Baby short of breath when feeding
Laryngomalacia (for Parents) - Nemours KidsHealth
What Is Laryngomalacia?
Laryngomalacia is a common cause of noisy breathing in infants. It happens when a baby's larynx (or voice box) is soft and floppy. When the baby takes a breath, the part of the larynx above the vocal cords falls in and temporarily blocks the baby's airway.
Laryngomalacia (luh-ring-oh-muh-LAY-shuh) usually gets better on its own by the time a baby is 1 year old.
What Are the Signs & Symptoms of Laryngomalacia?
Babies with laryngomalacia make a harsh, squeaky sound when breathing in. This sound, called stridor, can start as soon as the baby is born or, more often, in the first few weeks after birth. Symptoms usually get worse over several months.
Most babies with laryngomalacia do not have trouble breathing or feeding, even though their breathing is noisy. Breathing usually gets noisier when the baby is crying, feeding, sleeping, lying down, or has an upper respiratory infection.
Most babies with the condition have mild symptoms. A baby whose symptoms are more serious might have:
- trouble breathing (look for tugging in at neck or stomach)
- feeding problems
- poor weight gain
- breathing pauses (apnea)
- blue skin or lip color (cyanosis)
Call the doctor right away if your baby has these symptoms or breathing suddenly gets worse.
Babies with laryngomalacia often have gastroesophageal reflux (GER). This happens when food and acid go back up into the esophagus. If stomach acid reaches the voice box, symptoms may get worse. Formulas or medicines to help with reflux may help with breathing symptoms.
What Causes Laryngomalacia?
Doctors don't know what causes laryngomalacia, but it may have something to do with how the voice box formed before the baby was born. The muscles supporting the voice box may be weak or don't coordinate well with breathing. Gastroesophageal reflux may also play a role.
How Is Laryngomalacia Diagnosed?
Doctors often suspect laryngomalacia at birth or soon after based on the baby's symptoms and an exam. To confirm the diagnosis, a pediatric ear, nose, and throat (ENT) specialist will do a procedure called flexible laryngoscopy. To do this, the doctor passes a thin tube through the baby's nose or mouth to look at the airway and vocal cords in the voice box.
The doctor may check oxygen levels and order other tests to check for swallowing problems or GER. The baby's good weight gain and growth are very important.
How Is Laryngomalacia Treated?
Most of the time, laryngomalacia gets better on its own, usually by a baby's first birthday. Doctors will do regular exams to check the baby's breathing and weight. Because most babies also have GER, doctors usually prescribe anti-reflux medicine.
A baby who has severe breathing problems or poor growth may need a surgery called supraglottoplasty (soo-pruh-GLOT-oh-plass-tee). Doctors do this procedure through the baby's mouth to tighten the floppy tissue above the voice box. This will improve the baby's feeding and breathing.
This will improve the baby's feeding and breathing.
What Else Should I Know?
Noisy breathing and other laryngomalacia symptoms usually get worse over several months, then start to improve after 3–6 months. Symptoms clear up completely in most kids. Occasionally, an older child with a history of laryngomalacia may have noisy breathing while exercising, during a viral infection, or when sleeping.
Reviewed by: Steven M. Andreoli, MD
Date reviewed: October 2019
What’s Typical and When You Should See a Doctor
Newborns often make unusual noises while breathing. Most of them are no cause for concern. But being aware of your baby’s typical breathing pattern can help you identify any concerns early.
Newborns often have irregular breathing patterns that concern new parents. They can breathe fast, take long pauses between breaths, and make unusual noises.
Newborns’ breathing looks and sounds different from adults because:
- They breathe more through their nostrils than their mouth.

- Their breathing pathways are much smaller and easier to obstruct.
- Their chest wall is more pliable than an adult’s because it’s made of mostly cartilage.
- Their respiration isn’t fully developed since they still have to learn to use their lungs and the associated breathing muscles.
