Can a breastfed baby have food allergies
CMPI - Cow’s Milk Protein Intolerance
Usually when it is recommended that a breastfeeding mother eliminate dairy produce from her diet, it is because of a problem that may be caused by the protein it contains, not because of lactose intolerance. Human milk is full of lactose, and nature has made certain that babies and toddlers can digest it. Large protein molecules from cow’s milk can pass into human milk fairly intact and it is these particles that can bother a sensitive baby. If your baby has Cow’s milk protein intolerance (CMPI) he might have colic-like symptoms, and be wheezy, vomit, have diarrhea (including bloody diarrhea), constipation, a rash, eczema and/or a blocked nose.
If you suspect your baby is sensitive to the cow’s milk protein in your diet you can remove dairy products and see if it makes a difference. It can take up to 21 days for all traces of cow’s milk protein to leave your system so it’s best to wait for two to three weeks to evaluate the results. Some babies will react well if you remove visible dairy products such as milk, yoghurt, cheese, cream and ice-cream; others will not show any improvement unless you remove every trace of cow’s milk protein from your diet so you may need to read the labels of all the food you eat and eliminate hidden sources.
Many babies grow out of their sensitivity, so even if your baby is affected you may be able to add dairy back into your diet as your baby gets older. Some mothers wait until their baby has weaned to reintroduce dairy to their diet.
Some babies will show no improvement and it’s possible other elements of a mother’s diet are causing a problem. See our post on allergies.
If you do eliminate dairy from your diet there are many other sources of calcium, such as broccoli, collard greens, kale, bok choi, pak choi, ground sesame seeds, blackstrap molasses, almonds, brazil nuts, canned sardines or salmon (with soft bones).
Some kinds of calcium supplement are better absorbed and utilized by your body than other types. If you want to take one you can ask your healthcare professional which types of calcium supplement you might take.
If you want to take one you can ask your healthcare professional which types of calcium supplement you might take.
Your body will take what it needs from your nutritional stores to make the perfect milk for your baby. Your body might go short on calcium, but your breastmilk won’t! There is also research showing that while a breastfeeding mother will have reduced bone density while she is breastfeeding, she piles on bone density after her baby weans and is actually at reduced risk for osteoporosis compared to a woman who has never breastfed a baby.
When considering if your baby may be sensitive to something you have eaten it is worth checking if another carer has given him anything at all to eat besides your milk.
Smoking cigarettes and drinking caffeinated or alcoholic beverages can sometimes lead to a fussy baby.
Even if your baby is sensitive to something in your milk, it is still the perfect milk for him. Artificial baby milks are made from cow’s milk.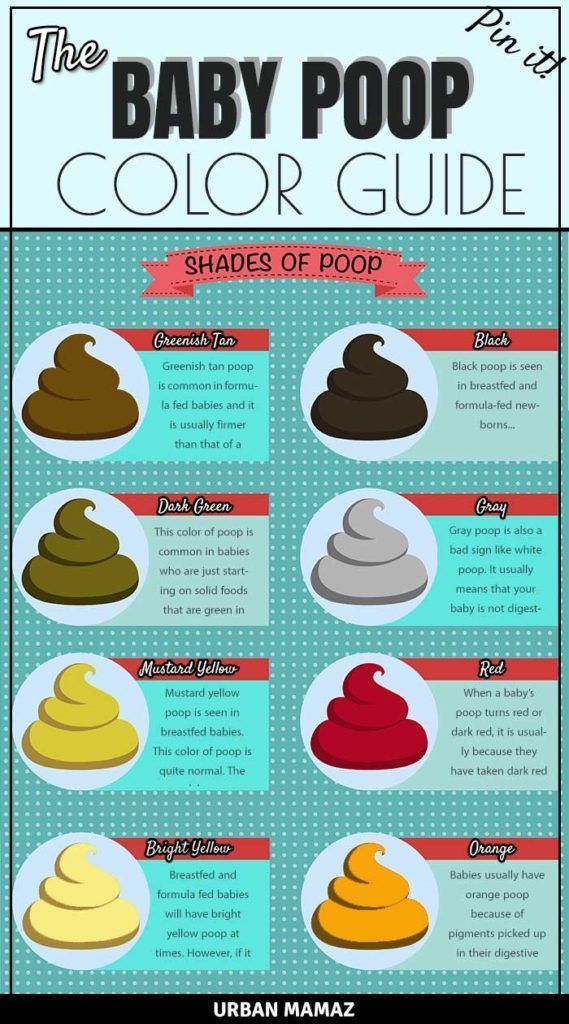 Around half of babies who are sensitive to dairy are also sensitive to soya, and many also react to goat’s and sheep’s milk.
Around half of babies who are sensitive to dairy are also sensitive to soya, and many also react to goat’s and sheep’s milk.
Reflux
Allergies
Alergia a la Proteína de la Leche de Vaca – APLV
Published January 2018.
