Best foods for reflux babies
Feeding Solid Foods To A Baby With Reflux: 5 Tips
Home / baby-solids-how / Feeding Solid Foods To A Baby With Reflux: 5 Tips
by Emily DeJeu in baby-solids-how —
Reflux: it’s a problem that affects many babies (up to 50% of babies age 0-3 months!) And if your baby has ever struggled with reflux, you know how hard it can be — the gas, the vomiting, the constant fussiness.
Since reflux is a digestive issue, introducing solid foods to your baby will definitely have an impact on her reflux symptoms. Some parents find their babies’ reflux symptoms actually improve with the introduction of solid foods; others find that starting solids increases reflux symptoms like gas and vomiting.
5 Tips For Feeding Babies With RefluxDoes your baby struggle with reflux? Below, we’ve included 5 tips to help you feed solid foods to your baby with reflux.
Offer good “first foods”.Rice cereal is usually considered a good first food for babies without reflux, and it may be fine for a baby with reflux, too. However, rice cereal has been known to cause constipation and gas in some babies, so you may want to avoid offering it right away, if your baby has reflux.
Instead, consider starting with these foods:
- Avocado — Foods that are high in fat, like avocados, can be good for babies with reflux. Babies with reflux may eat less than babies without, so it’s considered good practice to offer them high fat, high calorie foods.)
- Pears — Pears are one of the least acidic fruits, and since acid can trigger reflux, pears make a great first food for your baby.
- Bananas — Bananas have been shown to actually help with digestion.
Foods that are known to cause gas can cause lots of pain and discomfort for a baby who already struggles with reflux. Those foods include:
- Onions
- Garlic
- Broccoli
- Cucumber
- Brussel sprouts
- Cabbage
- Cauliflower
- Corn
Other foods that have been known to increase reflux symptoms include:
- Dairy products (particularly milk)
- Acidic foods, like tomatoes and oranges
- High-fat meats
- Carbonated drinks (not that you should be offering those to your baby anyway! 😉 )
Remember the 4 Day Rule? Essentially, the 4 Day Rule advises you to wait 4 days between introducing new foods to your baby. This allows you to figure out which (if any) foods your baby might be allergic to.
This rule works for babies with reflux, too. After you’ve offered your baby a new food, wait a few days to see if it triggers any reflux symptoms. This’ll make it much easier for you to uncover your baby’s “trigger foods” and keep those out of her diet as much as possible.
Offer frequent, small meals (but not too close to bedtime!)Your baby will have an easier time digesting small quantities of food than larger ones. And for some babies, eating large meals triggers reflux symptoms. So consider creating your own daily feeding schedule that’ll include 4 or 5 (or even 6) small meals.
What’s more, avoid offering your baby any solids in the hour before bedtime. This’ll help ensure that if he does have any reflux symptoms after eating, they won’t interfere with his nighttime sleep.
If your baby’s struggled with reflux since birth, you probably know this one already. The fact is that keeping your baby in an upright position after feeding can actually help him digest food, and can help prevent vomiting. This is true for babies when they’re breastfeeding or bottle feeding; it’s also true for babies when they’re eating solid foods!
Sit babies upright when it’s time for a solids meal, and avoid laying them down flat on their backs (or their stomachs) after eating. It’s also recommended that you avoid placing your baby in a walker or exersaucer (or anything else that’ll put pressure on his stomach) after he’s eaten.
Everything You Need To Know About Starting Solids – All In One e-Book!What if you could find everything you needed to know about starting your baby on solid foods – when it’s best to start solids, how to introduce solids, complications, food allergies, etc. – in one easy-reference guide? Now you can! Your Baby’s Start To Solid Foods: A Comprehensive Guide will walk you through every step of starting solids. Plus, your e-Book package includes several bonus materials, designed to maximize your success in starting solids. You’ll get a thorough guide to treating constipation, a dietitian’s advice on how to avoid 5 common solid-foods mistakes, and a weekly meal plan for your baby’s first year. Grab your e-Book today, and ensure your baby has the healthiest possible start to solid foods!
