Breast feeding baby not latching on
When Your Baby Has Trouble Latching on or Sucking
Nationwide Children’s Hospital
Babies must be able to effectively remove milk from the breast during breastfeeding if they are to obtain enough milk to gain weight and “tell” the breasts to increase or maintain milk production. When they can’t, milk production decreases, resulting in poor weight gain.
It is important to recognize the signs that a baby is unable to effectively remove milk during breastfeeding so that steps can be taken to remedy any problem. Signs of a baby’s ineffective sucking may include the following:
-
Does not wake on cue for feedings eight or more times in 24 hours
-
Cues to feed 14 or more times in 24 hours
-
Latches on and then lets go of the breast repeatedly
-
Falls asleep within five minutes of latching on or after sucking for only two or three minutes
-
Feeds for more than 45 minutes without acting satisfied or full after a meal
-
Produces fewer than three stools in 24 hours by the end of the first week (for the first four to eight weeks)
-
Produces fewer than six soaking wet diapers in 24 hours by the end of the first week
When a difficulty with latching on or sucking persists beyond the first several days after birth, it can be discouraging. But stay positive—most babies will learn to breastfeed effectively if given time. Until the issue resolves; however, work with your baby’s pediatrician and a certified lactation consultant, and take these steps to make sure your baby is getting enough to eat:
-
Wake your baby to breastfeed every two to three hours if he or she is sleepy and still has not mastered feeding cues.
-
Massage your breast with downward and inward strokes to deliver milk into your baby’s mouth when he or she begins to fall asleep at the breast too soon after starting to feed.
-
Use a hospital-grade, electric breast pump to ensure milk removal. Express milk for several minutes after breastfeeding.
-
Offer additional calories by giving baby any expressed breast milk available first or a prescribed infant formula based on his or her progress at breast.
-
Make skin-to-skin contact with your baby.
 This seems to help babies get to the breast more effectively, sooner, and it helps you maintain milk production.
This seems to help babies get to the breast more effectively, sooner, and it helps you maintain milk production. -
Try pumping one breast while breastfeeding your baby on the other when your baby has the basic idea of effective sucking but cannot seem to do it consistently.
-
Get support. Contact a representative of a breastfeeding support organization, who will have lots of information and will provide you with moral support whenever you need it.
Online Medical Reviewer: Louise Jovino, DO
Date Last Reviewed: 4/6/2010
© 2000-2018 The StayWell Company, LLC. 800 Township Line Road, Yardley, PA 19067. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.
© 2000-2018 The StayWell Company, LLC. 800 Township Line Road, Yardley, PA 19067. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.
This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.
- Breastfeeding Best Bet Against Baby Allergies
- Breastfeeding May Keep Babies from Inheriting Food Allergies
- Breastfeeding Quiz
- Breastfeeding Your Premature Infant at Home
- High-Risk Newborns and Low Milk Production
- How Long Should You Breastfeed?
- Is Your Baby Getting Enough Milk?
- Your Baby’s Nutrition in the First Few Days
Show More
Difficulty with Latching On or Sucking
A baby must be able to remove enough milk from the breast during breastfeeding to gain weight and "tell" the breasts to increase or maintain milk production. If the baby does not get enough milk, he or she will have poor weight gain. Also, the amount of milk being made for the baby will decrease.
If the baby does not get enough milk, he or she will have poor weight gain. Also, the amount of milk being made for the baby will decrease.
A baby's ability to suck and remove milk may be affected in different ways. Prematurity, labor and delivery medicine, and conditions such as Down syndrome may initially make it difficult for a baby's central nervous system to remain alert or coordinate suck-swallow-breathe actions. Acute health conditions, such as jaundice or infection and chronic conditions, such as cardiac defects may also influence a baby's level of alertness or the ability to suck. A "mechanical" issue, such as tongue-tie or a cleft lip or palate might directly interfere with a baby's ability to use the structures in the mouth for effective sucking.
Sometimes, the cause is obvious, but often it is not. However, it is important to recognize the signs that a baby is unable to effectively remove milk during breastfeeding so that steps can be taken to remedy any problem. Signs of ineffective sucking may include the following:
Signs of ineffective sucking may include the following:
The baby who consistently:
Does not wake on his or her own to cue for feedings.
Cues fewer than 8 times in a 24-hour period.
Cues to feed 14 or more times in a 24-hour period.
Latches on and then lets go of the breast repeatedly.
Pushes away or resists latch-on.
Falls asleep within 5 minutes of latch-on or after sucking for only two or three minutes.
Does not suck almost continuously for the first seven to 10 minutes of a feeding.
Nurses on one side for longer than 30 to 40 minutes.
Feeds for more than 45 minutes without acting satisfied or full after a meal.
Produces fewer than 3 to 4 stools in 24 hours (3 to 4 stools per day is normal for a baby who is more than one week old and younger than one month).
Seems "gassy" or produces green, frothy stools after the first week.
Produces fewer than 6 wet diapers in 24 hours (a baby produces 6 wet diapers a day by the end of the first week).
Has difficulty taking milk by other alternative feeding methods.
The mother who:
Has persistently sore or bruised nipples or areola.
Develops red, scraped or cracked nipples.
Often observes misshapen nipples after feedings (for example, creasing or flattening).
Rarely or never notices breast fullness prior to nursing and breast softening after nursing, especially if there are several hours between feedings.
Experiences more than one episode of plugged milk ducts or mastitis.
How you can help with the breastfeeding process
When a difficulty with latch-on or sucking persists beyond the first several days after birth, it can be discouraging. Although most babies will learn to breastfeed effectively if given time, it is important to work with the baby's healthcare provider and a certified lactation consultant (IBCLC) if a baby has difficulty sucking. Until the issue resolves there are several things you can do to help breastfeeding progress while you make sure your baby is getting enough to eat. Always talk with your baby's healthcare provider for more information:
Until the issue resolves there are several things you can do to help breastfeeding progress while you make sure your baby is getting enough to eat. Always talk with your baby's healthcare provider for more information:
Wake the baby to breastfeed every 2 to 3 hours if he or she is sleepy and still has not mastered feeding cues.
Your baby probably will do better for some feedings. Do not be discouraged if he or she is too sleepy or seems to forget from feeding to feeding.
Some feedings will last longer than others. Your baby may need time to "get going" at the breast for some feeds.
Massage your breast with downward and inward strokes (or use one hand to gently squeeze the breast) to deliver milk into the baby's mouth when he or she is nursing. This is also helpful when your baby begins to fall asleep at the breast too soon after starting to feed.
Chart the number, amount, and color of urine and stools for wet and dirty diapers on a daily record.

Use a hospital-grade, electric breast pump to ensure complete milk removal. Many women will express milk by pumping for several minutes after breastfeeding. How long you will need to continue to pump depends on how quickly your baby learns to breastfeed effectively. Also, how much milk your baby needs to grow beyond what you are providing with breastfeeding.
