Baby squirming during bottle feeding
Why Baby Squirms And Cries While Bottle Feeding?
As a parent, there is nothing more crucial than ensuring your child is secure, content, and a healthy baby. When you’re attempting to satisfy one of your baby’s fundamental needs, it might be upsetting to watch them in tears.
You might be perplexed as to why your baby is sobbing while being bottle-fed. If your baby is formula-fed, they may be crying while you are bottle-feeding them. Your baby may not constantly cry due to allergies, though.
A growth spurt, a lack of hunger, a loss of milk, or the need to be burped may also occur. It’s crucial to take into account all the potential explanations. Let’s look at some of the most typical causes of squirming and crying while bottle feeding in babies.
Common signs of bottle feeding problemsDo your babies display any trouble behaviors when they’re bottle-fed, such as…
- Refuses a bottle
- Turning away from the drink.
- Not closing her lips around the nipple.
- Not holding the nipple in the mouth but letting it hang out.
- Refusing to take any more than a small amount at first.
- Crying when placed into a nursing position or at the sound of the bottle.
- A milk bottle coming out of a child’s mouth.
- Too fast eating.
- Eating too slowly.
- Falling asleep during the feed.
- When coughing and spluttering, stop feeding for a few minutes
- Not drinking enough milk.
- Wanting more milk than expected.
- Throwing up large quantities of milk.
If you’re having trouble breastfeeding, then there may be things you can do to help calm your baby down and encourage him/her to accept a bottle.
Common Reasons that make a baby squirms and cries while bottle feedingFollowing are the behavioral reasons why your baby squirms or excessive crying when being fed by bottle.
DistractionsBabies begin moving or squirming while being fed by a bottle as soon as they can see and recognise their surroundings.![]() It might occur in as little as three to four months. While being fed from a bottle, babies will squirm as they start to explore the light, sounds, and things in their environment.
It might occur in as little as three to four months. While being fed from a bottle, babies will squirm as they start to explore the light, sounds, and things in their environment.
For instance, if they are being bottle-fed and notice their siblings playing in the background, they will stop and react to the sound or noise they are creating. Additionally, as your baby gets a little older and gains a bit more mobility, they will wriggle even more when being fed by bottle.
SolutionYou might wish to feed your baby alone if they are squirming or moving about a much when being fed from a bottle. Bring them into a calm space, turn down the light, give them their favourite toy, and bottle-feed them.
Silent RefluxSilent reflux may also be the cause of the baby’s squirming when being fed by bottle. When stomach contents return up into the oesophagus, reflux develops. Normal reflux causes a baby to vomit up the formula, whereas silent reflux causes the content to linger in the oesophagus.
As a result of their inability to spit up silently, babies frequently arch their backs, which can make them appear to be squirming while being fed a bottle or refusing to eat. Since there is no excessive spitting, silent reflux can be difficult to identify, and symptoms of reflux are frequently mistaken for infantile colic symptoms.
SolutionConsult your pediatrician if you think your child may be experiencing silent reflux. They will then direct you. Silent reflux can be controlled with modest adjustments such as:
- Lessen the pressure on the stomach by feeding more frequently and in smaller portions.
- Bottle nipple with a slow flow helps bottle-fed babies consume less air or air bubbles while drinking from the bottle.
- When feeding a baby by the bottle, keep them upright position both during and after the feeding. These feeding positions will assist to lessen reflux symptoms.
- infant frequently burps while being fed by bottle
Your first assumption might be that your baby has an allergy if they cry during a bottle feeding. Many parents genuinely worry about this. However, you can also notice additional symptoms such as vomiting, diarrhoea, rash, and blood or mucus in your baby’s stool if they do have an allergy to cow’s milk or another ingredient in their baby formula.
Many parents genuinely worry about this. However, you can also notice additional symptoms such as vomiting, diarrhoea, rash, and blood or mucus in your baby’s stool if they do have an allergy to cow’s milk or another ingredient in their baby formula.
Before changing your baby’s formula or feeding schedule, it is best to consult your paediatrician if you do detect any of those symptoms. Lactose intolerance in babies is extremely uncommon, and you shouldn’t change your baby’s feeding habits and not adopt poor feeding habits before consulting a health professional, according to the University of Michigan School of Medicine.
SolutionThankfully, there are now many formulas on the market designed specifically for babies who have a lactose sensitivity or allergy. You can choose from them according to your needs.
Tummy acheWhile you are bottle-feeding your baby, if they begin to kick or squirm, it can indicate a stomach ailment. If your baby has a tummy ache, it’s probable that they need to be burped.
If your baby has a tummy ache, it’s probable that they need to be burped.
Additionally, you might want to consider how you are feeding your baby. When bottle-feeding, the bottle must be held at an angle. This will guarantee that the bottle is empty of air.
SolutionAfter each feeding, touch your baby to help ease any discomfort. After feeding, you might also try a soft tummy massage on your baby’s stomach.
Age-Appropriate Nipple sizeYour baby’s bottle nipple may need to be double-checked to make sure it is the right or age-appropriate nipple size. You might discover that your baby isn’t getting enough milk or that the bottle isn’t working properly for them.
SolutionAccording to Verywellfamily.com, when the bottle is turned over, the milk or formula should be flowing at a rate of one drop per second. If it comes out more quickly or more slowly than this, you might want to replace the bottle feeding nipple.
In some circumstances, you might need to adjust the bottle’s feeding nipple size. For babies, a slow flow nipple is ideal. Over time, it will gradually transform.
Feeding patternsSome babies grow into grazing or crunchy snacks, who will only consume little amounts of formula at a time and then become a hungry baby to demand frequent feedings, maybe every hour or two. Although babies won’t experience any issues with this as long as they consume enough formula in a 24-hour period, it can be exceedingly exhausting for parents to keep up with their constant cries for feeding.
Solution- Encourage your infant to consume as much milk as they can in the next 45 minutes. But if she chooses not to feed, don’t force her. If she decides not to go on, stop sooner.
- Make sure the baby receives enough deep sleep because infant sleep is important so your baby doesn’t become a colicky baby or fussy baby.

- Don’t let the baby nod off while being fed.
- By providing som gripe water, a pacifier, a proper nap times, playing with her, or taking her for a stroll, you can encourage your baby to go longer between feedings. In order to avoid upsetting her, try to persuade her to wait at least three hours after you started her previous meal.
- The Period between feeds can be gradually increased if necessary. Your baby will gradually take larger amounts at each feeding as she becomes accustomed to going longer intervals without feedings.
Does warm formula help with gas?
The more mixing and shaking involved, the more air gets mixed into the mixture, which can then be inhaled by your baby and cause them to experience some sort of discomfort. Warm water or little hot water is better than cold or room-temperature water when making smoothies for babies.
What sleeping position is best for gassy baby?On the belly is also the best sleeping posture for a gassy baby (and the best sleep position for babies until they’re one year old). On the stomach. Stomach massages have lots of benefits, including helping to ease digestive issues.