– in one easy-reference guide? Now you can! Your Baby’s Start To Solid Foods: A Comprehensive Guide will walk you through every step of starting solids. Plus, your e-Book package includes several bonus materials, designed to maximize your success in starting solids. You’ll get a thorough guide to treating constipation, a dietitian’s advice on how to avoid 5 common solid-foods mistakes, and a weekly meal plan for your baby’s first year. Grab your e-Book today, and ensure your baby has the healthiest possible start to solid foods!
*Some of this information was taken from homemade-baby-food-recipes.com.
The Baby Sleep Site® is a participant in the Amazon Services LLC Associates Program and other product affiliate programs. If you click on a product link and make a purchase, The Baby Sleep Site® may (but not always) receive a small commission from the company selling the product, but will not affect your purchase price. We only recommend products that we believe are quality products and are good for our readers.
We only recommend products that we believe are quality products and are good for our readers.
If you are tired of wading through stacks of baby sleep books that just aren't working, if you are beyond exhausted and just can't solve your child's sleep problems on your own...then personalized sleep consulting is for you. We have been around since 2008 and invite you to tap into our MANY years of experience. Our team of expert consultants will create a Personalized Sleep Plan® just for your family and then support you through every step of implementing your plan. We encourage you to consider our personalized, one-on-one baby and toddler sleep consultation packages if you want to see real, meaningful results now. Your consultation package also includes ample follow-up help, designed to help you troubleshoot problems and tweak your plan as needed.
Learn More About Services
For those persistent nighttime struggles, check out The 3 Step System to Help Your Baby Sleep. Using the same unique approach and practical tools for success, this e-book helps you and your baby sleep through the night.
Learn More About The 3-Step System
If you’re looking for ways to get your baby or toddler into a healthy sleeping routine during the day, explore Mastering Naps and Schedules, a comprehensive guide to napping routines, nap transitions, and all the other important “how-tos” of good baby sleep. With over 45 sample sleep schedules and worksheets, Mastering Naps and Schedules is a hands-on tool ideal for any parenting style.
Learn More About Mastering Naps
For those persistent toddler sleep struggles, check out The 5 Step System to Help Your Toddler Sleep. Using the same unique approach and practical tools for success, this e-book helps you and your toddler sleep through the night and enjoy a better daytime schedule.
Using the same unique approach and practical tools for success, this e-book helps you and your toddler sleep through the night and enjoy a better daytime schedule.
Learn More About The 5-Step System
Join our VIP Members Area packed with exclusive content and resources: e-Books, assessments, detailed case studies, expert advice, and more. As a VIP member, you'll also enjoy a weekly chat with an expert sleep consultant.
Learn More About VIP Membership
In over 10 years, we have over 10,000 comments on our blog.
At this time, we’ve turned the comment sections off. We would, of course, love to hear from you! For help with your specific sleep problems, please learn more about our DIY resources or our sleep consultation services. Or, consider emailing us for a fast and helpful response!
Feeding a baby with reflux | weaning advice | Babyexpert
As if coping with reflux wasn't tough enough, now your baby is ready for the new challenge of solid food. So if your baby finds it difficult to keep down milk, how will she cope with solids?
So if your baby finds it difficult to keep down milk, how will she cope with solids?
The good news is that some mums find weaning their babies on to solids can actually reduce reflux. However, others find it doesn't make a difference, it's just becomes a different challenge.
With expert advice, we've put together some useful info to help you and your baby with weaning...
Talk to your doctor or health visitor about when to start weaning
Because weaning may help to improve reflux for some (but not all) babies, you may be keen to start weaning early - ie, before the official guideline of 6 months. It's thought that the improvement may come because food is thicker than milk and is more likely to stay in your baby’s stomach, however there's no clear evidence for this.
"Some babies with reflux will improve once weaning has started and so doctors may advise early weaning for babies with reflux (though no earlier than 17 weeks)," says GP Dr Philippa Kaye.
