diagnosis-treatment/drc-20351412
org/diseases-conditions/infant-acid-reflux/diagnosis-treatment/drc-20351412 - Rosen LD, et al. (2007). Complementary, holistic, and integrative medicine.
pedsinreview.aappublications.org/content/28/10/381 - Saavedra MA, et al. (2003). Infantile colic incidence and associated risk factors: A cohort study. .
ncbi.nlm.nih.gov/pubmed/14502331 - Sung V, et al. (2014). Treating infant colic with the probiotic Lactobacillus reuteri: Double blind, placebo controlled randomised trial. DOI:
10.1136/bmj.g2107 - Symptoms & causes of GER and GERD in infants. (2015).
niddk.nih.gov/health-information/digestive-diseases/acid-reflux-ger-gerd-infants/symptoms-causes
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Current Version
Oct 3, 2018
Written By
Chaunie Brusie
Edited By
Nizam Khan (TechSpace)
Medically Reviewed By
Karen Richardson Gill, MD
Share this article
What to do if the child has increased irritability.
 June 25, 2020 and emotional overload), as well as premature birth, by caesarean section, or in difficult natural childbirth. Irritability can be a response to the environment or excessive demands on the child, without taking into account the age and individual characteristics of the psyche.
June 25, 2020 and emotional overload), as well as premature birth, by caesarean section, or in difficult natural childbirth. Irritability can be a response to the environment or excessive demands on the child, without taking into account the age and individual characteristics of the psyche.
Up to 3 years any reason - improper diet, loud noises, bright lights, uncomfortable clothes, change of scenery, manifestation of negative emotions of adults - can cause irritation, tearfulness, sleep problems, and rapid fatigue of the child. What can parents do?
- Try to eliminate discomfort and calm the child as soon as possible. Ensure compliance with the daily routine, proper nutrition, physical and psychological stress, adequate to his age and condition. Don't try to build endurance and endurance in a young child, this will only make him more uncomfortable and make it harder to return to an emotionally stable state.
- Prepare the child in advance for any changes, tell and explain what will happen, soften the content of unpleasant information. For example, tell us why you need to go to the doctor and why it is good, when and for what reason guests will come to you, how much time the child will spend without you (with a grandmother or a nanny), what he will do in a children's institution. If it's time to end the game and go to bed, tell them that the toys are tired, look sleepy and suggest putting them to bed first, and then going to bed yourself.
For example, tell us why you need to go to the doctor and why it is good, when and for what reason guests will come to you, how much time the child will spend without you (with a grandmother or a nanny), what he will do in a children's institution. If it's time to end the game and go to bed, tell them that the toys are tired, look sleepy and suggest putting them to bed first, and then going to bed yourself.
- Keep calm yourself, do not get infected by the child's emotions. While the parent is calm, he is able to influence the situation and help the child cope with emotions. Do not show your fear or disappointment, do not frighten the child with suggestions of what might happen, and do not tire him with moralizing.
Preschool age. The older the child becomes, the more important the factors of education become in the development and consolidation of irritability, so parents should pay attention to the parenting strategies used and their own behavior, which the child can copy.
- Be an example of constructive conflict resolution and respect for all family members. Do not be afraid to apologize if you were wrong or said hurtful words in the heat of the moment. Learn to switch your emotional state, recognize and prevent outbursts of irritation. Watch your psychological health, do not bring yourself to a state of exhaustion and "driven".
- If your child is anxious and reacts violently to failures, give him more independence in situations that do not threaten his health, do not surround him with excessive care. The experience of overcoming difficulties is important for the child, this gives him confidence in his abilities.
- At the same time, demand a respectful attitude towards elders, observance of the daily routine, rules of courtesy and norms of behavior in public places. Otherwise, permissiveness and complete freedom can lead to frequent irritation and expression of dissatisfaction, even with necessary and reasonable demands.
- Talk to the child, explain your position to the child. Be patient and willing to spend as much time as it takes for the child to understand you and come to the appropriate conclusions. Rudeness, neglect, threats, blackmail injure the child's psyche and are unacceptable in education.