On the stomach. Stomach massages have lots of benefits, including helping to ease digestive issues.
Some babies may not wake up when their stomachs gurgle, burp, or pass wind, but they might wake up if they feel pain from these events. If the baby feels pain during these events, he or she should be able to fall back asleep once the event has passed.
Do pacifiers cause gas?While pacifiers aren’t the main cause of producing flatulence, they’re one of the smaller ones. When babies suck on their pacifiers, they may inadvertently ingest some air into their stomachs. And when babies cry, they often produce burps.
When does colic begin to improve?Babies with colicky crying spells may not eat enough, or get enough rest. They may also be constipated. In most babies, these symptoms disappear within a month or two. However, if your baby continues to cry after three weeks, consult your doctor.![]()
Mixing up different types of formulas for babies isn’t a big deal, even though some parents worry that switching from one brand to another might cause fussier behavior or change in stools. In fact, you’re free to switch between different brands of the same kind of infant milk if you think your child would respond better to one than another.
Final thoughtsYou should always check to see if your baby is gaining weight properly or not having poor weight gain and shows no signs of illness whenever they are having feeding issues. A paediatric gastroenterologist can assist with bottle and formula feeding issues in addition to your child’s paediatrician. In the event that your child vomits blood, green, or yellow liquid, seek immediate medical treatment.
0 shares
Bottle Feeding Problems - Why Your Baby Squirms, Appears Uncomfortable – Baby Care Advice
When your baby squirms, appears uncomfortable during a feed, fusses, cries or refuses a bottle, seemingly fights the bottle despite being hungry, it can be challenge to figure out the cause. The timing and type of behavior she exhibits provides vital clues.
The timing and type of behavior she exhibits provides vital clues.
Does your baby display troubled behavior in relation to bottle-feeding, such as….
- Refuses a bottle
- Turning away from the bottle.
- Refusing to close her mouth around the nipple.
- Holding nipple in the mouth but not sucking.
- Taking only a small amount and then refusing more.
- Screaming when placed into a feeding position or at the sight of the bottle.
- Milk pouring out of baby's mouth.
- Feeding too quickly.
- Feeding too slowly.
- Falling asleep before the feed is completed.
- Coughing and spluttering when feeding.
- Not consuming as much milk as expected.
- Wanting more milk than expected.
- Throwing up large amounts of milk.
Then there may be steps you can take to remedy the situation and get your baby to calmly and happily take a bottle.
‘Behavioral’ means baby’s behavior is in response to the circumstances rather than a physical cause. Behavioral reasons are the most common of all reasons for infant feeding problems. There are numerous behavioral reasons for a baby to experience feeding problems and/or display problematic feeding behavior. Common reasons include:
1. Misinterpreting baby's cues as signs of hunger Does baby at times refuse feeds?Does she take only a little and not want more?
Babies are in an oral stage of develop. Sucking is the primary way babies soothe. They also learn by sucking and mouthing objects. Many babies have a strong desire to suck for reasons that extend beyond hunger, such as tiredness, boredom, discomfort and soothing. There may be times when you mistake your baby’s desire to suck for these reasons as hunger.
Newborn babies have an active sucking reflex. This means a newborn baby may accept a feed even when she’s not hungry, and she might guzzle down the bottle because she cannot choose to not suck when her sucking reflex is triggered. Once her sucking reflex has disappeared (usually by 3 months of age) she will willingly take only the amount she wants to take.
This means a newborn baby may accept a feed even when she’s not hungry, and she might guzzle down the bottle because she cannot choose to not suck when her sucking reflex is triggered. Once her sucking reflex has disappeared (usually by 3 months of age) she will willingly take only the amount she wants to take.
If you have mistakenly interpret her fussing or desire to such as hunger and offer her a feed, she might take a little and refuse the rest, or she refuse from the start. If you try to make her drink more than she wants, she will understandably get upset and fuss, cry and pull back from the bottle.
WHAT TO DO- See Hungry baby for more reasons why babies often appear
- See Infant reflexes
In around one third of consultations I have had with parents regarding an infant feeding problem, I found that parents were trying to make their baby drink more than he or she needed.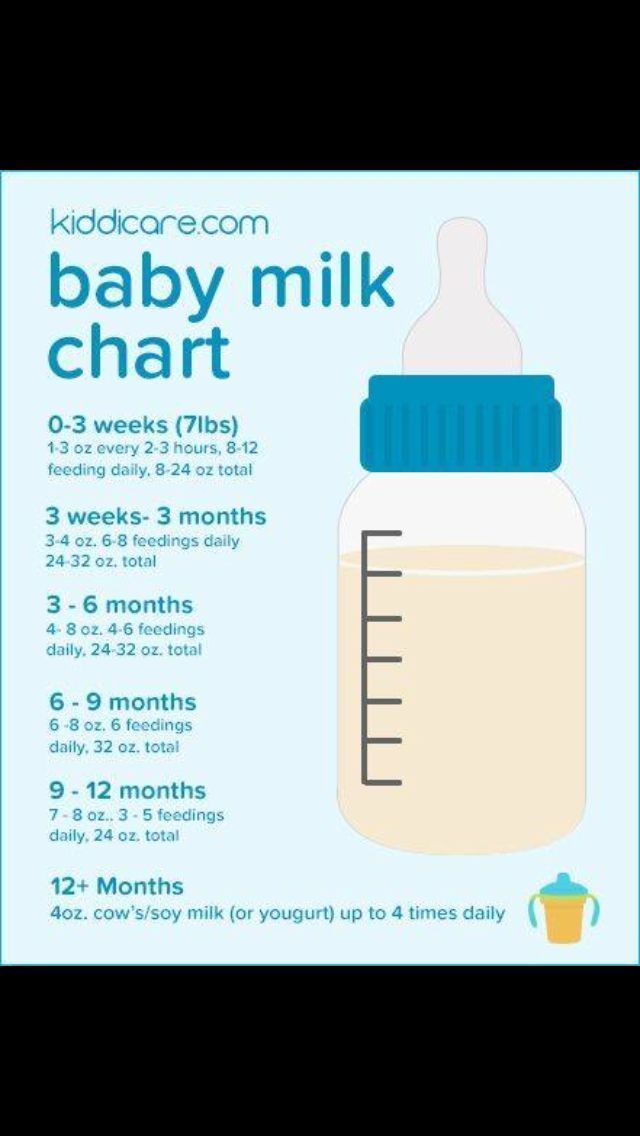 In some cases, this was because of errors made their health professionals. They either failed to adjust calculations as baby matured or failed to consider baby as an individual. As a result, overestimated baby’s milk requirements.
In some cases, this was because of errors made their health professionals. They either failed to adjust calculations as baby matured or failed to consider baby as an individual. As a result, overestimated baby’s milk requirements.