Weigh the baby regularly or record a test-weight before and after a feeding. This is best done at the office of a lactation consultant or the baby's healthcare provider with a medical-grade scale.
Offer additional calories by giving baby expressed breast milk in a bottle as instructed by your baby's healthcare provider.
Certain breastfeeding devices or alternative feeding methods may encourage effective sucking or provide your baby with additional nutrition during the "learning to breastfeed" process. Although a specific device may have advantages for your situation, every device also has disadvantages.
 To avoid pitfalls, any breastfeeding device should be used with the guidance of a certified lactation consultant (IBCLC) or healthcare provider with advanced knowledge of breastfeeding. Devices that may be helpful in certain situations include the following:
To avoid pitfalls, any breastfeeding device should be used with the guidance of a certified lactation consultant (IBCLC) or healthcare provider with advanced knowledge of breastfeeding. Devices that may be helpful in certain situations include the following:Nipple shield. A thin silicone or latex nipple shield, which is centered over the nipple and areola, has been shown to encourage a better latch, more effective sucking pattern, and better milk intake during breastfeeding for certain babies.
Feeding tube system. A feeding-tube system may be taped to the breast or your finger so that a baby receives additional milk through the tube when the baby sucks. When a thin feeding tube is attached to a syringe and taped to the breast or your finger (finger-feeding), you or a helper can gently press the plunger to deliver a few drops of milk in the baby's mouth if the baby "forgets" to suck. Commercial feeding-tube systems are also available.
Alternative feeding methods.
 In addition to a feeding-tube system, there are other alternative feeding methods that will ensure that your baby gets enough food, yet are less likely to interfere with long-term breastfeeding. These include cup-feeding, syringe-feeding, spoon-feeding, or (eye) dropper-feeding. If using a bottle, bottle nipples (teats) with a slower rate of flow usually are preferred.
In addition to a feeding-tube system, there are other alternative feeding methods that will ensure that your baby gets enough food, yet are less likely to interfere with long-term breastfeeding. These include cup-feeding, syringe-feeding, spoon-feeding, or (eye) dropper-feeding. If using a bottle, bottle nipples (teats) with a slower rate of flow usually are preferred.
If any structural variation in the baby's mouth is found, work with the proper healthcare professionals to correct or treat it. Depending on the type of variation, this may involve anything from oral exercises to some type of surgical treatment.
Other ways to help the baby with ineffective sucking
Other hints for the baby include the following:
Skin-to-skin contact seems to help a lot of babies with nursing. This also helps you maintain milk production.
When a baby has the basic idea of effective sucking but cannot seem to do it consistently, try pumping one breast while breastfeeding your baby on the other.

You may want to limit breastfeeding duration if you or your baby get too frustrated or if the feedings take more than 40 to 45 minutes. By stopping when frustrated or limiting the time of feedings, you will have more time to pump and remove milk effectively. You may find it is easier to remain patient through the learning process. You can always express milk and give it by an alternative feeding method.
You may want to let the baby's father or other family members and friends handle alternative feedings, so you do not become overwhelmed. This frees you to concentrate on breastfeeding, maintain pumping sessions, and enjoy periods of cuddling skin-to-skin with your baby.
Do not throw away any breastfeeding device or an alternative feeding method because you did not like it or it did not work when first suggested. The device or method that did not help one day may work great the next and vice versa.
Once your baby is growing and developing properly and his or her nutritive sucking ability is improving, ask your baby's healthcare provider when you can stop waking him or her for feedings and begin to wait to see if he or she will demonstrate feeding cues.
 You will also want to know when it is safe to start decreasing supplementary breast milk or formula.
You will also want to know when it is safe to start decreasing supplementary breast milk or formula.Keep thinking positively. It is normal to get frustrated and think your baby will never learn to breastfeed effectively. It is normal if some days seem an eternity of breastfeeding practice, alternative feedings, and breast pumping sessions. It is normal for your confidence to rise and fall. Try to maintain perspective by having a sense of humor. Think about how far your baby and you have come since his or her birth rather than how far you still may have to go.
Get support. In addition to staying in touch with your healthcare provider and a certified lactation consultant (IBCLC), contact a representative of a breastfeeding support organization. He or she will have lots of information and will provide you with moral support whenever you need it.
Solutions to six breastfeeding problems in the first week
Are you having difficulty breastfeeding your newborn baby? Read on for expert advice on tackling the main challenges of the first week of breastfeeding.
Share this information
Cathy Garbin, child health nurse, midwife and lactation consultant:
Cathy, a mother of two, was a research fellow at the renowned Human Lactation Research Institute, founded by Peter Hartmann, for seven years, providing support to breastfeeding mothers in clinics and at home. Today, she still works as a family counselor, and also conducts seminars for attending physicians and speaks at international conferences.
Breastfeeding is not always easy, so if
you are having difficulty, know that you are not alone. A US study found that out of 500 new mothers surveyed, 92% experienced breastfeeding problems by the third day. 1 Fortunately, most early breastfeeding problems are easy to resolve. Below you can read recommendations for solving the main problems that mothers often face in the first week of feeding.
Problem #1. Breastfeeding hurts!
Pain during feeding is usually associated with tenderness or inflammation of the nipples, especially when milk "comes" on the second to fourth day after birth.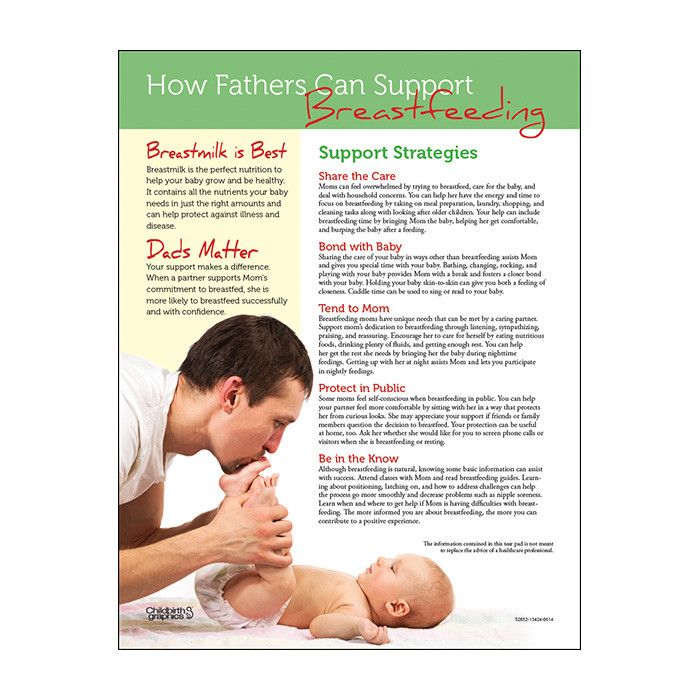 2 The baby will beg for a breast every couple of hours, and this can quickly aggravate the problem: some mothers' nipples crack, bleed, or blister. This is, of course, very annoying.
