Baby reflux after every feed
Reflux | Breastfeeding Challenges | Start for Life
Breastfeeding challenges
There may be times when breastfeeding is challenging. Never ignore any issues you may have – talk to your health visitor, midwife, GP or breastfeeding specialist as soon as possible, they will be able to help you sort it out quickly.
Here are some common breastfeeding issues, and tips on what to do.
- Colic
- Constipation
- Mastitis
- Milk supply
- Reflux
- Sore nipples
- Thrush
- Tongue-tie
Baby reflux
If your baby brings up milk, or is sick during or after feeding, this is known as reflux. Reflux, also called posseting or spitting up, is quite common and your baby should grow out of it, usually by the time they are 12 months old.
What causes baby reflux?
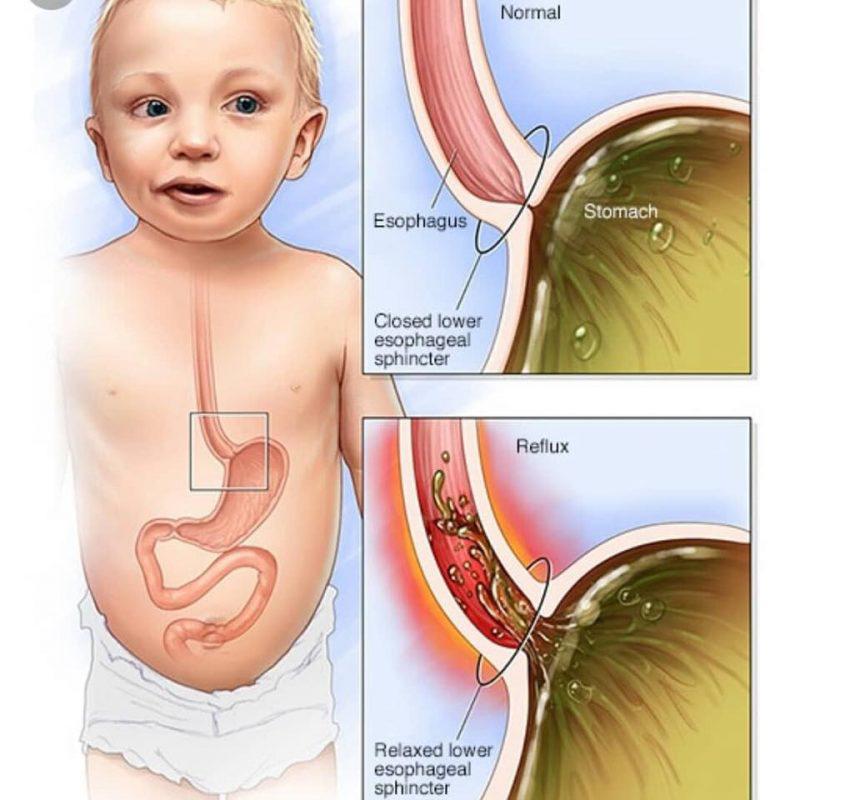
The muscle at the bottom of the food pipe acts as a kind of door into the stomach – so when food or milk travels down, the muscle opens allowing the food into the stomach.
However, while this muscle is still developing in the first year, it can open when it shouldn't (usually when your baby's tummy is full) allowing some food and stomach acid to travel back up again. Acid in the stomach is normal and a necessary part of the digestion process – it helps break down food.
In most babies, reflux is nothing to worry about as long as they are healthy and gaining weight as expected.
Baby reflux symptoms
- Constant or sudden crying when feeding.
- Bringing up milk during or after feeds (regularly).
- Frequent ear infections.
- Lots of hiccups or coughing.
- Refusing, gagging, or choking during feeds.
- Poor weight gain.
- Waking up at night a lot.
GORD
When reflux becomes painful and it happens frequently, this is known as 'gastro-oesophageal reflux disease' (GORD). GORD is more serious than mild, everyday reflux. The strong stomach acid can irritate and make the food pipe sore and inflamed, which is painful for your baby and may result in them needing medication.
