Baby not satisfied after bottle feeding
Baby Never Satisfied After Breastfeeding
Your baby is never satisfied after breastfeeding, despite frequent and long nursing sessions. Learn 4 reasons why (and how to change it).
My newborn would nurse for hours if I had let him.
I’d breastfeed for 20 minutes on each side, but he’d start rooting again only minutes after latching him off. He always seemed hungry, practically eating and waking up every hour, and would cry even though I had just fed him. Sometimes I felt like I shouldn’t even bother with a shirt because I was nursing so often.
I couldn’t imagine how he was already hungry minutes after eating. Sure, he had plenty of wet diapers and was gaining weight just fine, but he never seemed satisfied after breastfeeding. He would sometimes doze off, but he’d often cry after I’d put him down.
I worried he wasn’t getting enough breastmilk, especially since I couldn’t exactly measure how much he was drinking. When he was given a bottle of pumped milk, he’d guzzle it down and fall asleep quickly, seeming so much more settled that way.
When your baby is never satisfied after breastfeeding
The worst experience as a mom to a newborn is feeling like you’re alone.
That you’re the only one who feels stuck nursing a baby who’s rarely relaxed or sleepy after feedings. You might take him off the breast after he has fallen asleep, but he just wakes up screaming within a minute. But as soon as you put him back on the breast, he’s fine once again.
As much as you love the bonding experience, you can’t help but feel resentful of how little time you get to yourself anymore. Couple that with worries about weight gain and producing milk, and breastfeeding has been challenging.
I can relate, mama.
And thankfully, I learned that there are reasons why your baby never seems satisfied after breastfeeding. These reasons reassured me that I wasn’t doing anything “wrong,” that most of these behaviors weren’t worrisome.
And more importantly, I realized I could make simple changes to help my baby feel satisfied, not fussy, after feedings. I hope you find this article reassuring, as one parent wrote:
“Thank you for writing this article. It was an answer to my prayers! I started reading this in the middle of the night as I frustratingly nursed my newborn yet again and started to feel my mental/emotional stability lean downhill. You somehow wrote my exact thoughts and feelings. I love the real, practical advice. It really helped me find hope and camaraderie in these sensitive postpartum weeks.” -Aliese
Take a look at these reasons, and what you can do about each one:
1. Your baby is not actually eating
I didn’t realize until much later that the constant need to suckle doesn’t necessarily signal hunger. I assumed that my baby needed to nurse because he was hungry, not because he was soothed by the sucking motion of nursing.
Comfort nursing isn’t bad—many moms love being able to soothe a fussy baby and bonding at the same time.
But if, say, your nipples are taking a beating or you desperately need a break, rest assured that your baby might be nursing for comfort, not hunger.
If that’s the case, try to keep him awake while he nurses. Change positions, burp often, take a break, even change his diaper. This will keep him from dozing off when he’s supposed to be eating.
How do you know he’s actually eating? Check his throat—if he were truly swallowing, you’d see movement around his throat, indicating that the milk is going down. You can also listen for a gulping sound—again, a sign that he’s taking in milk, not just moving his mouth.
And if he takes to it, see if he’ll be happy with a pacifier. He may simply want to be soothed to sleep through a sucking motion. You might try to sneak a pacifier in as he’s dozing off on the breast, or offer it as he’s starting to get fussy.
Free email challenge: Feeling stuck in motherhood? Sign up for the Motherhood Motivation 5-Day Challenge! You’ll get one actionable tip a day that will make you think (and act) about motherhood differently:
2.
 Your baby is going through a growth spurt
Your baby is going through a growth spurtBabies go through so many changes in the first few months than at any other time of their lives. They’ve also got tiny stomachs and immature digestive systems exactly at this age. Combine the two, and no wonder your baby never seems satisfied after breastfeeding.
Frequent feedings stimulate and increase your milk supply, far better than a pump could. Don’t see it as a hassle, but an opportunity—a strategy—to ensure you’re producing enough milk.
At this stage, feed on demand as much as possible. Our pediatrician told us that the biggest reason babies cry is because of hunger—i’s rarely that their clothes are itchy or that the room is too cold. For now, follow your baby’s lead and feed when he’s hungry.
Learn how to increase your milk supply.
3. You forget that fussiness is normal
Sometimes, we simply have to remember that fussiness is normal during the newborn stage. This is when babies cry the most, have crazy gas issues, and seem to be the most inconsolable.
Just because your baby used to sleep in three-hour stretches, doesn’t mean he won’t ever have a rough night again. Speak to any newborn mom, and she’ll tell you at least one episode when her baby cried and felt extra needy.
If you suspect issues with gas, try tricks like bicycle kicks, pushing his knees to his chest, or massaging his tummy. You might feed him after waking up so he has more opportunities to stay upright after eating.
This is also the time when he’ll be most attached to your breast, whether out of hunger or comfort. Any time you feel like things should be better by now, know that progress goes up and down, even if the general trend is going up. You’ll hit dips even as life continues to improve overall.
And should you truly feel concerned, reach out to a lactation consultant or find a support group like La Leche League. They can evaluate for particular issues that could be making breastfeeding more difficult than it needs to be.
Check out newborn tips and tricks new moms should know.
4. You’ve painted a negative picture
No one is going to argue that caring for a newborn is hard work. As a first-time mom, these first few weeks and months will likely be some of the most challenging moments in your life.
And yet, despite those challenges, a glimmer of joy can still be found. Try to make the experience a positive one, given your circumstances.
Maybe you’ll see these nursing sessions as an excuse to binge watch television, listen to podcasts, catch up on reading, or simply to rest. Grab magazines, DVDs, a reusable water bottle, and snacks to keep you comfortable.
