Baby vomiting solid food
Vomiting in babies | Pregnancy Birth and Baby
beginning of content5-minute read
Listen
From birth to 12 months, babies are known to vomit — it’s just one of their design features. However, as normal as vomiting is, it can also be worrying for parents. Occasionally, vomiting can be a sign of illness or complications, but for most babies, vomiting and reflux occurs simply because their guts are still developing.
What are the different types of vomiting
There are a few different types of vomiting and although the result is the same, the reasons are different:
- Possetting is the name for small amounts of milk brought up after a feed.
- Reflux happens when the valve at the top of a baby’s stomach is not tight enough to keep milk in there. A baby’s oesophagus (food pipe) is short, so when the valve opens and there’s only a short distance between it and their mouth, vomiting can occur.
- Projectile vomiting is vomiting with force. Projectile vomiting can be a symptom of a blockage at the outlet of a baby's stomach. If it's happening after most or all feeds, take your baby to a doctor.
What causes babies to vomit?
Generally, mild vomiting occurs because a young baby is still getting used to feeding on, digesting and eliminating milk. On average, a newborn baby’s stomach can hold around 20 millilitres, so it doesn’t take much milk for them to fill up and vomit the excess.
How can I tell if my baby is sick?
Vomiting by itself can be reassuring. However, if your baby has a temperature, is not feeding well, has diarrhoea or a rash, or experiences any other symptoms, your baby needs to see a doctor. If your baby seems healthy and well and is bright and alert, you may just want to monitor their vomiting to see when and how often it happens — but note that the amount that a baby vomits can be hard to work out and may seem larger than it really is.
What’s the difference between vomiting and reflux?
Vomiting caused by reflux generally occurs after feeding. It can seem effortless or cause pain. Some babies with reflux constantly 'spill' after and in-between their feeds. It’s important to think about how your baby’s vomiting affects them. If your baby seems happy, is thriving and gaining weight, you could simply try changing the frequency and amount of feeds you give them. If your baby seems to be in pain and/or not thriving, take them to a doctor. Sometimes medication is necessary for reflux.
Does breast or formula feeding cause more vomiting?
Breastfed babies can vomit as much as babies who are formula fed. There's no real difference between the two. Generally, the only difference is that feeding on formula makes a baby’s vomit smell and look different to that after feeding on breastmilk.
Can solids cause vomiting?
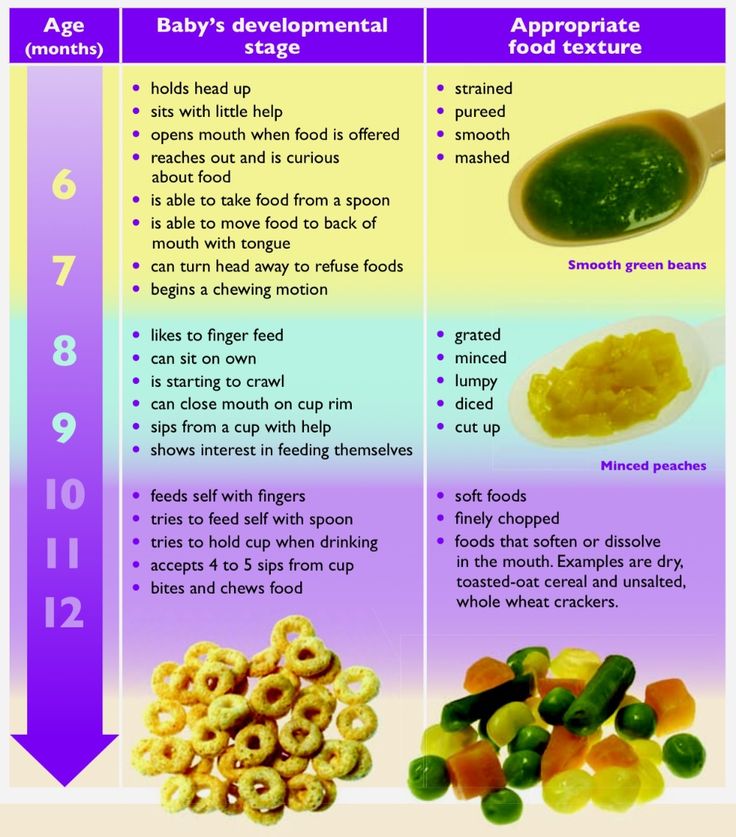
Some babies take time to adjust to digesting solid foods. They can vomit more when solids are introduced. This can occur because of overfeeding. Their stomachs are simply too small to accommodate extra volume. Start small when introducing solids — around 1-2 teaspoons of solids are ideal.
