Baby upset when feeding
My baby fusses or cries when breastfeeding
By Kelly Bonyata, BS, IBCLC
© Lsantilli - Fotolia.com
Some babies will fuss, cry or pull off the breast during breastfeeding. There are a number of reasons why this might be happening. It’s pretty common to see this type of behavior at around 6-8 weeks, though it can occur at any time. If your baby is generally fussy (not just when nursing) see My baby is fussy! Is something wrong?
Determining the problem
Here are some of the problem-solving steps I go through when my baby is fussy at the breast or a mother asks me why her baby is fussing while breastfeeding:
Now infants can get
all their vitamin D
from their mothers’ milk;
no drops needed with
our sponsor's
TheraNatal Lactation Complete
by THERALOGIX. Use PRC code “KELLY” for a special discount!
How old is baby? Most babies go through growth spurts during the first few days at home and around 7-10 days, 2-3 weeks, 4-6 weeks, 3 months, 4 months, 6 months, 9 months, etc. Many babies are fussy during growth spurts.
Is baby working on anything new developmentally? Babies who are starting to notice the world around them can be notoriously distractible. Any kind of new developmental step that baby is working on can affect nursing temporarily, whether it be fussy nursing behavior or simply more frequent nursing.
When is baby fussing? To figure out the cause it’s helpful to pay attention to when the fussy behavior happens, both during the nursing session and during the day.
If baby is fussy right when your milk is letting down (or immediately after), there’s a good chance that the fussy nursing is related to a fast let-down. If baby is fussy before let-down, or a few minutes into nursing (and a while after let-down), then baby may be impatient for the fast flow of milk that comes with let-down. Fussing at the end of a nursing session (or what seems to be the end) may mean that baby needs to burp, or is ready to finish nursing, or just wants to suck (and doesn’t want to deal with a new let-down at this point), or wants to continue nursing on the other side or with a faster flow of milk.
If the fussy behavior is mainly in the mornings, it might be due to a faster than usual let-down if baby has just had a longer sleep period and mom’s breasts are fuller than usual. If baby is fussier during evening nursings, it may be due to the normal fussy time that most babies have during the evening. Although most babies don’t react to foods that mom eats, some do. If you eat a particular food at about the same time each day (or most days) and baby has a regular time where she fusses during nursing, try not eating that food for a week or two to see if things improve.
Does fussing occur on both sides equally or only on one side? Most moms have a faster let-down and/or a more abundant milk supply on one side than the other, so if your baby fusses more on one side, it may be due to these differences.
What else is going on with baby? Is she sick or teething? Is something new or different going on in her environment? Has she started solids or is she trying a new food? Is she exhibiting other symptoms besides the fussy nursing?
Below are discussions of some of the different things that can lead to fussy nursing behavior. Keep in mind that the problem may also be a combination of several things.
Keep in mind that the problem may also be a combination of several things.
Does baby need to burp?
Many babies will cry, fuss, pull off the breast, etc. if they need to burp. Try to burp between breasts and after a feeding, but don’t worry if baby does not burp and is content. Breastfed babies overall don’t take in as much air during a feeding as bottle-fed babies do, so usually don’t need to burp as often. If baby has been crying before she nurses, or is so hungry that she nurses “frantically” or if mom has a fast let-down, baby could be taking in more air and may need to be burped more often.
Burping is usually only necessary during the first few months, though it may extend longer. Once your baby is moving more freely, she will be able to relieve the gastric gas herself. This usually will occur between the 4th and 6th month, but may be shorter in some children and longer in others.
If baby has a hard time burping, try burping more often during a feeding. The best burping position is one that applies firm pressure to the baby’s tummy. Placing baby over the shoulder way up so that there is pressure on baby’s abdomen often works well. Walking around while doing this might distract her long enough to get a good burp. You may even want to lie baby down on her stomach and burp her that way.
The best burping position is one that applies firm pressure to the baby’s tummy. Placing baby over the shoulder way up so that there is pressure on baby’s abdomen often works well. Walking around while doing this might distract her long enough to get a good burp. You may even want to lie baby down on her stomach and burp her that way.
Growth spurt
Babies often pull off and fuss during growth spurts. Most babies go through growth spurts, sometimes called frequency days, during the first few days at home and around 7-10 days, 2-3 weeks, 4-6 weeks, 3 months, 4 months, 6 months and 9 months (more or less). More growth spurt information in this link.
Distractible baby
If baby seems to be pulling off the breast at any distraction (real or imaginary), then see The Distractible Baby.
Forceful let-down
Some babies will pull off the breast soon after let-down if mom has a forceful let-down. Baby may be frustrated by the too-fast flow of milk with let-down. A too-forceful let-down can also cause excessive gas or spitting up/vomiting. There is more information here on symptoms of and how to deal with a fast let-down reflex.
A too-forceful let-down can also cause excessive gas or spitting up/vomiting. There is more information here on symptoms of and how to deal with a fast let-down reflex.
Slow let-down
Some babies get very impatient if mom has a slow let-down. There is more information here on speeding up a slow let-down reflex.
Baby wants a faster milk flow
Even very young babies can be quick to notice that pulling off, kneading the breast, etc. can cause an additional let-down, and can facilitate a faster, easier milk flow. Some babies become impatient with the slower milk flow following the initial fast flow at let-down. This may or may not be related to a slow let-down.
When a feeding begins at the breast there are drops of milk. Then when the initial let-down occurs (several seconds to a minute into the feeding), the milk flow speeds up quite a bit. At that time it may drip very quickly, squirt, or even spray. Some minutes later it slows again and the baby must continue to suck vigorously in order to elicit further let-downs. This pattern can continue through successive, multiple let-downs as long as the baby is continuing to nurse vigorously. Eventually, baby will learn that the flow will pick back up again if she’ll only continue to vigorously suck/swallow.