2 The baby will beg for a breast every couple of hours, and this can quickly aggravate the problem: some mothers' nipples crack, bleed, or blister. This is, of course, very annoying.
Solutions 3
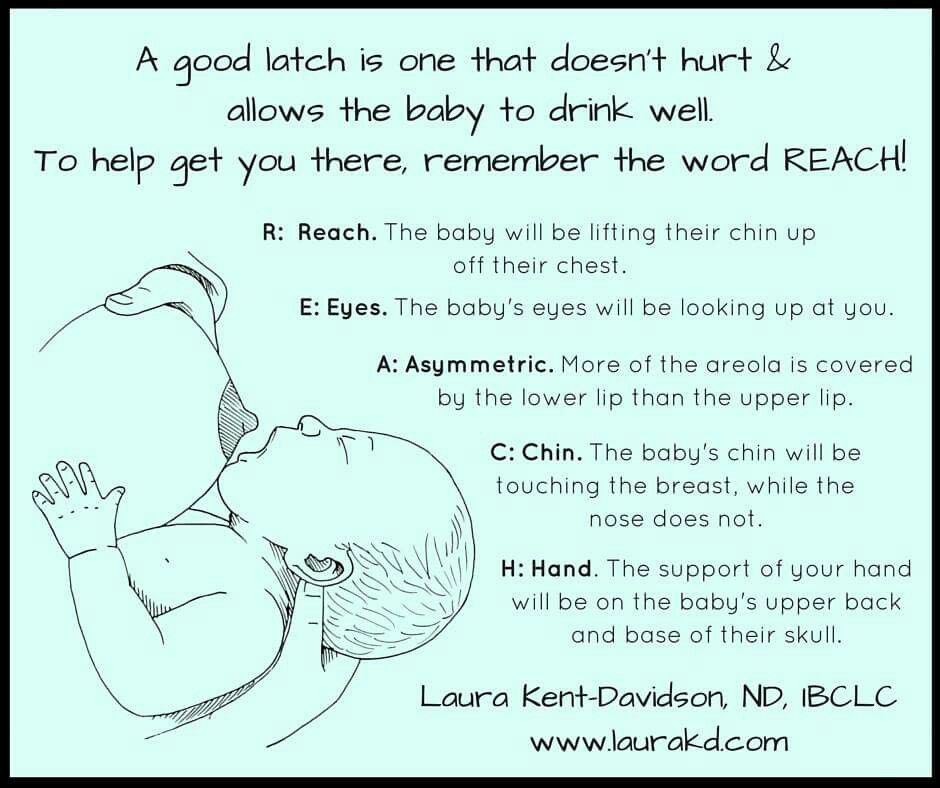
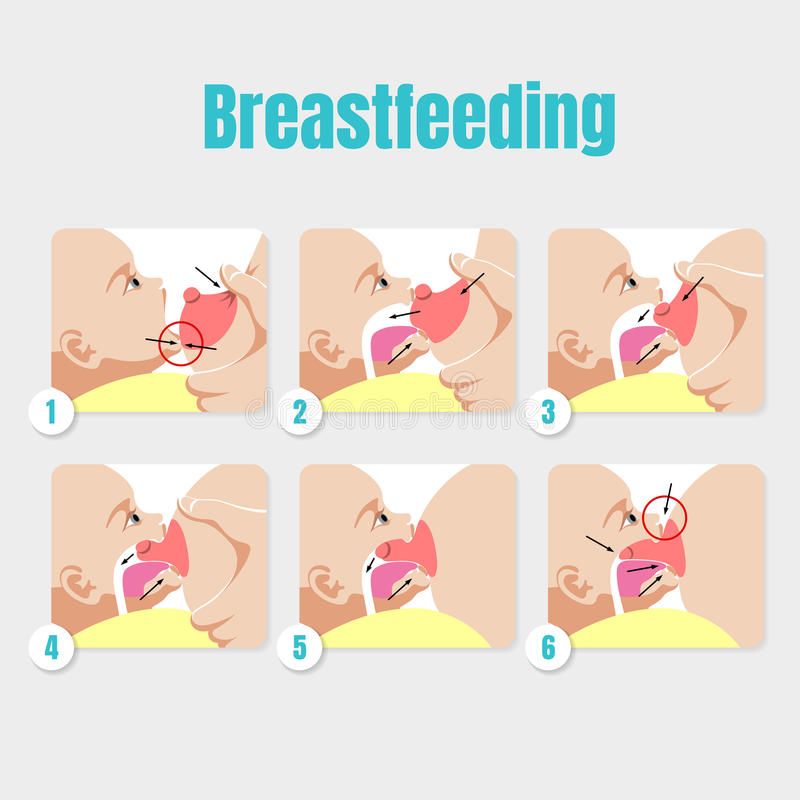
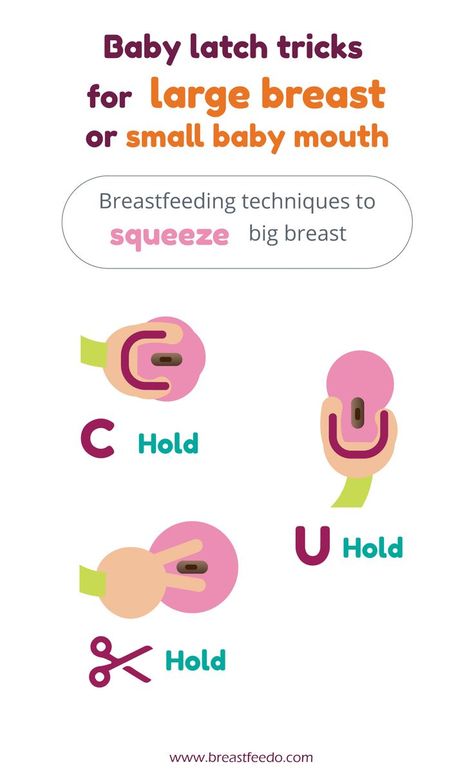
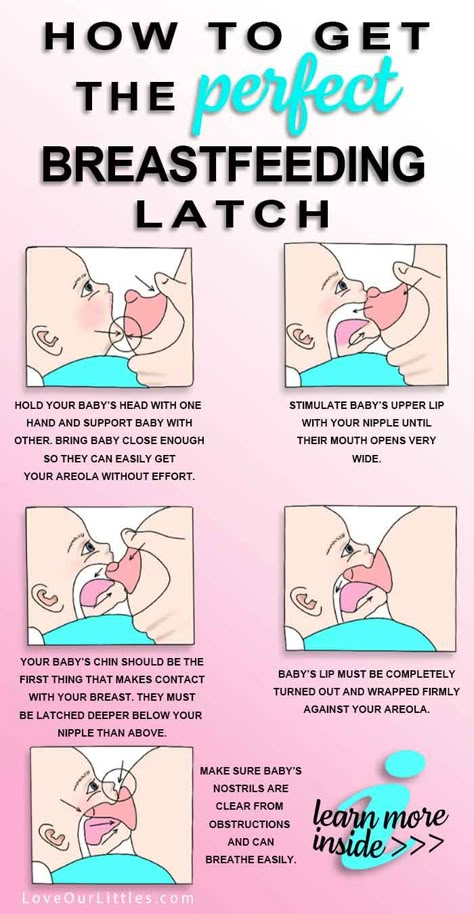
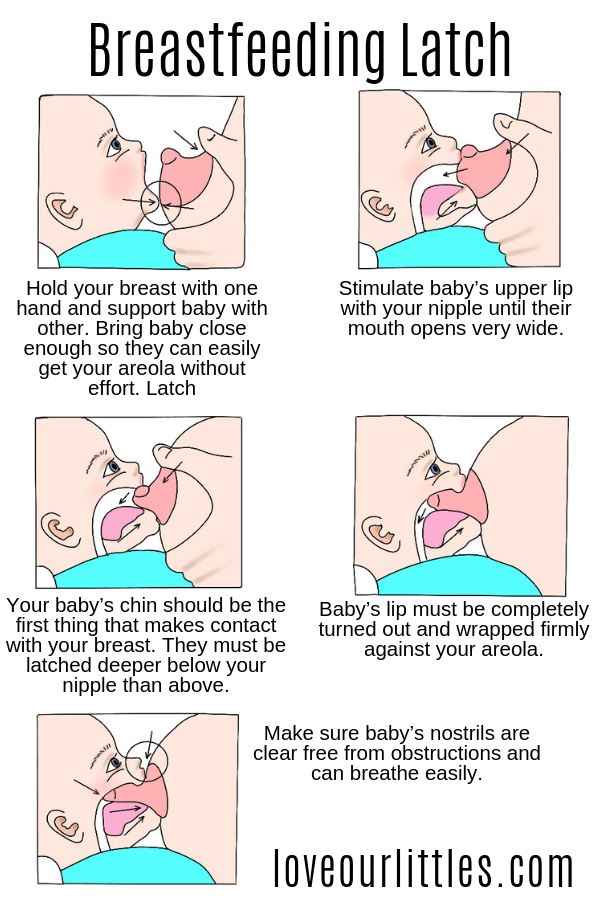
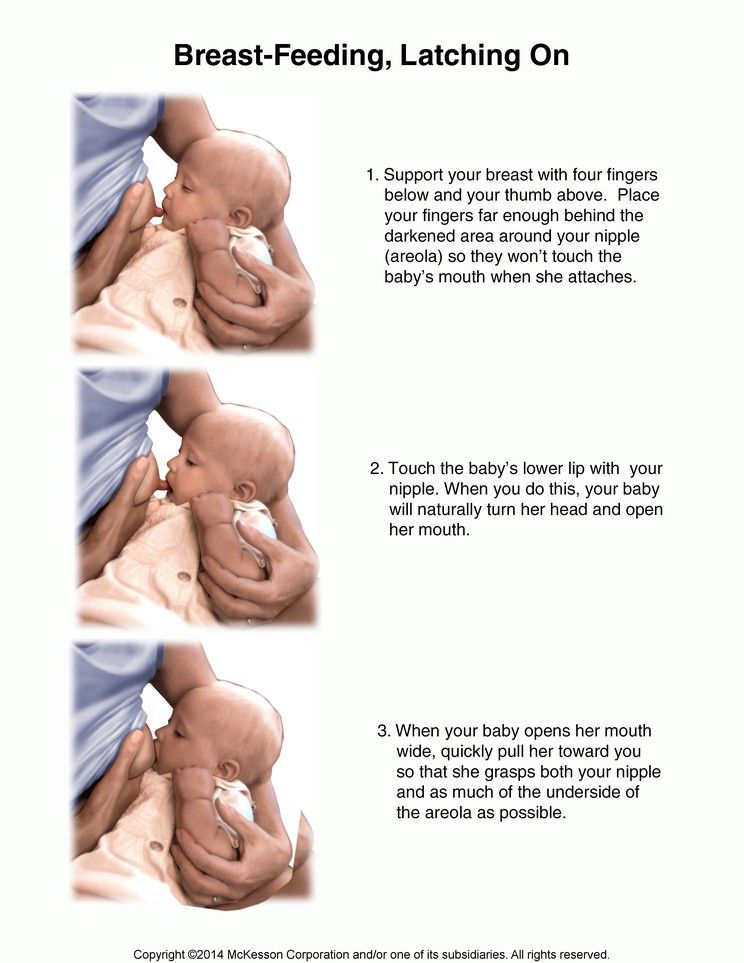
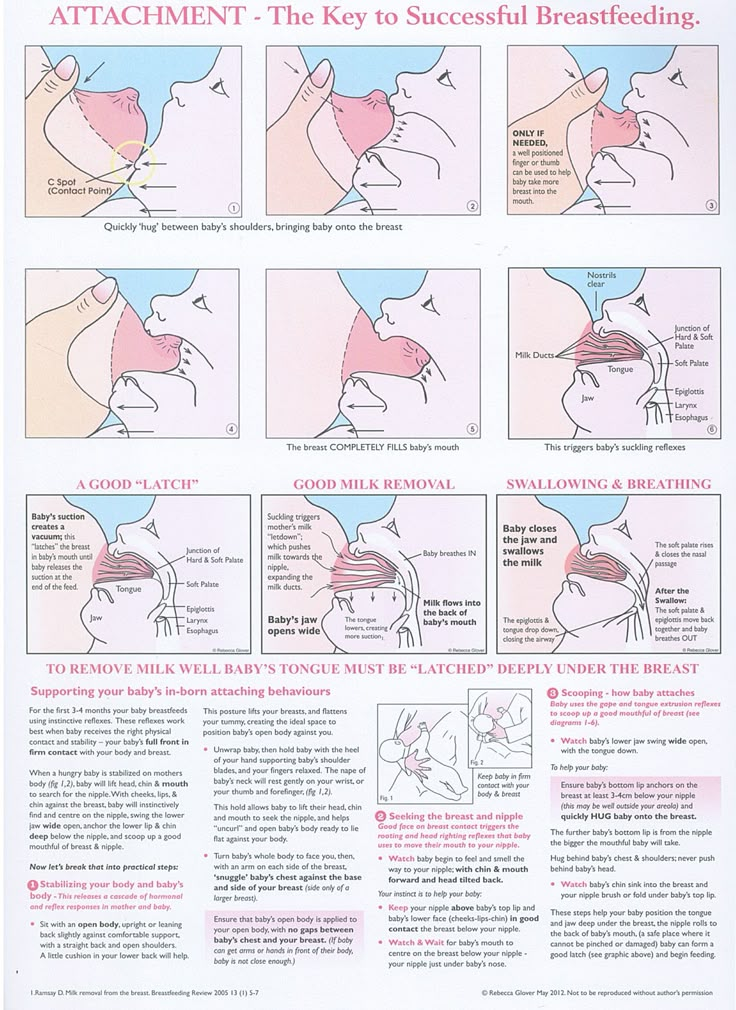