This can occur because of overfeeding. Their stomachs are simply too small to accommodate extra volume. Start small when introducing solids — around 1-2 teaspoons of solids are ideal.
Is vomiting a sign of allergies?
Some allergies can cause vomiting, especially allergies to cow's milk. Your baby can react to particular foods or ingredients if they’re sensitive to them. Your doctor can help guide you to decide which foods are best for your baby.
How can I treat my vomiting baby?
Most babies recover quickly after vomiting and don't need any specialised care. They can seem hungry again straight away or take a while to want to feed again. However, if they vomit a lot and have other symptoms, a doctor needs to assess them.
Generally, babies are not given medication for vomiting unless they can’t keep any milk or fluids down. Dehydration is generally managed by giving intravenous fluids.
Sometimes changing feeding positions and frequency can reduce the likelihood of vomiting. It's still important to always follow the safe sleeping guidelines when settling your baby, even if they vomit. Back sleeping is protective against choking.
It's still important to always follow the safe sleeping guidelines when settling your baby, even if they vomit. Back sleeping is protective against choking.
When should you see a doctor?
You should take your baby to see your doctor if:
- you are concerned about your baby's vomiting
- your baby is showing other signs of illness
- your baby seems lethargic, sleepy and not interested in feeding
- your baby is losing weight and not thriving
- there is blood or bile in their vomit
- their vomiting isn’t stopping or getting worse
Sources:
Raising Children (Vomiting), Red Nose Australia (Will baby choke if he/she vomits while sleeping on the back?), Safer Care Victoria (Vomiting in neonates), The Royal Australian College of General Practitioners (The vomiting child)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: September 2022
Back To Top
Related pages
- Knowing your baby is well - podcast
- How to know when your baby is well - video
- Reflux
- Vomiting in children
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Baby Vomiting After Introducing Solids?
·
Written by Jo Charnock
·
Written by Jo Charnock
On this Page:
- Types Of Baby Vomiting
- Causes Of A Baby Vomiting
- Other Symptoms To Look Out For
- Treatment For Your Baby Vomiting
- Reducing Reflux Vomiting
- Signs That Baby May Be Allergic To Foods
- When To See Your Doctor
- Things To Remember
Is your baby vomiting after eating? Is it happening after introducing solids? Are you concerned? Don’t worry, we’ve gathered some helpful advice for you here!
Vomiting in young babies and small children is very common. This is especially true in the early weeks of introducing solids and new foods (so around 4 months old), and as their small bodies develop. A baby vomiting may seem quite scary at first, but if your baby is generally happy and healthy then there shouldn’t be anything to worry about. Vomiting can be a symptom of many different minor illnesses in babies, but it’s usually nothing serious, and they normally recover quickly. The amount of vomit can look like a lot, too much to come out of your little one, but remember it’s only what went in that’s coming out!
This is especially true in the early weeks of introducing solids and new foods (so around 4 months old), and as their small bodies develop. A baby vomiting may seem quite scary at first, but if your baby is generally happy and healthy then there shouldn’t be anything to worry about. Vomiting can be a symptom of many different minor illnesses in babies, but it’s usually nothing serious, and they normally recover quickly. The amount of vomit can look like a lot, too much to come out of your little one, but remember it’s only what went in that’s coming out!
Types Of Baby Vomiting
There are three different types of baby vomiting which include the following:
- ‘Posetting’– is when your baby brings up small quantities of milk or food after a feed. Its not really vomiting as it’s normally a gentle, burp-like movement, which causes your baby no stress.
- ‘Reflux’– occurs when food backs up the food pipe, or oesophagus, from your baby’s stomach.
 This will cause your baby to vomit gently, or spit the food up. Reflux is rarely a problem and your baby should grow out of it by the time they are around 18 months old.