Peanut Allergy - La Leche League International
Claire K. Dalidowitz, Connecticut, USA
Peanut allergy is a complex medical issue involving many factors such as family history, genetics, ethnicity, environmental influences, baby’s health and development. Claire Dalidowitz is a member of LLLI’s Health Advisory Council (HAC) and in this article she summarizes current research and recommendations for reducing the risk of peanut allergy. Leaders are not medical professionals and as such, can not give advice about peanut allergy or any other medical condition. Leaders can share general information with parents who may be concerned about peanut allergy and encourage them to discuss any concerns with their baby’s health care provider.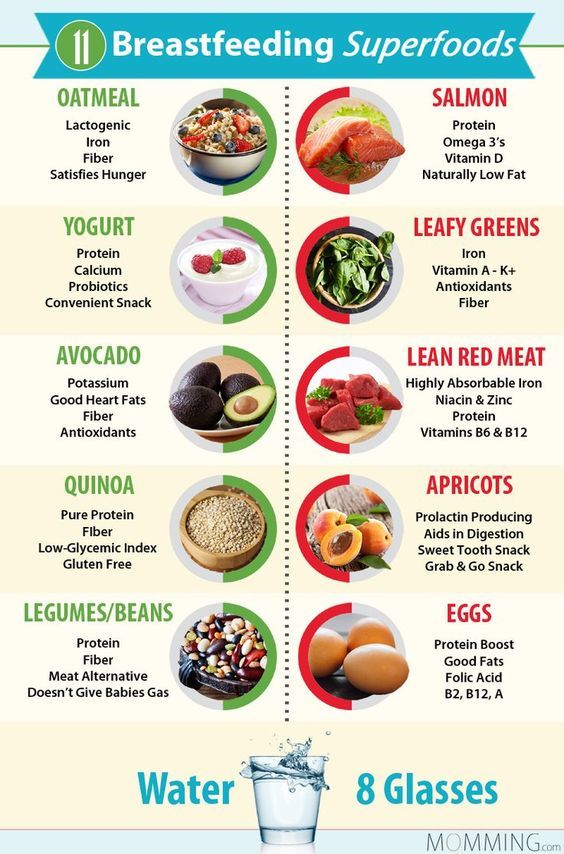
Peanut allergy affects 1.4% to 5% of people depending on their global location. Peanut allergy generally presents at around 18 months of age but can occur sooner or later. From 1997‑2008, peanut allergy increased 11% in developed countries (Savage 2016). Food allergy is influenced by both parental genetics and environmental influences.
Health risksPeanut is one of the allergens that can cause more severe reactions and a higher risk of an anaphylactic reaction causing throat swelling and breathing difficulty. Peanut allergy is less likely to be outgrown than other allergies. In one study, only 22% of children with a confirmed peanut allergy outgrew it by four years of age (Peters, 2015).
Peanuts and pregnancyIn the past, dietary avoidance of peanut during pregnancy was thought to be the best way to avoid peanut allergy. However, this has not been shown to decrease peanut allergy. One study with 8059 non-allergic pregnant mothers who consumed peanut more than five times per month had infants with significantly less peanut allergy than mothers consuming peanut less than once per month (Miles, 2015).
One study with 8059 non-allergic pregnant mothers who consumed peanut more than five times per month had infants with significantly less peanut allergy than mothers consuming peanut less than once per month (Miles, 2015).
Peanut protein (Ara h 6) has been shown to transfer to breast milk within ten minutes after consumption of one ounce (30 g) of peanut protein. The amount in breast milk peaks after one hour but peanut protein can still be detected over a 24 hour period. A study with mice showed that immune complexes IgA and IgG (peanut allergen complexes) are also secreted and led to partial oral tolerance (Bernard 2014). Restricting peanut while breastfeeding is not recommended as it does not prevent peanut allergy (Boyce, 2011)(Kramer, 2012).
Introduction of peanutIn 2000 the American Academy of Pediatrics (AAP) published recommendations to prevent food allergy in infants at risk for allergic disease. It was recommended that peanut introduction be delayed until age three years if there was a history of atopy (allergic symptoms) such as food allergy, atopic dermatitis (eczema) or if there was atopy in two or more first-degree family members (Gupta, Sicherer 2017). During the next decade, the incidence of all allergies increased however. As a result, the AAP re-examined their recommendations and in January 2008 stated that there was no convincing evidence to delay allergenic foods. Agreement came from other professional groups including the European Society for Pediatric Gastroenterology, Hematology and the Nutrition Committee and the Section on Pediatrics of the European Academy of Allergology and Clinical Immunology (Fleischer, 2013).
It was recommended that peanut introduction be delayed until age three years if there was a history of atopy (allergic symptoms) such as food allergy, atopic dermatitis (eczema) or if there was atopy in two or more first-degree family members (Gupta, Sicherer 2017). During the next decade, the incidence of all allergies increased however. As a result, the AAP re-examined their recommendations and in January 2008 stated that there was no convincing evidence to delay allergenic foods. Agreement came from other professional groups including the European Society for Pediatric Gastroenterology, Hematology and the Nutrition Committee and the Section on Pediatrics of the European Academy of Allergology and Clinical Immunology (Fleischer, 2013).
In 2015, a study on the introduction of peanuts called the LEAP study (Learn Early About Peanuts) was published in the United Kingdom. Infants at high risk for allergy were given small amounts of peanut products three times per week. The relative risk of peanut allergy, when compared to a control group restricting peanut, declined 80% if introduced between four and 11 months of age (Du Toit 2015, Fleischer, 2015). In another subsequent study EAT (Enquiring About Tolerance) multiple allergens were given to breastfed infants at three months of age. When the data was analyzed, there were no cases of peanut allergy among the 310 infants who had early introduction of peanut and 13 cases of peanut allergy in those (525 infants) who introduced peanut per parental discretion after six months (Perkin 2016). The amounts of solid food being discussed in connection with peanut allergy trials are very small and can be considered as tastes or “therapy” rather than introducing large amounts of solid food.
The relative risk of peanut allergy, when compared to a control group restricting peanut, declined 80% if introduced between four and 11 months of age (Du Toit 2015, Fleischer, 2015). In another subsequent study EAT (Enquiring About Tolerance) multiple allergens were given to breastfed infants at three months of age. When the data was analyzed, there were no cases of peanut allergy among the 310 infants who had early introduction of peanut and 13 cases of peanut allergy in those (525 infants) who introduced peanut per parental discretion after six months (Perkin 2016). The amounts of solid food being discussed in connection with peanut allergy trials are very small and can be considered as tastes or “therapy” rather than introducing large amounts of solid food.
Most professional groups recommend exclusive breastfeeding for six months. World Health Organization (WHO), American Academy of Pediatrics (AAP), UK’s National Health Service and the Canadian Pediatric Society (CPS), all recommend exclusive breastfeeding for six months due to its nutritional benefits and protection against disease. The Womanly Art of Breastfeeding (p249) explains that introducing solids around the middle of the first year ties in with the arrival of the baby’s own digestive enzymes and their developmental readiness. Will new research on allergy prevention, especially peanut, mean new recommendations for infants who are at high risk for peanut allergy?