Be patient and willing to spend as much time as it takes for the child to understand you and come to the appropriate conclusions. Rudeness, neglect, threats, blackmail injure the child's psyche and are unacceptable in education.
- Suggest and analyze together possible options for behavior in situations that cause irritation in a child, ways to respond to troubles. Encourage his reasoning and engage in dialogue, helping the child learn to overcome difficulties. Praise and support if things don't work out. For example: “You are good for trying to cope on your own. Learning is always difficult, but you will soon learn it.”
In younger schoolchildren , feelings and irritability will also be associated with high responsibility, academic workload, relationships with classmates and teachers, and the atmosphere in the classroom. Your task in a calm home environment is to help the child respond to insults, support him and help switch attention.
- Talk to your child about situations that trigger an emotional response.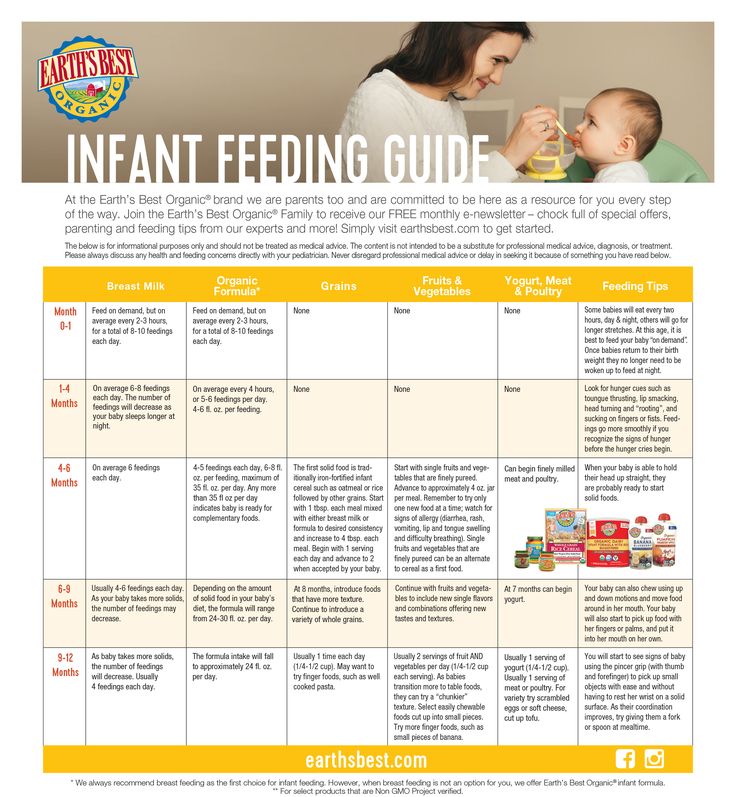 Children's awareness of their own thoughts, emotions and actions occurs with the help of adults. Therefore, by analyzing the situation, we help the child to be aware of it. The habit of keeping feelings inside can lead to nervous tension, increased anxiety, night terrors, and even the development of somatic diseases.
Children's awareness of their own thoughts, emotions and actions occurs with the help of adults. Therefore, by analyzing the situation, we help the child to be aware of it. The habit of keeping feelings inside can lead to nervous tension, increased anxiety, night terrors, and even the development of somatic diseases.
- Do not demand perfect completion of assignments in all subjects, this will cause irritation and reluctance to do anything before starting work. It is normal that children are more capable of some sciences, some subjects are easier for them than others. Do not push or scold the child, do not compare with other children or with yourself in childhood.
- Organize your child the opportunity to relax, change the type of activity and communicate with peers outside the school team - in various circles, sports sections, a music school, with friends in the yard.
Increased irritability, aggressiveness, nervousness - characteristic features of adolescence . Their appearance is primarily associated with hormonal changes occurring in the body. The nervous system cannot quickly adapt, teenagers often do not realize and cannot control their emotions, they feel loneliness due to their emotional instability.
Their appearance is primarily associated with hormonal changes occurring in the body. The nervous system cannot quickly adapt, teenagers often do not realize and cannot control their emotions, they feel loneliness due to their emotional instability.