The main signs and symptoms of GORD in your baby are:
- spitting up frequently
- abdominal pain
- feeding difficulties
- seeming unsettled and grizzly after a feed
These symptoms can lead to your baby not gaining weight, or even losing weight.
Silent reflux
Silent reflux can be confusing as there are no obvious signs or clues (such as spitting up). It's when the food travels back up the food pipe – but it's swallowed rather than spat out so is harder to identify. But your baby may display similar symptoms to those of regular reflux.
Breastfeeding Friend from Start for Life
The Breastfeeding Friend, a digital tool from Start for Life, has lots of useful information and expert advice to share with you – and because it's a digital tool, you can access it 24 / 7.
Breastfeeding tips for babies with reflux
- Feeding little and often (smaller feeds stop their tummy getting too full).
- Burping them requently during feeds – have a look at our guide to burping your baby for techniques.
- Try a different feeding position – check out our our guide to breastfeeding positions.
- Keep your baby upright, for at least an hour after feeding, this should help keep the milk down.
If you are mixed feeding (combining breastmilk and formula feeds), have a look at our advice on bottle feeding and reflux.
When to see the GP
If your baby has difficulty feeding or refuses to feed, regularly brings milk back up and seems uncomfortable after a feed, talk to your pharmacist, GP, or health visitor. They'll be able to give you practical advice on how to ease the symptoms and manage it – they may also need to rule out other causes (such as cow's milk allergy).
It might be helpful to keep a record of when your baby feeds, with details of how often and how much your baby brings the food back up, and how often your baby cries or seems distressed. This will help your health visitor or GP decide if your baby needs treatment.
Reflux in babies - NHS
Reflux is when a baby brings up milk, or is sick, during or shortly after feeding.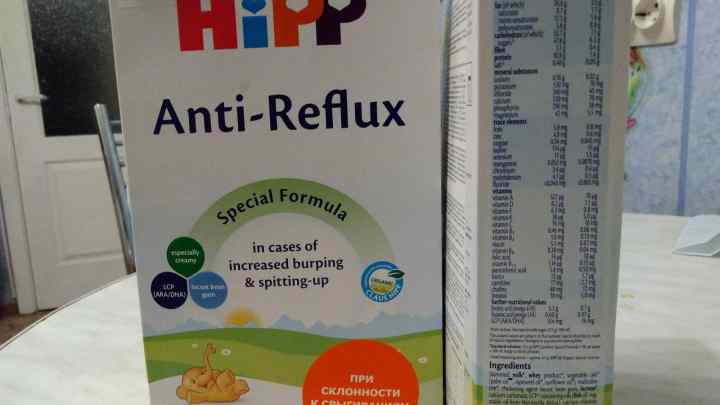 It's very common and usually gets better on its own.
It's very common and usually gets better on its own.
Check if your baby has reflux
Reflux usually starts before a baby is 8 weeks old and gets better by the time they're 1.
Symptoms of reflux in babies include:
- bringing up milk or being sick during or shortly after feeding
- coughing or hiccupping when feeding
- being unsettled during feeding
- swallowing or gulping after burping or feeding
- crying and not settling
- not gaining weight as they're not keeping enough food down
Sometimes babies may have signs of reflux but will not bring up milk or be sick. This is known as silent reflux.
Things you can try to ease reflux in babies
Your baby does not usually need to see a doctor if they have reflux, as long as they're happy, healthy and gaining weight.