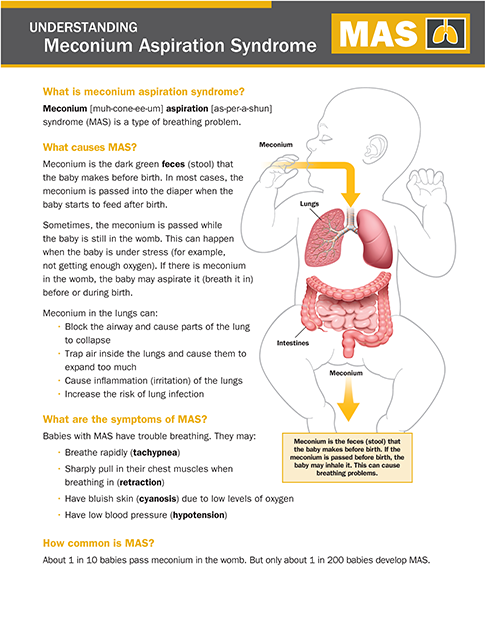
- They may still have amniotic fluid and meconium in their airways right after birth.
Usually, there’s nothing to worry about, but parents and caregivers may worry anyway.
One thing you can do is to pay careful attention to your newborn’s typical breathing pattern. This way you can learn what’s usual for them — so you’ll be able to tell if something is different later.
Typically, a newborn takes 30 to 60 breaths per minute. This can slow down to 30 to 40 breaths per minute while they sleep. At 6 months, babies breathe about 25 to 40 times per minute. An adult, meanwhile, takes about 12 to 20 breaths per minute.
Newborns can also take rapid breaths, then pause for up to 10 seconds at a time. All of this is very different from adult breathing patterns, which is why new parents might be alarmed.
All of this is very different from adult breathing patterns, which is why new parents might be alarmed.
Within a few months, most of the irregularities of newborn breathing resolve themselves.
Some newborn breathing concerns are more common in the first few days, such as transient tachypnea. But after 6 months, most breathing concerns are probably due to allergies or a short-term illness like the common cold.
It’s important that you become familiar with your baby’s typical breathing sounds and patterns. If something sounds different, listen carefully so you can explain what’s different to your pediatrician.
Respiratory distress is one of the most common causes of neonatal intensive care hospital admittance, according to 2020 research.
The following are common sounds you might hear and their potential causes.
Whistling noise
This might be a blockage in the nostrils that will clear when it’s suctioned (removed). Ask your pediatrician how to gently and effectively suction mucus.
Hoarse cry and barking cough
This noise may be from a windpipe blockage. It might be mucus or inflammation in the voice box, such as croup. It can be a sign of croup, in which case it may get worse at night.
Deep cough
This is likely a blockage in large bronchi. Large bronchi are tubes that carry air between the windpipe and lungs. A doctor will need to listen with a stethoscope to confirm this diagnosis.
Wheezing
Wheezing can be a sign of blockage or narrowing of the lower airways. The blockage might be caused by:
- asthma
- pneumonia
- respiratory syncytial virus
Fast breathing
This can mean there’s fluid in the airways from an infection, such as pneumonia. Fast breathing can also be caused by fever or other infections and should be evaluated right away.
Snoring
This is usually due to mucus in the nostrils. In rare cases, snoring can be a sign of a chronic condition, such as sleep apnea or enlarged tonsils.
Stridor
Stridor is a constant, high-pitched sound that indicates airway obstruction, according to 2021 research. It can sometimes be caused by laryngomalacia.
Grunting
A sudden, low-pitched noise on an exhale usually signals an issue with one or both lungs. It can also be a sign of severe infection. You should visit a doctor immediately if your baby is ill and is grunting while breathing.
Frequent sneezing
Sneezing is common in newborns and is not usually cause for concern.
This is because newborns have smaller nasal passages than adults and are still adjusting to breathing through their noses as they grow and develop.
If sneezing is accompanied by other symptoms like coughing, difficulty breathing, or a fever, you should talk with a doctor. It could be a sign of a respiratory infection, according to 2021 research.
Frequent sneezing can also be a sign of an allergy to certain types of formula as well as neonatal abstinence syndrome. Per 2020 research, neonatal abstinence syndrome occurs when babies are exposed to opioid drugs before birth.
Per 2020 research, neonatal abstinence syndrome occurs when babies are exposed to opioid drugs before birth.
Periodic breathing
Periodic breathing is common in newborns. It is characterized by pauses in breathing that lasts at least 3 seconds, followed by clusters of breaths, which are often fast and shallow.
This is typical and doesn’t usually require any treatment. However, if pauses in breathing last more than 20 seconds, it may indicate a problem such as infant apnea.
