Breast feeding tips for new born baby
Our Top 19 Breastfeeding Tips
Breastfeeding can have many positive effects for both you and your baby. However, it doesn’t come as easy for every mom. These tips and tricks can help you ease into breastfeeding and all the challenges that go along with it.
The Benefits of Breastfeeding
Breastfeeding offers many benefits for babies and mothers. Breast milk is packed with nutrients and antibodies that help boost your baby’s immune system, and breastfeeding can help you form a strong bond with your little one.
Because of these great benefits, it’s worth trying some of these breastfeeding tips and tricks, and speaking to a lactation consultant or your healthcare provider for personalized advice if you need help with breastfeeding.
Each woman's and each baby's experience is different, with some new moms finding that breastfeeding takes a little more effort than others. Whether breastfeeding comes fairly easily or presents a few challenges for you, know that you’re doing great and that things will fall into place over time.
19 Breastfeeding Tips and Tricks
Here are 19 tips and tricks to help make breastfeeding go as smoothly as possible.
1. Attend Breastfeeding Classes
It’s a good idea to get some information and instruction on how to breastfeed while you’re still pregnant, especially if you’re a first-time mother (or if it’s been a while since you’ve breastfed). Research shows that women who learn about breastfeeding during pregnancy are more likely to be successful than those who do not.
Breastfeeding classes may be available at a community center or hospital near you. Your healthcare provider will be able to point you in the direction of classes or a one-on-one session with a lactation consultant.
2. Arm Yourself With the Right Nursing Supplies
Anything that can help make your life simpler and more comfortable while you breastfeed your baby is a welcome addition. Here are some things to consider buying:
A well-fitting nursing bra can give your breasts the right level of support and make it possible to feed your baby without completely undressing.
 You may wish to stock up on nursing bras before your baby is born. Think about buying a size bigger, because your breasts may be larger after you give birth.
You may wish to stock up on nursing bras before your baby is born. Think about buying a size bigger, because your breasts may be larger after you give birth.Breast pads can come in handy as your breasts might leak a little milk from time to time. Avoid plastic liners that can irritate your nipples. If you don’t want to buy pads, you can fold up a piece of absorbent cloth or use a handkerchief.
You'll need a breast pump, bottles, and breast milk storage bags so you can pump milk and store it for later.
You may like the extra comfort of a nursing pillow.
A rocking chair or glider can help make breastfeeding more comfortable for you, and the rocking or gliding motion might help soothe your little one.
A footstool can help raise your legs and lap higher and get your baby even closer to your breasts. If you buy a nursery glider, it may come with a matching ottoman or a built-in footrest.
3. Let Your Healthcare Provider Know You Plan to Breastfeed
It’s a good idea to tell your healthcare provider while you’re still pregnant that you’d like to breastfeed your baby.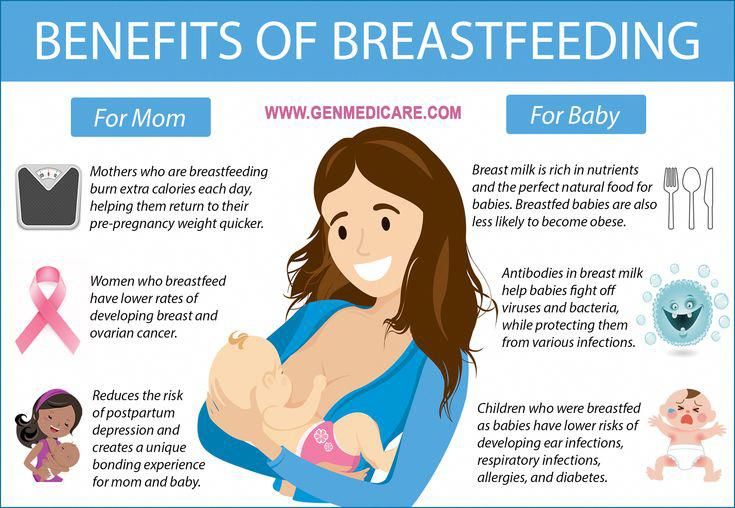 That way, your provider can make sure you have the information and resources you need. If you’re putting together a birth plan, you can include your wishes about breastfeeding in that document and also remind your healthcare team about your plans when you're admitted to the hospital to give birth.
That way, your provider can make sure you have the information and resources you need. If you’re putting together a birth plan, you can include your wishes about breastfeeding in that document and also remind your healthcare team about your plans when you're admitted to the hospital to give birth.
If you're taking any medications, your healthcare provider should definitely know that you're planning to breastfeed. In some cases, your provider may recommend an alternative medication for the period while you breastfeed your little one.
4. Breastfeed Right After Birth
It’s beneficial to breastfeed your little one very soon after he is born. Newborns are typically ready to nurse within the first hour after birth.
Those first feeds nourish your baby, of course, and get you both started in figuring out this new skill and routine of breastfeeding. Other benefits include the following:
The milk that comes through in the first few days is actually colostrum —a thick, yellow fluid that’s packed with protein and antibodies that support your baby’s growth and development.
Breastfeeding encourages the release of the hormone oxytocin, which may help you bond with your baby, and help you feel more confident about your nurturing abilities.
Skin-to-skin contact during breastfeeding helps stabilize your baby’s body temperature, heart rate, breathing, and blood sugar levels.
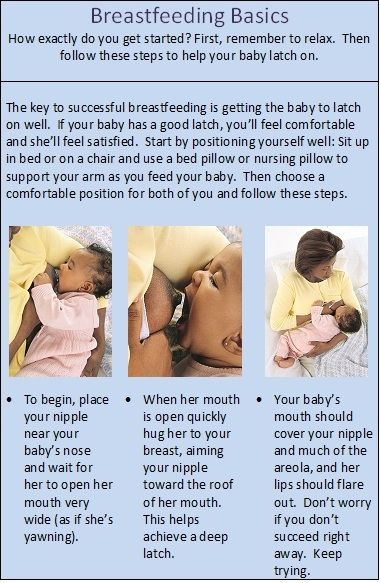
5. Consider Different Ways to Latch
To breastfeed, your baby needs to “latch on.” This is when your baby is properly attached to your breast with his mouth wide open over your nipple, covering most of your areola, and his nose, lips, and chin close to your breast.
Here are two ways to get your baby to latch on when breastfeeding:
After getting into a comfortable breastfeeding position, cup your breast with your hand and guide the nipple to stroke your baby’s lip. This action stimulates your baby’s natural rooting reflex to open his mouth wide and suckle. Make sure to bring your baby close to your breast and aim your nipple toward the roof of his mouth.
“Baby-led” latching or “laid-back” breastfeeding involves you lying on your back and placing your baby on your chest with your baby’s cheek close to your breast. Your baby will naturally explore his surroundings, find your nipple, and latch on.
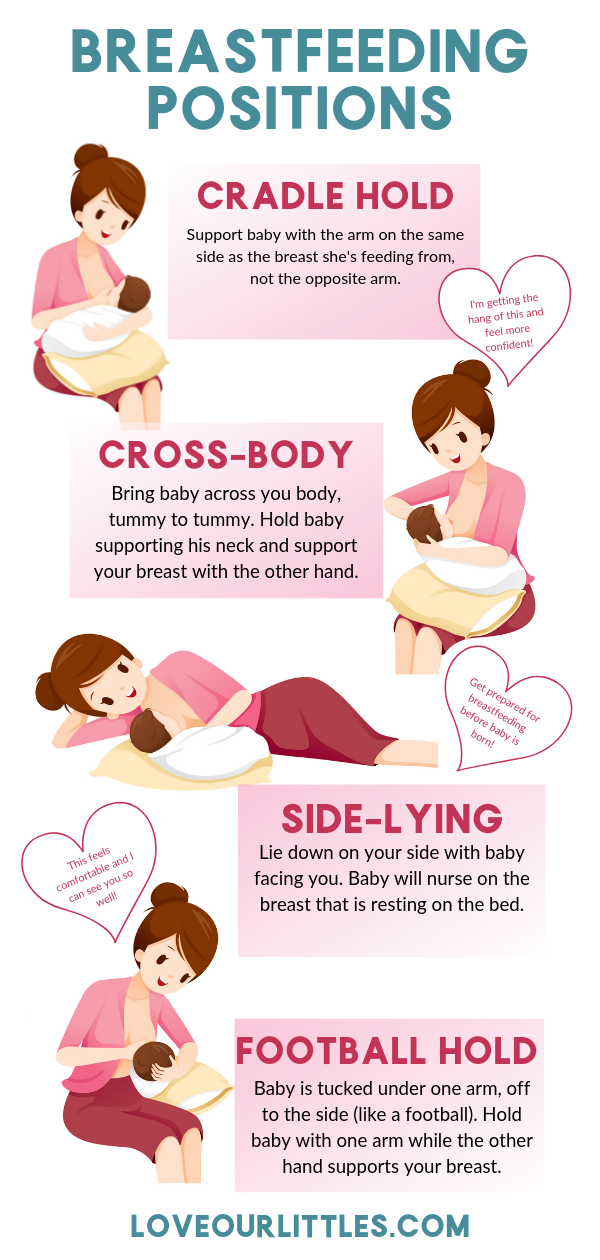
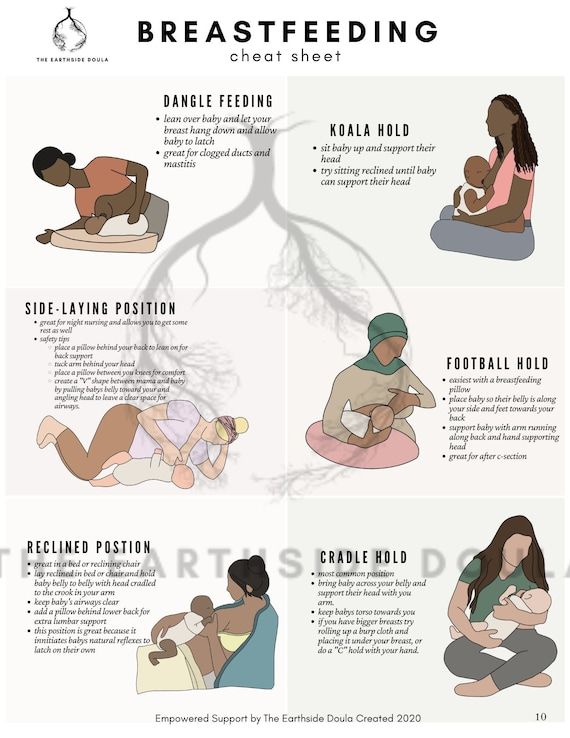
6. Try Different Breastfeeding Positions
There are a variety of breastfeeding positions you could use to help your baby latch on better and help empty your breasts more effectively.