The Womanly Art of Breastfeeding (p249) explains that introducing solids around the middle of the first year ties in with the arrival of the baby’s own digestive enzymes and their developmental readiness. Will new research on allergy prevention, especially peanut, mean new recommendations for infants who are at high risk for peanut allergy?
An important study that supports breastfeeding in preventing peanut allergy is the Canadian Asthma Primary Prevention Study (CAPPS). Convincing evidence from this 1994 Canadian study found that the best reduction in peanut allergy occurred when the breastfeeding mother consumed peanuts while breastfeeding and introduced a peanut product to her infant before 12 months of age. It is thought that the passive transmission of peanut allergens in the breast milk along with the maternal immunomodulatory factors in the milk, primes the infant’s immune system to develop tolerance to peanut when it is introduced later (Pitt, 2017). Although there is some evidence for early peanut introduction, there is no convincing evidence for early introduction of other foods (Gupta 2017). Further research on other allergens is in process which will provide more guidance to breastfeeding mothers in the future.
Although there is some evidence for early peanut introduction, there is no convincing evidence for early introduction of other foods (Gupta 2017). Further research on other allergens is in process which will provide more guidance to breastfeeding mothers in the future.
Recommendations for introducing peanut to a baby’s diet varies in different parts of the world.
In UK
The Scientific Advisory Committee on Nutrition (SACN) and the Committee on Toxicity of Chemicals in Food, Consumer Products and the Environment (COT) produced a recent statement: Assessing The Health Benefits And Risks Of The Introduction of Peanut And Hen’s Egg Into The Infant Diet Before Six Months of Age In The UK, SACN-COT, 2018 which recommends introducing peanut alongside breastfeeding between 6-12 months of age. After which time, if well tolerated, it should continue to be included in the diet. For babies at high risk of allergy, medical advice can be sought before introducing allergenic food.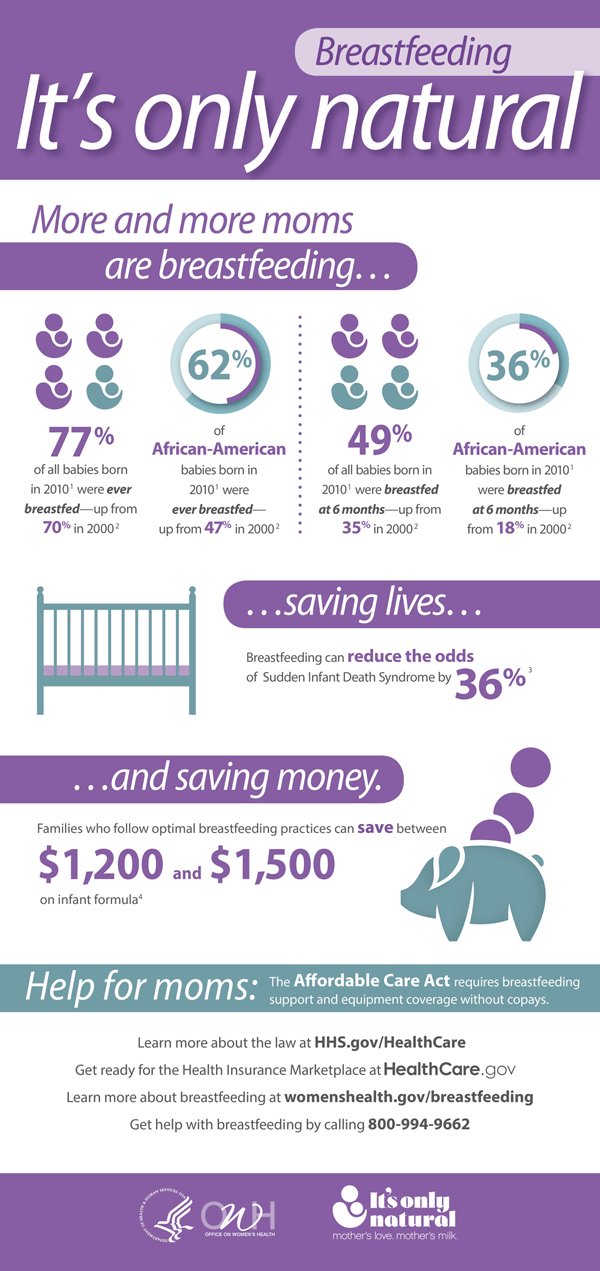
In USA
The National Institute of Allergy and Infectious disease published an addendum to their 2010 recommendations. It recommends that:
- Infants who have severe eczema or those with an egg allergy are at high risk for peanut allergy.
- Screening for peanut allergy with a skin prick test or serum blood test to only peanut should be conducted. Other food allergens should not be tested as they may give false positive results which would result in unnecessary restriction of food.
- If IgE (Immunoglobulin E) blood levels (a marker to measure allergy) are <0.35 KU/L, peanut can be introduced between four and six months of age, under the care of a food allergist who will also evaluate if the baby is developmentally ready to eat solids. The amount of peanut protein to be introduced is very small (two grams, with a total of six grams per week).
- If the IgE level is >0.35 KU/L a food allergist should be contacted to help with the assessment.

- Infants with mild to moderate eczema should start peanut products at around six months of age.
- Those with no history of eczema or food allergy can start peanuts as part of complementary foods during the second six months of life in accordance with family and cultural practices (Togias, 2017).
