Block feeding baby
What to Know About Block Feeding: How to Handle Hypergalactia
Written by WebMD Editorial Contributors
In this Article
- What Is Block Feeding?
- Who Should Try Block Feeding?
- Similar Treatment
A lot of breastfeeding women have an oversupply of breast milk, or hypergalactia, when they first start out. When your body overproduces milk for your baby, you could experience mastitis, clogged breast ducts, or other negative side effects. Block feeding can relieve such discomfort and help decrease your milk supply.
Block feeding is a common way to slow down milk production. It is one of many ways to treat hypergalactia. It has been proven to relieve discomfort and help your baby regulate its eating.
What Is Block Feeding?
Block feeding is a method used to make your body produce less milk. It focuses on feeding your baby one breast at a time. Block feeding can look like this:
- About an hour before your baby should eat, pump or express both your breasts as much as you can.
- When your baby is hungry, feed them from one side.
- For the next 3-hour block of time, if your baby initiates more feedings, let them drink from that same breast.
- Let your baby feed as often as they want from that side.
- After 3 hours, switch to the other side and do the same thing.
- If your unused breast gets uncomfortably full, self-express milk until you feel comfortable.
After a few days of block feeding, if your hypergalactia doesn’t improve, add more hours to your blocks. You can try feeding in 5- or 6-hour blocks if you still have an oversupply of breast milk.
Block feeding helps battle hypergalactia by utilizing your own body’s natural milk-making process. When your breasts are full for 3 to 6 hours, breast cells release the feedback inhibitor of lactation (FIL). It is a whey protein that tells your body to slow down lactation or milk production.
When you feed in blocks from one breast and leave the other breast full, FIL is released. The protein calms down your overactive milk supply one breast at a time.
The protein calms down your overactive milk supply one breast at a time.
Who Should Try Block Feeding?
If you have an oversupply of breast milk, you should try block feeding. You don’t need a diagnosis from your healthcare provider. When you have hypergalactia, both you and your baby will have symptoms. Block feeding can help prevent them.
If you have increased milk production, your let-down reflex can be too intense for your child. Your letdown reflex is the release of breast milk when the nerves in your breasts are stimulated from your baby’s sucking. Your baby could experience any of the following symptoms:
- Green foamy poop
- Stomach pain and more gas than usual
- Choking or coughing at the beginning of a feeding
- Frequent vomiting
- Refusing your breast
- Visible discomfort while breastfeeding
You will notice your own symptoms, too. Keep in mind that it’s common for women to have too much milk during the first few weeks of breastfeeding. But it typically self-regulates. If the following symptoms continue for longer than a few weeks, you’ll need to take action:
But it typically self-regulates. If the following symptoms continue for longer than a few weeks, you’ll need to take action:
- Full, tight breasts
- Lumps or pain that won’t go away
- Mastitis
- Pumping after feedings
- Painful letdown reflex
- Frequent leaking
Similar Treatment
If block feeding doesn’t work for you, there are other options for treating your oversupply of breast milk. Be careful when trying new things that will affect your baby’s diet. You need to address your oversupply. But the most important thing is to make sure your baby is getting enough to eat.
Herbs. Some herbs have been proven to reduce milk supply. Sage and parsley can be eaten or made into tea. Jasmine and peppermint can be directly applied to the breast. You should research each herb before trying it to make sure that you and your baby stay safe.
Medicine. Before you use pharmaceuticals to reduce your milk supply, talk to your healthcare provider. Some decongestants can decrease milk production. Estrogen, which is found in many birth control pills, helps reduce milk supply. Anti-prolactin drugs are specifically used to slow down the release of the milk-making hormone prolactin.
Some decongestants can decrease milk production. Estrogen, which is found in many birth control pills, helps reduce milk supply. Anti-prolactin drugs are specifically used to slow down the release of the milk-making hormone prolactin.
Feeding patterns. You can help your baby control how much they eat. Let them drink milk from your first breast as if it were their main meal. Then, offer your second breast as dessert. Don’t expect them to eat as much on the second side as they did on the first.
Let your baby stop when they want to. If your second breast starts to feel too full or uncomfortable, express or pump just enough milk to feel comfortable. Alternate which breast is the meal and which is the dessert. Over time, your milk supply will go down.
If you try block feeding and still have an oversupply of breast milk, contact your healthcare provider. They can help you resolve your hypergalactia or put you in touch with a lactation consultant you can talk to.
Is It Right For You?
