Baby struggling to breathe when feeding
Laryngomalacia (for Parents) - Nemours KidsHealth
What Is Laryngomalacia?
Laryngomalacia is a common cause of noisy breathing in infants. It happens when a baby's larynx (or voice box) is soft and floppy. When the baby takes a breath, the part of the larynx above the vocal cords falls in and temporarily blocks the baby's airway.
Laryngomalacia (luh-ring-oh-muh-LAY-shuh) usually gets better on its own by the time a baby is 1 year old.
What Are the Signs & Symptoms of Laryngomalacia?
Babies with laryngomalacia make a harsh, squeaky sound when breathing in. This sound, called stridor, can start as soon as the baby is born or, more often, in the first few weeks after birth. Symptoms usually get worse over several months.
Most babies with laryngomalacia do not have trouble breathing or feeding, even though their breathing is noisy. Breathing usually gets noisier when the baby is crying, feeding, sleeping, lying down, or has an upper respiratory infection.
Most babies with the condition have mild symptoms. A baby whose symptoms are more serious might have:
- trouble breathing (look for tugging in at neck or stomach)
- feeding problems
- poor weight gain
- breathing pauses (apnea)
- blue skin or lip color (cyanosis)
Call the doctor right away if your baby has these symptoms or breathing suddenly gets worse.
Babies with laryngomalacia often have gastroesophageal reflux (GER). This happens when food and acid go back up into the esophagus. If stomach acid reaches the voice box, symptoms may get worse. Formulas or medicines to help with reflux may help with breathing symptoms.
What Causes Laryngomalacia?
Doctors don't know what causes laryngomalacia, but it may have something to do with how the voice box formed before the baby was born. The muscles supporting the voice box may be weak or don't coordinate well with breathing. Gastroesophageal reflux may also play a role.
How Is Laryngomalacia Diagnosed?
Doctors often suspect laryngomalacia at birth or soon after based on the baby's symptoms and an exam. To confirm the diagnosis, a pediatric ear, nose, and throat (ENT) specialist will do a procedure called flexible laryngoscopy. To do this, the doctor passes a thin tube through the baby's nose or mouth to look at the airway and vocal cords in the voice box.
The doctor may check oxygen levels and order other tests to check for swallowing problems or GER. The baby's good weight gain and growth are very important.
How Is Laryngomalacia Treated?
Most of the time, laryngomalacia gets better on its own, usually by a baby's first birthday. Doctors will do regular exams to check the baby's breathing and weight. Because most babies also have GER, doctors usually prescribe anti-reflux medicine.
A baby who has severe breathing problems or poor growth may need a surgery called supraglottoplasty (soo-pruh-GLOT-oh-plass-tee). Doctors do this procedure through the baby's mouth to tighten the floppy tissue above the voice box. This will improve the baby's feeding and breathing.
This will improve the baby's feeding and breathing.
What Else Should I Know?
Noisy breathing and other laryngomalacia symptoms usually get worse over several months, then start to improve after 3–6 months. Symptoms clear up completely in most kids. Occasionally, an older child with a history of laryngomalacia may have noisy breathing while exercising, during a viral infection, or when sleeping.
Reviewed by: Steven M. Andreoli, MD
Date reviewed: October 2019
Aspiration in Babies and Children
ABOUT CAUSES DIAGNOSIS TREATMENT NEXT STEPS
What is aspiration in babies and children?
Aspiration is when something enters the airway or lungs by accident. It may be food, liquid, or some other material. This can cause serious health problems, such as pneumonia. Aspiration can happen when a person has trouble swallowing normally. This is known as dysphagia. It can also happen if a child has gastroesophageal reflux disease (GERD). This is when the contents of the stomach come back up into the throat.
This is known as dysphagia. It can also happen if a child has gastroesophageal reflux disease (GERD). This is when the contents of the stomach come back up into the throat.