This pattern can continue through successive, multiple let-downs as long as the baby is continuing to nurse vigorously. Eventually, baby will learn that the flow will pick back up again if she’ll only continue to vigorously suck/swallow.
With bottle feeding, the flow is instant and continuous. The baby is required to work very little. Once a baby has had a bottle, especially a lot of bottles, she may begin to prefer the ease of bottle-feeding over the work of breastfeeding. She may become frustrated at the breast after the first let-down occurs and the flow of milk begins to slow.
If baby is getting bottles you might consider putting them away, at least for a while. When you must use a bottle, only use a newborn nipple for as long as baby will tolerate it so that she never gets a really fast flow of milk from the bottle, but has to work a little more to get the milk.
Sometimes babies of moms with oversupply or fast let-down will also get very used to the fast flow and object when it normally slows somewhere between 3 weeks to 3 months.
It can be helpful to do some breast compression when this fussiness starts or right before you expect it to. This will help speed up the milk flow again. Once compression stops helping, try switching baby to the other side when she begins to fuss and back and forth again (after using compression) as you need to.
Baby is done nursing for the moment
If baby is fussing after she’s been nursing for a while, and you’ve ruled out other causes, she may be in the process of changing her nursing pattern. Babies become very efficient at the breast with growth and maturity. They can milk the breast in a lot less time per feeding session than they required before. Baby’s frustration may just be a sign that she’s finished and wants to move on.
On a similar note, an occasional baby will just want to suck at the end of a nursing session and the flow of milk with let-down frustrates her. You might see if offering her a finger or pacifier (if baby is older than 4-6 weeks) to suck on during these times seems to help.
Baby prefers one side
Sometimes babies will refuse or fuss at a breast when the let-down is slower or too forceful, or the supply a bit lower. They in turn will prefer the side which lets down more/less quickly and in which the supply is more bountiful. See also: Lopsided! What can I do?
Fussy in the evening
Many young babies tend to pull off and fuss at the breast in the evening. See the article Cluster Feeding and Fussy Evenings.
Teething
Teething can cause fussy nursing behavior, as some babies experience gum discomfort with sucking. Baby might start to nurse, but then pull off and cry or fuss and not want to nurse anymore. See Teething for more information and tips.
Thrush
Frequent pulling off the breast can be a symptom of thrush.
Stuffy nose
A stuffy nose can cause fussy nursing behavior. If your baby has a stuffy nose and is having a hard time breathing and nursing at the same time, see colds & congestion.
Allergy or food sensitivity
Some babies with allergies or food sensitivities exhibit fussy nursing behavior. Often when there is a sensitivity to something in mom’s diet, baby will come to the breast hungry but when she tastes/smells something in the milk that will cause her GI distress, she pulls off, bats her head back and forth, etc. Sensitivities to foods in mom’s diet are rare. If this is the problem, you will most likely notice other symptoms, such as excessive spitting up or vomiting, colic, diarrhea, rash, persistent congestion or runny nose, or excessive gas. More information on food sensitivities in babies and links to more allergy information can be found in my article Dairy and other Food Sensitivities in Breastfed Babies.
Low milk supply
Low milk supply can cause baby to be fussy at the breast. If you feel that your milk supply may be low, see this page for more info: Increasing low milk supply.
Reflux
Reflux can result in baby being fussy at the breast. See Reflux and Breastfeeding for more information.
See Reflux and Breastfeeding for more information.
Tongue-Tie
Tongue-Tie can result in baby being fussy at the breast. See Breastfeeding a Baby with Tongue-Tie (Resources) for more information.
Baby Fusses or Cries During Feeding: Causes & Solutions
Is your baby fussy every time you offer the breast? Do they cry, making it hard to breastfeed?
I’ve been there and know how it can be distressing when your baby is irritable while breastfeeding. It can make you question whether you’re doing something wrong and why the experience isn’t turning out how you imagined.
To help set your mind at ease and offer you some hope, we’ll share everything we know about what makes a baby upset during breastfeeding.
We’ll help you determine the cause of your baby’s fussiness. We’ll also offer our solutions so your breastfeeding sessions can return to being a peaceful experience you both enjoy.
Causes of Baby Crying During Feeding
Half the battle is finding out why your baby is crying and fussing when they should be enjoying their time at the breast. You want to know your baby is getting enough milk and thriving. But it’s hard to be sure when they always latch on and off, crying in between.
You want to know your baby is getting enough milk and thriving. But it’s hard to be sure when they always latch on and off, crying in between.
Let’s discuss some possible causes.
1. Baby Isn’t Latching On
If your baby is fussing or crying, getting them to latch on to feed can be challenging. Whether overtired, overstimulated, or just plain hungry, a crying baby is unlikely to latch.
The Solution
Begin breastfeeding while your baby is calm and awake, before they get too hungry. Watch for early hunger cues such as rooting, smacking their lips, sucking their hands, sticking their tongue out, or waking from sleeping. Crying is a late sign of hunger.
Swaddling your baby and holding them close, dimming the lights, or moving somewhere peaceful and quiet might also help.
Another thing you can try is squeezing a few drops of milk onto your breast to entice your baby to latch on. The taste and smell of the milk might stimulate them to feed. Changing position or changing breasts can also work sometimes (1).
2. The Milk Flow Is Too Fast or Too Slow
Paying attention to when your baby starts to cry might shed some light on the reason.
If your baby is fussier in the morning, it could be that your overly full breasts release too much milk too quickly. Your breasts may have become engorged with milk during the night and your baby can’t cope with this forceful let-down.
Conversely, if they are fussier in the evenings, maybe the milk release is too slow and they get frustrated. They become impatient, waiting for the flow of milk that comes with the let-down, and start crying.