You can also remind yourself that these moments are temporary. Now, when you’re with a newborn, every week, even every day, can feel like forever, so I understand that “temporary” is relative. But know that however challenging frequent nursing is, it won’t always be this way.
Learn hope to stop your baby from snacking on the breast.
Conclusion
It can be hard to tell if your baby is satisfied with breastfeeding, especially when he still seems hungry after feedings. Hopefully you’ve seen four compelling reasons why he never seems full, and what you can do about it.
For one thing, he may not be actually eating, especially if he uses nursing to soothe himself to sleep. If he is, then a growth spurt could be contributing to his constant nursing.
The other two reasons have more to do with us, the parents. We forget that babies do tend to fuss and cry at this stage. And sometimes, our very own stories that we tell ourselves depict it as a negative experience when it could very well be a positive one.
Your baby will eventually feel satisfied after breastfeeding, and that, yes, you can bother with keeping a shirt on after a while.
Get more tips:
- Is Your Baby Nursing for an Hour and STILL Hungry?
- 6 Ways to Handle Your Newborn Constantly Feeding
- When Does Breastfeeding Finally Stop Hurting?
- Burping a Newborn After Breastfeeding: Necessary or Not?
- When Breastfeeding Hurts (Even with a Good Latch)
Free email challenge: Feeling stuck in motherhood? Want to enjoy raising your kids again? Sign up for the Motherhood Motivation 5-Day Challenge! You’ll get one actionable tip a day that will make you think (and act) about motherhood differently:
Feeding Your 1- to 3-Month-Old (for Parents)
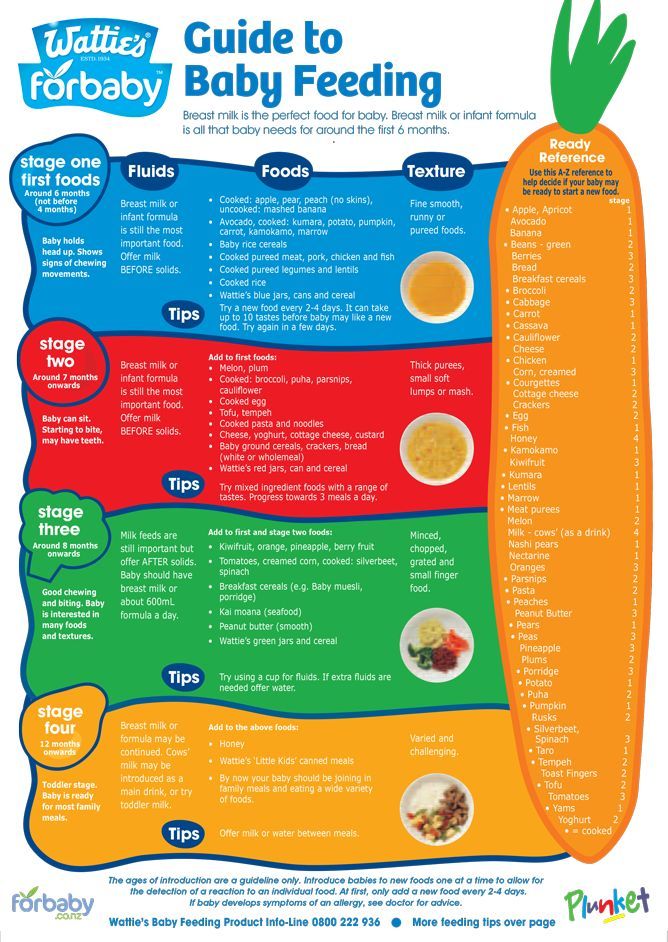
During your baby's first 3 months, breast milk or formula will provide all the nutrition needed. Doctors recommend waiting until your baby is about 6 months old to start solid foods. Some babies may be ready for solids sooner than 6 months, but wait until your baby is at least 4 months old.
Doctors recommend waiting until your baby is about 6 months old to start solid foods. Some babies may be ready for solids sooner than 6 months, but wait until your baby is at least 4 months old.
What Changes Should I Expect?
As your infant grows, feeding will change. Babies will start drinking more milk during each feeding, so they won't need to feed as often and will sleep longer at night.
Your baby's appetite will increase during growth spurts. Continue to feed on demand and increase the number of feedings as needed.
Your infant also will become more alert as the weeks go by, cooing and smiling. So there will be more interaction between you and your baby during feedings.
The following are general guidelines, and your baby may be hungrier more or less often than this. That's why it's important to pay attention to your baby's signals of being hungry or full. A baby who is getting enough might slow down, stop, or turn away from the breast or bottle.
Breastfeeding: How Much and How Often?
As babies get older, they will start to breastfeed less often and sleep for longer periods at night. Your infant probably is eating enough if he or she:
Your infant probably is eating enough if he or she:
- seems alert, content, and active
- is steadily gaining weight and growing
- feeds six to eight times per day
- is wetting and soiling diapers on a regular basis
Babies might not be eating enough if they:
- don't appear satisfied
- cry constantly
- are irritable, even after feeding
- are not making wet diapers
Call your doctor if you're concerned your baby isn't eating enough.
A few weeks after birth, breastfed babies tend to have fewer bowel movements (BMs, or poop) than they did before. At around 2 months of age, your baby may not poop after each feeding, or even every day. During growth spurts, you may notice that your little one wants to feed more often. This frequent nursing sends a signal to make more milk. Within a couple of days, supply and demand will get into balance.
Babies who get breast milk only should get vitamin D supplements within the first few days of life. Other supplements, water, juice, and solid foods aren't usually needed.