If you think your baby is not drinking enough milk (breast milk or infant formula) you’re naturally going to feel concerned. If your concern translates into trying to pressure her to drink more than she wants or needs (gently or otherwise), you’re going to upset her. So it is very important for your peace of mind and your baby’s enjoyment at feeding times that you have realistic expectations about how much she needs.
WHAT TO DO- See How much milk does baby need for standard estimations for age and weight, and reason why a baby might take more or less than recommended.
- Follow your baby's feeding cues. Don't try to make her take more when she indicates she has had enough.
Sleeping and feeding are closely related when it comes to the needs of babies. Both are equally important to a baby's health, growth and development and feelings of wellbeing. You are no doubt aware that if your baby does not feed well she might not sleep well. But are you aware that the opposite is equally true. If she’s not getting enough sleep this has the potential to negatively impact on her feeding.
Both are equally important to a baby's health, growth and development and feelings of wellbeing. You are no doubt aware that if your baby does not feed well she might not sleep well. But are you aware that the opposite is equally true. If she’s not getting enough sleep this has the potential to negatively impact on her feeding.
Physical fatigue can cause baby to fuss during feeds or falling asleep before the feed is completed. If you have a hungry/tired baby on your hands, tiredness will usually win out.
WHAT TO DO- Ensure baby gets enough sleep.
- Feed her before she becomes too tired.
- Aim to establish a flexible feeding and sleep routine to minimize the risk of feeding and sleep times clashing.
If your baby is often irritable and not sleeping enough, (see Overtired baby for signs and symptoms) you might find that resolving any underlying sleeping problem will cause feeding difficulties to spontaneously resolve once she receives adequate sleep.
- See our sleep section.
- Download or order a paperback copy of my infant sleep book Your Sleepless Baby: The Rescue Guide. There you will find comprehensive information on the reasons and solutions to various infant sleeping problems.
Babies over the age of 4 months can easily become distracted while feeding. They are often much more interested in the activities going on around them than they are in feeding.
WHAT TO DOFeed your baby in a quiet environment away from noise and distractions of other children.
5. Feeding managementSome feeding problems can be related to what may appear like insignificant details but which can make feeding difficult or uncomfortable for a baby. For example, how you hold your baby will affect her ability to feed from a bottle. If her head is too far forward or too far back or her neck is twisted this can make it difficult for her to suck or swallow.
For example, how you hold your baby will affect her ability to feed from a bottle. If her head is too far forward or too far back or her neck is twisted this can make it difficult for her to suck or swallow.
See How to bottle-fed a baby
6. Feeding aversionDoes your baby refuse to feed even when hungry?Does she scream at the sight of a bottle or when placed into a feeding position?Have you resorted to trying to feed her while asleep?A baby can develop an aversion to feeding when past feeding experiences have taught her that feeding is unpleasant, stressful or painful. Typically, baby is diagnosed with reflux and/or milk protein allergy or intolerance to explain her aversive feeding behavior. However, a behavioral feeding aversion (related to feeding management rather than a physical cause) is a far more common cause of infant feeding aversion.
A feeding aversion is the most complex of all infant feeding problems. An effective solution relies heavily on accurate identification of the cause.
WHAT TO DOSee Feeding aversion for more information. Or purchase or download a copy of 'Your Baby's Bottle-Feeding Aversion: Reasons and Solutions'.
7. Feeding equipmentDoes your baby gag, cough or splutter during feed?Does baby make clicking sounds while feeding?It could be the nipple is too long, too short, too fast or too slow.
The most important piece of feeding equipment is the nipple. The nipple needs to be the right size and speed for your baby's size, age and sucking ability. If the nipple is too long, too short, too fast or too slow for your baby, she may experience feeding difficulties and express her frustration by fuss or crying.
WHAT TO DO- See Feeding equipment for more information on choosing a feeding nipple.

- Experiment with nipples of different lengths, shapes and speed.
It's possible her feeding difficulties could be due to the nipple ring being screwed on too tight.
In order to maintain a neutral balance in air pressure within the bottle air needs to be able to enter the bottle to replace the void left by the milk the baby is removing. If the bottle is vented, this is achieved via the venting system. However, in the case of a non-vented bottle, the only ways air can enter the bottle are between the nipple ring and the rim of the bottle and through the holes at the end of the nipple. While sucking, a baby will maintain a seal over the holes at the end of the nipple with her tongue and prevent air entry in this way. If the nipple ring is screwed down tightly this also prevents air entry.
If the nipple ring is screwed down tightly this also prevents air entry.
If air is prevented from entering the bottle, this causes a negative pressure to build in the bottle. As the pressure builds, baby need to work harder and harder to extract further milk, until such time and the air pressure is returned to normal. The effort required to suck against the negative pressure can cause a newborn baby to tire and fall asleep before completing the feed. An older baby may simply give up or express her frustration.
WHAT TO DOThe nipple collapsing (not all will) or stopping to burp baby allows air to enter through the holes and neutralize the pressure. But you don’t want to wait for this to resolve the problem. By then baby is already tiring or getting frustrated. See ‘Collapsing nipple’ for ways to manage this problem.
9. Feeding patternsIs your baby often take only small amounts, refuse more, but then wants to feed again an hour or two later?Some babies develop a grazing or snacking feeding pattern where they will only drink small amounts of formula at a time and then want to be feed frequently, possibly every hour or two. Although this will not cause any problems for a baby, provided she drinks enough formula in total over a 24 hour period, it can become very tiring for parents to keep up with her constant demands for feeding.
Although this will not cause any problems for a baby, provided she drinks enough formula in total over a 24 hour period, it can become very tiring for parents to keep up with her constant demands for feeding.
- Try to encourage your baby to take as much milk as possible within 45 minutes. But don't try to make her feed if she doesn't want to. Stop sooner if she does not want to continue.
- Ensure baby gets plenty of sleep.
- Avoid allowing baby to fall asleep while feeding.
- Support your baby to extend the time between feeds, by offering a little water, a pacifier, a nap, playing with her, or taking her for a walk. Aim to encourage her to wait at least 3 hours from time you started her previous feed, but only if it's reasonable to do so without distressing her. If necessary extend the time between feeds gradually. As your baby gets used to going longer periods between feeds she will gradually take larger amounts at each feed.

Unless your baby was born prematurely or is very small for her age, developmentally she no longer requires feeding during the night beyond the age 6 months. If nighttime feeding continues past this age its not going to harm her but it could have a negative effect on her appetite and feeding patterns during the day.
Your baby only needs a certain number of calories in her day (24 hours) to provide for her growth and energy needs. If after the age of 6 months she continues to receive calories from nighttime feeds this will dampen her appetite during the day and she will not need to drink as much formula during daytime feeds. You might find she is content to go for long periods of time between feeds (which is usually what would happen at night). She might fuss or refuse some of her daytime bottles when they are offered simply because she's not hungry at the time. Or she might graze during the day.
Or she might graze during the day.
