Can food cause eczema in babies
7 Foods to Avoid in Babies and Toddlers with Eczema
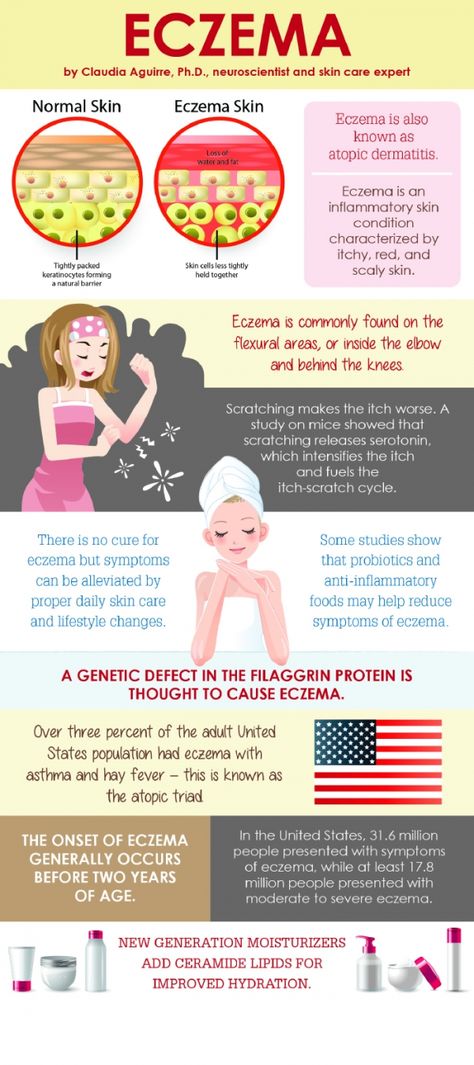
Also known as atopic dermatitis, eczema is a common condition characterized by red, itchy, and inflamed skin.
Although eczema can affect anyone, it’s especially common among children. In fact, about 60% of cases develop within the first year of life (1).
Many factors can worsen eczema flare-ups, including foods.
Research shows that certain foods may trigger eczema in 20–30% of cases of moderate to severe eczema. Additionally, foods are more likely to worsen symptoms in children and infants under age 5 (2).
While foods do not directly cause eczema, making dietary changes could help reduce symptoms, especially for those who have a sensitivity or allergy to specific foods (3).
In children with a confirmed food allergy, eliminating trigger foods from the diet may significantly improve symptoms of eczema within just 1–2 months (4).
However, keep in mind that it’s not necessary to avoid all the foods listed below to help manage your child’s eczema.
SummaryCertain foods may worsen symptoms of eczema, especially in children and infants. However, it depends on the child’s particular allergies or sensitivities, so speak with a healthcare professional to determine which foods might be best to eliminate.
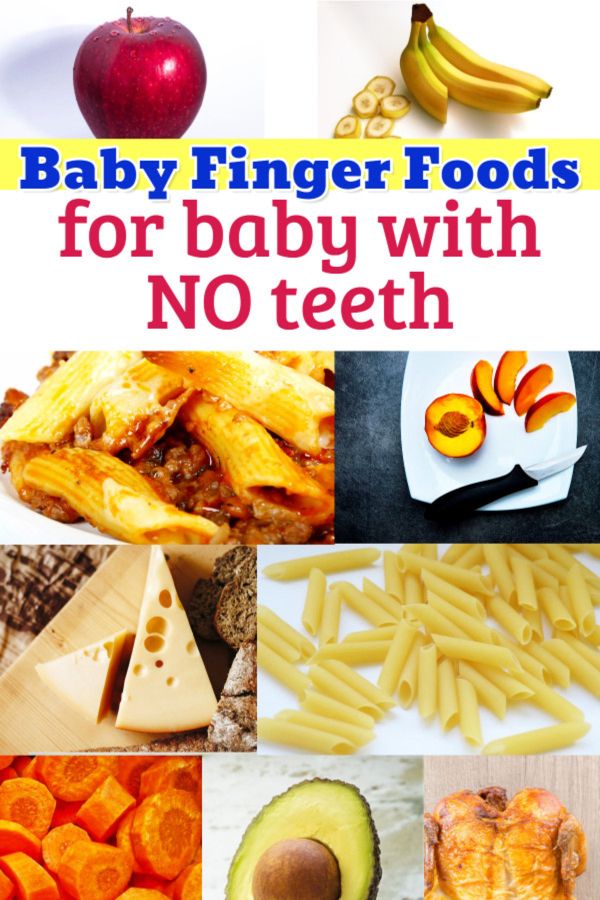
Preventing food allergies
Introducing common allergen foods to an infant early in life may actually help prevent them from developing food allergies, including to eggs and peanuts (5).
If you’re considering eliminating certain foods from your child’s diet or you’re concerned about your child developing food allergies, speak with a healthcare professional. They can help you develop a diet plan based on your child’s needs.
Research has shown that eliminating one or more of these foods from the diet may significantly improve symptoms of eczema in some children.
1. Dairy
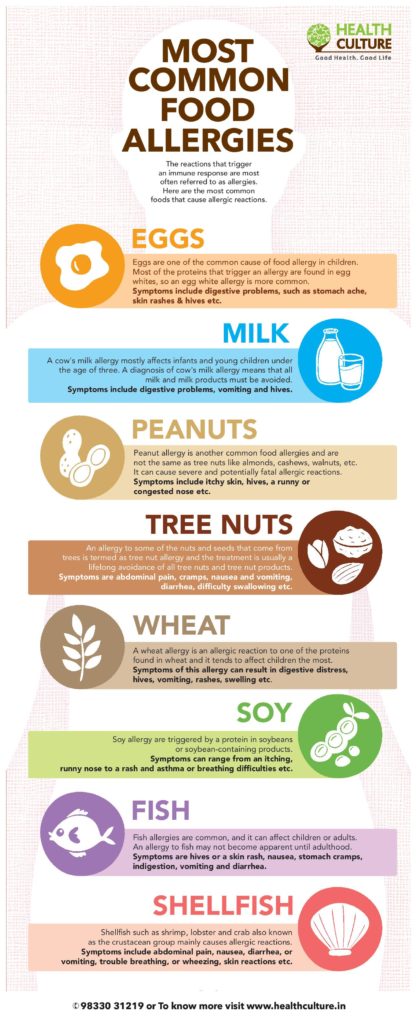
Not only is a cow’s-milk allergy the most common food allergy in young children, but dairy products like milk, yogurt, and cheese are also common triggers for eczema (6).