The Solution for Fast Milk Flow
A strong release of milk, or overactive let-down, can make your little one choke, gag, or cough when they’re feeding. They might unlatch from the breast because they don’t like or can’t cope with the fast flow. They could also be gulping a lot of air with the milk and getting gassy, which causes more upset.
They could also be gulping a lot of air with the milk and getting gassy, which causes more upset.
These are some of the things you can do to counteract this:
- Express before feeding: Pumping some of your milk before feeding, or expressing by hand, can help slow down the flow. After you feel the first let-down pass and you see the flow is slowing, put your baby to your breast.
- Lie back when nursing: Adopting a laid-back feeding position with your baby lying on top of you can slow the flow. You could latch your baby on and then lie back against some cushions or pillows. Milk will flow against gravity and won’t pour down your baby’s throat.
- Burp regularly: When your milk is flowing fast, your baby may gulp lots of air while feeding. A gassy baby is a fussy baby, so burp them regularly, during and after the feed.
- Feed one side at a time: Alternate your breasts at each feed. That way, once the flow slows down on the breast your baby is feeding on, they might stop fussing.

- Take a feeding break: If your flow is too much for your little one to cope with, remove them from the breast for a few seconds. Let the excess milk leak onto a towel, and offer the breast again when it stops. This might make your baby fussier for a while, but it will pay off in the long run.
The Solution for Slow Milk Flow
Your baby is hungry, but your milk is not coming quick enough. Just as we can get “hangry” when we need food or drink and aren’t getting it, our babies can too!
Luckily, we have some things you can try to combat a slow flow or delayed let-down:
- Stimulate the flow: Either pumping or hand expressing a little milk before latching can kick-start your let-down reflex. Once you have a steady flow, then you can put your baby to your breast.
- Warm compress: Use a warm towel or compress for a few minutes to stimulate letdown. Place it on your breasts just before each feed.

- Massage: Massaging your breasts before and during a feed can help the milk flow faster.
- Try breast compressions: If you notice your baby is about to start fussing and might unlatch, squeeze your breast. This will give your baby a burst of milk, keeping them actively feeding.
- Get comfortable: Breastfeeding a fussy baby can be frustrating for you as well. Try and feed in a relaxing position, away from distractions. It’s a perfect time to just concentrate on your baby.
- Make sure your baby gets enough milk: All that fussing and crying might make your little one tired, and they may fall asleep at the breast before they’ve eaten enough. Try and stimulate them to continue feeding by tickling their foot or stroking their cheek. The more your baby feeds, the more milk you will produce.
- Some dos and don’ts: When breastfeeding, avoid smoking and alcohol. Also, try and steer clear of soda and coffee.
 All these could affect your milk production. Ensure you eat a balanced diet and stay hydrated, too (2).
All these could affect your milk production. Ensure you eat a balanced diet and stay hydrated, too (2).
3. Baby Is Going Through a Growth Spurt
There are times during a baby’s first year of life when they go through growth spurts. Their weight and length will increase, as will their head circumference.
Your baby may want to feed more often during a growth spurt and can become fussy. It’s not uncommon for a baby to suddenly feed up to 18 times in 24 hours.
While one does not necessarily lead to the other, it makes sense that a growth spurt and sudden, frequent feeding go hand in hand. Your baby will need more milk to support the growth spurt, and nursing more will naturally boost your supply.
During this time, babies can also become fussier than usual. They might appear unsettled and clingy, and they may not sleep as well as usual.
Growth spurts generally happen several times during the first year. These are the ages when they are likely to occur:
- Two weeks old.
- Three weeks old.
- Six weeks old.
- Three months old.
- Six months old.
Not all babies will follow this timetable; some might have more growth spurts or they may be at different times. For some babies, there might be no change in their behavior when they have a growth spurt.
The Solution
During this time, follow your baby’s lead. Respond to their needs, whether it’s more feeds, extra cuddles, or just quiet time and a nap.
Your baby might get fussy if you aren’t producing as much milk as they want. It can take a day or so for your supply to catch up with the demand. The more you let your baby feed, the more milk your breasts will produce.
Your baby may seem hungry after normal feeding time, so don’t be afraid to nurse again. Keep yourself feeling good during this time by staying hydrated and eating balanced meals. Remember, you are not Superwoman; let family and friends help with chores and shopping while you spend time with your baby.
Remember, you are not Superwoman; let family and friends help with chores and shopping while you spend time with your baby.
4. Baby Is Going Through a Developmental Stage
Your baby is constantly developing mentally and learning new skills as they go along. It can be a bit overwhelming and confusing for them, and there might be weeks when they are fussier than usual. Sometimes called the “Wonder Weeks,” it can explain mood changes in your baby (3).
You might find that during these periods, your baby becomes more curious and distracted while feeding. They might want to feed more or, conversely, not stay latched on long enough for a good feed. They can be cranky and fussy and cry a lot when you’re trying to breastfeed.
The good news is that these periods generally only last a few days before your baby returns to normal behavioral patterns.
Not all babies will fit into the pattern of wonder weeks and develop at different times.
The Solution
Feed your baby in a quiet room where there are likely to be fewer distractions. There’s nothing worse than having a situation where your little one latches on, then hears their dad or sees the dog and stops feeding (or worse yet, turns their head with your nipple still in their mouth!).
There’s nothing worse than having a situation where your little one latches on, then hears their dad or sees the dog and stops feeding (or worse yet, turns their head with your nipple still in their mouth!).
Trying to get your baby to pay attention can make them fussier and be a constant battle.
You might also find that your baby is fussier and wants to feed more often during these periods. Again, take your cue from them, and give them the extra time and attention they need.
5. Baby Needs to Burp
Babies often fuss, cry, or pull away from the breast when they need to burp. A fast flow of milk can exacerbate this. They can also swallow more air when they’re fussy or gulp down milk faster than usual if they’re over-hungry.