This will cause your baby to vomit gently, or spit the food up. Reflux is rarely a problem and your baby should grow out of it by the time they are around 18 months old. - ‘Projectile’– is when your baby is vomiting in a more forceful way rather than just bringing up small quantities of food. A baby vomiting is quite natural and can be caused by simple things like car sickness, indigestion or even something as simple as crying too much. A baby vomiting may seem scary for both you and your baby, but rest assured, it is very normal. But if your baby is projectile vomiting after every meal then we recommend consulting your doctor.
Causes Of A Baby Vomiting
A baby vomiting is often the sign of a minor illness or infection. It can be caused by:
- a minor infection like the common cold,
- a dose of ‘gastro’ or gastroenteritis, which is very common,
- car or motion sickness caused by travelling in a moving vehicle.
More serious illnesses that can cause your baby to vomit can include the following:
- urinary tract infections,
- ear infections,
- appendicitis,
- meningitis,
- food allergies.

If your baby’s vomiting is accompanied by fever or diarrhoea, it’s usually a sign of a virus infection. Plus if your baby is vomiting for more than 12 hours then dehydration will be a major concern. If your baby is showing these signs then it’s time to see your doctor.
Other Symptoms To Look Out For:
Keeping in mind that vomiting in babies is normal and mostly no cause for real concern, you should be on the look out for the following symptoms:
- nausea
- diarrhoea
- stomach or abdominal pain
- dehydration
- lethargy
- weight loss
While not all are a cause for any immediate action, it is important to take note, and be aware if the symptoms improve or get worse.
Treatment For Your Baby Vomiting
While a baby vomiting can be a very unpleasant experience for both you and your baby, they usually recover quickly. Vomiting can be easily treated with rest, lots of fluids and plenty of reassurance and comfort. To prevent dehydration, liquids should be given little and often. Checking your baby’s nappy will give you a good indication; if it’s drier than normal then your baby is not drinking enough.
To prevent dehydration, liquids should be given little and often. Checking your baby’s nappy will give you a good indication; if it’s drier than normal then your baby is not drinking enough.
Don’t give your baby over the counter medicine or any medication that has not been prescribed by your doctor.
Reducing Reflux Vomiting
While reflux vomiting is normal for young babies, the following tips may help to reduce his or her discomfort:
- switching to anti-colic teats and bottles
- holding and feeding your baby in an upright position,
- trying smaller and more frequent feedings,
- avoid bouncing or getting your baby excited after feeding,
- trying thicker foods like cereals,
- giving your baby milk or water after feeding to reduce acid and indigestion,
- make sure feeding time is a quiet time with no outside stimulation.
Signs That Baby May Be Allergic To Foods
Food allergies may cause vomiting, but are often accompanied by other symptoms like diarrhoea and skin rashes or hives. Keeping a record of what you are feeding your young baby when introducing solids is recommended. If you suspect a food allergy you can consult your doctor about what may be the cause. Foods generally associated with food allergies include eggs, wheat, nuts, some berries, milk, fish and seafood. Most of these you should avoid feeding your baby until they are at least 12 months old.
Keeping a record of what you are feeding your young baby when introducing solids is recommended. If you suspect a food allergy you can consult your doctor about what may be the cause. Foods generally associated with food allergies include eggs, wheat, nuts, some berries, milk, fish and seafood. Most of these you should avoid feeding your baby until they are at least 12 months old.
When To See Your Doctor
While we’ve mentioned that a baby vomiting is normal and children will mostly get over vomiting very quickly, there will be times when you need to consult your doctor or health worker. It’s time to see your doctor when any of the following symptoms occur:
- your baby has been vomiting for more than 12 hours,
- there is blood or bile in the vomit,
- your baby is not gaining weight,
- there are signs your baby has stomach pain or a swollen abdomen,
- your baby has persistent indigestion or heartburn,
- your baby seems generally unwell.

Use your instincts, if your baby is showing signs or symptoms of being unwell, go and see your doctor.
Things to Remember
In general, symptoms found in babies are similar to those found in adults, so you don’t need to panic every time your baby throws up. Vomiting can lead to diarrhoea, fever, and sometimes abdominal cramps. However, the symptoms can be easily treated by allowing some time to rest, lots of rehydration and maybe some soft foods.