When your child swallows food, it passes from the mouth down into the throat. This is called the pharynx. From there, the food moves down through a long tube (esophagus) and into the stomach. This journey is made possible by a series of actions from the muscles in these areas. If your child has dysphagia, the muscles don’t work normally. They cause problems with the swallowing process.
The pharynx is also part of the system that brings air into the lungs. When a person breathes, air enters the mouth and moves into the pharynx. The air then goes down into the main airway (trachea) and into the lungs. A flap of tissue called the epiglottis sits over the top of the trachea. This flap blocks food and drink from going down into the trachea when your child swallows. But in some cases, food or drink can enter the trachea. It may go down as your child swallows. Or it may come back up from the stomach. A child with dysphagia is much more likely to aspirate. A child with a developmental or health problem is more likely to have dysphagia.
It may go down as your child swallows. Or it may come back up from the stomach. A child with dysphagia is much more likely to aspirate. A child with a developmental or health problem is more likely to have dysphagia.
Aspiration can happen during a feeding or meal. And it can happen after a feeding or meal. This is common in babies and children with certain health conditions. Aspiration can also happen at any time when your child swallows saliva.
If your child aspirates a small amount of material, it may not cause much harm. This can happen in children who don’t have a health problem. It can happen when eating, sleeping, or talking. But aspiration that happens often or in a large amount can be serious.
What causes aspiration in babies and children?
Aspiration is often caused by dysphagia. This is when the muscles don’t work normally in the throat and lead to swallowing problems. Different medical conditions can lead to this, such as:
- Abnormal anatomy, such as a cleft palate or a problem in the esophagus
- Delayed growth, from premature birth or a condition such as Down syndrome
- Brain damage or other problems, such as from cerebral palsy or infection
- Problems with the cranial nerves that control the muscles of swallowing
- Neuromuscular disease, such as spinal muscular atrophy
- Medical procedures, such as a nasogastric tube or a tracheostomy
Gastroesophageal reflux disease (GERD) can also cause aspiration.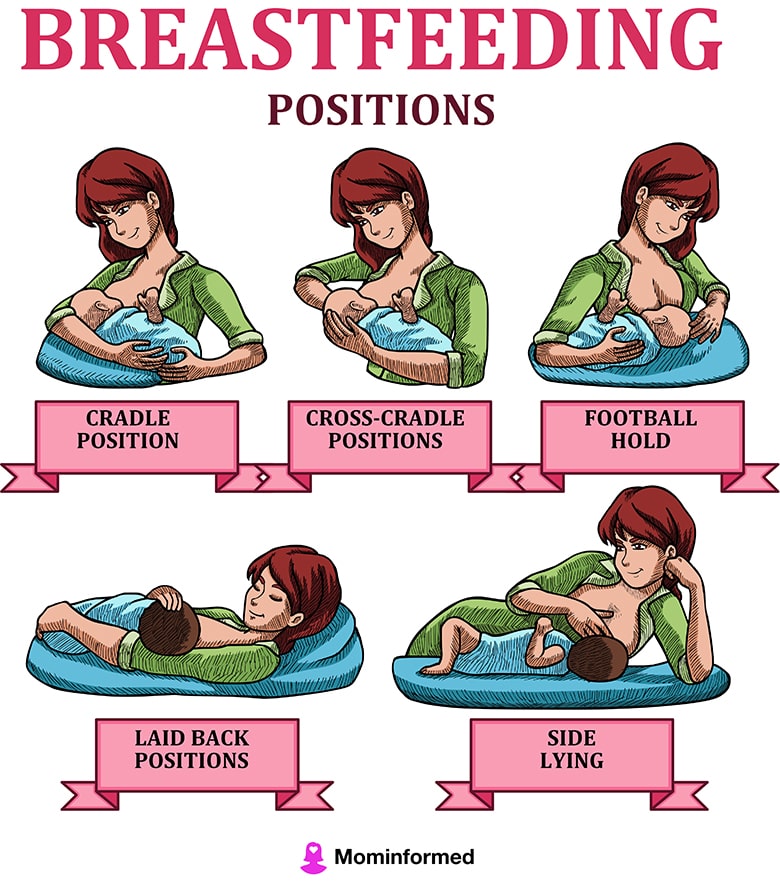 This is when the contents of the stomach come back up into the throat.