While some breastfeeding moms consider milk oversupply a dream, for others it can seem more like a nightmare. Oversupply might mean you’re struggling with engorgement issues and a fussy baby who can’t latch or swallow well.
If you think you might have oversupply issues, you may have heard of block feeding. But before you try it, make sure you talk to a lactation consultant. Sometimes what you think might be oversupply is actually another issue altogether, like overactive letdown.
If your lactation consultant confirms you’re making more than enough milk for your growing baby, and your baby has been gaining weight at a healthy rate, they might suggest block feeding as a solution.
So, is it the right technique for you? How do you do it? What does a block feeding schedule look like? Don’t worry, we won’t leave you hanging without answers…
Block feeding is a breastfeeding method used to manage milk supply by reducing production to match your baby’s needs.
Breast milk is produced on a supply and demand basis. When your breast is stimulated frequently and emptied fully, it produces more milk. When milk is left in your breast and your breast is not stimulated, it stops producing as much milk.
Block feeding leaves milk inside your breast for a longer period of time, so that your body won’t think it needs to keep producing at such a high rate.
First, decide what feeding will be the beginning of your block feeding schedule. About an hour before, use your breast pump for a short period of time on each breast. This will help soften the breast and relax the milk ejection reflex just enough, setting you up for success.
When your baby gets hungry and the feeding starts, offer only one breast. Let your baby eat from that breast as long as they want. For the next 3 to 6 hours, bring baby back to that same side, only.
Your goal is to feed your baby on the same side, only, for the entire block of time. Your baby should still feed on demand during this time, whenever they give cues that they’re hungry.
For the next block, offer the other breast, and repeat the process on the other side.
If the unused breast starts to feel uncomfortable during your 6-hour block, try to pump only enough to relieve pressure. Avoid emptying the breast if you can, because that will tell your body to make more milk.
You can also use a cool compress on that breast to decrease discomfort — use the compress for no more than 30 minutes at a time with at least an hour break between uses.
For most people, it’s recommended to start with a short block schedule of only 3 hours at a time. If you’re a lactating parent with a large amount of extra milk, you may need longer blocks — like 8 to 10 hours — before switching sides.
As your body adjusts to the block feeding schedule, it’s possible you may get very uncomfortable. If you decide to pump fully, restart the block feeding schedule.
Block feeding is usually only used for a temporary period to get milk supply to a manageable level. It’s generally not recommended to block feed for longer than a week. Consult with your doctor, midwife, or lactation specialist to see how long you should block feed.
It’s generally not recommended to block feed for longer than a week. Consult with your doctor, midwife, or lactation specialist to see how long you should block feed.
Because block feeding is used for people trying to manage oversupply, this strategy should not be used by anyone who wants to increase their milk production.
Block feeding is not advised in the very early days after the birth of your baby. During the first 4 to 6 weeks postpartum, your breast milk volume is increasing rapidly and adapting to your growing baby.
It’s usually a good idea to establish your body’s natural milk supply by feeding on both breasts at each feeding. Or alternate breasts at each feed, depending on your baby’s hunger level.
Consult a lactation specialist about oversupply if, after 4 to 6 weeks, you find:
- your breasts are frequently feeling engorged despite regular feeds
- your baby is gagging, gulping, or coughing during feeds
- your breasts are frequently leaking milk
While block feeding may seem like an easy solution to oversupply issues, milk is being left inside the breast for longer periods of time than normal. This means there is an increased risk of clogged ducts and mastitis.
This means there is an increased risk of clogged ducts and mastitis.
To prevent these issues, there are some things you can do:
- Make sure to keep your breast area clean to avoid any bacterial infection.
- Take measures to ensure a good latch.
- Massage your breasts during feedings to help encourage full drainage.
- Switch feeding positions often to ensure that your breasts are being properly drained from all sides.
- Consider easing into block feeding by slowly extending the time you feed exclusively on one breast.
If you do see evidence of a clogged duct or mastitis, take action quickly to prevent it from getting worse! See your care provider immediately if you notice signs of infection, such as a fever, red marks, or extreme pain.
For people struggling with oversupply, feeling less engorgement (and the unpleasant side effects that can follow) is a major benefit of block feeding.
However, block feeding also has benefits for the baby.![]() Block feeding allows babies to get at more of the high protein, high fat hindmilk found at the end of a breastfeeding session.
Block feeding allows babies to get at more of the high protein, high fat hindmilk found at the end of a breastfeeding session.
Drinking more hindmilk can often improve digestion and prevent your baby from experiencing excessive gas, according to the La Leche League.