Please keep the following in mind:
- mild vomiting is normal in most babies and improves over time,
- most babies need simple treatment, or none at all,
- having an upright feeding position may help,
- never give any medication unless prescribed by your doctor,
- after vomiting, try to give your baby a small amount of liquid or a little food,
- if your child seems unwell or shows any worrying symptoms, see a doctor!
Important
You shouldn’t use over-the-counter medications to stop vomiting in children. The side effects of these medications can be very serious. Sometimes doctors prescribe medications to stop vomiting, but they do this only after a proper medical review.
The side effects of these medications can be very serious. Sometimes doctors prescribe medications to stop vomiting, but they do this only after a proper medical review.
Hopefully, this has helped to shed some light about the causes of a baby vomiting
Read more about our Homemade baby food recipes.
Need some more info about introducing solids to bub? Download your free Guide here!
Any questions or comments? sound off below 🙂
References
The Royal Children's Hospital Melbourne
The Raising Children
Better Health Channel - Victoria State Goverment
Tagged in
- Starting solids
Continue reading
Baby Thermometers: Ear vs Forehead Thermometer?
How To Warm A Baby Bottle Safely
Feeding Schedule For Your 6 Month Old Baby
Viral Gastroenteritis (Children 2-5 Years)
Most cases of diarrhea and vomiting in children are caused by a virus. This is viral gastroenteritis. Many people call it "stomach flu" but it has nothing to do with the flu. This virus infects the stomach and intestinal tract. The disease lasts from 2 to 7 days. Diarrhea means loose or watery stools that are different from a baby's normal bowel movements.
This is viral gastroenteritis. Many people call it "stomach flu" but it has nothing to do with the flu. This virus infects the stomach and intestinal tract. The disease lasts from 2 to 7 days. Diarrhea means loose or watery stools that are different from a baby's normal bowel movements.
The child may also have the following symptoms:
The main danger of this disease is that it leads to dehydration. This is the loss of a large amount of water and mineral salts by the body. In such cases, fluid loss by the body must be replenished. This is done with oral rehydration solution. These solutions are available from pharmacies and most grocery stores without a prescription.
Antibiotics are not effective for this disease.
Home Care
Follow your pediatrician's instructions.
If you are giving medicine to your child:
-
Do not use over-the-counter diarrhea medicines unless your doctor has prescribed them.
-
Acetaminophen or ibuprofen can be used for pain and fever.
 Or another medicine as prescribed.
Or another medicine as prescribed. -
Aspirin as an antipyretic is contraindicated in children under 18 years of age. Its use can lead to serious liver problems and a life-threatening condition called Reye's syndrome.
To prevent the spread of the disease:
-
Remember that alcohol-based soap and disinfectants are the best way to prevent the spread of infection.
-
Wash your hands before and after caring for your sick child.
-
Clean the toilet after every use.
-
Dispose of soiled diapers in an airtight container.
-
Keep your child away from other people until the doctor says so.
-
Wash your hands before and after preparing food.
-
Wash hands and utensils after using cutting boards, countertops and knives that have been in contact with raw food.
-
Keep raw meat away from cooked and ready-to-eat foods.
-
Please note that people with diarrhea or vomiting should not prepare food for others.

How to properly drink and feed
The main goal in the treatment of vomiting or diarrhea is to prevent dehydration. To do this, the child should often consume liquids in small portions.
-
Keep in mind that fluid is more important than food right now. Give a small amount of liquid at a time, especially if the child has stomach cramps or is vomiting.
-
If you have diarrhea: If you are giving milk to your baby and the diarrhea does not stop, refuse the milk. In some cases, milk can make diarrhea worse. If this happens, use an oral rehydration solution. Eliminate apple juice, soda, sports or other sweetened drinks. Drinks with sugar can make diarrhea worse.
-
For vomiting: Start with oral rehydration solution at room temperature. Give 1 teaspoon (5 ml) every 5 minutes. Even if the child is vomiting, continue to give the solution. Most of the fluid will be absorbed despite vomiting. After 2 hours without vomiting, start with a small amount of milk or formula and other fluids.