Nighttime feeding will cause your baby no harm, so if you're happy to continue feeding her during the night there's no reason to change a thing. However, it is important that you don't expect her to consume as much milk during the day as she may have otherwise taken if she did not feed at night.
Many babies will give up night time feedings on their own accord, but others will continue to wake and demand feeds overnight for months and possibly years while parents continue to provide feeds at night. Usually the reason babies continues to demand night feeds beyond the age of 6 months is because they have learned to rely on feeding as a way to fall asleep, or because their internal body clock gets turned around - where the baby has decreased appetite during the day because of the continued night feeds and as a consequence of small feeds during the day the baby wakes hungry during the night. Body clock problems can easily become a cyclical pattern that will continue over the long term unless parents take steps to change the situation. Healthy, thriving babies who continue to demand feedings at night beyond the age of 6 months often require guidance and support from parents to cease feeding at night and turn their body clock around to a normal day-night feeding pattern.
Healthy, thriving babies who continue to demand feedings at night beyond the age of 6 months often require guidance and support from parents to cease feeding at night and turn their body clock around to a normal day-night feeding pattern.
Aim to cease overnight feeds after 6 months of age. However, before attempting to do this it's important to address any feeding to sleep issues your baby might have. She would need to learn to fall asleep in a different way before you will be able to successfully encourage her to cease night feeds.
11. Starting solids earlyHave you started giving your baby solids before the age of 4 months?Have you been advised to start solids early?6 months is the recommended age for starting solid foods. Although a small number of babies may benefit from solids prior to this age, it's generally not recommended to start a baby on solid foods before the age of 4 months. An early start on solids has the potential to cause bottle feeding problems because solid foods may decrease the baby's appetite for milk (breast milk or formula).
An early start on solids has the potential to cause bottle feeding problems because solid foods may decrease the baby's appetite for milk (breast milk or formula).
- If your baby is less than 6 months old, either cease or reduce the amount of solids you offer to see if this helps to improve the situation.
- See our article on starting solids.
If solids are offered prior to bottle feeds, either directly before or mid way between feeds, when it's time for your baby's bottle feed she might be feeling full from the solids, in which case she's probably not going to take much milk from her bottle.
WHAT TO DO- For babies 4 - 9 months (when milk is still the most important food) offer solids 15 - 20 minutes after bottle feeds.
- For babies 9 - 12 months (when solids are becoming increasingly more important to a baby's diet) offer solids shortly before or shortly after her bottle, whichever you find works best.
 Babies at this age are often down to 3 bottles per day plus 3 main meals and 1 or 2 snacks.
Babies at this age are often down to 3 bottles per day plus 3 main meals and 1 or 2 snacks.
In these early stages of learning to eat solids (4 - 7 months) solids are not needed to add value to a baby's nutritional intake, rather they are offered primarily to provide learning experiences. The baby is exposed to new food proteins that help prime her immune system. She gets to discover new tastes and textures and become accustomed to eating from a spoon. It is at this age that babies are most willing to accept new tastes. So variety rather than quantity is what solids are about.
Many babies, particularly very young babies, experience difficulty self-regulating their dietary intake. Some babies will continue to eat solid foods for as long their parents keep offering. Some babies will prefer eating solids compared to drinking formula. However, too much solids and not enough milk is not a balance diet for a baby. It may be necessary for parents to limit the amount of solids they offer in order to encourage their baby to have a greater appetite for milk feeds.
However, too much solids and not enough milk is not a balance diet for a baby. It may be necessary for parents to limit the amount of solids they offer in order to encourage their baby to have a greater appetite for milk feeds.
See our article on estimating how much milk your baby needs to make sure she's getting enough.
14. Weaning difficultiesDoes your breastfed baby refuse bottle-feeds?Does your baby have a breast preference?While some breastfed babies willing accept milk from a bottle many will not, at least not straight away.
Difficulty weaning from breast to bottle is rarely resolved by finding the 'right' feeding nipple. (All feeding nipples will feel equally foreign to a breastfed baby.) Nor does a solution lie in finding a formula with the 'right' taste. All formula will taste strange to a breastfed baby). The difficulty associated with weaning to a bottle most often lies in the fact that bottle-feeding requires a very different sucking action to breastfeeding. While breastfeeding the movement of your baby's tongue milks the breast, where as bottle-feeding requires a sucking action. A baby who has been exclusively breastfed beyond the age of 3 months will often refuse milk from a bottle because it "doesn't feel right" and she doesn't know how to suck from a bottle.
While breastfeeding the movement of your baby's tongue milks the breast, where as bottle-feeding requires a sucking action. A baby who has been exclusively breastfed beyond the age of 3 months will often refuse milk from a bottle because it "doesn't feel right" and she doesn't know how to suck from a bottle.
It takes time and practice before a breastfed baby learns how to suck on a bottle.
WHAT TO DO- Try offering expressed breast milk in a bottle initially. (Don't be too optimistic and put too much in to start with. It would be a shame to waste it).
- A soft flexible nipple often works better.
NOTE: Many breast fed babies will refuse to accept a bottle while they are still being breastfed at times. They will simply wait until a breastfeed is offered. For these babies it will be the case of breastfeeding or bottle-feeding, but not both.
How we can help your baby take a bottle- Your Baby's Bottle-feeding Aversion book
- Baby Care Advice consultation
- Rowena Bennett's Online Bottle-Feeding Aversion Program
In my book, ‘Your baby’s Bottle-feeding Aversion’, I have described physical and behavioral reasons for babies to develop an aversion to bottle-feeding. How to identify the cause and the solutions to match. Included are step-by-step instructions on how to regain your baby’s trust and resolve a feeding aversion caused or reinforced by repeated pressure to feed.
How to identify the cause and the solutions to match. Included are step-by-step instructions on how to regain your baby’s trust and resolve a feeding aversion caused or reinforced by repeated pressure to feed.
While the book was written for bottle-fed babies, many nursing mothers have found that applying the same strategies has also helped them to successfully resolve a breastfeeding aversion.
You might find that reading this book is all you need to do to understand the steps you need to take to resolve your baby’s feeding aversion and get him back to the point of enjoying eating until satisfied.
Baby Care Advice ConsultationsIf you would like an individualized assessment of all reasons for infant feeding problems, not just feeding aversion, we also provide a consultation service. Baby Care Advice consultants have extensive experience in pinpointing the cause of feeding aversion and other behavioral feeding problems such as those related to equipment and the parent’s feeding practices. (For more on what’s included in a consultation).
(For more on what’s included in a consultation).
By Rowena Bennett, RN, RM, CHN, MHN, IBCLC.
Copyright www.babycareadvice.com 2021. All rights reserved. Permission from the author must be obtained to reproduce all or any part of this article.
Rowena's Online Bottle-Feeding Aversion ProgramSix time-saving modules to help your family enjoy feeding again with Rowena's step-by-step plan. Enjoy additional tools to manage anxiety, troubleshoot any issues, introduce new carers, how to manage illness/teething and much more.