If you do want to start early, it's vital that your baby is showing the 7 signs of readiness for weaning and that you talk to your GP or health visitor first.
If you're starting solids at 4 or 5 months, you will need to begin with purees, as your baby won’t be ready for baby led weaning. Once your baby is 6 months, baby led weaning or purees can be used.
Remember, you should never give your baby solids before 4 months (17 weeks).
How to give your baby solid food
- Start weaning slowly and take your lead from your baby as to how much she needs as she will still be getting the majority of her nutrition from milk
- Don't rush each meal. Let the food settle in her stomach
- Start with food that is as smooth as possible. Some babies with reflux can be sensitive to different textures, so it may help to introduce new textures slowly. Your baby may want to stay on purees for a little longer than a baby without reflux. You can slowly make purees thicker and slightly lumpier - aim to introduce more lumps between 7-9 months
- Although she has reflux, your baby does not need more solid foods than milk, and if she has stopped gaining weight or is losing weight then see your doctor
- Feed your baby in an upright position.
 Look for a highchair that offers a lot of support so even a young baby is sitting upright as possible
Look for a highchair that offers a lot of support so even a young baby is sitting upright as possible - Some mums find that giving solids after a milk feed helps their babies to keep the milk in their stomachs
- Keep a daily food diary. This will help you identify which food types your baby reacts more or less to
- Introduce new foods every three days, rather than every day. Your baby may not react immediately to a new food type, so you need a little time to see the effects
Best foods for a reflux baby
Each baby is unique and will have different reactions to foods. The best approach is to talk to your GP or dietician for individual advice. However, the current thinking is that good foods to give when starting weaning are:
- Purees of root vegetables, such as potatoes, carrots, pumpkin, swede, parsnips and sweet potato
- Non-acidic fruit
Foods you may want to avoid
These foods may exacerbate reflux or make it more painful:
- citric fruit, such as oranges, apples and grapes
- tomatoes, peppers, courgettes, cucumber and aubergines
- foods containing cows' milk proteins
- spicy foods
Is feeding a reflux baby more difficult?
In a nutshell, yes, it can be. This is because of the problems and pain caused by reflux, so many babies with this condition do at some point find feeding upsetting. If this happens to your baby, you’ll need lots of patience and persuasion.
This is because of the problems and pain caused by reflux, so many babies with this condition do at some point find feeding upsetting. If this happens to your baby, you’ll need lots of patience and persuasion.
If your baby starts to get very upset during feeding, it may help to let her out of the highchair and play for a period, and then try her again with the food 30 minutes later.
Does reflux made weaning harder? What mums say...
The results from our forum mums seemed to be a mixed bag: some hailed it a miracle for reflux problems, while others said it actually made things worse.
"We early weaned at 17.5 weeks for reflux - and there was absolutely no improvement. If anything it was worse because she then had more smelly stuff to bring up!! Her reflux didn't really clear up until she was about 9 or 10 months old, sometimes it just takes time.
More like this
"I've hated weaning and wish we'd held off for longer, it's a lot of extra hassle and heartache if your baby isn't a good eater.
"Sorry to put a downer on it but it's only fair you get both sides of the story!! Good luck with it, take it slowly and protect your floors!!" says Colligreen.
"We weaned Freya, who has silent reflux, at 22 weeks (we started 10 days ago!). I had really wanted to wait until 6 months, but she has needed to be held upright for about 2 - 3 hours after her bed time feed each night for about the last two months, and she is currently waking about 2-4 times a night. I couldn't cope with either and so we decided to see if solids would help," shares mum Alison E.
"She shows real interest in food, and weaning has been surprisingly easy so far (after a blip in the first few days, when I tried her on pure apple and carrot, but she was happier when it was mixed with baby rice and milk). I think it has started to help her reflux.
"She is on two meals a day and although she isn't sleeping better, for the last two nights we have been able to put her down an hour after she has eaten, which feels amazing!
