Baby too tired for last feed
Breastfeeding a Sleepy Baby - Breastfeeding Support
Newborn babies feed a lot and sleep a lot. But what if a baby seems to sleep all the time or keeps falling asleep as soon as they start breastfeeding? Can a baby be too sleepy? This article looks at newborn sleep, how often babies need breast milk and how to feed a sleepy baby. It is a companion article to How Often Should a Newborn Feed?
Search Articles
Need to look something up?
How long do newborn babies sleep?
Newborn babies sleep a lot, they may sleep for 18 hours out of every 24—usually for two to three hours at a time1 with perhaps one longer sleep of four to five hours2 . It is common for a baby to be particularly sleepy in the first 24 hours after birth 3.
How often should a newborn feed?
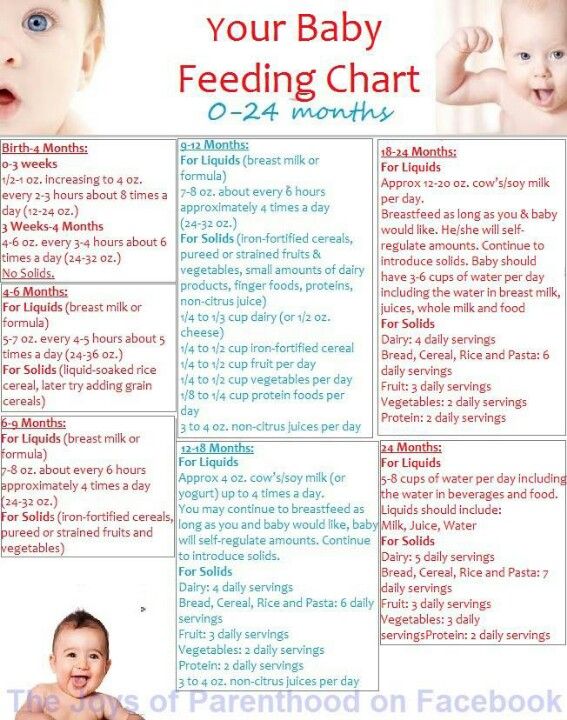
A breastfed baby generally feeds every two to three hours or more around the clock because breast milk is quickly digested and they only have small amounts at a time. For much more information see How Often Should a Newborn Feed? The excerpt below explains:
Excerpt from
How Often Should a Newborn Feed? Breastfeeding Support, 2019
Newborn babies sleep a lot, they may sleep for 18 hours out of every 24—usually for two to three hours at a timeBreast milk is easily and quickly digested—even as quickly as one hour—and babies have tiny tummies so they need to feed little and often. It is usually recommended that a baby has at least 8-12 feeds in 24 hours i.e. that they breastfeed every two to three hours from the start of one feed to the start of the next and this ties in with a newborn’s sleep patterns. Some babies may feed more frequently e.g. every hour at first.
How long should a newborn sleep without feeding?
How long a baby should sleep in one go will usually depend on how much milk they are getting at the breast during a breastfeed. How much milk a baby can get will depend on how much milk a breast can store (breast storage capacity), the latch (the way a baby attaches to the breast) and how many total feeds the baby has during any given 24 hour period. Feeding in clusters with occasional longer periods of sleep is normal especially when there are at least 8-12 feeds over a 24 hour period. If a baby is waking for lots of frequent feeds and feeding actively with plenty of swallows of milk and plenty of wet and dirty nappies and gaining weight, they can usually be left to sleep and feed on demand to their own timetable. If not, then reminding and encouraging a sleepy baby to breastfeed every two to three hours during the day and every four hours at night can be important to avoid them being underfed.
How much milk a baby can get will depend on how much milk a breast can store (breast storage capacity), the latch (the way a baby attaches to the breast) and how many total feeds the baby has during any given 24 hour period. Feeding in clusters with occasional longer periods of sleep is normal especially when there are at least 8-12 feeds over a 24 hour period. If a baby is waking for lots of frequent feeds and feeding actively with plenty of swallows of milk and plenty of wet and dirty nappies and gaining weight, they can usually be left to sleep and feed on demand to their own timetable. If not, then reminding and encouraging a sleepy baby to breastfeed every two to three hours during the day and every four hours at night can be important to avoid them being underfed.
Can babies be too sleepy?
Yes, sometimes babies can be too sleepy and if they are not getting enough milk because they are so sleepy or not feeding very well they can begin to sleep even more and feed even less. A baby who is not feeding frequently or not feeding well may become more and more difficult to rouse. If a baby is very sleepy, they could be at risk of higher than normal weight loss or poor weight gain, higher than normal levels of jaundice and a sleepy baby is a big risk factor for low milk supply because removing milk from the breasts regularly is an important signal to make more milk. If a baby continues to be sleepy and not feed well after a mother’s milk comes in, there is a higher risk of the mother’s breasts getting engorged or getting mastitis. Mastitis or engorgement can make a mother feel very poorly and reduce a milk supply further.
A baby who is not feeding frequently or not feeding well may become more and more difficult to rouse. If a baby is very sleepy, they could be at risk of higher than normal weight loss or poor weight gain, higher than normal levels of jaundice and a sleepy baby is a big risk factor for low milk supply because removing milk from the breasts regularly is an important signal to make more milk. If a baby continues to be sleepy and not feed well after a mother’s milk comes in, there is a higher risk of the mother’s breasts getting engorged or getting mastitis. Mastitis or engorgement can make a mother feel very poorly and reduce a milk supply further.
Encourage a sleepy baby to feed
Encouraging a sleepy baby to have regular breastfeeds and helping them to stay awake long enough to finish a feed will both protect the mother’s milk supply and keep baby well fed to protect their health (see below).
