Baby sick after feeding but still hungry
Vomiting (0-12 Months)
Is this your child's symptom?
- Vomiting (throwing up) stomach contents
- Other names for vomiting are puking, barfing and heaving
Causes of Vomiting
- Viral Gastritis. Stomach infection from a stomach virus is the most common cause. Also called stomach flu. A common cause is the Rotavirus. The illness starts with vomiting. Watery loose stools may follow within 12-24 hours.
- Food Allergy. Vomiting can be the only symptom of a food reaction. The vomiting comes on quickly after eating the food. Uncommon in infants, but main foods are eggs and peanut butter.
- Coughing. Hard coughing can also cause your child to throw up. This is more common in children with reflux.
- Serious Causes. Vomiting alone should stop within about 24 hours. If it lasts over 24 hours, you must think about more serious causes. An example is a kidney infection.
A serious cause in young babies is pyloric stenosis. See below for more on this.
Pyloric Stenosis (Serious Cause)
- The most common cause of true vomiting in young babies.
- Onset of vomiting is age 2 weeks to 2 months
- Vomiting is forceful. It becomes projectile and shoots out.
- Right after vomiting, the baby is hungry and wants to feed. ("hungry vomiter")
- Cause: The pylorus is the channel between the stomach and the gut. In these babies, it becomes narrow and tight.
- Risk: Weight loss or dehydration
- Treatment: Cured by surgery.
Vomiting Scale
- Mild: 1 - 2 times/day
- Moderate: 3 - 7 times/day
- Severe: Vomits everything, nearly everything or 8 or more times/day
- Severity relates even more to how long the vomiting goes on for. At the start of the illness, it's common for a child to vomit everything.
 This can last for 3 or 4 hours. Children then often become stable and change to mild vomiting.
This can last for 3 or 4 hours. Children then often become stable and change to mild vomiting. - The main risk of vomiting is dehydration. Dehydration means the body has lost too much fluid.
- The younger the child, the greater the risk for dehydration.
Dehydration: How to Tell
- The main risk of vomiting is dehydration. Dehydration means the body has lost too much water.
- Vomiting with watery diarrhea is the most common cause of dehydration.
- Dehydration is a reason to see a doctor right away.
- Your child may have dehydration if not drinking much fluid and:
- The urine is dark yellow and has not passed any in over 8 hours.
- Inside of the mouth and tongue are very dry.
- No tears if your child cries.
- Slow blood refill test: Longer than 2 seconds. First, press on the thumbnail and make it pale. Then let go. Count the seconds it takes for the nail to turn pink again. Ask your doctor to teach you how to do this test.

When to Call for Vomiting (0-12 Months)
Call 911 Now
- Can't wake up
- Not moving
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Dehydration suspected. No urine in over 8 hours, dark urine, very dry mouth and no tears.
- Stomach pain when not vomiting. Exception: stomach pain or crying just before vomiting is quite common.
- Age less than 12 weeks old with vomiting 2 or more times. Exception: normal spitting up.
- Vomited 3 or more times and also has diarrhea
- Severe vomiting (vomits everything) more than 8 hours while getting Pedialyte (or breastmilk)
- Head injury within the last 24 hours
- Weak immune system. Examples are sickle cell disease, HIV, cancer, organ transplant, taking oral steroids.
- Vomiting a prescription medicine
- Fever over 104° F (40° C)
- Fever in baby less than 12 weeks old. Caution: Do NOT give your baby any fever medicine before being seen.

- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Contact Doctor Within 24 Hours
- All other infants (age less than 1 year) with vomiting. See Care Advice while waiting to discuss with doctor.
Seattle Children's Urgent Care Locations
If your child’s illness or injury is life-threatening, call 911.
- Bellevue
- Everett
- Federal Way
- Seattle
Care Advice for Vomiting
- What You Should Know About Vomiting:
- Most vomiting is caused by a viral infection of the stomach.
- Vomiting is the body's way of protecting the lower gut.
- The good news is that stomach illnesses last only a short time.
- The main risk of vomiting is dehydration. Dehydration means the body has lost too much fluid.
- Here is some care advice that should help.
- Most vomiting is caused by a viral infection of the stomach.