This is when the contents of the stomach come back up into the throat.
What are the symptoms of aspiration in babies and children?
Aspiration can cause signs and symptoms in a baby such as:
- Weak sucking
- Choking or coughing while feeding
- Other signs of feeding trouble, like a red face, watery eyes, or facial grimaces
- Stopping breathing while feeding
- Faster breathing while feeding
- Voice or breathing that sounds wet after feeding
- Slight fever after feedings
- Wheezing and other breathing problems
- Repeated lung or airway infections
And aspiration can cause signs and symptoms in an older child such as:
- Choking or coughing while eating
- Voice that sounds wet after eating
- Slight fever after meals
- Complaints of food feeling stuck or coming back up
- Wheezing and other breathing problems
- Repeated lung or airway infections
Signs and symptoms can happen right after eating. Or they may happen over time. Your child may not have all of these signs and symptoms. The signs and symptoms may depend on the age of your child, and how often and how much your child aspirates.
Or they may happen over time. Your child may not have all of these signs and symptoms. The signs and symptoms may depend on the age of your child, and how often and how much your child aspirates.
Some children who aspirate do not have any signs or symptoms. This is called silent aspiration.
How is aspiration in babies and children diagnosed?
Your child will need to be checked for aspiration if he or she has:
- Any signs or symptoms of aspiration
- Health problem that can cause trouble swallowing
- GERD
The healthcare provider will ask about your child’s medical history and symptoms. This may be done by a speech-language pathologist (SLP). The SLP may ask about what foods or drink cause problems, and when your child’s symptoms happen. He or she may want to watch your child during a feeding.
Your child may also need tests. These can check for problems and show if food and fluid is going into your child’s lungs. The tests may include:
The tests may include:
- Chest X-ray or CT scan
- Modified barium swallow test (MBS)
- Fiber optic endoscopic evaluation of swallowing (FEES)
How is aspiration in babies and children treated?
Treatment for aspiration may vary depending on the cause and severity. Treatments for your child may include:
- Making changes in position and posture during meals
- Changing the thickness of liquids
- Changing the types of foods in your child’s diet
- Doing exercises to help with swallowing (for an older child)
- Medicines for GERD
- Medicines or Botox injection for children who make excess saliva
- Surgery to reduce reflux
- Surgery to correct a problem such as a cleft palate
If your child still has a high risk of aspiration despite these methods, he or she may need a special tube to help with eating for a while. The feeding tube will help your child get good nutrition until his or her risk of aspiration improves. Your child will not eat or drink normally until the tube is removed. A thin tube may be put through the nose down into the stomach. This is called a nasogastric tube. This may be used for a short time while other treatment is considered. Or a tube may be put directly into your child’s stomach during a surgery. This is called a gastrostomy tube.
The feeding tube will help your child get good nutrition until his or her risk of aspiration improves. Your child will not eat or drink normally until the tube is removed. A thin tube may be put through the nose down into the stomach. This is called a nasogastric tube. This may be used for a short time while other treatment is considered. Or a tube may be put directly into your child’s stomach during a surgery. This is called a gastrostomy tube.
In some children, aspiration lessens over time. In other cases, a child may need more treatment to address the cause. Your child’s healthcare providers will carefully watch your child so that he or she can return to normal eating as soon as possible.
Talk with your child’s healthcare provider if your child has a tracheostomy tube. You may need to suction food or liquid from the tube.
What are possible complications of aspiration in babies and children?