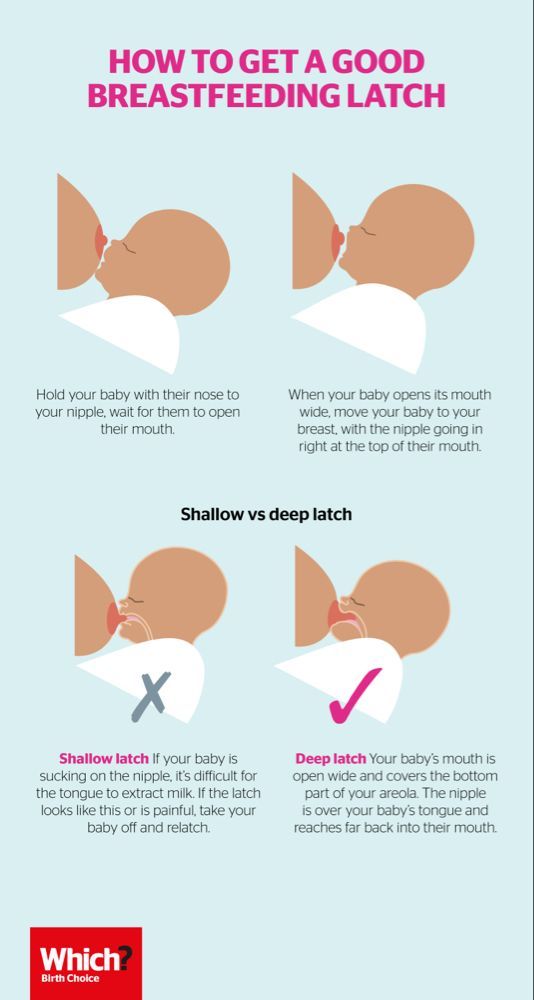
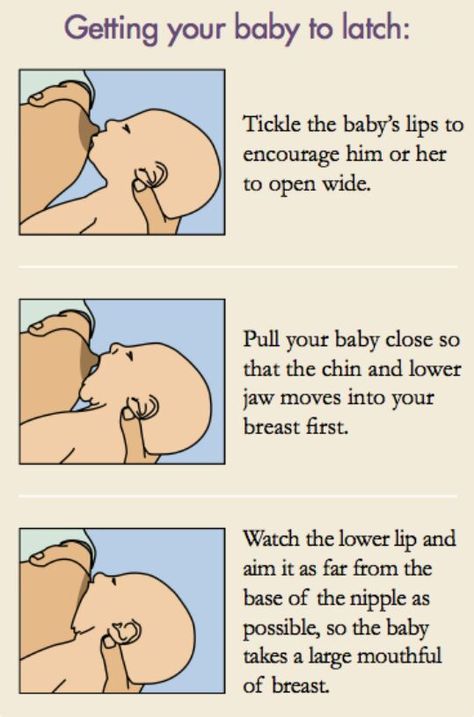
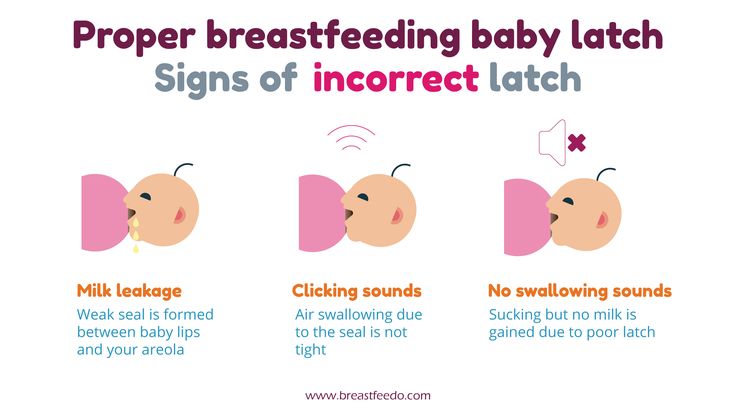
- Check how the baby latch on. An incorrect latch is one of the most common causes of pain during breastfeeding. A newborn baby should take most of the lower half of the areola (dark skin around the nipple) into his mouth, and your nipple should rest against his palate, supported from below by the tongue.