Here are four breastfeeding positions to try:
Cradle hold. This is the most traditional hold that many moms try first. Cradle your baby with the arm that’s on the side your baby is nursing from. Her head should be resting in the bend of your elbow, facing your breast, and her body should be turned inward to you. Be sure to always support your baby’s head as it will be a while before she can hold her head up on her own.
Cross-cradle hold. This is similar to the cradle hold, except here you’re holding your baby with the arm opposite to the breast she is nursing on.
 Support your baby’s head with your hand and have her bottom in the bend of your elbow. Your other arm can support your breast from underneath. You’ll want your baby’s body turned inward to you. This position is very good for newborns who are having trouble latching.
Support your baby’s head with your hand and have her bottom in the bend of your elbow. Your other arm can support your breast from underneath. You’ll want your baby’s body turned inward to you. This position is very good for newborns who are having trouble latching.Football hold. Just like it sounds, this position involves tucking your baby under your arm as if you were holding a football. You’ll want to hold your baby to your side at the level of your waist while supporting her back with your arm. Her head should be tilted up toward your breast. This position can work well if you’ve had a cesarean section, if you have large breasts, or if you’ve had twins and want to feed your babies simultaneously.
Side-lying position. While lying on your side, place your baby next to you, and lift your breast up to within your baby’s reach so she can easily access your nipple. This position is convenient for those late-night feedings (just be sure to put your baby back in her crib to sleep afterward).
 It’s also a good position to try if you’ve had a cesarean section.
It’s also a good position to try if you’ve had a cesarean section.
To help visualize these positions, check out the infographic below:
7. Breastfeed From Both Breasts Equally
If your baby has a preference for one breast, it’s a good idea to offer him the other breast at the next feeding to make sure that both your breasts get emptied equally.
Here’s a handy tip: If you tend to forget which breast your baby last nursed from, attach a safety pin to the bra strap of the other side after a feeding to remind you which side is next.
If your baby still wants to nurse from only one breast, you could pump from the other breast to relieve pressure and ensure that your breast milk supply doesn’t dwindle.
8. Ease the Pain of Engorgement
Engorgement is when the blood vessels in your breasts are swollen and your milk ducts are overfilled with milk, causing discomfort and even pain. It can happen if your baby doesn’t nurse often or efficiently.
The best prevention strategy is to feed your baby whenever she’s hungry, and to make sure she nurses from both of your breasts. The idea is to drain your breasts regularly in order to keep them from becoming painfully hard and swollen. You don’t want to have your breasts become so engorged that your baby can’t latch on properly.
The idea is to drain your breasts regularly in order to keep them from becoming painfully hard and swollen. You don’t want to have your breasts become so engorged that your baby can’t latch on properly.
Here are a few more tips for dealing with engorgement:
Express your breast milk manually or pump some milk to help relieve the pressure before nursing your baby
Massage your breasts to help the milk flow
Soak a hand towel in warm water and place it over your chest before you breastfeed You could also take a warm shower. Warmth can help the milk flow.
If you find that heat doesn’t work, try using a cool compress in between or after each breastfeeding session
Mix up your breastfeeding positions to help drain different areas of your breasts.
If these tips don’t work, contact your lactation consultant or your healthcare provider for advice. You don’t have to suffer with breast discomfort or pain—there is help available.
9. Don’t Give Up Breastfeeding If You Have Mastitis
Occasionally a clogged milk duct can get infected. This is a condition called mastitis, and the symptoms include fever- and cold-like symptoms; swollen, painful breasts; breasts that feel hot when touched; a hard lump on your breast; and red streaks on the skin of the breasts.
If you think you may mastitis, call your healthcare provider. Your provider may prescribe an antibiotic that is safe for you to take while breastfeeding your baby. Remember to finish the entire course of antibiotics, even if your symptoms have improved.
In the meantime, there are a few home remedies you can try:
Apply a warm compress of wet or dry heat to the lump, or take a warm shower
Offer your baby the breast with the blocked duct and let him nurse for a long period, as this can help drain the blocked duct. Don’t worry—it’s safe for your baby to nurse, as the infection can’t be passed onto him. In fact, continuing to breastfeed may actually help the infection clear sooner.

Massage the lump at the same time as you nurse your baby
Wear loose-fitting tops or don’t wear a bra for a few days
Pump any remaining milk after nursing your little one to help drain the blocked duct
Take every opportunity to rest and drink lots of water.
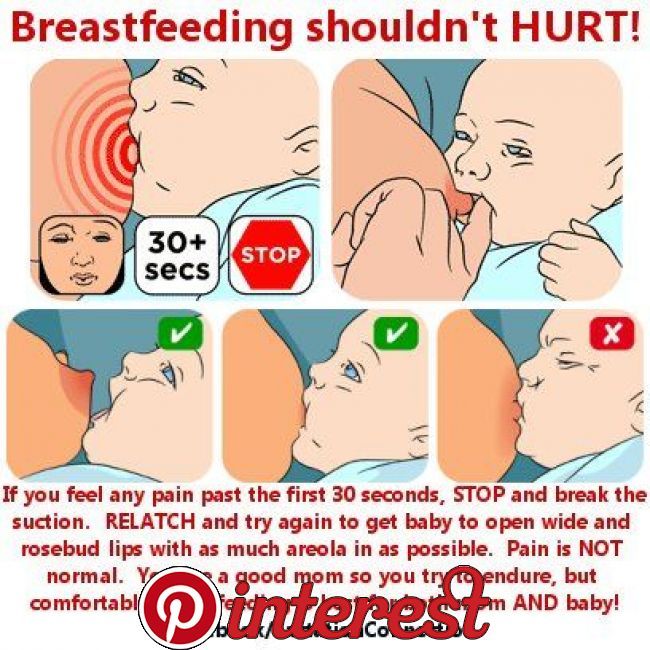
10. Care for Your Nipples
Tender nipples are not unusual during the first few weeks of breastfeeding. Eventually this tenderness will likely go away. To help reduce or prevent nipple discomfort, follow these breastfeeding tips:
Make sure your baby is latched properly by checking that your baby’s mouth is open wide, covering your areola and not just the tip of your nipple
Change up your baby’s breastfeeding position from time to time.
After your baby breastfeeds, try these aftercare tips for your nipples:
For a soothing effect, let some breast milk dry on your nipple
If you live in a humid climate, expose your breasts to sunlight as the hot air can help alleviate sore and cracked nipples
Use bra pads in between feedings, especially if your breasts tend to leak.
 Just don’t use ones lined with plastic as those can trap moisture, which can cause friction and irritation.
Just don’t use ones lined with plastic as those can trap moisture, which can cause friction and irritation.When bathing, wash your breasts with water and avoid the use of soaps, shampoos, or other cleansers that irritate your skin
Ask your healthcare provider to recommend an ointment or cream that can help treat or prevent sore, cracked, or bleeding nipples.
11. Follow Your Baby’s Cues When It Comes to Breastfeeding
Every baby is different, and yours may want to feed more or less often than other babies, so don’t worry if your baby doesn’t follow the schedule you had expected beforehand.
There is no feeding schedule that you must follow to the letter. Instead, pay attention to your baby’s hunger signals. Keep in mind that how often your baby wants to feed will also change over time, and may go up and down periodically as a result of things like growth spurts.
Signs your baby is hungry may include when she
is awake and alert
puts her hands to her lips
sucks on her fingers
flexes her arms with her hands in a fist
whimpers and moves her arms and hands
nuzzles your breast.

Crying can be a late sign of hunger, so try not to wait until your baby starts to cry to feed her.
In your baby’s first weeks, your newborn will likely want to feed as often as every 2 to 3 hours (8 to 12 times per day). She may spend 10 to 15 minutes nursing on each breast, or she may even breastfeed for longer stretches.
Extended nursing sessions, as well as feeding more often for a period of time, may be a sign of cluster feedings, which typically happen in the evenings during growth spurts, for example.
12. Check That Your Baby Is Getting Enough Breast Milk
You’re probably wondering if there’s an easy way to check that your baby is getting enough nourishment. Here are five tips for checking that your newborn is getting a sufficient amount of breast milk:
Listen for your baby swallowing while nursing, typically after several sucks.
Keep an eye on your baby to see if he appears satisfied for a few hours after the feeding session.
 For example, your baby’s arms will most likely be relaxed with open palms, signaling that he is full and content.
For example, your baby’s arms will most likely be relaxed with open palms, signaling that he is full and content.Before a feeding, your breasts may feel full and firm, but after a feeding they will feel softer. This is a sign your little one has been fed. As time goes by you’ll notice this difference less. You may think your breasts are completely empty of milk, but know that your breasts are always in the process of producing milk.
A very accurate sign that your baby is getting enough to eat is steady growth. Your healthcare provider will check your baby's weight, length, and head circumference at each checkup. Know that it’s normal for a newborn to lose up to 10 percent of his birth weight in the first few days, but by the end of his second week, he should be back to gaining weight at a steady pace.
Keeping track of your little one’s wet and dirty diapers helps you know he's eating well. In your baby’s first month, he may produce about six or more wet diapers a day with light-colored urine, and have three to four bowel movements a day that are soft and yellowish in color.
 Later on, the frequency of bowel movements may decrease.
Later on, the frequency of bowel movements may decrease.
If you’re ever concerned that your baby isn’t eating enough, call your healthcare provider—don’t wait for the next scheduled checkup.