The Solution
Breastfed babies tend not to need burping as often as bottle-fed ones. However, there are times when gas can make them uncomfortable and they need to get it out.
If your baby is fussing, stop the feed and try and burp them. If you let them carry on feeding while they’re crying, then they can take in more air and make the problem worse. Eventually, it can end up with them spitting up.
If you let them carry on feeding while they’re crying, then they can take in more air and make the problem worse. Eventually, it can end up with them spitting up.
It’s a good idea to burp your little one mid-feed, even if they don’t appear to be in too much discomfort. Try to do it when switching breasts or when your baby latches off the nipple.
Other Reasons for Crying During Breastfeeding
We’ve looked at some of the main reasons your baby might cry while breastfeeding. There are a few other things that can cause this, including:
- Baby prefers one side: Your milk supply might be better on one breast than the other. This may be apparent if your baby only fusses when fed on one side.
- Teething: This can be a painful and uncomfortable time for your baby, and they might fuss more when feeding. You might first realize it’s happening when they clamp down on your nipple and you feel the teeth through the gums. I’m all too familiar with that pain! But trust me, your baby isn’t trying to hurt you; they just want to relieve their pain (4).

- Baby has eaten enough: If your little one starts fussing toward the end of a feed, this might be a sign they’ve had enough. Try offering the breast again a few times. If they don’t want it, move on. If you have ruled out any other causes for their crying, their little tummy might be full.
- Baby wants to be pacified: Your little one might be full but still wants to suckle. However, it can be frustrating for them when milk is still flowing. This could be an excellent time to offer a pacifier for them to suckle.
- Thrush: This fungal infection can affect your nipples or a baby’s mouth. If your baby has oral thrush, feeding will be uncomfortable, and they can get fussy. If you suspect this, contact your health care provider (5).
- Baby has a cold: Trying to feed and breathe through a stuffy nose simultaneously can be challenging for a little one. They will become fussy and break away from the breast a lot.
 Use a nasal aspirator to try to clear their nose, or ask your pediatrician for advice.
Use a nasal aspirator to try to clear their nose, or ask your pediatrician for advice. - Food sensitivity or allergy: While you might enjoy eating spicy food for dinner, your baby may not. The flavor of the food you eat comes through in your milk, and your little one might not always like the taste or the smell. You might notice they are fussier when you have consumed certain foods they don’t like or are allergic to (6).
- Reflux: Although it’s not very common in breastfed babies, sometimes food comes back up from a baby’s stomach. This can make them cry and feel uncomfortable when feeding (7). Speak with your baby’s doctor if you suspect this is causing your baby to be fussy or cry during breastfeeding.
Feedback: Was This Article Helpful?
Thank You For Your Feedback!
Thank You For Your Feedback!
What Did You Like?
What Went Wrong?
Breastfeeding after 1 month: what to expect
Do you know when breast milk production stabilizes? And how does the frequency and duration of feedings change as the baby grows? You will find answers to these questions in our recommendations for breastfeeding after the first month.
Share this information
Congratulations: You made it through the first month of breastfeeding. Your breast milk has reached full maturity 1 , its production stabilizes, and it leaks almost or not at all from the chest. Don't worry, it's not getting less milk, it's just that your breasts are better able to produce and store it now. 2 At the age of six weeks, your baby will begin to please you with his charming toothless smiles, and by two months you will already have 500-600 feedings behind you. With a favorable development of events, problems with latch on by this point will already be resolved, and you can simply enjoy the convenience and benefits of breastfeeding.
When does breastfeeding decrease?
"Normal" feeding frequency for babies aged one to six months varies considerably, with some needing four feedings a day, others asking to be breastfed 13 times a day. 3
“From the age of one month, the amount of milk a baby consumes per feed increases, so that he can go without food for longer,” explains Cathy Garbin, a recognized international expert on breastfeeding, “A baby’s stomach grows, so he eat more at one time. In addition, mature milk allows him to stay full longer.”
In addition, mature milk allows him to stay full longer.”
Feeding can last from 12 minutes to one hour -
the habits of babies vary so much! 3 But if the child is gaining weight and falls within this range, there is no cause for concern.
What is most surprising, no matter how often the baby eats, he consumes approximately the same amount of milk per day - both at one month and at six, when it is time to start complementary foods with solid food. 4
“However, sometimes the baby eats more and sometimes less, especially when he is unwell. It’s better to just listen to his needs,” Katie explains.
Is breast milk enough for the first six months?
Yes. Breast milk contains everything a baby needs for the first 90,023 six months of life—exclusively breastfed babies don't even need to drink more water! 5 Until about six months of age, a child's digestive system is simply not adapted to the digestion of solid food, and he will be able to drink cow's milk only after a year.
In addition, breastfeeding during this period prepares the child for further development. It strengthens the muscles of the mouth, develops the jaw and helps straighten the teeth 6.7 . All this will come in handy when the baby begins to eat and talk. And because what you eat and drink affects how your breast milk tastes, your baby discovers new tastes even before he starts eating solid foods. 8
In addition, when your baby is sick, your body produces breast milk that is
rich in antibodies that help fight infection. 9 In other words, milk continues to protect the baby for many months as he grows and becomes more active.
Breastfeeding is also very comfortable once you get used to it. Claudia, a mother of two from the UK, notes: “No need to sterilize a mountain of bottles, prepare formula, carry it all with you, warm it up - in general, breastfeeding turned out to be very convenient, especially when my babies grew up and we began to leave the house more often. ".
".
At what age does a breastfed baby start sleeping through the night?
Waking up at night is normal for babies. Most babies between the ages of one and six months consume a fifth of their daily milk requirement at night, so nighttime feedings should not be neglected if you want your baby to get the required amount of calories. 3
"It really depends on what you mean by 'sleep through the night,'" says Cathy. "And it's better than waking up every two hours anyway! I have met infants who, starting at six weeks old, fell asleep at 19:00 and woke up at 7:00, but most continue to wake up frequently at night after this age. All children are different."