 Increase the amount depending on tolerance. Do not give your child plain water, milk, formula, or other liquids until the vomiting stops. Give more oral rehydration solution as vomiting decreases. Increase the interval between doses. Continue until the child has urine and is no longer thirsty (no interest in drinking). If there has been no vomiting within 4 hours, resume feeding solid food. After 24 hours without vomiting, resume normal eating.
Increase the amount depending on tolerance. Do not give your child plain water, milk, formula, or other liquids until the vomiting stops. Give more oral rehydration solution as vomiting decreases. Increase the interval between doses. Continue until the child has urine and is no longer thirsty (no interest in drinking). If there has been no vomiting within 4 hours, resume feeding solid food. After 24 hours without vomiting, resume normal eating. -
Gradually, the child's normal diet can be resumed as he/she feels better. Don't force your child to eat, especially if they have stomach pain or cramps. Do not feed your baby large portions at a time, even if he is hungry. Tobacco smoke can make a child feel worse. Over time, the child can be given more food, provided it is tolerated. Foods that are allowed include cereals, mashed potatoes, applesauce, mashed bananas, crackers, dry toast, rice, oatmeal, bread, noodles, pretzel, rice or noodle soups, and cooked vegetables.
-
If symptoms return, return to a simple or no cure diet.
Follow-up
See or follow your pediatrician's instructions. If a stool or culture test is taken, see your doctor for results as directed.
Call 911
Call 911 if your child has any of these symptoms:
-
Difficulty breathing
-
Consciousness of consciousness
-
Extreme drowsiness or loss of consciousness
-
Problems with
-
Fast pulse
-
Breast pain
90009000 9000 9000 Seek medical attention
Seek medical attention immediately in the following cases:
-
Abdominal pain worsens
-
Constant pain in the lower right side of the abdomen
-
Repeating vomiting after the first 2 hours of fluid administration
-
Episodic vomiting for more than 24 hours
-
Long -term strong diarrhea over more than 24 hours
-
Blood in stool or vomit
-
Decreased ability to eat orally
-
Darkening or absence of urine within 6 to 8 hours in older children, 4 to 6 hours in infants
-
Wakes or crying, when a child is not possible to reassure
-
Unusual drowsiness
-
New rashes on the skin
-
DIOLS lasts more than 10 days
-
The temperature (see “Temperature and children” below below.
 )
)
Temperature and children
Always use a digital thermometer to take your child's temperature. Never use a mercury thermometer.
For infants and toddlers, use the rectal thermometer properly. A rectal thermometer can accidentally break a hole (perforate) in your rectum. It can also carry germs from the stool. For proper use, always follow the manufacturer's directions. If you feel uncomfortable taking your rectal temperature, use another method. At your pediatrician's appointment, let them know which method you used to take your child's temperature.
Temperature advice. Ear temperature is inaccurate until 6 months of age. Do not take oral temperature until your child is 4 years old.
Infants under 3 months:
-
Ask your doctor how to take your temperature correctly.
-
Rectal or frontal (temporal artery) temperature 100.4°F (38°C) or higher, or as directed by physician
Child aged 3 to 36 months:
-
Rectal, frontal (temporal artery), or ear temperature of 38.
 9°C (102°F) or higher, or as directed by a physician
9°C (102°F) or higher, or as directed by a physician - armpits 38.3°C (101°F) or higher, or as directed by a physician
Child of any age:
-
Repeated fever of 40°C (104°F) or higher, or as directed by a physician
-
Temperature lasting more than 24 hours in a child under 2 years of age. Or a temperature that lasts for 3 days in a child aged 2 years or older.
Was this helpful?
Yes noTell us more.
Check all that apply.
Wrong topic—not what I was looking for.
It was hard to understand.
It didn't answer any of my questions.

I still don't know what to do next.
other.
NEXT ▶
Last question: How confident are you filling out medical forms by yourself?
Not at all A little Somewhat Quite a bit Extremely© 2000–2020 The Stay Well Company, LLC. All rights reserved. This information is not a substitute for professional medical advice. Always follow your doctor's instructions.