Developmental oral-motor readiness is important when solid foods are introduced. A pureed type baby food could be introduced first to assess the ability of the infant to consume a more solid food. Soft peanut products are available for infants because peanuts themselves and peanut butter are a choking hazard. Options are thinned smoothed peanut butter (add breast milk), peanut butter powder (with breast milk), smooth peanut butter puree (thinned with breast milk) (Gupta 2017). The purpose of this introduction is to allow the infant’s immune system to adapt to the peanut protein. The quantity given is quite small and is not to be considered as a meal or a supplement.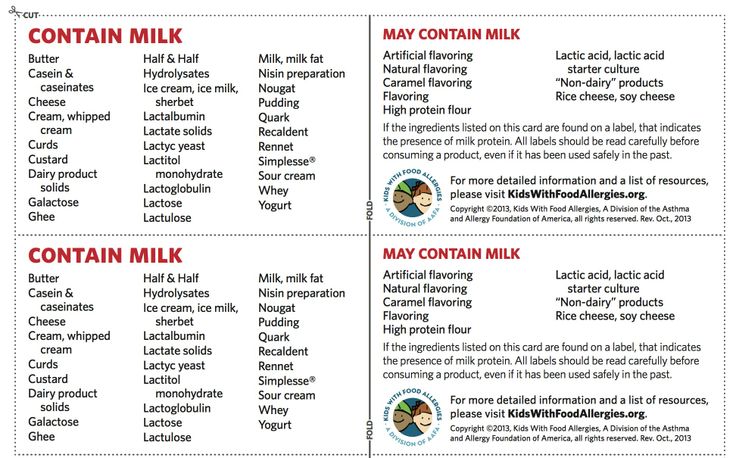
If a sibling has a confirmed peanut allergy, there is a 7% likelihood that the infant may have the same allergy. Some parents may want a food allergy evaluation by a food allergist before introduction (Fleischer, 2013).
Philippines
The Philippine Society of Allergy, Asthma and Immunology published guidelines for allergy prevention and these recommend peanut introduction at 4-11 months (Recto, 2017).
Middle East and North Africa
In a study on physician practice in food allergy prevention in the Middle East and North Africa, 62.5% recommend postponing introduction of allergenic foods despite current research (Vandenplas, 2017).
ExceptionsAllergen introduction may not be able to be generalized to all populations. In Singapore, mothers of Chinese, Malay and Indian ethnicity introduced peanut at a mean age of 19 months. No significant associations were found between this timing and increased food allergy and in fact the incidence was low. Peanut allergy is rare in this population. (Tham, 2017).
Peanut allergy is rare in this population. (Tham, 2017).
Research is ongoing to find other potential ways to prevent the development of food allergy such as the use of probiotics and vitamin D (Fiocci, 2015 and Yepes-Nunez, 2016). Other studies have looked at fish consumption by the mother, omega three fatty acids, ratio of omega six to omega three fatty acids, child’s antioxidant status, and exposure to cigarette smoke and other pollutants (Netting, 2014). Results so far are inconclusive.
Oral Immunotherapy is now being used with older children to diminish the reaction to peanut ingestion. This is used with those who have a confirmed peanut allergy. It involves desensitization by the giving of tiny amounts of peanut protein with increasing doses as tolerated. The benefit of this therapy is that children may tolerate accidental ingestion of small amounts of peanut protein without reaction (Factor, 2012). Oral immunotherapy should only be undertaken with strict medical supervision.
Food allergy and the accompanying atopic diseases asthma, rhinitis, and atopic dermatitis are complex and appear to be multi-factorial. There is some research to support the early introduction of peanut, especially in infants with severe eczema. There is also research to say that all infants should have peanut introduced before 11 months of age (Du Toit 2015; Fleischer 2015). In the non-Asian population, there is, however, support for breastfeeding, consumption of peanuts in the mother’s diet and introduction of peanut to the infant before 12 months (Pitt, 2017), suggesting that both breastfeeding and timing of peanut introduction are important. Parents will need to consult with their health care provider for individualized recommendations for introducing peanut to their child’s diet.
Folllow up research has not shown that early introduction of peanut will prevent other allergic diseases such as asthma, eczema, or tree allergies suggesting that factors for other allergic diseases are genetic or environmental and are distinct from peanut allergy (Du Toit, 2017).
Eating peanuts during lactation promotes the passage of immunomodulatory factors (factors that modify the immune system) into breast milk which helps babies tolerate peanut when it is introduced before 12 months of age. Recommendations for the timing of introduction of peanut to a baby’s diet varies across the world. Parents of infants at high risk of allergy should check with their health care professionals for the latest recommendations in their area and to enable the health professional to guide and supervise the introduction of the peanut product on an individual basis (Togias 2017). All other infants should be exclusively breastfed until six months, when, after successful introduction of some complementary food, a peanut product can be added. Some families may want further evaluation before introduction (Sicherer, 2017).
AAP has retracted their prior recommendations to restrict the major food allergens until after one year of age.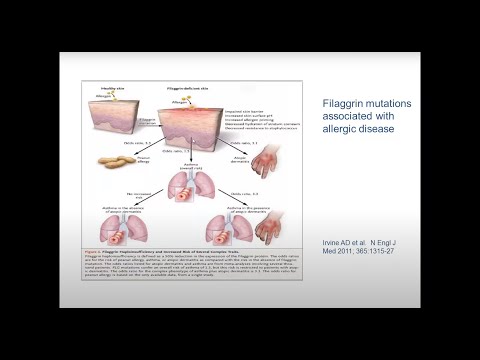
☒
Don’t restrict peanuts during pregnancy in the maternal diet☒
Don’t restrict peanuts in the mother’s diet during lactation☑
Do introduce very small amounts of peanut before 12 months☑
Do continue breastfeeding during the time of introduction as this reduces the possibility ofreaction to an allergen
References
Abrams EM, Greenhawt M, Fleischer DM, Chan ES. . J Pediatrics.2017; 184:13-18.
Bernard H, Ah-Leung S, Drumare MF et al. Peanut allergens are rapidly transferred in human breast milk and can prevent sensitization in mice. Allergy. 2014;888-897.
Bion V, Lockett GA, Soto-Ramirez N et al. Evaluating the efficacy of breastfeeding guidelines on long-term outcomes for allergic disease. Allergy. 2016; 71:661-670.
