Newborn baby not feeding milk
Why is my baby refusing the breast? 8 tips that help | Baby & toddler, Feeding articles & support
Whether your baby refuses the breast as a newborn or when they’re older, it can be very stressful. Here’s why it might happen and what to try…
Why won’t my newborn baby breastfeed?
Sometimes, newborn babies struggle to latch on to breastfeed after they’re born. It can be worrying for new parents when this happens – you might think something’s wrong.
There may be a simple explanation. This information could help you find your own solution, or decide if you need further support.
Some of the more common reasons for newborn babies finding it difficult to latch onto the breast could be:
- a difficult labour or birth – your baby might feel sore or have a headache if the mother has had interventions in labour or if they were born very quickly
- medication used during labour – anaesthesia, epidural or pethidine can make your baby sleepy or groggy
- your baby being separated from you after birth – even for a few minutes
- discomfort due to a birth injury or bruising
- swallowing mucus at birth can make your baby feel congested, nauseous or uncomfortable
- an early unpleasant experience of attempting to breastfeed, such as being forced onto the breast
- the baby might have tongue-tie
(LLLGB, 2016)
Why won’t my baby breastfeed anymore?
Sometimes, older babies seem to refuse to breastfeed when they’d been breastfeeding just fine until then. This is known as a 'nursing strike.' They might refuse to breastfeed for 2-4 days, but it can be up to 10 days (Mohrbacher, 2013).
Reasons that your older baby might refuse to feed at the breast could include:
- something has changed that makes it difficult for baby to latch
- a strong or fast flow of milk, which your baby is struggling to take
- a painful mouth, due to an infection like thrush or because they’re teething
- being more aware of their surroundings and being easily distracted, for example by noise
- a change in the taste of your milk, such as that due to your menstrual cycle
- the introduction of more solid food
- a small number of babies might struggle because of severe or persistent reflux, known as gastro-oesophageal reflux disease (GORD), so they may link feeding with pain.
(Mohrbacher, 2013; Gonzalez, 2014; BellyBelly, 2016; NICE, 2017; Public Health England, ND)
What can I do when my baby refuses to breastfeed?
8 top tips to help your baby who’s refusing to breastfeed:
1. Try to identify what’s going on for your baby. Knowing the cause can help not only with a plan but it can be reassuring to understand what is happening and know there’s a solution. You could think about the following:
Try to identify what’s going on for your baby. Knowing the cause can help not only with a plan but it can be reassuring to understand what is happening and know there’s a solution. You could think about the following:
- Do they have a cold or an infection?
- Was there something that might have caused them to not want to feed?
- Talk to one of our Breastfeeding Counsellors or contact our Infant Feeding Line on 0300 330 0700 (option 1) for further support. It can be a great way to get some help to find out what’s happening.
- You could also contact a health professional to investigate any medical reasons why your baby might not be feeding.
2. Try to stay calm and not force a feed. Instead, allow your baby to take the lead.
3. Especially for young babies, many mums find skin-to-skin contact in a laid-back position helps to take the pressure out of the situation. It allows your baby to use their own natural instincts to feed (Burbridge, 2017).
4. Don’t worry if your baby bobs their head or moves it from side to side, they’re not rejecting the breast as it might appear. These are your baby’s natural ways of finding your breast (Coulson, 2012).
5. Try a different feeding position to see if you can get your baby more comfortable. Some babies find a laid-back breastfeeding (also called biological nurturing) position helpful if they are struggling to get a deep latch or if you have a strong let-down of milk (Coulson, 2012).
6. Sometimes, feeding your baby while they’re sleepy or even asleep can be helpful. Many mums say that these ‘dream feeds’ can be very effective for a baby who is uninterested when awake (Pitman and Bennett, 2008).
7. You could try feeding your baby while rocking them or walking around, singing or playing with them or playing white noise or background music to them (Australian Breastfeeding Association, 2017).
8. You might want to try feeding in a quiet room, away from distractions, as some babies are so keen to be involved that they limit their feeds (Gonzalez, 2014).
You might want to try feeding in a quiet room, away from distractions, as some babies are so keen to be involved that they limit their feeds (Gonzalez, 2014).
What can I do if I’ve tried everything but my baby still won’t breastfeed?
One of the key things to consider is maintaining your milk supply. You might need to consider expressing, either by hand or with a pump. You can find more information about expressing and storing your milk here.
Another consideration is making sure your baby is getting enough milk. How might you know how much milk your baby is getting, you might ask. The answer lies in their dirty and wet nappies. You can expect six wet nappies in 24 hours if your baby is over a week old (UNICEF, 2016). If you’re unsure, it’s best to ask for support from your health visitor, GP or NCT breastfeeding counsellor.
In the short term, you might need to look at alternative ways to feed your baby if you think they’re not getting enough milk. A newborn baby needs to be fed regularly and parents can use syringe or cup feeding as an alternative to a bottle in the early days (Flint et al, 2016; NHS, 2016).
If you decide to use a bottle, it might be helpful to feed with plenty of skin-to-skin contact (UNICEF, 2018). Gently offering the bottle to your baby by tickling their top lip, waiting for the wide-open gape might also help mimic a breastfeed (UNICEF, 2019). That can support the transition back to the breast.
Taking frequent breaks during the bottle feed, and perhaps swapping sides, can be helpful (UNICEF 2018). Continuing to have skin-to-skin time with your baby and allowing them access to the breast will help this. It’ll also be a bonding and calming experience for you both.