Start New Patient Education Search
Vomiting food - causes, diagnosis and treatment
Vomiting food is a complex reflex act in which gastric juice with partially fermented food masses is released through the mouth as a result of increased pressure on the muscles of the gastrointestinal tract and diaphragm .
 The symptom is often combined with nausea, abdominal pain, stool instability. Vomiting occurs with organic and functional diseases of the upper digestive tract, but sometimes has a physiological origin. To identify the prerequisites for the violation, ultrasound, radiography, endoscopy, manometry, and laboratory tests are performed. To stop the symptom, prokinetics, sorbents are used.
The symptom is often combined with nausea, abdominal pain, stool instability. Vomiting occurs with organic and functional diseases of the upper digestive tract, but sometimes has a physiological origin. To identify the prerequisites for the violation, ultrasound, radiography, endoscopy, manometry, and laboratory tests are performed. To stop the symptom, prokinetics, sorbents are used. Causes of food vomiting
In most cases, the appearance of a symptom is caused by various morphological or functional disorders of the digestive system. Physiological causes include overeating, which is accompanied by stretching of the gastric wall and reflex excitation of the vomiting center in the medulla oblongata. The symptom is often provoked by the use of a large amount of heavy food with alcohol. Vomiting food is also one of the manifestations of toxicosis in the first half of pregnancy.
Pyloric stenosis
Vomiting of ingested food is a common symptom of narrowing of the junction between the stomach and the duodenum, which can be either congenital or associated with organic lesions of the gastroduodenal zone.
 With pyloric stenosis, there is a long delay in the chyme in the stomach, which causes overstretching of the organ. Nerve impulses from receptors are transmitted mainly through the vagus nerve to a specific center of the brain, which triggers a sequential vomiting act.
With pyloric stenosis, there is a long delay in the chyme in the stomach, which causes overstretching of the organ. Nerve impulses from receptors are transmitted mainly through the vagus nerve to a specific center of the brain, which triggers a sequential vomiting act. The frequency of vomiting depends on the severity of the stenosis. With a mild to moderate degree of narrowing of the pyloric sphincter, the manifestation is observed once every few days. With decompensated pyloric stenosis, antiperistaltic contractions occur after each meal. The vomit has a rotten smell. Characterized by constant heaviness and dull pain in the epigastrium, a feeling of fullness in the stomach, bloating. With a long course of the disease, exhaustion progresses up to complete cachexia.
Poisoning
Dyspeptic disorders are the main symptoms of food poisoning provoked by the use of low-quality products contaminated with staphylococci, enterobacteria and other pathogens.
 An attack of vomiting occurs a couple of hours after eating and is combined with diarrhea, cramping abdominal pain, and signs of general intoxication. Excitation of the vomiting center is caused by a massive exposure to toxins, an important role is played by the direct irritating effect of microbes on the gastric mucosa.
An attack of vomiting occurs a couple of hours after eating and is combined with diarrhea, cramping abdominal pain, and signs of general intoxication. Excitation of the vomiting center is caused by a massive exposure to toxins, an important role is played by the direct irritating effect of microbes on the gastric mucosa. Gastritis
The appearance of vomiting food is more typical for acute gastritis, which is accompanied by pronounced organic changes in the gastric mucosa. The symptom in most patients occurs immediately after eating due to irritation of the nerve endings. A combination of vomiting with sharp pains in the epigastric zone, constant nausea and belching with air is typical. Vomit may contain impurities of mucus and bile. There is also diarrhea up to 7-10 times a day, which sometimes leads to dehydration.
Gastroduodenal diseases
In diseases of the stomach and duodenum, vomiting is reflex in nature, it is preceded by nausea.
 The symptom is caused by excessive stimulation of the center of the medulla oblongata along the fibers of the vagus, phrenic nerves. Many patients note an improvement in well-being after the release of vomit, so sometimes they themselves induce vomiting. Complaints of abdominal pain, flatulence, diarrhea, constipation are typical. Vomiting of gastric chyme with food is manifested by:
The symptom is caused by excessive stimulation of the center of the medulla oblongata along the fibers of the vagus, phrenic nerves. Many patients note an improvement in well-being after the release of vomit, so sometimes they themselves induce vomiting. Complaints of abdominal pain, flatulence, diarrhea, constipation are typical. Vomiting of gastric chyme with food is manifested by: - Gastroparesis . A decrease in the contractility of the gastric muscles predisposes to the appearance of antiperistaltic contractions, which cause vomiting with the release of a large amount of food. Patients complain of nausea after eating, a feeling of fullness in the epigastrium, belching with air or rotten. Repeated vomiting is noted in severe disorders, when the chyme stagnates in the stomach for several days.