Boyce JA et al. Summary of the NIAID-sponsored expert panel report. Guidelines for the diagnosis and management of food allergy in the United States. Nutr Res. 2011; 31(1):61-75.
Nutr Res. 2011; 31(1):61-75.
Du Toit G et al. Randomized trial of peanut consumption in infants at risk for peanut allergy. N Engl j Med. 2015;372(9):803-813.
Du Toit G et al. Allergen specificity of early peanut consumption and effect on development of allergic disease in the Learning Early About Peanut Allergy study cohort. J Allergy Clin Immunol. 2017; Oct 31. pii: S0091-6749(17)31664-0. doi: 10.1016/j.jaci.2017.09.034. [Epub ahead of print]
Factor JM, Mendelson L, Lee J et al. Effect of oral immunotherapy to peanut on food-specific quality of life. Ann Allergy Asthma Immunol. 2012;
Feeney M et al. Impact of peanut consumption in the LEAP study: feasibility, growth and nutrition. J Allergy Clin Immunol. 2016;138(4):1108-1118.
Fewtrell M, Bronsky J, Campoy C et al. Complementary feeding: a position paper by the european society for pediatric gastroenterology, hematology, and nutrition (ESPGHAN) committee on nutrition. 2017;64(1):119-132.
Fiocchi et al. World allergy organization-McMaster university guidelines for allergic disease prevention (GLAD-P): Probiotics. WAOJ.2015; 8:4-13.
World allergy organization-McMaster university guidelines for allergic disease prevention (GLAD-P): Probiotics. WAOJ.2015; 8:4-13.
Fleischer DM, Sicherer S, Greenhawt M et al. Consensus communication on early peanut introduction and the prevention of peanut allergy in high-risk infants. Allergy, Asthma & Clin Immunol. 2015; 11:23-26.
Fleishcher DM, Spergel JM, Assa’ad AH, Pongracic JA. Primary prevention of allergic disease through nutritional interventions. J Allergy Clin Immunol: in practice. 2013;1:29-36.
Gupta M, Sicherer SH. Timing of food introduction and atopy prevention. Clinics in Dermatology. 2017;35:398-405.
Hornell A, Hofvander Y, kylberg E. Solids and Formula: Association With Pattern and Duration of Breastfeeding. Pediatrics. 2001;107:E38.
Koid AE, Chapman MD, Hamilton RG et al. Ara h 6 complements ara h 2 as an important marker for IgE reactivity to peanut. J Agric Food Chem. 2014; 62(1): 206-213.
Kramer MS, Kakuma R. Maternal dietary antigen avoidance during pregnancy or lactation, or both, for preventing or treating atopic disease in the child.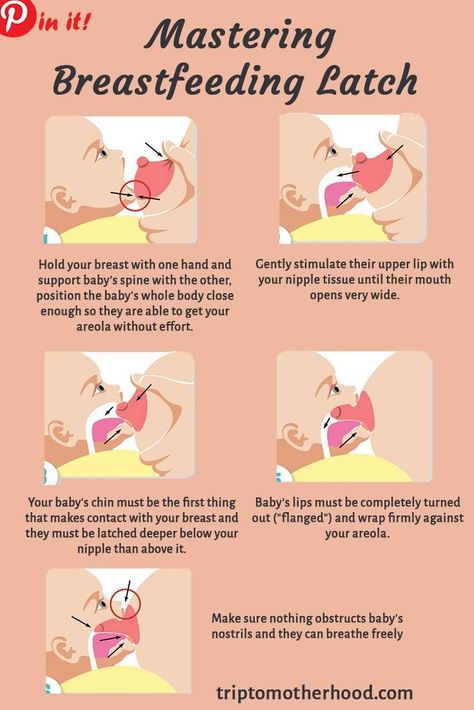 lCochrane Database of Systematic Reviews . 2012; 9:. art No.: CD000133.
lCochrane Database of Systematic Reviews . 2012; 9:. art No.: CD000133.
Lodge CJ, Allen KJ, Lowe AJ, Dharmage SC. Overview of evidence in prevention and etiology of food allergy: a review of systematic reviews. Int J. Environ Res. Public Health. 2013; 10:5781-5806.
Martin-Munoz MF, Pineda F, Parrado GG et al. Food allergy in breastfeeding babies. Hidden allergens in human milk. Eur Ann Allergy Clin Immunol. 2016;48(4):123-128.
Miles EA , Calder PC. Maternal diet and its influence on the development of allergic disease. Clin Exp Allergy. 2015; 45(1):63-74.
Netting MJ, Middleton PF, Makrides M. Does maternal diet during pregnancy and lactation effect outcomes in offspring? A systematic review of food-based approaches. Nutrition. 2014;30:1225-1241.
Pastor-Vargas C, Maroto AS, Diaz-Perales A et al. Sensitive detection of major food allergens in breast milk: first gateway for allergenic contact during breastfeeding. Allergy. 2015;70(8):1024-7.
Perkin MR et al. . N. Engl. J. Med. 2016;374:1733-1743.
Perkin MR, Logan K, Marrs T et al. Enquiring about tolerance (EAT) study: feasilbility of an early allergenic food introduction regimen. J Allergy Clin Immunol 2016;137:1477-86.e8.
Pitt TJ et al. Reduced risk of peanut sensitization following exposure through breast-feeding and early peanut introduction. J Allergy Clin Immunol 2017; article in press.
Recto MST, Genuino MLG, Castor MAR et al. Dietary primary prevention of allergic diseases in children; the Philippine guidelines. Asia Pac allergy. 2017; 7:102-114
Savage J, Sicherer S, Wood R. The natural history of food allergy. J Allergy Clin Immunol Pract. 2016;4(2): 196-203.
Sicherer SH, Sampson, HA, Eichenfield LF, Rotrosen D. The benefits of new guidelines to prevent peanut allergy. Pediatrics. 2017; 139(6):1-4.