Why might a baby be too sleepy?
Reasons for being particularly sleepy might include:
- A difficult birth or birth interventions such as ventouse, forceps or if a mother has received any pain relieving drugs that have affected baby.
- Prematurity, health issues or other medical reasons can make a baby sleepy.
- Breastfeeding problems. If a baby is not getting enough milk they will have less energy and this can quickly make them more sleepy. Sometimes a baby may seem to be breastfeeding but actually they are sleeping with the breast in their mouth and not swallowing anything or very little.
- Jaundice (yellowing of the skin due to a build up of bilirubin) can make a baby sleepy and is more likely in a baby who is not getting enough milk creating a vicious cycle.
- Overstimulation. If a baby is overstimulated by excessive handling by strangers or even family members, bright lights or constant loud noise they might tend to shut down and go to sleep to escape.
- Missed feeding cues. When a baby is swaddled 4, has a pacifier, is too warm or is not in close contact with his mother there is a higher chance of missing feeding cues so that a baby sleeps for longer and feeds less.
- Severe breast engorgement. Severe breast engorgement after the birth may hinder baby getting milk and any unrelieved engorgement will tend to reduce a milk supply. If less milk is available a baby may become sleepier. Conversely, if a baby is already very sleepy and not feeding well there is a higher chance that a mother may experience painful engorgement (swollen breasts full of milk) leading to a vicious cycle of sleepy baby getting less milk, breasts reducing supply due to the engorgement, less milk for baby and so on. See our articles on Engorged Breasts and Engorgement Relief When Milk Won’t Flow for more information to deal with engorgement.
How can I wake my sleepy baby to feed?
If your baby is not waking at least 8-12 times in 24 hours he may need reminding when to feed. Ideas to wake and feed a sleepy baby include:
Ideas to wake and feed a sleepy baby include:
- Look for light sleep and feeding cues. A baby can breastfeed in light sleep and it’s easier to latch or wake a baby in light sleep i.e. when his eyes are moving under his closed eyelids (rapid eye movement or REM) and he is starting to move, fidget or fuss in his sleep. Other feeding cues include a baby sucking his fists or fingers, opening his mouth and turning his head from side to side to search for the breast (rooting). It can be helpful to cluster feed in these light sleep/more active periods.
- Hold your baby. Sometimes just picking up and holding your baby in a breastfeeding position will motivate him to begin rooting and latch on (attach to the breast). Holding your baby as much as possible allows you to spot those moments when your baby is in light sleep and try to latch him on.
- Skin-to-skin. Remove your baby’s clothes so that he is skin-to-skin or lightly dressed against his mother’s chest.
 Being held in skin-to-skin contact in a tummy down position against a mother’s chest is a great position to trigger a baby’s feeding reflexes. In this position, babies will often start actively searching for the breast using their hands and mouth even if they are not fully awake. Skin-to-skin contact can therefore encourage more breastfeeds5. The mother’s body will keep baby warm, a blanket can be draped over mother and baby as needed. See Why Skin to Skin? for more explanation of how helpful this technique can be used at any time in the early weeks not just after the birth. Remember to remove any scratch mittens.
Being held in skin-to-skin contact in a tummy down position against a mother’s chest is a great position to trigger a baby’s feeding reflexes. In this position, babies will often start actively searching for the breast using their hands and mouth even if they are not fully awake. Skin-to-skin contact can therefore encourage more breastfeeds5. The mother’s body will keep baby warm, a blanket can be draped over mother and baby as needed. See Why Skin to Skin? for more explanation of how helpful this technique can be used at any time in the early weeks not just after the birth. Remember to remove any scratch mittens. - Change baby’s nappy. Changing a baby’s nappy will often rouse them. Some parents combine this with gentle massage of hands and feet.
- Different positions. Try holding your baby in different breastfeeding positions to see if any help him to stay awake.
 Some babies may be more wakeful in a rugby hold or in an upright position such as a straddle hold compared with a traditional cradle hold. Some may be more active in reclining positions while some may fall into a deep sleep. You can see the different positions to try in Breastfeeding Positions for Newborns.
Some babies may be more wakeful in a rugby hold or in an upright position such as a straddle hold compared with a traditional cradle hold. Some may be more active in reclining positions while some may fall into a deep sleep. You can see the different positions to try in Breastfeeding Positions for Newborns. - Dimming the lights. Bright lights can make a baby want to shut their eyes which encourages sleep, try soft lighting instead.
- Quiet time. Try to create a peaceful atmosphere so baby does not get overstimulated. Passing a baby around family members and constant loud noise can cause some babies to “withdraw” and go to sleep to escape.
- Avoid a dummy. A dummy can encourage a baby to sleep longer. Sucking releases hormones to pacify or calm baby back to sleep and can therefore lead to missed feeding opportunities. See Pacifier, Dummy or Soother, Yes or No?
How do I keep my baby awake during feedings?
Getting baby latched and drinking well at the start of a feed is not always the end of the story. Once the initial let-down subsides, a sleepy baby is quite likely to fall asleep again before he has finished the feed. The following ideas can help your sleepy baby to feed effectively:
Once the initial let-down subsides, a sleepy baby is quite likely to fall asleep again before he has finished the feed. The following ideas can help your sleepy baby to feed effectively:
Skin-to-skin. Undressing your baby and placing them skin-to-skin on your chest maximises their feeding reflexes and helps stimulate feeding cues.
Position and latch. If your baby is not latched and positioned well it will be difficult for them to get milk (and breastfeeding may hurt!). Check positioning in Breastfeeding Positions for Newborns and see Latching Tips and Why Does Breastfeeding Hurt? Try different positions, upright positions may help your baby stay awake to breastfeed longer.
