Baby supplemental feeding
Breastfeeding FAQs: Solids and Supplementing (for Parents)
Breastfeeding is a natural thing to do, but it still comes with its fair share of questions. Here's what you need to know about about introducing formula, solids, and more.
Is it OK to Give My Baby Breast Milk and Formula?
Breast milk is the best nutritional choice for babies. But in some cases, breastfeeding (or exclusive breastfeeding) isn’t possible or an option. What’s best for your baby's health and happiness is, in large part, whatever works for your family. So if you need to supplement, your baby will be fine and healthy, especially if it means less stress for you.
Babies who need supplementation may do well with a supplemental nursing system. This is when moms place a small tube by their nipple that delivers pumped milk or formula while a baby is breastfeeding.
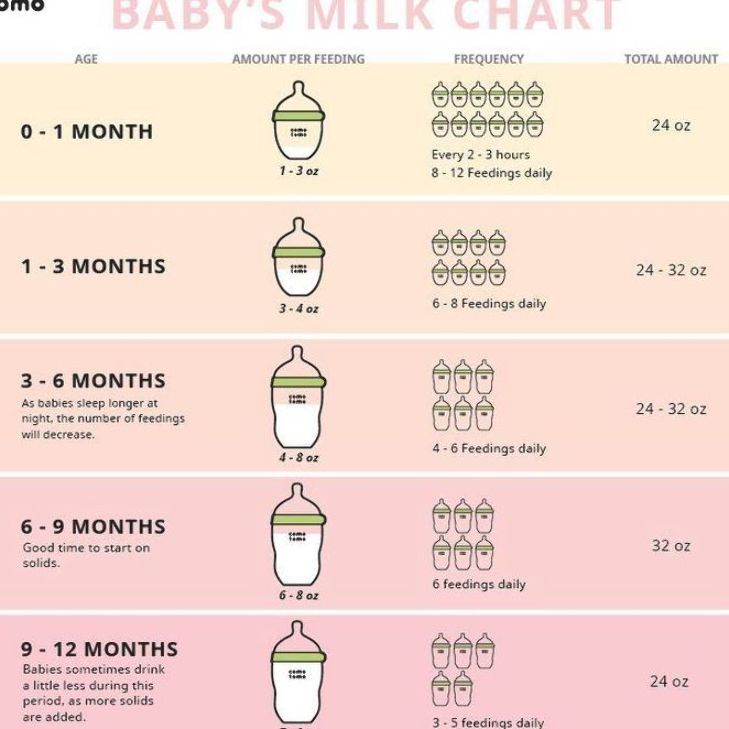
Babies also can get pumped milk or formula by bottle. But it’s a good idea to wait until your baby has gotten used to and is good at breastfeeding. Lactation professionals recommend waiting until a baby is about 3-4 weeks old before offering artificial nipples of any kind (including pacifiers).
If I Give My Baby Formula, How Do I Start?
If you're using formula because you're not producing the amount of milk your baby needs, nurse first. Then, give any pumped milk you have and make up the difference with formula as needed.
If you're stopping a breastfeeding session or are weaning from breastfeeding altogether, begin to replace breastfeeding with bottle feeds. As you do this, pump to reduce uncomfortable engorgement. Engorgement is when your breasts overfill with milk and other fluids and get painful, swollen, warm, or hard. This can lead to problems with plugged ducts (when the ducts won’t drain well or at all) or a breast condition called mastitis.
When you reduce the number of nursing sessions, your milk supply will decrease. Your body will adapt to produce just enough milk to fit your new feeding schedule.
How Might a Diet With Formula Affect My Baby?
Starting your breastfed baby on formula can cause some change in the frequency, color, and consistency of your baby’s poop. Be sure to talk your doctor, though, if your baby has trouble pooping.
If your baby refuses formula alone, you can try mixing some of your pumped breast milk with it to help the baby get used to the new taste.