Do
-
ask a health visitor for advice and support
-
get advice about your baby's breastfeeding position or how to bottle feed your baby
-
hold your baby upright during feeding and for as long as possible after feeding
-
burp your baby regularly during feeds
-
give formula-fed babies smaller feeds more often
-
make sure your baby sleeps flat on their back (they should not sleep on their side or front)
Non-urgent advice: See a GP if your baby:
- is not improving after trying things to ease reflux
- gets reflux for the first time after they're 6 months old
- is older than 1 and still has reflux
- is not gaining weight or is losing weight
Urgent advice: Ask for an urgent GP appointment or call 111 if your baby:
- has vomit that's green or yellow, or has blood in it
- is projectile vomiting (being sick with more force than usual)
- has blood in their poo
- has a swollen or tender tummy
- has a very high temperature or they feel hot or shivery
- keeps being sick and cannot keep fluid down
- has diarrhoea that lasts for over a week or has signs of dehydration
- will not stop crying and is very distressed
- is refusing to feed
Also call your GP or 111 if you have any other concerns about your baby.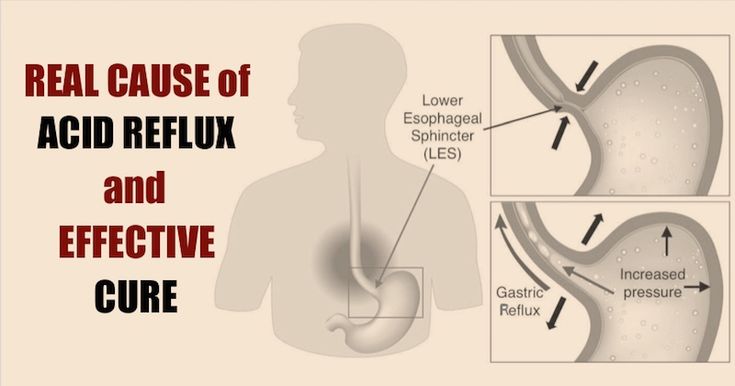
Treatment for reflux in babies
A GP or specialist may sometimes recommend treatments for reflux.
If your baby is formula-fed, you may be given:
- a powder that's mixed with formula to thicken it
- a pre-thickened formula milk
If the thickening powder does not help or your baby is breastfed, a GP or specialist might recommend medicines that stop your baby's stomach producing as much acid.
Very rarely, surgery might be needed to strengthen the muscles to stop food or milk travelling back up. This is usually only after trying other things or if their reflux is severe.
Causes of reflux
Reflux usually happens because your baby's food pipe (oesophagus) has not fully developed, so milk can come back up easily.
Your baby's oesophagus will develop as they get older and the reflux should stop.
Page last reviewed: 13 December 2021
Next review due: 13 December 2024
GASTROESOPHAGEAL REFLUX: FROM NORM TO PATHOLOGY
If your child often suffers from acute respiratory diseases, it may be time for you, do not be surprised, to contact a gastroenterologist. Today we will talk about gastroesophageal reflux (GER) with Ph.D., head of the pediatric department of the Consultative and Diagnostic Center of the Children's Hospital No. G.N. Speransky Elena Vladislavovna Vigurzhinskaya, who will tell you why it is impossible to give yogurt to a child at night, which children with GERD also need the treatment of a neurologist.
Gastroesophageal reflux, or GER, is the backflow of contents from the stomach into the esophagus. Curious fact: Symptoms of reflux in children under 7 years of age are associated with structural features of the upper gastrointestinal tract and the immaturity of the sphincter apparatus of the digestive system. Please note: Reflux in children under one year old is a regurgitation syndrome. Spitting up to a tablespoon after each feeding is a variant of the norm. If the baby spits up in a larger volume, sometimes not immediately after feeding, and at the same time begins to gain weight poorly, then in this case a correction is already required - there are therapeutic, anti-reflux mixtures for this (if the child is artificially fed). Important: During the first months of a breastfed child's life, the mother must follow a strict hypoallergenic diet with a restriction of dairy, sweet foods and foods that increase gas formation: legumes, yeast bread, pastry, grapes, mushrooms, etc. With increased gas formation, reflux in babies it intensifies and frequent regurgitation occurs.