- Contact a lactation consultant or healthcare professional to make sure your baby's mouth and torso are properly positioned during feeding and there are no other latch-on problems. The doctor may also examine the baby's mouth for physical abnormalities.
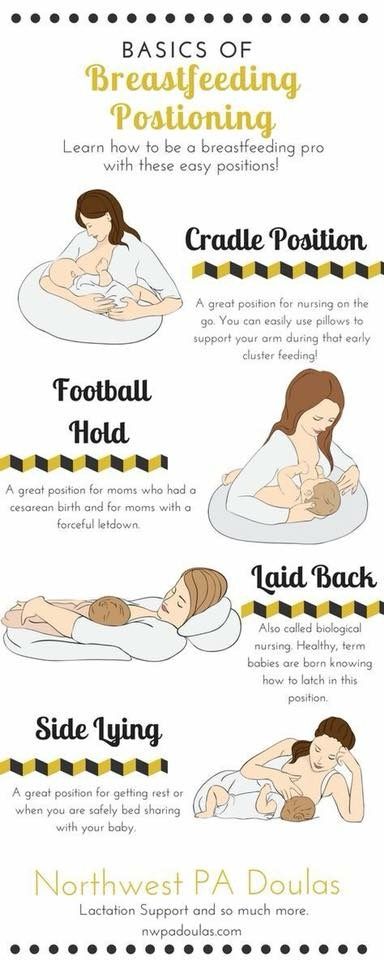
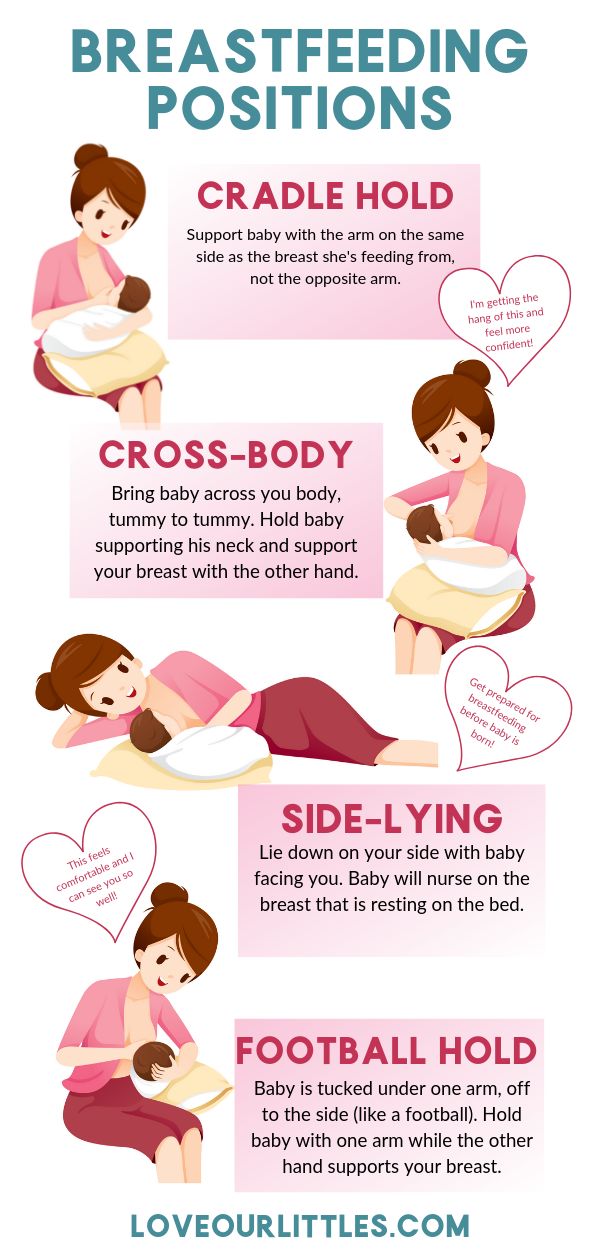
- Try other feeding positions. Reclining, cross cradle, underarm, or lying positions can relieve pressure on the most painful areas of your breasts.