How can I deal with the stress of my baby refusing to breastfeed?
When a newborn refuses the breast, or an older baby goes through a nursing strike, it can be very upsetting for both you and your baby. You’re definitely not alone in struggling with the emotions of breastfeeding problems. So here are some tips that might help:
- Try to take time to enjoy plenty of extra cuddles and quiet time together.

- Many mums find a ‘babymoon’ helpful for allowing their baby access to the breast in a non-pressurised way. A babymoon means spending some hours together in a relaxed setting, such as lying down snuggling in bed. This can allow you to enjoy your baby without worrying about feeding.
- For older babies, some mums find that having a bath with their baby or bringing their baby into bed with them helps their baby to latch.
- Try to find some support from other mums and trained breastfeeding supporters. Chatting with other people about this can help to unburden the stresses and worries you might be feeling. Breast refusal is not uncommon and you might find that chatting to someone who understands is invaluable while you’re struggling.
- For many mums, time and patience can help the situation. Your baby’s instincts and behaviour can change and develop, especially in the early days.
- If you’re struggling, do contact the NCT Infant Feeding Line and speak to a breastfeeding counsellor.
 They’ll listen, offer you information and will support you to find your own path.
They’ll listen, offer you information and will support you to find your own path.
This page was last reviewed in August 2019.
Further information
NCT supports all parents, however they feed their baby. If you have questions, concerns or need support, you can speak to a breastfeeding counsellor by calling our helpline on 0300 330 0700, whether you are exclusively breastfeeding or using formula milk. Breastfeeding counsellors have had extensive training, will listen without judging or criticising and will offer relevant information and suggestions. You can also find more useful articles here.
National Breastfeeding Line (government funded): 0300 100 021.
NHS information on mastitis.
Best Beginnings - Bump to Breastfeeding DVD Chapter 7 'Overcoming Challenges'.
Healthtalkonline.org: Managing Breastfeeding – dealing with difficult times.
References
Australian for Breastfeeding Association (2017) Breast refusal. https://www.breastfeeding.asn.au/bf-info/breast-refusal [Accessed 22nd February 2019]
https://www.breastfeeding.asn.au/bf-info/breast-refusal [Accessed 22nd February 2019]
BellyBelly. (2016) Breast refusal – 13 tips for a baby that refuses the breast.
https://www.bellybelly.com.au/breastfeeding/breast-refusal/ [Accessed 22nd February 2019]
Burbridge A. (2017) Nursing strikes. La Leche League GB. Available at: https://www.laleche.org.uk/nursing-strikes/ [Accessed 1st August 2019]
Coulson S. (2012) Biological nurturing: the laid-back breastfeeding revolution. Midwifery Today, 101 Available at: https://midwiferytoday.com/mt-articles/biological-nurturing/ [Accessed 1st August 2019]
Flint A, New K, Davies MW. (2016) Cup feeding versus other forms of supplemental enteral feeding for newborn infants unable to fully breastfeed. Cochrane Database Syst Rev. (8):CD005092. Available from: https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD005092.pub3… [Accessed 1st August 2019]
Gonzalez C. (2014) Breastfeeding Made Easy. London: Pinter &Martin
LLLGB. (2016) My baby won’t breastfeed. Available at https://www.laleche.org.uk/my-baby-wont-breastfeed/ [Accessed 1st August 2019]
(2016) My baby won’t breastfeed. Available at https://www.laleche.org.uk/my-baby-wont-breastfeed/ [Accessed 1st August 2019]
Mohrbacher N. (2013) Is your formerly nursing baby refusing to breastfeed? Breastfeeding Reporter Blog. Available at http://www.nancymohrbacher.com/articles/2013/1/26/is-your-formerly-nursing-baby-refusing-to-breastfeed.html?rq=refusing [Accessed 1st August 2019]
NICE. (2017) Breastfeeding problems. National Institute for health and Care Excellence, Clinical Knowledge Summaries. Available at: https://cks.nice.org.uk/breastfeeding-problems#!scenario [Accessed 1st August 2019]
Pitman T, Bennett H. (2008) 0-1 year: nursing strikes; breastfeeding while baby’s falling asleep may help end a nursing strike. Today’s Parent. 7:137.
Public Health England. (ND) Breastfeeding challenges. NHS, Start 4 life. Available at: https://www.nhs.uk/start4life/baby/breastfeeding/breastfeeding-challenges/reflux/ [Accessed 1st August 2019]
UNICEF. (2016) Breastfeeding checklist for mothers – How can I tell that breastfeeding is going well? UNICEF UK Baby Friendly Initiative. Available at https://www.unicef.org.uk/babyfriendly/wp-content/uploads/sites/2/2016/10/mothers_breastfeeding_checklist.pdf [Accessed 1st August 2019]
Available at https://www.unicef.org.uk/babyfriendly/wp-content/uploads/sites/2/2016/10/mothers_breastfeeding_checklist.pdf [Accessed 1st August 2019]
UNICEF. (2018) Skin-to-skin contact. Available from: https://www.unicef.org.uk/babyfriendly/baby-friendly-resources/guidance-for-health-professionals/implementing-the-baby-friendly-standards/further-guidance-on-implementing-the-standards/skin-to-skin-contact/ [Accessed 1st August 2019]
UNICEF. (2019) Responsive bottle feeding. Available from: https://www.unicef.org.uk/babyfriendly/wp-content/uploads/sites/2/2019/04/Infant-formula-and-responsive-bottle-feeding.pdf [Accessed 1st August 2019]
Why Baby May Suddenly Refuse the Breast
It's very rare for babies to wean themselves off the breast. So, if your baby suddenly seems reluctant to breastfeed, it might be what's referred to as a nursing strike. It signals that something is different-though not necessarily wrong-and has caught your baby's attention. Don't take it personally! Comfort your baby, and keep offering your breast. Before long, your baby will start nursing again. If they don't, reach out to your WIC breastfeeding staff for tips and support.