Breast compressions. Putting gentle pressure on the breast with a free hand while baby suckles can help to keep milk flowing at a faster pace and so keep a baby feeding longer. See What is Breast Compression?
Keep switching sides. As soon as sucking slows on the first breast offer the other breast before baby falls asleep. By switching and repeating you can help to keep baby awake and feeding actively for longer.
By switching and repeating you can help to keep baby awake and feeding actively for longer.
Look for active feeding. Watch your baby carefully. Is he actively moving his jaw to suck and can you hear swallowing or see the pause in his suck as he swallows? Watch for the baby who is frequently flutter sucking or comfort nursing but not swallowing anything. If your baby isn’t getting enough milk he will probably fall asleep hungry and your milk supply will continue to drop.
Express and top up if needed. If baby is still falling asleep before he has had enough to eat, pumping and topping him up with expressed breast milk will help his energy levels for feeding longer at the next feed. The more breast milk your baby gets the sooner he will be more wakeful and better able to breastfeed effectively. And pumping will protect your supply, only by frequent emptying of the breasts will they know to make more milk.
Get support. Mothers across the world have traditionally taken several weeks to nest with their newborn baby and get breastfeeding established. Finding support with preparing meals or looking after older children can be invaluable. Your sleepy baby will benefit from your focussed attention to get breastfeeding established. And if your otherwise healthy baby continues to be sleepy or is not feeding very well seek the help of a breastfeeding specialist e.g. an IBCLC lactation consultant.
Finding support with preparing meals or looking after older children can be invaluable. Your sleepy baby will benefit from your focussed attention to get breastfeeding established. And if your otherwise healthy baby continues to be sleepy or is not feeding very well seek the help of a breastfeeding specialist e.g. an IBCLC lactation consultant.
How can I tell if my baby is feeding well?
Our sister article How Often Should a Newborn Feed? explains:
Excerpt from
How Often Should a Newborn Feed? Breastfeeding Support, 2019
When a baby is feeding actively, even if they look like they are asleep, the baby’s jaw will move as they suck and they will swallow regularly e.g. in a pattern of one or two sucks per swallow for 10-15 minutes or more at a time from one or both breasts. The length of time a baby is attached to the breast is not as important as how effectively that baby is feeding. Even if a baby is latched on for an hour, if he isn’t feeding actively with plenty of swallows of milk he might not be getting enough milk.
It is important to be aware that just being attached to the breast and making mouth movements alone doesn’t guarantee that a baby is drinking well. Although a baby can feed well in their sleep sometimes, other times they can be dreaming about sucking but not swallowing, sometimes for hours at a time. It’s helpful to be able to tell the difference between active feeding and flutter sucking and comfort nursing. The way the baby is attached to the breast is important too—see Latching Tips.
Even if a baby is latched on for an hour, if she isn’t feeding actively with swallows of milk she might not be getting enough milkIs my baby getting enough milk?
There are lots of ways to determine whether a baby is getting enough breast milk without seeing the volume that has been drunk e.g. looking for active feeding, plenty of dirty nappies and weighing baby regularly. See Is My Baby Getting Enough Milk? and Breastfed Baby Poop for more reading. How Often Should a Newborn Feed? has a guide to the volumes of breast milk a newborn baby might need at each feed.
What if my baby is too sleepy to breastfeed?
If, despite trying the ideas above, your baby is still not waking up to breastfeed, or is latching but not actively getting enough milk, supplements of expressed breast milk will keep them well fed. Topping your baby up every two to three hours will give him more energy to wake up to breastfeed at the next feed. A baby is much more likely to be able to breastfeed effectively if they are gaining weight. Expressing your milk as often as baby ought to be feeding (at least eight times a day) will stimulate the breasts to make more milk and provide the perfect supplement for your baby. If you can’t express any breast milk to keep your baby well fed, and if donor milk is not available, your baby may need infant formula until you can get more help with your milk supply.
- Check in with your health professional if your baby is consistently too sleepy to breastfeed to make sure they are not poorly or getting dehydrated.
- Hand expressing or pumping your milk will protect your milk supply and provide a breast milk supplement to keep your baby fed until they can breastfeed. See Hand Expressing, How to Increase Milk Supply When Pumping and How Long Does Breast Milk Last?
- Supplementing a sleepy baby. A sleepy baby can be given small amounts of expressed breast milk (or formula if needed) by teaspoon, syringe or bottle. If your baby is alert and awake but not ready to latch on, another option is to offer a cup feed. Although a bottle teat could introduce a bottle preference or teat confusion it can be helpful for a very sleepy baby who needs larger volumes. Following the ideas in Tips to Bottle Feed your Breastfed Baby and Best Bottle for a Breastfed Baby can help minimise any problems.
 If a baby is too sleepy to breastfeed properly a supplemental nursing system is probably not going to be helpful at this stage as it relies on a baby sucking actively.
If a baby is too sleepy to breastfeed properly a supplemental nursing system is probably not going to be helpful at this stage as it relies on a baby sucking actively. - Check in with a breastfeeding specialist for tailored suggestions to help your baby breastfeed well and maximise your milk supply.
Poor weight gain
A sleepy baby who is not feeding well is at risk of not gaining enough weight or losing weight. This situation can be prevented or quickly reversed by expressing your milk to both protect your milk supply and to keep your baby well fed until you can get more urgent help with breastfeeding. With more milk inside him, your baby will have more energy to stay awake and breastfeed. See Baby Not Gaining Weight, Supplementing an Underweight Baby and How Often Should a Newborn Feed? for much more information.