One study in 132 children with food-triggered eczema found that 39% of children developed an immediate reaction after consuming cow’s milk (2).
A 2019 review reported that infants with eczema were six times more likely to have an allergy to cow’s milk, eggs, or peanuts at 12 months of age compared with infants without eczema (7).
Fortunately, there are several simple plant-based milks available as an alternative to cow’s milk, including soy milk, almond milk, and cashew milk.
However, be sure to check the ingredients lists carefully, as some of these products are high in calories and added sugar.
2. Fish and shellfish
The term “shellfish” refers to any aquatic animal that has a shell-like exterior, including crabs, lobsters, oysters, mussels, and shrimp. Meanwhile, most types of fish, including salmon, trout, tuna, and tilapia, have fins and scales.
Although both fish and shellfish are highly nutritious and can be great sources of protein and omega-3 fatty acids, they can also worsen symptoms of eczema for many children.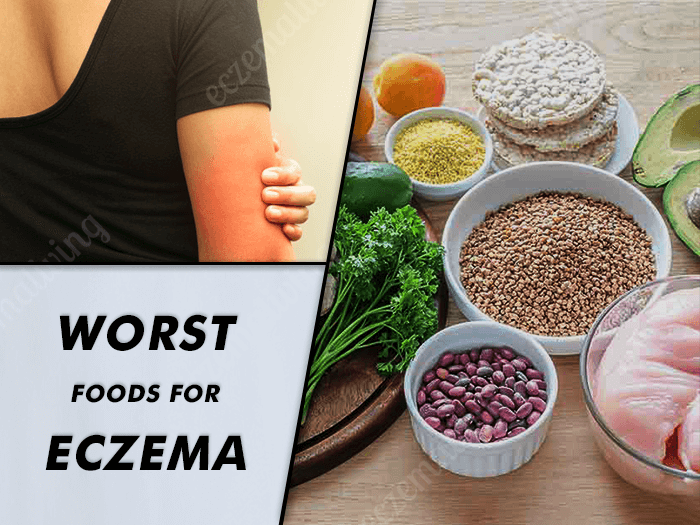
This is because fish and shellfish allergies are common and can cause a wide range of side effects, including hives, itching, and eczema (8, 9).
While some children may be sensitive to finned fish or shellfish, others may experience reactions only to certain types, such as crustaceans (like shrimp and crab) or mollusks (like oysters and clams) (8).
A pediatrician or registered dietitian can help determine which specific types of seafood may trigger symptoms for your baby or toddler.
3. Soy products
For those with a soy allergy, consuming soy products like soy milk, tofu, or edamame can cause an immune response, which could trigger skin reactions such as eczema (10).
Compared with allergies to other major food allergens, soy allergies are not nearly as common (11, 12).
For example, one 2013 study in 175 people with eczema found that around 30% had an immune reaction to soy. However, only about 3% of people experienced symptoms, such as hives and itching, after consuming soy (13).
If your baby or toddler has a sensitivity to soy products, keep in mind that many processed foods contain soy-based ingredients, all of which could worsen symptoms of eczema. Examples include (14):
- soy sauce
- tamari
- soy protein
- textured vegetable protein
4. Eggs
Share on PinterestElena Botta/Getty Images
Some babies or toddlers may have an allergy to the proteins found in egg whites or yolks, which could trigger symptoms of eczema (15).
Egg allergy is one of the most common food allergies, affecting an estimated 1.3% of children under 5 in the United States (16).
Furthermore, one study reported that infants with eczema are nearly 6 times as likely to develop an egg allergy by 12 months of age compared with those without eczema (7).
However, most egg allergies in children resolve by around age 5 (17).
Additionally, some babies and toddlers who are sensitive to eggs may be able to tolerate them in some forms, such as baked eggs (16).
5. Tree nuts
Tree nuts could worsen eczema for many young children with a tree nut allergy. Examples of tree nuts include:
- almonds
- cashews
- walnuts
- pecans
Tree nut allergies are very common and may affect up to 4.9% of children and adults (18).
Unfortunately, tree nut allergies can be very serious, and some research suggests that more severe reactions to tree nuts are often associated with severe cases of eczema, asthma, and seasonal allergies (19).
In addition to avoiding tree nuts specifically, your child may need to avoid foods that contain tree nuts, including pesto, nut butters, coconut products, and certain types of cereals, cookies, crackers, or candies.
6. Wheat or gluten
Wheat is a type of cereal grain and a staple ingredient in many foods, such as bread, pasta, and baked goods.
Gluten is a specific protein found in wheat, barley, and rye that gives dough its structure and elasticity.
For those with a wheat allergy, consuming products that contain wheat may worsen eczema and could also cause other symptoms, including hives, asthma, and digestive issues (20, 21).
Eczema and skin rashes can also be caused by a sensitivity to gluten, as well as by celiac disease, an autoimmune condition that triggers an immune reaction when gluten-containing foods are consumed (22, 23, 24).
While there is no test available to diagnose non-celiac gluten sensitivity, your child’s pediatrician can use a skin or blood test to help determine if your child has celiac disease or an allergy to wheat.
7. Peanuts
Peanuts are a common allergen and are associated with several skin reactions, including rashes, hives, itching, and eczema (25).
Peanut allergies are especially common among babies and toddlers, as most peanut allergies appear within the first 2 years of life (25).
Additionally, some research shows that peanut allergies are more common among infants with moderate to severe eczema (26).
If peanuts cause flare-ups of eczema for your baby or toddler, try swapping other ingredients into your favorite recipes instead, such as seeds or seed butters.
SummarySome of the most common foods that cause allergies in infants and toddlers are dairy, fish, shellfish, soy products, wheat, peanuts, tree nuts, and eggs.