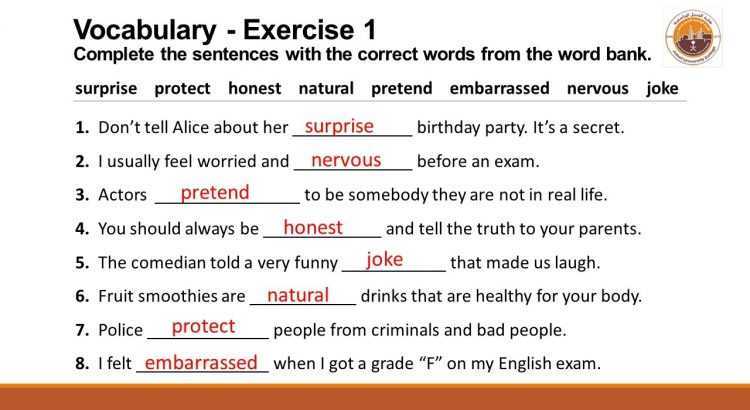
- Formula Fed Babies - May Give Oral Rehydration Solution (ORS) for 8 Hours:
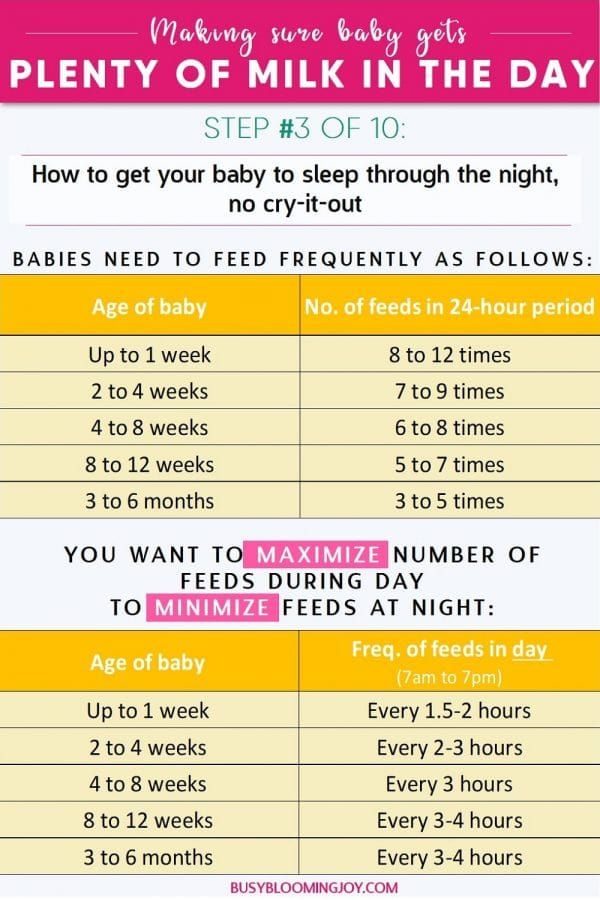
- If vomits once, give half the regular amount of formula every 1 to 2 hours.
- If vomits formula more than once, offer ORS for 8 hours. If you don't have ORS, use formula until you can get some.
- ORS is a special fluid that can help your child stay hydrated. You can use Pedialyte or the store brand of ORS. It can be bought in food stores or drug stores.
- Spoon or syringe feed small amounts. Give 1-2 teaspoons (5-10 mL) every 5 minutes.
- After 4 hours without throwing up, double the amount.
- Return to Formula. After 8 hours without throwing up, go back to regular formula.
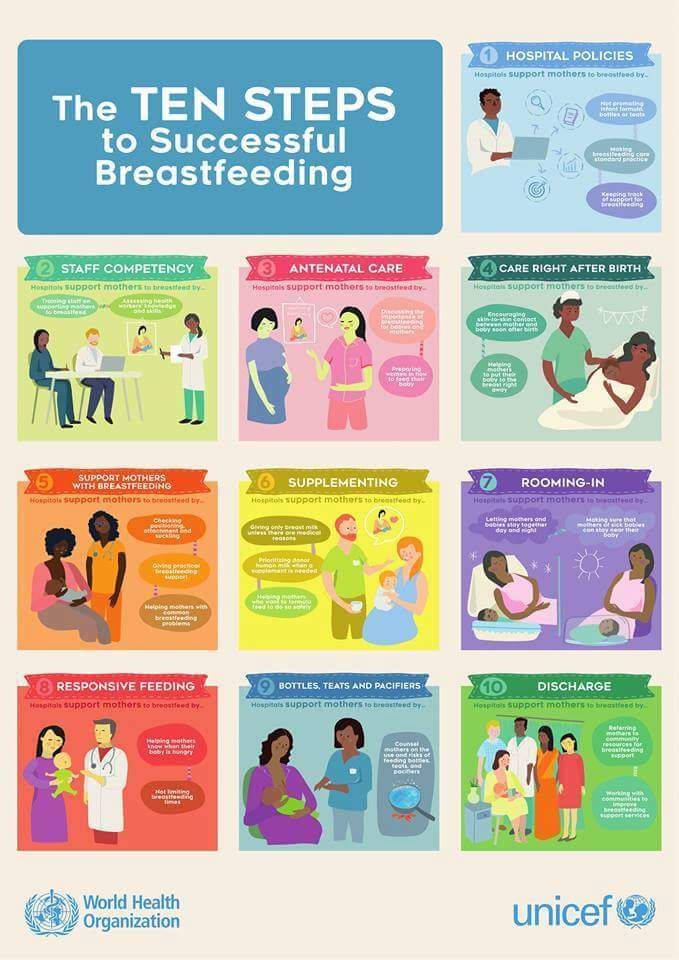
- Breastfed Babies - Reduce the Amount Per Feeding:
- If vomits once, nurse half the regular time every 1 to 2 hours.
