Breast feeding and colic baby
Do Breastfed Babies Get Colic? | Parenting Blog | Babocush
Colic is extremely common, affecting between 10% and 40% of children, according to the American Academy of Family Physicians. Although there is no known cause for colic, there are several breastfeeding-related conditions that may play a role in the symptoms. Some things you should know about breastfeeding a colicky baby and how to get through the first few months are listed below.
What Is Colic?
When your baby seems perfectly healthy, has no obvious signs of distress and yet cries continually, they may be suffering from colic. Colic is prolonged bouts of excessive, frequent crying for no apparent reason, although some abdominal discomfort is thought to accompany it due to the way many babies draw their knees up when they cry which would indicate trapped wind. These episodes can be very distressing for both baby and parent, and can last for several weeks.
Mother's Diet & Breast Milk
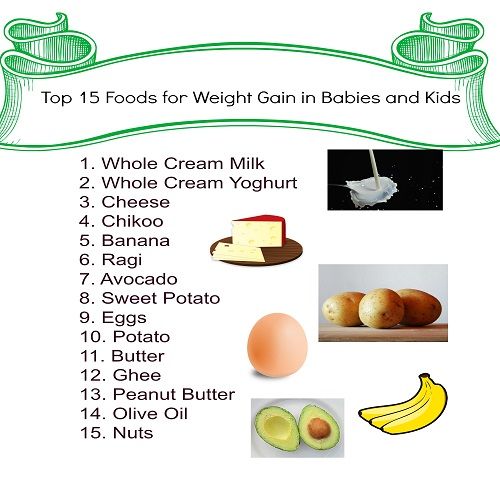
Although the precise cause of colic is unclear, several factors are believed to play a role, including the maternal diet. Through your breast milk, the foods you eat find their way to your little one. Certain substances can cause a reaction or an allergy in some babies. The most popular perpetrators are cow's milk and dairy products, which may trigger digestive issues that result in colic or colic-like symptoms.
You can try to remove dairy products from your diet to see if the colic improves. Nuts, soy, eggs, caffeine, garlic, spicy foods, and shellfish are all foods that your baby may react too. When you remove foods from your allow for up to a week for any changes to occur. Also inquire about probiotics with your doctor. Studies have shown that lactobacillus reuteri, a probiotic, has been shown to help alleviate colic in breastfed infants.
Overactive Let-Down
An overactive let-down may also be a cause of colic. When your milk flows rapidly and vigorously from your breast into your baby's mouth, they’d have to gulp at speed to keep up with the flow. When a baby is feeding, they’re also swallowing a lot of air. Gas and stomach pain can be caused by trapped air in the stomach and intestines.
Gas and stomach pain can be caused by trapped air in the stomach and intestines.
You will alleviate the pressure in your breast and reduce the initial forceful let-down by pumping to withdraw a small amount of breast milk before you feed. Then, when your milk flow has decreased, you can start feeding your baby. Breastfeeding in a reclined position, such as lying on your back or sitting back in a chair, will also help to slow the flow of your breast milk.
Overabundant Supply
Colic may also be caused by an overabundance of breastmilk. Your baby could be consuming too much foremilk if you have an abundance of milk. The thinner milk that flows from the breast at the start of a feeding is known as foremilk. It has a higher lactose, or milk sugar, content. When a baby breastfeeds, the foremilk eventually converts into hindmilk, which is creamier and more filling.
However, if there is an overabundance of foremilk, the baby can consume it before receiving enough hindmilk. This is known as a foremilk-hindmilk imbalance, and it can result in gas, loose green bowel movements, and colic symptoms.
This is known as a foremilk-hindmilk imbalance, and it can result in gas, loose green bowel movements, and colic symptoms.
Breastfeeding from just one breast at a time will ensure that your baby receives both foremilk and hindmilk at each feeding. Your baby is more likely to get foremilk from both sides if you have an overabundant milk supply and swap breasts during feeding.
However, if you only breastfeed on one breast the whole time, your child is more likely to hit the hindmilk as that breast is completely drained. If required, you can also pump from the other breast.