False “first cold”
Many newborns seem to experience symptoms of a false first cold very early, which occurs because their nasal passages are very small and can become easily clogged.
Though this doesn’t usually require any treatment, you may consider talking with a pediatrician about ways to help improve their breathing if needed, such as using saline drops or a nasal aspirator.
If your baby is also experiencing other cold symptoms like irritability, decreased appetite, or difficulty sleeping, it’s best to talk with a doctor to address any concerns and determine whether they may have a cold or other infection.
Hiccups
Hiccups are common and can happen in babies, children, and adults.
Eating too quickly and swallowing air while feeding are two of the possible causes of hiccups in newborns.
Hiccups may also be a symptom of gastroesophageal reflux, which occurs when the contents of the stomach flow into the esophagus, causing regurgitation.
Never hesitate to reach out to your doctor if you’re concerned about your baby’s breathing.
Irregular breathing can be very alarming and may cause anxiety in parents or caregivers. But first, slow down and look at your baby to see whether they look like they’re in distress.
Here are some tips if you’re concerned about your baby’s breathing:
- Learn your child’s typical breathing patterns so you’re better prepared to identify what’s not typical.
- Take a video of your baby’s breathing and show it to a doctor. Many medical professionals now offer online appointments or communication by email, saving you a possibly unnecessary trip to the office.

- Always have your baby sleep on their back. This decreases your baby’s risk of sudden infant death syndrome (SIDS), per 2021 research. If your baby has a respiratory infection and isn’t sleeping well, ask your doctor for safe ways to help clear congestion. It’s not safe to prop them up or put their crib on an incline.
- Saline drops, sold over the counter at drugstores, can help loosen thick mucus.
- Sometimes, babies breathe fast when they’re overheated or upset. Clothe your baby in breathable fabrics. You should only add one extra layer more than what you yourself are wearing for the weather that day. So, if you’re wearing pants and a shirt, your baby might wear pants, a shirt, and a sweater.
Safety note
Sleep positioners and wedges are not recommended while feeding or sleeping.
These padded risers are intended to keep your baby’s head and body in one position but are not recommended by the Food and Drug Administration due to the risk of SIDS.
Catching an issue early gives your baby the best chance for recovery in the short term and decreases future concerns.
A change in a newborn’s breathing pattern may indicate a serious breathing problem. If you’re ever concerned, call your doctor right away. Memorize the doctor’s after-hours phone numbers or have them available at all times. Most offices have a nurse on call that can answer and help direct you.
Doctors may use a chest X-ray to diagnose breathing concerns and make a treatment plan.
If your child experiences any of these symptoms, call 911 or your local emergency services:
- blue color in lips, tongue, fingernails, and toenails
- doesn’t breathe for 20 seconds or more
See your doctor immediately if your child:
- is grunting or moaning at the end of each breath
- has nostrils flaring, which means they’re working harder to get oxygen into their lungs
- has muscles pulling in on the neck, around collarbones, or ribs
- has difficulty feeding in addition to breathing issues
- is lethargic in addition to breathing issues
- has a fever as well as breathing issues
Babies tend to breathe faster than older kids and adults. Sometimes they make unusual noises. Rarely, infants may have trouble breathing because of a serious health concern.
Sometimes they make unusual noises. Rarely, infants may have trouble breathing because of a serious health concern.
It’s important that you can tell right away if your baby is having trouble breathing. Familiarize yourself with your baby’s usual breathing patterns and get help right away if something seems wrong.
Shortness of breath in children
Sometimes during emotional excitement, anxiety, fright, too active outdoor games, you may notice that your child's breathing rhythm is disturbed and there is a shortage of air. This is quite normal and appropriate for the situation. But if the baby has difficulty breathing in a calm state and with very slight physical exertion, we can talk about shortness of breath .
So what is this manifestation so familiar to us from a medical point of view?
Shortness of breath is a condition in which there is a failure of the respiratory rhythm, frequency and depth of breathing. In this case, the patient feels a short-term lack of air and shortness of breath.
In this case, the patient feels a short-term lack of air and shortness of breath.
Oddly enough, shortness of breath does not only occur in older or obese people. It can also apply to children. Such a lack of oxygen in a child is not an independent disease, but a symptom of ailments associated with a malfunction of various organs.