- If vomits more than once, nurse for 5 minutes every 30 to 60 minutes. After 4 hours without throwing up, return to regular nursing.
- If continues to vomit, switch to pumped breastmilk. (ORS is rarely needed in breastfed babies. It can be used if vomiting becomes worse).
- Spoon or syringe feed small amounts of pumped milk. Give 1-2 teaspoons (5-10 mL) every 5 minutes.
- After 4 hours without throwing up, return to regular feeding at the breast. Start with small feedings of 5 minutes every 30 minutes. As your baby keeps down the smaller amounts, slowly give more.
- Pumped Breastmilk Bottle-Fed Infants - Reduce the Amount per Feeding:
- If vomits once and bottle-feeding breastmilk, give half the regular amount every 1-2 hours.
- If vomits more than once within last 2 hours, give 1 ounce (30 mL) every 30 to 60 minutes.
- If continues to vomit, give 1-2 teaspoons (5-10 mL) every 5 minutes. Only if not tolerating breastmilk, switch to ORS (e.g., Pedialyte) for every 5 minutes for a few hours.
- After 4 hours without vomiting, return to regular feedings. Start with 1 ounce (30 mL) every 30 minutes and slowly increase as tolerated.
- Stop All Solid Foods:
- Avoid all solid foods and baby foods in kids who are vomiting.
- After 8 hours without throwing up, gradually add them back.
- If on solid foods, start with starchy foods that are easy to digest. Examples are cereals, crackers and bread.
- Do Not Give Medicines:
- Stop using any drug that is over-the-counter for 8 hours. Reason: Some of these can make vomiting worse.
- Fever. Mild fevers don't need to be treated with any drugs. For higher fevers, you can use an acetaminophen suppository (such as FeverAll). This is a form of the drug you put in the rectum (bottom).
 Ask a pharmacist for help finding this product. Do not use ibuprofen. It can upset the stomach.
Ask a pharmacist for help finding this product. Do not use ibuprofen. It can upset the stomach. - Call your doctor if: Your child vomits a drug ordered by your doctor.
- Try to Sleep:
- Help your child go to sleep for a few hours.
- Reason: Sleep often empties the stomach and removes the need to vomit.
- Your child doesn't have to drink anything if his stomach feels upset and he doesn't have any diarrhea.
- Return to Child Care:
- Your child can return to child care after the vomiting and fever are gone.
- What to Expect:
- For the first 3 or 4 hours, your child may vomit everything. Then the stomach settles down.
- Vomiting from a viral illness often stops in 12 to 24 hours.
- Mild vomiting and nausea may last up to 3 days.
- Call Your Doctor If:
- Vomits clear fluids for more than 8 hours
- Vomiting lasts more than 24 hours
- Blood or bile (green color) in the vomit
- Stomach ache present when not vomiting
- Dehydration suspected (no urine in over 8 hours, dark urine, very dry mouth, and no tears)
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.

Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Last Reviewed: 12/04/2022
Last Revised: 09/21/2022
Copyright 2000-2022 Schmitt Pediatric Guidelines LLC.
Spitting Up - Reflux
Is this your child's symptom?
- Spitting up small amounts of breastmilk or formula. Also called reflux.
- Spitting up 1 or 2 mouthfuls of milk at a time
- No effort or crying
- Normal symptom in half of young babies
Symptoms of Normal Spitting Up
- Smaller amounts often occur with burping ("wet burps")
- Larger amounts can occur after overfeeding
- Most often seen during or shortly after feedings
- Occurs mainly in children under 1 year of age
- Begins in the first weeks of life
- Caution: normal reflux does not cause any crying
Complications of Spitting Up (GERD)
- Most infants are "happy spitters.
 " Normal spitting up (normal reflux) occurs in half of babies. It does not cause crying or colic.
" Normal spitting up (normal reflux) occurs in half of babies. It does not cause crying or colic. - Normal crying occurs in all babies. Frequent crying (called colic) occurs in 15% of babies. Crying and colic are not helped by heartburn meds. These meds also have side effects.
- If they develop complications, it's called GERD (gastro-esophageal reflux disease). This occurs in less than 1% of babies.
Symptoms of GERD
GERD problems occur in less than 1% of infants:
- Choking on spit up milk
- Heartburn from acid on lower esophagus. Infants with this problem cry numerous times per day. They also act very unhappy when they are not crying. They are in almost constant discomfort.
- Poor Weight Gain
Cause
- Poor closure of the valve at the upper end of the stomach (weak valve)
- Main trigger: overfeeding of formula or breastmilk
- More than half of all infants have occasional spitting up ("happy spitters")
Reflux Versus Vomiting: How to Tell
- During the first month of life, newborns with true vomiting need to be seen quickly.
 The causes of vomiting in this age group can be serious. Therefore, it's important to tell the difference between reflux and true vomiting.
The causes of vomiting in this age group can be serious. Therefore, it's important to tell the difference between reflux and true vomiting.
