Baby pushing breast while feeding
Why Does My Baby Knead Me While Breastfeeding? Science Explains
Life
poplasen/Fotolia
by Cat Bowen
I began breastfeeding my daughter in just a matter of minutes after she was born. The nurse set her on my bare chest, and quickly, she found gold. She rewarded me by punching my breasts. I can't be the only one to wonder, why does my baby knead me while breastfeeding?
Not surprisingly, this is not the most comfortable thing in the world. Who knew a tiny baby's fists could hurt like that? But, when your breasts feel as though they're a mere 10 milliliters from splitting at the sides like an overfilled pastry, those baby fists may as well be Balboa fists. It's not always painful — sometimes it's just funny. They get such a concentrated look on their little scrunchy faces while they speed bag your boobs like they've been personally affronted by the mammary glands.
Lindsay Greenfield, International Board Certified Lactation Consultant (IBCLC) tells Romper that your baby kneading your breasts is a way to stimulate milk production in the mother. Greenfield also notes that their little fists help them guide themselves to the nipple to latch — and science is there to back that up.
Tera Hamann, IBCLC points moms to a video from the World Health Organization (WHO) that shows a baby crawling across the bare chest of a mom just moments after birth, because that baby knew what's up. According to the WHO, there are chemicals on the nipple and coming from the milk that lay just beneath that are like a siren's call to newborns, because it smells like the amniotic sac.
In their article "Facilitating Autonomous Infant Hand Use During Breastfeeding," scientists Catherine Watson Genna, IBCLC and Diklah Barak wrote that it is actually an important stage of development for the newborn. They found that babies who are not swaddled and allowed to root on their own, using their hands, are more likely to self-latch than babies who are bound in cloth or discouraged from using their hands while nursing.
They noted that this kneading motion also increases the level of oxytocin in the mother, stimulating production, allowing for easier let-downs of milk, and that it also has the added benefit of making the areola pucker, projecting the nipple into a better shape for breastfeeding.
So while it may be uncomfortable at times, an article in Early Human Development, found that this is a normal, primitive neonatal reflex that can be witnessed across the world in every corner of new motherhood, and should not be discouraged as it is beneficial for successful feeding, however peculiar it may seem.
I know it looks like a cat kneading at your leg or a blanket, but Hamann tells Romper that if you think about it, humans are, after all, mammals, so it makes sense that there are similar behaviors. Maybe be grateful that baby doesn't have claws? (Who am I kidding, baby nails basically are claws.)
My baby fusses or cries when breastfeeding
By Kelly Bonyata, BS, IBCLC
© Lsantilli - Fotolia. com
com
Some babies will fuss, cry or pull off the breast during breastfeeding. There are a number of reasons why this might be happening. It’s pretty common to see this type of behavior at around 6-8 weeks, though it can occur at any time. If your baby is generally fussy (not just when nursing) see My baby is fussy! Is something wrong?
Determining the problem
Here are some of the problem-solving steps I go through when my baby is fussy at the breast or a mother asks me why her baby is fussing while breastfeeding:
.
How old is baby? Most babies go through growth spurts during the first few days at home and around 7-10 days, 2-3 weeks, 4-6 weeks, 3 months, 4 months, 6 months, 9 months, etc. Many babies are fussy during growth spurts.
Is baby working on anything new developmentally? Babies who are starting to notice the world around them can be notoriously distractible. Any kind of new developmental step that baby is working on can affect nursing temporarily, whether it be fussy nursing behavior or simply more frequent nursing.
When is baby fussing? To figure out the cause it’s helpful to pay attention to when the fussy behavior happens, both during the nursing session and during the day.
If baby is fussy right when your milk is letting down (or immediately after), there’s a good chance that the fussy nursing is related to a fast let-down. If baby is fussy before let-down, or a few minutes into nursing (and a while after let-down), then baby may be impatient for the fast flow of milk that comes with let-down. Fussing at the end of a nursing session (or what seems to be the end) may mean that baby needs to burp, or is ready to finish nursing, or just wants to suck (and doesn’t want to deal with a new let-down at this point), or wants to continue nursing on the other side or with a faster flow of milk.
