Best food to start feeding baby
When, What, and How to Introduce Solid Foods | Nutrition
For more information about how to know if your baby is ready to starting eating foods, what first foods to offer, and what to expect, watch these videos from 1,000 Days.
The Dietary Guidelines for Americans and the American Academy of Pediatrics recommend children be introduced to foods other than breast milk or infant formula when they are about 6 months old. Introducing foods before 4 months old is not recommended. Every child is different. How do you know if your child is ready for foods other than breast milk or infant formula? You can look for these signs that your child is developmentally ready.
Your child:
- Sits up alone or with support.
- Is able to control head and neck.
- Opens the mouth when food is offered.
- Swallows food rather than pushes it back out onto the chin.
- Brings objects to the mouth.
- Tries to grasp small objects, such as toys or food.
- Transfers food from the front to the back of the tongue to swallow.
What Foods Should I Introduce to My Child First?
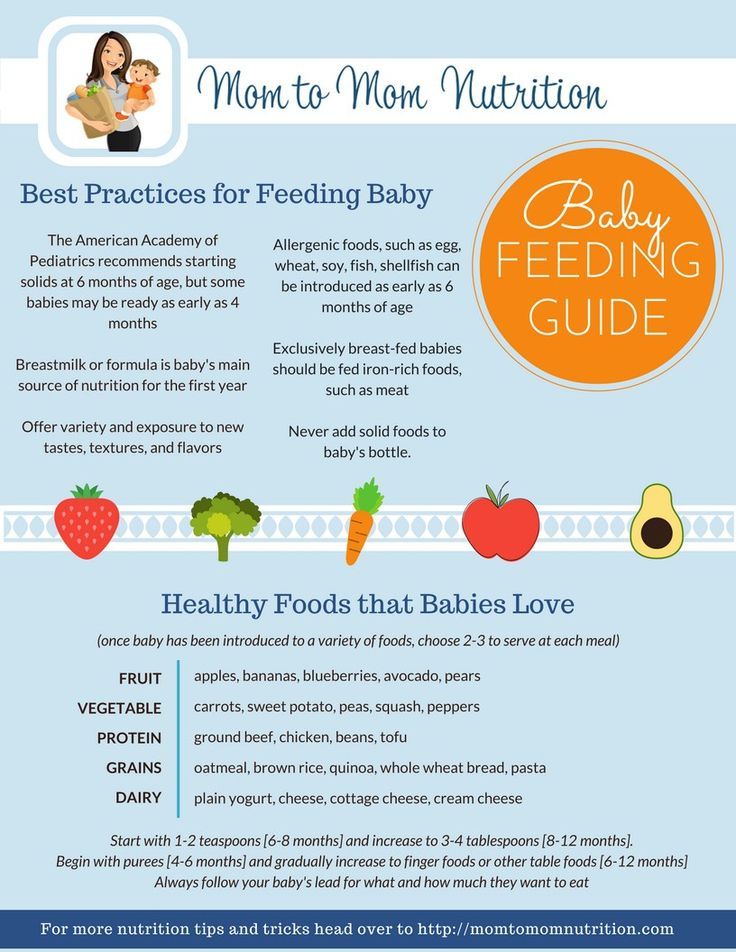
The American Academy of Pediatrics says that for most children, you do not need to give foods in a certain order. Your child can begin eating solid foods at about 6 months old. By the time he or she is 7 or 8 months old, your child can eat a variety of foods from different food groups. These foods include infant cereals, meat or other proteins, fruits, vegetables, grains, yogurts and cheeses, and more.
If your child is eating infant cereals, it is important to offer a variety of fortifiedalert icon infant cereals such as oat, barley, and multi-grain instead of only rice cereal. Only providing infant rice cereal is not recommended by the Food and Drug Administration because there is a risk for children to be exposed to arsenic. Visit the U.S. Food & Drug Administrationexternal icon to learn more.
How Should I Introduce My Child to Foods?