"Just a hint - I hadn't realised but some solids can make refulx worse - namely acidic things like apple and pear (apparently banana also makes it worse - which sounded odd but she was a bit refluxy after she had banana for the first time).
"We are still giving her those things, but only in the morning and mixed with lots of milk and rice. In the evening it is solid easy stuff like carrot and sweet potato. THis has made things better - she was really refluxy the first time we gave her pear because I didn't know it could make it worse and it was at bedtime."
Posy took things slowly and had a positive result, sharing: "We weaned early at 4.5 months mainly due to reflux issues and not getting enough milk down my LO."
"It was slow going with baby rice/cereal, and baby rice mixed with veggies/fruit to start with for the first 6 wks, but things did turn a corner and at nearly 10 months now she is loving her food and it has def helped with the reflux.
"The only thing I would say is that she still has fairly small portions to help with food not refluxing back up again. She is still on Omeprazole however, but should be coming off it in the next month under consultant's instructions, yippee!"
And Peeptoe1 added: "I started weaning Hugo (24 weeks) on the weekend and so far it seems to have made things worse.
"He is on IG for reflux but that doesn't seem to be dealing with his acid as effectively now that we've introduced solids. He is back to looking really uncomfortable, arching, pulling his legs up, squealing and screeching and grunting, as well as being in a constant bad mood (as you would be if you were in pain!)
"He's also got the wet hiccups again, farting, burping and possetting a lot more (milk only, not food).
"So far I have only been giving him fruit (banana/apple/pear) mixed with a teaspoon of baby rice around mid morning and he is otherwise exclusively breastfed. It's really disrupting his sleep as well - nighttime and daytime."
What medicines can you give?
The first recommended medication is normally a paediatric version of Gaviscon. Never give your baby the adult over-the-counter version. The medication comes in powder form and is mixed with either breast milk, formula or water and thickens the milk as well as keeping the stomach contents in your baby’s tummy to prevent reflux.
Other medication such as antacids and anti-vomiting medicines may also be used but always speak to your GP or health visitor before using any medicine.
Read more:
- Weaning tips, recipes and guides from MFM
- What you'll need to buy for weaning
- From bottle to cup: when's the right time?
Proper nutrition for GERD - Clinic on Leninsky
The key to solving many problems with the gastrointestinal tract is proper nutrition. Gastroenterologist at the Clinic on Leninsky Katerina Chesskaya tells what you can and should eat for those who suffer from reflux disease.
What is GERD?
Gastroesophageal reflux disease (GERD) is a chronic relapsing disease in which there is a spontaneous, regularly repeated reflux of stomach contents into the esophagus. As a result, the lower esophagus is affected. The reflux of stomach contents into the esophagus is considered normal if it occurs occasionally and is not accompanied by negative factors. The disease is evidenced by the frequent recurrence of casting and inflammatory processes of the gastrointestinal tract.
The disease is evidenced by the frequent recurrence of casting and inflammatory processes of the gastrointestinal tract.
GERD is usually manifested by belching and heartburn after eating or bending forward, and also at night. Another indication of the presence of GERD is pain behind the sternum, extending to the interscapular region, lower jaw, and the left half of the chest. There are also signs of GERD that are not directly related to the esophagus - a cough, shortness of breath, often occurring when lying down, hoarseness, dry throat, rapid satiety, and bloating. The cause of chronic inflammatory diseases of the nasopharynx (pharyngitis, laryngitis, sinusitis, tonsillitis) in 30% of cases is GERD. It has been proven that against the background of GERD there is a risk of developing obstructive pulmonary diseases, including bronchial asthma.
Proper nutrition for GERD
As in the case of many other diseases of the gastrointestinal tract, the main principle of the treatment of GERD is proper nutrition. There are foods that relax the lower esophageal sphincter, which leads to the reflux of acidic stomach contents into the esophagus, that is, reflux. These include; strong tea, coffee, chocolate, citrus fruits, tomatoes, bitters (garlic, onion), fresh mint. As well as fatty varieties of fish, meat and products that cause gas formation: muffins, hot pastries, legumes, brown bread, cakes, pastries, grapes, cucumbers, carbonated drinks. Alcohol and smoking also reduce the tone of the lower esophageal sphincter.