Low food allergy prevalence despite delayed introduction of allergenic foods – Data from GUSTO cohort. J Allergy Clin Immunol Pract. 2017
2017
Togias A, Cooper SF, Acebal ML, et al. Addendum guidelines for the prevention of peanut allergy in the United States: Report of the National Institute of Allergy and infectious diseases-sponsored expert panel. Ann Allergy Asthma Immunol. 2017;118:166-173.
Vendenplas Y, AlFrayh AS, Almutairi B et al. Physician practice in food allergy prevention in the middle east and north Africa. BMC Pediatrics. 2017; 17:118-123.
Yepes-Nunez J et al. World allergy organization-McMaster University guidelines for allergic disease prevention (GLAD-P): vitamin D. WAOJ. 2016; 9:17-28
Claire K. Dalidowitz MS, MA, RD, CD-N is a registered dietitian who counsels food allergic children and their families at Connecticut Children’s Medical Center as well as serving as the dietitian for the Food Allergy Clinic at the hospital. She is an adjunct professor at the University of New Haven where she teaches graduate level maternal and child nutrition. Claire has recently completed the food allergy guidelines and teaching material for the Pediatric Nutrition Care Manual for the American Academy of Nutrition and Dietetics. Claire’s interest in lactation goes back many decades where her master’s research focused on the lactation outcome of mothers with insulin dependent type 1 diabetes. She was instrumental in starting the lactation committee at Connecticut Children’s Medical Center and developed many of their breastfeeding policies. Claire chaired the national practice group (of the Academy of Nutrition) on Women and Reproductive Nutrition, served as secretary on the International Board of Consultant Lactation Examiners(IBLCE) and currently is a member of the Health Advisory Committee of LLLI.
Claire’s interest in lactation goes back many decades where her master’s research focused on the lactation outcome of mothers with insulin dependent type 1 diabetes. She was instrumental in starting the lactation committee at Connecticut Children’s Medical Center and developed many of their breastfeeding policies. Claire chaired the national practice group (of the Academy of Nutrition) on Women and Reproductive Nutrition, served as secretary on the International Board of Consultant Lactation Examiners(IBLCE) and currently is a member of the Health Advisory Committee of LLLI.
Food allergies in young children!
Food allergies in young children!
Every mother remembers the calm days of pregnancy, where you could eat various foods in your diet without dieting. The main table during pregnancy should be as balanced as possible, fortified and the necessary ratio of proteins, fats, carbohydrates. There comes a happy moment in life, this is the birth of a baby. Acquaintance of mother and child, caring for the baby, providing the necessary conditions for caring for the baby, as well as creating the most favorable conditions. nine0003
Acquaintance of mother and child, caring for the baby, providing the necessary conditions for caring for the baby, as well as creating the most favorable conditions. nine0003
Very often, young parents face the first difficulties in the neonatal period (such as intestinal colic), in early childhood, such manifestations as rashes on the body, stool disorders (loose stools / constipation).
The most frequently asked questions of parents we will consider in this article:
- How does a food allergy manifest itself?
2. What is the duration of manifestation of external signs? nine0011 3. Is it worth giving up breastfeeding in favor of artificial (hydrolyzed and amino acid mixtures) or switching to goat's milk?
4. Blood streaks in the stool: is it worth going to the infectious disease hospital for inpatient care?
Food allergy is a food-induced reaction that causes a pathological reaction based on immune mechanisms (specific IgE-mediated reactions, cellular immune response (non-IgE-mediated) or a combination of both - a mixed type reaction).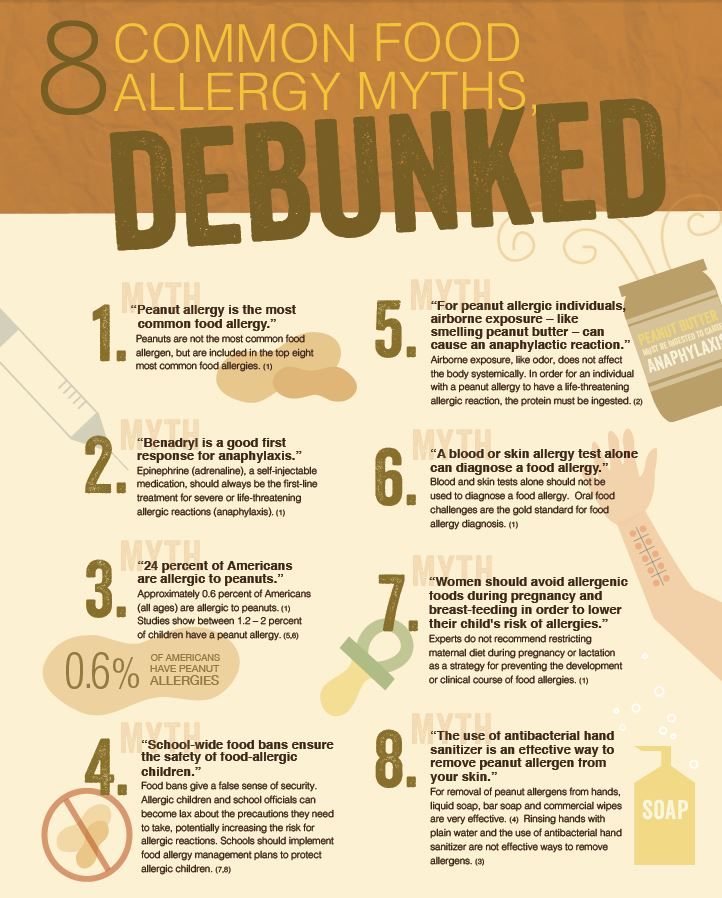 nine0007
nine0007
As a food allergen, there can be any substances, most often of a protein nature, that stimulate the production of IgE.
The most common foods that cause allergic reactions are cow's milk, chicken eggs, peanuts, tree nuts, fish, seafood, wheat, soy, and beef.