A major complication of aspiration is harm to the lungs. When food, drink, or stomach contents make its way into your child’s lungs, it can damage the tissues there. The damage can sometimes be severe. Aspiration also increases the risk of pneumonia. This is an infection of the lungs that causes fluid to build up in the lungs. Pneumonia needs to be treated with antibiotics. In some cases, it may cause death.
When food, drink, or stomach contents make its way into your child’s lungs, it can damage the tissues there. The damage can sometimes be severe. Aspiration also increases the risk of pneumonia. This is an infection of the lungs that causes fluid to build up in the lungs. Pneumonia needs to be treated with antibiotics. In some cases, it may cause death.
Other possible complications from aspiration include:
- Dehydration
- Malnutrition
- Weight loss
- Increased risk of other illness
When should I call my child's healthcare provider?
Let your child’s healthcare provider know right away if your child has any signs or symptoms of aspiration. It needs to be treated as soon as possible.
Key points about aspiration in babies and children
Aspiration is when something enters the airway or lungs by accident. It may be food, liquid, or some other material. This can cause serious health problems, such as pneumonia. Aspiration can happen when a child has trouble swallowing normally. This is known as dysphagia.
Aspiration can happen when a child has trouble swallowing normally. This is known as dysphagia.
- Your child might have aspiration caused by problems with growth, development, or certain health conditions.
- Your child may have a signs such as breathing problems and a wet-sounding voice after meals.
- Some children with aspiration don’t have any signs or symptoms. This is known as silent aspiration.
- If your child has any symptoms of aspiration, he or she needs to be checked and treated right away.
- Aspiration may be treated by addressing the cause of dysphagia. It can also be managed with methods to help your child feed better.
Next steps
Tips to help you get the most from a visit to your child’s healthcare provider:
- Know the reason for the visit and what you want to happen.
- Before your visit, write down questions you want answered.

- At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you for your child.
- Know why a new medicine or treatment is prescribed and how it will help your child. Also know what the side effects are.
- Ask if your child’s condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if your child does not take the medicine or have the test or procedure.
- If your child has a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your child’s provider after office hours. This is important if your child becomes ill and you have questions or need advice.
The baby gets tired quickly when feeding and breathes often: symptoms, diagnosis
With the advent of the baby, all the mother's attention is focused on feeding the baby. After all, I really want the baby to gain weight well. But often during feeding, a woman notices that the baby gets tired quickly. In such a situation, the baby's breathing quickens, which prevents him from eating the prescribed norm. If such a picture is observed with frightening frequency, it is necessary to find out the cause of the problem.
After all, I really want the baby to gain weight well. But often during feeding, a woman notices that the baby gets tired quickly. In such a situation, the baby's breathing quickens, which prevents him from eating the prescribed norm. If such a picture is observed with frightening frequency, it is necessary to find out the cause of the problem.
In pediatric cardiology, there are several important signs that indicate heart problems in a young patient. The children's cardiologist of the multidisciplinary center "Edkarik" will be able to figure out what caused the difficulties in feeding. At the first negative symptoms in the baby, parents should contact us to exclude the presence of a serious heart pathology in the crumbs. nine0003
Features of breathing in infants
It should be noted right away that difficulty breathing during feeding is not always an indicator of an existing heart pathology. Such a symptom is typical for respiratory diseases, breathing difficulties may be associated with structural features of the nasal septum. This problem is often observed in the first weeks due to undeveloped breasts in the mother. The child has to make every effort to get the right portion of food. Therefore, he quickly gets tired, and his breathing goes astray from the normal rhythm. nine0003
This problem is often observed in the first weeks due to undeveloped breasts in the mother. The child has to make every effort to get the right portion of food. Therefore, he quickly gets tired, and his breathing goes astray from the normal rhythm. nine0003
The breathing of children in the first months of life has its own characteristics. Babies need twice the amount of oxygen, but their respiratory system is not yet fully formed. Certain difficulties in the respiratory function are imposed by narrow nasal passages and weakness of the pectoral muscles. Therefore, breathing in children up to a year is uneven. The child often takes quick breaths, so his breathing is shallow and intermittent.