Coping with a baby who has colic
There is no clear remedy for colic since the exact cause is unknown. That isn't to suggest there isn't something you can do about it but keep in mind that what works for one baby might not work for another. Furthermore, what works one day might not work the next. Dealing with colic necessitates a certain amount of trial and error. Here are a few things you can do to help:
Babies cry. It’s how they communicate. But, when your baby cries uncontrollably, and nothing you do can console them, it can be frustrating, stressful, and heartbreaking. All of these feelings are normal. Colic isn’t your fault (or your baby's), and you’re not a bad parent. In fact, many other parents are in the same boat.
It’s how they communicate. But, when your baby cries uncontrollably, and nothing you do can console them, it can be frustrating, stressful, and heartbreaking. All of these feelings are normal. Colic isn’t your fault (or your baby's), and you’re not a bad parent. In fact, many other parents are in the same boat.
You can only do what you can to try to soothe your child. They know you are there for them. Remind yourself to stop and take a break when you need it. It may seem like it’s never going to get better. And, when you're in the thick of it, a few weeks can feel like years. But, thankfully, colic does go away, sometimes as suddenly as it arrived. You’ll get there. It just takes a little time, love, and patience!
Related Blogs:
- Help and Advice on Dealing With Infant Colic
- How to soothe a colicky baby with Babocush
Colic | Breastfeeding Challenges | Start for Life
There may be times when breastfeeding is challenging. Never ignore any issues you may have – talk to your health visitor, midwife, GP or breastfeeding specialist as soon as possible, they will be able to help you sort it out quickly.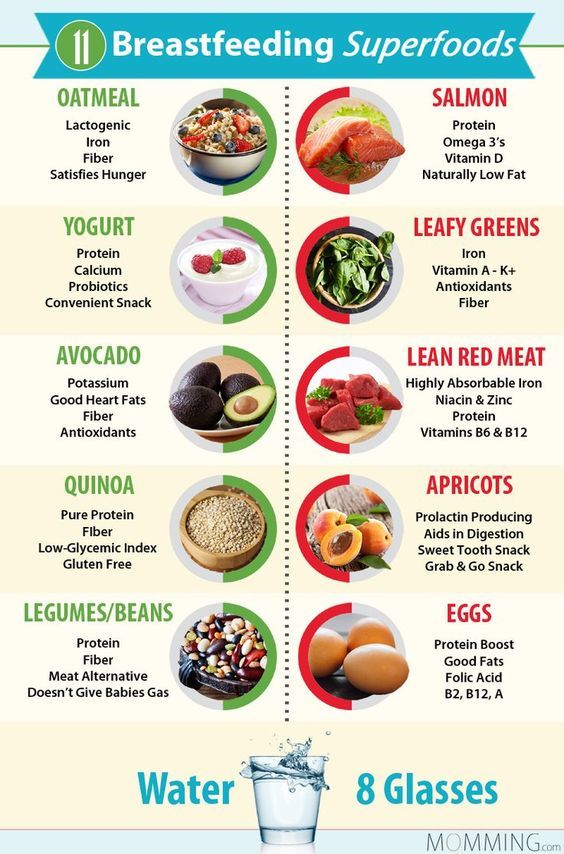
Here are some common breastfeeding issues, and tips on what to do.
There are other reasons why your baby may be crying, it's a good idea to check if they:
- are hungry
- have a dirty or wet nappy
- have wind
- are too hot or too cold
- are bored or overstimulated
If your baby tends to cry during or after feeds, it's worth checking whether this could be reflux. Our guide to reflux in breastfed babies has information on the signs and symptoms.
What causes colic?
There are no known reasons why some babies get colic &ndash some doctors think it's a type of stomach cramp. But it may happen because babies find it harder to digest food when they are really young.
Constant crying could also be due to food allergies, such as cow's milk allergy. If you think this is the case, talk to your GP before making any changes to your baby's diet.
Colic remedies for breastfed babies
Sadly, there is no actual cure for baby colic, only methods to provide relief and soothe them. These are some of the tried and tested techniques that other parents use to relieve colic symptoms in breastfed babies:
These are some of the tried and tested techniques that other parents use to relieve colic symptoms in breastfed babies:
Burping
Burp (or wind) your baby during and after every feed – have a look at burping your baby for techniques.
Sit your baby up
When breast or bottle feeding, sit your baby up as straight as possible. This will help minimise the amount of air they swallow. If you are bottle feeding, try to make sure the milk fills the teat and there are no air pockets – you could try using an anti-colic bottle to see if that helps.