Is it OK for Me to Give My Baby the First Bottle?
If possible, have someone else give the first bottle. This is because babies can smell their mothers and they're used to receiving breast milk from mom, not a bottle. So try to have someone else — like a caregiver or partner — give the first bottle.
Also consider being out of the house or out of sight when your baby takes that first bottle, since your little one will wonder why you're not doing the feeding as usual. Depending on how your baby takes to the bottle, you might need to keep doing this until your baby gets used to bottle feeding.
If your baby has a hard time adjusting to this new form of feeding, be patient and keep trying. Talk to your doctor if you have questions.
Does My Breastfed Baby Need Supplements?
Breast milk contains many vitamins and minerals. But it’s a good idea to give a daily supplement for some nutrients that may be lacking. It all depends on your baby’s age.
Here are some guidelines:
- Vitamin D. Breastfed babies need to take a daily vitamin D supplement. Vitamin D is added to infant formulas. Vitamin D is made by the body when the skin is exposed to sunlight, but it is not safe for infants under 6 months to be in direct sunlight. (After 6 months, use sunscreen when in the sun to protect your baby’s sensitive skin).
- Iron. Iron is a mineral found in breastmilk during the first 4 months of life. After that, babies need an iron supplement until they begin eating enough iron-rich foods (such as cereals or meats) when they’re around 6 months old.
 If your baby gets a mix of breast milk and iron-fortified formula, talk to your doctor about whether your little one needs a supplement. After they start on solids, some babies still need iron supplements if they don’t eat enough iron-rich foods. You doctor can tell you if your baby is getting enough iron.
If your baby gets a mix of breast milk and iron-fortified formula, talk to your doctor about whether your little one needs a supplement. After they start on solids, some babies still need iron supplements if they don’t eat enough iron-rich foods. You doctor can tell you if your baby is getting enough iron. - Fluoride. Babies younger than 6 months do not need a fluoride supplement. After your baby is 6 months old, you can start supplementing with fluoride if your water supply lacks fluoride. Well water, bottled water, tap water in some communities, and ready-to-feed formulas do not have fluoride.
It’s important to find out if your water supply has fluoride in it. You can ask your doctor, dentist, or local water utility agency if the water in your community is fluoridated. Giving a child too much fluoride can cause white marks on the teeth, so there is no need to give a fluoride supplement if your child gets enough fluoride from water.
When Should I Introduce Solid Foods?
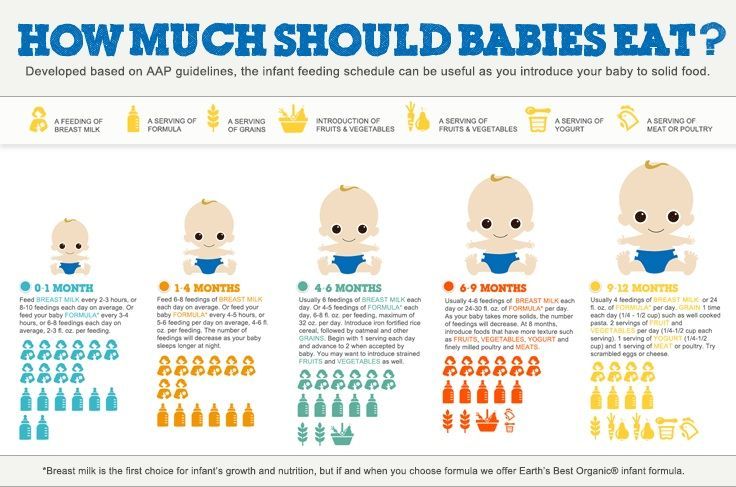
The best time to introduce solid foods is when your baby has the skills needed to eat, usually between 4 and 6 months of age.![]() This is when your baby:
This is when your baby:
- has good head and neck control
- can sit up
- has lost the tongue-thrust reflex (which causes babies to push food out of the mouth)
- has the motor skills needed to transfer food to the back of the mouth to swallow
- shows an interest in food (by watching others eat, reaching for food, or opening the mouth as food approaches)
By this age, babies usually weigh twice their birth weight, or close to it.