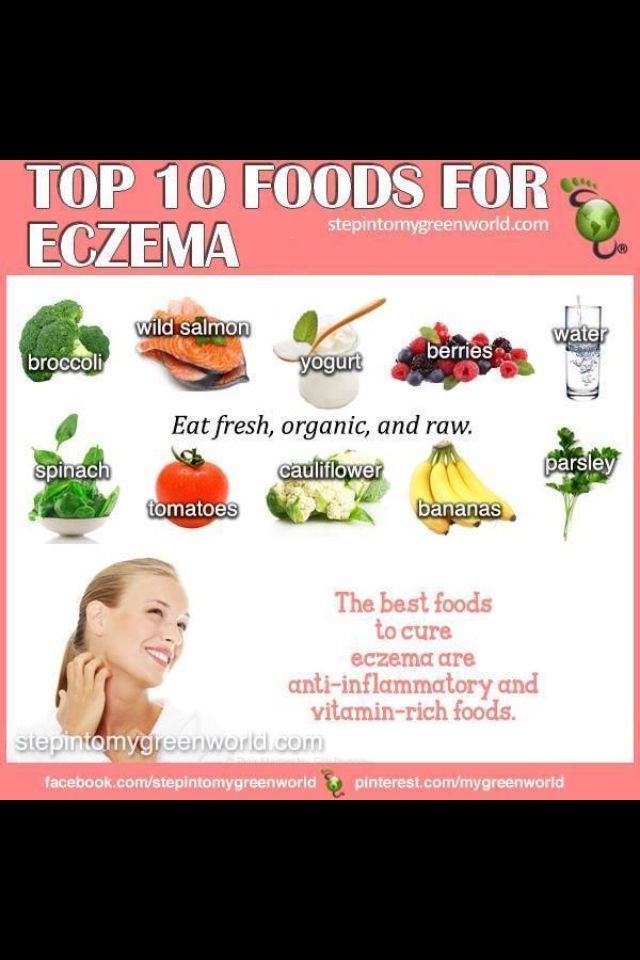
Several foods can be beneficial for eczema and may help reduce symptoms such as itching and inflammation.
For example, fruits and vegetables are rich in antioxidants, which are compounds that can protect against oxidative stress, cell damage, and inflammation (27).
Although studies in humans are still limited, some research suggests that reducing oxidative stress could play a role in managing eczema (28).
Increasing your intake of probiotics through fermented foods or supplements may also be helpful.
According to one review of 13 studies, certain strains of probiotics were effective at reducing eczema severity in children. These strains included Lactobacillus fermentum and Lactobacillus salivarius (29).
However, more research is needed because other studies have found that probiotics do not have a significant effect on symptom severity or quality of life for those with eczema (30).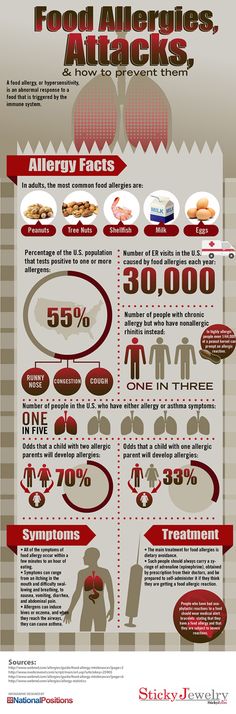
SummaryIncluding more foods rich in antioxidants and probiotics in your child’s diet could be beneficial for eczema, but more research is needed.
For many babies and toddlers, diet can play a key role in managing symptoms of eczema.
While certain foods can make eczema symptoms worse, others may decrease inflammation and oxidative stress, which could reduce symptoms.
However, it’s best to talk with a pediatrician or dietitian before making any changes to your child’s diet, especially because eliminating certain foods from their diet could make it harder for them to meet their nutritional needs.
Additionally, keep in mind that many other factors can contribute to eczema and some children may also need other types of treatment to help relieve symptoms.
Just one thing
Try this today: Consider experimenting with some at-home remedies for your child’s eczema. Check out this article for a few ideas to help provide relief for your baby or toddler.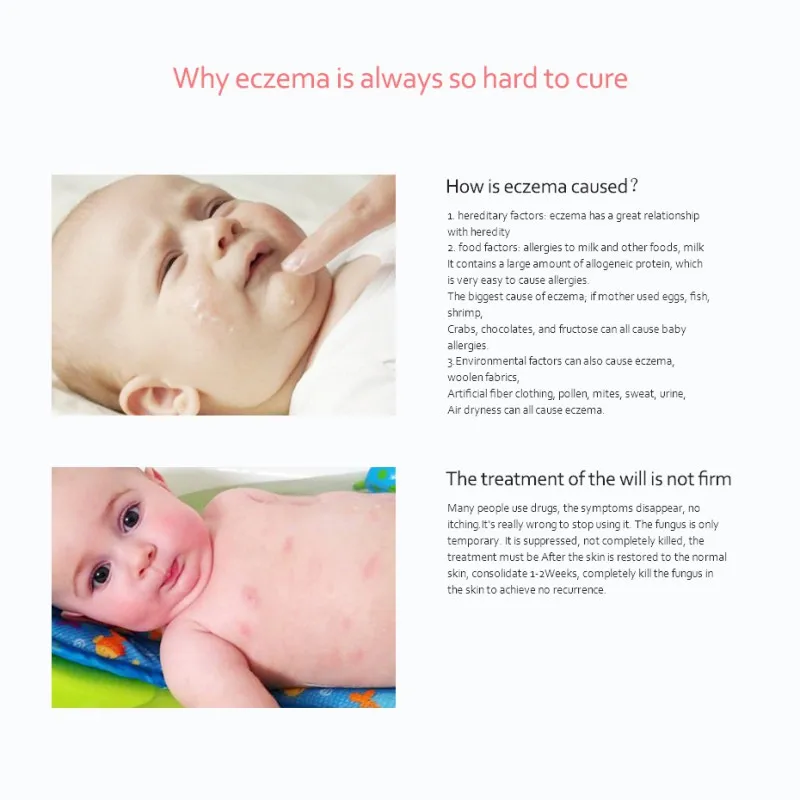
What You Need To Know
Trying to figure out what is triggering your baby’s eczema flare-ups can be a tricky thing. It could be something as obvious as the scratchy blanket in their crib. On the other hand, it could be something considerably less obvious like dust or even the food they come in contact with.
If you’ve taken steps to remove potential triggers from your baby’s environment but they are still suffering from flare-ups, the problem could be food related. Eczema and food allergies are not automatically linked, so diagnosing the specific food that is responsible for a flare-up can be difficult, if not impossible. Additionally, how can you tell if your baby is allergic to specific foods? And what should you do if you suspect that your baby’s eczema is caused by food? Mustela’s experts will answer those questions and tell you everything you need to know about food and your baby’s eczema.