- Module 1: Understanding feeding aversions
- Module 2: Identify the cause
- Module 3: Prepare for success
- Module 4: How to resolve your baby's bottle-feeding aversion
- Module 5: What to expect
- Module 6: Troubleshooting
- BONUS: Guided meditations
Breastfeeding / Breastfeeding / Useful information / Children's polyclinic / Departments of the KDMC sometimes light as dew, sometimes enveloping like white clouds. How many times it healed me and I became strong again, or wrapped me in a sweet slumber when I was very tired. At your chest, I heard the singing of a lark high in the sky, and the whisper of leaves in a birch grove, and autumn rain outside the window, and the chime of waxwings on a winter day.
Even after many years I will remember it, we will remember it...
E. Ibragimova
Published in the special issue of the magazine "Liza. My child" special issue 01/2016
Many mothers, expecting their first baby, seriously think about how childbirth will take place, and less often they think about how they will feed the baby. Meanwhile, childbirth is a very short period of time, and the rest of the time of life with the baby will be devoted to building relationships with him through breastfeeding.
Some mothers-to-be are hesitant to breastfeed at all.
Let's look at their assumptions first:
- Does breastfeeding ruin breast shape?
Breast shape changes during pregnancy. On the contrary, when feeding for more than a year and smooth weaning, the breast acquires an almost “pre-pregnant” shape. According to studies, smoking has a stronger effect on the shape of the breast than feeding.
- Will it be impossible to leave the child?
The first 3 months are possible short (1-1.5 hours) separation from the child, from 3 months absence can be longer, after 9months, the mother can go to work full-time, leaving the baby with expressed milk.
- If the mother is nervous or very tired, does the milk “burn out” or become bad for the baby?
There are no conditions in the mammary gland for "burning out" of milk. When breastfeeding, endorphins are released into the blood of a woman, and HB helps her to endure stress more easily and is the best prevention of depression. Yes, and the child himself calms down at the breast, even if before that he sees the unusual behavior of his mother.
When breastfeeding, endorphins are released into the blood of a woman, and HB helps her to endure stress more easily and is the best prevention of depression. Yes, and the child himself calms down at the breast, even if before that he sees the unusual behavior of his mother.
- Is formula practically the same as breast milk?
The manufacturers of infant formulas, who invest millions of dollars in advertising and bribes, have tried hard to make women have such doubts.
Let's look at a few differences between breastfeeding and formula feeding:
|
| GW | Blend |
| Economy | free | about 100 tr. in the first year of a child's life. If hypoallergenic mixtures are required, then about 240 tr. |
| Number of substances | over 700! | 30- 50 |
| Stem cells | yes | no |
| Antibodies against diseases | yes | no |
| Growth factors for maturation of the intestines | enough | little |
| Effect of | normal maturation of the gastrointestinal tract, normal development of the immune system | constipation, diarrhea, increased risk of many diseases: allergies, gastrointestinal problems, various infections, diabetes, etc. |
| Proteins | easily absorbed whey
| hard to digest casein clots
|
| Change in composition | adapts to the needs of the baby (varies depending on the season, time of day, age of the baby, etc.) | the composition is the same for all children |
| Vitamins and minerals | easily digestible | low absorption |
| Availability | no need to cook | it is necessary to go to shops, sterilize the bottle, dilute the mixture with water, etc. |
| Excess substances | no | cases of salmonella infection, radioactive particles, etc. |
| Emotional connection between mother and child | strong | weak |
And the list of differences goes on.
Can you imagine how a bottle of formula can replace the happy moments at the mother's breast?
With the right information and help, almost every woman can successfully and sustainably breastfeed. And you can!
What information can help you?
Firstly immediately after delivery (before measurements) skin-to-skin contact between the newborn and the dried, covered with a dry diaper, contact duration - at least 40 minutes, optimally 2 hours or more. (This right of mother and child is also enshrined in the Methodological Letter of the Ministry of Health and Social Development of the Russian Federation dated July 13, 2011 N 15-4 / 10 / 2-6796 "On the organization of the work of the obstetric service in the context of the introduction of modern perinatal technologies").
Why is this important:
a) At the same time, the baby's body is colonized by the same bacteria that live on the body of his mother. This, in combination with HB, is considered an important prevention of allergic diseases.
This, in combination with HB, is considered an important prevention of allergic diseases.
b) If a newborn is separated from his mother immediately after birth, he becomes vulnerable to aggressive hospital flora, the risk of nosocomial infections increases dramatically.
c) This calms the baby and mother, because they both experience severe stress in childbirth.
d) The baby is more likely to be able to latch on correctly (especially if the birth was completed without medication).
Second , breastfeed within the first hour after birth. Don't panic if the baby doesn't take the breast right away. Children should eat when they show they are ready, and if the child is in close contact with the mother, she will notice this readiness. The recommended duration of application is at least 20 minutes from each breast.
The baby's first food should be colostrum. Colostrum is the secret of the mammary glands, which is produced during pregnancy and the first 3-5 days after childbirth (before milk arrives). It is a saturated thick liquid from light yellow to orange color. Do not be afraid that there is not enough colostrum. Colostrum is very concentrated, so the baby needs just drops.
It is a saturated thick liquid from light yellow to orange color. Do not be afraid that there is not enough colostrum. Colostrum is very concentrated, so the baby needs just drops.
Why is it important:
A) Colostrum contains several times more protein than mature milk, especially immunoglobulin A. Immunoglobulins are responsible for protecting the baby from infections and allergens, thanks to special mechanisms they are quickly absorbed in the baby's stomach and intestines.
B) Has laxative properties to help the baby quickly get rid of the original stool - meconium, and also reduces the risk of physiological jaundice in the baby.
C) The mother triggers the oxytocin reflex, which contributes to uterine contraction and faster recovery after childbirth.
Thirdly, the correct position of the baby at the breast and the correct attachment of to the breast. Let's dwell on the key points.
For example, you feed while seated. How to hold a baby:
How to hold a baby:
a) The child's body and head are on the same line.
b) The baby's belly should be turned towards the mother's belly and touch it.
c) The WHOLE body of the child must be supported.
The baby is brought to the breast with the NOSE to the nipple so that it is necessary to reach for the breast. When he opens his mouth wide, we press the baby to ourselves.
If it is not possible to attach the baby well, gently insert the little finger into the corner of the mouth and open the gums, remove the breast.
What does proper attachment look like? The baby's mouth is open wide; lips turned out; his chin touches his mother's breasts; areola capture radius is 2-3 cm from the base of the nipple; except for swallowing, sniffing and even breathing, no other sounds are heard (smacking, etc.); mom is not in pain.
There are many positions for feeding - sitting, lying down, close at hand, relaxed feeding, etc.
Nuance: good breast sucking is affected by the frenulum under the tongue of the baby, ask the pediatrician at the maternity hospital to check it. If it turns out to be short, it is better to cut it immediately.