13. Increase Your Milk Supply, If Needed
To help increase your milk supply, here are four things you can do:
Breastfeed more often, as this will result in your breasts producing more milk
Pump after nursing, as this can help stimulate your breasts to produce more milk
Drink plenty of water and eat a nutritious diet
Try to reduce stress and relax. For example, take some time for yourself every day, even if it’s just 15 minutes.
Here are some reasons why you may have a low milk supply:
You might not be breastfeeding often enough (remember that newborns feed about 8 to 12 times a day). Breastfeeding or pumping too infrequently may signal your breasts to produce less milk.
If your baby was born prematurely, your preemie may not be strong enough to nurse enough milk from your breasts.
 This can lead to a decrease in milk production.
This can lead to a decrease in milk production.
Contact your lactation consultant or healthcare provider for more personalized advice on increasing your breast milk supply.
14. Consider Using a Breast Pump
You may need or want to pump if
circumstances make it difficult for you to feed your newborn; for example, if your baby is born prematurely and is in the NICU
your breasts are engorged after or between feeds
you have mastitis; pumping can help relieve the discomfort associated with this condition
your baby wants to nurse from only one breast and not the other
you would like to have some extra breast milk stored so that someone else, such as your partner or a babysitter, can bottle-feed your baby
you’re heading back to work and plan to pump during the day.
There are many different breast pumps available; another option is to choose hand expression. If you’re having trouble deciding, speak with your lactation consultant or healthcare provider for advice. Your lactation consultant can also help you learn how to master hand expression or how to use your new breast pump.
Your lactation consultant can also help you learn how to master hand expression or how to use your new breast pump.
At first, your baby may be a little leery of feeding from a bottle, especially since it will be new to him, but eventually he will get used to it. In some cases, your baby may refuse to take a bottle from you, but he’ll happily take it from your partner or a babysitter. So it’s worth trying different approaches.
15. Wait With Introducing a Pacifier
Giving your baby a pacifier can help soothe her between feeds; however, offering it in those first few weeks can have a negative effect on your milk supply, and discourage your baby from wanting to nurse.
Experts recommend waiting until your baby has gotten used to breastfeeding before offering a pacifier.
Of course, you may use a pacifier sparingly to comfort your baby earlier than that, like when she’s getting a vaccination, but you could also offer her your clean pinky finger to suckle on for comfort during these short periods.
16. Get Prepared for Breastfeeding in Public (If You Choose To!)
At some point, you may like to breastfeed your baby while you’re in a public place. Here are some tips for breastfeeding in public:
Wear clothing that allows you to easily access your breasts, like a loose top or a button-down shirt
You may wish to use a nursing cover, oversized scarf, or light blanket to cover yourself when you’re breastfeeding. Practice this at home so that you and your baby can get used to it.
Breastfeed while wearing your baby in a sling or soft baby carrier. Not only is this practical, it also keeps your baby comfortably close to you.
Find a women’s lounge or a dressing room in a department store so that you have somewhere peaceful to breastfeed.
17. Pay Attention to Your Nutrition and Well-Being
Maintaining a healthy lifestyle is just as important now that you’re breastfeeding as it was when you were pregnant, and at other times in your life.
Here are some tips to help you stay on track:
Eat healthy, well-balanced meals while breastfeeding. Include lots of fruits, vegetables, whole grains, and protein-packed foods like lean meats, beans, and dairy products. To make breast milk, your body may need about 450 to 500 extra calories a day (2,500 calories total) if you're at a normal weight.
Take a multivitamin or other supplement if it’s recommended by your healthcare provider
Drink plenty of water. Aim for at least eight glasses a day to stay hydrated since breastfeeding uses a lot of fluid. Stay away from sugary drinks, even juices.
Rest up as much as you can and try to sleep when your baby sleeps to take advantage of those opportunities for rest.
18. Avoid Alcohol and Smoking, and Limit Certain Foods
The following tips are reminders that as long as you’re breastfeeding, you’re passing on what you eat and drink to your baby, which means certain things need to be avoided or limited to ensure your baby isn’t affected in a negative way:
Limit your caffeine intake to 200 mg a day.
 Caffeine can irritate your baby and affect his sleep.
Caffeine can irritate your baby and affect his sleep.Limit consuming seafood that’s high in mercury like swordfish, king mackerel, and tilefish
Avoid smoking, since nicotine can interfere with your baby’s sleep and health. Secondhand smoke also increases the risk of Sudden Infant Death Syndrome (SIDS) and respiratory illnesses in your baby.
Avoid drinking alcohol, as it’s not safe for your baby. If you do happen to have the occasional drink, wait two to three hours for it to leave your system before breastfeeding. “Pumping and dumping” your milk won’t speed up the removal of alcohol from your breast milk.
19. Get Help If You’re Struggling With Breastfeeding
If breastfeeding is difficult or uncomfortable, don't hesitate to reach out for help, and don't be embarrassed. Breastfeeding is a natural process but it does takes time and practice, and problems can crop up along the way. There are many people and resources you can turn to for guidance and support: your own healthcare provider, the nurses and staff in the hospital, a lactation consultant, and also organizations such as La Leche League International.
The Bottom Line
Breastfeeding can be challenging at times, especially if you’re a new mom, and it’s normal to feel a little anxious about it.
By following these tips and getting some professional help, you’ll soon get the hang of it. Plus, the more you nurse, the more milk you’ll produce, and the more practice you’ll get. Before long, breastfeeding will become a routine and enjoyable part of your day, and you’ll look forward to the special bonding time it gives you and your baby.
The 12 Best Breastfeeding Tips For New Mothers
One of your first nurturing acts as a new mother will likely be feeding your baby. For many women, that will mean breastfeeding. As natural as breastfeeding is, you may still worry and stress about providing the proper nutrients for your baby. And you probably have a million questions about how it all works and how to do it correctly.
And you probably have a million questions about how it all works and how to do it correctly.
Our best advice: relax, you and your baby will get the hang of it eventually. To help calm your worries, we’ve put together a list of the 12 best breastfeeding tips for new mothers.
Breastfeeding Tips For New Mothers
1) Anticipate Your Baby’s Desires
Rather than waiting for your baby to cry, you can anticipate their needs by watching for a few tell-tale signs. When your baby is hungry, they may:
- Turn or raise their head repeatedly.
- Open and close their mouth.
- Stick out their tongue.
- Suck on whatever is near.
If you see your baby making these moves, offer your breast right away. Your baby will be happy that they don’t have to struggle to get your attention, and you’ll build a level of intimacy that will deepen your mother/baby relationship.
2) Let Your Baby Determine How Often And How Long To Nurse
Your baby knows their needs better than you do right now. Let them determine how often to nurse. Don’t set a predetermined interval between feedings and then deny your baby food just because not enough time hasn’t gone by.
Let them determine how often to nurse. Don’t set a predetermined interval between feedings and then deny your baby food just because not enough time hasn’t gone by.
On the other hand, there’s no need to wake a sleeping baby to feed them simply because three hours have passed. Let your sleeping baby lay peacefully and feed them when they wake.
Similarly, let your baby determine how long to nurse. Remember, your little one knows how much they need better than you do right now. Don’t worry if nursing time only lasts ten minutes, and don’t panic if it stretches on for forty-five. Some babies are fast eaters, while some like to take their time.
3) Get Comfortable While Nursing
You’re going to be spending a significant amount of time holding your baby to your breast while they feed. If you do this in an unsupported sitting position, it can get uncomfortable quickly. Additionally, trying to maintain an uncomfortable position for a prolonged period of time can lead to significant back, shoulder, and neck pain.
Not to mention, the constant squirming and moving on your part can disrupt your baby’s breastfeeding and result in irritability and increased hunger. That’s why it’s so important for you to be comfortable throughout the process.
We recommend one of two positions for comfortable breastfeeding:
- Lie on your side with your baby facing you.
- Sit in a reclined position with your baby lying in your arms.
A bed or a large couch with plenty of pillows to support your back and arms make these positions ideal for breastfeeding. Find the one that’s right for you but don’t be afraid to mix it up once in a while depending on your own needs. The more attentive you are to your own comfort, the more nursing sessions will be a pleasant break for both you and your baby.
4) Relax
In addition to making sure you and the baby are comfortable while nursing, try your best to relax. Your baby can sense if you’re tense and nervous about breastfeeding, and they won’t latch on correctly.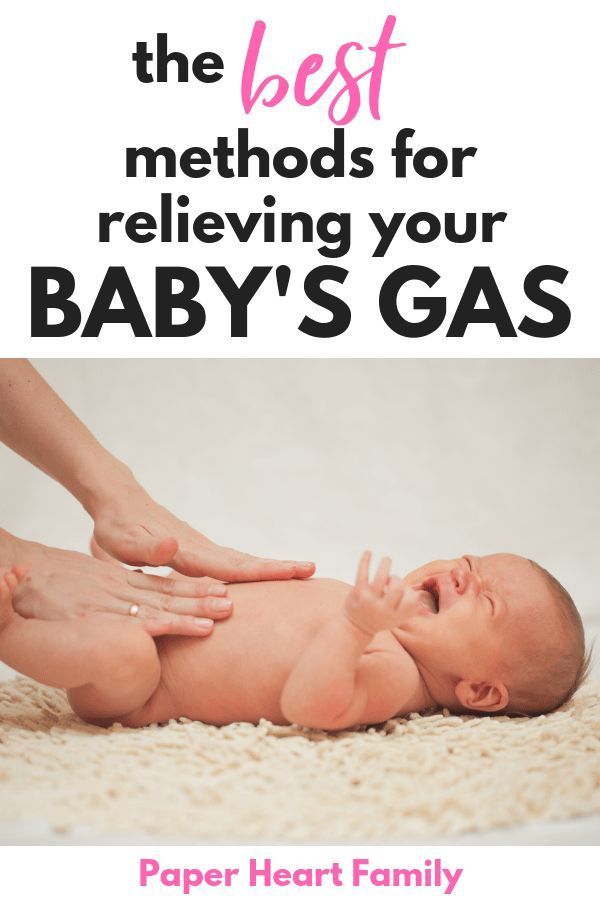 Your baby can’t relax if you’re not relaxed.