In Wales, a study of more than 700 infants showed that almost 80% of children aged 6 to 12 months wake up at least once a night, and 25% of them wake up three times or more. And it did not depend on what type of feeding the child is on - breastfeeding or artificial. 10
And if nighttime awakenings are unavoidable anyway, breastfeeding is at least comfortable! Maina, a mother of two from Australia, agrees: “You can even take a nap while feeding in the middle of the night - both the body and the baby do their job on autopilot. No need to plan, measure, sterilize anything - ready-made food at the right temperature is right in your chest. I think it's ideal."
No need to plan, measure, sterilize anything - ready-made food at the right temperature is right in your chest. I think it's ideal."
My child wakes up more often. Perhaps he is hungry?
Around four months of age, a baby's sleep patterns change as they develop deep and light sleep phases like an adult. Because of this, he may wake up more often at night. “At four months, sleep is more of a problem than feeding,” Cathy admits. “It can be exhausting, but try to adapt and be patient.”
Some call this " a four-month sleep regression ", but "progress" is more appropriate here. From the outside it may look like a step back, but in fact the child is approaching an important stage of development. He learns quickly, begins to become aware of the world around him, his perception is sharpened and, perhaps, there is anxiety about being separated from his mother. Crying when waking up and being able to eat milk cuddled up to mommy’s chest is a way for a baby to calm down.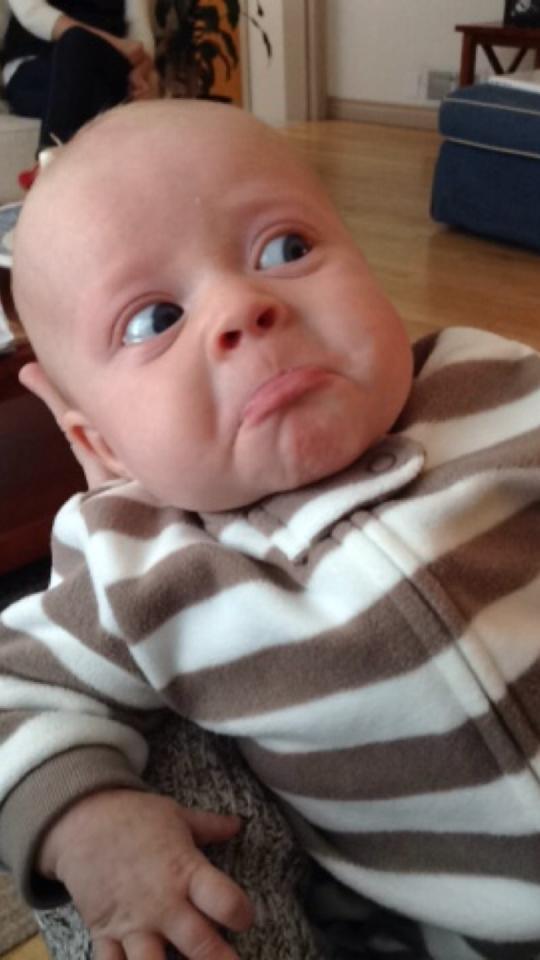 11–13
11–13
Resist the urge to “supplement” your baby with formula or start solid foods early
in an attempt to improve his sleep. Breast milk contains
hormones that make you sleepy and help you both relax
. Research shows that breastfeeding mothers actually sleep longer at night than mothers of formula-fed or mixed-fed babies
. 14
How does teething affect breastfeeding?
Teething usually begins around four months of age. When a baby has gum pain, he becomes restless, throws his chest and cries. All this, of course, is unpleasant.
However, breastfeeding can be an excellent sedative.
Studies have shown that babies who are breastfed
during the vaccination period cry less and forget pain more quickly. 15 Breastfeeding during teething can have the same calming effect.
An unpleasant side effect may be the child's attempts to try out his new teeth on the mother's breast. “Sometimes children flirt and bite their mother’s nipples. This can be felt in advance by how the behavior of the child changes when feeding: before biting, he removes his tongue, explains Cathy, “Usually this is not a problem and only happens a couple of times. It is enough to stop feeding, affectionately say that biting is not good, and the baby will soon leave this fun.
This can be felt in advance by how the behavior of the child changes when feeding: before biting, he removes his tongue, explains Cathy, “Usually this is not a problem and only happens a couple of times. It is enough to stop feeding, affectionately say that biting is not good, and the baby will soon leave this fun.
How to continue feeding if you have to be separated from the baby?
It happens that during the first six months, when the baby is still fully breastfed, the mother needs to be away for several hours - or even longer if she has to go to work or go away on business for a couple of days.
But this does not mean that you should stop breastfeeding. You can still feed your baby healthy breast milk - just express it and have someone give it to your baby when you're away. Here's Katie's advice:
“Start expressing milk a couple of days in advance, in small batches, 40-60 ml at a time. So you will have the necessary supply for the time of your absence, but at the same time the amount of milk produced will remain the same.
If you have to return to work, check with your employer about your daily schedule. Many mothers breastfeed their babies in the morning, evening and night, and pump milk at lunchtime to relieve discomfort and create a reserve for the next day.
This usually turns out to be much easier than one might think, and today many companies are well placed to do this, notes Cathy. “Breast pumps make it easy to solve this problem.”
Natalie, mother from the USA, shares her experience: “I feed Dylan as soon as he wakes up, and sometimes again before leaving for work, in order to maintain milk production and not lose contact with the child. At work, I pump twice the next day (in my absence, he eats two bottles of breast milk), and after work I rush home for the evening feed. I don't pump on the weekends - we resume regular breastfeeding."