If it turns out to be short, it is better to cut it immediately.
Fourth, frequent breastfeeding . The term “on demand” is commonly used, which confuses many moms. Many people think that a baby "demands" when it cries. At the same time, crying is the last thing a hungry child decides to do.
Signs of readiness to suckle in a newborn :
Muscles tense in the child, for example, he clenched his fists and flexed his arms at the elbows.
The child rolls, twists and arches his back.
The child makes different sounds.
The child draws his hands to his mouth (even if his eyes are closed, he can suck his own hand).
If the child's hand is close to the face, he turns towards the hand, pokes, opens his mouth.
A newborn in the first 3 months of life may want to kiss 15-25 times a day. After all, his stomach is very small (on the 1st day after birth - 5-7 ml, on the 3rd day - 22-27 ml, on the 7th day - 45-60 ml) and breast milk is quickly absorbed. In addition to receiving nourishment, the child also finds comfort in his mother's breast. Therefore, it is not recommended to feed the baby "according to the regime" - for example, once every 3 hours or to limit his time at the breast - for example, to feed no more than 15 minutes. Night feedings are crucial for successful lactation - thanks to them, the level of prolactin is maintained at the required level.
In addition to receiving nourishment, the child also finds comfort in his mother's breast. Therefore, it is not recommended to feed the baby "according to the regime" - for example, once every 3 hours or to limit his time at the breast - for example, to feed no more than 15 minutes. Night feedings are crucial for successful lactation - thanks to them, the level of prolactin is maintained at the required level.
Why frequent breastfeeding is important:
a) The number of prolactin receptors in the breast increases, which contributes to sufficient milk production in the future.
b) Promotes a more relaxed flow of milk, without pronounced symptoms of engorgement.
c) When feeding “according to the regimen”, there is a high risk that the child will be offended by the mother (after all, they do not immediately respond to his needs) and will behave restlessly at the breast.
Fifth, it is not recommended to give pacifiers to the child.
Why it's important:
a) Soothers artificially delay feeding time, resulting in poor weight gain and decreased milk production.
b) The child finds solace not at the mother's breast, but in a silicone object and may refuse the breast.
c) It spoils the grip of the breast, which leads to cracks, lactostasis.
Sixth, if you need to supplement with expressed milk and/or formula, then avoid the use of bottles.
Why is this important:
A) The baby gets used to a strong and constant flow of milk from the bottle and begins to behave restlessly at the breast, “lazy” to suck.
B) When sucking a bottle and a breast, different muscle groups are used, so the grip on the breast often deteriorates, the child sucks milk poorly, gains weight worse.
Seventh, the joint sleep of mother and child.
It is perfectly normal to sleep with your baby. A child should not be spoiled with attention or held too much in his arms. The more children are held in their arms, the more attention is paid to them, the better they grow. The presence of the mother, her smell, constantly encourages him to suckle the breast more often, which means sucking out more milk.
A child should not be spoiled with attention or held too much in his arms. The more children are held in their arms, the more attention is paid to them, the better they grow. The presence of the mother, her smell, constantly encourages him to suckle the breast more often, which means sucking out more milk.
Western parents are advised to leave their child to "shout out" before going to bed in order to raise an independent child who is used to loneliness and is able to calm himself down. However, modern research shows that in this case, the child's brain is irreparably damaged.
Safe sleep:
- The child should sleep on a clean and hard surface.
- Avoid sleeping with your baby if you are excessively tired.
- Do not leave your baby unattended in an adult bed.
- In cold weather, cover yourself with several layers of thin bed linen instead of one thick layer.
- Pets must not be in bed
- No one should smoke in the room where the baby sleeps.

Now consider some common cases:
- Mother's Rh negative or blood type incompatibility is not a contraindication to breastfeeding. Rh-conflict, blood type conflict or hemolytic disease of the newborn is not a contraindication. Rh antibodies are destroyed in the gastric juice of the newborn. Studies also show that in children with hemolytic disease, HB does not increase the breakdown of erythrocytes, red blood cells.
- The administration of anti-Rh immunoglobulin to prevent Rh conflicts in subsequent pregnancies in an Rh-negative mother is not a contraindication to breastfeeding. Anti-Rhesus immunoglobulin almost does not penetrate into breast milk. Most immunoglobulins are destroyed in the gastric juice of the newborn.
- Is it possible to breastfeed with jaundice?
Even with severe physiological jaundice in children in the first days of life, it is impossible to refuse breastfeeding. Early attachment of the baby to the breast and frequent feedings are an important factor in the prevention of jaundice, since colostrum, having a laxative effect, leads to a faster discharge of meconium (original feces). With insufficient nutrition of a newborn baby, jaundice may be more intense and prolonged due to the thickening of bile. (source - NATIONAL PROGRAM OF OPTIMIZATION OF FEEDING OF CHILDREN OF THE FIRST YEAR OF LIFE IN THE RUSSIAN FEDERATION, p.17).
With insufficient nutrition of a newborn baby, jaundice may be more intense and prolonged due to the thickening of bile. (source - NATIONAL PROGRAM OF OPTIMIZATION OF FEEDING OF CHILDREN OF THE FIRST YEAR OF LIFE IN THE RUSSIAN FEDERATION, p.17).
It is absolutely pointless to give the child water, glucose, activated charcoal, smectite, etc. in such a situation. - from this, the activity of liver enzymes, the function of which is reduced, will not increase. In some cases, it may be necessary to carry out phototherapy with special lamps, which can usually be rented from the hospital home.
- What to do if you are separated from your child?
It is recommended to express at least eight times a day. Whether you can pump something or not, breast stimulation is important to maintain and increase your milk supply.
If there is no joint stay in the maternity hospital, or if the baby was taken to the children's department for some medical reasons - do not hesitate to visit him and feed him there! If your and his condition allows, try to feed the baby only colostrum and then breast milk.
Try not to give supplements from a bottle, but from a spoon, pipette or syringe without a needle.
"Arrival" of milk.
Milk comes on 3-4 days after birth, less often - on 5-7. Your chest becomes hot, heavy, tight. If the mother rarely put the baby to the breast before, then engorgement may occur. At the same time, remember that you can do without pain and rough straining. Act according to the scheme: heat - light massage - removal of swelling from the areola - decant a little - attach the child - cold compress.
"Hard" straining, which is often used in the hospital, leads to severe swelling and worsening of the situation. Alcohol compresses, Vishnevsky ointment, etc. are not recommended.
How to remove swelling from the areola? Use the Pressure Softening technique introduced by international consultant Jean Kotterman.
It is necessary to evenly and gently press on the areola towards the chest and hold the pressure for at least a full minute (up to 2-3 minutes).
How to express properly? Fingers are placed on the border of the areola and white skin. First, the fingers are pressed in the direction of the chest: you seem to grab the milk-filled ducts that lie under the areola, and only then roll over them with your fingers. Important: the fingers do not fidget over the skin, they stand in one place on it.