Attachment
Check that your baby is attached (latching on) properly as this may help reduce colic symptoms. If you are unsure that your baby is attaching properly while breastfeeding, have a look at our guide to latching on.
Diet
There is no evidence that changing your diet will help &ndash however some people say that cutting down on spicy foods, caffeine and acohol has made a difference for them.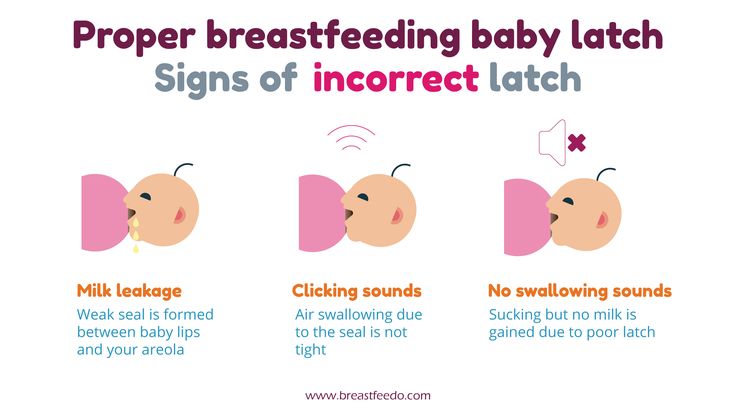
If you are mixed feeding (combining breast and bottle feeding), have a look at our guide to colic when bottle feeding.
Other ways to soothe your baby
Hold them
During bouts of crying, hold your baby to your chest so they can feel and hear your heartbeat.
Rock your baby
Sometimes the swaying motion of rocking your baby in your arms can help.
Warm bath and a massage
A warm bath can be soothing, followed by a gentle tummy massage (with gentle, circular strokes on the tummy).
Create a calming atmosphere
Babies can become overstimulated with lots of noise and activity around them. Try to quieten your surroundings, switch the TV off, dim the lights, and try to take some deep breaths yourself.
Diet changes for colic in infants
Review question
Do infants with colic improve if breastfeeding mothers follow a hypoallergenic diet and use special formulas when formula-fed?
Relevance
Infantile colic is a common problem affecting otherwise healthy babies in the first three months of life.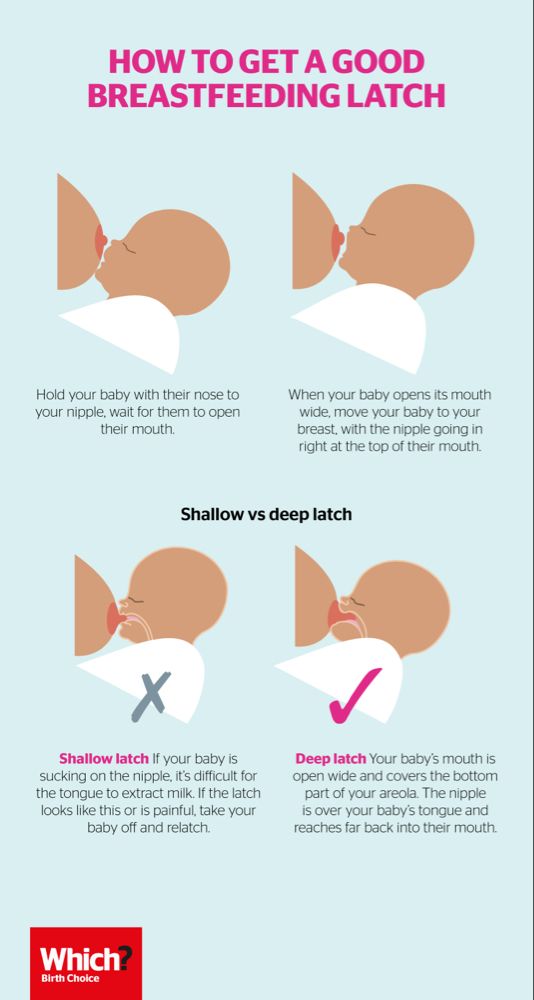 They are characterized by bouts of inconsolable crying for more than three hours a day, more than three days a week, for at least three weeks. nine0005
They are characterized by bouts of inconsolable crying for more than three hours a day, more than three days a week, for at least three weeks. nine0005
This can be distressing for parents.
Diet changes, such as eliminating cow's milk from breastfeeding mothers or switching to artificial soy formula, may relieve symptoms of colic in infants.