Reflux
The following suggests reflux (normal spitting up):
- You've been told by a doctor your baby has reflux
- Onset early in life (85% by 7 days of life)
- Present for several days or weeks
- No pain or crying during reflux
- No effort with spitting up
- No diarrhea
- Your baby acts hungry, looks well and acts happy.
Vomiting
The following suggests vomiting:
- Uncomfortable during vomiting
- New symptom starting today or yesterday
- Forceful vomiting
- Contains bile (green color)
- Diarrhea is also present or
- Your baby looks or acts sick.
Pyloric Stenosis (Serious Cause)
- This is the most common cause of true vomiting in young babies.
- Onset of vomiting age 2 weeks to 2 months
- Vomiting is forceful.
 It shoots out of the baby's mouth. This is called projectile vomiting.
It shoots out of the baby's mouth. This is called projectile vomiting. - Right after vomiting, the baby is hungry and wants to feed. ("hungry vomiter")
- Cause: the pylorus is the channel between the stomach and the gut. In these babies, it becomes narrow and tight.
- Risk: weight loss or dehydration
- Treatment: cured by surgery.
When to Call for Spitting Up - Reflux
Call Doctor or Seek Care Now
- Blood in the spit up
- Choked on milk and turned blue or went limp
- Age less than 12 weeks and spitting up changes to vomiting (forceful or projectile)
- Age less than 1 month old and looks or acts abnormal in any way
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Contact Doctor Within 24 Hours
- You think your child needs to be seen, but the problem is not urgent
Contact Doctor During Office Hours
- Chokes a lot on milk
- Poor weight gain
- Frequent crying
- Spitting up is getting worse
- Age more than 12 months old
- Spitting up does not get better with this advice
- You have other questions or concerns
Self Care at Home
- Normal reflux (spitting up) with no problems
Seattle Children's Urgent Care Locations
If your child’s illness or injury is life-threatening, call 911.
- Bellevue
- Everett
- Federal Way
- Seattle
Care Advice for Spitting Up (Reflux)
- What You Should Know About Spitting Up:
- Spitting up occurs in most infants (50%).
- Almost always doesn't cause any pain or crying.
- Spitting up does not interfere with normal weight gain.
- Infants with normal reflux do not need any tests or medicines.
- Reflux improves with age.
- Here is some care advice that should help.
- Feed Smaller Amounts:
- Skip this advice if age less than 1 month or not gaining weight well.
- Bottlefed Babies. Give smaller amounts per feeding (1 ounce or 30 mL less than you have been). Keep the total feeding time to less than 20 minutes. Reason: Overfeeding or completely filling the stomach always makes spitting up worse.
- Breastfed Babies. If you have a good milk supply, try nursing on 1 side per feeding. Pump the other side. Switch sides you start on at each feeding.
- Longer Time Between Feedings:
- Formula. Wait at least 2½ hours between feedings.
- Breastmilk. Wait at least 2 hours between feedings.
- Reason: It takes that long for the stomach to empty itself. Don't add more milk to a full stomach.
- Loose Diapers:
- Do not put the diaper on too tight. It puts added pressure on the stomach.
- Don't put pressure on the stomach right after meals.
- Also, do not play too hard with your baby during this time.
- Do not put the diaper on too tight. It puts added pressure on the stomach.
- Upright Position:
- After meals, try to hold your baby in the upright (vertical) position.
- Use a front-pack, backpack, or swing for 30 to 60 minutes after feedings.
- Decrease the time in a sitting position (such as infant seats).
- After 6 months of age, a jumpy seat is helpful. The newer ones are stable.
- During breast or bottle feeds, hold your baby at a slant. Try to keep your baby's head higher than the stomach.
- Less Pacifier Time:
- Frequent sucking on a pacifier can pump the stomach up with swallowed air.
- So can sucking on a bottle with too small a nipple hole.
- The formula should drip 1 drop per second when held upside down. If it doesn't, the nipple hole may be clogged. Clean the nipple better. You can also make the nipple hole slightly bigger.

- Burping:
- Burping is less important than giving smaller feedings. You can burp your baby 2 or 3 times during each feeding.
- Do it when he pauses and looks around. Don't interrupt his feeding rhythm in order to burp him.
- Burp each time for less than a minute. Stop even if no burp occurs. Some babies don't need to burp.
- Add Rice Cereal to Formula:
- If your baby still spits up large amounts, try thickening the formula. Mix it with rice cereal.
- Start with 1 level teaspoon of rice cereal to each ounce of formula.
- Acid Blocking Medicines:
- Prescription medicines that block acid production are not helpful for normal reflux.
- These medicines also can have side effects.
- They do not reduce excessive crying from colic.
- They are only useful for symptoms of heartburn.
- What to Expect:
- Reflux gets better with age.
- After learning to sit well, many babies are better by 7 months of age.
- Reflux gets better with age.
- Call Your Doctor If:
- Spitting up changes to vomiting (forceful or projectile)
- Poor weight gain
- Your baby does not get better with this advice
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Last Reviewed: 12/04/2022
Last Revised: 01/13/2022
Copyright 2000-2022. Schmitt Pediatric Guidelines LLC.