How do you know if your baby is getting enough milk?
Newborns lose up to 6-10% of their birth weight in the first two days of their lives. This is a physiological norm. Most children regain their weight or begin to put on weight by 5-7 days of life.
- "Wet diaper test" .
Urination rate (per day) for a child up to 10 days old = number of days + 1.
That is, for example, a 2-day-old baby who has enough milk pees 3 times a day.
Babies over 10 days of age should write 12 or more times a day.
These calculations are correct if there is no water addition and no drips.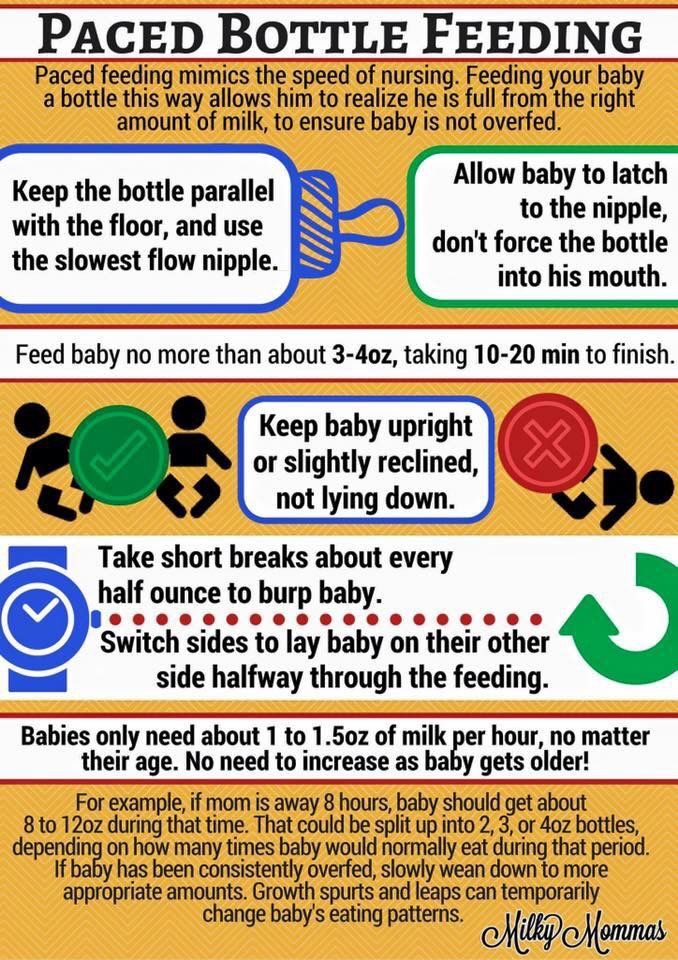
- Weight kit . The rate of weight gain for babies in the first 6 months of life is from 500 to 2000 g per month.
The set is not calculated from birth weight, but from the minimum (usually this is discharge weight). If the weight gain is less than 150g per week, we advise you to contact the AKEV specialists and the pediatrician.
- An infant should have at least 3-4 bowel movements per day (up to about 3-6 weeks). Then the chair is reduced - up to 1 time per day or less.
All other signs - crying of the baby, little pumping from the breast, no milk leakage, etc. - are not reliable signs of milk sufficiency / lack of milk .
Breastfeeding lifestyle:
- Care: it is recommended to wash the breasts 1-2 times a day while taking a shared shower (just with water, no soap).
- Diet: you should not sit on a "dry ration", the menu should be varied and healthy (without the use of chemical additives), eat according to your appetite.
 In large quantities, you should not consume whole milk, red vegetables and fruits, exotic fruits. Drink water and tea as needed.
In large quantities, you should not consume whole milk, red vegetables and fruits, exotic fruits. Drink water and tea as needed. - Sports: Moderate sports can be started as early as 6 weeks postpartum.
Don't worry if not everything was done at the maternity hospital. Feeding can still be improved. After discharge from the hospital, you can ask an experienced breastfeeding mother or breastfeeding specialists from large associations to help you.
Elvira Ibragimova, breastfeeding specialist in Naberezhnye Chelny, Association of Breastfeeding Consultants (AKEV), Republic of Tatarstan ), AKEV consultants: L. Kazakova, Y. Yakovlev, I. Ryukhova, E. Savosina, O. Gutyum, N. Zaslavskaya, M. Gudanova.
Tips for Breastfeeding - Kiev City Maternity Hospital №2
Home › Helpful Tips › Tips for Breastfeeding
Every mother looks forward to the moment when she puts her baby to her breast for the first time. In the maternity hospital, we will show you how to apply the baby correctly and control the feeding process. In just a few times, the mother begins to understand exactly how to put the baby to the breast, and she even forms her own special feeding ritual. But the child himself begins to suckle correctly only two months after birth, and all this time the mother must teach him and control the process of breastfeeding.
In just a few times, the mother begins to understand exactly how to put the baby to the breast, and she even forms her own special feeding ritual. But the child himself begins to suckle correctly only two months after birth, and all this time the mother must teach him and control the process of breastfeeding.
The concept of proper nipple latch
The most common mistake is the belief that the nipple plays a key role in the process of feeding a newborn. However, in fact, the correct latch on the nipple occurs when the nipple is not involved in the feeding process.
In order for the child to eat properly, he needs to stimulate the areola, in which the milk sinuses are located. The nipple acts only as a conductor for milk.
If the baby is properly attached to the breast, has a wide open mouth, it captures the breast as much as possible, and the nipple is pointing up. The baby should be tightly pressed to the mother, and to get milk, the lower jaw works intensively. This process does not cause pain or injury to the nipple.
This process does not cause pain or injury to the nipple.
If is not properly applied, the baby does not latch onto the entire breast, but only receives milk from the nipple, without stimulating production. In this case, the baby may be half-starved, and the mother may develop milk stagnation, mastitis, or cracks. Some mothers do not take such difficulties seriously, and continue to feed the child incorrectly, decanting milk residues and treating mastitis and fissures. However, this will not help eliminate the problem and only the correct feeding technique can correct the situation.
Tips for proper feeding technique
The mother should be in a comfortable position in which her shoulders are completely relaxed. If a woman is not allowed to sit after giving birth, it is better to feed the baby lying down.