Study profile
We found 15 randomized controlled trials in which 1121 infants with colic were randomly assigned to one of two or more treatment groups. The evidence is current to July 2018. nine0005
Infants (both boys and girls) were less than 3 months old.
Main results
Most studies reported data on a combination of outcomes: duration of crying, number of participants in each post-intervention group (ie those who experienced a reduction in daily crying duration), or frequency of crying episodes. No studies reported on parental or family quality of life, infant sleep, or parental satisfaction. Six studies reported no side effects as a result of dietary changes. nine0005
Six studies reported no side effects as a result of dietary changes. nine0005
Hypoallergenic diet
In one study (90 infants), more infants were found to respond to a hypoallergenic diet of lactating mothers than to a standard diet with known potential allergens.
One study (120 infants) found little difference between breastfed infants whose mothers were on a hypoallergenic diet (10/16; 62.5%) and formula-fed infants fed soy milk (29/44; 65.9%. However, researchers found that breastfed infants responded more to dicyclomine hydrochloride (a tablet used to treat stomach cramps) than formula-fed infants.
Hydrolyzed milk formula
In 2 studies (64 infants), no difference was found in crying time between the hydrolyzed (hypoallergenic) and regular cow's milk groups. One of these studies (43 infants) reported a greater reduction in crying time by the end of the study in infants fed hydrolyzed milk. nine0005
A third study (22 infants) showed that two types of hydrolysed formulas were equally effective in resolving colic symptoms in infants starting with standard formula.
In the fourth study (21 infants), infants whose parents received information and support were reported to have reduced crying time faster than infants fed hydrolysed formulas or milk and soy-free formulas (for 9 days).
In the fifth study (267 infants), hydrolyzed formula with oligosaccharides (carbohydrates) and standard formula with simethicone (a medicine to treat symptoms of gas) were found to reduce the number of episodes of colic after 7 days. However, after 2 weeks, the effects were more pronounced in the hydrolyzed mixture with oligasaccharides group. nine0005
Addition of lactase enzyme
Three studies (138 infants) evaluated the effect of adding lactase (an enzyme that helps break down lactose (sugar) in milk) to infant milk. The results were presented in a form that did not allow analysis.
Fennel, chamomile and lemon mint extracts
One study (93 infants) found that average daily crying in infants was reduced within one week of treatment with fennel extract, chamomile and lemon balm. nine0005
nine0005
Soy Protein Blend
One study (19 infants) found that compared to cow's milk formula, soy formula reduced crying time and increased the number of babies that responded to dietary changes. However, international guidelines do not support the use of soy milk due to concerns that it may affect the hormonal balance of children, and therefore these results are not relevant.
One study (27 infants) compared soy formula with oligosaccharides (carbohydrates) to soy formula without additives, but the results were presented in a form that did not allow analysis. nine0005
Quality of evidence
Many studies included only small numbers of participants and were of poor quality. We found no evidence for the effectiveness of most dietary interventions. When studies reported any benefit, it was not significant enough.
Terminals
Based on the available evidence, we cannot recommend any of the dietary changes assessed in this review.
Translation notes:
Translation: Kim Alina Valievna. Editing: Kukushkin Mikhail Evgenievich. Project coordination for translation into Russian: Cochrane Russia - Cochrane Russia (branch of the Northern Cochrane Center on the basis of Kazan Federal University). For questions related to this translation, please contact us at: [email protected]; [email protected]
Infant colic and breastfeeding - is there a link? | Zhdanova
1. Barr R.G., St. James-Roberts I., Keefe M/R. New evidence on unexplained early infant crying: its origins, nature and management. Skillman, NJ: Johnson & Johnson Pediatric Institute; 2001.
2. Treem W.R. Infant colic. A pediatric gastroenterologist's perspective. Pediatric Clin North Am. 1994;41:1121–1138.
3. Shamir R. Infant colic and functional gastrointestinal disorders: is there more than a “gut feeling”? J Pediatr Gastroenterol Nutr. 2013;57:S1–S2.
4. Barr R.G., Young S.N. , Wright J.H., Gravel R., Alkawaf R. Differential calming responses to sucrose taste in crying infants with and without colic. Pediatrics. 1999;103:e68.
, Wright J.H., Gravel R., Alkawaf R. Differential calming responses to sucrose taste in crying infants with and without colic. Pediatrics. 1999;103:e68.