- Gently wipe soaked nipples with water-soaked cotton swabs after each feed to remove milk residues that can cause infection.
- Air dry nipples or blot with a clean, soft muslin or flannel cloth to prevent bacterial growth in a humid environment. Use disposable or reusable bra pads to absorb leaking milk and remember to change them regularly.
- Soften your nipples. An ultra-pure lanolin treatment will help relieve inflammation and dry skin. You can also apply a few drops of your own breast milk to your nipples. In both cases, you do not have to wash your breasts before the next feeding. You can also apply refrigerated hydrogel pads* to your nipples. They soothe the nipples and help relieve pain during feeding, as well as speed up healing.
- Protect your nipples. Nipple shields* protect the sore area from rubbing against clothing.
- Be patient. The inflammation usually resolves after a few days as your body adjusts to breastfeeding and your baby learns to suckle.
- Seek medical attention, if pain during feeding does not go away after a few days. Constant inflammation of the nipples may indicate an infection that requires prompt treatment.
Problem #2. Baby doesn't latch on properly
Some newborns do not latch on properly right away. Maybe both of you just need more time to learn how to breastfeed, or maybe the baby was born prematurely, feels unwell after a difficult birth, or mom has flat or inverted nipples.
Solutions
- Contact a lactation consultant or healthcare professional who can help identify the cause of the problem and suggest solutions.
- Flat or inverted nipples must be pulled out. Nipple formers* fit comfortably in the bra and apply gentle pressure to the nipples to help them come out for easier feeding.
- Try different positions and ways to support your newborn. The baby needs to feel supported.
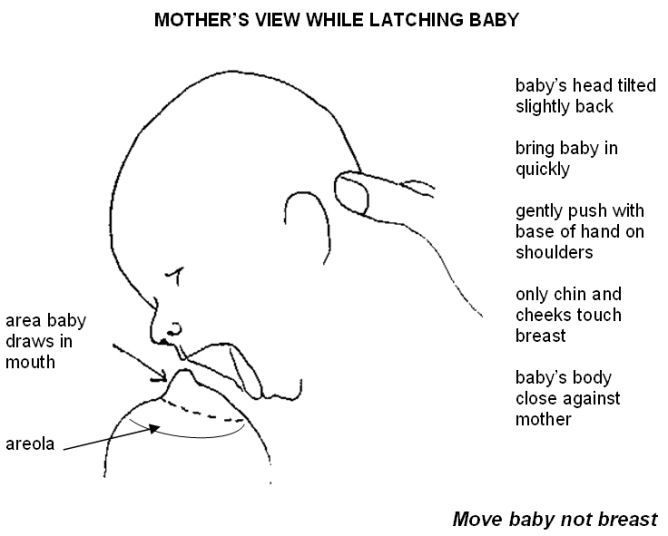 He must be comfortable and breathe freely in order to suckle properly. Do not hold the child by the head and do not put pressure on it. Lean back and let your child take the lead. This stimulates his natural reflexes and helps him find and latch on to his breasts. 4
He must be comfortable and breathe freely in order to suckle properly. Do not hold the child by the head and do not put pressure on it. Lean back and let your child take the lead. This stimulates his natural reflexes and helps him find and latch on to his breasts. 4 - When feeding, try to find the optimal position. Instead of putting your baby on and off, stressing both of you, try to position him in a way that is easy and comfortable for him. Hold the torso and legs of the baby close to you, support him by the shoulders and hold him firmly so that he feels safe. Let the baby's head rest freely on your arm so that he can tilt it back slightly and breathe freely. The chin should be pressed against your chest. If these small adjustments don't make feeding more comfortable for your baby, seek help from a lactation consultant or healthcare professional.
- Use nursing pads. If your baby is having difficulty latch-on, a lactation consultant or healthcare professional may suggest trying nursing pads*.
 A nipple with an overlay is more convenient to take in the mouth, so it is larger and more rigid. Do not use nursing pads for a long time.
A nipple with an overlay is more convenient to take in the mouth, so it is larger and more rigid. Do not use nursing pads for a long time.
Problem #3. Not enough breast milk
You will produce little breast milk at the very beginning, as the hormonal changes that trigger milk production occur slowly and do not end until the second or fourth day after birth. 2 You may be worried that your baby is not getting enough milk, but in the early days his stomach is still too small and feedings are frequent, so don't worry. The only things to worry about these days are excessive weight loss, too few wet and soiled diapers, or signs of dehydration in the baby. For more information on how often a newborn should urinate and void, see Breastfeeding Newborns: What to Expect in the First Week.
Solutions
- Contact a Lactation Consultant or your healthcare provider who can determine if you have problems with milk production.
 The sooner you do this, the better.
The sooner you do this, the better. - Feed your baby on demand, not on a schedule. In the first week after birth, your baby will ask to breastfeed every two to three hours (or more often!), both day and night. Such frequent feeding helps to establish the production of breast milk.
- Take care of yourself. It's not always easy with a newborn, but try to rest whenever you can, eat right, and accept any help around the house or with older children that your loved ones can give you to fully focus on breastfeeding.
- Try expressing milk. If a baby is feeding frequently but not gaining any weight, a lactation consultant or doctor may recommend pumping to increase breast milk production. If milk is not coming out at all, you can try the Medela Symphony Dual Electric Clinical Breast Pump**. It features an Initiate program that mimics a baby's natural sucking rhythm for the first few days.