If the fussy behavior is mainly in the mornings, it might be due to a faster than usual let-down if baby has just had a longer sleep period and mom’s breasts are fuller than usual. If baby is fussier during evening nursings, it may be due to the normal fussy time that most babies have during the evening. Although most babies don’t react to foods that mom eats, some do. If you eat a particular food at about the same time each day (or most days) and baby has a regular time where she fusses during nursing, try not eating that food for a week or two to see if things improve.
If baby is fussier during evening nursings, it may be due to the normal fussy time that most babies have during the evening. Although most babies don’t react to foods that mom eats, some do. If you eat a particular food at about the same time each day (or most days) and baby has a regular time where she fusses during nursing, try not eating that food for a week or two to see if things improve.
Does fussing occur on both sides equally or only on one side? Most moms have a faster let-down and/or a more abundant milk supply on one side than the other, so if your baby fusses more on one side, it may be due to these differences.
What else is going on with baby? Is she sick or teething? Is something new or different going on in her environment? Has she started solids or is she trying a new food? Is she exhibiting other symptoms besides the fussy nursing?
Below are discussions of some of the different things that can lead to fussy nursing behavior. Keep in mind that the problem may also be a combination of several things.
Keep in mind that the problem may also be a combination of several things.
Does baby need to burp?
Many babies will cry, fuss, pull off the breast, etc. if they need to burp. Try to burp between breasts and after a feeding, but don’t worry if baby does not burp and is content. Breastfed babies overall don’t take in as much air during a feeding as bottle-fed babies do, so usually don’t need to burp as often. If baby has been crying before she nurses, or is so hungry that she nurses “frantically” or if mom has a fast let-down, baby could be taking in more air and may need to be burped more often.
Burping is usually only necessary during the first few months, though it may extend longer. Once your baby is moving more freely, she will be able to relieve the gastric gas herself. This usually will occur between the 4th and 6th month, but may be shorter in some children and longer in others.
If baby has a hard time burping, try burping more often during a feeding. The best burping position is one that applies firm pressure to the baby’s tummy. Placing baby over the shoulder way up so that there is pressure on baby’s abdomen often works well. Walking around while doing this might distract her long enough to get a good burp. You may even want to lie baby down on her stomach and burp her that way.
The best burping position is one that applies firm pressure to the baby’s tummy. Placing baby over the shoulder way up so that there is pressure on baby’s abdomen often works well. Walking around while doing this might distract her long enough to get a good burp. You may even want to lie baby down on her stomach and burp her that way.
Growth spurt
Babies often pull off and fuss during growth spurts. Most babies go through growth spurts, sometimes called frequency days, during the first few days at home and around 7-10 days, 2-3 weeks, 4-6 weeks, 3 months, 4 months, 6 months and 9 months (more or less). More growth spurt information in this link.
Distractible baby
If baby seems to be pulling off the breast at any distraction (real or imaginary), then see The Distractible Baby.
Forceful let-down
Some babies will pull off the breast soon after let-down if mom has a forceful let-down. Baby may be frustrated by the too-fast flow of milk with let-down. A too-forceful let-down can also cause excessive gas or spitting up/vomiting. There is more information here on symptoms of and how to deal with a fast let-down reflex.
A too-forceful let-down can also cause excessive gas or spitting up/vomiting. There is more information here on symptoms of and how to deal with a fast let-down reflex.
Slow let-down
Some babies get very impatient if mom has a slow let-down. There is more information here on speeding up a slow let-down reflex.
Baby wants a faster milk flow
Even very young babies can be quick to notice that pulling off, kneading the breast, etc. can cause an additional let-down, and can facilitate a faster, easier milk flow. Some babies become impatient with the slower milk flow following the initial fast flow at let-down. This may or may not be related to a slow let-down.
When a feeding begins at the breast there are drops of milk. Then when the initial let-down occurs (several seconds to a minute into the feeding), the milk flow speeds up quite a bit. At that time it may drip very quickly, squirt, or even spray. Some minutes later it slows again and the baby must continue to suck vigorously in order to elicit further let-downs. This pattern can continue through successive, multiple let-downs as long as the baby is continuing to nurse vigorously. Eventually, baby will learn that the flow will pick back up again if she’ll only continue to vigorously suck/swallow.
This pattern can continue through successive, multiple let-downs as long as the baby is continuing to nurse vigorously. Eventually, baby will learn that the flow will pick back up again if she’ll only continue to vigorously suck/swallow.