Please note: Reflux in children under one year old is a regurgitation syndrome. Spitting up to a tablespoon after each feeding is a variant of the norm. If the baby spits up in a larger volume, sometimes not immediately after feeding, and at the same time begins to gain weight poorly, then in this case a correction is already required - there are therapeutic, anti-reflux mixtures for this (if the child is artificially fed). Important: During the first months of a breastfed child's life, the mother must follow a strict hypoallergenic diet with a restriction of dairy, sweet foods and foods that increase gas formation: legumes, yeast bread, pastry, grapes, mushrooms, etc. With increased gas formation, reflux in babies it intensifies and frequent regurgitation occurs.
- In some children, over time, reflux becomes pathological and triggers a cascade of many other problems, including the child suffering from frequent, viral infections, ENT diseases - explains Elena Vladislavovna Vigurzhinskaya . - This happens because when gastric contents (gastric secretion or food bolus) are thrown into the esophagus and, possibly, into the oropharynx, the pH changes, the flora of the oral cavity is disturbed and local immunity decreases, and the child falls into the so-called group "frequently ill children". In older children, GER clinically manifests itself in the form of heartburn, belching (air and food) Parents may also experience bad breath
- This happens because when gastric contents (gastric secretion or food bolus) are thrown into the esophagus and, possibly, into the oropharynx, the pH changes, the flora of the oral cavity is disturbed and local immunity decreases, and the child falls into the so-called group "frequently ill children". In older children, GER clinically manifests itself in the form of heartburn, belching (air and food) Parents may also experience bad breath
Important: Plaque on the teeth, geographical tongue, bad breath, frequent ENT pathologies, croup and obstructive bronchitis are a serious reason to seek advice from a gastroenterologist!
Interesting fact: In impulsive and emotional children, GER may be more pronounced. In this case, the child will fall into the hands of not only a gastroenterologist, but also a neurologist.
Factors contributing to the development of GER : anatomical features of the structure of the upper gastrointestinal tract in young children, morpho-functional immaturity of the sphincter apparatus, hereditary predisposition, stressful situations, great physical and psychological stress, violation of the daily routine, malnutrition.
– If you undergo treatment, adjust your diet and adjust your daily routine, then you can get rid of GER, says the head of the pediatric department. - Do not give your child sour foods at night. Previously, kefir was advised to children at bedtime, but this dairy product acidifies the stomach and acts aggressively. With reflux, we do not recommend acidic foods (and especially before bedtime) - yogurt, kefir, as well as juices, sour berries and fruits. You can drink fermented baked milk or eat neutral yogurt in the afternoon. But in general, I recommend limiting acidic foods, including dairy products.
How is GER detected? The specialist decides on an individual basis which test to order. First of all, taking an anamnesis: the doctor asks the parents about the child's complaints. Then, an ultrasound examination of the abdominal cavity is prescribed (strictly on an empty stomach, do not brush your teeth) with a water-siphon test. Fibrogastroduodenoscopy and a chest x-ray with barium may be prescribed.
Treatment of GER: Gastroenterologists prescribe prokinetics, antacids, proton pump inhibitors (drugs that reduce the production of hydrochloric acid by stomach cells)
. Important: Gastroesophageal reflux can be a symptom of Helicobacter pylori infection. Therefore, first of all, it is necessary to identify and remove the bacterium. Another possible cause of reflux is a gastrointestinal form of food allergy. Keeping a food diary will help parents understand what kind of “inedible” product the child’s stomach is trying to get rid of.
What happens if GER is not treated? It is possible to develop a chronic condition that can lead to inflammation, erosions and even ulcers in the esophagus, the replacement of normal cells in the esophagus by pathological ones.