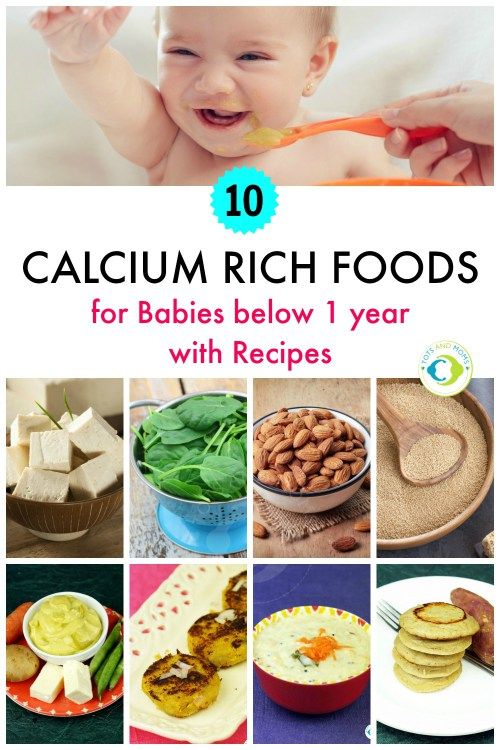
Your child needs certain vitamins and minerals to grow healthy and strong.
Now that your child is starting to eat food, be sure to choose foods that give your child all the vitamins and minerals they need.
Click here to learn more about some of these vitamins & minerals.
Let your child try one single-ingredient food at a time at first. This helps you see if your child has any problems with that food, such as food allergies. Wait 3 to 5 days between each new food. Before you know it, your child will be on his or her way to eating and enjoying lots of new foods.
Introduce potentially allergenic foods when other foods are introduced.
Potentially allergenic foods include cow’s milk products, eggs, fish, shellfish, tree nuts, peanuts, wheat, soy, and sesame. Drinking cow’s milk or fortified soy beverages is not recommended until your child is older than 12 months, but other cow’s milk products, such as yogurt, can be introduced before 12 months. If your child has severe eczema and/or egg allergy, talk with your child’s doctor or nurse about when and how to safely introduce foods with peanuts.
How Should I Prepare Food for My Child to Eat?
At first, it’s easier for your child to eat foods that are mashed, pureed, or strained and very smooth in texture. It can take time for your child to adjust to new food textures. Your child might cough, gag, or spit up. As your baby’s oral skills develop, thicker and lumpier foods can be introduced.
Some foods are potential choking hazards, so it is important to feed your child foods that are the right texture for his or her development. To help prevent choking, prepare foods that can be easily dissolved with saliva and do not require chewing. Feed small portions and encourage your baby to eat slowly. Always watch your child while he or she is eating.
Here are some tips for preparing foods:
- Mix cereals and mashed cooked grains with breast milk, formula, or water to make it smooth and easy for your baby to swallow.
- Mash or puree vegetables, fruits and other foods until they are smooth.

- Hard fruits and vegetables, like apples and carrots, usually need to be cooked so they can be easily mashed or pureed.
- Cook food until it is soft enough to easily mash with a fork.
- Remove all fat, skin, and bones from poultry, meat, and fish, before cooking.
- Remove seeds and hard pits from fruit, and then cut the fruit into small pieces.
- Cut soft food into small pieces or thin slices.
- Cut cylindrical foods like hot dogs, sausage and string cheese into short thin strips instead of round pieces that could get stuck in the airway.
- Cut small spherical foods like grapes, cherries, berries and tomatoes into small pieces.
- Cook and finely grind or mash whole-grain kernels of wheat, barley, rice, and other grains.
Learn more about potential choking hazards and how to prevent your child from choking.
Top of Page
When to Start Baby Food
Starting solids is an exciting and important milestone in baby’s development—one that not only opens them up to a brand-new world of flavors and textures, but also puts them on the right path to growing healthy and strong. Here’s what you need to know about how and when to start baby food for a smooth transition.
Here’s what you need to know about how and when to start baby food for a smooth transition.