Before long, your baby will start nursing again. If they don't, reach out to your WIC breastfeeding staff for tips and support.
What might be the cause
Many moms are confused when their babies go on strike. Some common reason why babies may go on strike are:
- Your baby is not feeling well. It could be from a cold, ear infection, stuffy nose, upset stomach, injury, teething, thrush, cold sore, or other reasons.
- Your baby is upset. Maybe there is a big change in nursing routine, you were apart for a long time, or your baby's environment is uncomfortable.
- Your baby is distracted. Perhaps there are fun things happening nearby.
- Your baby is getting less milk from you. Supplemental bottles may cause milk production to drop, but there are other reasons for low milk supply as well.
- You smell different. This can be from a new soap, deodorant, or perfume.

- Your baby bit you while nursing. Your baby may pause breastfeeding if a bite caused you to react strongly, like a loud "ouch!"
What you can do
Don't worry. With your gentle persistence, the refusal will end. If your baby is less than 1 year old and has been breastfeeding well up to this point, chances are they're not ready to give up breastfeeding. Here's what to do:
- Keep putting your baby to your breast. Try this when your baby shows hunger signs or seems sleepy, and just after your baby wakes up. If your baby is frustrated, stop and try again later.
- Give your baby extra loving. Give your baby extra cuddles, touches, and comfort. Hold your baby skin to skin, and keep your baby close.
- Pump or hand express your milk. Do so at the times your baby used to nurse. Feed your milk to your baby. That way, you will keep making enough milk and will be less likely to get plugged ducts or engorged breasts.

- Try different nursing positions. A different breastfeeding position can make your baby more comfortable.
- Nurse in a calm, quiet spot. Babies may strike when they are older, as they begin to notice the world. They may snack instead of nursing for long sessions. Try breastfeeding away from TV sounds and bright lights.
- Keep your routine. Keep your baby's routine as regular as you can.
- Visit your baby's doctor. Make sure there's not a medical cause for your baby not wanting to breastfeed, and ask for advice.
Above all, keep trying to breastfeed your baby. Your baby will most likely be breastfeeding again before you know it. Need help? Ask your WIC breastfeeding staff.
Signs of lack of milk | Improving lactation
Many mothers are concerned about insufficient milk production, but it is not always easy to find out if milk is really low. Read our article to understand if this is true and what can be done about it.
Share this information
“Do I have enough milk?” - a question that is often asked by young mothers. If your baby is healthy and growing well, there is no reason to worry. However, if you are still worried about milk production, it is best to consult a specialist as soon as possible. If everything is in order, he will be able to calm you down. In addition, you will not needlessly feed the baby formula, because of which milk production can really decrease. nine0003
Causes of insufficient milk supply
Some mothers do not produce enough breast milk for medical reasons, which include: approximately three days after birth). 1
 3
3 If you have any of the conditions listed, contact your lactation consultant or healthcare provider.
How milk is produced
With the advent of milk, the breast begins to work on the principle of supply and demand. Each time after it is emptied, whether it is feeding the baby or pumping, even more milk will be produced.
This is why milk production may be reduced if you give formula to your baby - your body will not get the signal to produce more milk because it will remain.
The way your baby eats also affects milk production. The more often and better he sucks the breast, the bigger it will be. If your baby eats only a small portion at one feeding, it is necessary to express milk regularly to maintain the level of its production. Read more about this below. nine0003
Signs that the baby is not getting enough milk
Although low milk production is rare, the baby may have difficulty feeding in the first few weeks, but for other reasons. You may not be feeding him often enough or for enough time, especially if you're trying to stick to a specific schedule. The baby may not latch on properly, or it may have features that make it difficult to take in milk. nine0003
You may not be feeding him often enough or for enough time, especially if you're trying to stick to a specific schedule. The baby may not latch on properly, or it may have features that make it difficult to take in milk. nine0003
The following signs indicate that the baby is not getting enough milk:
- Poor weight gain. In the first few days of life, newborns normally lose 5 to 7%, and sometimes even up to 10%, of their birth weight. However, after that, they should gain at least 20–30 g per day and regain their birth weight by 10–14 days. 5,6,7 If your baby has lost 10% or more of their weight in the early days, or has not started gaining weight by 5-6 days, you should contact your doctor immediately. nine0018
- Not enough wet and soiled diapers. A good indicator of whether a baby is getting enough milk is the number of diapers used per day. Check out our article detailing the norm for wet and soiled diapers in Breastfeeding Your Newborn: What to Expect in the First Week.