With bottle feeding, the flow is instant and continuous. The baby is required to work very little. Once a baby has had a bottle, especially a lot of bottles, she may begin to prefer the ease of bottle-feeding over the work of breastfeeding. She may become frustrated at the breast after the first let-down occurs and the flow of milk begins to slow.
If baby is getting bottles you might consider putting them away, at least for a while. When you must use a bottle, only use a newborn nipple for as long as baby will tolerate it so that she never gets a really fast flow of milk from the bottle, but has to work a little more to get the milk.
Sometimes babies of moms with oversupply or fast let-down will also get very used to the fast flow and object when it normally slows somewhere between 3 weeks to 3 months.
It can be helpful to do some breast compression when this fussiness starts or right before you expect it to. This will help speed up the milk flow again. Once compression stops helping, try switching baby to the other side when she begins to fuss and back and forth again (after using compression) as you need to.
Baby is done nursing for the moment
If baby is fussing after she’s been nursing for a while, and you’ve ruled out other causes, she may be in the process of changing her nursing pattern. Babies become very efficient at the breast with growth and maturity. They can milk the breast in a lot less time per feeding session than they required before. Baby’s frustration may just be a sign that she’s finished and wants to move on.
On a similar note, an occasional baby will just want to suck at the end of a nursing session and the flow of milk with let-down frustrates her. You might see if offering her a finger or pacifier (if baby is older than 4-6 weeks) to suck on during these times seems to help.
Baby prefers one side
Sometimes babies will refuse or fuss at a breast when the let-down is slower or too forceful, or the supply a bit lower. They in turn will prefer the side which lets down more/less quickly and in which the supply is more bountiful. See also: Lopsided! What can I do?
Fussy in the evening
Many young babies tend to pull off and fuss at the breast in the evening. See the article Cluster Feeding and Fussy Evenings.
Teething
Teething can cause fussy nursing behavior, as some babies experience gum discomfort with sucking. Baby might start to nurse, but then pull off and cry or fuss and not want to nurse anymore. See Teething for more information and tips.
Thrush
Frequent pulling off the breast can be a symptom of thrush.
Stuffy nose
A stuffy nose can cause fussy nursing behavior. If your baby has a stuffy nose and is having a hard time breathing and nursing at the same time, see colds & congestion.
Allergy or food sensitivity
Some babies with allergies or food sensitivities exhibit fussy nursing behavior. Often when there is a sensitivity to something in mom’s diet, baby will come to the breast hungry but when she tastes/smells something in the milk that will cause her GI distress, she pulls off, bats her head back and forth, etc. Sensitivities to foods in mom’s diet are rare. If this is the problem, you will most likely notice other symptoms, such as excessive spitting up or vomiting, colic, diarrhea, rash, persistent congestion or runny nose, or excessive gas. More information on food sensitivities in babies and links to more allergy information can be found in my article Dairy and other Food Sensitivities in Breastfed Babies.
Low milk supply
Low milk supply can cause baby to be fussy at the breast. If you feel that your milk supply may be low, see this page for more info: Increasing low milk supply.
Reflux
Reflux can result in baby being fussy at the breast. See Reflux and Breastfeeding for more information.
See Reflux and Breastfeeding for more information.
Tongue-Tie
Tongue-Tie can result in baby being fussy at the breast. See Breastfeeding a Baby with Tongue-Tie (Resources) for more information.
Solving nine breastfeeding problems in the first month
Expert advice on solving major breastfeeding problems in the first month.
Share this information
Cathy Garbin, child health nurse, midwife and lactation consultant:
Cathy, a mother of two, was a research fellow at the renowned Human Lactation Research Institute, founded by Peter Hartmann, for seven years, providing support to breastfeeding mothers in clinics and at home. Today, she still works as a family counselor, and also conducts seminars for attending physicians and speaks at international conferences. nine0003
Breastfeeding is as much a skill as driving a car, and in the first month mother and baby may encounter some obstacles along the way. It takes time and experience to make it familiar to both of you. Solving breastfeeding problems in the first month helps to establish good milk production and increase the duration of breastfeeding in the future. Below you will find tips on how to overcome the main breastfeeding challenges that mothers often face from the end of the first week to the end of the first month after giving birth. nine0003
It takes time and experience to make it familiar to both of you. Solving breastfeeding problems in the first month helps to establish good milk production and increase the duration of breastfeeding in the future. Below you will find tips on how to overcome the main breastfeeding challenges that mothers often face from the end of the first week to the end of the first month after giving birth. nine0003
Problem #1. A painful lump appeared in the breast
Lumps and lumps in the breast of a nursing woman can appear for various reasons. One of the most common is blockage of the milk ducts, which results in a hard and painful lump that can become inflamed.