Other supplements, water, juice, and solid foods aren't usually needed.
Formula Feeding: How Much and How Often?
Babies digest formula more slowly than breast milk, so if you're bottle-feeding, your baby may have fewer feedings than a breastfed infant.
As babies grow, they can eat more at each feeding and may go for longer stretches between feedings. You'll also notice that your baby is starting to sleep longer at night.
During the second month, infants may take about 4 or 5 ounces at each feeding. By the end of 3 months, your baby may need an additional ounce at each feeding.
It's easy to overfeed a baby when using a bottle because it easier to drink from a bottle than from a breast. Make sure that the hole on the bottle's nipple is the right size. The liquid should drip slowly from the hole and not pour out. Also, resist the urge to finish the bottle when your baby shows signs of being full.
Never prop a bottle. Propping a bottle might cause choking and it increases the chances of getting ear infections and tooth decay.
Should I Worry About Spitting Up?
It's normal for infants to "spit up" after eating or during burping. Spitting up a small amount — usually less than 1 ounce (30 ml) — shouldn't be a concern as long as it happens within an hour of feeding and doesn't bother your baby.
You can reduce spitting up in these early months by:
- feeding before your baby gets very hungry
- keeping your baby in a semi-upright position during the feeding and for an hour after
- burping your baby regularly
- avoiding overfeeding
- not jostling or playing vigorously with your baby right after a feeding
If your baby seems to be spitting up large amounts, is spitting up forcefully, is irritable during or after feedings, or seems to be losing weight or is not gaining weight as expected, call your doctor. And if your child has a fever or shows any signs of dehydration (such as not wetting diapers), call the doctor right away.
Call your doctor if you have any questions or concerns about feeding your infant.
Reviewed by: Mary L. Gavin, MD
Date reviewed: November 2021
Baby won't take a bottle | Philips Avent
search support iconSearch Keywords
Home ›› What to do when your baby refuses a bottle
↑ top
any problems. If your breastfed baby refuses a bottle, don't worry. This is a common occurrence in many babies who are used to breastfeeding. Obviously, this can create certain difficulties for moms, especially if you need to return to work in the near future.
3 Philips Avent products to help you bottle feed:
So why is your baby refusing to bottle and crying? There are many ways to quickly and easily teach a breastfed baby to a bottle. Here are important tips on what to do when your baby refuses a bottle.
Is the baby refusing the bottle? Take a step back
If your baby cries while bottle feeding, the first thing to do is to start over and rethink your feeding approach and technique. Try the following steps when bottle feeding your baby: [1]
Try the following steps when bottle feeding your baby: [1]
- Lift and tilt your baby's head forward. Before inserting the pacifier into the baby's mouth, make sure that the baby's head is raised and tilted over his body to avoid choking: so that the baby does not choke and have the opportunity to burp during bottle feeding.
- Insert the pacifier. Bring the pacifier to the baby's lips and gently guide it into the baby's mouth. In no case do not try to press the nipple on the baby's lips and try to push it into his mouth. After touching the pacifier to the baby's lips, wait for the baby to open his mouth and take the pacifier.
- Hold the bottle at an angle. Tilt the bottle at an angle so that the nipple is only half full. So the child can eat at his own pace.
- Let the baby burp during and after feeding. It can be useful for a child to burp not only after feeding, but also approximately in the middle of the process. This will help reduce gas or tummy discomfort that your baby may experience from swallowing too much air.

- Stop in time, do not overfeed the baby. If the baby begins to turn his head away from the bottle or closes his mouth, then he is full and you need to stop feeding.
- Perhaps the flow of milk from the nipple to the baby is weak or, on the contrary, too fast, so he is naughty and refuses the bottle. Try changing the nipple to a nipple with a different flow.
Other tips if your baby refuses the bottle
If you've followed the steps above and your baby still refuses the bottle, don't worry. There are other ways to help bottle feed your baby. Here are some simple tricks you can add to your bottle feeding process. [2]
1. Remind your child about mom.
Sometimes a child can be fed by someone other than his mother - dad, grandmother or, for example, a nanny. If your baby fusses while bottle feeding, try wrapping the bottle in something that smells like mommy, like a piece of clothing or some fabric. This will make it easier to feed the baby when the mother is not around.
This will make it easier to feed the baby when the mother is not around.
2. Try to maintain skin contact while bottle feeding.
Some babies need contact with their mother, so try bottle feeding while leaning against you. However, some babies are better at bottle feeding when they are in the exact opposite position than when they are breastfed. For example, there is a position with bent legs. Lay the child on your bent knees, facing you, pointing the child's legs towards your stomach. During feeding, the baby will be able to look at you and contact you in this way. If your baby refuses a bottle, experiment to see which works best.
3. Move while feeding.
Sometimes all it takes to get your baby to take the bottle is a little wiggle or walk. The next time your baby starts crying while bottle feeding, try moving around a little rhythmically to calm him down.
4. Try changing the milk temperature.
Try changing the milk temperature.
If the baby still does not want to take the bottle, check if the milk in the bottle is too hot or too cold. Before feeding, put some warm breast milk on the inside of your wrist to check the temperature. Milk should be warm, but if it seemed hot to you, just place the bottle for a short while under a stream of cold water.
Choosing the right bottle for your baby If you plan to combine bottle feeding with breastfeeding, it is advisable to choose bottles with a nipple that will have a wide base as the bottle will grip closer to the breast. Also pay attention to the fact that the nipple is firm and flexible, the child must make an effort to drink from the bottle, as well as from the breast. Give preference to nipples with an anti-colic valve that vents air out of the bottle.