- I repeat that a diet and a healthy daily routine must be maintained for life, - says the gastroenterologist. - The child needs fractional nutrition. You can not overeat, eat dry food, drink food best with water, weak tea, compote (pear, apple).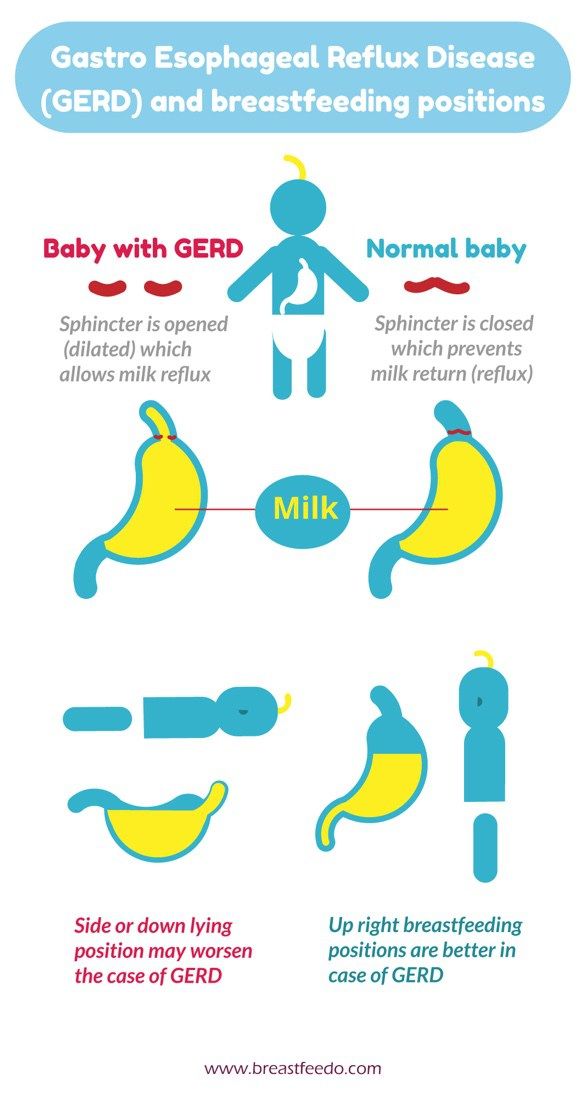 It is also not recommended to go to bed on a full stomach. Chocolate and buns, alas, are banned.
It is also not recommended to go to bed on a full stomach. Chocolate and buns, alas, are banned.
Infant Reflux: Symptoms and Treatment
Search Support IconSearch Keywords
Home ›› What is Reflux in Infants?
Home ›› What is reflux in babies?
↑ Top
Signs and what to do
Post-feed regurgitation is a common occurrence in the first few months of life. This is usually harmless and completely normal, but parents should read about gastroesophageal reflux (GER) and laryngopharyngeal reflux (LPR) in infants and how long it lasts to give them peace of mind.
We look at signs of reflux in babies, symptoms of different types of reflux, and how to help a child with signs of reflux. If you require further information, always contact your healthcare provider.
What is reflux in babies?
So we know reflux is common, but what causes reflux in babies? Because young children have not yet fully developed the lower esophageal sphincter (LES), that is, the muscle at the bottom of the esophagus that opens and closes to let food into the stomach and keep it there, food can easily pass back up the esophagus.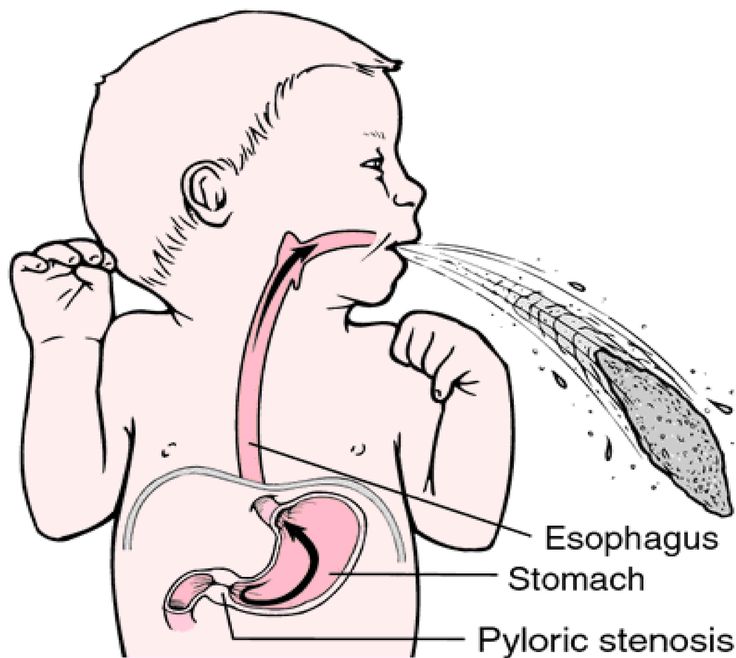
Acid reflux, also known as gastroesophageal reflux (GER), is a normal reflux that occurs in babies. This type of reflux is considered normal and occurs in 40-65% of babies.