Position the baby correctly at the breast. The body of the baby should be returned to the mother, and the head and mouth should be at the level of the nipple.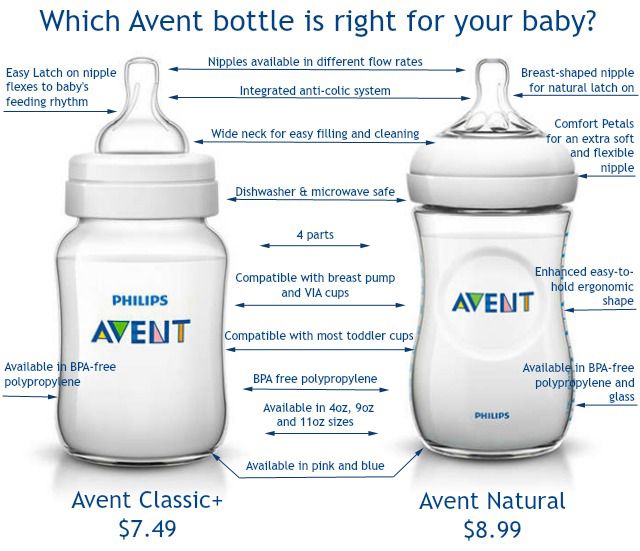 If the baby takes the wrong position, he will pull the breast too hard and injure the nipples. One of the best positions for feeding a baby is considered to be the position in which both mother and child lie on their sides facing each other, and the mother holds the child by the back and buttocks. Some mothers are afraid that when the child rests on the chest with his nose, it becomes more difficult for him to breathe. But this is not the case, since the baby receives a sufficient amount of air during feeding through the edge of the nostrils. Therefore, you do not need to hold the chest with your hand, while simultaneously blocking the milk channels.
If the baby takes the wrong position, he will pull the breast too hard and injure the nipples. One of the best positions for feeding a baby is considered to be the position in which both mother and child lie on their sides facing each other, and the mother holds the child by the back and buttocks. Some mothers are afraid that when the child rests on the chest with his nose, it becomes more difficult for him to breathe. But this is not the case, since the baby receives a sufficient amount of air during feeding through the edge of the nostrils. Therefore, you do not need to hold the chest with your hand, while simultaneously blocking the milk channels.
How to apply the baby when feeding? Every baby is born with a reflex that allows him to latch onto the breast. But for the first few feedings, the baby can be helped by moving the areola along the upper lip. Gradually, the baby himself will learn to reach for the breast and grab the nipple, and the mother will only need to guide his head. When the baby is ready to feed, her mouth is wide open, the lower lip is retracted and covers most of the areola, being far from the nipple.
When the baby is ready to feed, her mouth is wide open, the lower lip is retracted and covers most of the areola, being far from the nipple.
Feeding process. When the baby is suckling, part of the gum and tongue will be visible on the lower lip, which make wave-like movements to squeeze out milk. While eating, the baby's lips should be turned around (in no case drawn in), the nose and chin should be pressed to the chest, and the cheeks should move freely. When the child eats well, hear how he makes swallowing movements.
Best positions for feeding
There are several basic positions that will help you understand how to put your baby on for comfortable feeding.
Tummy to Tummy is one of the most common and comfortable positions, and for extra comfort, mom can put a pillow or cushion under her arm.
Feeding while sitting mother and child from the tummy to tummy position should be mentally "planted". In this position, the child is also deployed with the body to the mother, leaning his head on the mother's hand. It is best if the baby's head is in the crook of the elbow.
In this position, the child is also deployed with the body to the mother, leaning his head on the mother's hand. It is best if the baby's head is in the crook of the elbow.
Armpit posture
For feeding in this position, the mother needs to sit on the sofa, put a pillow next to it, and the baby on it so that his body is under his arm. This position is convenient because the process of breastfeeding is easier to control, the mother's hands do not get tired, and the baby grabs the breast faster.
Lying position
This position is more suitable for mothers who cannot sit up after giving birth. In fact, these are just variations of the tummy to tummy pose.
Standing feeding
If the baby is in a sling, it is possible to feed him standing, but for this the baby must be in a sitting or reclining position. It is not allowed to feed the baby when he lies on his mother's stomach. Firstly, in this position, it is inconvenient for him to make sucking movements, and secondly, pressure on the stomach can lead to regurgitation of milk.
Proper feeding of twins
It is best to try out several positions to find the most comfortable for feeding two babies at the same time. So the children will eat on time, and the mother will not rush during feeding.
Duration of feeding
There is no single time period that is considered sufficient for feeding. The time a baby spends suckling at the breast depends on his temperament, sucking speed, mother's mammary glands and many other factors. On average, the duration of one feeding is from 5 to 20 minutes. Sometimes the child falls asleep right in the process of eating. If this happens, you need to slightly twist it by the cheek so that the child wakes up and continues to eat. Many mothers are interested in the question of whether it is possible to give the child both breasts in one feeding. If a woman has no problems with lactation, and the child is alone, the baby should suckle only one breast at a time (i.e., it is necessary to give each breast in turn for a new feeding). Therefore, when sucking one of the breasts, the second will be filled with milk automatically.
Therefore, when sucking one of the breasts, the second will be filled with milk automatically.
What is the right way to finish feedings?
It is important that a full baby releases the nipple on his own, so you can not try to remove it by force. Firstly, this can make the baby angry, and secondly, when the nipple is pulled out, the child will reflexively clench his jaw and pinch the nipple in his mouth, which can lead to injury. In this case, it is enough just to take the nipple to the side, to the corner of the mouth, and the baby will release it himself.
Approximate feeding frequency.
As with the duration of feeding, there is no clear time frame in this matter, most adhere to the feeding schedule on demand. You can understand that the baby is hungry by his behavior: he begins to cry, turn his head and open his mouth when he touches his face. The first few days after birth, the baby asks for breasts from 7 to 14 times a day, but in the future, the frequency of attachments increases and can reach up to 4 times per hour.
How to breastfeed a child who cries a lot?
The breast perfectly calms the baby, but this remedy should not be abused. In order for the child to properly grab the breast and eat well, you need to hold her in your arms a little so that she calms down a little, and even better, stops crying altogether. An emotionally excited baby can squeeze a drop of milk onto his lips, or draw a nipple on his cheek - then he will quickly calm down.
How to understand that the baby is full?
Babies can't suck as much milk from their breasts at one time as they can from a bottle, so babies suckle at their mother's breasts much more often than formula-fed babies.
You can understand that the baby has enough mother's milk by the following signs:
- After sucking, there is a feeling of emptiness in the breast
- The child often attaches to the breast
- The baby has regular stools and urination (about 5-6 diapers should go per day)
- The baby's general health is good: he is in a good mood, willing to play, his eyes are clear and firm skin is clear.

Physiologically, there are no microorganisms on the female breast. For proper care, it is enough just to take a shower twice a day, but the use of soap destroys the natural lubrication of the breast, which protects it from viruses and bacteria.
✖ - During feeding, the mother holds the breast from above, keeps it on weight, fearing that the baby will suffocate.
When a baby suckles at the breast, his or her nose may fit snugly against it or even press into the breast. This is absolutely normal, and you do not need to hold your chest. The baby gets enough oxygen through the edges of the nostrils, and milk comes in response to sucking movements, and not due to the special position of the breast.
✖ - Drink water or tea after feeding. Breast milk is a very balanced product that is not only food, but also drink. Therefore, it is not necessary to give the baby any additional fluids.
✖ - Switching to formula milk for infectious diseases or cracked nipples.