Natural bottle allows you to combine breast and bottle feeding. 83.3% of babies switch from a Natural bottle to breastfeeding and back. *
*
If you choose a bottle for artificial feeding, traditional bottles are fine, but it is desirable that the nipple is made of a hypoallergenic material, such as silicone, has an anti-colic valve and did not stick together when bottle fed. In case your baby spit up often, then use special bottles with anti-colic and anti-reflux valve, which reduces the risk of spitting up and colic.
Bottle with unique AirFree valve reduces the risk of colic, gas and spitting up. With this bottle, you can feed your baby in an upright or semi-upright position to reduce spitting up. Due to the fact that the nipple is filled with milk and not air during feeding, the baby does not swallow air, which means that feeding will be more comfortable.
Both bottles are indispensable if you want to breastfeed, bottle feed or just bottle feed your baby.
“My baby refuses to breastfeed but bottle feeds – help!”
Sometimes a baby gets used to bottle feeding and refuses to breastfeed. Therefore, it is important to use bottles that are suitable for combining breastfeeding with bottle feeding. If, nevertheless, you are faced with the fact that the child refuses to take the breast, try using silicone nipple covers to make the transition from the bottle to the breast and back more imperceptible.
Therefore, it is important to use bottles that are suitable for combining breastfeeding with bottle feeding. If, nevertheless, you are faced with the fact that the child refuses to take the breast, try using silicone nipple covers to make the transition from the bottle to the breast and back more imperceptible.
Remember that if you want to combine breastfeeding and bottle feeding, it is worth waiting at least a month before offering a bottle, so that you are lactating and have time to get used to each other and develop a breastfeeding regimen.
Breastfeed and bottle feed your baby with pleasure
Remember that it takes a while for your baby to get used to bottle feeding. This is completely normal. If you have to go to work, be sure to set aside enough time to bottle train your baby beforehand.
Remember that every child is different, so what works for one may not work for another. With a little time and patience, you will find out what works best for your baby when he refuses a bottle.
You will identify your child's unique needs. However, if your baby still refuses the bottle after all the steps above, check with your pediatrician.
Articles and tips from Philips Avent
References:
*O.L. Lukoyanova, T.E. Borovik, I.A. Belyaeva, G.V. Yatsyk; NTsZD RAMS; 1st Moscow State Medical University THEM. Sechenova, "The use of modern technological methods to maintain successful breastfeeding", RF, 10/02/2012 3 llli.org - The Baby Who Doesn't Nurse
llli.org - Introducing a Bottle to a Breastfed Baby
Baby+ app
Download the app and track your child's development and growth with trackers and save those special moments forever.
Download app:
You are leaving the Philips Healthcare (“Philips”) official website. Any links to third party websites that may be included on this site are provided solely as a convenience to you. Philips makes no warranties regarding any third party websites or the information they contain.
I understand
You are about to visit a Philips global content page
Continue
You are about to visit the Philips USA website.
I understand
Women's clinics | Genus. House number 5
The function of the mammary glands after childbirth reaches its highest development. During pregnancy, milk ducts form and glandular tissue grows. Under the influence of prolactin, blood flows intensively to the mammary glands and increased secretion of milk begins. Mother's milk is the only natural biological product that provides physiologically adequate nutrition for infants. It is the gold standard for early childhood nutrition.
Women's breasts are a generous source of baby food that can saturate the baby's growing body with the necessary substances, protect it from diseases, and bind mother and child together for several hours a day.
Breastfeeding is a soft and optimal postpartum adaptation of mother and child, the basis for the health and proper development of the child.
BREASTFEEDING BENEFITS
Breastfeeding promotes the formation of a close, tender relationship between mother and child, from which the mother receives emotional deep satisfaction. Close contact with the child immediately after birth helps to establish these relationships. Feeding time is not just for feeding your baby, it gives you the opportunity to get to know and love each other. Babies cry less and develop faster if they stay with their mothers immediately after birth. Breastfeeding mothers respond affectionately to their children.
Mother's milk is the only food that fully meets the needs of the newborn. It is easily digested and completely absorbed, has the necessary temperature, contains antibodies that help protect the child from certain infections and allergies. Breastfeeding helps avoid unwanted pregnancies, protects the health of the mother, and is less expensive than artificial nutrition. Contributes to the best social adaptation of the child
It is important to have the desire to breastfeed even during pregnancy, and for this you need to learn, because pregnancy is just the right time to replenish your knowledge about the health of the unborn baby.
The amount of breast milk depends in part on the thoughts, feelings and sensations of the mother. It is important that the baby and the mother are together all the time, day and night, it is necessary to help the mother so that she strives to continue breastfeeding. Many difficulties can arise from improper attachment of the baby to the breast. The amount of milk in the breast depends on how long the baby suckles and how much milk he sucks. The more the baby suckles, the more milk the mother produces. Breastfeeding will be successful in most cases if the mother feels well, the baby is properly attached to the breast to allow him to suckle effectively, the baby suckles as often and for as long as he wants, and the environment is conducive to breastfeeding. For the formation of a warm relationship, it is necessary that the mother stroke the child during feeding, look at him, talk to him. Those sensations that the child receives during feeding, according to some reports, can affect his entire subsequent life.
Sucking for a baby is a necessity and a pleasure that is not directly related to the feeling of hunger. Thanks to sucking, the baby develops the jaw apparatus, muscles of the mouth and tongue, which is important in the development of speech .