It’s also easier for little mouths to properly latch on less engorged breasts. Furthermore, because your baby will be able to control the flow of milk better with their tongue instead of clamping down on the breast, you may experience less nipple pain.
While these might sound like small benefits, they can make a big difference in comfort, nutrition, and ease of breastfeeding for both mom and baby.
Depending on the recommendations of your doctor, midwife, or lactation consultant, your block feeding schedule may look different than the one below, with longer or shorter blocks for each breast.
Here’s an example block feeding schedule, with an anticipated first feeding at 8 a.m. and 6-hour blocks:
- 7 a.
 m.: Pump just enough to relieve pressure on both breasts
m.: Pump just enough to relieve pressure on both breasts - 8 a.m.: Feed your baby on your right breast. Let your baby decide when they’re finished.
- 8:30 a.m. to 2 p.m.: All feedings that follow in this window stay on the right breast.
- 2 p.m.: Feed baby on your left breast. Let your baby decide when they’re finished.
- 2:30 p.m. to 8 p.m.: All feedings that follow in this window stay on your left breast.
If you’re experiencing breast milk oversupply issues, you’re probably willing to try just about anything to end the uncomfortable side effects! Check with a lactation consultant to confirm your oversupply, and talk to your pediatrician to make sure your baby’s weight is appropriate.
Block feeding can be an effective way to get your milk supply under control, but it’s important to keep an eye out for clogged ducts or mastitis if you use this method. You’ll also want to make sure that your little one doesn’t seem overly hungry after a few feeds on the same breast, too.![]()
Remember, block feeding is just temporary until your milk supply is more manageable. After your milk supply decreases, you can return to feeding as usual to keep your milk supply at the right volume for your growing baby.
Termination of breastfeeding | Stopping breastfeeding
When is it time to stop breastfeeding and what is the best way to do it? Read our article for useful practical tips on weaning.
Share this information
How long should breastfeeding continue? Three months? Six? Year? Or maybe a few years?
The World Health Organization (WHO) and other authorities recommend that infants be exclusively breastfed for the first six months and then continue to be breastfed along with other foods (complementary foods) for at least two years. 1
The fact is that breast milk is not just food. It is a natural sedative if the child is anxious or tired. In addition, milk contains immune-boosting components, the amount of which increases dramatically when the baby gets sick. 2
2
According to anthropologists, the natural age of a person to stop breastfeeding is even more than two years. Given factors such as tooth development, body weight, comparison with other primates, and historical evidence, some scientists believe that breastfeeding may last up to two to four years. A number of researchers even believe that our ancestors breastfed children up to six or seven years of age. 3
Today, more than 60% of mothers in developed countries start giving their babies formula or complementary foods before six months of age, 4 although WHO does not recommend this.
When is it time to stop breastfeeding?
Weaning means that you gradually stop breastfeeding your baby. Ideally, the first step in this process is the gradual introduction of complementary foods, starting at about six months of age. In this case, breastfeeding continues. The weaning process continues until the mother's milk has been completely replaced by other foods and drinks.
“After six months, the baby needs higher doses of certain nutrients, such as iron, zinc, vitamins B and D, that he cannot get from breast milk or from his own reserves,” says Sarah Beeson, health visitor from Great Britain.
“But solid food should at first only supplement the main diet with breast milk and gradually replace it. Mother's milk remains the main source of nutrition for the baby for many months to come.”
On average, a seven-month-old baby gets 93% of its calories from breast milk. And even between the 11th and 16th months, milk provides him with about half of the daily calorie intake. 5
“Sometimes moms think that breastmilk isn't that important once a baby has started solid foods, but the truth is, no matter how many months old a baby is, there's nothing better than your milk,” continues Sarah.
In fact, the process of finishing breastfeeding can take as long as mother and baby want. “When to stop breastfeeding is up to you,” says Sarah. The only thing that matters is what you think is right for you and your child.”
The only thing that matters is what you think is right for you and your child.”
How to wean
Whenever you decide to start weaning your baby, it's best to do it gradually. An abrupt cessation of breastfeeding can lead to lactostasis, blockage of the milk ducts and mastitis, and in a child such a sudden change can adversely affect the state of the digestive and immune systems. In addition, it will be difficult for both of you psychologically.
When should I stop breastfeeding?