Try different positions, upright positions may help your baby stay awake to breastfeed longerBabies do sleep a lot but they will normally wake every two to three hours to feed. If a baby is not waking to breastfeed and is constantly sleeping longer than two to three hours, reminding them to breastfeed can both keep your baby well fed and healthy and also protect your milk supply. Hand expressing or pumping your breast milk to provide a supplement for a sleepy baby may sometimes be needed for a while. There is no advantage to keep weighing a sleepy baby every few days and watching their weight stay the same (or go down) hoping it will pick up eventually. Getting help with breastfeeding as soon as possible will be much more effective in protecting your milk supply and getting breastfeeding on track.
If a baby is not waking to breastfeed and is constantly sleeping longer than two to three hours, reminding them to breastfeed can both keep your baby well fed and healthy and also protect your milk supply. Hand expressing or pumping your breast milk to provide a supplement for a sleepy baby may sometimes be needed for a while. There is no advantage to keep weighing a sleepy baby every few days and watching their weight stay the same (or go down) hoping it will pick up eventually. Getting help with breastfeeding as soon as possible will be much more effective in protecting your milk supply and getting breastfeeding on track.
Footnotes & References
-
Normal Sleep Development, Baby Sleep Info Source (BASIS), 2019
-
Mohrbacher, Breastfeeding Answers Made Simple, 2010 p 86
-
ABM Clinical Protocol #5: Peripartum Breastfeeding Management for the Healthy Mother and Infant at Term, ABM Revision 2013
-
Franco et al, Influence of swaddling on sleep and arousal characteristics of healthy infants.
 Pediatrics, 2005
Pediatrics, 2005 -
ABM Clinical Protocol #3: Supplementary Feedings in the Healthy Term Breastfed Neonate, Revised 2017
Sleepy Baby – Why And What To Do
Nobody likes to disturb a sleeping baby, but sometimes a baby can be too sleepy for their own good. At times like this they may need you to take action.
Your newborn baby needs to nurse actively for one or both breast at each feed. Offer the second breast after they seem to have finished at the first, although they may not want both sides at every feed.
What makes a baby sleepy?
Recovering from birth: In the first few days, some babies are sleepy or uninterested in feeding. It’s especially true for small babies, after a difficult labour or birth, or if you received drugs for pain relief during labour.
Jaundice or an infection may make a baby sleepy. Newborn jaundice is normal but frequent breastfeeding helps prevent it becoming a problem.
Not enough milk: Your baby may sleep to conserve energy if they are not getting enough food. They may also sleep longer that is good for them if they are apart from you.
Is my baby too sleepy?
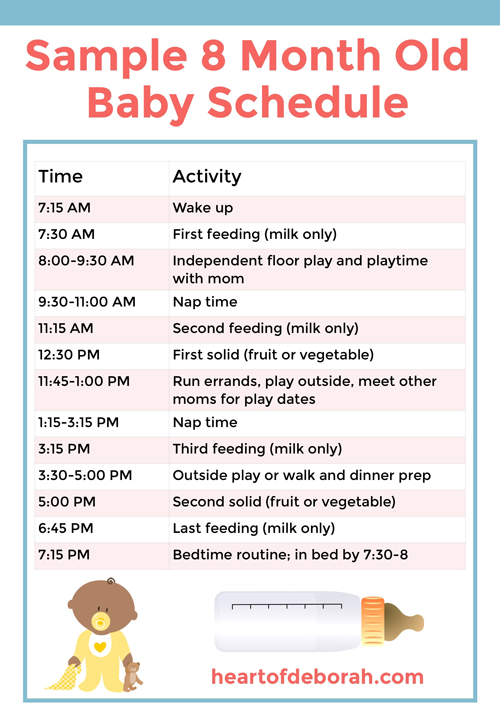
To gain weight and stimulate your milk production, expect your newborn to:
- Breastfeed effectively at least 8–12 times in 24 hours
- Feed actively from one or both breasts at each feed, swallowing regularly.
- Nurse at least every 2–3 hours from the start of one feed to the next, with one longer sleep of 4–5 hours.
- Have periods where they breastfeed on and off for several hours, usually in the evening.
- Gain weight from day 4 and regain birth weight by about two weeks.
Look at our page Beginning Breastfeeding for more information. If your baby is too sleepy to do all these things they may need your active help to ensure they are nursing effectively and getting enough milk.
Is my baby getting enough milk?
A baby may lose up to 7% of their birth weight during the first few days. From around day 3-4, expect them to start gaining, and to regain their birth weight by 10-14 days. Many breastfed babies gain around 200-235g (7-8oz) as week for the first 2-3 months. If you baby consistently gains less, or they haven’t regained their birthweight by 14 days, seek skilled help to assess whether they are getting enough milk. What comes out is a sign of what has gone in, so counting dirty nappies can be a useful guide between weighing sessions. For more information to help you know if your baby is getting enough milk in the first few days, you could read our article here about signs of effective feeding in the early days. And then after the first few days, this article will help you decide if your baby is getting enough milk.
From around day 3-4, expect them to start gaining, and to regain their birth weight by 10-14 days. Many breastfed babies gain around 200-235g (7-8oz) as week for the first 2-3 months. If you baby consistently gains less, or they haven’t regained their birthweight by 14 days, seek skilled help to assess whether they are getting enough milk. What comes out is a sign of what has gone in, so counting dirty nappies can be a useful guide between weighing sessions. For more information to help you know if your baby is getting enough milk in the first few days, you could read our article here about signs of effective feeding in the early days. And then after the first few days, this article will help you decide if your baby is getting enough milk.