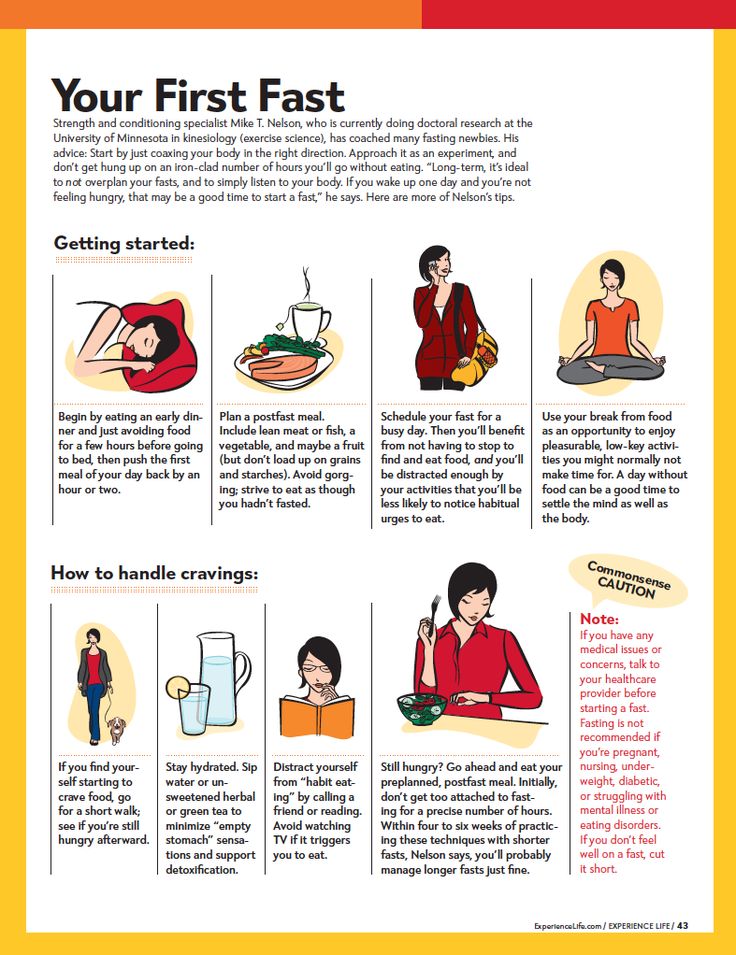
Feeding a sick child
Publication date: 12/15/2016 08:22
April 22nd, 2016 Olga.
While the child grows up, he will be ill with various diseases more than once.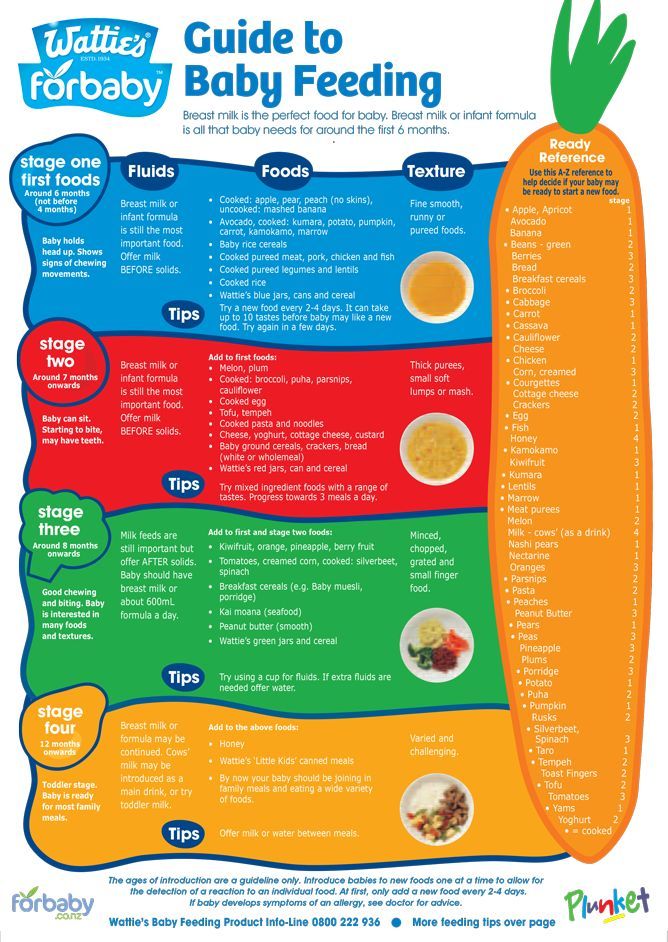 About 80% is accounted for by SARS. Any disease (we are now talking about the flu, SARS) is characterized by poor health of the child - malaise, cough, runny nose, weakness, and maybe intestinal upset. And all this affects the appetite of the child. If a child has caught a cold, mothers always ask themselves the question: how to feed him properly? Proper nutrition of a sick child will help to quickly cope with the disease.