Sometimes mothers mistakenly believe that it is time to stop breastfeeding, when in fact there is no reason to. If you're returning to work, breastfeeding can be a great way to stay close to your baby during this difficult time for both of you. You can express milk at work, and morning and evening feeding sessions will give you the opportunity to spend time alone with your baby. If you need to leave without your baby, you can also express milk and bring or send it home.
If you get sick, this is not always a reason to stop breastfeeding. Read our advice in the article on breastfeeding when sick and consult with your healthcare professional.
Read our advice in the article on breastfeeding when sick and consult with your healthcare professional.
Weaning up to six months
If you cannot continue breastfeeding until six months and want to try weaning your baby, start by replacing one feeding a day with a bottle of formula.
“It's best to start with midday feedings. Babies are very alert and able to smell breast milk nearby, so ask your partner or relative to give your baby a bottle when you're in the other room,” Sarah advises.
“Be hygienic when preparing meals. Be prepared for the fact that the baby will take fewer servings of expressed milk per day than if he was fed directly from the breast. Don't make him eat more milk than he wants."
You will probably feel that your breasts are fuller and more tender. This is due to the fact that your body is rebuilding to produce less milk. If this creates discomfort, try expressing some milk—just enough to relieve the discomfort without stimulating extra production.
When your body adjusts to the new volume - usually after a few days - replace with formula for one more meal a day. Continue this until you have changed all feedings and your baby is completely weaned.
“I had complications after my first birth, as a result I lost a lot of weight very quickly, and besides, I developed mastitis. Lactation was very weak, and at three months I was forced to stop breastfeeding,” recalls Jennifer, a mother of two from the UK, “I gradually replaced one feeding, so physically it was easy, but mentally it was hard for me.”
If you want to maintain closeness with your baby and all the health benefits of breastfeeding, but still need to cut down on breastfeeding, try partial weaning, replacing only a few feeds a day with formula.
Weaning after six months
Once your baby starts eating solid foods (about six months old), you will notice that breastfeeding naturally occurs less and less. For a year, it can be reduced to just a couple of times a day, and feedings will be replaced by full meals and healthy snacks.
Anyway, if you intend to continue to reduce breastfeeding, do it gradually, replacing one feeding at a time. Use formula milk if your baby is under 12 months old. With cow's milk, you should wait at least up to a year.
“When I decided to wean my son, I breastfed him three times a day and gave him other foods three times plus light snacks. Gradually, I replaced all breastfeedings with formula. By 11 months, we only had one nighttime breastfeed left,” says Ruth, a UK mom.
There are various ways to distract a child from changes in his diet. Some mothers suggest that instead of breastfeeding something to drink and eat together to maintain a sense of closeness. You can also change your daily routine, play your favorite game, or replace feeding with caresses - from you or from your partner. Some children take longer to get used to the new food, but in the end everything falls into place. If you are having difficulty weaning, ask your healthcare provider for advice.
Ending breastfeeding naturally
Ending breastfeeding can be guided by the baby's wishes. This is called baby-initiated weaning, or the natural termination of breastfeeding. Such a process is likely to be long and gradual. Month after month, feeding sessions will become shorter and less frequent, until one day the child completely loses interest in the breast.
“My daughter stopped breastfeeding on her own when she was four years old,” says Sarah, a mother from the UK. And once, when we were on vacation, she seemed to just forget about her breasts. Now, six months later, she sometimes still asks for breasts, but she already knows that there is no milk there.
You will have a huge amount of time for the body to adapt, so there should be no discomfort or swelling of the breast. However, you may find it difficult emotionally, so spend more time petting and bonding with your baby.
“Child-initiated termination of breastfeeding was right for me because I never gave my son formula or a bottle. I didn’t want to abruptly stop feeding and refuse him,” recalls Kelly, a mother from the UK, “He himself lost interest in breasts at the age of two and a half years. For us, it was the best scenario, although emotionally it was not very easy for me.”
I didn’t want to abruptly stop feeding and refuse him,” recalls Kelly, a mother from the UK, “He himself lost interest in breasts at the age of two and a half years. For us, it was the best scenario, although emotionally it was not very easy for me.”
What if you need to stop breastfeeding quickly?
It is best not to stop breastfeeding abruptly, but sometimes it is necessary for medical reasons or because you cannot be near the baby.
If you have been breastfeeding your baby up to this point, you will most likely have to express your milk to avoid breast swelling. Some mothers prefer to use a breast pump for this, others find it easier to express milk manually. You only need to pump a little, just to eliminate the discomfort, otherwise your body will take it as a signal to produce more milk.