Can breastfeeding continue after the introduction of solid foods?
When your baby begins to show interest in food and can sit up on his own - usually around six months of age - it's time to start solid foods. However, it is not necessary to stop breastfeeding, Cathy explains: “A baby’s iron stores during pregnancy are depleted by six months, so he needs additional sources of this element.
However, it is not necessary to stop breastfeeding, Cathy explains: “A baby’s iron stores during pregnancy are depleted by six months, so he needs additional sources of this element.
Start complementary foods with solid foods, but remember that breast milk remains a more important source of calories and nutrients until the baby is eight to nine months old. By this time, he will be eating much more solid food, but he will still need to breastfeed four to five times a day. By 12 months, the frequency of feeding may be two to six times a day. All babies are different, and many of them at this age are still getting half their daily calorie intake from breast milk.”
Don't forget that breast milk can be added to solid foods, such as cereals and purees, so that the baby can taste the familiar taste. If possible, use milk expressed just before feeding (not thawed) and add just before serving to keep bacteria and nutrients alive. 16
You may be pressured by others to stop breastfeeding when your baby is six months old, but the longer you breastfeed or pump milk, the better for you and your baby.
How long can I continue breastfeeding?
“The World Health Organization recommends breastfeeding along with solid foods until at least two years of age because it plays an important role in supporting immunity,” says Cathy. feels bad".
At eight months, the baby sometimes breastfeeds four times a day, but by one year old, the frequency of feedings can be reduced to two times a day. You yourself will understand which feeding regimen is more suitable for you and your baby. For example, Jane, a mother of two from the US, breastfed until the age of two: “I breastfed when I was at home - in the evenings and on weekends, when the children wanted to be close to me,” says Jane, “It helped a lot when they were sick . Breastfeeding has become my favorite form of comfort."
“When my son got a little older and bolder, he still often asked me to breastfeed him - as if to calm down and gain strength,” recalls Amy, a mother of two children from Canada, “When he happened to hit or skin his knee , breastfeeding was a wonderful way to comfort him. ”
”
If your baby is over a year old and you are still breastfeeding, people around you will probably tell you that this way he will never wean. But if children are not pressured, they usually refuse to breastfeed themselves between the ages of two and four. 17
“I didn’t intend to breastfeed for so long, but as a result, I still breastfeed my four-year-old daughter and 22-month-old son,” says Suzanne, mother of two from the UK, “I breastfeed my youngest before and after work, and in I express milk on business trips. The eldest daughter likes to breastfeed a little before bed or when she is upset - this is a great way to make contact. When I get tired of it, I remind myself what great benefit and comfort it brings them. I now plan to pursue a baby-initiated end breastfeeding strategy — let them decide when to stop.”
For more information on what to expect and lots of tips and tricks, see our guide Breastfeeding Problems After the First Month.
Literature
1 Ballard O, Morrow AL. Human milk composition: nutrients and bioactive factors. Pediatr Clin North Am . 2013;60(1):49-74. - Ballard O., Morrow A.L., "Composition of breast milk: nutrients and biologically active factors." Pediatrician Clean North Am. 2013;60(1):49-74.
Human milk composition: nutrients and bioactive factors. Pediatr Clin North Am . 2013;60(1):49-74. - Ballard O., Morrow A.L., "Composition of breast milk: nutrients and biologically active factors." Pediatrician Clean North Am. 2013;60(1):49-74.
2 Kent JC et al. Principles for maintaining or increasing breast milk production. J 2012;41(1):114-21. - Kent J.S. et al., "Principles for Maintaining and Increasing Milk Production". J Obstet Ginecol and Neonatal Nurse. 2012;41(1):114-121.
3 Kent JC Volume and frequency of breastfeedings and fat content of breast milk throughout the day. Pediatrics. 2006;117(3): e 387-395. - Kent J.S. et al., "Amount and frequency of breastfeeding and fat content of breast milk during the day." Pediatrix (Pediatrics). 2006;117(3):e387-95.
2006;117(3):e387-95.
4 Kent JC et al. Longitudinal changes in breastfeeding patterns from 1 to 6 months of lactation. Breast Med . 2013;8(4):401-407. - Kent J.S. et al., Longitudinal changes in breastfeeding patterns from 1 to 6 months of lactation. Brest Med. 2013;8(4):401-407.
5 Almroth S, Bidinger PD. No need for water supplementation for exclusively breast-fed infants under hot and arid conditions. Trans 9 R Soc Trop Med 1990;84(4):602-604. - Elmroth C, Bidinger PD, "No need for supplementation of exclusively breastfed infants in hot, dry conditions." Trans R Sots Trop Med Hyg. 1990;84(4):602-604.
6 Victora CG et al . Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet. 2016;387(10017):475-490. - Victor S.J. et al., "Breastfeeding in the 21st century: epidemiology, mechanisms and long-term effects". Lancet 2016;387(10017):475-490.
Lancet. 2016;387(10017):475-490. - Victor S.J. et al., "Breastfeeding in the 21st century: epidemiology, mechanisms and long-term effects". Lancet 2016;387(10017):475-490.
7 Peres KG et al. Effect of breastfeeding on malocclusions: a systematic review and meta - analysis. Acta Paediatr. 2015;104( S 467):54-61. - Perez K.G. et al., "The impact of breastfeeding on malocclusion: a systematic review and meta-analysis". Akta Pediatr. 2015;104(S467):54-61.
8 Mennella JA, Beauchamp GK. Maternal diet alters the sensory qualities of human milk and the nursling's behavior. Pediatrics. 1991;88(4):737-744. - Mennella, JA, Beauchamp, GK, "Maternal nutrition influences the organoleptic properties of breast milk and infant behavior." Pediatrix (Pediatrics). 1991;88(4):737-744.