In this article:
When to start baby food
How to start baby on solids
Best first foods for baby
Introducing allergenic foods
When to Start Baby Food
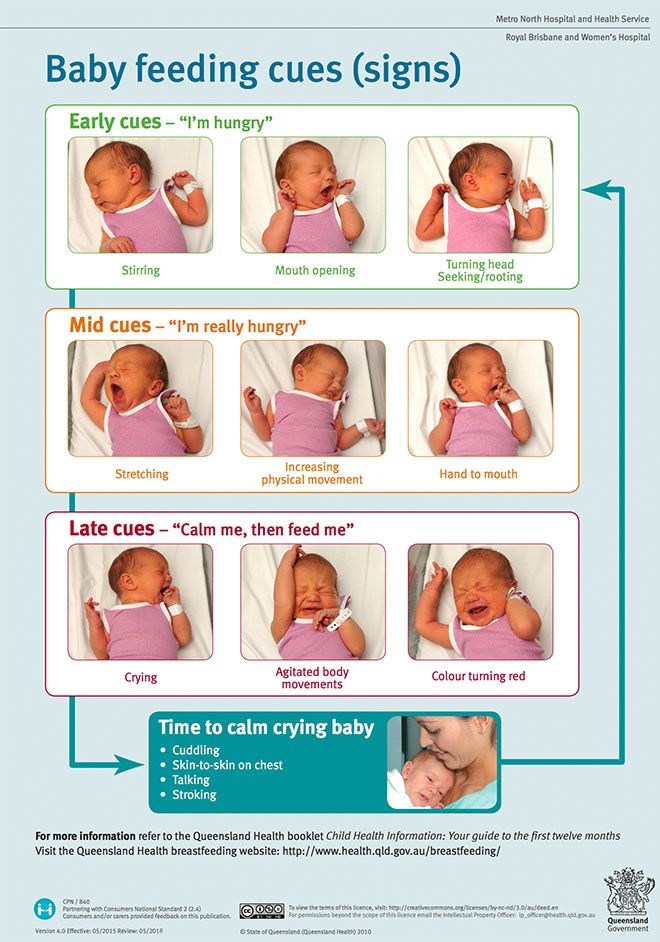
Knowing when to start baby food is both crucial and tricky. Starting baby on solids too early means you might increase the risk of choking, obesity and bellyaches, but introducing solids too late means you might slow baby’s growth and encourage an aversion to solid foods, among other conditions. Fortunately, doctors have zeroed in on a sweet spot for starting baby food, which is sometime between 4 and 6 months of age—though, ideally, baby should be receiving their nutrition exclusively from breast milk until the six-month mark, according to the American Academy of Pediatrics (AAP). How to tell if it’s time for starting solids for your little one? Baby will give you clues, including:
• Baby can sit in a high chair comfortably on their own. This is a major sign in terms of when to start baby food, says Lauren Kupersmith, MD, a pediatrician at Hassenfeld Children’s Hospital at NYU Langone in New York City. It means baby can hold their head up and doesn’t need to be propped up to stay in the upright position, which is important to avoid choking.
This is a major sign in terms of when to start baby food, says Lauren Kupersmith, MD, a pediatrician at Hassenfeld Children’s Hospital at NYU Langone in New York City. It means baby can hold their head up and doesn’t need to be propped up to stay in the upright position, which is important to avoid choking.
• Baby looks interested at mealtime. Babies likes to mimic what we do, so if your child likes to sit up like a big kid and watch you eat, then by all means let them try eating too.
• Baby can move food to the back of their throat to swallow. But if baby tends to push the food out of their mouth—not because they don’t like it, but because they can’t seem to get the food to where it needs to go—hold off on starting solids.
How to Start Baby on Solids
At 4 to 6 months, most of baby’s nutrition will still come from breast milk or formula, so don’t worry if baby doesn’t like eating food right away. Introducing solids is a gradual process, and every baby learns in their own time. Here are some general guidelines for how to start baby on solids:
Here are some general guidelines for how to start baby on solids:
• Feed baby with a spoon. Letting your child go at it with their hands may seem tempting (and super-cute), but it’s best that they learn the right way from the get-go. (And even then, be prepared to clean up more than a few messes!) Also, never put cereal (or any other food) in baby’s bottle—it’s a choking hazard.
• Start slowly. When introducing solids, a half spoonful will do at first—you may even want to talk baby through it (“Yummy!”). To make it easier for baby to get accustomed to the idea of swallowing solids, start mealtime with a little breast milk or formula, then offer some food (again, no more than a half teaspoon at a time) and finish off with more breast milk or formula. If baby cries or turns away when you present the spoon, try again some other time. Start off with introducing solids at one meal a day, then slowly work your way up. The morning is a good place to start, since baby is often hungriest at that time. When starting solids, baby typically won’t eat more than an ounce or two in one sitting.
When starting solids, baby typically won’t eat more than an ounce or two in one sitting.
• Try new foods more than once. Since babies’ tastes will evolve, you may need to try a food 20 times before a baby actually likes it, says Kupersmith.
• Stick with the same food for three days before trying another one. This makes it easy to track whether baby is allergic to a particular food.
• Try foods in different forms. If baby doesn’t like pureed food, try it mashed. After all, baby is learning about new textures as well as new tastes. It may be a case of trial and error until you find a winner.