5. Lester B.M., Boukydis C.Z., Garcia-Coll C.T., Hole W.T. Colic for developmentalists. Infant Ment Health J.1990;11:321–333.
6. DeSantis A., Coster W., Bigsby R., Lester B. Colic and fussing in infancy, and sensory processing at 3 to 8 years of age. Infant Ment Health J. 2004;25:522–539.
7. Milidou I., Sondergaard C., Jensen M.S., Olsen J., Henriksen T.B. Gestational age, small for gestational age, and infantile colic. Paediatr Perinat Epidemiol. 2014;28:138–145.
8. Douglas P., Hill P. Managing infants who cry excessively in the first few months of life. BMJ. 2011;343:d7772. nine0005
9. Talge N.M., Neal C., Glover V. Early Stress, Translational Research and Prevention Science Network: Fetal and Neonatal Experience on Child and Adolescent Mental Health. Antenatal maternal stress and long term effects on child neurodevelopment: how and why? J Child Psychol Psychiatry. 2007;48:245–261.
2007;48:245–261.
10. van den Berg M.P., van der Ende J., Crijnen A.A., Jaddoe V.W., Moll H.A., Mackenbach J.P. et al. Paternal depressive symptoms during pregnancy are related to excessive infant crying. Pediatrics. 2009;124:e96–e103.
11. Indrio F., Riezzo G., Raimondi F., Di Mauro A., Francavilla R. Gut motility alterations in neonates and young infants. J Pediatr Gastroenterol Nutr. 2013;57:S9–S11.
12. Gupta S.K. Is colic a gastrointestinal disorder? Curr Opin Pediatr. 2002;14:588–592.
13. Rhoads J.M., Fatheree N.Y., Norori J., Liu Y., Lucke J.F., Tyson J.E. et al. Altered fecal microflora and increased fecal calprotectin in infants with colic. J Pediatr. 2009;155:823–828.e1. nine0005
14. de Weerth C., Fuentes S., Puylaert P., de Vos W.M. Intestinal microbiota of infants with colic: development and specific signatures. Pediatrics. 2013;131:e550–e558.
15. Nooitgedagt J.E., Zwart P., Brand P.L. Causes, treatment and clinical outcome in infants admitted because of excessive crying to the pediatric department of the Isala clinics, Zwolle, the Netherlands, 1997/’03. Ned Tijdschr Geneeskd. 2005;149:472–477.
Ned Tijdschr Geneeskd. 2005;149:472–477.
16. Lucassen P.L., Assendelft W.J., Gubbels J.W., van Eijk J.T., van Geldrop W.J., Neven A.K. Effectiveness of treatments for infantile colic: systematic review. BMJ. nineteen98;316:1563–1569.
17. St James-Roberts I., Halil T. Infant crying patterns in the first year: normal community and clinical findings. J Child Psychol Psychiatry. 1991;32:951–968.
18. Barr R.G. The normal crying curve: what do we really know? Dev Med Child Neurol. 1990;32:356–362.
19. Freedman S.B., Al-Harthy N., Thull-Freedman J. The crying infant: diagnostic testing and frequency of serious underlying disease. Pediatrics. 2009;123:841–848.
20. Shamir R., St James-Roberts I., Di Lorenzo C., Burns A.J., Thapar N., Indrio F. et al. Infant crying, colic, and gastrointestinal discomfort in early childhood: a review of the evidence and most plausible mechanisms. J Pediatr Gastroenterol Nutr. 2013;57(Suppl 1):S1–S45. nine0005
21. Wessel M. A., Cobb J.C., Jackson E.B., Harris G.S., Jr, Detwiler A.C. Paroxysmal fussing in infancy, sometimes called colic. Pediatrics. 1954;14:421-35.
A., Cobb J.C., Jackson E.B., Harris G.S., Jr, Detwiler A.C. Paroxysmal fussing in infancy, sometimes called colic. Pediatrics. 1954;14:421-35.
22. Benninga M.A., Nurko S., Faure C., Hyman P.E., St. James Roberts I., Schechter N.L. Childhood functional gastrointestinal disorders: neonate/ toddler. gastroenterology. 2016;150:1443–1455.
23. Drossman D.A. Functional gastrointestinal disorders: history, pathophysiology, clinical features and Rome IV. gastroenterology. 2016;150:1262–1279.e2.