- Talk kindly, be interested in the experiences of a teenager. Show more attention and love to him, just for what he is. Then the teenager will feel more confident, his self-esteem will increase.
- Help a teenager to understand the reasons for his irritability by speaking in detail about various situations in order to teach a teenager to better understand and control his psychological state.
- Teenagers already consider themselves adults and will defend their rights if you treat them like children. Explain to him that being an adult is a big responsibility, that he must be able to control his emotions and be responsible for his actions.
- Give your teenager more freedom, subject to your agreements with him (calling at certain times, some important restrictions).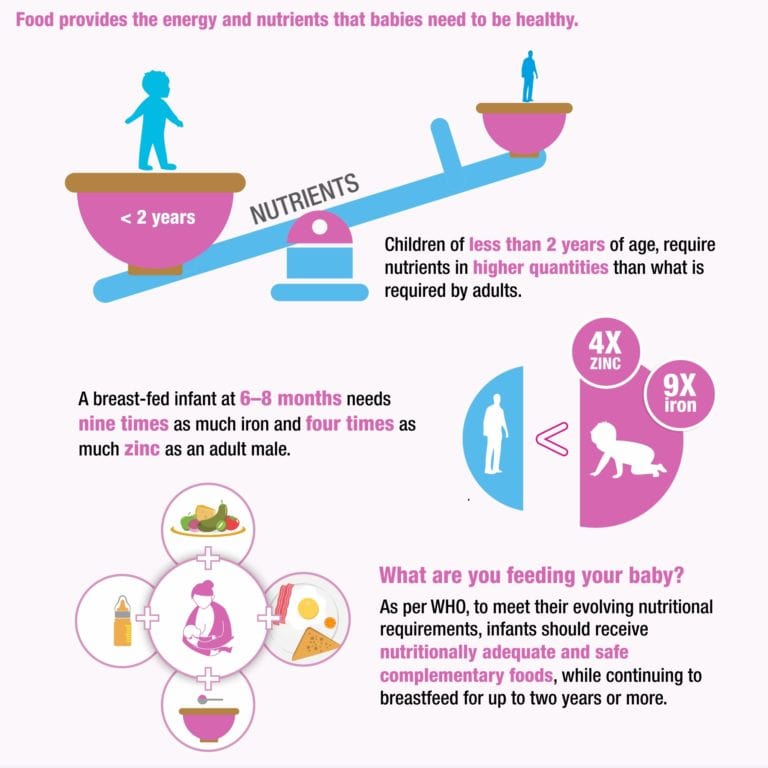 Let him say on his own when he comes, do something himself and praise him for the result, then the joy of success and the desire to do and be better arise.
Let him say on his own when he comes, do something himself and praise him for the result, then the joy of success and the desire to do and be better arise.
- Do not blame, but try to understand the teenager - see his problems, put yourself in his place, remember what experiences you had at that age. After all, teenagers often think that no one understands them, that significant people are indifferent to their interests and feelings.
- Do not focus on the shortcomings, rely on the positive qualities and help to see the resources. Even dissatisfaction with oneself can become an incentive for self-improvement.
Back to News List
Infant Reflux: Symptoms and Treatment
Search Support IconSearch Keywords
Home ›› What is Infant Reflux?
Home ›› What is reflux in babies?
↑ Top
Signs and what to do
Post-feed regurgitation is a common occurrence in the first few months of life. This is usually harmless and completely normal, but parents should read about gastroesophageal reflux (GER) and laryngopharyngeal reflux (LPR) in infants and how long it lasts to give them peace of mind.
This is usually harmless and completely normal, but parents should read about gastroesophageal reflux (GER) and laryngopharyngeal reflux (LPR) in infants and how long it lasts to give them peace of mind.
We look at signs of reflux in babies, symptoms of different types of reflux, and how to help a child with signs of reflux. If you require further information, always contact your healthcare provider.
What is reflux in babies?
So we know reflux is common, but what causes reflux in babies? Because young children have not yet fully developed the lower esophageal sphincter (LES), that is, the muscle at the bottom of the esophagus that opens and closes to let food into the stomach and keep it there, food can easily pass back up the esophagus.