Best First Foods for Baby
Got baby safely strapped into the high chair and bib? You’re ready to finally start feeding baby solids! There aren’t any official food rules for babies starting solids, and there’s no scientific evidence suggesting you should introduce one type of food before another, assuming the foods aren’t choking hazards. Nevertheless, baby cereal (such as oatmeal, rice and barley) is an “easy training food,” says Kupersmith, which is why it’s often recommended as baby’s first food; you can always mix it with more milk to build up to a thicker consistency. Many doctors also recommend starting vegetables before fruits, but there’s no evidence that this would make babies like vegetables more when they grow up—babies innately love sweets, and the order of introducing solids to baby doesn’t change that.
Nevertheless, baby cereal (such as oatmeal, rice and barley) is an “easy training food,” says Kupersmith, which is why it’s often recommended as baby’s first food; you can always mix it with more milk to build up to a thicker consistency. Many doctors also recommend starting vegetables before fruits, but there’s no evidence that this would make babies like vegetables more when they grow up—babies innately love sweets, and the order of introducing solids to baby doesn’t change that.
So why not simply start introducing solids with something you think baby will like? Here are a few common first foods for baby that are healthy and easy to eat (and, in the case sweet potato and banana, also easy to digest). Whatever you decide to feed baby, mash it with a fork or puree before serving whenever introducing solids.
- Baby cereal, such as oatmeal, rice, barley
- Sweet potato
- Banana
- Avocado
- Apples
- Pears
- Green beans
- Butternut squash
If your child has been breastfeeding, check with your pediatrician about getting a jump on pureed chicken or beef when you’re starting solids. These foods contain easily absorbable forms of iron and zinc, which baby needs by 4 to 6 months, according to the AAP.
These foods contain easily absorbable forms of iron and zinc, which baby needs by 4 to 6 months, according to the AAP.
At around 9 months, baby should have already worked their way up to a variety of foods, including cereal, vegetables, fruits, meats, eggs and fish (see below regarding the last two). (Keep in mind, though, that baby will still get the majority of their nutrients from breast milk or formula until age one.) By now, baby will probably settle on three meals a day along with two snacks. Let them consume about 4 ounces of solids at each meal (equivalent to a small jar of strained baby food) and about half that amount for each snack.
Save honey and cow’s milk for after baby’s first birthday—there’s a risk for infant botulism with honey (a type of bacterial poisoning), and baby’s tummy isn’t prepared to digest large amounts of cow’s milk until they’re about one year old. Avoid adult processed foods and foods that are choking hazards (such as sticky foods, like large gobs of peanut butter; hard foods that are difficult to gum, like raw vegetables, nuts, seeds and popcorn; and round, slippery foods that haven’t been cut up, like grapes and cherry tomatoes). Instead, the first foods for baby, and those in the months that follow, should be soft and served mashed, pureed or (once baby seems ready to move up from the really mushy stuff) cut up into really little bits. “There’s pretty much free reign at that point,” Kupersmith says.
Instead, the first foods for baby, and those in the months that follow, should be soft and served mashed, pureed or (once baby seems ready to move up from the really mushy stuff) cut up into really little bits. “There’s pretty much free reign at that point,” Kupersmith says.
Introducing Solids Chart
Hesitant about improvising your first foods for baby? That’s okay too. If you prefer an “introducing solids chart” to help you plan out baby’s path, the guide below can come in handy.
Image: The Bump
Introducing Allergenic Foods
Much of the confusion around when to start baby food stems from questions concerning allergenic foods. These are foods that babies are most often allergic to. The major culprits include dairy, eggs, fish, peanuts and tree nuts. In the past, parents were advised to hold off on exposing baby to these foods, but now doctors recommend introducing them early, often and in age-appropriate format, which means starting off with purees and soft textures.
“Dairy is an easy starting point, given options such as yogurt and cheese,” says David Stukus, MD, director of the Food Allergy Treatment Center at Nationwide Children’s Hospital and a spokesperson for the American College of Allergy, Asthma, & Immunology. You can also try scrambled eggs in small amounts, although baby may not be too pleased with the texture at first.
As far as peanut products go, the National Institutes of Health issued new guidelines in 2017 that encourage parents of children at high risk for peanut allergies to incorporate them into baby’s diet at 4 to 6 months of age. Giving these babies peanut products before the age of one actually decreases their risk of developing a peanut allergy before age 5 by 81 percent, compared to kids who are introduced to peanuts later in life. Parents of kids without the food allergy risk can start peanut products whenever they’d like, as long as the nuts are in an age-appropriate form: Peanut butter can be thinned out with water or mixed into a fruit or vegetable puree, and peanut powder can also be mixed into cereal and fruits. Don’t give whole peanuts or pieces of peanuts, since they’re a choking risk.