The Connection Between Eczema And Food
The connection between food allergies and eczema can be tricky and confusing. A July 2013 study published in the Journal of Investigative Dermatology reported that infants with eczema had a higher risk of developing food allergies. That said, while there is an increased association of food allergies in children with eczema, the overwhelming majority of children with eczema do not have food allergies.
So just because your baby’s eczema flares-up after a certain meal, it doesn’t mean that it was due to a food allergy. To help you better understand the connection between food and eczema, let’s examine the ways that food can affect your baby’s skin and body.
Food & Your Baby’s Body
At the most basic, there are only two ways that food can have an impact on your baby’s body:
- Through direct food-to-skin contact.
- Through ingestion (eating the food).
The interesting thing about each of these is that only one is likely to cause a localized eczema flare-up, while the other can cause a more system-wide reaction. We’ll explain both individually so you can see the distinction.
We’ll explain both individually so you can see the distinction.
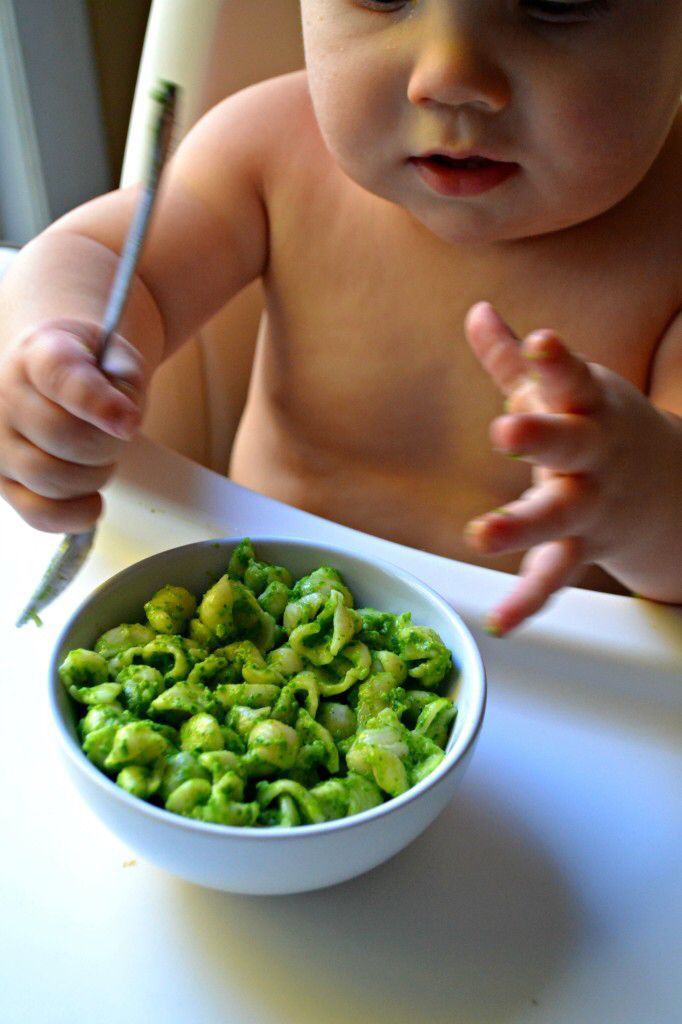
Food-To-Skin Contact
Food-to-skin contact is especially common in young babies who are just learning to feed themselves. We’ve all let our baby feed themselves only to have them smear food onto every corner of their skin. No doubt you’ve got the pictures to prove it. We do too.
If your baby suffers from eczema, it is this type contact that will often lead to a flare-up. That’s because eczema is caused by weakening of the skin’s protective barrier (the hydrolipidic layer) that allows dust, pollen, animal dander, and other allergens to irritate the skin. When this type of irritation occurs, the immune system responds by producing red, itchy, swollen skin at the point of contact. It’s similar to the runny nose and itchy eyes you get during the spring.
The bad thing is that allergens can take many forms, and the food your baby eats may be one of them. This doesn’t necessarily mean that your baby has a food allergy per se. It just means that when your baby touches the food and gets it all over themselves, something on the surface of the food is irritating their skin.
It just means that when your baby touches the food and gets it all over themselves, something on the surface of the food is irritating their skin.
Take tomatoes, and tomato products, for example. If you’ve ever fed your child spaghetti with marinara sauce, you may have noticed redness around their mouth afterward. And if they fed themselves, the redness can extend to their cheeks and hands as well. In eczema-prone skin, this can even trigger a flare-up in these locations. That’s because tomatoes are more acidic than most foods. When that acid comes into contact with your baby’s skin, it can cause irritation, redness, and swelling. This is true even in children who don’t have eczema. So just imagine what it can do to the tender skin of a child who does.
Again, an eczema flare-up caused by food-to-skin contact doesn’t necessarily mean that your baby has a food allergy. It’s just that their sensitive skin reacts to something on, or in, the food itself. An easy way to tell if it’s something in the food that is causing the flare-up is to examine where the redness occurs.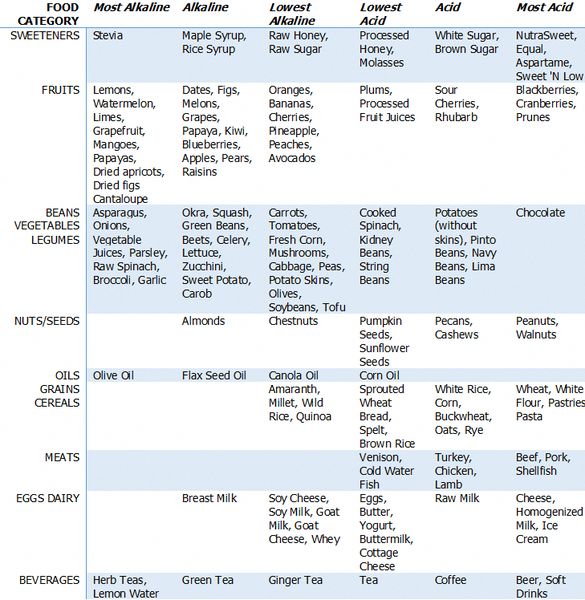 If the swollen skin is isolated to around the mouth and perhaps on the hands (if you let them feed themselves), skin-to-food contact is probably responsible.