Problem #4.
 Breast full and heavy
Breast full and heavy Your breasts will become fuller and heavier as milk comes in.
If the baby suckles well and often, this should not cause any problems. However, in some women, the breasts become so full that they become hard and painful. This condition, called breast swelling, can cause discomfort. The swollen chest seems to be “burning”, now all the activity of your body is concentrated in it, resembling a busy traffic at rush hour. Fortunately, this condition usually resolves within 24 to 48 hours. However, due to the swelling of the mammary glands, the nipples can become flat and the baby may have difficulty latch-on. 5
Solutions
- Feed your baby often. Try to breastfeed at least 8-12 times a day. This is the main way to alleviate this condition. For more tips and tricks, see the article on Breast Swelling. 6.7
- Call your healthcare provider, if symptoms persist for more than 48 hours, you have a fever, or your baby is unable to breastfeed due to swelling.

Problem #5. Milk is leaking
Breast leakage is very common in the early days of breastfeeding when milk production begins. Milk may leak from one breast while you are feeding the other, when you sleep on your stomach, or when something accidentally triggers the milk flow reflex, such as when you hear a baby crying in a store. The leakage usually stops after about six weeks.
Solutions
- Protect clothes from stains will help disposable or reusable bra pads to be used day and night.
- Don't waste precious drops! Breast milk collection pads* fit inside the bra and allow you to collect any leaking milk. This is a very useful thing when there is too much milk and the pads are not absorbing well, or when one breast is leaking while you are feeding the other. If you want to save the collected milk, use only the milk collected at the feeding. Place it in a sterile container and refrigerate immediately if you are not supplementing with it right away.
 Collected milk must be used within 24 hours. The breast milk collection sleeves should not be worn for more than two to three hours at a time.
Collected milk must be used within 24 hours. The breast milk collection sleeves should not be worn for more than two to three hours at a time.
Problem #6. There seems to be too much milk
Sometimes when milk comes in, too much is produced! In the first few weeks there may be an overabundance of milk, but usually everything returns to normal soon. 7 Up to this point, the breasts may be heavy and sore almost all the time, even immediately after a feed, and a lot of milk may leak. A strong flush can cause a baby to cough or choke, vomit immediately after a feed, have tummy discomfort, or have hard, frothy, greenish stools. These are all signs that you are having too much milk, but the problem may resolve itself as your breasts get used to the new function.
Solutions
- Express some milk by hand at the beginning of each feed to ease the force of the flush.
- Try to feed while leaning back: this will help your baby control the flow of milk.
 The "cradle" position is also good: hold the baby obliquely by the shoulders so that the head can lean back slightly while on your arm. The torso of the baby will be located diagonally on you.
The "cradle" position is also good: hold the baby obliquely by the shoulders so that the head can lean back slightly while on your arm. The torso of the baby will be located diagonally on you. - Be kind and patient. Let your baby rest and absorb milk both during and after feeding. Don't move your baby too much or too fast, as this can make him nauseous. As the baby grows, he will learn to better cope with the rush of milk, which is likely to weaken anyway.
- Use the towel or swaddle to soak up spilled milk if the baby can't handle the flush, and place the breast milk collection pad on the other breast to catch any spilled milk.
- Contact a lactation consultant or doctor if problems persist after a few weeks . He will examine you and may suggest one-sided feedings or hourly breast changes (“breast duty”) to reduce your milk supply.
Related materials: Difficulties in breastfeeding in the next few weeks and problems with breastfeeding after the first month
Literature
1 Wagner EA et al. Breastfeeding concerns at 3 and 7 days postpartum and feeding status at 2 months. Pediatrics . 2013: peds -2013. - Wagner I.A. et al., "Breastfeeding Problems at Days 3 and 7 of a Child's Life and Type of Feeding at 2 Months". Pediatrix (Pediatrics). 2013:e865–e875.
Breastfeeding concerns at 3 and 7 days postpartum and feeding status at 2 months. Pediatrics . 2013: peds -2013. - Wagner I.A. et al., "Breastfeeding Problems at Days 3 and 7 of a Child's Life and Type of Feeding at 2 Months". Pediatrix (Pediatrics). 2013:e865–e875.
2 Pang WW, Hartmann PE. Initiation of human lactation: secretory differentiation and secretory activation. J Mammary Gland Biol Neoplasia 2007;12(4):211-221. - Pang, W.W., Hartmann, P.I., "Lactation initiation in the lactating mother: secretory differentiation and secretory activation." G Mammary Gland Biol Neoplasia. 2007;12(4):211-221.
3 Cadwell K. Latching - On and Suckling of the Healthy Term Neonate: Breastfeeding Assessment. J Midwifery & Women ’ s 2007;52(6):638-642. — Cadwell, K., "Latching and sucking in healthy newborns: evaluation of breastfeeding." F Midwifery Women Health. 2007;52(6):638-642.
— Cadwell, K., "Latching and sucking in healthy newborns: evaluation of breastfeeding." F Midwifery Women Health. 2007;52(6):638-642.
4 Colson SD et al. Optimal positions for the release of primitive neonatal reflexes stimulating breastfeeding. Early Hum Dev . 2008;84(7):441-449. - Colson S.D. et al., "Optimal Positions for Provoking Primitive Innate Reflexes to Induce Breastfeeding." Airlie Hume Dev. 2008;84(7):441-449.
5 Jacobs A et al. S3-guidelines for the treatment of inflammatory breast disease during the lactation period. Geburtshilfe Frauenheilkd. 2013;73(12):1202-1208. - Jacobs A. et al., "Recommendations S -3 for the treatment of inflammatory diseases of the breast during breastfeeding. Geburtskhilfe und Frauenheilkünde. ABM clinical protocol# 4: Mastitis , revised March 2014 2014;9(5):239-243 - Amir L. H., Academy of Breastfeeding Protocol Committee, AVM Clinical Protocol #4: Mastitis, March 2014 edition of Brestfeed Med (Breastfeeding Medicine). 2014;9(5):239-243.
H., Academy of Breastfeeding Protocol Committee, AVM Clinical Protocol #4: Mastitis, March 2014 edition of Brestfeed Med (Breastfeeding Medicine). 2014;9(5):239-243.
7 Academy of Breastfeeding Medicine Protocol Committee. ABM clinical protocol # 20: Engorgement. Breastfeed Med . 2009;4(2):111-113. - Protocol Committee of the Academy of Breastfeeding Medicine, "AVM Clinical Protocol No. 20: Engorgement, Revision 2016". Brestfeed Med (Breastfeeding Medicine). 2009;4(2):111-113.
Read instructions before use. Consult a specialist about possible contraindications.
* RU No. ФСЗ 2010/07352 dated 07/19/10
** RU No. ФСЗ 2010/06525 dated 03/17/2021
Why does the baby refuse to breastfeed?