If you notice that your child's breathing rate is higher than normal, you can make an appointment for pediatrician to the multidisciplinary medical center "Medicenter" in St. Petersburg. After a careful examination and study of the anamnesis of a small patient, our qualified doctor will refer him to a narrow specialist, depending on the existing symptoms.
Main signs of shortness of breath in children:
- shortness of breath even without exercise;
- feeling short of breath;
- convulsive swallowing of air in a child;
- whistling or wheezing when breathing;
- rapid shallow breathing;
- chest breathing (in infants) and belly breathing (in children from 7 years of age).
If your baby develops shortness of breath after sports, brisk walking and other unusual physical activities and passes after a few minutes, then there is no need to worry. But in the case of low mobility, obvious obesity of the child or the presence of chronic diseases known to you, the nature of shortness of breath can be pathological and require mandatory consultation with a pediatric specialist, followed by treatment and elimination of the causes of this phenomenon.
There is no need to sound the alarm because of every uneven breath and failure in your child's breathing. But if you notice breathing problems in a baby regularly, regardless of his activity, you must definitely show the child to the doctor. Shortness of breath may be a symptom of the following diseases:
- bronchial asthma ;
- allergy ;
- lung diseases in a child;
- inflammation of the upper respiratory tract;
- false croup ;
- colds , viral diseases ;
- anemia in a child;
- oncological diseases ;
- diseases of the nervous system;
- congenital heart disease ;
- obesity;
- diseases of the thyroid gland;
- diabetes mellitus etc.
Inappropriate doses of medication can sometimes cause shortness of breath in children.
The treatment of dyspnea is prescribed depending on the diseases with which it accompanies. First of all, it is necessary to identify and eliminate the cause, and shortness of breath, as a rule, disappears along with the disease.
In case of many diseases, to eliminate shortness of breath, children are prescribed physiotherapy exercises , therapeutic massage , swimming, breathing exercises, physio - and psychotherapy .
Our clinics in St. Petersburg
Structural subdivision
Polikarpova
Alley Polikarpova 6k2
Primorsky district
- Pioneer
- Specific
- Komendantskiy
Structural subdivision
Zhukov
Marshal Zhukov Ave. 28k2
28k2
Kirovsky District
- Avtovo
- Veterans Avenue
- Leninsky Prospekt
Structural subdivision
Devyatkino
Okhtinskaya alley 18
Vsevolozhsk district
- Devyatkino
- Civil Avenue
- Academic
You can get detailed information and make an appointment by calling +7 (812) 640-55-25
Make an appointment
Shortness of breath in a child
Shortness of breath is rapid breathing that is significantly higher than normal. What should parents know about shortness of breath and how to behave when it appears in a child?
There are two types of shortness of breath in a child:
- Physiological.
 It may be present in the norm, for example, after intense physical activity or with the physiological immaturity of the respiratory center.
It may be present in the norm, for example, after intense physical activity or with the physiological immaturity of the respiratory center. - Pathological, that is, when there is a pathology of the organ. In this case, it is initially necessary to establish the cause of shortness of breath in order to prescribe etiotropic, and not just symptomatic therapy.
The main reasons why a child may experience shortness of breath:
- inflammation in the airways;
- pathology of the heart;
- pathology of ENT organs, more often adenoid hypertrophy;
- vegetative dystonia, hyperventilation syndrome;
- anemia;
- endocrine disorders;
- allergies;
- overweight.
Important! If in a small child (age - one and a half years) shortness of breath developed suddenly - you should exclude the ingress of a foreign body into the respiratory tract!
First aid - the "Pinocchio" technique: turn the child upside down, placing the baby on his forearm, pat him on the back.
A child with complaints of shortness of breath can be seen by: a pediatrician, an ENT doctor, a cardiologist, a pulmonologist, a neurologist.
After a thorough physical examination, collection of complaints and anamnesis, the doctor may suggest additional examinations, namely:
- spirometry to rule out functional pathology of the lungs and airways;
- ECG and ECHO-KG to detect arrhythmias and heart defects;
- EEG to exclude the neurological component of shortness of breath;
- take blood tests to rule out allergies.
You should not be afraid. As a rule, already at the initial appointment, the doctor determines in which direction the diagnosis should be moved!
What parents should watch out for when their child is short of breath:
- When it occurs (during the day or night, after physical exertion, at rest or with strong excitement).
- Where does shortness of breath appear (at home, on the street, in the gym, etc.