- Acute gastric dilatation . The clinical picture of the disease develops acutely due to a violation of the innervation of the gastric wall. There are sharp pains in the epigastric region, which are combined with nausea, hiccups.
 There is indomitable vomiting with the release of gastric contents with food (up to 8 liters per day), then bile may appear in the vomit. Vomiting occurs without the application of volitional efforts, does not bring relief.
There is indomitable vomiting with the release of gastric contents with food (up to 8 liters per day), then bile may appear in the vomit. Vomiting occurs without the application of volitional efforts, does not bring relief. - Duodenal stenosis . Regurgitation of food eaten indicates a decompensated state, when the gastric muscles cannot cope with the large amount of chyme that came as a result of duodeno-gastric reflux. Other dyspeptic disorders are likely: nausea after eating, belching rotten, sometimes patients complain of heartburn. Characterized by pain, a feeling of heaviness in the stomach.
- Adductor loop syndrome . In this variant of diseases of the operated stomach, partially digested chyme accumulates in the blind section of the intestine, the condition is aggravated by increased secretion of intestinal juice. With a significant expansion of the intestine, duodenostasis begins, which is complicated by jejunogastric reflux with profuse vomiting of food eaten.
 As a rule, the general condition is disturbed, intoxication increases.
As a rule, the general condition is disturbed, intoxication increases. - Neoplasms . Vomiting food often occurs when tumors are localized in the pyloric part, when they impede the passage of chyme into the underlying sections of the digestive tract. Benign formations develop oligosymptomatically, clinical signs appear only with large sizes of the polyp. In malignant tumors, vomit contains blood impurities; in severe situations, vomiting of “coffee grounds” begins.
Functional dyspepsia
Inorganic gastric disorders are characterized by polymorphism of clinical signs, their rapid appearance and disappearance. Dyspeptic symptoms are usually preceded by errors in the diet, stressful situations. Habitual vomiting is typical, occurring suddenly and associated with the effects of higher nervous structures on the medulla oblongata. In addition to regurgitation of food, flatulence, heaviness in the epigastrium, and instability of the stool are possible.
 Against the background of dyspeptic symptoms, symptoms of vegetovascular dystonia often appear.
Against the background of dyspeptic symptoms, symptoms of vegetovascular dystonia often appear. Pathologies of the esophagus
In the pathogenesis of esophageal vomiting, disorders in the coordination of contractions of the sphincters and the smooth muscle layer, as well as mechanical obstacles that impede the movement of food, are of great importance. Distinguish between early vomiting occurring directly during eating and caused by mechanical obstruction, and late as a manifestation of functional changes in the work of muscle sphincters. The symptom is combined with dysphagia, chest pain. The most common causes of vomiting are:
- Esophageal stenosis . In the case of congenital stenosis, symptoms in the form of regurgitation of uncured milk are detected already in the first days of life. With acquired constriction, the first sign is dysphagia, first of solid food, and then of semi-liquid and liquid. The delay of the food bolus over the site of stenosis and the expansion of the organ provokes vomiting.
 Inhalation of particles predisposes to coughing, shortness of breath, suffocation.
Inhalation of particles predisposes to coughing, shortness of breath, suffocation. - Esophageal diverticula . The formation of a saccular protrusion of the wall occurs more often in older people, who often suffer from other pathologies of the gastrointestinal tract. Food accumulates in the formation, which is then excreted during vomiting. For a diverticulum, the presence of retrosternal pain, bad breath, and belching is pathognomonic. Due to the improvement in the condition after vomiting, many patients cause it artificially.
- Dyskinesia . Regurgitation of just eaten food is possible with any violation of the contractile activity of the esophageal muscles. The symptom often occurs with hypomotor dyskinesia with a long delay in food masses at the entrance to the stomach. In addition to vomiting, swallowing disorders are determined, and with functional disorders, patients have difficulty swallowing liquids, and solid food passes without problems.