Two hormones involved in milk production are prolactin and oxytocin. Oxytocin is produced before and during feeding. The baby suckles the breast, sensory impulses come from the nipple to the pituitary gland, oxytocin enters the bloodstream and acts on muscle cells, causing them to contract and milk to be released. The release of oxytocin promotes uterine contraction. Prolactin is released after feeding to prepare the next feeding. The baby suckles the breast, sensory impulses from the nipple go to the pituitary gland. Entering the blood, prolactin acts on the cells that secrete milk and ducts, forcing them to secrete milk. Prolactin - inhibits ovulation, preventing unwanted pregnancy.
CHANGES IN THE COMPOSITION OF MILK
Colostrum is breast milk that is produced in a woman within 3-5 days after giving birth. It is thick yellowish in color, rich in immunoglobulins, which provides protection against infections and allergies. It has a laxative effect, promotes the removal of meconium and helps prevent jaundice. Contains growth factors, promotes intestinal maturation. Rich in vitamin A, prevents eye diseases.
It is thick yellowish in color, rich in immunoglobulins, which provides protection against infections and allergies. It has a laxative effect, promotes the removal of meconium and helps prevent jaundice. Contains growth factors, promotes intestinal maturation. Rich in vitamin A, prevents eye diseases.
Mature milk is milk produced after a few days, its amount increases, the breasts fill up, swell and become heavy. This moment is called the arrival of milk.
A distinction is also made between foremilk and hindmilk.
Foremilk is produced at the beginning of feeding, has a bluish tint and is produced in large volume, providing the baby with sufficient amounts of proteins, lactose and other components. Since the baby consumes a lot of foremilk, he receives with him all the amount of water he needs and he does not need to give additional water in the first six months of life. If he quenches his thirst with water, he will consume a small amount of milk. For the same reason that foremilk and hindmilk are different in composition, it is necessary to feed the baby in one feeding with one breast.
For the same reason that foremilk and hindmilk are different in composition, it is necessary to feed the baby in one feeding with one breast.
Hindmilk is the milk produced at the end of a feeding and is whiter in color because it contains more fat, which is the main source of nutrition during breastfeeding. Mother's milk has a unique individual composition, polyunsaturated fatty acids of breast milk contribute to the development of the brain.
A child is born with innate skills, and has:
Grasping reflex - when something touches the child's lips, he opens his mouth, the tongue goes down and moves forward.
Sucking reflex - when something touches the baby's palate, he starts to suck.
Swallowing reflex - when the baby's mouth fills with milk, he swallows. These reflexes are especially pronounced in the first hour after birth, so it is very important to start breastfeeding during this period.
By carefully observing the baby, the midwife or nurse notes the signs of the newborn's readiness to suckle the breast (opens the mouth, sticks out the tongue, turns the head, tries to crawl towards the breast) and draws the attention of the mother to them. And then they help to attach the baby to the breast for the first time.
And then they help to attach the baby to the breast for the first time.
To do this, the mother and child are located in the same plane, the mother needs to relax and listen to her feelings. The child should not be in diapers, he is pressed tightly against the mother's body. The mother presses the buttocks with her elbow, holds the back with her forearm, and the hand slightly supports the head, without pressing it to the chest. The child's nose is located at the level of the nipple or slightly higher, the mother takes the breast in such a way that 4 fingers are located under the breast, and one large one is on top. We move the nipple of the breast along the lips and nose of the child, it is necessary that the child opens his mouth wide and then he will grasp the breast well, it is necessary to carefully insert the nipple together with the areola into the child's mouth, directing the nipple to the upper palate. From the captured nipple and areola, a nipple is formed, in which the nipple occupies only 1/3 of the part. The child begins to suck quickly, then the sucking movements become more rare, measured, which indicates a good milk flow. As a rule, the child himself releases the breast, satisfied and sleepy.
The child begins to suck quickly, then the sucking movements become more rare, measured, which indicates a good milk flow. As a rule, the child himself releases the breast, satisfied and sleepy.
Signs of proper breastfeeding .
-
The baby's mouth is wide open;
- chin and nose touching the chest;
-
mother and child are in the same plane;
-
the child captures most of the areola, more from below than from above;
-
the tip of the nipple is in the depths of the mouth and touches its soft palate;
-
baby's cheeks are round,
-
the lower lip is turned outward;
-
the child makes swallowing movements.
-
the mother is not in pain, the child is happy.
Correct and incorrect application
Timely mastering the technique of applying the baby to the breast minimizes the appearance of possible problems that arise during breastfeeding.
On the first day, newborns may require the breast no more than 2-4 times. However, the main task of the mother is to learn how to give the child the breast correctly, and the child to suckle correctly. For this purpose, on the first day, it is advisable to put the baby to the chest during the day up to 10 times, and at night as many times as he wakes up.
Starting from 2-3 days after birth, breastfeeding is carried out at the request of the child. The mother must learn to recognize when the child asks for food, and not offer him the breast as soon as he shows concern, for any reason. However, free (on demand) feeding, during the neonatal period, for a number of reasons (the formation of lactation, the small size of the child's stomach, a high metabolic rate) requires quite frequent (from 7-8 to 12-16 times a day) energy intake into the child's body. and plastic material. Breast milk contains a sufficient amount of liquid, therefore, as a rule, there is no need for regular (daily) supplementation of the child with water. Water can carry the risk of infection and lack of demand for breast milk in sufficient quantities.
Water can carry the risk of infection and lack of demand for breast milk in sufficient quantities.
On the other hand, sometimes babies may just want water instead of the liquid in breast milk. Once complementary foods are introduced, water can be offered daily. Mothers must learn to identify the water needs of a child. Exclusively breastfed babies tend to wake up at night and need to be fed. By the way, frequent awakenings of the child also have a positive side, because. waking up and awake reduces the risk of sudden death syndrome.