How do I know if my child has acid (gastroesophageal) reflux?
If a baby is spitting up milk after a feed, it is most likely acid reflux. As babies get older, GER usually goes away on its own without any intervention. If a baby has complications beyond just spitting up a small amount of milk (such as feeding difficulties and discomfort), they may have gastroesophageal reflux disease (GERD).
Symptoms of GERD include:
- baby arching during or after feeding;
- crying more than three hours a day for no apparent reason;
- cough;
- gag reflex or difficulty swallowing;
- irritability, restlessness after eating;
- eating little or not eating;
- poor weight gain or loss;
- difficult breathing;
- severe or frequent vomiting.
GERD usually occurs when LES muscles are not toned in time, causing stomach contents to back up into the esophagus.
How do I know if my child has Laryngopharyngeal Reflux?
Another type of reflux, laryngopharyngeal reflux (LPR), also called silent reflux, is when the contents of a child's stomach leak back into the larynx, the back of the nasopharynx. This type of reflux does not always cause external symptoms, which is why it is called "silent". Babies can have GERD and silent reflux at the same time, but their symptoms are somewhat different.
The following are some of the symptoms of laryngopharyngeal reflux:
- breathing problems;
- gag reflex;
- chronic cough;
- swallowing problems;
- hoarseness;
- regurgitation;
- poor weight gain or weight loss.
We have looked at the signs of reflux in infants, now we will move on to the treatment and duration of silent reflux in children, as well as the treatment of GERD.
How to deal with laryngopharyngeal reflux in babies while breastfeeding?
Breastfeeding mothers may need to review their diet if their babies show signs of reflux. The American Academy of Pediatrics (AAP) recommends breastfeeding mothers cut eggs and milk from their diet for two to four weeks to see if their baby's reflux symptoms improve or disappear. It may be worth eliminating acidic foods from your diet.
In most cases, GER and laryngopharyngeal reflux go away on their own. Typically, children outgrow reflux in the first year of life. If a child has persistent symptoms of laryngopharyngeal reflux, parents should consult a doctor. If your baby is vomiting heavily, has blood in the stool, or has any of the symptoms of GERD listed above, parents should contact their pediatrician as soon as possible.
How can I help my child with reflux or GERD?
Reflux symptoms in babies usually go away on their own, but the following tips can help relieve symptoms:
- Thicken food with rice or a special milk thickener.

- Hold the bottle at an angle that fills the nipple completely with milk to reduce the amount of air your baby swallows. This can help prevent colic, gas, and reflux.
- Try the AirFree anti-colic bottle, designed to reduce air swallowing during feeding.
4. Let your baby burp during and after feeding. If the baby is bottle fed, parents can let him burp after every 30-60 ml. If the mother is breastfeeding, she may let the baby burp when changing breasts.
5. Hold baby upright after feeding. As a rule, in order for the milk to remain in the stomach, after feeding the baby, it is necessary to hold it in an upright position for 10-15 minutes. But, if the child has reflux, parents should keep him upright a little longer.
These tips may help relieve symptoms, but they do not replace a doctor's advice.
Parents should not change their infant formula formula without first talking to their healthcare provider.
Don't panic! Reflux is very common in babies during the first three months of life, and most babies outgrow it without any consequences.