24. Rasquin-Weber A., Hyman P.E., Cucchiara S., Fleisher D.R., Hyams J.S., Milla P.J. et al. Childhood functional gastrointestinal disorders. gut. 1999;45(Suppl 2):II60–II68.
25. Drossman D.A. The functional gastrointestinal disorders and the Rome III process. gastroenterology. 2006;130:1377–1390.
26. Hyman P.E., Milla P.J., Benninga M.A., Davidson G.P., Fleisher D.F., Taminiau J. Childhood functional gastrointestinal disorders: neonate/toddler. gastroenterology. 2006;130:1519–1526.
2006;130:1519–1526.
27. Rasquin A., Di Lorenzo C., Forbes D., Guiraldes E., Hyams J.S., Staiano A. et al. Childhood functional gastrointestinal disorders: child/adolescent. gastroenterology. 2006;130:1527–1537.
28. Barr R.G. Excessive crying. In: Sameroff A.J., Lewis M., Miller S.M., editors. Handbook of developmental psychopathology. 2nd ed. New York: Kluwer Academic/Plenum Publishers; 2000:327–350.
29. Wolke D. Behavioral treatment of prophylactic infant crying: evaluation, methods, and a proposal. In: Barr R.G., St. James-Roberts I., Keefe M.R., editors. New evidence on unexplained early infant crying: its origins, nature and management. Skillman, NJ: Johnson & Johnson Pediatric Institute; 2001:187–208. nine0005
30. Savino F., Ceratto S., De Marco A., Cordero di Montezemolo L. Looking for new treatments of Infantile Colic. Ital J Pediatr. 2014 Jun 5;40:53. Epub 2014 Jun 5.
31. Howard C.R., Lanphear N., Lanphear B.P., Eberly S., Lawrence R.A. Parental responses to infant crying and colic: the effect on breastfeeding duration. Breastfeed Med. 2006;1:146–55.
Breastfeed Med. 2006;1:146–55.
32. Callahan S., Sejourne N., Denis A. Fatigue and breastfeeding an inevitable relationship. J Hum Lact. 2006;22:182–7. nine0005
33. Sacco L.M., Caulfield L.E., Gittelsohn J. et al. The conceptualization of perceived insufficient milk among Mexican mothers. J Hum Lact. 2006;22:277–86.
34. Stifter C.A., Bono M. Parent characteristics and conceptualizations associated with the emergence of infant colic. J Reprod Infant Psychol. 2003;21:309–22.
35. Nevo N., Rubin L., Tamir A., Levine A., Shaoul R. Infant feeding patterns in the first 6 months: an assessment in full-term infants. J Pediatr Gastroenterol Nutr. 2007;45:234–9.
36. Aktas S., Kucuk Alemdar D. Correlation between Infantile Colic and Maternal Breastfeeding Self-Efficacy, Breastfeeding Success and Breast Milk Amount. JTrop Pediatrician. 2018 Aug 21. Epub ahead of print.
37. Saavedra M.A., Dacosta J.S., Garcias G. et al. Infantil colic incidence and associated risk factors: a cohort study. J Pediatr. 2003;79:115–22.
J Pediatr. 2003;79:115–22.
38. Evans K., Evans R., Simmer K. Effect of the method ofbreastfeeding on breast engorgement, mastitis and infantile colic. Acta Paediatr. nineteen95;84:849–52.
39. Cohen Engler A., Hadash A., Shehadeh N. et al. Breastfeeding may improve nocturnal sleep and reduce infantile colic: potential role of breast milk melatonin. Eur J Pediatr. 2012;171:729–32.
40. Sung V. Infantile colic. Aust Presc. 2018 Aug;41(4):105–110.
41. Salvatore S., Abkari A., Cai W., Catto-Smith A., Cruchet S., Gottrand F., Hegar B., Lifschitz C., Ludwig T., Shah N., Staiano A., Szajewska H., Treepongkaruna S., Vandenplas Y. Review shows that parental reassurance and nutritional advice help to optimize the management of functional gastrointestinal disorders in infants. Acta Pediatrica. 2018 May 25;107(9):15121520.
42. Steuerwald M.R. Review of the therapeutic use of simethicone in gastroenterology. Schweizerische Zeitschrift fur Ganzheits Medizin.