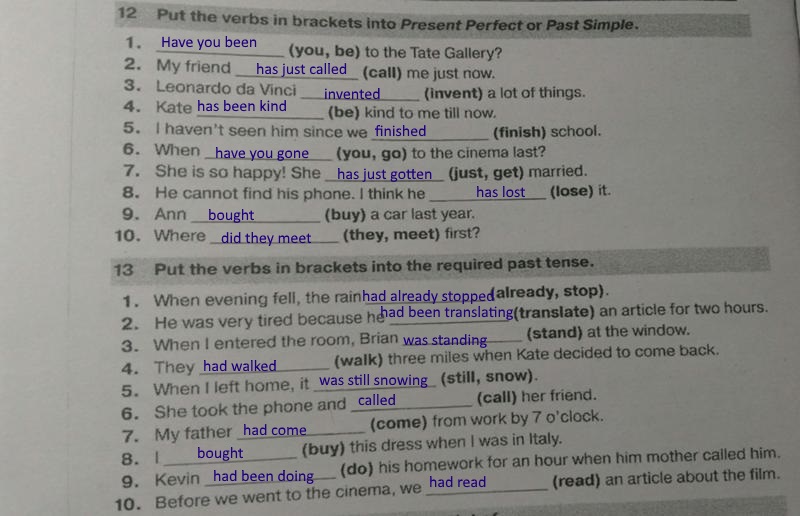
| Age | Dirty nappies per 24 hours |
|---|---|
| 1-2 Day | 1 or 2 greenish-black tarry meconium poos |
| 3-5 days | At least 3 green transitional poos |
| 5+ days | At least 3-5 yellow, loose unformed poos the size of a 2p coin or larger |
Remind your baby to nurse
If your baby is too sleepy or groggy to rouse themselves every few hours, you will need to wake them to feed to ensure they get enough milk. This will be easier if your baby is in a light sleep cycle: watch for rapid eye movements under their closed eyelids, arm and leg movements, sucking activity and changes in their facial expression.
This will be easier if your baby is in a light sleep cycle: watch for rapid eye movements under their closed eyelids, arm and leg movements, sucking activity and changes in their facial expression.
- Aim for your baby to feed at least 10 times in 24 hours, including at least once at night
- Encourage active nursing on the first breast, watching and listening for signs of swallowing.
- Use breast compression (see below) to keep your baby nursing actively.
- Offer the other side in the same way. You can switch back and forth several times if it helps your baby stay awake and feed.
- Encourage cluster nursing whenever your baby is more alert.
- Give expressed milk if they aren’t feeding well.
- Keep them close by—day and night—so they don’t sleep too long and you don’t miss their feeding cues.
Also try
- Dimming the lights and keeping your surroundings quiet and peaceful.
- Keeping the room temperature at around 18°C or undressing your baby a little if the room is warm.
 Being too hot can make a baby sleepy.
Being too hot can make a baby sleepy. - Unwrapping any blankets.
Newborn feeding cues
Signs of interest in feeding include:
- Mouth movements; smacking or licking his lips
- Sucking on lips, tongue, hands, fingers, toes, toys or clothing
- Rooting, head bobbing or nuzzling against whoever is holding them
- Fidgting and squirming a lot
- Fussing
- Crying – a late sign of hunger.
Do offer feed generously. A newborn won’t find it easy to feed well, if they have to wait and reached late hunger signs.
Helping your sleepy baby
Positioning and attachment
Getting a deep, comfortable latch is crucial. If your baby is not latched on well at the breast, they will have to work harder to get your milk. They may tire easily and fall asleep. Sometimes just a small adjustment to the way your baby comes to the breast can make a huge difference. An LLL Leader can provide individual suggestions tailored to your circumstances. If your breasts are engorged, gently hand express a little milk and/or ease swelling back with your fingertips to make it easier for your baby to latch on deeply and prevent you getting sore. See our longer article about Positioning and Attachment for more help on how to help your baby latch well, feed effectively and be comfortable for you.
If your breasts are engorged, gently hand express a little milk and/or ease swelling back with your fingertips to make it easier for your baby to latch on deeply and prevent you getting sore. See our longer article about Positioning and Attachment for more help on how to help your baby latch well, feed effectively and be comfortable for you.
Copyright Suzanne Tobin
Seek skilled help early on if you are finding breastfeeding difficult or uncomfortable.
Laid back breastfeeding
Try letting your baby lie on your body with their chest and tummy against you as you recline at about 45 degrees. If they can snuggle up close to your chest for periods of time, even when sleepy or during light sleep, they will often instinctively seek the breast and attach deeply and comfotably even during light sleep. This can be done skin-to-skin or with you and your baby lightly clothed. Watch for signs your baby is stirring and gently encourage feeding.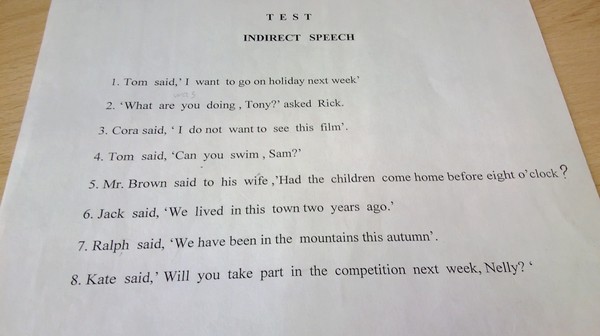 Spending time relaxing like this can make a real difference to how well your baby feeds and how much milk you make. Our page on Comfortable Breastfeeding has more ideas.
Spending time relaxing like this can make a real difference to how well your baby feeds and how much milk you make. Our page on Comfortable Breastfeeding has more ideas.