At first, the breasts may swell and become tender, but this will pass. Breast milk contains a so-called feedback lactation inhibitor. When breastfeeding is stopped, this inhibitor tells your body to slow down milk production, but it can take days or even weeks for your breasts to rebuild.
Certain medications can relieve pain and should be discussed with your doctor. Always follow your pharmacist's instructions or directions, and consult your healthcare professional before taking any medication.
“I had to abruptly stop breastfeeding when my daughter was eight months old because she had to take strong painkillers,” says Peggy, a mother from Switzerland. “It was very difficult because the baby was constantly looking for a breast and crying. I held her tightly to me as I gave her a bottle. This calmed her, and after a month everything was all right.
Can I continue breastfeeding if I want to get pregnant again?
Breastfeeding is a natural contraceptive. However, this method is not the most reliable, especially after six months or if you are not exclusively breastfeeding. This means that you can get pregnant even while you are breastfeeding.
Pregnant and breastfeeding mothers sometimes receive conflicting advice about whether to stop breastfeeding. Consistent feeding of two children of different ages is of course possible, and with the advent of the second baby, your body will produce the kind of milk that both of them need.
Consistent feeding of two children of different ages is of course possible, and with the advent of the second baby, your body will produce the kind of milk that both of them need.
It is not uncommon for an older child to refuse to breastfeed or skip feedings if the mother is pregnant. This may be due to changes in milk composition that occur during pregnancy. Milk can change the taste and become less sweet. 6 If your baby is under one year of age when he starts to stop breastfeeding, make sure he continues to gain weight.
Talk to your doctor if you want to continue breastfeeding during pregnancy, but have had a preterm birth or miscarriage, or have any bleeding in the past.
If you need medical help to conceive, certain drugs and procedures may not be suitable while you are breastfeeding. Discuss all possible options before deciding to stop breastfeeding.
And finally...
Whenever you decide to end breastfeeding, and whatever method you choose to do so, be kind to yourself and your baby. This is a huge change for both of you physically, hormonally, and emotionally, so proceed thoughtfully and carefully.
This is a huge change for both of you physically, hormonally, and emotionally, so proceed thoughtfully and carefully.
“Although my body responded normally to stopping breastfeeding, it was psychologically difficult for me. The thing that united us for so long is over, - Jane, a mother of two children from the USA, shares her impressions, - I worked long hours, five days a week, and breastfeeding made me feel that I occupy a special place in the lives of children. But when it stopped, we soon found other ways to be together.”
Literature
1 World Health Organization. [Internet] Health Topics: Breastfeeding: 2018 [Accessed: 02/08/2018]. Available from : http://www.who.int/topics/breastfeeding/en - World Health Organization. "Health Issues: Breastfeeding" [Internet]. Geneva, Switzerland: WHO; 2018 [Visit 02/08/2018]. Article linked: http://www.who.int/topics/breastfeeding/e
2 Hassiotou et al. Maternal and infant infections stimulate a rapid leukocyte response in breastmilk. Clin Transl Immunology. 2013;2(4): e 3. - Hassiot F. et al., "Infectious diseases of the mother and child stimulate a rapid leukocyte reaction in breast milk." Clean Transl Immunology. 2013;2(4):e3.
Maternal and infant infections stimulate a rapid leukocyte response in breastmilk. Clin Transl Immunology. 2013;2(4): e 3. - Hassiot F. et al., "Infectious diseases of the mother and child stimulate a rapid leukocyte reaction in breast milk." Clean Transl Immunology. 2013;2(4):e3.
3 Dettwyler KA. When to wean: biological versus cultural perspectives. Clin Obstet Gynecol . 2004; 47(3)712-723. - Dettwiler KA, "Time to wean: weaning from a biological and cultural point of view". Klin Obstet Ginekol (Clinical obstetrics and gynecology). 2004; 47(3):712-723.
4 Victora CG Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet. 2016;387(10017):475-490. - Victor S.J. et al., "Breastfeeding in the 21st century: epidemiology, mechanisms and long-term effects". Lancet 2016;387(10017):475-490.
5 Dewey KG et al. Breast milk volume and composition during late lactation (7-20 months). J Pediatr Gastroenterol Nutr . 1984;3(5):713-720. — Dewey C.G. et al., "Amount and composition of breast milk in late lactation (7-20 months)". F Pediatrician Gastroenterol Nutr. 1984;3(5):713-720.