The norm of respiratory movements in babies of the first month of life is 40-60, from the end of the fourth week and up to 3 months - up to 45, in the period of 4-6 months - 35-40. By the year, the baby is already taking about 30-35 breaths per minute, which is considered the norm. nine0003
Mom can determine the respiratory rate on her own.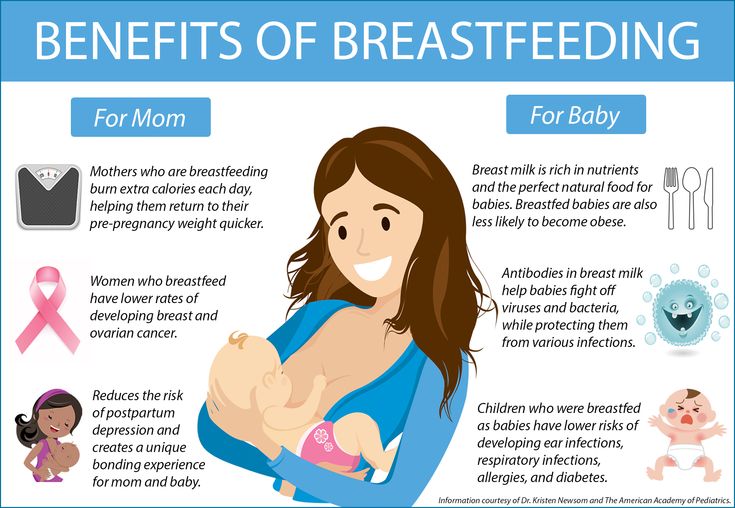 To do this, put the baby on his back, and use a stopwatch to count the number of breaths. Since babies "breathe" with their tummies, such a calculation is easy to make. The main condition for performing this procedure is that the child must be calm.
To do this, put the baby on his back, and use a stopwatch to count the number of breaths. Since babies "breathe" with their tummies, such a calculation is easy to make. The main condition for performing this procedure is that the child must be calm.
When there is no reason to worry
The nervous system of young children is still imperfect, so they cannot control their breathing. During active games and crying, the frequency of respiratory movements increases, and in a dream they often sniffle. If such features are observed sporadically, you should not worry. The sniffing nose can be washed with boiled water, and then carefully remove the dried mucus. nine0003
What should cause alarm
You need to see a doctor if the baby:
- holds his breath for a long time;
- exhales noisily;
- if breathing is accompanied by wheezing and wheezing.
Typically, such symptoms can be traced against the background of an acute period of respiratory diseases.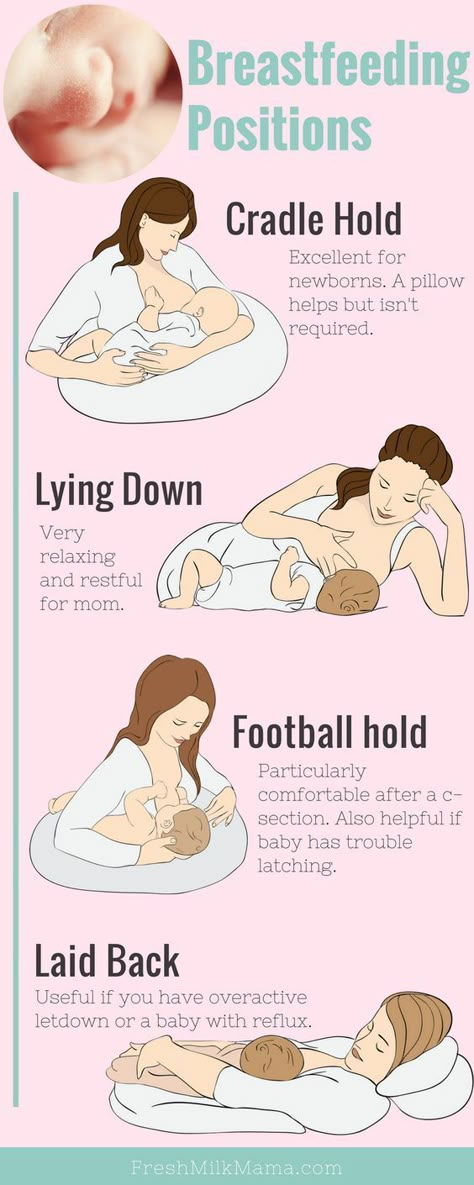 Timely treatment will help to quickly eliminate these negative signs, after which the child will be able to breastfeed normally again.