Breast compression
If your baby starts to doze at the breast, this technique will help him breastfeed actively and take more milk.
- Cup your breast with your hand, near your chest wall, thumb opposite fingers in a C shape. Keep your hand well back from the nipple area.
- Wait while your baby breastfeeds actively, with their jaw moving all the way to his ear. When they stop swallowing, compress your breast firmly. They probably start swallowing again. Hold it squeezed until they stop nursing actively, then release your hand.
- Rotate your hand around your breast and repeat step 2 on different areas of the breast as needed. Go gently—this should not hurt.
Try switching breasts at least two or three times during each feed—when your baby comes off the first breast on their own or when breast compression no longer keeps them breastfeeding actively.
Express milk for your baby
Until your baby gets the hang of feeding you may need to do some work for your baby. If they aren’t latching at all, or is not feeding well and gaining weight, then expressing your milk will help establish milk production. The earlier you start, the sooner you’ll produce plenty of milk. Hand expression is often easiest at first but when your milk comes in combining hand expression with pumping can be most effective.
Giving expressed milk
First, encourage your baby to nurse at both breasts. Watch for swallowing and use breast compression an switch nursing until they stop drinking and start to doze.
Next, give your baby expressed milk until they have had enough. (For more on how to give additional milk, our article here). Giving your baby your expressed milk after breastfeeding can help them overcome sleepiness and feed more effectively next time.
Then, once your baby has settled, express from both breasts switching back and forth and using compressions and hand expression to get the available milk. Store this milk in the fridge ready for the next feed.
Store this milk in the fridge ready for the next feed.
Aim to complete this process within about an hour.
Avoid bottles and dummies
You can give small amounts of expressed milk using a spoon, flexible feeding cup or syringe. If you decid to use bottles for larger amounts, you can give the bottle in a way that helps protect breastfeeding. For more information on ways to give your baby milk and bottles see our article on Bottles and other tools. An alternative is to use a nursing supplement: this acts like a straw to deliver extra milk through a tube along your breast as your baby nurses, avoiding the need for bottles. Our article Nursing Supplementers explains more.
Don’t give up too soon
If your baby doesn’t respond quickly to your efforts to get him to breastfeed more often and more effectively, don’t give up. Keep your baby fed, Keep your supply protected and Keep your baby close. You may find our article on Getting breastfeeding back on track after a tricky start helpful. Check with your doctor to eliminate any medical reasons and contact your local LLL Leader to find one-to-one breastfeeding help. You can find support and encouragement from breastfeeding mothers in your local LLL Group too.
Check with your doctor to eliminate any medical reasons and contact your local LLL Leader to find one-to-one breastfeeding help. You can find support and encouragement from breastfeeding mothers in your local LLL Group too.
Written by mothers of LLLGB. Photos courtesy of Ellen Mateer and Suzanne Tobin.
Further Reading
Comfortable Breastfeeding
Positioning and attachment
Engorged Breasts – Avoiding & Treating
Hand Expression of Breastmilk
Is my baby getting enough milk?
My Baby Needs More Milk
Nursing supplementers
Jaundice in Healthy Newborns
Getting back on track after a tricky start – the Three Keeps
My baby won’t breastfeed
Bottles and other tools
Other websites
Biological Nurturing™: www.biologicalnurturing.com/video/bn3clip.html
Natural Breastfeeding Position video, Nancy Mohrbacher:
Benefits of skin-to-skin contact: www.kangaroomothercare.com
Books
The Womanly Art Of Breastfeeding. LLLI, London: Pinter & Martin, 2010
LLLI, London: Pinter & Martin, 2010
This information is available to buy in printed form from our shop.
Copyright LLLGB 2020
Updated June 2022
When it's time to stop breastfeeding :: City polyclinic № 12
There are a lot of opinions on this matter: the time when it's time to wean a child from the breast varies from several months to infinity from the point of view of self-weaning supporters. But this issue has always been considered from the point of view of benefit to the baby. And what does medicine say about what terms of involution will be useful not for a child, but for a woman?
What is lactation involution? nine0006
Involution of lactation (from Latin involutio - coagulation) is a physiological process that completes the period of breastfeeding. This biological mechanism starts on the 40th day from the moment the baby was last attached to the breast. Since the onset of involution, the mammary glands decrease in size and stop producing breast milk. Usually, the process of involution is recommended to be carried out gradually so that the child can adapt to a new way of getting food, and also learn to calm down without being attached to the mother's breast. nine0003
Usually, the process of involution is recommended to be carried out gradually so that the child can adapt to a new way of getting food, and also learn to calm down without being attached to the mother's breast. nine0003
Under normal conditions, each mammary gland will continue to lactate as long as milk is removed from it - and this phenomenon, the same for animals and humans, is used in agriculture. As the volume of milk production decreases, its composition changes: the content of fat, immunoglobulins increases, and the level of lactose decreases. If lactation is not stopped forcibly, it can continue until the baby is weaned from the breast; under natural conditions, this usually occurs in 2 - 2.5 years. nine0003
The process starts when the pituitary gland stops producing enough of the hormone prolactin. Milk production continues for some time after the cessation of its suction. As they write in the materials of the WHO, “if in most mammals “drying” occurs on the 5th day after the last feeding, then the period of involution in women lasts an average of 40 days. During this period, it is relatively easy to restore full lactation if the child resumes frequent sucking.
During this period, it is relatively easy to restore full lactation if the child resumes frequent sucking.
Thus, as soon as attachments to the breast become rare and short, the process of involution begins. This can happen at any time - it is known that sometimes children themselves refuse breastfeeding for a variety of reasons that need to be discussed separately. There is an inhibition of protein synthesis and structural changes in the mammary gland - the reverse replacement of the glandular tissue with adipose tissue begins, which allows the breasts to return to their previous size and shape.