Your baby can’t relax if you’re not relaxed.
Examine your environment as well. If you’re in a stressful environment or an environment that makes you uncomfortable, opt for a change of scenery.
Maybe spend a few minutes before nursing to give yourself a pep talk. Take a few slow, deep breaths. Visualize your happy place. This is supposed to be an enjoyable time of bonding with your new bundle of joy, not a stressful one.
5) Help Your Baby Find The Right Position
Through the course of breastfeeding, your baby will likely find the position that’s best for them. Pay attention to this position so that you can make it easier to get into quickly. Every baby is different, but there are a few general guidelines that you can use to find a position that works for both you and your baby.
- Your baby should be positioned so that their mouth is level with your nipple.
- They should not have to turn their head much, if at all.
- Their head should be tilted backward slightly.

- If possible, they should latch onto the entire areola, not just the nipple.
- Their chin should be right up against your breast so that their nose is clear.
First and foremost, don’t force these positions. Your baby may prefer a slightly different position. Just let it happen naturally while you make sure that your baby is comfortable and can breathe while they nurse.
6) Don’t Be Alarmed, Leaking Is Natural
In the first few weeks of breastfeeding, it’s common for milk to leak from your breasts. Don’t be alarmed, this is completely natural. It can happen when you hear another baby cry, when your baby hasn’t nursed for several hours, when you think about your baby, or even when you feel a strong emotion.
This leaking will eventually lessen or disappear completely as your baby continues to nurse. In the meantime, simply place a nursing pad in your bra to absorb the leaks.
7) Take Care Of Your Skin
The skin of your breasts is very delicate. With regular nursing, your skin can become dry, chapped, irritated, and even cracked over time. This can make breastfeeding a painful experience. Luckily, you can protect against chapped, cracked skin by taking a few precautions.
With regular nursing, your skin can become dry, chapped, irritated, and even cracked over time. This can make breastfeeding a painful experience. Luckily, you can protect against chapped, cracked skin by taking a few precautions.
- Don’t overwash. One or two showers a day with a gentle cleanser is plenty.
- After a feeding, pat your breasts dry with a soft cloth.
- Let your breasts air out periodically to avoid irritation from clothing.
- After a feeding, apply a healing product like Mustela’s Soothing Moisturizing Balm or Bust Firming Serum.
- Use Mustela's Nursing Comfort Balm in-between feedings to ease discomfort and moisturize sensitized nipples.
Taking care of your skin with a healing product is one of the best ways to keep the breastfeeding process enjoyable for both you and your baby. When you’re comfortable, your baby will be comfortable and you can use nursing as a way to deepen the already strong bond you feel for your newborn child.
8) Don’t Worry, You’ll Have Enough Milk
Milk production depends primarily on your baby’s needs. Your little one’s sucking stimulates the release of the hormones prolactin and oxytocin which further stimulate milk production. But it doesn’t start with your baby’s first suckle. Your breasts have been preparing to give milk since the start of your pregnancy.
So don’t worry, you will have enough milk. The more your baby nurses, the more milk you’ll have.
During the first two or three days of breastfeeding, you may notice a thick yellowish-orange fluid coming out of your breasts. Don’t panic. That fluid is colostrum and it’s just what your baby needs at the moment. Colostrum is very nutritious and contains high levels of antibodies. These antibodies boost your baby’s immune system so they can fight off infection.
9) Look For Signs That Breastfeeding Is Going Well
- Your baby’s behavior and health will tell you if nursing is going well or not.
 Don’t worry if you don’t see these signs all the time. Even just one is an indication that your baby is well-fed.
Don’t worry if you don’t see these signs all the time. Even just one is an indication that your baby is well-fed. - While feeding, your baby should suck eagerly and swallow regularly. Keep in mind that, when your little one first starts feeding, they’ll swallow each time they suck. As milk decreases, they get full, or fall asleep, swallowing will decrease. That’s perfectly natural and nothing to worry about.
- At the end of a nursing session, your baby should release your breast and appear drowsy. Their skin will be a healthy pink and their muscles will be totally relaxed.
- Your baby’s diapers should be very wet while they are breastfeeding. They will likely have four to eight bowel movements each day during the first few weeks of life. This is due primarily to colostrum consumption. As time goes on, your little one will have fewer and fewer bowel movements. There may come a time when they only have one bowel movement or less per day. As long as those bowel movements remain soft and the diapers are wet with urine, there’s no need to be worried about constipation.

- Your baby is gaining weight regularly. It’s not necessary, however, to weigh your baby daily or, worse yet, to weigh them before or after each feeding. That would serve no purpose other than to cause you anxiety. If your baby is healthy, the monthly weigh-in by the pediatrician is more than sufficient. Still, if it makes you feel better, you can weigh your baby once per week at home.
10) Avoid Engorgement
Engorgement is a painful swelling and hardening of your breasts that occurs when you produce more milk than your baby consumes. Engorgement is most frequent when your milk first comes in right after your baby is born.
The swelling can actually make it more difficult for your baby to feed, which only increases the likelihood that engorgement will continue. The best way to avoid this painful condition is to nurse your baby as often as possible.
If engorgement persists, you can hand-express breast milk by gently massaging the areola between your fingers. You may want to express milk under a warm shower, which helps the milk flow more easily. If you don’t succeed, try using a pump, and continue until your breasts soften and feel comfortable again.
You may want to express milk under a warm shower, which helps the milk flow more easily. If you don’t succeed, try using a pump, and continue until your breasts soften and feel comfortable again.
11) Ask For Help
Reading and taking a class about breastfeeding is one thing — actually breastfeeding on your own is a different story. So ask for help within that first hour after birth when you’ll want to start breastfeeding your little one.
In your local hospital, a nurse will check on you and your baby while breastfeeding. She may even offer some advice and help you. But if you’re still having trouble, the lactation consultant can help further...but you have to ask. Otherwise, they won’t know your needs.
While you’re still in the hospital, the lactation consultant can come in to see for herself how your baby is latching on. She’ll be able to give you guidance and advice on how to position your baby and your body.
The lactation consultant is more than happy to help you and guide you in your breastfeeding journey.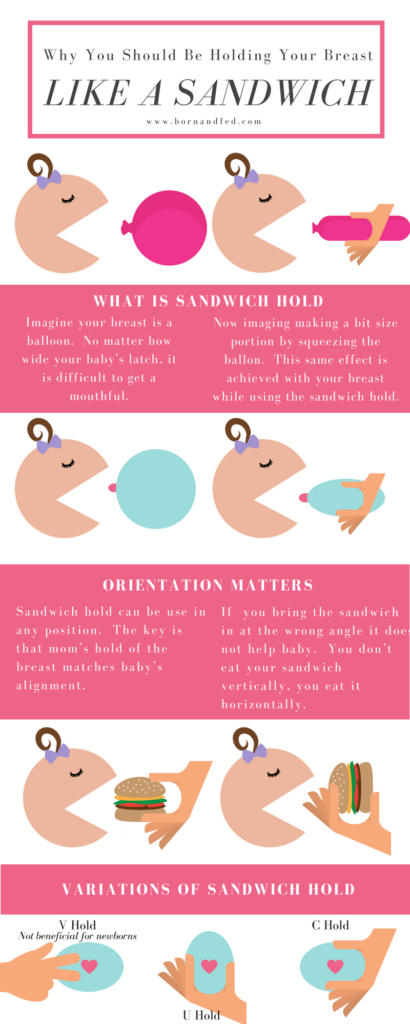 We know it can be a little nerve-wracking leaving the hospital and the support of the nurses, but feel free to call your local hospital and ask to speak to the lactation consultant with any questions you may have.
We know it can be a little nerve-wracking leaving the hospital and the support of the nurses, but feel free to call your local hospital and ask to speak to the lactation consultant with any questions you may have.
Breastfeeding might be uncomfortable at first when your baby latches on, but it shouldn’t be a painful experience for you. If breastfeeding is hurting bad enough to make you cringe, seek out help from a professional.
12) Stay Hydrated
Last, but certainly not least, stay hydrated. We can’t stress enough how important this tip is for you and your baby. After all, you’re still eating and drinking for two!
Water replenishes the body, so a good rule of thumb is to drink a glass of water whenever you breastfeed. Yes, every single time. This will ensure that your body can make enough milk and that you’re staying hydrated.
Breastfeeding Tips: Taking It All In
We know breastfeeding can be overwhelming at times, but putting the tips above into practice will help you make the most of your time with your little one while breastfeeding. So pay close attention to your little one’s needs, get comfortable, and relax. Evaluate the signs that breastfeeding is going well, and make sure you’re staying hydrated.
So pay close attention to your little one’s needs, get comfortable, and relax. Evaluate the signs that breastfeeding is going well, and make sure you’re staying hydrated.
Remember, there’s nothing wrong with asking for help. Your baby will thrive right before your eyes when you follow these tips!