If the swollen skin is isolated to around the mouth and perhaps on the hands (if you let them feed themselves), skin-to-food contact is probably responsible.
Ingestion
Ingestion is where the true food allergies present themselves. Thankfully, depending on how you look at it, true food allergies often present themselves differently than the skin-to-food contact we discussed above.
True food allergies produce symptoms such as:
- Wheezing or difficulty breathing.
- A drop in blood pressure.
- Vomiting.
- Diarrhea.
- Stomach cramps.
- Swelling or itching of the mouth and throat.
In general, food allergies result in much more serious symptoms than an eczema flare-up. That’s not to downplay the irritation your baby feels when their skin is itchy and tender, but when the alternative is a trip to the emergency room because their throat is swelling closed, you can see why we label the food allergy the way we do. Common foods that cause allergic reactions include peanuts, fish, eggs, wheat, milk, and soy.
Common foods that cause allergic reactions include peanuts, fish, eggs, wheat, milk, and soy.
Unfortunately, sometimes true food allergies (those caused when your baby ingest a food they are allergic to) can also cause eczema flare-ups. That’s what makes it so difficult to diagnose a simple contact flare-up from an ingestion flare-up. The thing about ingestion flare-ups is that they are usually more widespread than contact flare-ups. Depending on your child’s age, common flare-up sites include behind the ears, behind the knees, wrists, and belly.
So what should you do if you suspect your child’s eczema might be caused by either a contact reaction or an ingestion reaction (food allergy)?
Treat The Eczema And Visit A Doctor
When your child is dealing with an eczema flare-up, the best thing you can do is treat the symptoms with an emollient product like Mustela’s Stelatopia Emollient Cream, Stelatopia Emollient Face Cream, or Emollient Balm. The soothing formula found in Mustela products can reduce irritation by up to 95%. Best of all, Mustela’s emollient products can help your child’s skin begin to make its own protective layer again. This is good news for you and your baby.
Best of all, Mustela’s emollient products can help your child’s skin begin to make its own protective layer again. This is good news for you and your baby.
Expert tip: for added protection and relief, dress your little one in Mustela's Stelatopia Skin Soothing Pajamas before bed. Made with natural ingredients, these pajamas deliver soothing moisture to your baby's skin all night. This results in less scratching and faster healing.
We recommend treating a flare-up until it goes away, or for a week, whichever comes first. Then, if you still think your child’s eczema may be caused by food, visit a doctor to find out for sure. Your family doctor will refer you to a dermatologist or an allergist who will test your baby’s skin to determine exactly what they are allergic to. These tests will reveal if your baby has an allergy or not. Armed with that knowledge, you can take steps to prevent eczema flare-ups from happening again.
Eczema: what is it, symptoms, causes, types, treatment and diet
Eczema is a chronic inflammatory skin disease of an allergic nature. The causes of the onset and development of pathology have not yet been studied, but it is believed that allergic diseases and genetic prerequisites are provoking factors. Treatment of eczema is carried out successfully today. You just need to turn to experienced professionals.
The causes of the onset and development of pathology have not yet been studied, but it is believed that allergic diseases and genetic prerequisites are provoking factors. Treatment of eczema is carried out successfully today. You just need to turn to experienced professionals.
What is eczema?
This is a disease characterized by inflammatory processes and characterized by:
- A large number of developmental provoking factors
- Many variants of rash
- Tendency to relapse
- Highly resistant to treatment
Typically, an eczema rash concentrates on areas such as:
- Neck
- Knee bends
- Elbows
- Ankles
Symptoms of pathology can periodically increase. Such attacks last from a couple of hours to several days.
Classification
In accordance with the characteristics of the course of the pathological condition, the following are distinguished:
- Acute eczema.
 Her symptoms usually persist for 1-2 months
Her symptoms usually persist for 1-2 months - Subacute . Symptoms of this pathology are less pronounced. In this case, the pathology can accompany the patient up to 6 months
- Chronic. In this case, the disease may last for several years. Periods of relapses follow remissions
There are several types of pathology:
- True . Such eczema is characterized by a chronic course. Exacerbations occur frequently and are accompanied by the appearance of symmetrical foci of inflammation. At first, areas of the skin turn red and swell. After that, small bubbles form on them. Over time, they open with the release of exudate (a small amount of liquid)
- Microbial . This form of pathology is characterized by the formation of deep ulcers and fistulas. Pathology is accompanied by severe itching. In the microbial form, foci of inflammation spread mainly to the legs
- Seborrheic . This form is characterized by rashes on the face (on the forehead, near the eyebrows, behind the ears) and the scalp.
 Complete restoration of the skin is possible only with correct therapy
Complete restoration of the skin is possible only with correct therapy - Child . This form is characterized by a large amount of exudate
- Professional . This form of pathology is characterized by vivid manifestations. The rash can appear on various areas of the skin (usually those that come into contact with irritants). Irritants in occupational eczema can be either chemical or physical or mechanical. Usually, pathology is provoked by constant exposure to cosmetics, active chemicals, various plants, resins, metals (mainly nickel and chromium)
Causes
Eczema, the treatment of which should only be carried out by professionals, is quite common.
Its causes include a number of internal and external factors.
Internal factors for the development of eczema:
- Disorders of the nervous system
- Pathologies of internal organs
- Genetic factors (heredity)
External factors provoking pathology:
- Increase or decrease in temperature
- Exposure to aggressive chemicals
- Influence of extracts of various plants, etc.
Often, a combination of internal and external factors provokes pathology.
Eczema can be the body's response to:
- Contact with pollen
- Excessive sweating
- Immune system disorders
- Stress
- Taking medications
- Reception of certain products
Before starting the treatment of eczema, it is very important to identify the causes that provoked the onset of pathology. Only in this case, the therapy will be as effective as possible and will not drag on for a long time.
Symptoms
All types of eczema are characterized by the following symptoms:
- Appearance of individual inflamed areas on the skin
- Appearance of rash
- Itching
- Blisters
- Wounds and fissures that cause permanent discomfort
- Increase in body temperature during exacerbations
- General malaise and weakness
- Cracking of the skin, its pronounced dryness and loss of elasticity
Symptoms of the pathological condition largely depend on the stage of development of eczema.
At erythematous stage the disease manifests itself in the form of inflamed areas. Gradually, the spots can merge into a separate affected area, which has an impressive area.