Signs of lactation involution
If involution occurs naturally, it usually begins when the child is two years old. At this time, the frequency of attachment naturally decreases: the child has other interests, including interest in "adult" food. How can a nursing mother understand that involution has begun?
The breasts shrink slightly and do not fill with milk even if you do not feed for more than 12-24 hours. That is why if at this time the child stops breastfeeding, this does not cause any frustration and suffering from excess milk in the mother. Milk, in terms of composition, properties and appearance, is increasingly reminiscent of colostrum. nine0003
That is why if at this time the child stops breastfeeding, this does not cause any frustration and suffering from excess milk in the mother. Milk, in terms of composition, properties and appearance, is increasingly reminiscent of colostrum. nine0003
The baby's sucking activity is markedly increased. This is due to the fact that milk production is reduced, and the child is still trying to suck out the same amount of portion. A child for one feeding can be applied to one breast, then to the other - and so on several times. The period of such sucking activity can last up to several months.
Mother's psychological readiness for weaning. This is a very important sign that should not be ignored. As soon as a nursing mother is tired of breastfeeding, this is a sign that the process is either incorrectly regulated, or, if there have been no problems with lactation so far, it is coming to an end. nine0003
Psychological readiness of the child for weaning. Usually, by the age of two, the child is socialized, ceases to experience an urgent need for tactile contact with the mother, and begins to receive the necessary nutrients from other sources. The psychological need for the child gradually disappears
The psychological need for the child gradually disappears
Forced involution
If there is a need to wean the child prematurely, then you need to be prepared for the following consequences:
- pain and discomfort in the mammary glands of varying intensity;
- formation of indurations in the region of the mammary glands;
- fever;
- deterioration in general condition;
- purulent-inflammatory complications (breast abscess and mastitis).
If the need to interrupt lactation is associated with medical indications, then it is necessary to carry out involution under the supervision of a physician. What needs to be done first? Reduce the number of feedings by offering the baby a different food source. In addition, strict control of fluid intake with its restriction is necessary, and additional pumping may be required in order to avoid stagnation of milk. nine0003
If you are tired of breastfeeding
The psychological state of a breastfeeding mother is a very important criterion that must be paid close attention to. Lactation is a very energy- and resource-intensive project for the female body, and it is not surprising that exhaustion sets in sooner or later. Some nursing mothers can wait for natural involution without any problems, but for many there comes a point when, due to fatigue, continuing to feed is impossible. Unfortunately, this objective situation (the amount of forces and resources is strictly individual) often causes a feeling of guilt in a nursing mother, since the advertising of the need for breastfeeding before self-weaning has reached its maximum in recent years. What needs to be assessed at this moment? On one side of the scale, there is a benefit for the child, and on the other, the psychological and physical comfort of the mother. nine0003
Lactation is a very energy- and resource-intensive project for the female body, and it is not surprising that exhaustion sets in sooner or later. Some nursing mothers can wait for natural involution without any problems, but for many there comes a point when, due to fatigue, continuing to feed is impossible. Unfortunately, this objective situation (the amount of forces and resources is strictly individual) often causes a feeling of guilt in a nursing mother, since the advertising of the need for breastfeeding before self-weaning has reached its maximum in recent years. What needs to be assessed at this moment? On one side of the scale, there is a benefit for the child, and on the other, the psychological and physical comfort of the mother. nine0003
Many will choose the comfort of their mother in such a situation, and they will be right. How long breastfeeding will continue is up to her to decide, since only she can assess the degree of her exhaustion. After all, there are now excellent breast milk substitutes, and a calm and rested mother is an irreplaceable resource that cannot be replaced by anything.
Many experts say that breastfeeding up to a year and a half may be optimal. Thus, the well-known pediatrician Dr. Komarovsky recommends starting breastfeeding correction starting at the age of one: at this age it is already time to introduce calming rituals that replace breastfeeding, and also gradually reduce the number of daily feedings. WHO recommendations to breastfeed children for more than two years, according to Komarovsky, are due to high infant mortality rates in Asia and Africa, where a child's life often directly depends on how long his mother breastfeeds. As soon as breastfeeding ends in countries with objective water scarcity and with a high prevalence of intestinal infections, the life of the child is in danger, so prolonged breastfeeding in such countries saves children's lives. nine0003
For European countries, the situation with high child mortality is not relevant. Therefore, in our realities, it is necessary to make a decision on the involution of breastfeeding based on the needs of the child and the condition of the mother.
source: Medportal
08/21/2017 | Admin | View 52350 | Comm. x | Category: Our news
31.Mar.2021
Regurgitation is the reflux of small amounts of gastric contents or gastric juice mixed with saliva up the esophagus. Regurgitation often occurs in infants and in the vast majority of cases is a variant of the physiological norm. nine0003
The younger the child, the more often regurgitation can be observed. As the child grows, they gradually disappear until they disappear completely. In the first month, regurgitation occurs in 85% of children, this indicator does not depend on the type of feeding (formula or breast milk) and on the method of administration (bottle or natural feeding). After 3 months, regurgitation is much less common, and by one year it disappears completely.
In the new issue of " Doctor's Advice of the Day" , the local pediatrician of DPO No. 3 Shayakhmetova Yazgul Fayzrakhmanovna will give parents practical advice on topical and frequent questions about the features of feeding the baby and due to what factors the involuntary process of regurgitation occurs. nine0003
nine0003
Causes and mechanism of regurgitation
• Filling the stomach with air that the child can swallow while eating. This is the most common cause, which practically does not require special correction.