 Seek medical advice if something bothers you or you notice that the number of soiled diapers has begun to decrease. nine0018
Seek medical advice if something bothers you or you notice that the number of soiled diapers has begun to decrease. nine0018 - Dehydration. If your baby has dark urine, dry mouth or jaundice (yellowing of the skin or eyes), or baby is lethargic, has lost appetite, and may be dehydrated. 6 Dehydration can be caused by fever, diarrhoea, vomiting or overheating. If you notice any of these symptoms, seek medical attention as soon as possible.
Misconceptions about lack of milk
Newborns usually eat very frequently, about 10-12 times a day or every two hours. This does not mean that they do not have enough milk. Keep in mind that breastfeeding is also about comfort, so it's hard to tell how much milk a baby eats at each feed as the amount can vary.
You have enough milk even if:
- the child wants to eat often;
- the child does not want to be laid down;
- the child wakes up at night; nine0018
- feeding is fast;
- feeding takes a long time;
- after feeding, the child takes another bottle;
- Your breasts are softer than in the first weeks;
- milk does not leak or has stopped leaking;
- You cannot express much milk;
- You have small breasts.

What to do about insufficient milk production
If you suspect that your baby is not getting enough milk, contact a lactation consultant or your doctor. He will determine if you have enough milk and check how the baby is latch-on and if he is getting enough milk. He may also suggest changing the feeding position or the way the baby is attached to the breast to make it easier. nine0003
Also try holding your baby close to you more often to increase skin-to-skin contact before and during feedings. This stimulates the production of the hormone oxytocin, which promotes milk flow. Use relaxation techniques, such as listening to your favorite soothing music, to reduce anxiety that can negatively impact milk production. 8
With proper support, most under-lactating mothers can breastfeed their babies at least partially, and some manage to normalize production. nine0003
If your baby is unable to get enough milk directly from the breast (perhaps because he was born prematurely or has special needs), you need to express milk to support his production. Your doctor may prescribe you special drugs that stimulate lactation.
Your doctor may prescribe you special drugs that stimulate lactation.
If you are unable to express enough milk, you will need to supplement your baby with donor milk or formula. This should also take place under the supervision of a physician. The Supplemental Nursing System (SNS)* is a great way to help your baby get all the milk he needs at the breast. nine0003
How to increase your milk production with a breast pump
If you need to increase your milk production in the first five days after giving birth, you can use a dual electronic breast pump with lactation start technology, such as the Medela Symphony**. Such a breast pump imitates the sucking of the breast by a child and helps to increase milk production in the future. 9
After your milk comes in, double pumping allows you to get more milk in less time. nine0016 10 This method helps to better empty the breast, which also improves lactation.
Although every mother is different, it is often recommended to express milk immediately or one hour after a feed.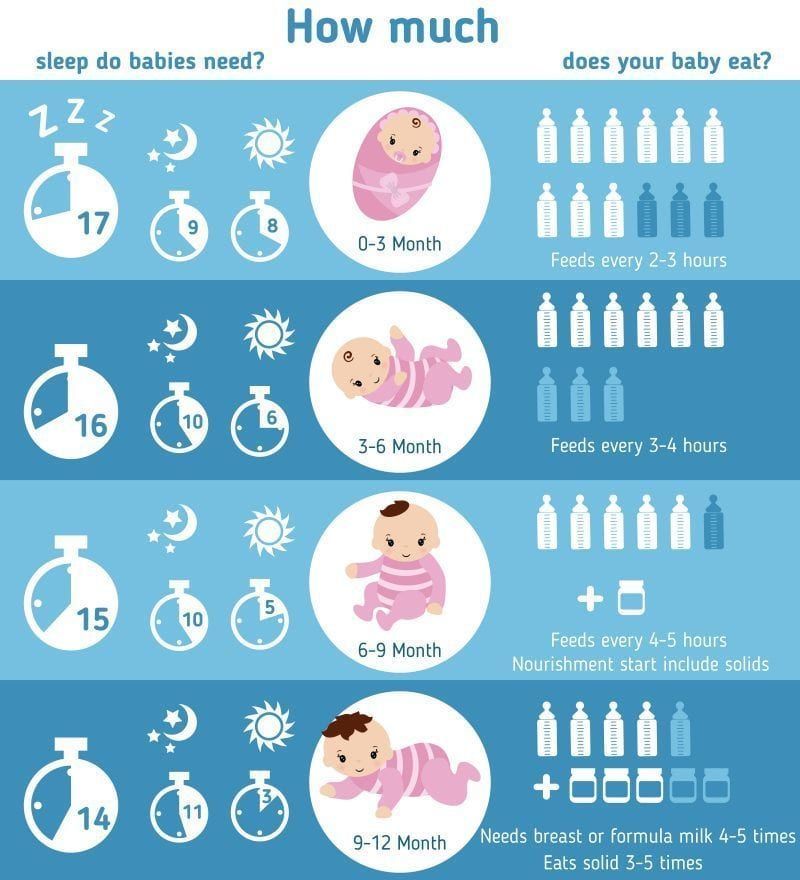 This may seem strange, since it is usually easier to express milk from a full breast. However, the pumping session should be seen as an "investment in tomorrow."
This may seem strange, since it is usually easier to express milk from a full breast. However, the pumping session should be seen as an "investment in tomorrow."