The success of maintaining and maintaining lactation largely depends on the ability of the mother and child to give and take the breast.
There are several ways to breastfeed a baby: lying down (on the side, on the back), sitting (holding the baby in the cradle position or from under the arm), standing up (upright or bent over a lying child), from under the arm . The most common position used by mothers to feed their babies is sitting. However, in almost all these positions, especially during the neonatal period, it is necessary to ensure closer contact between mother and child. Babies learn the world through sensations, and the more pleasant these sensations are, the more benevolent and calmer your child will be, and along with him, you.
However, in almost all these positions, especially during the neonatal period, it is necessary to ensure closer contact between mother and child. Babies learn the world through sensations, and the more pleasant these sensations are, the more benevolent and calmer your child will be, and along with him, you.
Current provisions for breastfeeding
« Classic cradle»
The child is located in the arms of the mother, as in a cradle: his head is on the elbow of one arm, with the other hand, the mother grabs and holds the back. The baby is turned to the mother "belly to stomach", and his mouth is directly opposite the nipple. In this position, the mother can feed from both the right and left breasts, shifting the baby's head from one hand to the other. A variation of this pose can be called standing feeding. The baby in the mother's arms is in the same position, only the mother herself does not sit, as is most often the case, but stands. Usually, this is how babies are fed during motion sickness and when they go to bed, with stitches on the perineum, when you can’t sit.
Usually, this is how babies are fed during motion sickness and when they go to bed, with stitches on the perineum, when you can’t sit.
"cross cradle"
The sitting mother holds the child with one hand - the opposite breastfeeding breast. His head rests in his mother's palm, and his body supports her forearm. This position is relevant in establishing a correct grip on the breast by a child, more often in premature babies
hand feeding
Mom sits straight, the child is under her arm on the side, at chest level, with her head towards her knees. A pregnancy pillow can be used to support the baby. This position is relevant when feeding twins, with blockage of the milk duct, with difficulties in grabbing the breast, with flat nipples, with the prevention of congestion in the lower and lateral segments of the mammary glands, with nipple cracks
Twin feeding
Feeding two children is very different from feeding one child. It can be organized in different ways. You can feed each separately. But in this way, more time per day for feeding may be required. You can feed at the same time.
It can be organized in different ways. You can feed each separately. But in this way, more time per day for feeding may be required. You can feed at the same time.
Try, in a combination of individual and group feedings, to give each baby at least one "personal" feeding per day. This approach cuts down on the total number of feeding hours, but allows you to have a little interaction with each one. You might want to put your expressed milk in the refrigerator so dad can give it to another baby during private feedings, or so you can get some sleep. Parents should be aware that each of the twins has its own personality. Their needs and diet are different. Please don't treat twins the same.
Frequent and prolonged breast sucking and an “empty breast” that seems to you is not a reason for supplementing a child with artificial mixtures. Before taking this serious step, be sure to check with your doctor, a breastfeeding specialist, remember that other liquid tea, water, milk formula, suppresses appetite. The newborn will not actively suckle the breast and this will lead to a decrease in milk production. One of the most common reasons mothers switch to bottle-feeding or stop breastfeeding is because they believe they are “not getting enough milk.” Studies show that less than 1% of women have actual physiological causes for inadequate milk production.
The newborn will not actively suckle the breast and this will lead to a decrease in milk production. One of the most common reasons mothers switch to bottle-feeding or stop breastfeeding is because they believe they are “not getting enough milk.” Studies show that less than 1% of women have actual physiological causes for inadequate milk production.
Signs of insufficient breast milk
If the mother does not have enough milk, the child has a feeling of hunger - the state of his health, as well as development in the first months of life, can be significantly shaken.
Therefore, you should pay attention to a number of signs of milk deficiency:
Valid:
Poor weight gain (in two weeks the child did not restore the “physiological” weight loss or gained less than 500 g in one month), 125 g in 1 week.
The average daily weight gain is less than 20 grams.
Infrequent urination with concentrated urine (less than 6 urination per day, provided that it is not supplemented with water, yellow urine).
Likely:
baby cries often
very frequent breastfeeding (after 1-1.5 hours)
Very long breastfeeding (more than 30 minutes)
stool rare, dense, "hungry", dry, not yellow
The mother feels that there is no milk in the mammary glands
If you notice such signs - do not make an independent decision about supplementary feeding of the baby! Be sure to discuss this with your doctor or pediatric nutritionist.
Criteria for breast milk sufficiency.
If a child gains weight at least 500 grams per month and urinates at least 6-8 times a day, his skin is of normal moisture, which means that he is getting enough milk.
Lactation crisis - temporary decrease in milk production, after seemingly already established lactation. The reasons for the decrease in milk production may be associated with periods of intensive growth of the child, with the physical or mental overwork of the mother, with hormonal changes in the woman's body (resumption of menstruation), with a sharp restriction in fluid and food intake, as well as with the mother's illness.
Calm down and believe that lactation will definitely be restored.
To restore a sufficient amount of milk produced, continue frequent breastfeeding (up to 10-15 times a day), including at night. Feed from both breasts in one feeding, be with the baby around the clock, sleep with him. Try to rest and improve your diet. Ask your family and friends to do housework. Use special lactogenic drinks, herbal teas, homeopathic medicines. Be sure to make sure that you are feeding your baby properly and that he is suckling properly. Do not hesitate to contact a medical institution for help. In the antenatal clinic, maternity hospital, children's clinics, the staff will do everything possible for the success of your breastfeeding.