6 Prosser CG et al. Mammary gland function during gradual weaning and early gestation in women. Aust J Exp Biol Med 9021 9029 Sci. 1984;62( Pt 2):215-228. - Prosser S.G. et al., "Breast Function During Gradual Weaning and Early Gestation." Aust J Exp Biol Med Sai. 1984;62( Pt 2):215-228.
Different breastfeeding positions
Try different breastfeeding positions to find the one that works best for you and your baby. You can see the options in our selection of photos
You can see the options in our selection of photos
Share this information
There is no right or wrong way to hold the baby while feeding
, and mom and baby are sure to find their favorite position.
It is important that both you and your child feel comfortable. 1.2 It's good to learn a few different breastfeeding positions and techniques because life's circumstances often require us to be flexible, especially as your baby gets older and you start to leave the house more often.
Whatever position you choose to breastfeed your baby, remember a few simple rules.
- Prepare everything you need before feeding, including drinks, food, mobile phone, TV remote control, book or magazine. And do not forget to go to the toilet - the feeding process can take a long time!
- Make sure your baby is comfortable. Whichever position you choose, it's important to keep your baby strong, level, and provide good support for their head, neck, and spine.

- You should also be comfortable. Don't stress. If necessary, use pillows of different sizes or rolls of towels to support your back or arms.
- Make sure your baby is latching on correctly. Proper grip is the key to comfort when breastfeeding.
- If your baby does not latch well or you experience pain while feeding, contact a lactation consultant for help. The specialist will also be able to show you how to hold your baby more comfortably.
1. Relaxed feeding or reclining position
The relaxed feeding position, also known as biological feeding, 1 is often the first position for most mothers. If, immediately after birth, the baby is placed on the mother’s chest or stomach, normally, he instinctively reaches for the breast and tries to grab the nipple. This phenomenon is known as the breast seeking reflex. Skin-to-skin contact stimulates the infant's feeding instinct, and gravity helps him to latch onto the breast and maintain balance.![]()
But it's not just newborns that can be fed in the reclining position - this position is great for babies of all ages. It can be especially helpful if your baby does not latch well in other positions or does not like to be touched during feeding, and also if you have too much milk flow or too large breasts. Isabelle, a mother from the UK, shares her experience: “I had large breasts, and the baby was born small - 2.7 kg, so it was not easy to find a comfortable position at first. After a few weeks, it became clear that there was no “correct” posture for me. As a result, I most often fed lying down, putting the baby on my chest. ”
It is more convenient to feed not lying flat on your back, but half-sitting, leaning on pillows. So you will have a back support and you will be able to watch the baby during feeding.
2. Cradle position
This is the classic
first thought of breastfeeding. Mom sits straight
, and the baby lies on her side on her arm, pressing her stomach against her stomach. 3 Although this is a very popular position, it is not always easy to master with newborns because it gives the baby less support. Try putting a pillow under your back, and put a special breastfeeding pillow on your knees and lean on it with your hands. So you can more reliably support the child, without overstraining your back and shoulders. Just make sure that the baby does not lie too high on the pillow for feeding. The breast should remain at a natural level so that the baby can grab it without effort, otherwise sore nipples cannot be avoided.
3 Although this is a very popular position, it is not always easy to master with newborns because it gives the baby less support. Try putting a pillow under your back, and put a special breastfeeding pillow on your knees and lean on it with your hands. So you can more reliably support the child, without overstraining your back and shoulders. Just make sure that the baby does not lie too high on the pillow for feeding. The breast should remain at a natural level so that the baby can grab it without effort, otherwise sore nipples cannot be avoided.
“I breastfed in the cradle position because it suited me perfectly! It was comfortable and I loved just sitting and looking at my little one,” recalls Rachel, a mother of two from Italy.
3. Cross Cradle
This breastfeeding position looks almost the same as the Cradle, but the baby is on the other arm. 3 This gives your baby support around the neck and shoulders so he can tilt his head to latch on. This position is great for breastfeeding newborns and small babies, as well as for babies who do not latch well. Since the baby lies completely on the other hand, it becomes easier to control his position and you can adjust the chest with your free hand.
This position is great for breastfeeding newborns and small babies, as well as for babies who do not latch well. Since the baby lies completely on the other hand, it becomes easier to control his position and you can adjust the chest with your free hand.
Julie, a UK mother of two, finds this position very practical: “I usually breastfeed my youngest in the cross cradle position. So I have a free second hand, and I can take care of an older baby at the same time. ”
Do not hold the baby's head at first, otherwise you may inadvertently press his chin against his chest. Because of this, the child will not be able to take the breast deeply, because the nipple will rest against the base of the tongue, and not against the palate, which will lead to inflammation of the nipples. As the child grows, this position becomes more comfortable, and he can rest his head on your palm (as shown in the photo above).