Timely treatment will help to quickly eliminate these negative signs, after which the child will be able to breastfeed normally again.
Which symptoms require special attention
We have listed physiological breathing problems. But sometimes the situation is much more serious than the usual runny nose. We list the signs that should be a strong argument for parents to urgently visit a pediatric cardiologist.
- Cyanosis
If holding the breath during feeding is accompanied by a blue nasolabial triangle, this sign indicates a lack of oxygen. In severe forms of cardiac pathologies, the chin and fingers of the baby turn blue. This symptom is characteristic of congenital malformations of both the heart and vascular anomalies. nine0003
- Shortness of breath
This symptom also indicates a lack of oxygen. Since the child has to expend more energy during sucking, this symptom is more pronounced than at rest. A cause for concern can be considered frequent breaks for rest during suckling. Normally, there are no more than two such pauses, and a child with heart disease takes breaks after 2-3 sips.
A cause for concern can be considered frequent breaks for rest during suckling. Normally, there are no more than two such pauses, and a child with heart disease takes breaks after 2-3 sips.
- Fatigue
Infants with congenital heart defects are much less active than healthy children. They are not able to suck out the norm during feeding, so they lose weight. The problem is aggravated by frequent breathing. The child simply suffocates under tension. nine0003
- Chest pain
Infants may not complain of such a symptom, but an observant mother will notice under what circumstances and how often the child begins to worry.
If all the described signs are repeated from the baby during feeding regularly, it is urgent to consult a pediatric cardiologist. A full-scale examination will determine the cause of the problem, and an experienced pediatric cardiologist will prescribe adequate therapy for the child. nine0003
nine0003
Peculiarities of diagnosing infants
Babies under one year old cannot describe the symptoms that prevent them from developing normally. Therefore, all hope for an objective examination. During the initial examination of the infant, the pediatric cardiologist:
- evaluates the general condition;
- notes the color of the skin;
- listens to the baby's heart;
- performs heart rate monitoring and saturation level measurement.
The doctor pays special attention to taking an anamnesis, since such information can indicate the cause of the problem. For example, an infection transmitted by a woman during her mother's pregnancy can provoke the development of congenital heart defects. An important factor is heredity, especially if there were cases of premature death (up to 50 years) among close relatives in the family. After collecting the data, the pediatric cardiologist will definitely prescribe the following types of diagnostic procedures:
- ECG with daily monitoring;
- ultrasound of the heart;
- Chest x-ray;
- Laboratory tests.

Instrumental methods of examination with the use of modern devices will clarify the parameters of the baby's heart and the features of its anatomical structure. Ultrasound diagnostics helps to identify defects in the heart chambers and great vessels. Having the data of all studies on hand, the pediatric cardiologist will draw up an individual treatment program or prescribe additional procedures. In severe cardiac pathologies and rhythm disturbances, the question of a surgical way to eliminate the problem can be decided. nine0003
Examination and treatment in the center "Edkarik"
Among our guarantees:
- professionalism of doctors;
- high quality service;
- comfortable conditions in the clinic;
- individual approach;
- a wide range of services;
- accompanying patients during the rehabilitation period.