Breastfeeding a newborn | What to Expect in the First Week
The first week of a baby's life is a wonderful but hectic time, especially if you haven't breastfed before. Our breastfeeding tips will help you settle in as quickly as possible
Share this information
The first time after childbirth, mothers are often confused. The body is still recovering, and you are already starting to get to know your newborn baby. The emotional state during this period can be unstable, especially between the second and fifth day, when many women have milk 1 and at the same time postpartum depression begins 2 .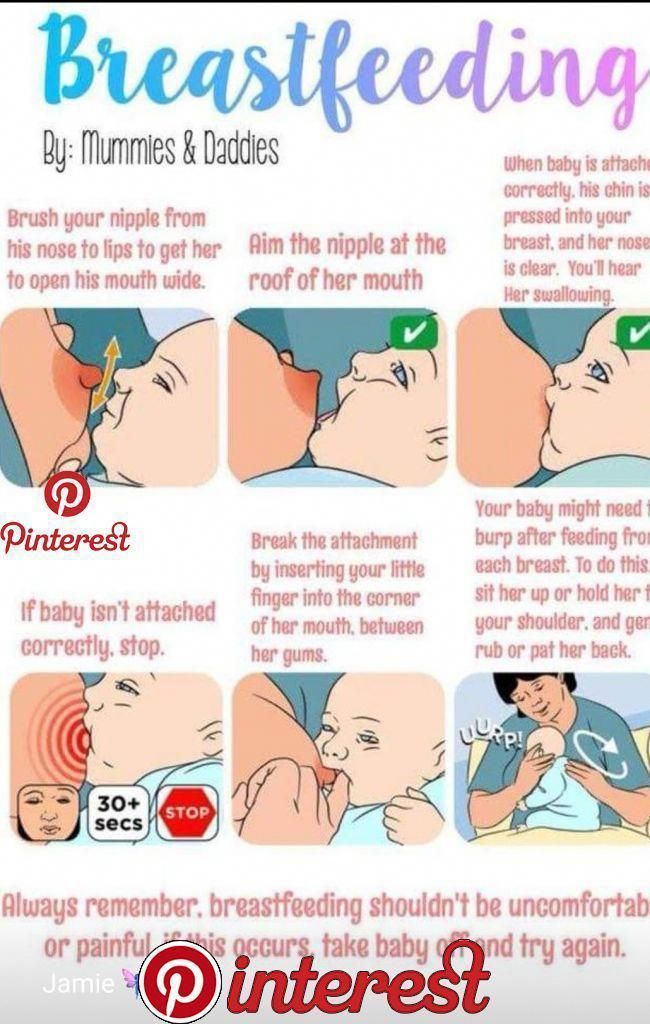 In addition, people around often expect (and demand) that a woman come to her senses as soon as possible and become a “super mom”. But the best thing to do this first week is just to be with your baby and get breastfeeding going.
In addition, people around often expect (and demand) that a woman come to her senses as soon as possible and become a “super mom”. But the best thing to do this first week is just to be with your baby and get breastfeeding going.
When should I start breastfeeding my newborn?
Try to breastfeed your baby within the first hour after birth. When the baby latch onto the breast and begins sucking rhythmically, it stimulates the mammary gland cells and starts milk production. 1 It is not for nothing that this time is called the “magic hour”!
“Ideally, the baby should be placed on the mother's stomach immediately after birth so that it can immediately attach to the breast. He won't necessarily eat, but he should be able to,” explains Cathy Garbin, an internationally recognized expert on breastfeeding.
“Hold your baby and let him find the breast on his own and put the nipple in his mouth. This is called the breast-seeking reflex. On the Internet you can watch videos that show what this process looks like. If the baby does not latch onto the nipple on its own, the midwife will help to properly attach it to the breast. But for starters, it’s good to give the baby the opportunity to do it on their own. In this case, the optimal position for the mother is reclining. ”
If the baby does not latch onto the nipple on its own, the midwife will help to properly attach it to the breast. But for starters, it’s good to give the baby the opportunity to do it on their own. In this case, the optimal position for the mother is reclining. ”
Don't spend that special first hour of your baby's life weighing and swaddling—or at least wait until he's suckling for the first time. Enjoy hugs and close skin-to-skin contact. This promotes the production of oxytocin, the hormone of love, in you and your baby, and oxytocin plays a key role in the supply of the first breast milk - colostrum. 3
“As soon as the obstetricians were convinced that our son was healthy, the three of us — me, my husband and our baby — were left to give us the opportunity to get to know each other. It was a very special hour - an hour of awkwardness, turbulent emotions and bliss. During this time, I breastfed my son twice, ”recalls Ellie, a mother of two from the UK.
Did you know that breastfeeding helps to recover after childbirth? This is because oxytocin stimulates uterine contractions.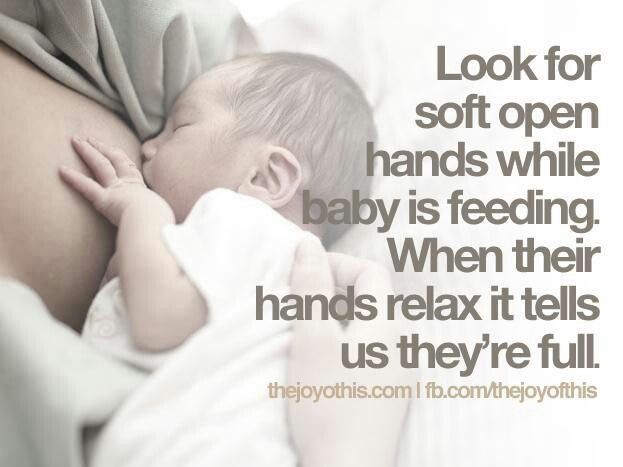 In the first hours after childbirth, this contributes to the natural release of the placenta and reduces blood loss. 4
In the first hours after childbirth, this contributes to the natural release of the placenta and reduces blood loss. 4
What if the birth did not go according to plan?
If you had a cesarean section or other complications during childbirth,
You can still make skin-to-skin contact with your baby and breastfeed him in the first hours after birth.
“If you can't hold your baby, have your partner do it for you and make skin-to-skin contact with the baby. This will give the baby a sense of security, care and warmth so that he can hold on until you recover, ”Katie advises.
If the baby is unable to breastfeed, it is advisable to start expressing milk as early as possible and do so as often as possible until the baby is able to feed on its own. “While breastfeeding in the first hours after birth lays an excellent foundation for the future, it is not so important,” Cathy reassures. “It is much more important to start lactation so that in the future, if necessary, you can start breastfeeding.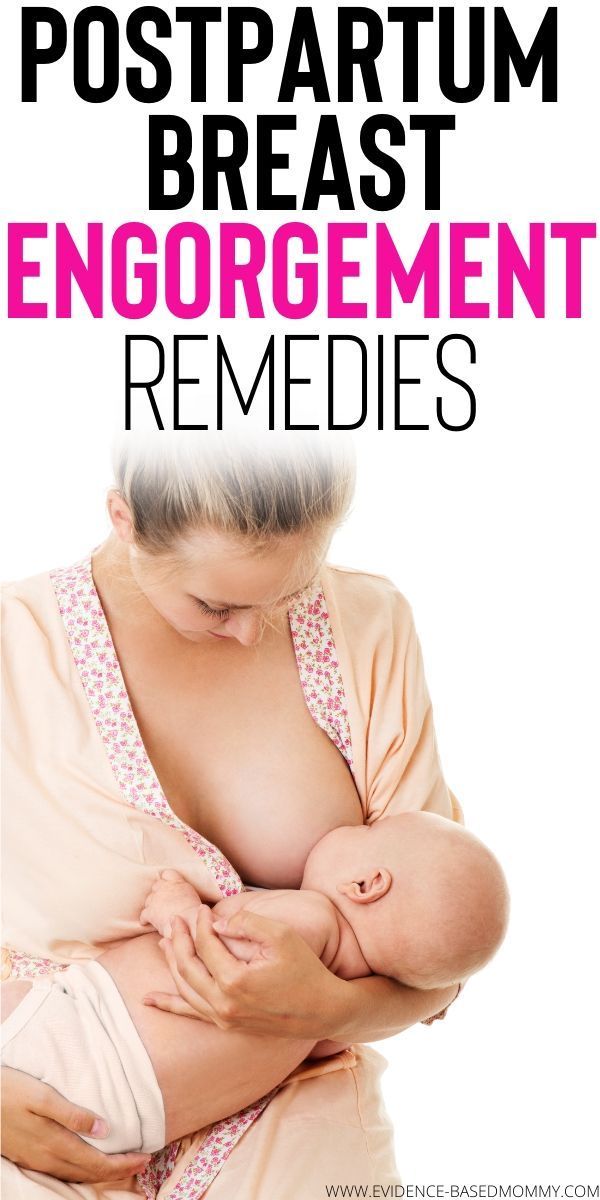 ”
”
To start milk production, you can express milk manually or use a breast pump that can be given to you at the hospital. 5 And with expressed precious colostrum, it will be possible to feed the child. This is especially important if the baby was born premature or weak, since breast milk is extremely healthy.
If a baby was born prematurely or has a medical condition and cannot be breastfed immediately, this is no reason not to continue breastfeeding. “I have worked with many new mothers who were unable to breastfeed their baby for the first six weeks due to preterm labor or other reasons. Nevertheless, all of them later successfully switched to breastfeeding,” says Kathy.
Does the baby latch on correctly?
Correct breastfeeding is essential for successful breastfeeding 6 , as it determines how effectively the baby will suckle milk and hence grow and develop. Latching on the breast incorrectly can cause sore or damaged nipples, so don't hesitate to ask your doctor to check that your baby is properly attached to the breast, even if you are told that everything is fine and you do not see obvious problems - especially while you are in the hospital.
“While I was in the hospital, I called the doctor at every feed and asked me to check if I was breastfeeding correctly,” says Emma, mother of two from Australia. - There were several cases when it seemed to me that everything seemed to be right, but it was painful to feed, and the doctor helped me take the baby off the breast and attach it correctly. By the time I was discharged, I had already learned to do it confidently.”
When applying to the breast, point the nipple towards the palate. This will allow the baby to take the nipple and part of the areola under it into their mouth. It will be easier for him to suck if he has both the nipple and part of the areola around in his mouth. 6
“When a baby latch on properly, it doesn't cause discomfort and it causes a pulling sensation, not pain,” Cathy explains. - The baby's mouth is wide open, the lower lip may be slightly turned outward, and the upper one lies comfortably on the chest. The body language of the child indicates that he is comfortable. There isn't much milk at this early stage, so you probably won't notice your baby swallowing, but he will suckle a lot and nurse frequently."
There isn't much milk at this early stage, so you probably won't notice your baby swallowing, but he will suckle a lot and nurse frequently."
How often should a newborn be fed?
The frequency and duration of breastfeeding in the first week can vary greatly. “The first 24 hours of life are completely different for different children. Someone sleeps a lot (after all, childbirth is tiring!), And someone often eats, says Katie. - Such a variety greatly confuses young mothers. Everyone gives different advice, so it's important to remember that every mother and child is different."