Solutions 1-3
- Massage the inflamed area, especially while breastfeeding or expressing, to clear the blockage. nine0027
- Gently apply warm flannel to your breasts or take a warm shower before feeding to relieve discomfort.
- Continue breastfeeding as usual to avoid milk accumulation that can cause mastitis.

- Try to express milk from the inflamed breast after feeding to ensure that it is completely emptied. This will help to remove the blockage and restore the patency of the duct. See what breast pumps* Medela has to offer and choose the right one for you. nine0027
- Try ultrasound therapy. If you have repeated blocked ducts, your lactation consultant or healthcare professional may suggest this procedure to help restore milk flow. The procedure is performed by a physiotherapist.
- Call your healthcare provider, if you notice signs of infection (breast redness and tenderness or flu-like symptoms such as fever, aches, malaise and headache), or if you think the lump is not related to breastfeeding . nine0027
Problem #2. The breast is red and sore
If one or both mammary glands are red and sore, and this is not due to blockage of the ducts, mastitis, that is, inflammation of the breast tissue, is not excluded.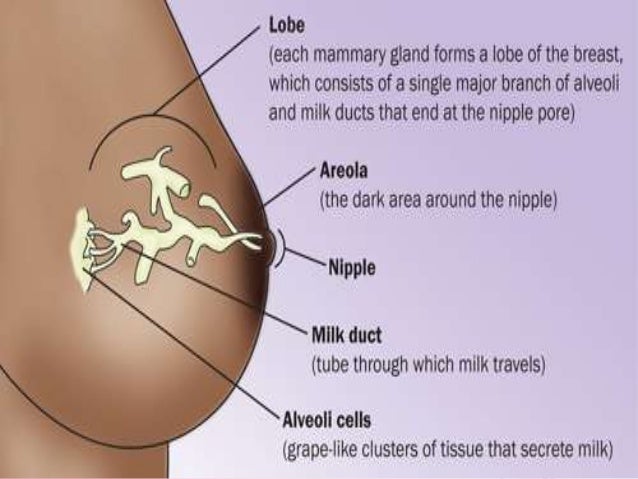 Mastitis is characterized by redness, burning, and soreness of the breasts, combined with flu-like symptoms: You feel hot and cold, your joints ache, and your temperature rises above 38.5 °C (101.3 °F). Seek medical attention immediately if you experience these symptoms. Mastitis needs to be treated as soon as possible, as your condition can worsen in just a few hours. nine0019 3
Mastitis is characterized by redness, burning, and soreness of the breasts, combined with flu-like symptoms: You feel hot and cold, your joints ache, and your temperature rises above 38.5 °C (101.3 °F). Seek medical attention immediately if you experience these symptoms. Mastitis needs to be treated as soon as possible, as your condition can worsen in just a few hours. nine0019 3
Mastitis can be caused by the following causes:
- untreated blocked ducts,
- Bacteria entering the breast through cracked and damaged nipples,
- incorrect attachment of the child to the breast,
- long periods between feedings,
- breasts too full,
- wearing a bra that is too tight or that cuts into the skin,
- Abrupt weaning,
- excess milk.
Solutions 3
In addition to seeking medical attention:
- Continue to breastfeed or express milk frequently.
 Your milk is still safe for your baby. Its release will help eliminate blockage of the ducts and prevent painful accumulation of milk. Sudden cessation of feeding or pumping may exacerbate symptoms. After feeding, it is advisable to express any remaining milk. nine0024 Give the child the inflamed breast first. This way the child can empty it completely. If it hurts too much, start feeding on the healthy breast, and when milk begins to flow, go back to the first one.
Your milk is still safe for your baby. Its release will help eliminate blockage of the ducts and prevent painful accumulation of milk. Sudden cessation of feeding or pumping may exacerbate symptoms. After feeding, it is advisable to express any remaining milk. nine0024 Give the child the inflamed breast first. This way the child can empty it completely. If it hurts too much, start feeding on the healthy breast, and when milk begins to flow, go back to the first one. - Have a good rest, drink and eat. You need to get enough fluids and good nutrition.