The most significant allergen is Cow's milk protein, which according to clinical guidelines is 2-3% among infants. With age, tolerance develops in 80% of sick children, by the age of 6 years, the incidence decreases by less than 1%. nine0011 Any protein component of milk can cause sensitization, but most often: beta-lactoglobulin, alpha-lactalbumin, bovine serum albumin and gamma globulin, alpha-casein and beta-casein.
Food allergy is a symptom complex of diseases and is not a nosological diagnosis.
Therefore, the clinical and etiological significance of food allergy is taken into account, it is included in the full clinical diagnosis after the designation of the nosological form.
Laboratory diagnostics:
- IgE (sIgE) - immunoglobulin E, specific immunoglobulin
The main function of IgE is to provide an individual immune response of the body to the introduction of an irritant (antigen) with a certain biological activity
nine0002- Food panel
In case of food allergy in young children, manifestations in the form of constant itching (characteristic of any age period), skin syndrome are more common. Atopic dermatitis in young children is infancy, during this period the exudative form of the disease predominates. The clinical picture is represented by erythematous spots, papules, vesicles on the forehead, cheeks, scalp, accompanied by intense itching, swelling, weeping. Pronounced red dermographism. Most often, rashes are localized on the extensor and flexor surfaces of the limbs. nine0007
nine0007
The duration of rashes depends on the timely start of treatment, as well as the complete exclusion of allergens (food). In children of the first year of life, the most common allergen is cow's milk protein.
Breastfed infants develop a clinically significant allergy to CMP due to the passage of dietary proteins into breast milk. I often see surprise in the eyes of young mothers and the rejection of the recommendation to exclude cow's milk protein. Counter questions: what exactly to use in the diet for mom? Dear mothers, a balanced diet for a nursing mother should be varied, complete and as natural as possible. The use of cereals (rice, buckwheat, corn, oatmeal, etc.), soups, meat products (turkey, chicken, pork), quail or chicken eggs, green fruits, etc. Therefore, the absence of whole cow's milk will not affect your menu variety in any way. nine0007
Should I give up breastfeeding?
Indeed, mothers often ask such questions. My answer is no! Breastfeeding is the key to the full development of the child. Only in the case when breastfeeding is impossible (complete hypogalactia of the mother, impossibility of breastfeeding due to congenital diseases (example: congenital malformation of cleft lip and palate), the presence of chronic infectious diseases in the mother are life-threatening for the child.
My answer is no! Breastfeeding is the key to the full development of the child. Only in the case when breastfeeding is impossible (complete hypogalactia of the mother, impossibility of breastfeeding due to congenital diseases (example: congenital malformation of cleft lip and palate), the presence of chronic infectious diseases in the mother are life-threatening for the child.
In the case where it is not possible to store the GW. The recommendations use hydrolyzed mixtures, or amino acids!
Hypoallergenic mixtures do not belong to clinical nutrition, they are prescribed only for children prone to developing allergies (taking into account history and heredity).
Soy Blend is also not a health food and can cause a cross reaction!
Switching to goat's milk is not the smart way. Since in this case, goat milk can act as a cross-allergen, causing cross-allergic reactions in patients with an allergy to CMP, and is an independent allergen, causing severe reactions in patients who are tolerant to cow's milk. And also the main allergens of milk practically do not lose their biological activity after boiling, pasteurization, ultra-high temperature treatment. nine0007
And also the main allergens of milk practically do not lose their biological activity after boiling, pasteurization, ultra-high temperature treatment. nine0007
Blood streaks in the stool: is it worth going to the infectious disease hospital for inpatient care?
Gastrointestinal manifestations are manifestations of the digestive organs. Food allergies are not only when there are rashes on the body. An allergen that passes through the gastrointestinal tract can cause dyspeptic manifestations (regurgitation, intestinal colic, abdominal pain, vomiting, blood streaks in the stool). Such children very often end up in an infectious diseases hospital. Receive symptomatic therapy, which brings only temporary improvement. If not diagnosed in time, unfortunately, this can lead to irreversible consequences. nine0007
If your baby does not have subfebrile / febrile body temperature, for a long time there is no improvement after a course of medication prescribed by your doctor, the presence of streaks of blood, mucus, discoloration in the stool, then most likely your child has a Gastrointestinal form of food allergy.
Gastrointestinal form of food allergy can occur both on breastfeeding and on artificial.
For mothers following a therapeutic diet with complete exclusion of CMP. Children with artificial feeding, the transition to clinical nutrition. The effect of timely treatment comes quickly. Following a diet in the future leads to a rapid recovery of the gastrointestinal tract. nine0007
Yours sincerely, pediatrician GAUZ KO KGDKB No. 1
Ryazanova Svetlana Sergeevna
Back
causes, treatment, diet - Dobrobut Clinic
Main
Medical Library Dobrobut
Publication date: 2020-03-09
How does allergy manifest itself in infants
Allergy is a pathological reaction of the body to various foreign substances. Clinically, such reactions are expressed in the form of allergic diseases: atopic dermatitis, food allergies, urticaria, allergic rhinitis, Quincke's edema, bronchial asthma.
Allergic diseases (AD) have long turned into a "disease of civilization". The increase in the number of allergy sufferers is most noticeable among children of the first year of life. One of the causes of allergies in an infant is the early rejection of the mother's breast or the lack of breastfeeding. In this case, the baby does not receive the necessary protective elements with mother's milk. You will learn about other causes of allergic diseases, about how to treat allergies in an infant, from our article. nine0007
Causes of allergies in infants
The direct cause of allergies is the child's contact with an allergen - a foreign substrate.