• Muscular weakness of the valve between the esophagus and stomach. It develops with the growth of the child and begins to function normally by the first year of life. Therefore, food can pass from the stomach into the esophagus without hindrance, which happens during regurgitation. nine0087 • Food allergy (or food intolerance). Most often, it is manifested by skin reactions, but in rare cases, regurgitation can be a symptom.
• Congenital defects of the gastrointestinal tract. The digestive system is quite complex, some violations in its structure can lead to digestive problems that will begin to appear immediately after birth. Thus, narrowing in the area of the gastrointestinal junction can lead to frequent atypical regurgitation. nine0003
Regurgitation and vomiting
Regurgitation is in most cases a physiological phenomenon that does not require special treatment and observation. But it can be similar to vomiting, being a sign of dangerous diseases, in which case a doctor's consultation is necessary. Regurgitation and vomiting are similar in their mechanism of occurrence, namely, the release of gastric contents into the oral cavity.
But it can be similar to vomiting, being a sign of dangerous diseases, in which case a doctor's consultation is necessary. Regurgitation and vomiting are similar in their mechanism of occurrence, namely, the release of gastric contents into the oral cavity.
It is important to distinguish between them, as vomiting in newborns is very dangerous and can lead to aspiration of the contents into the respiratory tract and respiratory arrest. nine0003
There are differences between regurgitation and vomiting:
• Regurgitation most often occurs after eating. Usually this is a single, non-recurring episode. The child spits up the food that he just ate, there are no foreign impurities in it.
• Vomiting usually recurs repeatedly. It may not be related to eating.
• Regurgitation does not affect the well-being and mood of the child - he is active, does not show signs of anxiety, smiles, plays. nine0087 • Vomiting is accompanied by a deterioration in general well-being. The child is lethargic or restless.
The child is lethargic or restless.
• Regurgitation usually occurs suddenly, vomiting is preceded by a decrease in activity and mood.
• Vomiting is rarely the only symptom - there are also other problems with the functioning of the digestive tract or fever. Vomiting in a child is a reason to see a doctor!
Tips for parents!
Let's figure out how to avoid the possible dangers associated with regurgitation. The main thing that responsible parents need to know is that most often children spit up in a prone position. This position is dangerous by aspiration (inhalation) of gastric contents. nine0087 Preventing aspiration is as simple as bringing the baby upright or turning it over on its side or stomach immediately after spitting up. Then the baby himself will be able to push the food out of his mouth.
It is worth remembering that it is unacceptable to leave a child with regurgitation syndrome without adult supervision, especially in the supine position.
Feeding rules
Frequent regurgitation can be prevented by following a few feeding rules.
• Keep your baby upright after feeding. Even if the baby is tired or wants to sleep, do not immediately put him down. Babies are very comfortable to hold on the shoulder. After waiting for the belching of air, the child can be given any position. nine0087 • The same should be done before feeding. The thing is that in an upright position, the child can release excess air from the stomach. If this is not done before eating, belching is guaranteed.
• There is a specific position recommended for breastfeeding. One of the main goals of the correct position of a nursing mother and baby is the prevention of regurgitation. The semi-upright position of the baby with the head raised above the level of the body must be maintained during each feeding. nine0087 • Feeding should be frequent but small. Overfeeding is fraught not only with regurgitation, but also with other digestive problems.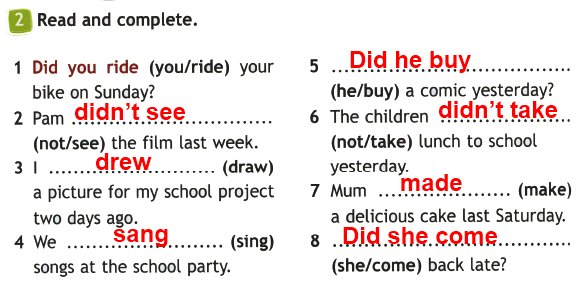
• It is important not to feed the baby when he is crying or laughing, otherwise he will swallow extra air.
• When feeding with a teat bottle, make sure that the opening of the teat is not too large and that the position of the bottle is such that the teat is always filled with formula and not with air. nine0087 • From active games you need to refrain from the first half hour after feeding.
Following these simple rules will help reduce the frequency of regurgitation.
Proper diet
If the above recommendations do not bring results, it is worth changing the diet. For a formula-fed baby, you can thicken each serving.
Breastfed babies may require additional treatment formulas.
There are also special mixtures against regurgitation. But they belong to therapeutic mixtures, which means that only a doctor can prescribe them. nine0003
Warning signs
Responsible parents should be aware of danger symptoms that require medical advice:
• The baby is very restless and often rolls over and arches its back when spitting up or feeding. Such a symptom may indicate chronic irritation of the esophagus.
Such a symptom may indicate chronic irritation of the esophagus.
• Regurgitation is frequent, plentiful, observed after each feeding.
• The child has signs of dehydration.
• Regurgitation, which first appeared after the first half of the year. nine0087 • Prolonged spitting up without improvement (same frequency and same amount of spitting up in a child aged 1 year and older).
• Regurgitation is accompanied by fever.
• The child is not gaining or even losing weight.
• You can't tell for yourself if the baby is spitting up or vomiting.
There are even more dangerous symptoms that require an ambulance call:
• The child stopped breathing after spitting up. nine0087 • A bluish tint appears on the lips and face.
• After spitting up, the child lost consciousness.
• Green or brown reflux (gastric contents) - this may be a sign of intestinal obstruction or stomach bleeding.
Aspiration is extremely dangerous in infants who are unable to get rid of food in the airways on their own.