“Colostrum is thicker than mature breast milk and is produced in smaller amounts, but has many benefits. When the baby eats colostrum, he learns to suck, swallow and breathe until milk begins to flow in more volume, ”explains Cathy.
Milk usually arrives on the second or fourth day after delivery. Until this time, the baby is applied to the breast 8-12 times a day (and sometimes more often!), including at night.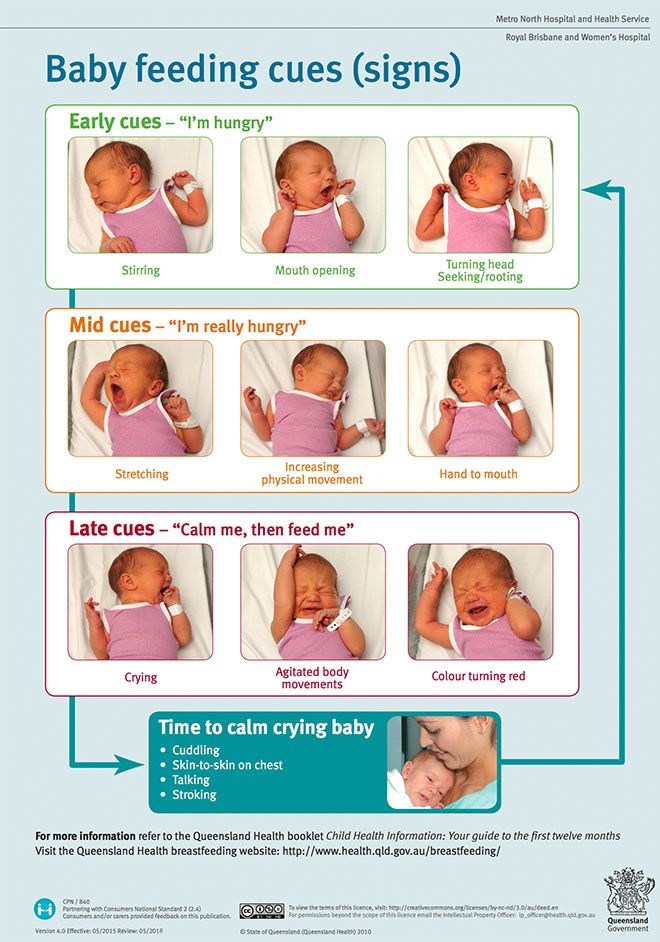 7 Feeding may last 10-15 minutes at this stage, or 45 minutes or even an hour, as the baby is just beginning to develop the muscles and coordination needed to suckle effectively.
7 Feeding may last 10-15 minutes at this stage, or 45 minutes or even an hour, as the baby is just beginning to develop the muscles and coordination needed to suckle effectively.
“At first, the intensity of feeding is very high, often higher than many people realize, and this is shocking to most new mothers,” says Cathy. - Sometimes mom has no time to go to the toilet, take a shower and have a snack. It usually comes as a surprise."
Camille, a mother from Australia, experienced this. “The first week, Frankie ate every two hours, day and night, and each time it took half an hour to an hour to feed,” she recalls. “My husband and I were completely exhausted!”
Do I need to feed my newborn on a schedule?
The good news is that frequent feeding promotes lactation and stimulates milk production. 7 The more your baby eats, the more milk you will have. Therefore, forget about feeding your newborn on a schedule - this way he will have less chance of feeding. Try to feed your baby when he signals that he is hungry 8 :
Try to feed your baby when he signals that he is hungry 8 :
- tossing and turning in her sleep;
- opens eyes;
- turns his head if he feels a touch on his cheek;
- sticks out tongue;
- groans;
- licks lips;
- sucks fingers;
- is naughty;
- whimpers;
- is crying.
Crying is the last sign of hunger, so when in doubt, just offer your baby the breast. If he bursts into tears, it will be more difficult to feed him, especially at first, when both of you are just learning how to do it. As your baby grows, he will likely eat less frequently and take less time to feed, so breastfeeding will seem more predictable.
Does breastfeeding hurt?
You may have heard that breastfeeding is not painful at all, but in fact, in the first days, many new mothers experience discomfort. And this is not at all surprising, given that the nipples are not used to such frequent and strong sucking.
“Breastfeeding can be uncomfortable for the first couple of days – your body and your baby are just getting used to it. If a baby eats for too long and does not latch well, the sensations are almost the same as from unworn new shoes, Cathy compares. Just as tight shoes can rub your feet, improper suckling can damage your nipples. Prevention is always better than cure, so if the pain persists after a few days of feeding, contact a lactation consultant or healthcare professional.”
Maria, a mother from Canada, agrees: “Although my son seemed to latch onto the breast well, he damaged his nipples while feeding, and I was in pain. As it turned out, the reason was a shortened frenulum of the tongue. The breastfeeding specialists at our city clinic have been of great help in diagnosis and treatment.”
In addition, you may experience period cramps during the first few days after breastfeeding, especially if this is not your first baby. This is the so-called postpartum pain. The fact is that oxytocin, which is released during breastfeeding, contributes to further contraction of the uterus to restore its normal size. 4
The fact is that oxytocin, which is released during breastfeeding, contributes to further contraction of the uterus to restore its normal size. 4
When milk arrives, the breasts usually become fuller, firmer and larger than before delivery. In some women, the breasts swell, harden and become very sensitive - swelling of the mammary glands occurs. 10 Frequent breastfeeding relieves these symptoms. For more breast care tips, read our article What is Breast Swelling?
How often does the newborn urinate and defecate?
What goes into the body must go back out. Colostrum
has a laxative effect, helping to eliminate meconium - the original feces. It looks a little scary - black and sticky, like tar. 11 But don't worry, it won't always be like this. Breastfed babies usually have a slightly sweet smell of stool.
How many times a day you will need to change diapers and how the contents should look like, see below.
Day one
- Frequency: once or more.

- Colour: greenish black.
- Texture: sticky like tar.
Day two
- Frequency: twice or more.
- Colour: dark greenish brown.
- Texture: less sticky.
Day three
- Frequency: twice or more.
- Colour: greenish brown to brownish yellow.
- Texture: non-sticky.
Fourth day and then the entire first month
- Frequency: twice or more.
- Color: yellow (feces should turn yellow no later than by the end of the fourth day).
- Texture: grainy (like mustard with grains interspersed). Leaky and watery.
The baby's urine should be light yellow. On average, babies urinate once a day for the first two days. Starting around the third day, the number of wet diapers increases to three, and from the fifth day onwards, diapers have to be changed five times a day or more often. In addition, during the first few days, the weight of wet diapers increases.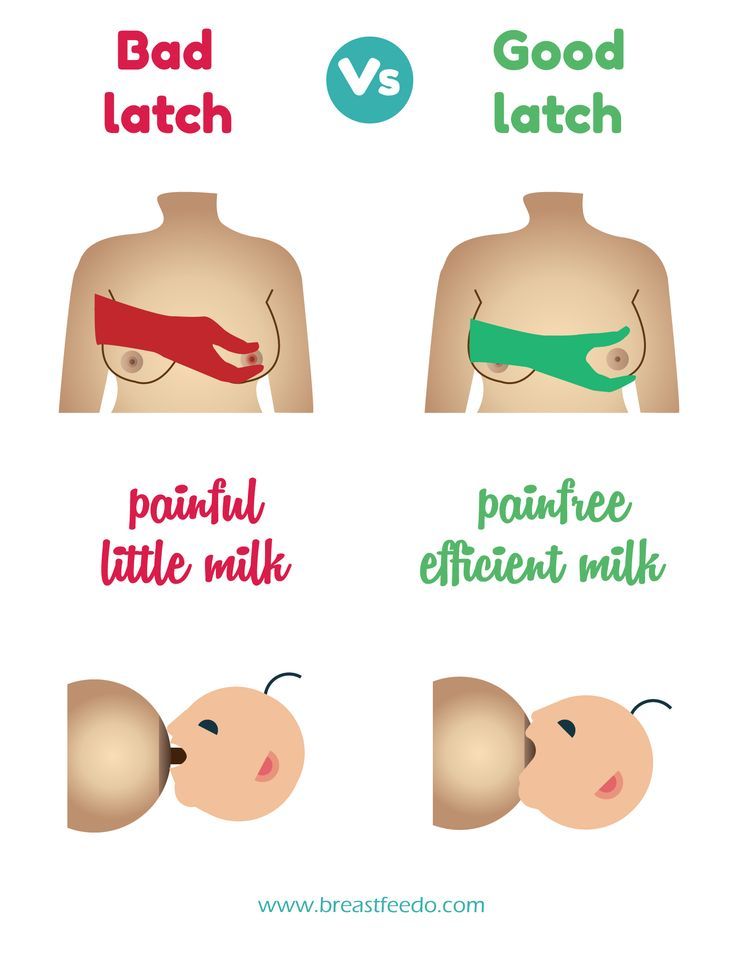 11
11
Is the baby getting enough breast milk?
Since very little milk is produced at first,
You may feel that this is not enough for your baby. But if you feed your baby on demand, you will produce exactly as much milk as he needs. If you want to keep the process under control, be guided by the frequency of diaper changes above. If your baby soils less diapers, check with your doctor.
“For the first three or four weeks, most babies just eat and sleep. If the child is worried and constantly asks for a breast, you should consult with your doctor, ”Katie recommends.