Wait until your baby is at least 4 months old and shows these signs of readiness before starting solids. Many babies exclusively breastfeed until 6 months of age, which is perfectly healthy.
Babies who start solid foods before 4 months are at a higher risk for obesity and other problems later on. They also aren't coordinated enough to safely swallow solid foods and may choke on the food or inhale it into their lungs.
How Should I Start Solids?
When the time is right, start with a single-grain, iron-fortified baby cereal. Rice cereal has traditionally been the first food for babies, but you can start with any you prefer. Start with 1 or 2 tablespoons of cereal mixed with breast milk, formula, or water. Never add cereal to a baby's bottle unless your doctor recommends it.
Rice cereal has traditionally been the first food for babies, but you can start with any you prefer. Start with 1 or 2 tablespoons of cereal mixed with breast milk, formula, or water. Never add cereal to a baby's bottle unless your doctor recommends it.
Another good first option is an iron-rich puréed meat. Feed your baby with a small baby spoon.
At this stage, solids should be fed after a nursing session, not before. That way, your baby fills up on breast milk, which should be your baby's main source of nutrition until age 1.
When your baby gets the hang of eating the first food, introduce others, such as puréed fruits, vegetables, beans, lentils, or yogurt. Wait a few days between introducing new foods to make sure your baby doesn't have an allergic reaction.
Experts recommend introducing common food allergens to babies when they're 4–6 months old. This includes babies with a family history of food allergies. In the past, they thought that babies should not get such foods (like eggs, peanuts, and fish) until after the first birthday.![]() But recent studies suggest that waiting that long could make a baby more likely to develop food allergies.
But recent studies suggest that waiting that long could make a baby more likely to develop food allergies.
Offer these foods to your baby as soon as your little one starts eating solids. Make sure they're served in forms that your baby can easily swallow. You can try a small amount of peanut butter mixed into fruit purée or yogurt, for example, or soft scrambled eggs.
When Can I Give My Baby Water?
In their first few months, babies usually don't need extra water. Breast milk and formula supply all the fluids that your baby needs. On very hot days, most babies do well with extra feedings.
When your baby starts eating solid foods, you can offer a few ounces of water between feedings, but don't force it.
What About Juice?
Fruit juices are not recommended for babies. Juice offers no health benefits, even to older children. Juice can fill them up (leaving little room for more nutritious foods), promote obesity, cause diarrhea, and even put a baby at risk for cavities when teeth start coming in.![]()
Supplemental feedings for the breastfed baby
With good instruction and support, most moms can breastfeed their babies exclusively for the first six months (and continue breastfeeding beyond). Unfortunately, many U.S. newborns are still fed something other than their own mother’s milk during their initial hospital stay. These supplemental, or supplementary, feedings are typically artificial infant formula, but they may be donor human milk or glucose water. Because unnecessary supplementation in the hospital has been associated with less exclusive breastfeeding, as well as a shorter duration of any breastfeeding, the Academy of Breastfeeding Medicine (ABM) has issued guidance on when otherwise healthy babies need supplementation or not.
When supplementation may not be necessary
The ABM encourages parents and health care providers to adopt a preventive approach to supplementation with:
- prenatal education
- in-hospital breastfeeding support
- breastfeeding immediately after birth
- skin-to-skin care after birth
- rooming-in
- instruction on milk expression (if necessary, such as when the mother and her infant must be separated)
In some cases, concern about a baby’s weight loss is identified as a reason for supplemental feedings. All babies do lose weight after birth. While this can be scary to new parents, it doesn’t necessarily mean that their baby isn’t feeding well; many factors influence the baby’s birth weight and weight changes, including gestational age, the method of birth (vaginal or cesarean), and the amount of fluid the mother received during labor. As long as the infant is “feeding well, urinating and stooling adequately,” and has weight loss “in the expected range” while “bilirubin levels are not of concern,” the ABM recommends adopting a watch and wait approach.