- Massage the sore area under a warm shower or apply a warm flannel or warm pack to clear the blockage and relieve symptoms before feeding or pumping. nine0027
- Apply a cooling pack after feeding, , to reduce inflammation.
Problem #3. My strength is running out
Breastfeeding in the first weeks can be very tiring and seem endless. The baby will ask for a breast every few hours, day and night, and you have not yet grown stronger after giving birth.
The baby will ask for a breast every few hours, day and night, and you have not yet grown stronger after giving birth.
Solutions
- Take care of yourself. This may be easier said than done when you have a newborn in your arms, but still try to get as much rest as possible, eat healthy and regular meals, and drink plenty of water. Do not refuse the help of your partner, relatives and friends, or even hire an assistant if you can afford it. nine0027
- Feed lying down. This will allow you to relax and reduce stress on sore spots, stitches or c-section scars.
- Do not skip feedings. Your partner may offer to bottle feed your baby while you are resting. However, despite this temptation, it should be remembered that milk production is best established in the first four weeks through breastfeeding. When breastfeeding is well established, you can give your baby expressed milk, but before that, ask family or friends to help you with other things so you can fully focus on breastfeeding.
 nine0027
nine0027
Problem #4. How can I increase breast milk production?
It's easy to question whether you're making enough breast milk, especially when your baby has developmental spikes between the third and fourth weeks. It may seem to you that the child asks for breasts more often because he does not have enough milk. However, if the number of wet and soiled diapers doesn't change—see Breastfeeding: What to Expect in the First Month—the baby is likely to breastfeed more often to calm down. The baby is surrounded by many new sounds and images that are easy to get tired of, and at the breast he feels safe. nine0019 4
Solutions 4.5
- Do not try to supplement your baby with formula, unless doctors are worried about weight gain or fluid loss. Continue breastfeeding your baby. This will help naturally increase breast milk production.
- Do not feed on a schedule. Feed your baby on demand.
 Thus, the production of breast milk will adapt to his needs. nine0024 Use the breast pump, , to help increase breast milk production while continuing to breastfeed.
Thus, the production of breast milk will adapt to his needs. nine0024 Use the breast pump, , to help increase breast milk production while continuing to breastfeed.
Problem #5. I have too much milk
Hyperlactation, or too much milk, can also be difficult for you and your baby. You may experience discomfort from swollen and leaking breasts, and your baby may have difficulty latch-on, choke on the milk flowing too fast, and be unable to empty the breast properly. nine0019 6
Solutions
- Express some breast milk at the start of a feed to reduce the force of the flush. Don't pump too much as this can aggravate the situation - pump only as much as needed to ease the discomfort. Try hand pumping or use a breast pump (check out the Medela* breast pump range and choose the right one for you).
- Use towel or pad to soak up excess milk, or place the Milk Collection Pad** on the other breast while you breastfeed first.
 nine0027
nine0027 - The child must feel supported. Hold him firmly (this gives a sense of security) and in a comfortable position so that he can turn his head. Talk to the baby during the first rapid flush, then he will not be frightened by surprise and will not push the breast.
- Contact a lactation consultant or health care professional who will monitor you and suggest single-sided feedings or hourly breast changes (“breast duty”) to normalize your milk supply. nine0027
- Be patient . Problems with milk production usually go away after a few weeks.
Problem #6. I have different breasts!
You have noticed that the baby has a preference for one breast, or that one breast produces more milk than the other, and as a result, the mammary glands have become of different sizes and shapes. This happens quite often and does not pose any problems for breastfeeding. If this does not bother you or your baby, you can leave everything as it is. If this makes you uncomfortable, try the following tricks. nine0003
If this makes you uncomfortable, try the following tricks. nine0003
Solutions
- During feeding, offer the less demanded breast first as babies usually suckle more vigorously at the beginning of feeding.
- Use the breast pump to increase breast milk production in the smaller breast.
- Don't give up on bigger breasts. Breastfeeding should continue with fuller breasts to avoid blocked ducts and mastitis.
- See a doctor. Sometimes an ear infection is the reason for a baby to latch on only on one side. However, some positions may cause him discomfort, so try to keep the child more upright. In addition, a breast infection can change the taste of milk and cause milk to be rejected as well.