At papular stage the affected skin becomes unpleasant to the touch. It forms small nodules with clear boundaries and a bright red color.
At vesicular stage nodules turn into vesicles.
At the stage of wetting , the vesicles gradually open, and liquid is released from them.
At the cortical stage the inflamed areas dry up. Yellowish crusts form on the skin.
At stage dry eczema the skin begins to peel off. Formed crusts gradually disappear. Do not try to rip them off yourself! This can provoke the resumption of pathology.
Diagnosis
Treatment of eczema in adults is possible only after a thorough assessment of its symptoms and causes. That is why it is very important for a doctor to conduct a high-quality diagnosis.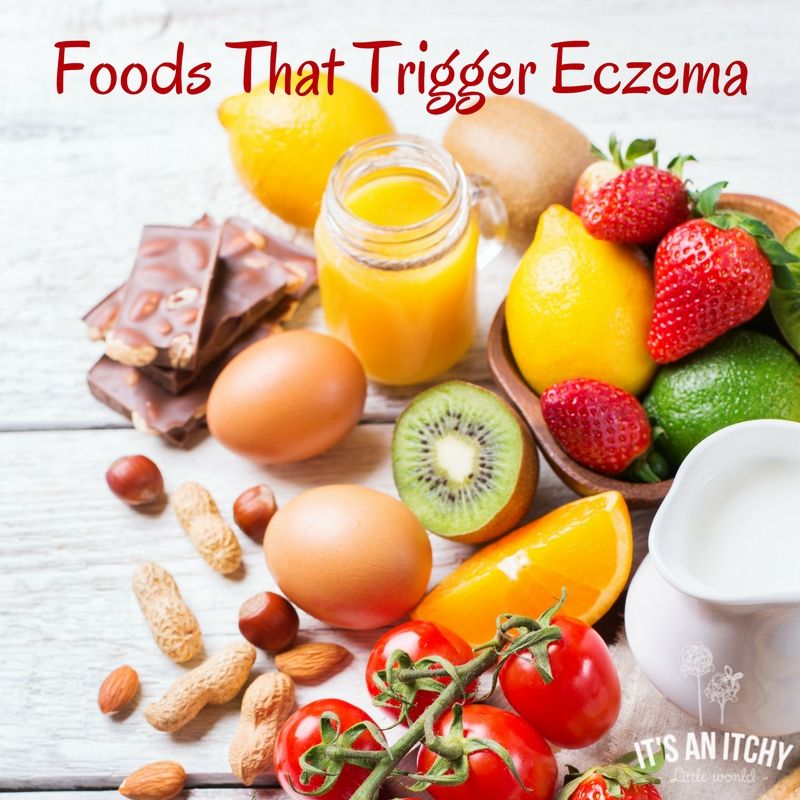
It begins with the collection of anamnesis.
The doctor explains:
- The first cases of manifestation of signs of a pathological process
- Presence of intolerance to certain foods and drugs
- Allergic reactions
At the first appointment, the dermatologist performs a dermatoscopy. This study is aimed at studying the condition of the skin, mucous membranes and scalp.
Then laboratory tests are carried out.
For the diagnosis of eczema are assigned:
- Urinalysis
- Blood tests
- Serum immunoglobulin test
During the examination, the specialist determines the general state of health of the patient, evaluates individual vital signs. If necessary, a consultation with a nutritionist and an immunologist-allergist is carried out.
In advanced situations, a comprehensive immunological and allergological examination with sampling is also prescribed. As part of such a diagnosis, doctors are able to identify irritating factors that can provoke symptoms of eczema and allow you to quickly begin to treat the pathology.
As part of such a diagnosis, doctors are able to identify irritating factors that can provoke symptoms of eczema and allow you to quickly begin to treat the pathology.
Treatment
The main task of the doctor after making a diagnosis such as eczema is to reduce or completely eliminate the factors that provoke the onset of symptoms.
Treatment of pathology is conditionally divided into several stages:
- Taking general medications
- Diet modification
- Use of topical agents in the form of ointments, emulsions, creams, etc.
- Physiotherapy
The following groups of drugs are used for therapy:
- Antihistamines . Such remedies are prescribed for acute eczema
- Glucocorticosteroids . These hormonal preparations relieve inflammation and prevent the development of allergic reactions
- Diuretics . Such funds are recommended for severe edema
- Tranquilizers .
 These drugs allow you to eliminate itching, ensure a sound and healthy sleep of the patient, his good rest even with severe discomfort in the acute stage of eczema
These drugs allow you to eliminate itching, ensure a sound and healthy sleep of the patient, his good rest even with severe discomfort in the acute stage of eczema - Enterosorbents . These funds allow you to quickly remove all the products of intoxication from the intestines
- Vitamins of group B aimed at normalizing the functioning of the nervous system
- Antibiotics . These funds are prescribed if, as a result of the diagnosis, it turned out that eczema is provoked by the action of aggressive microorganisms
Locally, applications with pastes and ointments are usually prescribed, which have:
- Antipruritic
- Anti-inflammatory action
- Antiseptic properties
Compositions of preparations for external use are often selected individually. In some cases, "talkers" are prescribed, which are prepared in pharmacies according to a doctor's prescription.
Important! It is strictly forbidden to use folk remedies, various oils, plant extracts, etc. for the treatment of eczema. They are able not to stop the development of the pathological process, but to provoke it.
for the treatment of eczema. They are able not to stop the development of the pathological process, but to provoke it.
With regard to physical therapy, patients are usually prescribed:
- UV irradiation
- Magnetotherapy
- Electrophoresis
Treatment of weeping eczema is carried out with the obligatory use of drugs that allow you to dry the skin and ensure the elimination of external signs of pathology. Treatment of other forms of the disease also has individual specificity. The attending physician will tell you about all the subtleties.
There are also general recommendations that should be followed by all patients suffering from the disease.
- Avoid skin contact with aggravating substances (if such substances are identified by tests and samples)
- Dieting. Cocoa, citrus fruits and chocolate should be completely excluded from the diet
- Skin care only with products recommended by a physician
- Elimination of nervous overload and stressful situations
Diet
The basis for the recovery of patients with eczema is often a properly selected diet. When selecting the products you need, the doctor takes into account both the general state of health and the stage and form of the pathology, as well as the presence of concomitant diseases.