A few tips: it is very good to drink hot freshly brewed green tea (you can with milk), juice, any fermented milk drink just before feeding. Various lactogenic drinks perfectly stimulate lactation. For example, blackcurrant juice, milk infusion with walnuts increases milk production. Since ancient times, various collections of lactogenic herbs have been used in folk medicine, but medicinal plants must be used very carefully .
Since ancient times, various collections of lactogenic herbs have been used in folk medicine, but medicinal plants must be used very carefully .
For this reason, instant herbal teas of industrial production, produced by both domestic and foreign manufacturers, are of undoubted interest. Cooking them is very fast and convenient, besides, the components included in them undergo strict environmental control. Instant herbal teas from different manufacturers differ from each other in composition, the number of herbs they contain, and the presence of additional additives. They not only increase lactation, but also have a general strengthening effect, promote good sleep, relieve the mother’s neuro-emotional stress, and normalize the functioning of the intestines of a nursing woman. Such tea well satisfies the increased need for fluid that occurs in the mother during breastfeeding, and also becomes an additional source of vitamins, but be careful not to overdose!
Laktostasis is the stagnation of milk, occurs when one or more lobes of the mammary gland cease to be released from milk. The duct leading to the lobe remains blocked. Your child can help you deal with lactose intolerance. To do this, apply the baby more often to the chest so that his chin is directed towards the seal. After a few feedings, you will notice how the seal becomes smaller. If the baby is unable to suckle, express milk manually or with a breast pump. Before feeding or pumping, apply a warm compress, do a light massage of the breast. After feeding or pumping, you can put a towel moistened with cold water on your chest for 5-10 minutes. Cold will help relieve discomfort and reduce the flow of milk into the stagnant lobe.
The duct leading to the lobe remains blocked. Your child can help you deal with lactose intolerance. To do this, apply the baby more often to the chest so that his chin is directed towards the seal. After a few feedings, you will notice how the seal becomes smaller. If the baby is unable to suckle, express milk manually or with a breast pump. Before feeding or pumping, apply a warm compress, do a light massage of the breast. After feeding or pumping, you can put a towel moistened with cold water on your chest for 5-10 minutes. Cold will help relieve discomfort and reduce the flow of milk into the stagnant lobe.
You should not use alcohol-based compresses, you can replace them with compresses from a mashed cabbage leaf
If the seal does not go away within a day, consult a doctor to prevent a serious problem like mastitis.
Milk stasis (Lactostasis) is a temporary difficulty that, with the right tactics of management, can be easily dealt with!
When, how and how much to express breast milk?
Readings :
Possibly while in the maternity hospital, for a successful start of lactation
On days of lactation crises, for additional stimulation of the mammary glands
· To leave milk in your absence
· With engorgement of the mammary glands
For feeding a low birth weight or weak baby
· When it is necessary to alleviate the condition of the mother. Usually this situation occurs with the "tides" of breast milk. To alleviate the condition, milk is not completely expressed, but only until the mother feels comfortable
Usually this situation occurs with the "tides" of breast milk. To alleviate the condition, milk is not completely expressed, but only until the mother feels comfortable
· To create an individual breast milk bank.
No equipment is required to express breast milk. Wash your hands thoroughly, sit/stand comfortably with the milk collection vessel next to your breast. The thumb is set on top along the edge of the halo, the index finger is opposite from below. Slightly press the gland towards the chest, then point the index finger and thumb towards each other. If the pumping technique is correct, then the woman does not experience pain. It is not recommended to place the nipple between other fingers, as the milk duct may be squeezed, which can cause milk stasis. The first movement of the brush is carried out towards the chest. Then the movement of the fingers of the 1st and 2-3rd towards each other is carried out. Pumping movements must be alternated with massaging the chest.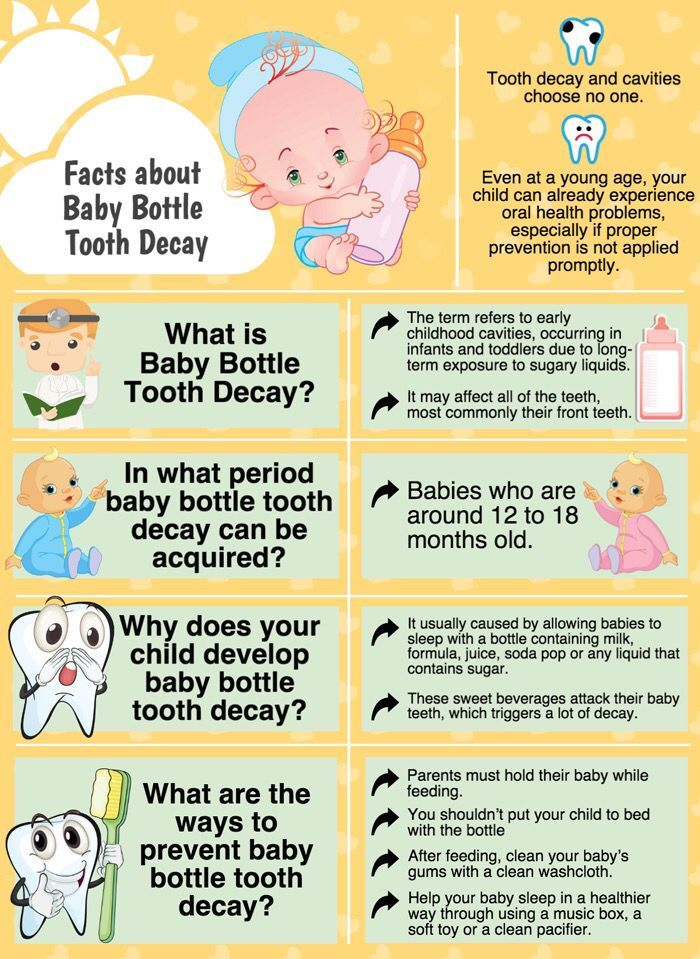 The procedure is repeated until the breast is soft. Fingers should not touch the nipple. Please also note that when pumping by hand, the purity of the milk is violated, a large number of microorganisms enter it, which creates the danger of the development of harmful bacterial flora. Therefore, hand-expressed milk must be consumed within 2 hours and is not recommended for freezing and breast milk banking.