Problem #7. A blister has appeared on the nipple
With frequent feeding, sometimes painful friction occurs, and a blood blister may appear on the breast,
nipple or areola. nine0019 7
nine0019 7
Solutions
- Ask a lactation consultant or specialist to check the baby's latch on. A shallow grip can cause blistering of the nipples and areolas.
- Talk to your doctor about what medicine you can take to relieve pain if needed.
- Try other feeding positions to avoid pressure on the painful area. nine0027
- Lubricate inflammation with pure lanolin.
- Use Breast Pads** to avoid rubbing your blister with clothing and help it heal faster with air circulation, or try cooling hydrogel pads** to help relieve pain and promote healing.
- Try expressing milk. Using a breast pump can be an alternative way to get breast milk without bladder irritation. Choose the correct funnel size so that the nipple can move freely and the bubble does not rub against the walls of the tunnel.
 nine0027
nine0027 - Do not pierce the vial as this may lead to infection.
- Seek medical attention, if the problem persists and causes you pain.
Problem #8. Painful white spot on nipple
When the orifice of the milk duct becomes blocked with milk or a thin layer of skin grows over it, a small white or yellowish spot may appear on the tip of the nipple. For some, these blocked ducts, sometimes called milk vesicles or blisters, cause pinpoint pain, especially during feeding or pumping. Others do not experience any discomfort. White blisters may persist for several days or weeks until the skin breaks and hardened milk comes out. nine0019 8
Solutions
- Follow the tips above to solve friction bubble problems.
- Remove the blockage, if you see that the milk cork is starting to bulge. Try to squeeze it out very gently with clean nails.

- Continue breastfeeding or pumping, to clear the milk duct. If the milk duct clears during feeding, it will not harm the baby in any way. nine0027
- Apply hot wet flannel to the vial just before feeding or pumping. This will help open the blocked duct. You can also try rubbing the area quickly with a clean, damp cloth.
- Manually express some milk before feeding, trying to push out hardened milk clots. If this does not help, feed the baby or express milk as usual. Repeat several times a day.
- Soak a cotton swab with olive oil and place it in the bra, pressing it against the bubble nipple. This will help soften the skin.
- Seek medical attention, if problem persists. Your doctor may remove the plug with a sterile needle. This should be done immediately after feeding, when the bubble is as inflated as possible.
Issue #9. My nipples hurt while breastfeeding
At the start of breastfeeding, my nipples may become more tender, sore, and even inflamed, but this usually goes away after a few days. If your baby's latch is checked by a specialist and the inflammation persists or the nipples hurt with every feeding, you may need medical attention to resolve this problem. nine0019 2.7
If your baby's latch is checked by a specialist and the inflammation persists or the nipples hurt with every feeding, you may need medical attention to resolve this problem. nine0019 2.7
The following symptoms and signs that appear on one or both breasts during or after feeding may indicate a bacterial infection or thrush:
- burning, itching or moderate to severe pain in the nipples
- pain in nipples aggravated by contact with clothing,
- nipple pain persists despite attempts to attach baby differently,
- nipples hurt to touch, nine0024 stitching, shooting, burning or deep aching pain,
- chest pain during feeding and almost an hour after,
- hot pink nipples,
- discoloration and texture of the areola (hot pink, darkening, dryness or peeling),
- white rash on chest or areola.
Also check if your child has the following symptoms and signs:
- hard white patches or coating on the tongue,
- white indelible spots on the cheeks,
- bright red spotted rash on buttocks not helped by diaper rash creams.
Solutions 7
- Seek medical attention. He will most likely suggest testing for infections to make a diagnosis. Bacterial and fungal (yeast) infections are treated differently, so appropriate treatment should be started as soon as possible. There are other reasons that can cause similar nipple pain, such as eczema, psoriasis or vasospasm (narrowing of the blood vessels) in the mother and problems with latch or tongue frenulum in the child. Therefore, it is very important to make an accurate diagnosis. nine0027
- Strict hygiene. Wash hands before and after feeding and applying any medication, and after changing diapers. Change bra pads regularly, wash bras, tank tops and towels in high temperature water, thoroughly wash breast cups and anything your baby puts in her mouth, such as nipples.