One of the factors contributing to the development of allergic diseases is hereditary predisposition. If one of the parents has an allergy, then the probability of its occurrence in a child is 60-70%, if both parents are ill, then the probability of developing AZ increases to 90%. The early development of allergic diseases in children is also facilitated by the unreasonable use of antibacterial drugs, especially in the first months of life. Bad habits of the mother (alcohol, drugs, smoking) increase the risk of developing allergic diseases in the child. The question of whether the diet of a pregnant woman affects the development of AD in a child is still under discussion. nine0007
Bad habits of the mother (alcohol, drugs, smoking) increase the risk of developing allergic diseases in the child. The question of whether the diet of a pregnant woman affects the development of AD in a child is still under discussion. nine0007
How do babies develop allergies? Its main symptoms are:
- peeling of the skin,
- various rashes,
- diaper rash,
- profuse regurgitation,
- nasal congestion,
- shortness of breath,
- liquid stool.
Angioedema may also develop (very rare).
Breastfeeding allergy
Allergy to breast milk is usually associated with the diet of a breastfeeding mother. In 85% of cases, food allergens are: cow's milk, fish and seafood, eggs, wheat, soybeans, hazelnuts, peanuts, honey. At the first sign of an allergy in a baby, a nursing mother should write down the names of the foods she consumed daily to determine what the child has an allergic reaction to.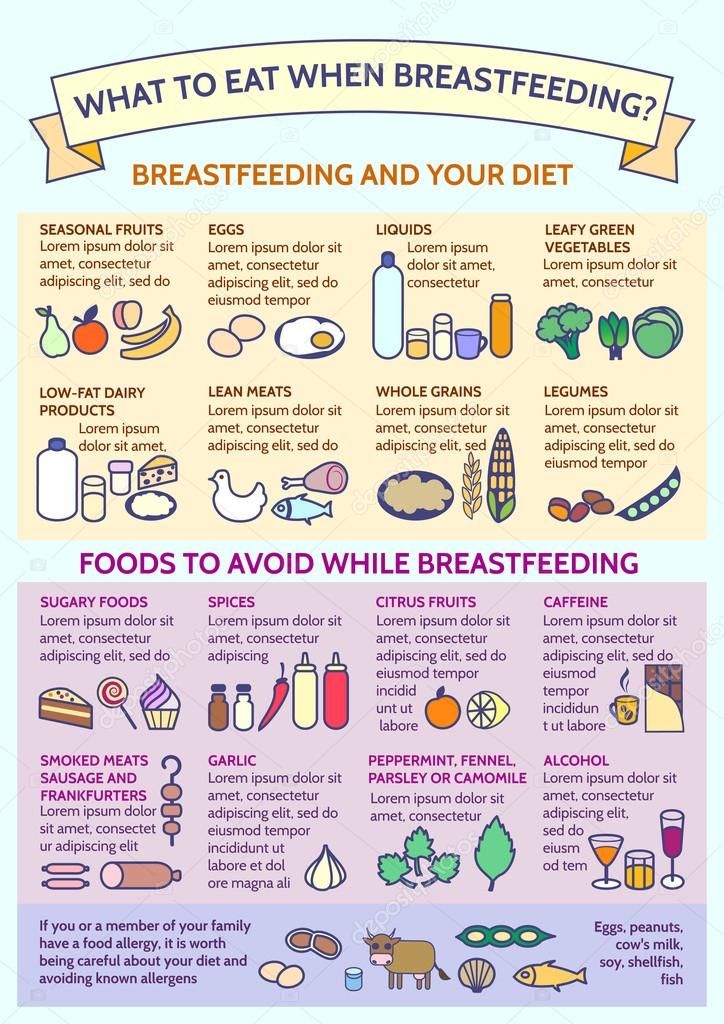 The list of products must be shown to the allergist.
The list of products must be shown to the allergist.
CMP (cow's milk protein) is usually the first complementary food protein that infants come into contact with. It can also cause allergies. nine0007
There are three groups of reactions to CMP:
- Skin rash. Swelling of the face.
- Gastrointestinal symptoms (diarrhea, vomiting).
Symptoms of atopic dermatitis may appear 1-5 days after the food test.
A well-adjusted diet for breastfeeding mothers has been shown to reduce the risk of developing allergies in babies.
Diet for allergies
Since allergies during breastfeeding can be associated with errors in the nutrition of a nursing mother, it is necessary to completely eliminate foods that cause an allergic reaction in a baby from her diet. nine0007
The most common cause of allergies is:
- chicken meat,
- eggs,
- milk and dairy products,
- fish,
- seafood,
- peanuts,
- citrus fruits,
- honey,
- nuts,
- red vegetables, fruits and berries.
Allergy diet is one of the main components of AD prevention and treatment. Drug therapy for allergic diseases in an infant should be prescribed by a doctor. Read about skin care for a child with atopic dermatitis on our website Dobrobut.com. nine0007
To avoid allergic reactions in your baby, you should follow some rules:
- introduce complementary foods only after consulting a pediatrician;
- Mom should try any product literally drop by drop and after feeding the child, carefully monitor the reaction of his body;
- maintain optimal temperature and humidity in the children's room;
- choose hypoallergenic baby care products; nine0028
- wash children's things with special means.
By following these recommendations, you can reduce the risk of allergic diseases in your baby.
Do you want to get an online explanation from the doctor of the Dobrobut MS?
Download our Google Play and App Store app
Our doctors
See all doctors 697
Our certificates
Certificate no. QIZ 804 468 C1
QIZ 804 468 C1
Certificate no. QIZ 804 469 C1
Certificate No. QIZ 804 470 C1
Certificate no. QIZ 804 471 C1
View all certificates
Request a call back
Enter your phone number
Other articles
Papillary thyroid carcinoma and other carcinomas. Diagnosis, therapy
Morphological aspects of carcinomas. Invasive ductal carcinoma of the breast. Methods for diagnosing carcinomas. Surgery for lung carcinoma with metastases and other methods of treatment.
Bladder cystostomy in men and women. Definition, indications
What is bladder cystostomy. Bladder puncture with a trocar. Technique for cystostomy of the bladder. Possible complications. Patient care after surgery
Treatment of laryngitis: drug therapy, voice rest, diet
Laryngitis in a child: types, causes and symptoms of the disease.