All babies do lose weight after birth. While this can be scary to new parents, it doesn’t necessarily mean that their baby isn’t feeding well; many factors influence the baby’s birth weight and weight changes, including gestational age, the method of birth (vaginal or cesarean), and the amount of fluid the mother received during labor. As long as the infant is “feeding well, urinating and stooling adequately,” and has weight loss “in the expected range” while “bilirubin levels are not of concern,” the ABM recommends adopting a watch and wait approach.
During this time, parents can focus on:
- recognizing early feeding cues
- keeping the baby safely skin-to-skin with the awake mother
- gently awakening the baby for frequent feedings
- hand expression of drops of colostrum to be fed to the baby
Parents, with the support of health care providers, should also pay attention to the baby’s feeding behavior, including the latch, positioning, and signs of discomfort. They should also look for signs of maternal fatigue, which can interfere with breastfeeding.
They should also look for signs of maternal fatigue, which can interfere with breastfeeding.
When supplementation may be necessary
There are situations in which supplementation may be necessary, even for an infant who is born full-term and seems healthy. The ABM identifies the following reasons for supplemental feeding of the infant during the hospital stay after birth:
- hypoglycemia that has been documented by lab test and is unresponsive to frequent breastfeeding; dextrose gel or intravenous (IV) glucose can be given, and breastfeeding should continue
- inadequate milk intake, as shown by significant dehydration, weight loss outside of normal range (with other factors), delayed or persistent meconium bowel movements (black, tarry stools)
- hyperbilirubinemia, sometimes with ongoing weight loss, few bowel movements, and uric acid crystals with urine; breastfeeding should continue during evaluation
- metabolic conditions of the newborn, requiring special supplements
- delayed maternal milk supply
- insufficient maternal mammary glands (estimated to affect less than 5 percent of women)
- past breast surgery affecting milk production
- medical cause, such as chemotherapy or other medication, or separation of mother and infant
- intolerable and unrelieved pain during breastfeeding
What supplement to give
Most parents find that even if they must, temporarily, give a supplement to their breastfed baby, breastfeeding can continue. The ABM ranks possible supplements in order of preference:
The ABM ranks possible supplements in order of preference:
- Mother’s own milk, gathered by hand expression or pump; use breast massage and/or warm compresses to help with letdown and consider pumping one breast while the baby breastfeeds on the opposite breast to increase milk yield.
- Donor human milk, which is preferable to artificial supplements.
- Protein hydrolysate formula, to avoid exposure to cow’s milk protein while conveying that supplementation is temporary.
- Other artificial formula, such as cow’s milk-based or soy-based formula, as determined appropriate for the baby’s age, amount needed, and potential effect on breastfeeding.
Note that glucose water is not considered an appropriate supplement, since it doesn’t provide nutrition or reduce bilirubin, and it poses a risk of hyponatremia or “water intoxication,” due to an imbalance of water and sodium in the body.
How to give a supplement
No single device has been shown to be better for all babies, and some babies may respond better to one feeding method than another. Mothers who are breastfeeding in addition to supplementing may wish to avoid bottles until 4-6 weeks after birth, since artificial nipples require different sucking patterns and can interfere with a baby’s ability to breastfeed (nipple confusion).
Mothers who are breastfeeding in addition to supplementing may wish to avoid bottles until 4-6 weeks after birth, since artificial nipples require different sucking patterns and can interfere with a baby’s ability to breastfeed (nipple confusion).