Sometimes the baby may vomit after feeding. If the vomit is the color of milk, this is not a cause for concern. But if there are orange, red, green, brown or black blotches in it, or the child vomits with a "fountain", consult a doctor. You should also consult a doctor if the baby has a high temperature, the fontanel (soft spot on the head) has sunk, blood is found in the stool, and also if the weight recorded at birth has not recovered within two weeks.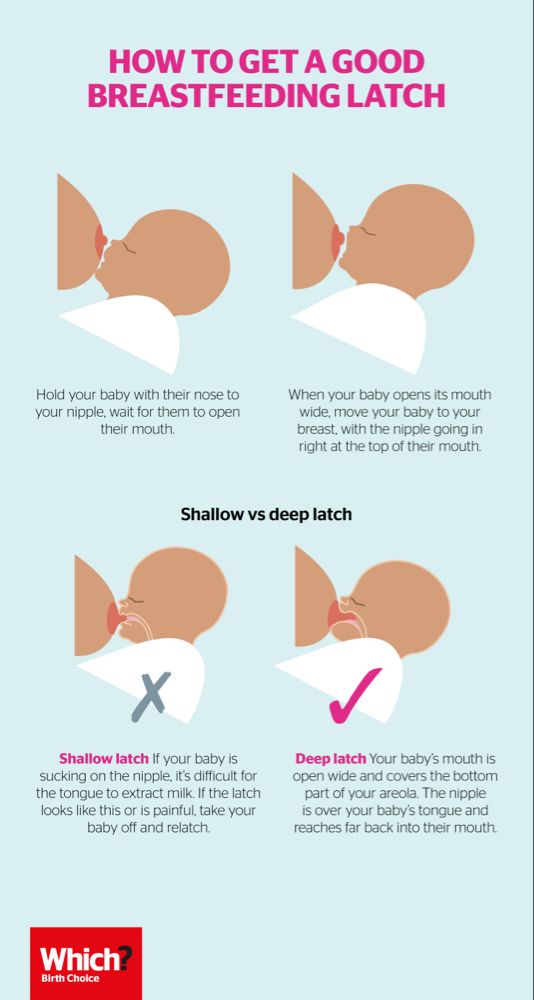 11
11
But if there are no frightening symptoms and the baby is growing at a normal pace, it means that he has enough milk. Soon you will both get used to breastfeeding and establish a more stable routine.
For the next step in breastfeeding, see Breastfeeding in the First Month: What to Expect.
Literature
1 Pang WW, Hartmann PE. Initiation of human lactation: secretory differentiation and secretory activation. J Mammary Gland Biol Neoplasia 2007;12(4):211-221. - Pang, W.W., Hartmann, P.I., "Lactation initiation in the lactating mother: secretory differentiation and secretory activation." G Mammary Gland Biol Neoplasia. 2007;12(4):211-221.
2 Shashi R et al. Postpartum psychiatric disorders: Early diagnosis and management. Indian J Psychiatry .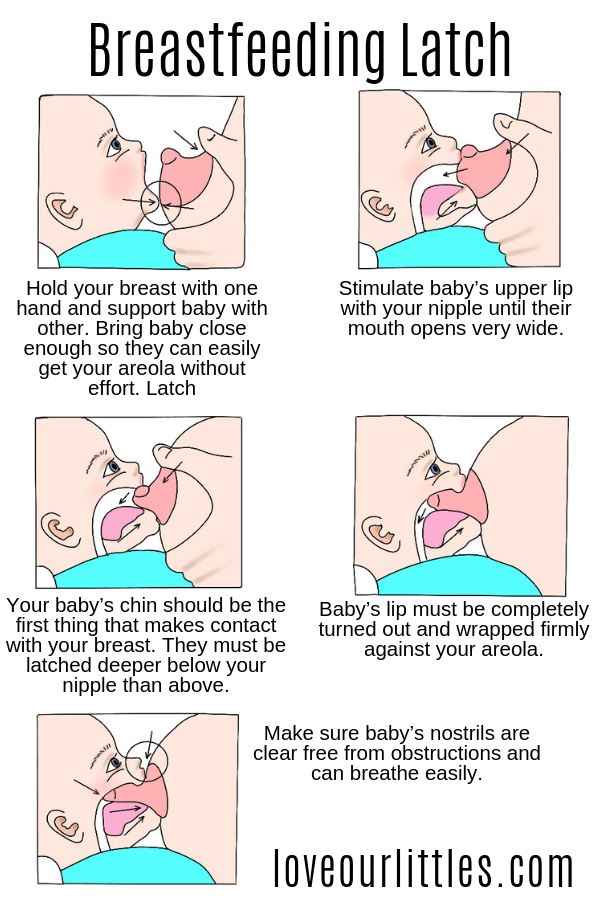 2015; 57( Suppl 2): S 216– S 221. - Shashi R. et al., Postnatal mental disorders: early diagnosis and treatment. Indian J Saikiatri. 2015; 57(App 2):S216-S221.
2015; 57( Suppl 2): S 216– S 221. - Shashi R. et al., Postnatal mental disorders: early diagnosis and treatment. Indian J Saikiatri. 2015; 57(App 2):S216-S221.
3 Moberg KU, Prime DK. Oxytocin effects in mothers and infants during breastfeeding. Infant . 2013;9(6):201-206. - Moberg K, Prime DK, "The effects of oxytocin on mother and child during breastfeeding." Infant. 2013;9(6):201-206.
4 Sobhy SI, Mohame NA. The effect of early initiation of breast feeding on the amount of vaginal blood loss during the fourth stage of labor. J Egypt Public Health Assoc . 2004;79(1-2):1-12. - Sobhi SI, Moham NA, "Early initiation of breastfeeding and its effect on vaginal bleeding in the fourth stage of labor." G Egypt Public Health Assoc.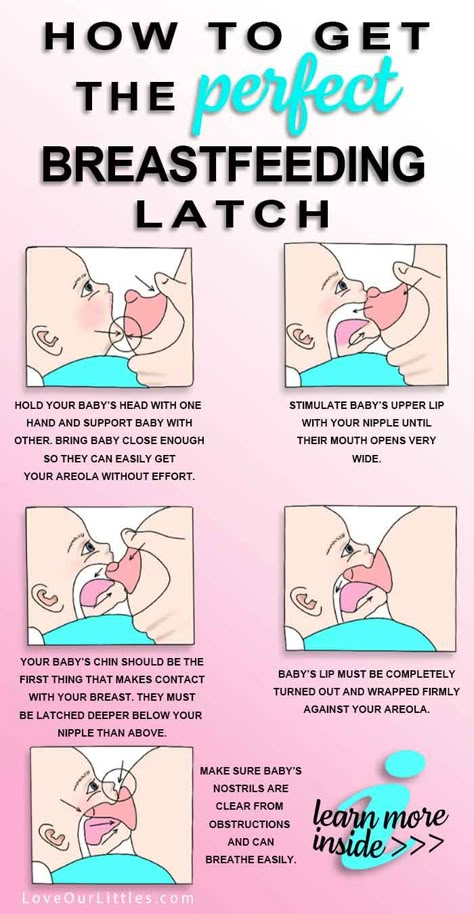 2004;79(1-2):1-2.
2004;79(1-2):1-2.
5 Meier PP et al. Which breast pump for which mother: an evidence-based approach to individualizing breast pump technology. J Perinatol . 2016;36(7):493. - Meyer P.P. et al., Breastpump Selection: A Scientific Approach to Customizing Pumping Technology. J Perinatol (Journal of Perinatology). 2016;36(7):493-499.
6 Cadwell K. Latching - On and Suckling of the Healthy Term Neonate: Breastfeeding Assessment. J Midwifery & Women ’ s 2007;52(6):638-642. — Cadwell, K., "Latching and sucking in healthy newborns: evaluation of breastfeeding." W Midwifery Women Health. 2007;52(6):638-642.
7 Kent JC et al. Principles for maintaining or increasing breast milk production. 2012;41(1):114-121. - Kent J.S. et al. , "Principles for Maintaining and Increasing Milk Production". J Obstet Ginecol Neoneutal Nurs. 2012;41(1):114-121.
, "Principles for Maintaining and Increasing Milk Production". J Obstet Ginecol Neoneutal Nurs. 2012;41(1):114-121.
8 Australian Breastfeeding Association [ Internet ]. Feeding cues ; 2017 Sep [ cited 2018 Feb ]. - Australian Breastfeeding Association [Internet], Feed Ready Signals; September 2017 [cited February 2018]
9 Jacobs A et al. S3-guidelines for the treatment of inflammatory breast disease during the lactation period. Geburtshilfe Frauenheilkd . 2013;73(12):1202-1208. - Jacobs A. et al., "Guidelines S -3 for the management of inflammatory breast disease during breastfeeding." Geburtskhilfe und Frauenheilkünde. 2013;73(12):1202-1208.
10 Lawrence RA, Lawrence RM.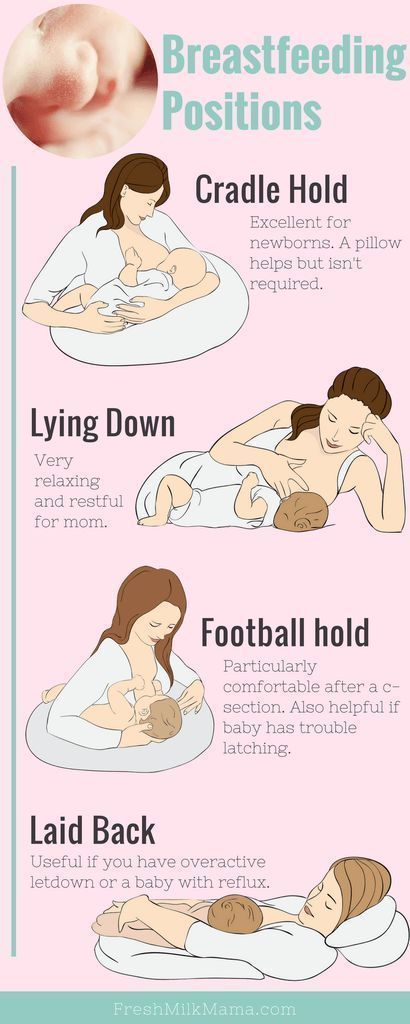 Breastfeeding: A guide for the medical profession. 7th ed. Maryland Heights MO, USA: Elsevier Mosby; 2010. 1128 p . - Lawrence R.A., Lawrence R.M., "Breastfeeding: A guide for healthcare professionals." Seventh edition. Publisher Maryland Heights , Missouri, USA: Elsevier Mosby; 2010. P. 1128.