- Let the nipples dry after feeding, as all infections love a warm and humid environment.
 nine0024 See your doctor again if there is no improvement after a few days. Do not let the problem run its course, otherwise the situation may worsen.
nine0024 See your doctor again if there is no improvement after a few days. Do not let the problem run its course, otherwise the situation may worsen.
Related materials. Breastfeeding: what to expect in the first month
Breastfeeding: what to expect after the first month
Breastfeeding problems after the first month
Literature
1 Academy of Breastfeeding Medicine Protocol Committee. ABM clinical protocol # 20: Engorgement. Breastfeed Med. 2009;4(2):111-113.- Breastfeeding Academy Protocol Committee, "AVM Clinical Protocol #20: Breast engorgement." Brestfeed Med (Breastfeeding Medicine). 2009;4(2):111-113.
2 Jacobs A et al. S3-guidelines for the treatment of inflammatory breast disease during the lactation period. Geburtshilfe and Frauenheilkunde . 2013;73(12):1202-1208. - Jacobs A. et al., "Recommendations 2014;9(5):239-243.
4 Kent JC et al. Principles for maintaining or increasing breast milk production. 2012;41(1):114-121. - Kent J.S. et al., "Principles for Maintaining and Increasing Milk Production". G Obstet Ginecol Neoneutal Nurs. 2012;41(1):114-121. nine0361
5 Amir L. Breastfeeding managing ‘supply’ difficulties. Aust fam physician . 2006;35(9):686. - - Amir L., "Breastfeeding: problems of 'supply'. Aust fam physis. 2006;35(9):686.
6 Trimeloni L, Spencer J. Diagnosis and management of breast milk oversupply Journal Am Board Fam Med . 2016;29(1):139-142. - Trimeloni L., Spencer J., "Diagnosis and correction of excess breast milk production." Journal Am Bord Fam Med. 2016;29(1):139-142.
7 Berens P et al. Academy of Breastfeeding Medicine. ABM Clinical Protocol# 26: Persistent pain with breastfeeding. Breastfeed Med. 2016;11(2):46-53. - Behrens, P. et al., Academy of Breastfeeding Medicine, AVM Clinical Protocol #26: Persistence of Breastfeeding Pain. Brestfeed Med (Breastfeeding Medicine). 2016;11(2):46-53. nine0361
Academy of Breastfeeding Medicine. ABM Clinical Protocol# 26: Persistent pain with breastfeeding. Breastfeed Med. 2016;11(2):46-53. - Behrens, P. et al., Academy of Breastfeeding Medicine, AVM Clinical Protocol #26: Persistence of Breastfeeding Pain. Brestfeed Med (Breastfeeding Medicine). 2016;11(2):46-53. nine0361
8 Australian Breastfeeding Association [Internet] White spot nipple; March 2015 [Accessed 02/08/2018]. - Australian Breastfeeding Association [Internet], "White spots on the nipples", March 2015 [visited 02/08/2018].
Read instructions before use. Consult a specialist about possible contraindications.
* RU № ФСЗ 2010/06525 of 03/17/2021
** RU ФСЗ 2010/07352 of 07/19/10
0001
“Recommend a mammologist!”
If you are a breastfeeding mother, you probably don't have much time. The child “hangs” on the chest, you get tired like never before in your life, you don’t often manage to sleep normally. What to say about the "campaigns" to the doctors.
What to say about the "campaigns" to the doctors.
It's much easier to go to the Internet, type in a symptom in a search engine, ask for advice on the mothers' forum.
However, who guarantees that the advice will be correct and the condition will not worsen? The mammologists of our center understand your concerns and are ready to solve all the issues that arise with breastfeeding mothers. nine0003
You are breastfeeding. What's going wrong?