In addition to bottles, there are many options parents can use to provide supplemental feedings to their breastfed infants including:
- supplemental feeding devices (Lact-Aid or Supplemental Nursing System)
- cup
- spoon
- dropper
- syringe
When selecting how you will administer your baby’s supplemental feeding, the ABM encourages parents and health care providers to consider the following:
- cost and availability
- ease of use and cleaning (cup-feeding is preferable when hygiene is a concern)
- long-term or short-term use
- stress to the infant
- how much supplement can be fed in 20-30 minutes
- mother’s or caregiver’s preference
- expertise of health care provider
- effect on baby’s breastfeeding skills
- effect on mother’s milk supply (supplemental nursing devices provide breast stimulation, as well as skin-to-skin contact)
In most cases, supplementation is given temporarily to help you and your baby overcome a difficulty and to get back on track with breastfeeding.![]() While your baby is receiving supplements, be sure to take steps to maintain and, if necessary, increase your milk supply.
While your baby is receiving supplements, be sure to take steps to maintain and, if necessary, increase your milk supply.
WHO | Supplementary feeding
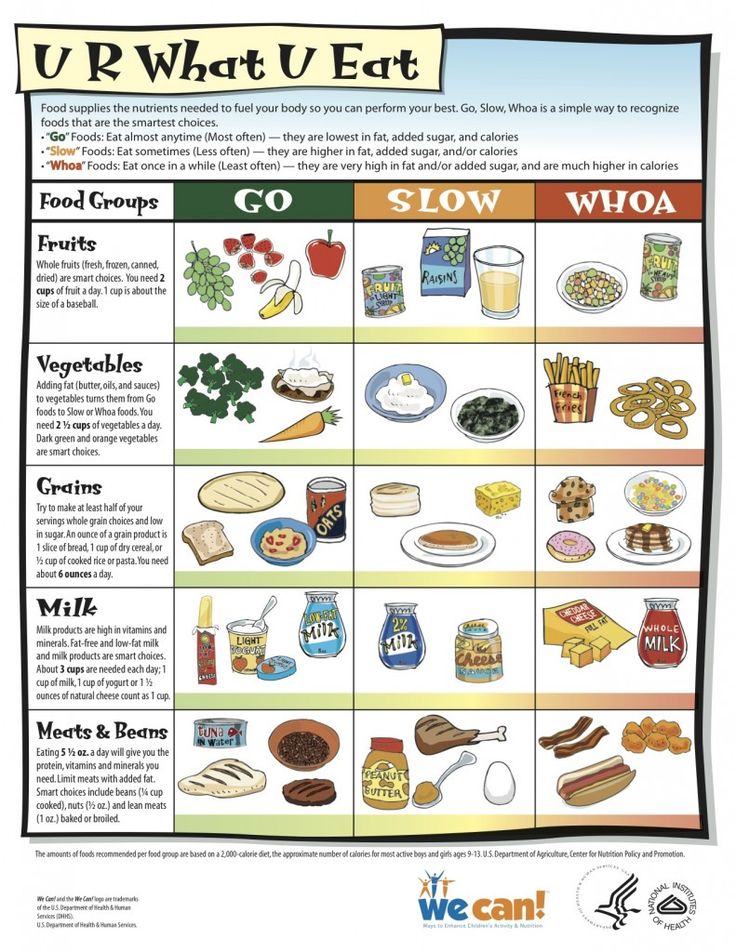
In cases where breast milk is no longer sufficient to meet the nutritional needs of the infant, supplementary food should be included in the child's diet. The transition from exclusive breastfeeding to food consumed in the family, which is called supplementary feeding, usually occurs between 6 and 18-24 months of age, which is a very vulnerable stage. This is when the onset of malnutrition in many infants is a significant factor in the high prevalence of malnutrition among children under five years of age worldwide. WHO estimates that 2 out of 25 children in low-income countries are stunted.