9 Hassiotou F et al. Maternal and infant infections stimulate a rapid leukocyte response in breastmilk. Clin Transl immunology. 2013;2(4). - Hassiot F. et al., "Infectious diseases of the mother and child stimulate a rapid leukocyte reaction in breast milk." Clean Transl Immunology. 2013;2(4).
Clin Transl immunology. 2013;2(4). - Hassiot F. et al., "Infectious diseases of the mother and child stimulate a rapid leukocyte reaction in breast milk." Clean Transl Immunology. 2013;2(4).
10 Brown A, Harries V. Infant sleep and night feeding patterns during later infancy: Association with breastfeeding frequency, daytime complementary food intake, and infant weight. Breast Med . 2015;10(5):246-252. - Brown A., Harris W., "Night feedings and infant sleep in the first year of life and their association with feeding frequency, daytime supplementation, and infant weight." Brest Med (Breastfeeding Medicine). 2015;10(5):246-252.
11 Infant sleep information source. [Internet]. Normal Infant Sleep Development; December 2017 [cited 2018 Feb] - All about baby sleep. [Internet] "The development of normal sleep in a child", December 2017 [cited February 2018].
12 Baby sleep science. [Internet]. The-Four-Month-Sleep-Regression-What-is-it-and-What-can-be-Done-About-it. March 2014 [ cited 2018 Feb ] - The science of baby sleep. [Internet], "Four-month sleep regression: what it is and what to do about it." March 2014 [cited February 2018].
13 The Myth Of Baby Sleep Regressions – What’s Really Happening To Your Baby’s Sleep? [Internet]. Pinky Mckay ; December 2017 [ cited 2018 Feb ] - "The Myth of Baby Sleep Regression - What's Really Happening to Your Baby?" [Internet]. Pinky McKay, December 2017 [cited February 2018].
14 Kendall - Tackett K ET Al . The effect of feeding method on sleep duration, maternal well-being, and postpartum depression. Clinical Lactation . 2011;2(2):22-26. - Kendall-Tuckett K. et al., "Influence of feeding pattern on sleep duration, maternal well-being and the development of postpartum depression." Clinical Lactation. 2011;2(2):22-26.
Clinical Lactation . 2011;2(2):22-26. - Kendall-Tuckett K. et al., "Influence of feeding pattern on sleep duration, maternal well-being and the development of postpartum depression." Clinical Lactation. 2011;2(2):22-26.
15) Harrison D et al. Breastfeeding for procedural pain in infants beyond the neonatal period. Cochrane Database Syst Rev . 2014;10. — Harrison D. et al., "Breastfeeding for Relief of Medical Pain in the Neonatal Period." Cochrane Database of System Rev. 2014;10:CD11248
16 Czank C et al. Retention of the immunological proteins of pasteurized human milk in relation to pasteurizer design and practice. Pediatr Res . 2009;66(4):374. - Zhank S. et al., "Retention of immunological proteins in pasteurized milk depending on the technique and practice of pasteurization". Pediatrician Res. 2009;66(4):374.
Pediatrician Res. 2009;66(4):374.
17 Weaning from the breast. (2004). Paediatr Child Health, 9(4):249–253. - "Weaning from the breast" (2004). Pediatrician Child Health, 9(4):249–253.
Benefits of breastfeeding for baby
1 Victora CG et al . Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect . Lancet . 2016;387(10017):475-490. - Victor S.J. et al., "Breastfeeding in the 21st century: epidemiology, mechanisms and long-term effects". Lancet (Lancet). 2016;387(10017):475-490.
2 Bode L et a It’s alive: microbes and cells in human milk and their potential benefits to mother and infant . Adv Nutr . 2014;5(5):571-573. "It's Alive: Breastmilk Microbes and Cells and Their Potential Benefits for Mother and Baby." Adv Nutr. 2014;5(5):571-573.
2014;5(5):571-573. "It's Alive: Breastmilk Microbes and Cells and Their Potential Benefits for Mother and Baby." Adv Nutr. 2014;5(5):571-573.
3 Ballard O Human milk composition: nutrients and bioactive factors . Pediatr Clin North Am . 2013;60(1):49-74. - Ballard O., Morrow A.L., "Composition of breast milk: nutrients and biologically active factors." Pediatrician Clean North Am. 2013;60(1):49-74.
4 Ladomenou F Protective effect of exclusive breastfeeding against infections during infancy: a prospective study. Arch Dis Child . 2010; 95(12):1004-1008. - Ladomenu, F. et al., "The effect of exclusive breastfeeding on infection protection in infancy: a prospective study." Arch Dis Child. 2010;95(12):1004-1008.
2010;95(12):1004-1008.
5 Vennemann MM et al. Does breastfeeding reduce the risk of sudden infant death syndrome? Pediatrics. 2009;123(3): e 406-410. - Wennemann M.M. et al., "Does Breastfeeding Reduce the Risk of Sudden Infant Death?" Pediatrix (Pediatrics). 2009;123(3):e406-e410.
6 Hassiotou F et al. Maternal and infant infections stimulate a rapid leukocyte response in breastmilk. Clinic Transl Immunology . 2013;2(4): e 3. - Hassiot F. et al., "Infectious diseases of the mother and child stimulate a rapid leukocyte reaction in breast milk." Clean Transl Immunology. 2013;2(4):e3.
7 Harrison D et al. Breastfeeding for procedural pain in infants beyond the neonatal period. Cochrane Database Syst Rev . 2016;10: CD 011248. - Harrison D. et al., "Breastfeeding for Pain Relief from Medical Intervention in the Neonatal Period." Cochrane Database of System Rev. 2014; 10: CD 11248
2016;10: CD 011248. - Harrison D. et al., "Breastfeeding for Pain Relief from Medical Intervention in the Neonatal Period." Cochrane Database of System Rev. 2014; 10: CD 11248
8 Johnson TJ ET Al . Economic benefits and costs of human milk feedings: a strategy to reduce the risk of prematurity-related morbidities in very-low-birth-weight infants. Adv Nutr . 2014;5(2):207-212. — Johnson T.J. et al., Economic benefits and costs of breastfeeding: a strategy to reduce the risk of preterm complications in very low birth weight infants. Adv. 2014;5(2):207-212.