Don’t give whole peanuts or pieces of peanuts, since they’re a choking risk.
Allergic reactions to food are never just a fluke; they will happen with every exposure. Symptoms can range from mild (such as a rash or vomiting) to severe (such as trouble breathing). If baby has a food allergy, you’ll notice a reaction within minutes or up to two hours after eating the problematic food, Stukus says. If the symptoms are severe, call 911 right away. Otherwise, talk to your pediatrician; she can help confirm whether it’s an allergy or some other type of condition (such as a viral illness).
Expert bios:*
Lauren Kupersmith, MD, IBCLC, is a pediatrician and clinical instructor at Hassenfeld Children’s Hospital at NYU Langone in New York City, as well as a certified lactation consultant. She earned her medical degree from New York Medical College in 2005.
David Stukus, MD, is the director of the Food Allergy Treatment Center at Nationwide Children’s Hospital, an associate professor of pediatrics in the division of allergy and immunology and a spokesperson for the American College of Allergy, Asthma, & Immunology. He earned his medical degree from University of Pittsburgh School of Medicine in 2002.
He earned his medical degree from University of Pittsburgh School of Medicine in 2002.
Updated January 2020
Please note: The Bump and the materials and information it contains are not intended to, and do not constitute, medical or other health advice or diagnosis and should not be used as such. You should always consult with a qualified physician or health professional about your specific circumstances.
The best product for the first complementary foods - Encyclopedia Baby food
Beginning of complementary foods
Levchuk Victoria ©
Usually, at the pediatrician's appointment, mothers learn that it is time to introduce the first complementary foods. It is here that the doctor advises to start complementary foods with one or another product. How do they explain it!
In case of insufficient weight gain, gluten-free dairy-free porridge from such cereals as rice, buckwheat, corn is introduced as the first complementary food.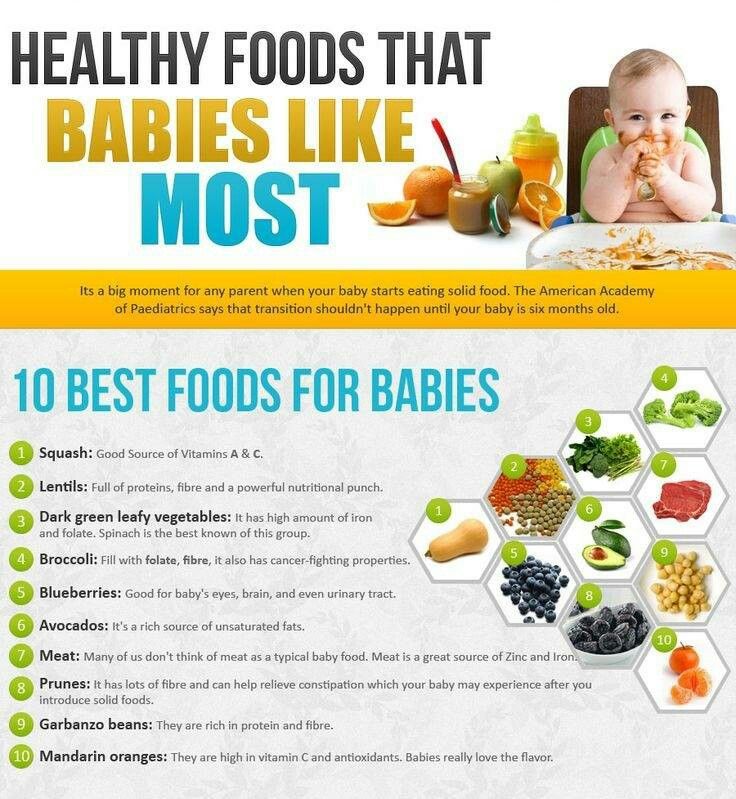 Usually the baby's first porridge is rice, as it is well absorbed and there is no allergy to it. However, buckwheat porridge is also useful, as it contains amino acids. Usually porridge is diluted with familiar food, i.e. formula or mother's milk.
Usually the baby's first porridge is rice, as it is well absorbed and there is no allergy to it. However, buckwheat porridge is also useful, as it contains amino acids. Usually porridge is diluted with familiar food, i.e. formula or mother's milk.