There are foods that relax the lower esophageal sphincter, which leads to the reflux of acidic stomach contents into the esophagus, that is, reflux. These include; strong tea, coffee, chocolate, citrus fruits, tomatoes, bitters (garlic, onion), fresh mint. As well as fatty varieties of fish, meat and products that cause gas formation: muffins, hot pastries, legumes, brown bread, cakes, pastries, grapes, cucumbers, carbonated drinks. Alcohol and smoking also reduce the tone of the lower esophageal sphincter.
Here is a list of foods to consider when planning your menu for the day.
Delete:
1. Bread: fresh rye bread, tarts and pancakes.
2. Meat: stewed and fried meat dishes from fatty meat, poultry.
3. Fish: fatty fish, fried, smoked, salty dishes.
4. Vegetables: white cabbage, turnip, rutabaga, radish, sorrel, spinach, onion, cucumbers, salted, pickled and pickled vegetables, mushrooms.
5. Fruit: Raw, sour, unripe fruit, dried fruit puree.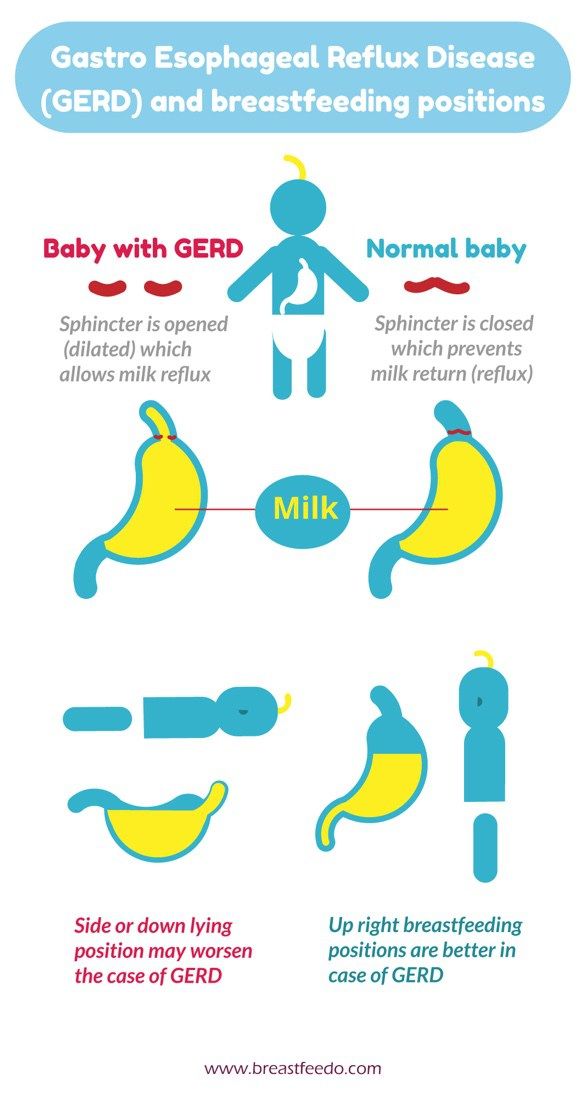
6. Cereals: millet, pearl barley, barley and corn grits, legumes.
7. High acidity dairy products, spicy and salty cheeses.
8. Sweet: halva, chocolate, ice cream, cakes.
9. Drinks: sour, carbonated, fruit drinks, strong tea, coffee and alcohol.
Recommended:
1. Bread: from wheat flour of the first or highest grade, yesterday, dry, uncomfortable baking.
2. Meat: Beef, veal, chicken, rabbit, turkey, all in the form of cutlets, meatballs, soufflés, mashed potatoes and quenelles.