Our clinic is known not only in Kaliningrad, but also in other regions of the country. Parents and their kids will feel comfortable in our center, because there is everything you need to make sick children feel at home with us. You can make an appointment with a pediatric cardiologist on the official website of our center. There are also contact numbers where parents can consult on issues of concern to them. nine0003
Parents and their kids will feel comfortable in our center, because there is everything you need to make sick children feel at home with us. You can make an appointment with a pediatric cardiologist on the official website of our center. There are also contact numbers where parents can consult on issues of concern to them. nine0003
Breathe to eat?!
08/15/2016
The topic of breastfeeding is very relevant both for those who are just preparing to become a mother, and for those who are already clutching their first child to their breasts. Mother's milk is truly the best food that can only be offered to a child up to a year old. It helps the baby grow healthy and strengthens his immunity. That is why it is especially necessary for a child in the first six months of life. Breast milk contains all the necessary nutrients for the baby, and in the optimal ratio and form, adapted to the characteristics of the digestive system of the newborn. In addition, it is rich in vitamins, enzymes, minerals and contributes to the creation of the necessary conditions for the formation of the "correct" intestinal microbial biocenosis. nine0003
nine0003
In addition, during breastfeeding there is direct communication between mother and child, which contributes to the formation of a positive emotional bond between them. The very act of sucking is extremely important for the baby. Sucking for an infant is a need and a pleasure that is not directly related to the feeling of hunger. Thanks to sucking, the baby develops the jaw apparatus, muscles of the mouth and tongue, which is especially important in the future, for example, in the development of speech.
But sometimes the process of feeding may not go as smoothly as a mother would like. One of the most common reasons a baby refuses to breastfeed is difficulty in breathing through the nose. A significant role in the development of this condition is given to the physiological characteristics of the nasal mucosa of the newborn, as well as the anatomical features of the child's nose itself. In an infant, the nasal passages are much wider and shorter, the mucous lining the nasal cavity is thickened and rich in a dense network of blood vessels, while the number of glands that produce mucus is not yet large. Even a small swelling of the mucosa can block nasal breathing. During breastfeeding, the baby has to suck and breathe at the same time, and if the nose is clogged, it is simply impossible to combine these processes. If the baby does not breathe through the nose, feeding turns into torment - the baby cannot suckle without interruption, because he is suffocating. nine0003
Even a small swelling of the mucosa can block nasal breathing. During breastfeeding, the baby has to suck and breathe at the same time, and if the nose is clogged, it is simply impossible to combine these processes. If the baby does not breathe through the nose, feeding turns into torment - the baby cannot suckle without interruption, because he is suffocating. nine0003
The child constantly has to let go of the chest in order to breathe in air through the mouth. This is repeated several times, and as a result, the baby drops the breast. In addition, swallowing air through the mouth contributes to its entry into the stomach, followed by regurgitation of its contents. Frequent regurgitation, in turn, contributes to irritation of the nasal mucosa and nasopharynx with gastric contents and the development of inflammation - rhinitis, which is manifested by prolonged difficulty in nasal breathing.
That is why it is so important for newborns to pay close attention to nasal hygiene to ensure and maintain free nasal breathing. On the Internet, you can find recommendations advising mothers to instill vasoconstrictors for babies in the nose of babies before feeding. Such advice can be useful only if the child has a runny nose, in all other cases, one should be aware of side effects and the inadmissibility of long-term use of such drugs, as well as the need to consult a doctor. nine0003
On the Internet, you can find recommendations advising mothers to instill vasoconstrictors for babies in the nose of babies before feeding. Such advice can be useful only if the child has a runny nose, in all other cases, one should be aware of side effects and the inadmissibility of long-term use of such drugs, as well as the need to consult a doctor. nine0003
For daily care and cleansing of the nasal mucosa, special products based on natural sea water have been developed. One of these products is the RINOSTOP® AQUA product line.