An allergic reaction to gluten is possible in a child, therefore cereals containing gluten are offered to a child after 8 months, and semolina in general after 3 years of age. Although our grandmothers and mothers introduced semolina from the age of 6 months, but now pediatricians recommend not to rush. Porridges are perfectly digested and less aggressively affect the baby's gastrointestinal tract. However, it must be remembered that cereals are strengthened, so if the baby suffers from constipation, then cereals in the form of the first complementary foods will not work.
1. The first food is vegetable puree. Vegetables in their composition do not contain fructose, which adversely affects the pancreas and stomach of the child, and the kidneys are less loaded. Moreover, vegetable purees are less allergic and perfectly normalize stools. Therefore, with frequent or periodic constipation and overweight, pediatricians recommend choosing vegetable puree as the first complementary food. First, the child is offered vegetable purees with delicate fiber from one type of vegetable (for example, zucchini, broccoli, cauliflower, pumpkin) and only then other vegetables (carrots, potatoes, white cabbage, etc.) are introduced.
Moreover, vegetable purees are less allergic and perfectly normalize stools. Therefore, with frequent or periodic constipation and overweight, pediatricians recommend choosing vegetable puree as the first complementary food. First, the child is offered vegetable purees with delicate fiber from one type of vegetable (for example, zucchini, broccoli, cauliflower, pumpkin) and only then other vegetables (carrots, potatoes, white cabbage, etc.) are introduced.
2. First food - fruit puree - green apple puree. Children will eat fruit puree with pleasure and get used to it faster. However, most pediatricians believe that it is better to offer vegetable purees first, and then fruit purees, since after sweet and tasty fruits, it is unlikely that a child will want to eat unsweetened squash or broccoli. The child receives all the necessary vitamins from milk formula or mother's milk, and much less from fruits.
3. The first food is baked apples and pears. If the child is prone to allergies, it is best to introduce baked fruit. During heat treatment, the allergenic properties of the product are lost. If the child does not have a reaction to the baked fruit, it can be administered raw.
If the child is prone to allergies, it is best to introduce baked fruit. During heat treatment, the allergenic properties of the product are lost. If the child does not have a reaction to the baked fruit, it can be administered raw.
Fruits and vegetables that are white and green in color are introduced into the first complementary foods. Foods must also be hypoallergenic (low allergenic), such as zucchini and green apples.
1. Zucchini, marrow, cauliflower, broccoli.
2. After the introduction of the first solid food - vegetable puree, you can try to give the baby porridge, and later fruit puree. At the beginning, you can introduce several types of vegetable purees, for example, everything listed above in paragraph 1, and then introduce several types of cereals, and then fruit. It may take about 5-6 weeks to introduce vegetables, but when introducing complementary foods, you should not rush, you need to monitor the reaction of the baby, let this period be a joy for both parents and the child. Remember that for him this is an important period in his life, for him everything is new, unusual and interesting, remember that you are laying the foundations for his future nutrition.
Remember that for him this is an important period in his life, for him everything is new, unusual and interesting, remember that you are laying the foundations for his future nutrition.
Social networks:
It is no secret that young and not very experienced mothers receive information on the nutrition of an infant, including recommendations on how to introduce the first complementary foods, mainly from two sources: grandmother's stories and from the Internet. Unfortunately, both of these respected sources of information may voluntarily or not voluntarily, but be very mistaken, since grandmothers grew up in a more prosperous time in terms of environmental conditions, and the Internet is littered with various articles that are rarely written by professionals, moreover, they rely either on explicit outdated guides on baby food, or frankly on unverified information.
In this article, I will try to combine the latest scientific data and recommendations on how to introduce the first complementary foods with many years of observations from the experience of a practical pediatrician and an allergist-immunologist.
At what age is it time to introduce the first complementary foods
According to the recommendations of the Research Institute of Nutrition of the Russian Academy of Medical Sciences, the first complementary foods can be introduced from 4.5 - 5 months, regardless of the type of feeding. This is "average". In practice, the choice of when to start introducing complementary foods still depends on the individual characteristics of the child. For example, for a child with widespread atopic dermatitis (diathesis), we will not introduce complementary foods until at least acute skin symptoms, such as cracks, weeping or secondary eczema, have steadily disappeared. Increased dryness and flaking of the skin, of course, require constant application of moisturizers to the skin, but in no case are they a contraindication to the start of the introduction of the first complementary foods.