3. Fish: boiled river fish - zander, pike, perch, any low-fat varieties.
4. Vegetables: carrots, cauliflower, potatoes, beets, squash and squash.
5. Fruits: Sweet berries, ripe fruits. Preferably mashed or baked.
6. Cereals: oatmeal, semolina, buckwheat (mashed), rice porridge, on the water with the addition of milk, boiled vermicelli.
7. Dairy products: milk, lean cheese and low-fat sour cream. Cottage cheese dishes made from pureed cottage cheese, for example, cheesecakes, casseroles.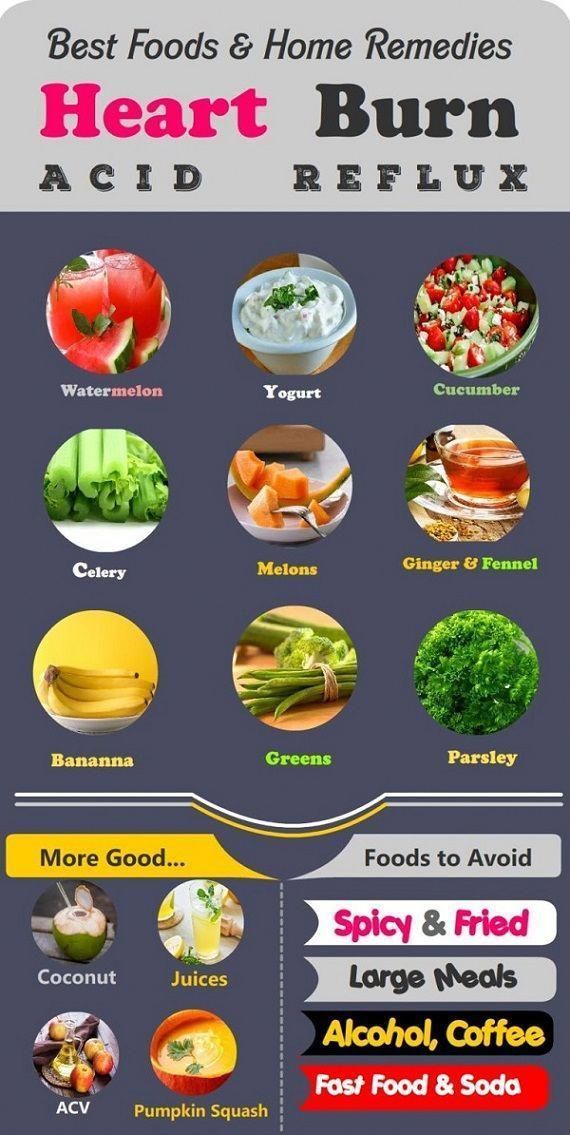
8. Sweet: jam, marshmallows, honey, marshmallow, cream and milk puddings.
9. Drinks: weak tea or cocoa with milk, sweet juices and decoctions.
It is also important to adhere to the diet:
— Fractional meals in small amounts and often up to 5-6 times a day.
- Do not lie down immediately after eating, the last meal is 2-3 hours before bedtime.
- Do not work in a slope, exclude the "gardener" pose.
- Do not wear tight belts and limit abdominal exercise.
- Obese people need to normalize body weight.
Remember that only a gastroenterologist can make a diagnosis of GERD (however, like any disease), to accurately determine the patient's condition. At the appointment, the doctor, together with the patient, will find the cause of the disease, outline a treatment plan and further supportive therapy in order to avoid relapses.
At the Clinic on Leninsky, an appointment is being made:
- pediatric gastroenterologist Natalya Medvedeva;
- gastroenterologist Ekaterina Chesskaya.

You can make an appointment with a gastroenterologist at the Clinic on Leninsky
by calling +7 (495) 668-09-86 .
Moscow, Leninsky prospect, building 67, building 2
Tel. .-Fri. 7:30–20:00 Sat-Sun 9:00–18:00
Diet for esophagitis of the esophagus | Sanatorium Gorny
Esophagitis is an inflammation of the esophageal mucosa due to weakness of the cardiac sphincter. A diet for esophagitis is a prerequisite for the complex treatment of the disease.