About 80% is accounted for by SARS. Any disease (we are now talking about the flu, SARS) is characterized by poor health of the child - malaise, cough, runny nose, weakness, and maybe intestinal upset. And all this affects the appetite of the child. If a child has caught a cold, mothers always ask themselves the question: how to feed him properly? Proper nutrition of a sick child will help to quickly cope with the disease.
During an illness, the baby always has a poor appetite. There are physiological reasons for this:
- at elevated temperatures, blood circulation in the stomach slows down. because the body sends blood to vital organs: the heart and lungs. The process of digestion and assimilation of food slows down and the child needs less food than usual;
- during an illness, the liver actively fights toxins, the products of the vital activity of viruses and the decay of damaged cells, so a large amount of food carries an additional burden;
- the toxins themselves poison the body and the child, when he feels bad, not at all before eating;
- blocked nose, sore throat, difficult to swallow.
- Nutrition should be appropriate for the child's age;
- during illness, do not introduce new foods into the diet;
- food should be sparing - liquid or semi-liquid;
- make small meals if the baby does not want to eat, and the number of feedings can be increased;
- if the child refuses to eat, let him drink more fluids (water, compote, fruit drink, rosehip broth).
From the diet during illness should be excluded:
- Hard-to-digest foods - fatty meat, whole grain cereals, fresh vegetables and fruits.
- Foods harmful to the liver - fatty dairy products, chocolate, vegetable oil, lard, confectionery.
- Rough, which can damage the mucous membrane - nuts, seeds, crackers, cookies.
Useful menu
During an illness, a child needs food that is well absorbed by a weakened body. Therefore, chicken broth, vegetable soups, stewed and boiled vegetables are perfect for feeding a child during SARS.
To avoid mechanical irritation of the stomach, choose foods that are low in fiber. What foods are low in fiber? These are potatoes, cauliflower, pumpkin, rice and semolina, animal products.
Potatoes are especially delicate in fiber, so include mashed potatoes in your menu more often. You can cook mashed potatoes with sausage, cheese. Beautifully decorate the dish.
Animal protein must be present in the diet of a sick child, since it is a building material for protective antibodies. They are rich in lean meat - veal, beef, lean pork. For soups, use secondary broths from turkey meat, rabbit, chicken breast.
What else can you feed a child during illness? Yogurt helps out well, especially homemade, with the addition of berries.
Cook porridge for the child: semolina, oatmeal, you can also add berries from jam or defrosted.
A sick child needs vitamins. You can make vitamin drinks from rose hips, berries, cook jelly, dried fruit compote, berry juice. . Such drinks will alleviate the condition of the baby if the throat hurts. But with indigestion, milk should not be given at all.
. Such drinks will alleviate the condition of the baby if the throat hurts. But with indigestion, milk should not be given at all.
To increase the appetite of the dish, it is desirable to arrange it beautifully so that the child immediately has a desire to eat it.
Nutrition for a convalescent child
After an acute period of illness, a period of convalescence begins, when the baby is on the mend and nutrition during this period plays an important role. The food of a recovering baby should be rich in energy in order to restore strength, contain minerals and vitamins, the food should be well absorbed.
As soon as the symptoms of the disease subside, do not rush to pounce on a child with enhanced nutrition, it will take a few more days to restore digestion. Continue to follow the diet, adding lean meat and fish, cheese, eggs, boiled vegetables and fruits to it.
Ideal for casseroles, puddings, steamed cutlets, vegetable soups. Introduce fruits and vegetables into the diet and do not forget about sour-milk products that will help restore the disturbed intestinal microflora. Let during this period the food be fractional, the child eat a little. And when the body gets stronger, the child will return to a normal diet.
Let during this period the food be fractional, the child eat a little. And when the body gets stronger, the child will return to a normal diet.
Choosing tactics
When feeding a sick child, parents must remember that it is impossible to force-feed a child!
We provide a diet with easily digestible products. Some parents find it difficult to feed the baby during illness, he categorically refuses to eat. Psychologists advise not to turn feeding into a circus with musical numbers so that the child eats "well, at least one spoonful."
If a child refuses to eat once, it will not bring much harm to health. He will not remain hungry, but will ask for something anyway when his appetite wakes up.
And don't scold the baby if he doesn't want to eat. Appetite will be restored.
Information from the site: deti-i-vnuki.ru/pitanie-bolnogo-rebenka/
Displaced feeding schedule: why does your baby eat all night, and how to change it?