WHO/J. Muriel
Complementary feeding should be timely, which means that all infants should begin to receive nutrition in addition to breast milk from 6 months. It must be adequate, which means that complementary foods should be given in the quantity, frequency, sequence, and variety of foods to meet the nutritional needs of the growing baby while breastfeeding continues. Food should be prepared and served in a safe manner, that is, care should be taken to minimize the risk of pathogen contamination. And they should be fed in an appropriate way, which means that their texture should be appropriate for the age of the child and that flexible feeding is applied, following the principles of psycho-social care.
Food should be prepared and served in a safe manner, that is, care should be taken to minimize the risk of pathogen contamination. And they should be fed in an appropriate way, which means that their texture should be appropriate for the age of the child and that flexible feeding is applied, following the principles of psycho-social care.
The adequacy of complementary foods (adequacy is a shorthand for timely, adequate, safe and appropriate) depends not only on the availability of a variety of foods in the family, but also on the feeding methods used by caregivers. Feeding young children requires active care and stimulation, where the caregiver responds to the child's signals of hunger and encourages the child to eat. Such feeding is also referred to as active or flexible feeding.
WHO recommends that infants be given complementary foods from 6 months in addition to breast milk, initially 2-3 times a day at 6-8 months of age, increasing to 3-4 times a day at 9-11 months, and at 12-24 months additionally include 1-2 times a day additional nutritious food, if desired.
Inappropriate feeding practices are often a more important determinant of inadequate food intake than family food availability. WHO has developed a protocol for tailoring feeding recommendations to allow program managers to find out local feeding practices, common feeding problems and suitable complementary foods. The protocol builds on existing information and suggests that improved feeding recommendations be tested in families. WHO recommends using this protocol to develop interventions to improve complementary nutrition and include it in the process of adapting the Integrated Management of Childhood Illness strategy.
Research has shown that caregivers need skilled support to feed their infants properly. Guidelines on appropriate feeding are included in the Early Childhood Feeding Advisory, Guidelines and First-Level Health Workers Training Course on Integrated Management of Childhood Illness. WHO has produced a guide, Supplementary Feeding: Family Table Food for Breastfed Children, which provides more detailed guidance for health care workers on how to support supplementary feeding.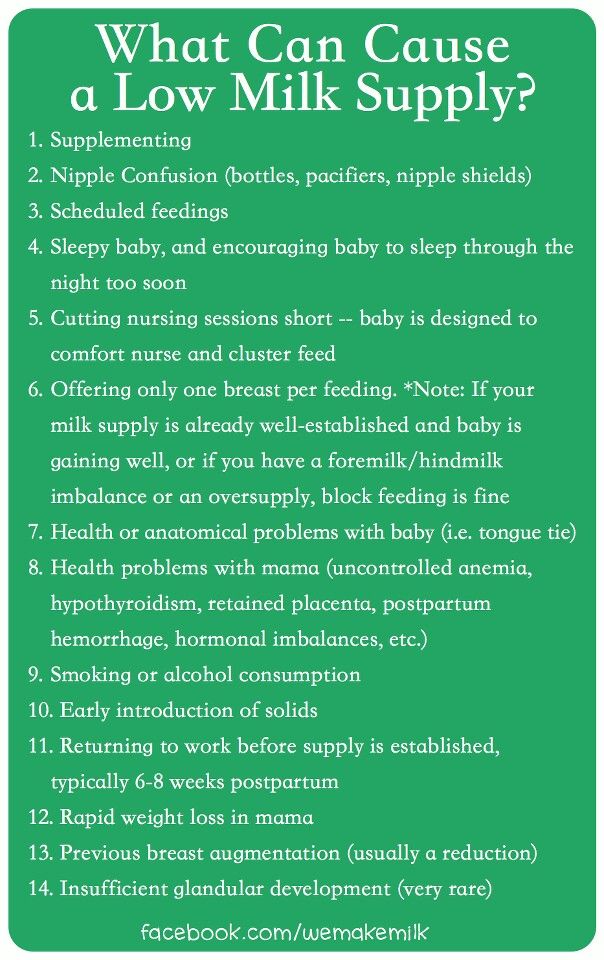
The WHO Global Consultation on Supplementary Feeding, 10-13 December 2001, resulted in updated recommendations on good feeding practices and guidance for program managers on their implementation. Background material prepared for these consultations is published in the Special Supplement to Food and Nutrition Bulletin 24(1) 2003 and supplements the WHO/UNICEF publication Supplementary Feeding of Young Children in Developing Countries: A Review of Current Scientific Knowledge, 1998, WHO/NUT/98.1. The Pan American Health Organization Guidelines on Complementary Feeding for Breastfed Children (2003) summarize the current scientific evidence on supplementary feeding and are intended to guide policy and programmatic action at the global, national and local levels, and The Guidelines for Feeding Non-Breastfeeding Children 6-24 Months of Age (2005) provide guidance on feeding children who are not breastfed.