Not enough milk
| You think you don't have enough milk. |
| Violation of the rhythm of feeding, improper attachment, overwork. |
| The child is restless, gains or loses weight poorly. nine0540 nine0540 |
| Breastfeed more frequently, consult a mammologist and lactation consultant. |
Too much milk
| | You think there is too much milk. |
| Individual features, excess prolactin. nine0540 |
| Too much milk is produced. |
| Change the rhythm of feeding, freeze excess milk, consult a mammologist and endocrinologist. |
Teat fissure
| Pain during feeding, skin defect, blood. nine0540 nine0540 |
| Heavy workload, slow recovery. |
| Limit feeding to this breast for the duration of treatment, express adequately when filling, consult a doctor for anti-inflammatories, antibiotics and physiotherapy as indicated. nine0003 |
Milk stasis
| What's bothering you? | Pain and distension in the chest. |
| Possible causes? | Ejection of milk is uneven in different parts of the gland, there is no muscular wall in the milk ducts, and the outward movement of milk is also uneven. The ducts may be compressed or twisted. |
| How does it manifest itself? | Painful, tight-elastic lump in the breast, does not disappear after feeding, without fever and redness. nine0540 nine0540 |
| What to do? | Change position during feeding, pumping, applying ice, consult a mammologist, do ultrasound, microflora culture (bacteria culture), discharge cytology |
| What worries you? | Depends on the stage - first, a painful focus of compaction, a decrease in the amount of milk, an increase in body temperature up to 38 degrees. nine0002 Further, the focus increases, there is swelling of the skin, axillary lymph nodes, high temperature, impurities in the milk. Further, redness joins, swelling increases, weakness, drowsiness, palpitations, the amount of impurities increases. |
| Possible causes | Unemptied stagnation, curdling of milk and clogging of the duct, penetration of infection through cracks leads to mastitis. |
| How does it manifest itself? | Depends on the stage - painful, stony density, swollen gland, redness of the skin, increased body temperature, symptoms of general intoxication, lactation is sharply reduced.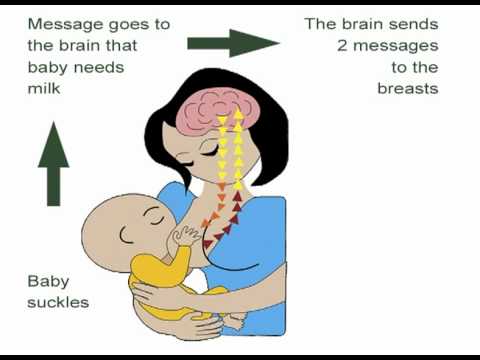 nine0540 nine0540 |
| What to do? | Seek immediate medical attention, often requiring hospitalization and surgical treatment. |
There is a hardening in the chest, it does not hurt
| What worries | Abruptly appeared soft and painless mass in the mammary gland, the condition is not disturbed. |
| Possible causes | Lactocele is an acute accumulation of milk in an overdistended duct. nine0540 |
| How it manifests itself | The formation is soft-elastic, painless, appeared acutely, lactation is preserved. |
| What to do | Contact a mammologist, you need ultrasound, aspiration of contents with cytology. |
Breast lump, spotting
| Painless, firm mass without clear contours in the presence of normal lactation. | |
| Possible causes? | Suspicion of an oncological process due to hormonal changes during lactation. |
| How does it manifest itself? | The formation is dense, painless, axillary lymph nodes are enlarged, lactation is preserved, there is bloody discharge from the nipple. |
| What to do? | Consult a mammologist, you need ultrasound, mammography, biopsy, cytology, histology, complex examination. |
How not to waste a breastfeeding mother's precious time? The CMC offers:
• Consultations of a competent mammologist with more than 15 years of experience with nursing mothers.
• Assistance in organizing breastfeeding - for ordinary issues we involve our consultant, in difficult situations - with the participation of our mammologist.
• Complete examination in 1-2 visits – we perform ultrasound, mammography, cultures, cytology and histology. nine0003
• Treatment of breastfeeding according to world standards: we perform therapeutic fine needle biopsy, therapeutic massage and pumping for lactostasis, conservative and surgical treatment.
1. What should a breastfeeding mother eat?
It is best if your diet is complete, balanced in proteins, fats and carbohydrates. It is advisable to drink fluids at least 2 liters per day. Milk will come to you more actively if you drink a cup of warm tea with milk before feeding. nine0003
2. What underwear to wear?
Choose by bust size and quality. Best of all - on a wide supporting strap, you can sport a cut. Your bra should not be constricting under your armpits or tight under your bust. The composition of the fabric is cotton.
3. What should I do to avoid cracks and mastitis?
Maintain good hygiene. Apply a natural cream on the nipples with a healing and moisturizing effect after each feeding, preferably without strong odors.

 Enlarged axillary lymph nodes on one or both sides. Bloody discharge from the nipples of one or both glands. nine0003
Enlarged axillary lymph nodes on one or both sides. Bloody discharge from the nipples of one or both glands. nine0003