General rules. duration of the diet.
The main task of clinical nutrition in esophagitis of the esophagus is the complete exclusion of damage to the mucous membrane by mechanical and chemical factors.
With esophagitis, table number 1 is prescribed. In nutrition, you must adhere to a number of rules:
- the number of meals should be 5-6 times.
 portions are small. Such a tactic in nutrition with esophagitis allows the stomach to stretch unnecessarily and produce excess hydrochloric acid.
portions are small. Such a tactic in nutrition with esophagitis allows the stomach to stretch unnecessarily and produce excess hydrochloric acid. - Food should not be too hot or cold. The optimum temperature for food is 25-50 C.
- You can not eat "on the go". Eat slowly and chew your food thoroughly.
- Do not drink water immediately after eating. It is permissible to drink only 30-40 minutes after eating.
- Meals can be steamed, stewed, baked or boiled. You can't fry.
- Limit salt intake as much as possible.
In case of exacerbation of esophagitis, diet 1A should be followed for no more than 10 days. This diet is strict and if you stick to it, then the symptoms of the disease stop quickly enough. As soon as the discomfort and symptoms of exacerbation subside, you can go to table 1B. This table is more complete in terms of nutrients.
Notice! Acute esophagitis is a contraindication for spa treatment: it is better to go to a hospital.
If you have a chronic form, then you should regularly carry out preventive treatment .
Nutrition for chronic esophagitis:
In chronic esophagitis, table number 1 must be observed. From the diet it is necessary to remove all foods that can cause increased secretion of gastric juice or provoke increased gas formation.
Most of the food should be taken in the morning. You can not "eat up" at night, it is better to eat easily digestible foods, such as vegetable dishes or cereals.
List of approved products:
| Porridges and cereals | Buckwheat, rice, semolina, oatmeal |
| Dairy | Milk, non-acidic sour cream, low-fat dairy products, butter, unsalted cheese |
| Vegetables | Potatoes, zucchini, cauliflower, carrots, pumpkin, beets |
| Meat | Beef, veal, chicken, rabbit, turkey |
| by-products | Boiled tongue and liver |
| Fish | Low-fat varieties of river fish |
| Fruit | Bananas, apricots, pears, sweet apples, melons |
| Soft drinks | Weak tea, rosehip broth, compotes and kissels from sweet fruits and berries |
List of fully or partially restricted products:
| bread | Sweet pastries, fresh wheat and rye bread, pancakes, pancakes, fried pies |
| Vegetables | White cabbage, radish, radish, legumes, bell pepper, turnip, radish, onion, garlic, sorrel, spinach |
| Groats | Millet, barley, corn, barley |
| Fruits and berries | All sour fruits: citrus fruits, currants, green apples |
| Meat | Goose, duck, pork, canned meat, lard, sausages, sausages, smoked meat, dried meat |
| Soft drinks | Strong tea, coffee, kvass, sparkling water, sweet fruit drinks |
Nutrition menu for esophagitis.
 Diet.
Diet. Nutrition for esophagitis should be based on the fact that food should not be digested for a long time. Dishes should be easily digestible, should not irritate the mucous membrane of the stomach and intestines. Products should envelop the gastric mucosa, and not irritate it.
Diet recipes for esophagitis:
Sample menu for one day:
Breakfast:
Oatmeal boiled in water with milk, red apple compote.
Second breakfast:
Steam omelet. Rosehip decoction
Lunch:
Chicken soup with vermicelli and vegetables. Pike perch fillet with boiled potatoes. Herbal tea.
High tea:
Low fat yogurt. Cookie. Weak tea.
Dinner:
Vareniki with cottage cheese. Tea with milk.
Before going to bed you can drink a glass of warm milk.
Dietitian comments:
Therapeutic nutrition for esophagitis allows you to quickly get rid of unpleasant symptoms and normalize the work of the entire gastrointestinal tract.