When selecting the products you need, the doctor takes into account both the general state of health and the stage and form of the pathology, as well as the presence of concomitant diseases.
There are also general recommendations regarding nutrition.
All patients during an exacerbation should:
- Avoid spicy, salty and smoked foods
- Refuse sweets
- Eliminate citrus fruits, eggs, alcoholic beverages, dairy products and processed foods from the diet
The diet should include:
- Green
- Lean cereals
- Vegetables
During periods of remission, it is desirable to use zucchini and pumpkin, watermelons, gooseberries, lingonberries, currants and cranberries, nuts. Patients who adhere strictly to the diet usually improve rapidly. After a month, the diet can be expanded.
With eczema, the following foods and drinks are strictly prohibited:
- Coffee and cocoa
- Sweets
- Fatty meat
- Tomatoes
- Garlic
- Buns and other pastries
- Melon
- Grenades
- Beetroot
- Strawberry
- Honey
It is advisable to use only those products that are hypoallergenic.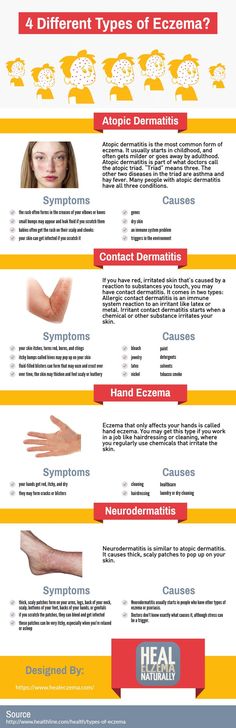 A complete list will be given to you by your doctor.
A complete list will be given to you by your doctor.
Benefits of treatment at MEDSI
- Comprehensive diagnosis of eczema . The examination includes laboratory tests, dermatoscopy and video dermatoscopy. Diagnostics is carried out on modern equipment. We have our own laboratory, which allows us to provide patients with test results in the CITO mode (urgent)
- Individual selection of methods for the treatment of eczema in adults and children. Therapy is prescribed taking into account the stage of the pathological process and the characteristics of its course
- Use of modern preparations in . Patients are prescribed anti-inflammatory, disinfectant and other drugs that have been developed recently, but already have proven effectiveness
- Modern physiotherapy procedures . Our clinics offer UVA therapy, ozone therapy, magnetotherapy. The combination of modern techniques allows you to achieve pronounced results of treatment in the shortest possible time
- Treatment of eczema with laser devices .
 Our clinic has the Excilite µ system. It belongs to the latest generation of excimer lasers. The procedures are painless and do not cause discomfort in patients. At the same time, the treatment of signs of eczema with such a system takes a minimum of time
Our clinic has the Excilite µ system. It belongs to the latest generation of excimer lasers. The procedures are painless and do not cause discomfort in patients. At the same time, the treatment of signs of eczema with such a system takes a minimum of time
To make an appointment with a doctor, just call +7 (495) 7-800-500. Reception is possible at a convenient time for you in a comfortable environment.
Do not delay treatment, see a doctor now:
- Dermatologist appointment
- Treatment of nail diseases, care and restoration
- Treatment of eczema
Good to know about ECZEMA (eksem)
Good to know about ECZEMA ( eksem)
Useful information about eczema Allergy and asthma sufferers - Information leaflet of the Norwegian Allergy and Asthma Association
What is eczema?
Eczema is a general name for various skin diseases accompanied by itching. The most common forms of eczema are atopic, occupational (contact), seborrheic, and childhood. Atopy means "difference". In this case, it refers to differences in skin properties and describes hereditary allergic eczema.
The most common forms of eczema are atopic, occupational (contact), seborrheic, and childhood. Atopy means "difference". In this case, it refers to differences in skin properties and describes hereditary allergic eczema.
Eczema may be chronic ie. with prolonged, or acute form of the course of the disease and in most cases is characterized by improvement in the summer and worsening in winter. The chronic form is characterized by the appearance of a rash with itching. The result of scratching is often the formation of thickened areas of the skin that crack easily. Acute eczema is characterized by itching, redness and swelling of the skin with the possible formation of watery blisters.
In eczema, there is a deterioration in the body's defense against infections, which easily leads to infectious inflammation, which can lead to a worsening of eczema.
Symptoms of eczema
Atopic eczema results in itchy, dry skin.
New or recurrent contact eczema is characterized by itching, redness and swelling of the skin with the formation of small and large blisters, as well as wet sores in places of direct exposure to the allergen.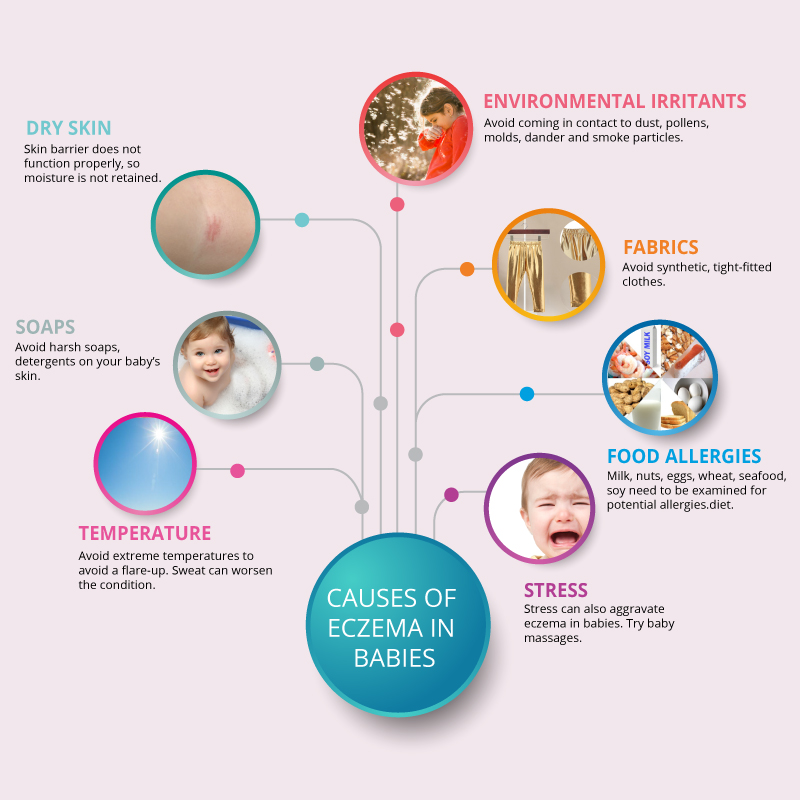 With prolonged contact eczema, the skin becomes increasingly dry and cracked. Severe itching is common. In the initial stage, eczema is observed only on the area of \u200b\u200bthe skin that was exposed to the allergen, but then the rash can spread to other areas.