Based on new knowledge, WHO, in collaboration with partners, has developed updated indicators for infant and young child feeding, including supplementary feeding. As a result, three publications have been produced: definitions, measurement and country profiles.
As a result, three publications have been produced: definitions, measurement and country profiles.
Publications
- Feeding newborns and young children: publications
Related links
- Promoting adequate feeding for infants and young children
- Exclusive breastfeeding
- Global Strategy for Infant and Young Child Nutrition
- World Health Organization recommendations for infant nutrition
What to feed children from 6 months. Complementary foods or complementary foods - ROCROS
When your baby is 4 months old, your baby should be introduced to complementary foods or complementary foods.
Complementary foods are all products (except mother's milk and mixtures) required for the development of the child's body, supplementing the baby's diet with nutrients.
The need to add new products arises in connection with the growing nutritional needs of the baby and to compensate for the difference between them and the beneficial substances contained in breast milk.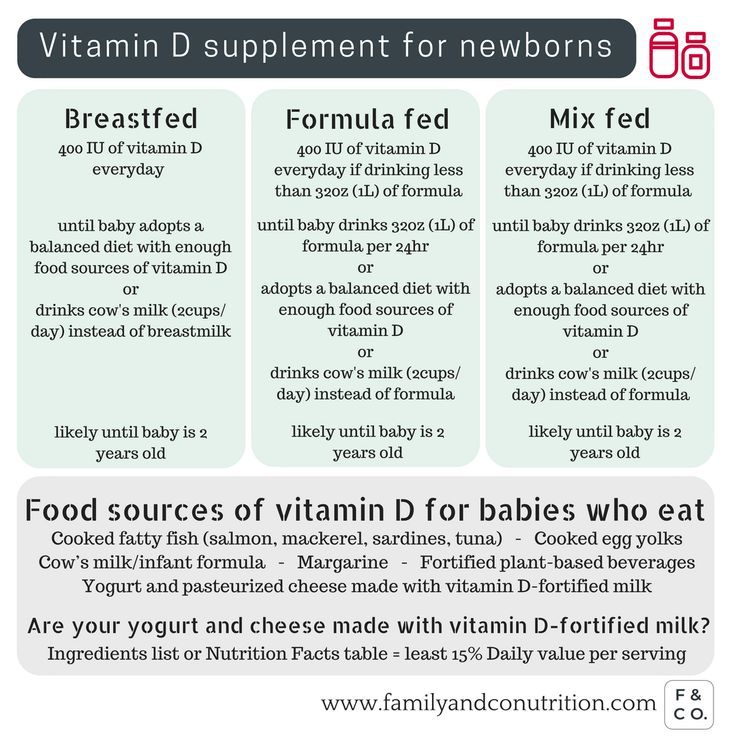
According to the "National program for optimizing the feeding of children in the first year of life in the Russian Federation", the minimum age at which the first complementary foods are added is 4 months. Until this age, the baby's body is not prepared for the absorption of food products that differ from women's milk and infant formula.
On the other hand, late introduction of complementary foods (after 6 months) can cause severe micronutrient deficiencies (such as iron, zinc, etc.) and other delayed consequences of improperly organized nutrition of the child.