If the baby began to take the breast poorly - this is not a reason to switch to mixed feeding, and even more so to stop breastfeeding. Breastfeeding is the best nutrition for a newborn and the basis of future health.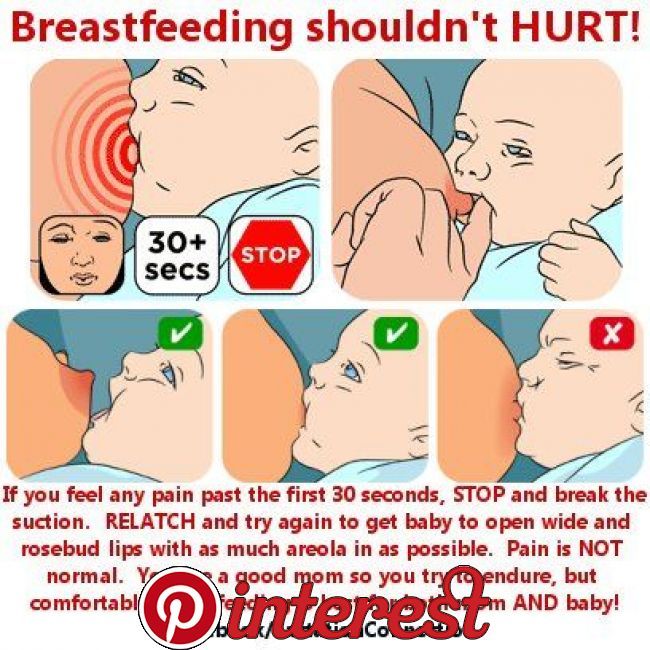 There are many reasons why a baby may refuse to breastfeed. It is important to familiarize yourself with the list of possible problems in order to avoid them in the future.
There are many reasons why a baby may refuse to breastfeed. It is important to familiarize yourself with the list of possible problems in order to avoid them in the future.
By choosing to breastfeed today, you are laying the foundation for the healthy development of your baby in the future. Problems such as lack of milk, lactation crises and refusal of the baby to breastfeed are not a reason to stop breastfeeding.
If your baby refuses to breastfeed, don't despair and don't stop trying to breastfeed. Every problem has its own solution, often the simplest one. If you don’t find yours in the list of reasons for your baby’s refusal to breastfeed, contact a supervising specialist or a Nutriсlub expert.
Discomfort
- A feeding position should be comfortable for both you and your baby.
- Check for stuffy nose. Clean your nose and continue feeding.
- The baby must grasp not only the nipple itself, but also the entire areola.

- The environment for feeding should be soothing.
Shape of the nipples
- The myth that flat nipples interfere with feeding has long been debunked. It is enough to hold the baby correctly during feeding and monitor the capture of the breast.
- If the nipples are naturally inverted, their shape can be corrected with a breast pump. When expressing, the nipple is pulled out.
Foreign smell
- From the moment of birth, the baby smells and knows your natural smell.
- Before feeding, do not use perfume, shower gels with a strong scent, use unscented deodorants.
- If you came from the street and "brought" extraneous odors with you, change into home clothes.
Stress
- Your stress is instantly transmitted to the baby, so before feeding you need to relax, give the baby the opportunity to properly latch on the nipple.
- Smile and speak gentle words to your child.
- It is better to feed the baby in a calm and familiar environment, preferably secluded.
Disease
- The baby may refuse to breastfeed due to weakness or lack of appetite. Wait and offer the breast later.
- If further attempts fail, express milk and offer it in a bottle, but start the next feeding with breast offering.
- If your baby has a runny nose, it may be difficult for him to suck because of nasal congestion.
Bottle preferred
- If you are supplementing your baby with a bottle, he may refuse to breastfeed because the nipple is easier to suck on.
- Don't stop trying to breastfeed your baby.
- Try to put the baby to the breast immediately after sleep, the sleepy baby will instinctively reach for the breast.
- Try to avoid the bottle, try using a special soft spoon for feeding babies instead.
The taste of milk
- Even small mistakes in the diet of a nursing mother can lead to breast rejection.
 Try not to use spices and spices in cooking, give up onions and garlic.
Try not to use spices and spices in cooking, give up onions and garlic. - The taste of milk may change when taking medicines and during menstruation. Express the first portion of milk and try again.
- Experts recommend storing expressed milk in the freezer for several feedings. Warm up the milk and offer it in a bottle or in a spoon, express your milk to maintain lactation.
Restlessness
- At the age of 4-7 months, the baby is learning new skills and it may be difficult for him to concentrate on feeding.
- Feeding should take place in a quiet, private environment.
Introduction of complementary foods
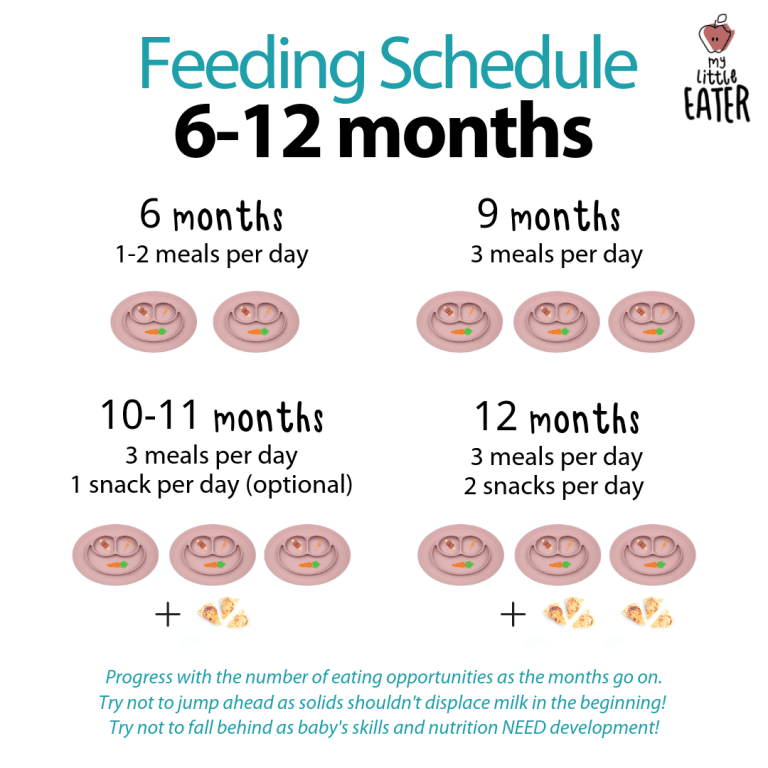
- Breast milk is the main component of the baby's diet, but from about 6 months the child begins to receive the first complementary foods.
- It is important to correctly plan the baby's nutrition so that the baby does not refuse the breast. Maintain the correct proportions between breast milk and complementary foods.