4. Underarm breastfeeding
In this position, also known as the "ball grip", the mother sits and the baby lies along her arm at the side, legs towards the back of the chair (or any other seat). 3 Another comfortable position for newborn breastfeeding, you can give your baby good support, full control of his position and a good view of his face. And the baby feels safe in close contact with the mother's body. This position is especially good for those who have had a caesarean section or a premature birth, as well as mothers of twins and women with large breasts.
“When I breastfed my first daughter, I had very large K-sized breasts—twice the size of her head,” recalls Amy, an Australian mother of two. - I put rolls of towels under each breast, because they were very heavy, and fed my daughter in a pose from under the arm, but only sitting straighter so as not to crush her. This position was also convenient because I had a caesarean section and could not put the baby on my stomach.”
5. Side-lying position
The side-lying position is ideal for relaxed
feedings at night in bed or on the couch. If you had a
caesarean section or ruptures during childbirth, this position may be more comfortable than sitting down. 3 In this position, mother and baby lie side by side, tummy to tummy.
“It was difficult for me to sit during endless night feedings, firstly because of the caesarean section, and secondly because of lack of sleep,” recalls Francesca, a mother from the UK. “And then I discovered that you can feed your baby lying on your side and rest at the same time.”
“Because of the short tongue frenulum, Maisie could only properly latch on to her breasts while lying on her side. The lactation consultant showed me how it's done. In this position, the flow of milk was optimal for my daughter, and it was easier for her to keep the nipple in her mouth. As she got older, she became much better at grabbing her breasts in normal positions,” says Sarah, mother of two from Australia.
6. Relaxed breastfeeding after caesarean section
If you can't find a comfortable position for breastfeeding after caesarean section, 3 try holding the baby on your shoulder in a reclining position – this does not stress the postoperative suture and allows you to breastfeed your baby comfortably. You can also try side feeding.
You can also try side feeding.
7. Upright breastfeeding or “koala pose”
When breastfeeding in an upright position or “koala pose”, the baby sits with a straight back and a raised head on the mother's hip. 4 This position can be tried even with a newborn if it is well supported, but it is especially convenient for feeding a grown child who can already sit up by himself. The upright sitting position, or “koala pose,” is great for toddlers who suffer from reflux or ear infections and feel better sitting. In addition, this pose may be suitable for children with a shortened frenulum of the tongue or reduced muscle tone.
“When my daughter got a little older, I would often feed her in an upright position, which was more comfortable for both of us, and I could still hold her close,” recalls Peggy, a mother from Switzerland. “Besides, it was possible to discreetly breastfeed her in public places.”
8. Overhanging position
In this position, the baby lies on his back, and the mother bends over him
on all fours so that the nipple falls directly into his mouth.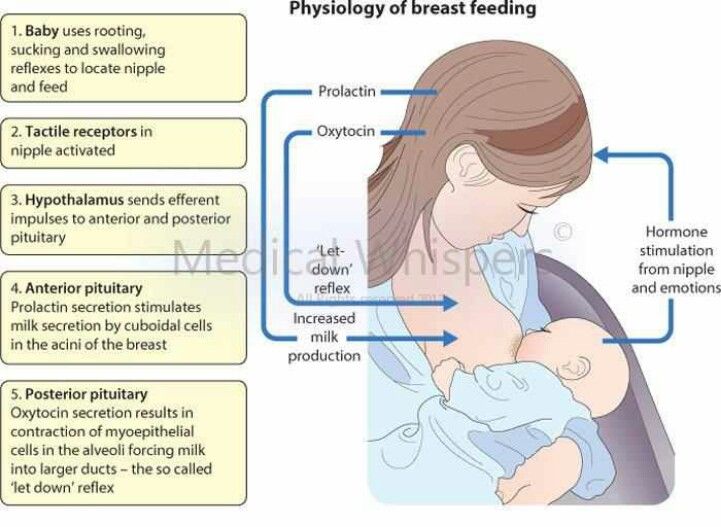 4 Some moms say this breastfeeding position is good to use occasionally for mastitis, when touching the breasts is especially unpleasant. Some say that this breastfeeding position helps with blockage of the milk ducts, although there is no scientific evidence for this yet. You can also feed in the “overhanging” position while sitting, kneeling over the baby on a bed or sofa, as well as reclining on your stomach with support on your elbows. Pillows of various sizes that you can lean on will help you avoid back and shoulder strain.