Given the above reasons, complementary foods should be started at 4-6 months on an individual basis for each baby.
Why should I introduce additional food or complementary foods?
Complementary foods
- This is an additional source (other than breast milk or formula):
- Vegetable and animal proteins
- Carbohydrates
- Vegetable and animal fats
- Microelements
- Vitamins
- Dietary fiber
- the increase in calorie expenditure should be equal to their increase.
- Promotes the proper development of the digestive system in accordance with the age of the child (for example, enzyme apparatus, activation of the motor activity of the intestines of the baby).
- Promotes the functioning of the chewing apparatus (first thick and then dense food is consumed, biting and chewing skills are developed, which prepare for independent eating).
- Teaches to a healthy diet (correct taste habits are formed due to the use of various healthy foods with new tastes and aromas in the diet).
What is important to remember when introducing complementary foods?
- Adding the first meals of complementary foods to the baby's menu takes place within 5-7 days. The introduction of each product should be carried out gradually, starting with a small amount (1/2 tsp), and gradually increase it to the required volume.
- When a new dish is added to the menu, the baby must be healthy.
- Do not add complementary foods in hot weather and during vaccination.
- Complementary foods should be given before lunch in order to track a possible reaction to it.
- To reduce the possibility of developing an allergic reaction, one should start with one-component puree and dairy-free cereals.
- The first meal of complementary foods should be vegetable puree or porridge.
- Do not introduce more than one new dish at a time. The transition to new types of food is possible only after the baby gets used to the previous complementary foods.
- If there are symptoms of poor tolerance of the product (impaired bowel function, allergies, etc.), stop giving it and re-introduce it later. If the negative reaction repeats, you should abandon this product and change it to a similar one (for example, we change applesauce to pear, buckwheat porridge to rice, etc.).
- It is recommended to introduce commercially produced complementary foods first.
- To maintain lactation, complementary foods should be given to the baby before breastfeeding (or formula) using a spoon.
What complementary foods are available?
• Complementary grain (porridge) is the main source of carbohydrates, vegetable proteins and fats, dietary fiber, iron, selenium, vitamins B1, B2, PP, etc. The introduction of grain complementary foods should begin with gluten-free cereals (rice, buckwheat , later corn). Porridges are on milk and without milk. Dairy-free cereals are bred using breast milk or infant formula, which is fed to the baby. Later, you can use cereals from a mixture of cereals, from the second year of life - cereals containing gluten (oatmeal, barley, wheat, semolina) and cereals consisting of mixtures of cereals.
• Vegetable puree is a source of organic acids, potassium, iron and dietary fiber, including pectins. A special group of vegetables (which includes carrots, pumpkin, spinach, etc.) contains β-carotene. When introducing vegetable supplements, it is important to remember that it should include one type of vegetable that is dominated by tender fiber, such as zucchini or cauliflower, and then gradually move to mixtures of vegetables, slowly expanding the range to include potatoes, pumpkin and carrots.
• Cottage cheese and egg yolk are valuable sources of animal proteins and fats, minerals (calcium), and B2 vitamins.
Dairy products for children
• Meat - contains complete animal protein. In beef, lean pork, rabbit meat, chicken, chicken, turkey and horse meat, protein is about 20–21%. Meat also contains heme iron, magnesium, zinc, and B vitamins. Meat puree is introduced into the children's menu no earlier than 6 months.
• Fish is a valuable source of proteins and fats, polyunsaturated fatty acids. Fish purees are introduced into the children's menu from 8–9 months, with precautions, taking into account the individual reaction of the baby. Puree with fish is usually given to the baby 1-2 times a week, alternating with mashed meat.
• Juices are an excellent source of natural sugars (glucose, fructose, sucrose), organic acids (malic, citric, etc.), which have a positive effect on the digestive process and the absorption of other nutrients.