Acid reflux, also known as gastroesophageal reflux (GER), is a normal reflux that occurs in babies. This type of reflux is considered normal and occurs in 40-65% of babies.
How do I know if my child has acid (gastroesophageal) reflux?
If a baby is spitting up milk after a feed, it is most likely acid reflux. As babies get older, GER usually goes away on its own without any intervention. If a baby has complications beyond just spitting up a small amount of milk (such as feeding difficulties and discomfort), they may have gastroesophageal reflux disease (GERD).
As babies get older, GER usually goes away on its own without any intervention. If a baby has complications beyond just spitting up a small amount of milk (such as feeding difficulties and discomfort), they may have gastroesophageal reflux disease (GERD).
Symptoms of GERD include:
- baby arching during or after feeding;
- crying more than three hours a day for no apparent reason;
- cough;
- gag reflex or difficulty swallowing;
- irritability, restlessness after eating;
- eating little or not eating;
- poor weight gain or loss;
- difficult breathing;
- severe or frequent vomiting.
GERD usually occurs when LES muscles are not toned in time, causing stomach contents to back up into the esophagus.
How do I know if my child has Laryngopharyngeal Reflux?
Another type of reflux, laryngopharyngeal reflux (LPR), also called silent reflux, is when the contents of a child's stomach leak back into the larynx, the back of the nasopharynx. This type of reflux does not always cause external symptoms, which is why it is called "silent". Babies can have GERD and silent reflux at the same time, but their symptoms are somewhat different.
This type of reflux does not always cause external symptoms, which is why it is called "silent". Babies can have GERD and silent reflux at the same time, but their symptoms are somewhat different.
Some of the symptoms of laryngopharyngeal reflux are listed below:
- trouble breathing;
- gag reflex;
- chronic cough;
- swallowing problems;
- hoarseness;
- regurgitation;
- poor weight gain or weight loss.
We have looked at the signs of reflux in infants, now we will move on to the treatment and duration of silent reflux in children, as well as the treatment of GERD.
How to deal with laryngopharyngeal reflux in babies while breastfeeding?
Breastfeeding mothers may need to review their diet if their babies show signs of reflux. The American Academy of Pediatrics (AAP) recommends breastfeeding mothers cut eggs and milk from their diet for two to four weeks to see if their baby's reflux symptoms improve or disappear. It may be worth eliminating acidic foods from your diet.
It may be worth eliminating acidic foods from your diet.
In most cases, GER and laryngopharyngeal reflux go away on their own. Typically, children outgrow reflux in the first year of life. If a child has persistent symptoms of laryngopharyngeal reflux, parents should consult a doctor. If your baby has severe vomiting, blood in the stool, or any of the symptoms of GERD listed above, parents should contact their pediatrician as soon as possible.
How can I help my child with reflux or GERD?
Reflux symptoms in babies usually go away on their own, but the following tips can help relieve symptoms:
- Thicken food with rice or a special milk thickener.
- Hold the bottle at an angle that fills the nipple completely with milk to reduce the amount of air your baby swallows. This can help prevent colic, gas, and reflux.
- Try the AirFree anti-colic bottle, designed to reduce air swallowing during feeding.
4. Let your baby burp during and after feeding. If the baby is bottle fed, parents can let him burp after every 30-60 ml. If the mother is breastfeeding, she may let the baby burp when changing breasts.
5. Hold baby upright after feeding. As a rule, in order for the milk to remain in the stomach, after feeding the baby, it is necessary to hold it in an upright position for 10-15 minutes. But, if the child has reflux, parents should keep him upright a little longer.
These tips may help relieve symptoms, but they do not replace a doctor's advice.
Parents should not change their infant formula formula without first talking to their doctor.
Don't panic! Reflux is very common in babies during the first three months of life, and most babies outgrow it without any consequences. Although GERD is a slightly more serious condition, there are many treatments, ways to manage it, and help newborns. Feel free to contact your doctor with any questions or concerns you may have.