9 Schanler RJ et al. Randomized trial of donor human milk versus preterm formula as substitutes for mothers' own milk in the feeding of extremely premature infants. Pediatrics . 2005;116(2):400-406. - Chanler R.J. et al., "Randomized Trial of Donor Human Milk Versus Premature Formula as a Breast Milk Substitute in Severely Preterm Infants". Pediatrix (Pediatrics). 2005;116(2):400-406.
- Chanler R.J. et al., "Randomized Trial of Donor Human Milk Versus Premature Formula as a Breast Milk Substitute in Severely Preterm Infants". Pediatrix (Pediatrics). 2005;116(2):400-406.
10 Brown A, Harries V. Infant sleep and night feeding patterns during later infancy: association with breastfeeding frequency, daytime complementary food intake, and infant weight. Breastfeed Med . 2015;10(5):246-252. - Brown A., Harris W., "Night feedings and infant sleep in the first year of life and their association with feeding frequency, daytime supplementation, and infant weight." Brest Med (Breastfeeding Medicine). 2015;10(5):246-252.
11 Sánchez CL et al. The possible role of human milk nucleotides as sleep inducers. Nutr Neurosci . 2009;12(1):2-8. - Sanchez S.L. et al., "Nucleotides in breast milk may help the baby fall asleep." Nutr Neurosai. 2009;12(1):2-8.
2009;12(1):2-8.
12 Dekaban AS. Changes in brain weights during the span of human life: relation of brain weights to body heights and body weights. Ann Neurol . 1978 4(4):345-356. - Dekaban A.S., "Change in the weight of the human brain throughout life: the relationship of brain weight with height and body weight." Ann Neirol. 1978 4(4):345-356.
13 Deoni SC et al. Breastfeeding and early white matter development: A cross-sectional study. Neuroimage . 2013;82:77-86. - Deoni S.S. et al., Breastfeeding and early white matter development: a cross-sectional study. Neuroimaging. 2013;82:77-86.
14 Straub N et al. Economic impact of breast-feeding-associated improvements of childhood cognitive development, based on data from the ALSPAC. Br J Nutr . 2016:1-6. - Straub, N. et al., "Economic Impact of Breastfeeding-Associated Cognitive Development in the Child (According to ALSPAC )". Br J Nutr. 2016;1-6.
Br J Nutr. 2016;1-6.
15 Victora CG et al. Association between breastfeeding and intelligence, educational attainment, and income at 30 years of age: a prospective birth cohort study from Brazil. Lancet Glob Health . 2015; 3(4): e 199-205. - Victor S.J. and co-authors, "Relationship between breastfeeding and intelligence, educational attainment and income level at age 30: a prospective cohort study in Brazil." Lancet Globe Health. 2015; 3(4):e199-205.
16 Horta BL, Victora CG. Breastfeeding and adult intelligence – Authors’ reply. Lancet Glob Health . 2015;3(9): e 522. - Horta B.L., Victora S.J., "Breastfeeding and intelligence in adulthood - Author's response". Lancet Globe Health. 2015;3(9):e522.
17 Belkind-Gerson J et al. Fatty acids and neurodevelopment. J Pediatr Gastroenterol Nutr. 2008;47 Suppl 1:7-9 - Belkind-Gerson, J. et al., "Fatty acids and brain development." J Pediatrician Gastroenterol Nutr. 2008;47 Appendix 1:7-9
Fatty acids and neurodevelopment. J Pediatr Gastroenterol Nutr. 2008;47 Suppl 1:7-9 - Belkind-Gerson, J. et al., "Fatty acids and brain development." J Pediatrician Gastroenterol Nutr. 2008;47 Appendix 1:7-9
18 Heikkilä K et al. Breast feeding and child behavior in the Millennium Cohort Study. Arch Dis Child . 2011;96(7):635-642. - Heikkila K. et al., Breastfeeding and Child Behavior in a Millennial Cohort Study. Arch Dis Child. 2011;96(7):635-642.
19 Tharner A et al. Breastfeeding and its relation to maternal sensitivity and infant attachment. J Dev Behav Pediatr . 2012;33(5):396-404. — Tarner, A. et al., "Breastfeeding and its relation to maternal sensitivity and infant attachment." J Dev Behave Pediatrician. 2012;33(5):396-404.
20 Montgomery SM et al. Breast feeding and resilience against psychosocial stress. Arch Dis Child . 2006;91(12):990-994. - Montgomery S.M. et al., Breastfeeding and resilience to psychosocial stress. Arch Dis Child. 2006;91(12):990-994.
Breast feeding and resilience against psychosocial stress. Arch Dis Child . 2006;91(12):990-994. - Montgomery S.M. et al., Breastfeeding and resilience to psychosocial stress. Arch Dis Child. 2006;91(12):990-994.
21 Bener A et al. Does continued breastfeeding reduce the risk for childhood leukemia and lymphomas? Minerva Pediatr. 2008;60(2):155-161. - Bener A. et al., "Does long-term breastfeeding reduce the risk of leukemia and lymphoma in a child?". Minerva Pediatrician. 2008;60(2):155-161.
22 Singhal A et al. Infant nutrition and stereoacuity at age 4-6 y. Am J Clin Nutr . 2007;85(1):152-159. - Singhal A. et al., Nutrition in infancy and stereoscopic visual acuity at 4-6 years of age. Am F Clean Nutr. 2007;85(1):152-159.
23 Peres KG et al.