03/12/2017
133144
78
Feeding and sleep
3-6 months --9 months–18 months
Article
Natalya Trofimova
Natalya Trofimova
Senior Consultant, Pediatrician
222 Mom of two daughters
Does your baby eat little or rarely during the day, but hangs on her chest for a long time at night or often asks for a bottle? This is called a "shifted feeding schedule.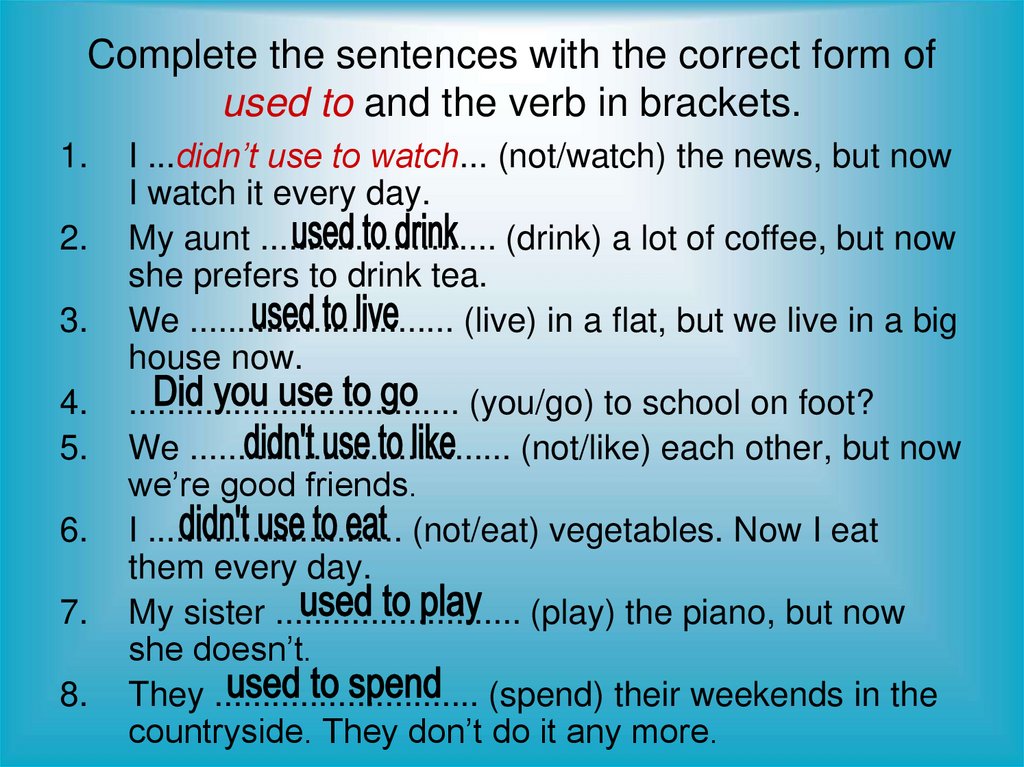 " With this organization of nutrition, the child receives the bulk of the calories at night. During the day, feedings are either short or rare, or the baby refuses the breast or bottle altogether. After six months, there may be difficulties with the introduction of complementary foods, especially with unformed nutritional interest.
" With this organization of nutrition, the child receives the bulk of the calories at night. During the day, feedings are either short or rare, or the baby refuses the breast or bottle altogether. After six months, there may be difficulties with the introduction of complementary foods, especially with unformed nutritional interest.
Child crisis calendar
Why is this happening?
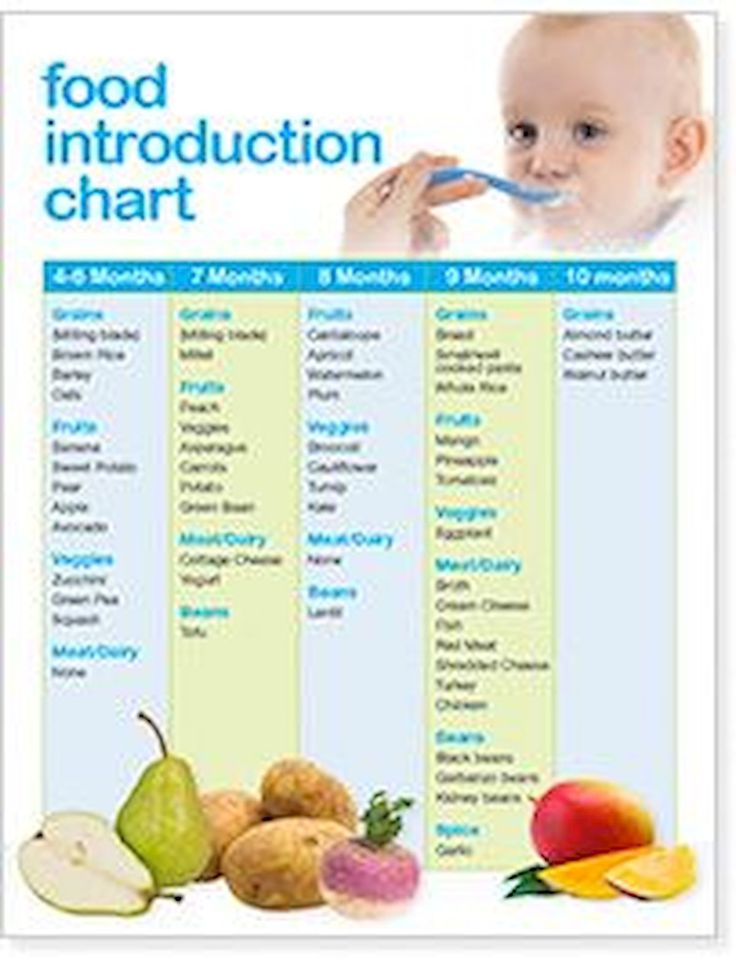
- During periods of crisis in a child's development (a developmental leap, teething, an acute illness, any strong emotional experiences), a temporary and sharp increase in the number of feedings is normal, it just needs to be waited out.