RINOSTOP® AQUA contains 100% natural sea water, widely known for its beneficial properties. No preservatives, stabilizers or other chemicals that can cause irritation of the nasal mucosa are used in the process of production and purification of water; preserved macro- and microelements of natural sea water (K, Mg, Na, Ca, Cl). nine0003
The products of the line are available in bottles of different sizes; equipped with nozzles that take into account the anatomical structure of the nose and provide a continuous spray of water of different intensity - in the form of a jet, shower or soft shower.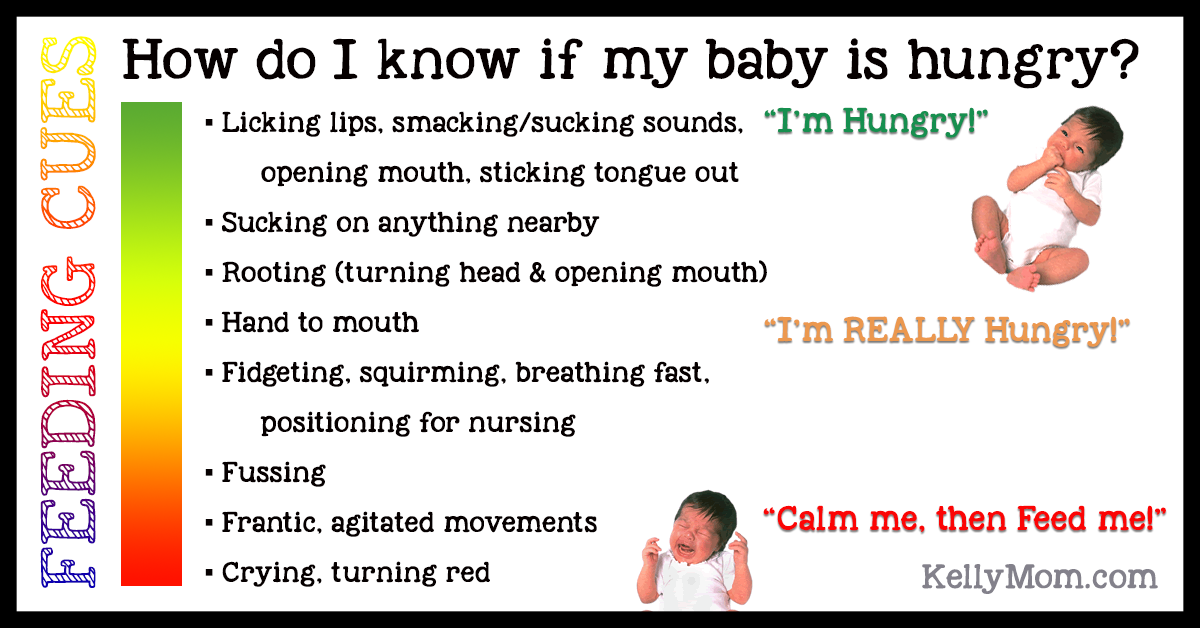
The special design of the "BAG-ON-VALVE" bottles allows the use of funds in any position of the bottles with a full consumption of the contents without residue.
RINOSTOP® AQUA BABY is perfect for daily hygiene and moisturizing of little noses from birth. It contains sea water in an isotonic concentration close in its physiological characteristics to human plasma. Micro-diffusion water supply in the form of a soft shower provides:
- gentle care for the delicate nasal mucosa of babies;
- uniform irrigation of the entire surface of the mucosa by spraying sea water in the form of tiny particles mixed with air - "water vapor"; it is this spray that minimizes the risk of getting into the middle ear cavity;
- cleansing of mucus, crusts, dust and small foreign particles;
- maintaining the normal physiological state of the nasal mucosa and facilitating nasal breathing in babies, contributing to the normalization of good sleep and optimizing the process of breastfeeding; nine0028
- moisturizing the nasal mucosa of infants, incl.