- Achalasia cardia . In case of violations of the innervation of the lower esophageal sections, the cardiac sphincter closes reflexively, which makes it difficult for food to pass into the stomach. The esophagus expands, stagnation of food masses develops. This leads to regurgitation due to contraction of the esophageal muscles and is manifested by profuse "mouthful" regurgitation. Patients have dysphagia when taking both liquid and solid foods.
- Ulcer defect . For lesions of the esophageal mucosa, the appearance of sharp chest pains, heartburn immediately after eating is pathognomonic. At the height of the pain, vomiting begins, which brings relief. In the allocated masses, in addition to the food eaten, blood impurities are detected, indicating bleeding from the ulcer. With a prolonged course of the disease, there is a significant loss of body weight up to cachexia.
Examination
Vomiting food is often a sign of the presence of functional or organic diseases of the digestive system, so the diagnosis is carried out by a gastroenterologist, and the research is aimed at a comprehensive study of the state of the gastrointestinal tract.
 The use of instrumental examination methods allows you to establish the root cause of vomiting, laboratory tests are prescribed to confirm the diagnosis. In diagnostic terms, the most valuable are:
The use of instrumental examination methods allows you to establish the root cause of vomiting, laboratory tests are prescribed to confirm the diagnosis. In diagnostic terms, the most valuable are: - Endoscopy . With the help of EGDS, the state of the esophageal, gastric and duodenal mucosa is visualized. The method allows to identify volumetric neoplasms, strictures and cicatricial deformities of the digestive canal. In doubtful cases, a biopsy of pathological foci for further histological examination is additionally recommended.
- Radiography . Highly informative is the method of X-ray imaging using an oral contrast agent - it helps to assess the nature, coherence of the work of the gastric and esophageal sphincters, to determine the speed of food movement through the gastrointestinal tract. Radiography is also needed to detect organic lesions.
- Ultrasound . Ultrasound of the abdominal cavity belongs to the group of fast non-invasive methods that are prescribed for screening examination of gastroenterological patients and the choice of further tactics.
 According to the indications, after a survey sonography, a targeted ultrasound of individual organs is performed to detect pathological changes.
According to the indications, after a survey sonography, a targeted ultrasound of individual organs is performed to detect pathological changes. - Esophageal manometry. With a possible esophageal origin of vomiting, the pressure in different parts of the organ must be measured. Usually, a study is made of contractions of the upper and lower smooth muscle sphincters, as well as an assessment of pressure in the body of the esophagus. If necessary, the study is supplemented with antroduodenal manometry.
- Bacteriological tests . Dyspeptic symptoms are possible with various intestinal infections. In order to exclude this group of diseases, it is necessary to sow feces and vomit on nutrient media, which makes it possible to identify the main pathogens. When confirming the infectious etiology of the process, the blood is additionally examined for antibodies.
If vomiting of food eaten is likely to be associated with disorders of the acid-producing function of the stomach, it is advisable to measure the acidity of gastric juice and the amount of free hydrochloric acid.
 A biochemical blood test is shown to determine the level of amylase, lipase, concentration of gastrin, pepsinogen. In the absence of organic lesions of the digestive organs, a neurological examination is prescribed to rule out functional disorders.
A biochemical blood test is shown to determine the level of amylase, lipase, concentration of gastrin, pepsinogen. In the absence of organic lesions of the digestive organs, a neurological examination is prescribed to rule out functional disorders. Esophagogastroduodenoscopy
Symptomatic therapy
If vomiting occurs one-time or episodically and is provoked by overeating, it does not require specific treatment. To reduce the load on the digestive system after heavy feasts, it is advisable to consume easily digestible low-calorie food for several days, refrain from taking fatty meat dishes, smoked meats. If you suspect food poisoning, you should rinse the stomach, take sorbents. With pathologies of the gastrointestinal tract, complex therapy of the underlying disease is necessary.
Until an accurate diagnosis is made, medications can be used to reduce unpleasant symptoms: prokinetics, anticholinergics. Do not take strong antiemetics on your own, as this can be dangerous to health.

-








.jpg)