- Babies in their first months of life can “mix day and night” and, accordingly, stay awake and eat mainly at night.
- Older children become interested in everything and are easily distracted during the daytime feedings, butting for a short time, because they have too many important things to do during the day.
- With the introduction of complementary foods, mothers sometimes begin to replace daytime feedings with breast milk or formula with low-calorie fruit and vegetable purees, and the baby has to “get” calories at night.
- Mixed-fed, when breast milk and formula are clearly separated by time of day. When breastfeeding only during the day, the baby may refuse the breast if he prefers a bottle that is given only at night. And vice versa, when feeding during the day with a mixture, and at night with a breast, if the baby prefers the breast.
- Breastfeeding mother works outside the home or is separated most of the day from the baby (even with the possibility of pumping). When sleeping together, the baby is often applied, replenishing contact and helping to stimulate lactation. This option is not bad as a solution, provided that co-sleeping is suitable for the family and everyone gets enough sleep.
Answer a few questions to understand if your feeding schedule is shifted:
- How many times does the child eat during the day and how, how many times does he wake up at night?
- Does he eat for a long time every night when he wakes up, are sips audible, or is it mostly short attachments with superficial sucking for a couple of minutes?
- Are the daily feeds long, does the baby let go of the breast when it is full, or is it often torn off and distracted?
- Can a baby fall asleep without breastfeeding or a bottle (both day and night) or is this the only way to fall asleep?
Frequent nightly “snacking” does not always indicate that the feeding schedule has been shifted. If feeding is a way to relax and fall asleep, then when awakened at night between sleep cycles, the breast or bottle will again be required to fall asleep. This is an association with sleep, the way and habit of falling asleep.
If feeding is a way to relax and fall asleep, then when awakened at night between sleep cycles, the breast or bottle will again be required to fall asleep. This is an association with sleep, the way and habit of falling asleep.
What these feedings usually look like:
- The baby wakes up every 1–1.5 hours at night and asks for food, and during the day he usually eats after 3 hours, which means he is unlikely to experience hunger.
- The child eats very little at night: he kissed his breast for a minute or a bottle, ate 10-20 ml and fell asleep - in this case, he does not have a goal to eat.
- If there is an association for sleep, but the daily appetite does not suffer, mother and baby get enough sleep, there is nothing to worry about. In order for the number of nightly awakenings and feedings to allow sufficient sleep, even if there is an association for sleep, the child must be well suited to sleep and wakefulness.
Is it possible to change the habit of eating at night and when should I wait?
As much as one would like to reduce the number of night feedings, there are situations when they are necessary. For example, a baby in the first months of life does not gain weight well, there are problems with lactation (little milk, false breastfeeding), adaptation to a therapeutic mixture with a specific taste and refusal to wake up, the baby feels unwell (sick, teeth are being cut), a child is experiencing a developmental leap, stress, a long separation from her mother.
For example, a baby in the first months of life does not gain weight well, there are problems with lactation (little milk, false breastfeeding), adaptation to a therapeutic mixture with a specific taste and refusal to wake up, the baby feels unwell (sick, teeth are being cut), a child is experiencing a developmental leap, stress, a long separation from her mother.
The assistance will depend on the age and the reason for the predominance of night eating. In the first months of life, with the "confusion of day and night," it is important to show the baby when it is day and when it is night. For daytime sleep, you do not need to create a strong blackout, and at night you need to ensure maximum darkness in the room. Limit overly long naps. All activities, walks, communication - during the day, no games at night.
If the baby is distracted during feedings and “forgets” to eat, you need to create the most calm atmosphere during feedings: turn off the TV, do not use the phone, retire to a darkened quiet room, turn on white noise. You can put a bright scarf around your neck, slingobuses, any baby rattle on a ribbon. Try a different position with less visibility, such as kneeling facing you or in a sling.
You can put a bright scarf around your neck, slingobuses, any baby rattle on a ribbon. Try a different position with less visibility, such as kneeling facing you or in a sling.
With the introduction of complementary foods, do not rush to replace breastfeeding or mashed formula. The first vegetable or fruit purees are not comparable in calories to breast milk and formula. Occupying volume in the stomach, they reduce milk intake during the day. Complementary foods can fully replace feeding only after 8 months, when it will make up about 20–30% of nutrition and the baby will eat cereals, meat, and vegetables.
On mixed feeding, it is desirable to supplement the baby with the mixture in the required amount after each application to the breast, or feed the mixture by the hour (at regular intervals), and breastfeed on demand.
A working mother who is breastfeeding and co-sleeping has the hardest time reducing nighttime feedings. To do this, you need to feed the baby often enough during the day, a maximum of 3–3.