You will probably only be able to express a little milk at first, but don't be discouraged - if you express regularly, your milk supply will increase. Try to empty your breasts - by putting your baby to your breast or expressing milk - 8 to 12 times a day, including one nightly session, when your levels of prolactin (the hormone responsible for producing milk) are highest. The more often you empty your chest, the better. After two to three days of regular pumping, you will notice a significant increase in milk production. For tips on how to get more milk with every pump, see Tips for Using a Breast Pump. nine0003
Pumping with massage to get more milk
If your baby is not lating at all or you are not yet able to express enough milk for him, a technique called “massage pumping” may be helpful. It helps mothers increase the amount of milk they get in one pumping session. 11.12 The whole process takes about 25-30 minutes. Remember that the better you empty your breast, the faster milk is produced in it.
11.12 The whole process takes about 25-30 minutes. Remember that the better you empty your breast, the faster milk is produced in it.
A few simple steps are required:
- Massage your breasts.
- Perform a double pump while wearing a special bustier top that allows you to keep your hands free.
- While expressing, squeeze the chest with all fingers for a few seconds. Release and repeat. Squeeze both breasts until the milk flows in a thin stream.
- Massage the chest again.
- Express milk manually or with a single breast pump, squeezing each breast in turn to empty them as completely as possible. nine0018
When your baby starts to gain weight and milk production increases, you can switch to exclusive breastfeeding.
Literature
1 Pang WW, Hartmann PE. Initiation of human lactation: secretory differentiation and secretory activation. J Mammary Gland Biol Neoplasia. 2007;12(4):211-221. - Pang, W.W., Hartmann, P.I., "Lactation initiation in the lactating mother: secretory differentiation and secretory activation." J Mammary Gland Biol Neoplasia. 2007;12(4):211-221. nine E et al . Breastfeeding in polycystic ovary syndrome. Acta Obstet Gynecol Scand. 2008;87(5):531-535. - Wanky, I. et al., "Breastfeeding in the setting of polycystic ovaries." Akta Obstet Ginecol Scand. 2008;87(5):531-535.
- Pang, W.W., Hartmann, P.I., "Lactation initiation in the lactating mother: secretory differentiation and secretory activation." J Mammary Gland Biol Neoplasia. 2007;12(4):211-221. nine E et al . Breastfeeding in polycystic ovary syndrome. Acta Obstet Gynecol Scand. 2008;87(5):531-535. - Wanky, I. et al., "Breastfeeding in the setting of polycystic ovaries." Akta Obstet Ginecol Scand. 2008;87(5):531-535.
3 Neifert MR et al. Lactation failure due to insufficient glandular development of the breast. Pediatrics. nine0148 1985;76(5):823-828. - Neifert M.R. et al., "Inability to Lactate Due to Deficiency of Glandular Breast Tissue". Pediatrix (Pediatrics). 1985;76(5):823-828.
4 Neifert M et al. The influence of breast surgery, breast appearance, and pregnancy-induced breast changes on lactation sufficiency as measured by infant weight gain. Birth. 1990;17(1):31-38. - Neifert M. et al., "Influence of breast surgery, breast appearance, and pregnancy-induced breast changes on milk supply as measured by weighing the baby." nine0148 Bers. 1990;17(1):31-38.
Birth. 1990;17(1):31-38. - Neifert M. et al., "Influence of breast surgery, breast appearance, and pregnancy-induced breast changes on milk supply as measured by weighing the baby." nine0148 Bers. 1990;17(1):31-38.
5 C Tawia S, McGuire L. Early weight loss and weight gain in healthy, full-term, exclusively-breastfed infants. Breastfeed Rev . 2014;22(1):31-42. - S. Tavia S., McGuire L., "Natural Weight Loss and Gain in Healthy, Exclusively Breastfed Full-Term Infants." Brestfeed Rev (Breastfeeding Review). 2014;22(1):31-42.
6 Lawrence RA, Lawrence RM. Breastfeeding: A guide for the medical profession. 7th ed. Maryland Heights MO, USA: Elsevier Mosby; 2010. 1128 p . - Lawrence R.A., Lawrence R.M., "Breastfeeding: A guide for healthcare professionals." Seventh edition. Publisher Maryland Heights , Missouri, USA: Elsevier Mosby; 2010. P. 1128.
P. 1128.
7 World Health Organization. [Internet]. Neonatal Care . 2012;12(2):112-119 - Keith D.R. et al., "Effects of listening to music on the amount, fat content, composition and calorie content of breast milk in mothers of premature and seriously ill children." Adv Neonatal Care. 2012;12(2):112-119
9 Meier PP et al. Breast pump suction patterns that mimic the human infant during breastfeeding: greater milk output in less time spent pumping for breast pump-dependent mothers with premature infants. J. Perinatol. nine0148 2012;32(2):103-10. - Meyer P.P. et al., "Pumping patterns that mimic breastfeeding behavior: more milk and less time for constantly pumping mothers of preterm infants." J Perinatol (Journal of Perinatology). 2012;32(2):103-10.
10 Prime DK et al. Simultaneous breast expression in breastfeeding women is more efficacious than sequential breast expression. Breastfeed Med . 2012;7(6):442-447. - Prime D.K. and co-authors. "During the period of breastfeeding, simultaneous pumping of both breasts is more productive than sequential pumping." Brestfeed Med (Breastfeeding Medicine). 2012;7(6):442-447.
Breastfeed Med . 2012;7(6):442-447. - Prime D.K. and co-authors. "During the period of breastfeeding, simultaneous pumping of both breasts is more productive than sequential pumping." Brestfeed Med (Breastfeeding Medicine). 2012;7(6):442-447.