Breastfeeding: A guide for the medical profession. 7th ed. Maryland Heights MO, USA: Elsevier Mosby; 2010. 1128 p . - Lawrence R.A., Lawrence R.M., "Breastfeeding: A guide for healthcare professionals." Seventh edition. Publisher Maryland Heights , Missouri, USA: Elsevier Mosby; 2010. P. 1128.
Breastfeeding for beginners | Philips Avent
search support iconSearch Keywords
Home ›› Beginner Breastfeeding
Home ›› Beginner Breastfeeding
↑ Top
Some of the most common questions about newborns have to do with feeding, which will take up a lot of time during the first few months of a baby's life. In this article, we will discuss all of its main aspects, from the basic principles of breastfeeding to the best tips for effective newborn feeding.
As always, if you have any questions or concerns, seek the opinion of another expert.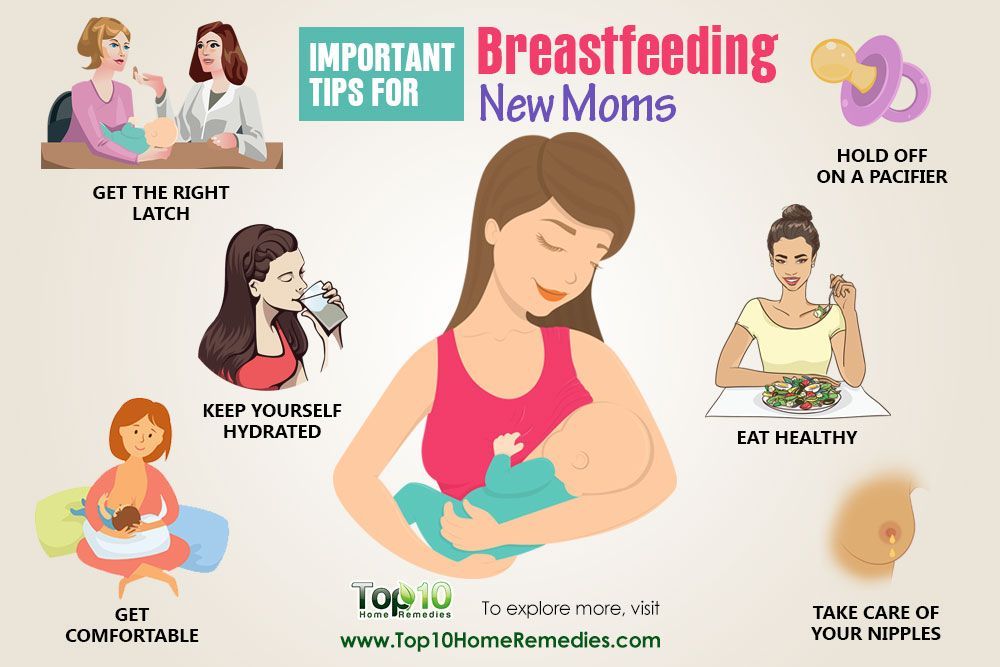
Basic principles of breastfeeding
Although every baby is different, newborns usually eat every two to three hours, for a total of 8 to 12 times a day. In the first one or two days after birth, babies usually drink 25-50 ml of milk per feeding. This volume will gradually increase to 50-75 ml when the baby is about two weeks old.
More information on how much a newborn should eat can be found here.
How long does one feeding last?
Again, every baby is different, so there is no set time frame for every newborn. But in general, breastfeeding a newborn takes five minutes to one hour. This time depends on the size, age of the baby and the frequency and duration of feeding the newborn.
How to start breastfeeding?
In the first minutes of a child's life, the mother should put the baby on her chest and ensure body contact. This time is called the "golden hour": it is at this hour that a connection is established between mother and child and the newborn's natural instinct to seek the breast manifests itself.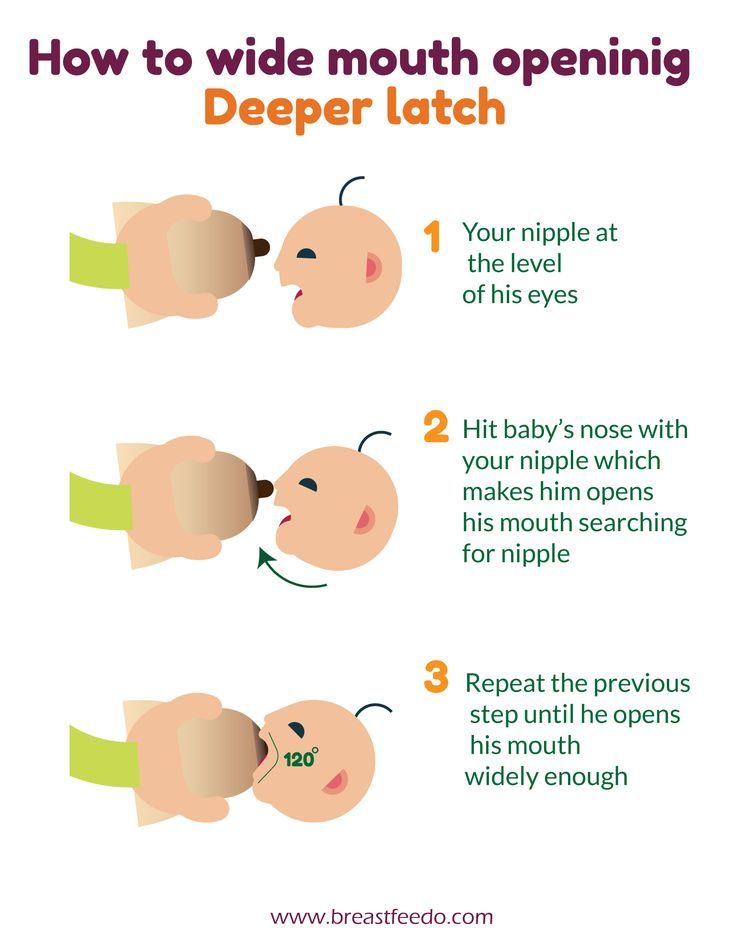 As soon as the child begins to show signs of hunger, you need to give him a breast.
As soon as the child begins to show signs of hunger, you need to give him a breast.
Mothers who are just learning to breastfeed their newborns should remember that comfort is key. There is no better way to ensure breastfeeding success than by creating a comfortable and relaxing environment for the mother. For starters, mom can sit comfortably on the couch, on the bed, or in a chair with pillows to support her back while feeding. Breastfeeding moms can get creative with breastfeeding and choose specific lighting, soothing music, or anything else that helps them relax.
Bring your baby to your breast, not the other way around. If you want to make breastfeeding a newborn easier, then do not lean towards the baby, but bring it to your chest. The baby's mouth should be opposite the nipple, the neck should be straight, and the shoulders and hips should be in line. Mom can also lightly touch her nipple to her baby's nose and mouth to encourage him to latch on.
Support your chest. Holding the newborn with one hand, the mother can place the other hand directly under the breast to support it. When learning to breastfeed, some mothers prefer to leave one hand free; in this case, a rolled towel can be used.
Holding the newborn with one hand, the mother can place the other hand directly under the breast to support it. When learning to breastfeed, some mothers prefer to leave one hand free; in this case, a rolled towel can be used.
Breastfeeding can be done in different positions; experiment with them to find the most comfortable for you and your baby. Below we list the most common breastfeeding techniques:
- Cradle. In this position, the baby lies on the mother's hand from the side of the breast, which he sucks. The baby's head lies on the mother's elbow during feeding.
- Cross cradle. With a cross cradle, the mother holds the baby with the hand opposite to the mammary gland that the baby sucks. With the other hand, mom can support her breasts.
- Underhand or Football. In this position, the mother holds the child next to her, putting her back on her arm. With the other hand, she supports the baby's head, facing the mammary gland, with which she feeds the baby.
- Lying on the side. In this position, the mother lies on her side, and the child lies next to her, facing her chest. Mom can support the child under the back with the hand that is on top, or put a folded towel under the back of the child.
Newborn Breastfeeding Tips
After looking at breastfeeding techniques, here are some tips for new mothers:
1. Make sure your baby latch on properly. A good grip is important for both mother and baby. With a good grip, the baby will suck out milk correctly, and the mother's nipples will not hurt. To achieve a good latch, the mother needs to find a position that makes it easier for the newborn to latch onto the breast, and to do this, she should experiment with different positions. If a mother is having difficulty feeding, she should contact a lactation consultant.
2. Maintain milk supply. Sometimes a nursing mother cannot be constantly with her child during feedings. In such cases, it is very important to maintain milk production. An excellent solution for maintaining milk production when mother and baby are not together is pumping milk.
In such cases, it is very important to maintain milk production. An excellent solution for maintaining milk production when mother and baby are not together is pumping milk.
Take a look at this double breast pump: it reduces pumping time and features a massage petal attachment to gently stimulate milk flow.
3. Breastfeeding everywhere. One of the many benefits of breast milk is that mom always has it with her. But some moms feel awkward at first when they have to breastfeed their baby in public. For such mothers, we recommend that you first practice breastfeeding your newborn in front of a mirror and choose clothes that allow you to cover your breasts during feeding. A shawl or scarf can help with this - with them, the mother will feel more comfortable when feeding the baby outside the home.
And to keep clothes dry and clean while breastfeeding, we recommend that mums use these disposable bra pads with a porous and breathable structure: they do not leak and let air through.
Be prepared for difficulties. It is important for moms not to panic or get upset when faced with a common breastfeeding problem, such as insufficient milk production, breast engorgement, clogged milk ducts, mastitis, or sore nipples. To feel calm and confident during all stages of breastfeeding a baby, mothers need a circle of support: family members, friends, and healthcare professionals. The main thing is to stay calm, but if a mother is concerned about any aspect of breast health, she should definitely see a doctor. Learn more about breastfeeding difficulties and how to overcome them.
Articles and tips from Philips Avent
Baby+ app
Download the app and track your baby's development and growth with trackers and keep those special moments forever.
Download app:
Pregnancy+ app
Download one of the world's best pregnancy tracking apps for weekly helpful information, articles and tips about pregnancy and baby development.