Another important point when choosing the time to start introducing complementary foods is the dynamics of the child's weight gain. The more intensively the child gains in height and weight, the sooner he may need additional calories, since the energy value of breast milk or artificial formula alone will most likely not be enough for a child who grows faster than his peers by 4 - 5 months. We must not forget that natural products contain a fairly large range of minerals and vitamins, and a mother’s body, alas, cannot be an eternal and bottomless source of useful nutrients, somewhere something will gradually begin to be missed.
The more intensively the child gains in height and weight, the sooner he may need additional calories, since the energy value of breast milk or artificial formula alone will most likely not be enough for a child who grows faster than his peers by 4 - 5 months. We must not forget that natural products contain a fairly large range of minerals and vitamins, and a mother’s body, alas, cannot be an eternal and bottomless source of useful nutrients, somewhere something will gradually begin to be missed.
In addition, the nature of lactation in the mother has a great influence on the timing of the introduction of complementary foods. If a nursing mother begins to feel a lack of milk, I would prefer to first give her advice on stimulating lactation, and at the same time begin to introduce complementary foods. It will be better than introducing an artificial mixture. But I repeat that the earliest start date for the introduction of the first complementary foods is the age of 4 months, before the child's body is not yet ready, the risk of developing allergies is also high.
So, we agree with you that the first complementary foods can be introduced no earlier than 4 months of a child's life.
First complementary foods: Which foods to choose?
The first complementary foods, as a rule, should consist of vegetable or fruit purees, but in no case juices. Still, juices, even for children, are highly filtered, mainly contain a large amount of organic acids and “light” carbohydrates (that is, sugar, to make it clear to everyone). I will not waste time explaining why juices are harmful to an infant, but I will describe a clinical case from practice.
Parents with an 8-month-old girl came to the reception. Somewhere from 5 months she practically did not gain weight, although before that all indicators were normal. In the analyzes, apart from visible signs of iron deficiency, slightly reduced hemoglobin, no pathology was also detected. The main complaint: "does not eat anything." And when I began to find out what she still eats, it turned out that the child drinks half a liter of juice every day. But porridge or cottage cheese, or mashed potatoes cannot be forced together, they spit everything out. I don't like the taste. And so - for three months. The child, of course, became very nervous, yelling at night, demanding juice.
But porridge or cottage cheese, or mashed potatoes cannot be forced together, they spit everything out. I don't like the taste. And so - for three months. The child, of course, became very nervous, yelling at night, demanding juice.
So draw your own conclusions and be careful.
For the first feeding, this is now recognized by everyone, the best dishes are vegetable purees from green varieties of vegetables: zucchini, cauliflower, broccoli. The first complementary foods are introduced, starting with half a teaspoon, in the morning for three days, then gradually increase the amount of the product to 40-50 grams per week. Supplemented with breast milk or formula.
For problems with stools, constipation, it’s good to start introducing prune puree, green apple, you can try pumpkin, even apricot puree, but in no case start with carrots. Beta-carotenoids, which are abundant in carrots, are generally poorly absorbed and can cause allergies in a child.
Second food.
 Porridge or meat?
Porridge or meat? Even 5 - 6 years ago, we taught students at the medical institute that from 5 - 5.5 months old, an infant should begin to give cereal porridge for complementary foods. This is rice, buckwheat, corn. The first week you can cook 5% porridge: 5 grams of ground cereal per 100 ml of water. Then the porridges are cooked already denser: 10 grams of cereal per 100 ml of water. But now, basically everyone uses instant (soluble) cereals, which are diluted with water according to the instructions on the package. In addition, ready-to-eat liquid cereals are on sale: for example, Bellakt, Frutonyanya, etc.