4 Some moms say this breastfeeding position is good to use occasionally for mastitis, when touching the breasts is especially unpleasant. Some say that this breastfeeding position helps with blockage of the milk ducts, although there is no scientific evidence for this yet. You can also feed in the “overhanging” position while sitting, kneeling over the baby on a bed or sofa, as well as reclining on your stomach with support on your elbows. Pillows of various sizes that you can lean on will help you avoid back and shoulder strain.
“I have breastfed several times in the 'overhang' position for clogged milk ducts when no other means of dissolving the blockage worked. And this pose seems to have helped. I think it's because of gravity, and also because the breasts were at a completely different angle than with normal feeding, and my daughter sucked her differently, ”says Ellie, a mother of two from the UK.
Feeding in the "overhanging" position is unlikely to be practiced regularly, but in some cases this position may be useful.
“I used to breastfeed in the overhang position when my baby was having trouble latch-on,” says Lorna, mother of two in the UK. - This, of course, is not the most convenient way, but then I was ready for anything, if only he could capture the chest. We succeeded and have been breastfeeding for eight months now!”
9. Feeding a baby in a sling or “on the fly”
Breastfeeding in a sling takes some practice, but it can be used to go out of the house, look after older children or even do a little household chores.
The sling is also useful if the baby does not like to lie down or is often attached to the breast. Lindsey, a mother of two in the US, notes: “I used the carrier frequently for both of my children. When we were out, I tied the sarong around my neck and covered the carrier with it. Under such a cape, the baby can eat as much as he wants until he falls asleep.
This breastfeeding position is best when the baby is already good at breastfeeding and can hold his head up by himself. Any slings are suitable for breastfeeding, including elastic and rings, as well as carrying bags. Whatever option you choose, the main thing is that you can always see the face of the child, and his chin does not rest against his chest.
Any slings are suitable for breastfeeding, including elastic and rings, as well as carrying bags. Whatever option you choose, the main thing is that you can always see the face of the child, and his chin does not rest against his chest.
10. Double hand-held breastfeeding
Double hand-held breastfeeding (or “double-ball grab”) is great for mothers of twins—you can breastfeed both at the same time and still have relatively free hands. 4 When feeding in this position, it is advisable to use a special pillow for breastfeeding twins, especially at first. It will provide extra support and help keep both babies in the correct position, as well as reduce the burden on the abdomen if you had a caesarean section. In addition, the hands are freer, and if necessary, you can deal with one child without interfering with the second.
“My twins were born very tiny and had to be fed every two hours at any time of the day or night. Very soon it became clear: if I want to do anything besides feeding, I need to feed them both at the same time, - says Emma, mother of two children from the UK. “I breastfed them two by hand using a breastfeeding pillow.”
“I breastfed them two by hand using a breastfeeding pillow.”
Other good positions for breastfeeding twins are two criss-cross cradles, one baby in the cradle and the other close at hand, reclining feeding, or sitting upright (one baby on one side, the other on the other).
11. Breastfeeding in the “hand-supported breast” or “dancer's hand” position
muscle tone (which is typical for premature babies, children suffering from various diseases or Down syndrome), try supporting his head and your chest at the same time. 4 Grasp your chest with your palm underneath so that your thumb is on one side and all the others are on the other. Move your hand slightly forward so that your thumb and forefinger form a "U" just in front of your chest. With the other three fingers, continue to support the chest. With your thumb and forefinger, hold the baby's head while feeding so that his chin rests on the part of the palm between them, your thumb gently holds the baby on one cheek, and your index finger on the other. So the baby gets excellent support, and you can control his position and see if he is holding his breast.
So the baby gets excellent support, and you can control his position and see if he is holding his breast.
Literature
1 Colson SD et al. Optimal positions for the release of primitive neonatal reflexes stimulating breastfeeding. Early Hum Dev . 2008;84(7):441-449. - Colson S.D. et al., "Optimal Positions for Provoking Primitive Innate Reflexes to Induce Breastfeeding." Early Hume Dev. 2008;84(7):441-449.
2 UNICEF UK BFHI [ Internet ]. Off to the best start ; 2015 [ cited 2018 Feb ]. - UNICEF UK, Baby-Friendly Hospital Initiative, Start the Best You Can [Internet]. 2015 [cited February 2018].
3 Cadwell K. Latching - On and Suckling of the Healthy Term Neonate: Breastfeeding Assessment.