11 Stanford University School of Medicine [Internet]. Stanford, CA, USA: Maximizing Milk Production with Hands-On Pumping; 2017. [ Accessed 04/30/2018]. - Stanford University School of Medicine [Internet]. Stanford, CA, USA: "Increased milk production from hand expression"; 2017. [Page accessed 04/30/2018].
12 Morton J et al. Combining hand techniques with electric pumping increases milk production in mothers of preterm infants. J. Perinatol. 2009;29(11):757-764. - Morton J. et al., "Manual pumping combined with an electric breast pump increases breast milk production in mothers of preterm infants. " J Perinatol (Journal of Perinatology). 2009;29(11):757.
" J Perinatol (Journal of Perinatology). 2009;29(11):757.
Read instructions before use. Consult a specialist about possible contraindications. nine0011
*RC No. ФСЗ 2010/07352 dated 07/19/10
**RC No. ФСЗ 2010/06525 dated 03/17/2021
Breastfeeding after 1 month: what to expect
Do you know when breast milk production stabilizes ? And how does the frequency and duration of feedings change as the baby grows? You will find answers to these questions in our recommendations for breastfeeding after the first month.
Share this information nine0003
Congratulations: You made it through the first month of breastfeeding. Your breast milk has reached full maturity 1 , its production is stabilizing, and there is little or no leakage from the breast. Don't worry, it's not getting less milk, it's just that your breasts are better able to produce and store it now. 2 At the age of six weeks, your baby will begin to please you with his charming toothless smiles, and by two months you will already have 500-600 feedings behind you. With a favorable development of events, problems with latch on by this point will already be resolved, and you can simply enjoy the convenience and benefits of breastfeeding. nine0003
With a favorable development of events, problems with latch on by this point will already be resolved, and you can simply enjoy the convenience and benefits of breastfeeding. nine0003
When does breastfeeding decrease?
The "normal" feeding frequency for babies aged one to six months varies considerably, with some needing four times a day, others asking to be breastfed 13 times a day. 3
“From the age of one month, the amount of milk a baby consumes per feed increases so that he can go without food for longer,” explains Cathy Garbin, a recognized international expert on breastfeeding, “A baby’s stomach grows, so he eat more at one time. In addition, mature milk allows him to stay full longer.” nine0003
Feeding can last from 12 minutes to one hour -
the habits of babies vary so much! 3 But if the child is gaining weight and falls within this range, there is no cause for concern.
What is most surprising, no matter how often the baby eats, he consumes approximately the same amount of milk per day - both at one month and at six, when it is time to start complementary foods with solid food. 4
4
“However, sometimes the baby eats more and sometimes less, especially when he is unwell. It’s better to just listen to his needs,” Katie explains. nine0003
Is breastmilk sufficient for the first six months?
Yes. Breast milk contains everything a baby needs for the first 90,351 six months of life—exclusively breastfed babies don't even need to drink more water! 5 Until about six months of age, a child's digestive system is simply not adapted to the digestion of solid food, and he will be able to drink cow's milk only after a year.
In addition, breastfeeding during this period prepares the child for further development. It strengthens the muscles of the mouth, develops the jaw and helps straighten the teeth 6.7 . All this will come in handy when the baby begins to eat and talk. And because what you eat and drink affects how your breast milk tastes, your baby discovers new tastes even before he starts eating solid foods. 8
8
In addition, when your baby is sick, your body produces breast milk that is
loaded with antibodies that help fight infection. 9 In other words, milk continues to protect the baby for many months as he grows and becomes more active. nine0003
Breastfeeding is also very comfortable once you get used to it. Claudia, a mother of two from the UK, notes: “No need to sterilize a mountain of bottles, prepare formula, carry it all with you, warm it up - in general, breastfeeding turned out to be very convenient, especially when my babies grew up and we began to leave the house more often. ".
At what age does a breastfed baby start sleeping through the night?
Waking up at night is normal for babies. Most babies between the ages of one and six months consume a fifth of their daily milk requirement at night, so nighttime feedings should not be neglected if you want your baby to get the required amount of calories. nine0016 3
"It really depends on what you mean by 'sleep through the night,'" says Cathy. "And it's better than waking up every two hours anyway! I have met infants who, starting at six weeks old, fell asleep at 19:00 and woke up at 7:00, but most continue to wake up frequently at night after this age. All children are different."
"And it's better than waking up every two hours anyway! I have met infants who, starting at six weeks old, fell asleep at 19:00 and woke up at 7:00, but most continue to wake up frequently at night after this age. All children are different."
In Wales, a study of more than 700 infants showed that almost 80% of children aged 6 to 12 months wake up at least once a night, and 25% of them wake up three times or more. And it did not depend on what type of feeding the child is on - breastfeeding or artificial. nine0016 10
And if nighttime awakenings are unavoidable anyway, breastfeeding is at least comfortable! Maina, a mother of two from Australia, agrees: “You can even take a nap while feeding in the middle of the night - both the body and the baby do their job on autopilot. No need to plan, measure, sterilize anything - ready-made food at the right temperature is right in your chest. I think it's ideal."
My child wakes up more often. Perhaps he is hungry?