Why meat? You ask. According to modern recommendations (they really began to change quite often), but in this case I support: if a child has a pronounced decrease in hemoglobin in the blood below 100 g / l by the age of 5 months, it makes sense to start introducing fruit or vegetable purees as a second types of complementary foods - meat purees as a source of the most well-absorbed heme iron.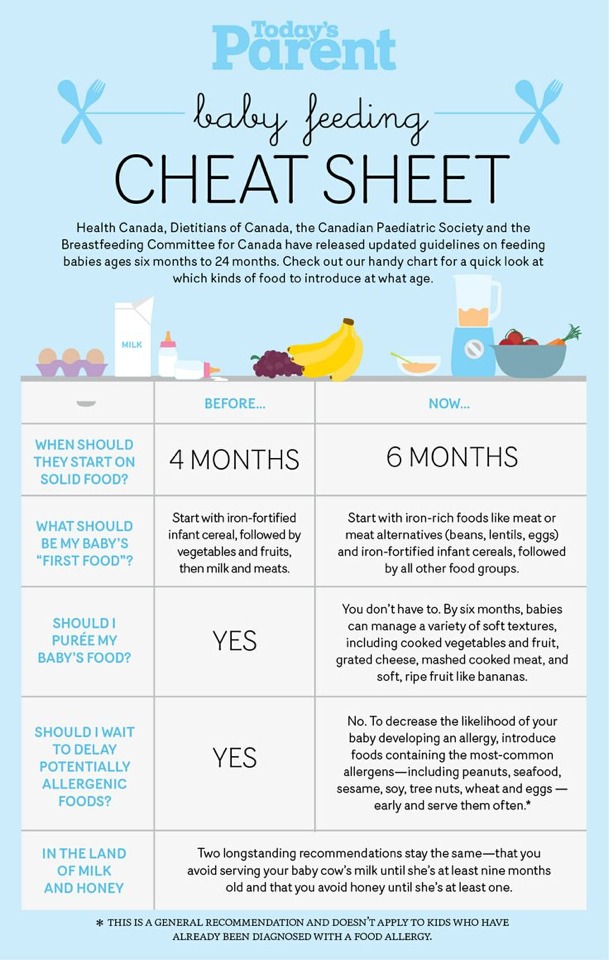 You need to choose from varieties such as turkey, rabbit, lamb. Beef and veal can only be offered to children who did not have red cheeks and diathesis.
You need to choose from varieties such as turkey, rabbit, lamb. Beef and veal can only be offered to children who did not have red cheeks and diathesis.
In the absence of problems with low hemoglobin, feel free to introduce porridge as the second meal of complementary foods, especially if the child is small and does not gain weight very well. In this case, we can recommend breeding cereals with the addition of breast milk or a mixture (Nan, Nutrilon, Celia, Nanny). With mixtures based on goat's milk, parents of children with a predisposition to allergies should be very careful. Goat milk formulas are not the best choice for babies who are allergic or intolerant to cow's milk protein, whatever the internet says. Believe me, there are serious scientific articles by foreign authors, which provided data on a very high frequency of cross-allergy between cow and goat milk proteins in children who were transferred to goat milk mixtures. And I saw it myself in my practice, when a child with dermatitis was transferred to a mixture of goat's milk, there was a clear improvement for a month or two, and then all over again and with a doubled degree of allergic skin damage.
Introduction to fermented milk products
This is the most difficult question. I am sure that most of our grandparents demand that their stupid parents start drinking milk and kefir as soon as possible. In a number of cases, children really start to absorb sour-milk products quite well after 6 months, but before this age I am very careful even with sour-milk Agusha, and even introducing milk or kefir before 6 months is a bad form, believe me, and can lead to very bad consequences for the child. I understand the Western European medical community, which has recently banned its pediatricians from recommending fermented milk products for complementary foods for children under 3 years of age, just imagine!
They (the Europeans) need to do something with their artificial milk mixtures. Even 20 years ago, we did not know other mixtures after the "two", that is, the second formula for children from 6 to 12 months. Then there were formulas for children from 1 to 2 years old, then from 2 to 3 years old, and now there are already mixtures for children up to 4 years old, and I think if this goes on, then until the age of sixteen there will be their own milk substitutes. Dismiss me, I don't think this approach is correct. But the fact is that our grandparents had much better genetics than the generation of our children, alas. In the context of the growth of medical capabilities, genetically determined diseases are also growing, and in this case, intolerance to cow's milk protein, and with every 10 years there are more and more such people among us. But if a child really suffers from an allergy to cow's milk protein or is severely deficient in enzymes, then he will carry this peculiarity through his whole life, and most likely he will not drink milk or kefir himself, and there is no need to force him if he himself won't want to!
Dismiss me, I don't think this approach is correct. But the fact is that our grandparents had much better genetics than the generation of our children, alas. In the context of the growth of medical capabilities, genetically determined diseases are also growing, and in this case, intolerance to cow's milk protein, and with every 10 years there are more and more such people among us. But if a child really suffers from an allergy to cow's milk protein or is severely deficient in enzymes, then he will carry this peculiarity through his whole life, and most likely he will not drink milk or kefir himself, and there is no need to force him if he himself won't want to!
But you are lucky with genetics, and no one in the family has ever had an allergy (which is hard to imagine nowadays), and most importantly, if your child has always had perfectly clean skin, then the first of the dairy products - cottage cheese, you will begin to offer your child with 7 months, kefir - from 10 months.