The procedure is repeated until the breast is soft. Fingers should not touch the nipple. Please also note that when pumping by hand, the purity of the milk is violated, a large number of microorganisms enter it, which creates the danger of the development of harmful bacterial flora. Therefore, hand-expressed milk must be consumed within 2 hours and is not recommended for freezing and breast milk banking.
Expression with a breast pump
In some cases, there are problems that prevent normal sucking and emptying of the mammary gland, which leads to the formation of lactostasis and threatens the development of mastitis.
Manual pumping requires skills and strength, so mothers need to learn how to use modern breast pumps.
Breast pumps are designed for gentle and comfortable pumping of breast milk. During the period of formation, maintenance of lactation or the creation of a breast milk bank, breast pumps may be required by every woman who is breastfeeding a child.
Sometimes a mother can be separated from her baby. The breast pump will allow her to express milk in such a way that the breastfeeding process will not be interrupted.
Using a breast pump will help eliminate lactose and also ensure that the mammary glands receive the stimulation they need to increase milk production.
If a mother works outside the home, using a breast pump will allow her to go to work and continue breastfeeding. In addition, the breast pump provides the opportunity to breastfeed premature babies or those who have difficulty suckling.
Setting up a breast milk bank
During breastfeeding, situations may arise when a nursing mother needs to express and store milk for her baby. This happens when a mother needs to be away from home, when a mother must undergo a course of treatment that makes it impossible to breastfeed. In all these cases, prolonging breastfeeding will help INDIVIDUAL BREAST MILK BANK . It is personal expressed breast milk, which is placed in portions in convenient containers, stored at low temperatures and can be used to feed the baby at any time.
It is personal expressed breast milk, which is placed in portions in convenient containers, stored at low temperatures and can be used to feed the baby at any time.
In the first months of a baby's life, the mother usually produces more milk than is necessary for feeding the baby. During this period, it is recommended to prepare milk for future use. The safety of the quality of frozen breast milk also depends on the container in which it is stored. Glass containers are the least convenient, as they can burst or break. In addition, some biologically active components adhere strongly to the glass and are thus lost from the milk. This disadvantage is less inherent in plastic bags and polypropylene containers. They are sold sterile packaged and do not need to be sterilized before first use. Allow multiple sterilization.
The container with a portion of expressed milk should be tightly closed with a lid. If you use bags, tightly snap a special fastener on them. Write the date and time of pumping on the surface of the container.![]() Milk from multiple pumping episodes in the same day can be pooled into one serving. After each pumping, the milk should be placed in the refrigerator, taken out after the next pumping to top up the next portion, and placed again in the refrigerator. 150-200 ml is an approximate portion, sufficient for one feeding.
Milk from multiple pumping episodes in the same day can be pooled into one serving. After each pumping, the milk should be placed in the refrigerator, taken out after the next pumping to top up the next portion, and placed again in the refrigerator. 150-200 ml is an approximate portion, sufficient for one feeding.
Breast milk should be stored in tight plastic or glass containers, or in special bags for storing frozen milk.
IMPORTANT Remember that before adding a new batch to already frozen milk, it must be cooled.
Milk that has been at room temperature for 2 hours must not be frozen or refrigerated!
Thawed milk cannot be re-frozen, but can be stored in the refrigerator for up to 24 hours.
thawed breast milk
Frozen breast milk that has been reheated can be left in the refrigerator for up to 24 hours. Attention! It is impossible to re-freeze such milk!
How to heat breast milk
In order to defrost milk, you need to put the container in the refrigerator chamber. Then, after it melts, heat to room temperature. After that there are several ways:
Then, after it melts, heat to room temperature. After that there are several ways:
Warm up in a water bath to 30-35 ° C. This method is low-cost and technically not always easy to use. In addition, it is difficult to control the temperature of the milk, so overheating is possible.
REMEMBER: only boil-resistant, BPA-free bottles may be placed in the water bath*
*a harmful substance contained in the polycarbonate used in the production of traditional low-price plastic bottles. When heated or when food is stored for a long time in a dish, Bisphenol-A passes from plastic to food. Dangerous even in very small quantities.
Under running hot water. Shake the bottle periodically to evenly distribute the heat. Use special surface thermometers to monitor temperature changes.
In a bottle warmer. Specially designed for warming baby food, the devices are equipped with a thermostat, you only need to set the desired temperature. At the same time, overheating of milk is excluded, and, therefore, all useful substances are preserved.
Do not heat breast milk in the microwave! During heating, it is difficult to control the temperature of the milk. In addition, some pediatricians consider the use of microwave technologies to be wrong, since a microwave can be used to sterilize, for example, dishes, during which vitamins and other biologically active substances are destroyed.
How long to breastfeed?
Let the little creature determine the duration of breastfeeding
The child continues to receive vitamins and other nutrients in the second year of life. Breast sucking for a child older than a year is needed not so much to get enough, but to communicate with his mother. Responding to anxiety and crying by breastfeeding, you form in the crumbs the confidence that mom is always there and ready to help.
Listen to our advice - and you will succeed!
· Begin breastfeeding within the first 30-40 minutes after delivery.