Around four months of age, a baby's sleep pattern changes as he, like an adult, develops deep and light sleep phases. Because of this, he may wake up more often at night. “At four months, sleep is more of a problem than feeding,” Cathy admits. “It can be exhausting, but try to adapt and be patient.” nine0003
Because of this, he may wake up more often at night. “At four months, sleep is more of a problem than feeding,” Cathy admits. “It can be exhausting, but try to adapt and be patient.” nine0003
Some call this " a four-month sleep regression ", but "progress" is more appropriate here. From the outside it may look like a step back, but in fact the child is approaching an important stage of development. He learns quickly, begins to become aware of the world around him, his perception is sharpened and, perhaps, there is anxiety about being separated from his mother. Crying when waking up and being able to eat milk cuddled up to mommy’s chest is a way for a baby to calm down. nine0016 11-13
Resist the urge to "finish" your baby with formula or to start complementary foods early
in an attempt to improve his sleep. Breast milk contains
hormones that make you sleepy and help you both relax
. Studies show that breastfeeding mothers actually sleep longer at night than formula- or formula-fed mothers
. 14
14
How does teething affect breastfeeding?
Teething usually begins around four months of age. When a baby has gum pain, he becomes restless, throws his chest and cries. All this, of course, is unpleasant.
However, breastfeeding can be an excellent sedative.
Studies have shown that babies who are breastfed
during the vaccination period cry less and forget pain more quickly. 15 Breastfeeding during teething can have the same calming effect. nine0003
An unpleasant side effect may be the child's attempts to try out his new teeth on the mother's breast. “Sometimes children flirt and bite their mother’s nipples. This can be felt in advance by how the behavior of the child changes when feeding: before biting, he removes his tongue, explains Cathy, “Usually this is not a problem and only happens a couple of times. It is enough to stop feeding, affectionately say that biting is not good, and the baby will soon leave this fun.
How to continue feeding if you have to be separated from the baby? nine0011
It happens that during the first six months, when the baby is still fully breastfed, the mother needs to be away for several hours - or even longer if she has to go to work or go away on business for a couple of days.
But this does not mean that you should stop breastfeeding. You can still feed your baby healthy breast milk - just express it and have someone give it to your baby when you're away. Here's Katie's advice:
“Start expressing milk a couple of days in advance, in small batches, 40-60 ml at a time. So you will have the necessary supply for the time of your absence, but at the same time the amount of milk produced will remain the same. nine0003
If you have to return to work, check with your employer about your daily schedule. Many mothers breastfeed their babies in the morning, evening and night, and pump milk at lunchtime to relieve discomfort and create a reserve for the next day.
This usually turns out to be much easier than one might think, and today many companies are well placed to do this, notes Cathy. “Breast pumps make it easy to solve this problem.”
Natalie, mother from the USA, shares her experience: “I feed Dylan as soon as he wakes up, and sometimes again before leaving for work, in order to maintain milk production and not lose contact with the child. At work, I pump twice the next day (in my absence, he eats two bottles of breast milk), and after work I rush home for the evening feed. I don't pump on the weekends - we resume regular breastfeeding." nine0003
Can breastfeeding continue after the introduction of solid foods?
When your baby begins to show interest in food and can sit up on his own - usually around six months of age - it's time to start solid foods. However, it is not necessary to stop breastfeeding, Cathy explains: “A baby’s iron stores during pregnancy are depleted by six months, so he needs additional sources of this element.
Start complementary foods with solid foods, but remember that breast milk remains a more important source of calories and nutrients until the baby is eight to nine months old. By this time, he will be eating much more solid food, but he will still need to breastfeed four to five times a day. By 12 months, the frequency of feeding may be two to six times a day. All babies are different, and many of them at this age are still getting half their daily calorie intake from breast milk.” nine0003
Don't forget that breast milk can be added to solid foods, such as cereals and purees, so that the baby can taste the familiar taste. If possible, use milk expressed just before feeding (not thawed) and add just before serving to keep bacteria and nutrients alive. 16
You may be pressured by others to stop breastfeeding when your baby is six months old, but the longer you breastfeed or pump, the better for you and your baby. nine0003
How long can I continue breastfeeding?
“The World Health Organization recommends breastfeeding along with solid foods until at least two years of age because it plays an important role in supporting immunity,” says Cathy. feels bad".
feels bad".
At eight months, the baby sometimes breastfeeds four times a day, but by one year old, the frequency of feedings can be reduced to two times a day. You yourself will understand which feeding regimen is more suitable for you and your baby. For example, Jane, a mother of two from the US, breastfed until the age of two: “I breastfed when I was at home - in the evenings and on weekends, when the children wanted to be close to me,” says Jane, “It helped a lot when they were sick . Breastfeeding has become my favorite form of comfort." nine0003
“When my son got a little older and bolder, he still often asked me to breastfeed him - as if to calm down and gain strength,” recalls Amy, a mother of two children from Canada, “When he happened to hit or skin his knee , breastfeeding was a wonderful way to comfort him.”
If your baby is over a year old and you are still breastfeeding, people around you will probably tell you that this way he will never wean. But if children are not pressured, they usually refuse to breastfeed themselves between the ages of two and four. nine0016 17
nine0016 17
“I didn’t intend to breastfeed for so long, but as a result, I still breastfeed my four-year-old daughter and 22-month-old son,” says Suzanne, mother of two from the UK, “I breastfeed my youngest before and after work, and in I express milk on business trips. The eldest daughter likes to breastfeed a little before bed or when she is upset - this is a great way to make contact. When I get tired of it, I remind myself what great benefit and comfort it brings them. I now plan to pursue a baby-initiated end breastfeeding strategy — let them decide when to stop.” nine0003
For more information on what to expect and lots of tips and tricks, see our guide Breastfeeding Problems After the First Month.
Literature
1 Ballard O, Morrow AL. Human milk composition: nutrients and bioactive factors. Pediatr Clin North Am . 2013;60(1):49-74. - Ballard O., Morrow A. L., "Composition of breast milk: nutrients and biologically active factors." nine0148 Pediatrician Clean North Am. 2013;60(1):49-74.
L., "Composition of breast milk: nutrients and biologically active factors." nine0148 Pediatrician Clean North Am. 2013;60(1):49-74.
2 Kent JC et al. Principles for maintaining or increasing breast milk production. J Obstet , Gynecol , & Neonatal Nurs . 2012;41(1):114-21. - Kent J.S. et al., "Principles for Maintaining and Increasing Milk Production". J Obstet Ginecol and Neonatal Nurse. 2012;41(1):114-121. nine0148
3 Kent J.C. Volume and frequency of breastfeedings and fat content of breast milk throughout the day. Pediatrics. 2006;117(3): e 387-395. - Kent J.S. et al., "Amount and frequency of breastfeeding and fat content of breast milk during the day." Pediatrix (Pediatrics). 2006;117(3):e387-95.
4 Kent JC et al. Longitudinal changes in breastfeeding patterns from 1 to 6 months of lactation. Breast Med . 2013;8(4):401-407. - Kent J.S. et al., Longitudinal changes in breastfeeding patterns from 1 to 6 months of lactation. Brest Med. 2013;8(4):401-407.
Breast Med . 2013;8(4):401-407. - Kent J.S. et al., Longitudinal changes in breastfeeding patterns from 1 to 6 months of lactation. Brest Med. 2013;8(4):401-407.
5 Almroth S, Bidinger PD. No need for water supplementation for exclusively breast-fed infants under hot and arid conditions. Trans R Soc Trop Med 1990;84(4):602-604. - Elmroth S., Bidinger P.D., "No need for supplementation of exclusively breastfed infants in hot, dry conditions." Trans R Sots Trop Med Hyg. 1990;84(4):602-604.
6 Victora CG et al . Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet. 2016;387(10017):475-490. - Victor S.J. et al., "Breastfeeding in the 21st century: epidemiology, mechanisms and long-term effects". Lancet 2016;387(10017):475-490.
Lancet 2016;387(10017):475-490.
7 Peres KG et al. Effect of breastfeeding on malocclusions: a systematic review and meta - analysis. Acta Paediatr. 2015;104( S 467):54-61. - Perez K.G. et al., "The impact of breastfeeding on malocclusion: a systematic review and meta-analysis". Akta Pediatr. 2015;104(S467):54-61.
8 Mennella JA, Beauchamp GK. Maternal diet alters the sensory qualities of human milk and the nursling's behavior. Pediatrics. 1991;88(4):737-744. - Mennella, JA, Beauchamp, GK, "Maternal nutrition influences the organoleptic properties of breast milk and infant behavior." nine0148 Pediatrix (Pediatrics). 1991;88(4):737-744.
9 Hassiotou F et al. Maternal and infant infections stimulate a rapid leukocyte response in breastmilk. Clin Transl immunology. 2013;2(4). - Hassiot F. et al., "Infectious diseases of the mother and child stimulate a rapid leukocyte reaction in breast milk. " Clean Transl Immunology. 2013;2(4).
" Clean Transl Immunology. 2013;2(4).
10 Brown A, Harries V. Infant sleep and night feeding patterns during later infancy: Association with breastfeeding frequency, daytime complementary food intake, and infant weight. Breast Med . 2015;10(5):246-252. - Brown A., Harris W., "Night feedings and infant sleep in the first year of life and their association with feeding frequency, daytime supplementation, and infant weight." Brest Med (Breastfeeding Medicine). 2015;10(5):246-252.
11 Infant sleep information source. [Internet]. Normal Infant Sleep Development; December 2017 [cited 2018 Feb] - All about baby sleep. [Internet] "The development of normal sleep in a child", December 2017 [cited February 2018]. nine0148
12 Baby sleep science. [Internet]. The-Four-Month-Sleep-Regression-What-is-it-and-What-can-be-Done-About-it. March 2014 [ cited 2018 Feb ] - The science of baby sleep. [Internet], "Four-month sleep regression: what it is and what to do about it." March 2014 [cited February 2018].
[Internet], "Four-month sleep regression: what it is and what to do about it." March 2014 [cited February 2018].
13 The Myth Of Baby Sleep Regressions – What’s Really Happening To Your Baby’s Sleep? [Internet]. Pinky Mckay ; December 2017 [ cited 2018 Feb ] - "The Myth of Baby Sleep Regression - What's Really Happening to Your Baby?" [Internet]. Pinky McKay, December 2017 [cited February 2018].
14 Kendall - Tackett K ET AL AL0147 . The effect of feeding method on sleep duration, maternal well-being, and postpartum depression. Clinical Lactation . 2011;2(2):22-26. - Kendall-Tuckett K. et al., "Influence of feeding pattern on sleep duration, maternal well-being and the development of postpartum depression.