With prolonged contact eczema, the skin becomes increasingly dry and cracked. Severe itching is common. In the initial stage, eczema is observed only on the area of \u200b\u200bthe skin that was exposed to the allergen, but then the rash can spread to other areas.
With seborrheic eczema in infants, there is the formation of areas with oily, red skin, covered with oily crusts, on the forehead, head, face, as well as in the skin folds on the neck and in the perineum. In adults, it appears as scaly, red, oily skin on the central areas of the face, on the head, behind the ears, and on the chest.
Baby eczema is accompanied by the formation of red, smooth, sometimes wet areas of the skin in diaper wear areas.
Who can get eczema?
Atopic eczema primarily affects young children. It is estimated that about 15% of Norwegian children suffer from eczema. Often the disease occurs in children in the first months of life, in 60% of them it disappears by the age of four.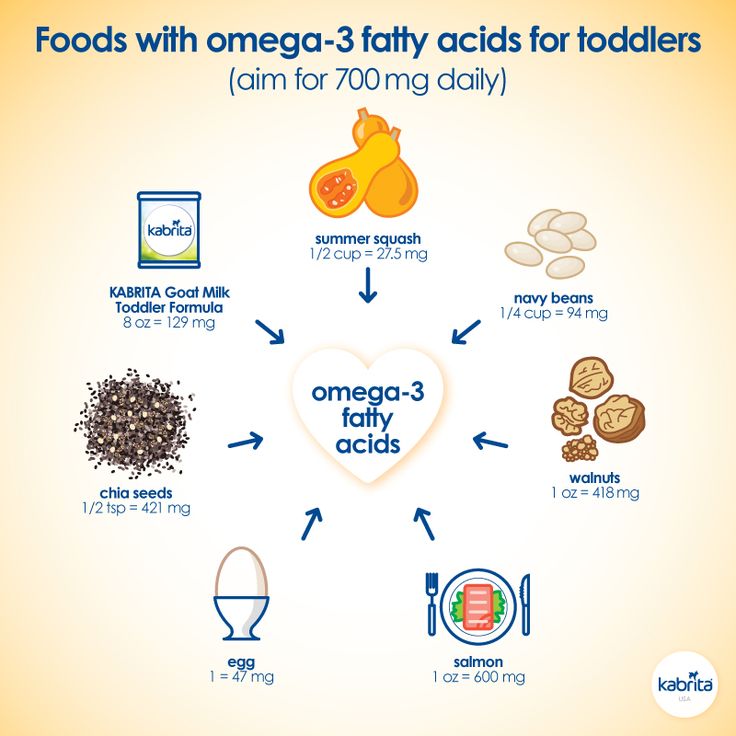 However, recurrence of the disease may occur in adolescence or adulthood.
However, recurrence of the disease may occur in adolescence or adulthood.
Contact eczema is rare in young children, but its occurrence is becoming more common from school age. Ear piercings, body piercings and base metal contact with the skin are responsible for a significant increase in nickel contact allergies. Getting a tattoo can lead to allergic contact eczema, which can occur weeks or even months after getting a tattoo. Hair coloring is also an increasingly common cause of eczema, especially as more and more young people dye their hair.
Seborrheic eczema is relatively common. Eczema can appear as early as the first months of life, but usually occurs in adults.
Causes of eczema
The cause of atopic eczema is unknown. Allergies can play a role, but only in conjunction with other factors. The disease has a connection with heredity and the environment. The presence of atopic diseases in other family members (asthma, eczema or allergic rhinitis) is common. In 20-30% of patients, allergies can be detected, which for some of them may be the cause of eczema. Food allergies are never the only cause of eczema.
In 20-30% of patients, allergies can be detected, which for some of them may be the cause of eczema. Food allergies are never the only cause of eczema.
Seborrheic eczema is not caused by hypersensitivity, but by a painful reaction in the sebaceous glands, possibly caused by a specific yeast normally found on the surface of the skin. This form of eczema is especially prone to people with oily skin and increased productivity of the sebaceous glands.
Contact eczema occurs when the skin reacts to contact with certain substances. The reaction may be allergic or non-allergic. A non-allergic reaction occurs in direct contact with skin irritating substances such as detergents or disinfectants. An allergic reaction is caused by allergenic substances such as nickel, chromium, rubber, formaldehyde and perfumes. Paraphenylenediamine (PPD) is one of the substances frequently associated with allergic contact eczema. PPD is found in many types of hair dye.
Childhood eczema is caused by irritants found in urine and feces.
Treatment of eczema
In the treatment of eczema, the most important thing is hygiene, the systematic use of creams and ointments to prevent drying of the skin, refraining from scratching, reducing exposure to irritants and refraining from eating foods known to be allergic. Sunlight and salt baths work well for mild to moderate eczema. Regular bathing with calcium permanganates gives a good preventive effect.
However, in most cases a cortisone ointment is necessary. The indicated treatment will give the desired result, provided that the correct drug is applied to the appropriate area of \u200b\u200bthe body at the prescribed frequency. Once control of eczema is established, it is important to reduce the concentration of cortisone ointment, and, if necessary, increase the intervals between applications of the ointment. Proper use of cortisone ointment does not lead to negative effects. The attending physician will give you the necessary recommendations for the use and reduction of the concentration of the drug.
In general terms, it can be said that it is necessary to use strong drugs for a sufficiently long period of time. By opting for weaker drugs, you will not be able to get eczema under control. In this case, the whole process of cortisone treatment may be in vain. Often this leads to increased eczema. It is important to remember that the poor effect of cortisone ointment is due to infection in the eczema itself, which should be treated with antibiotics, both locally and in general.
In the event of a new flare-up of eczema in a child with a history of the condition, treatment may be initiated with cortisone group 2 or 3. Once the condition has stabilized, the application may be made less frequently (at intervals of 2-3 days). With further improvement in the condition, you can switch to a weaker ointment in order to eventually switch to applying the drug with an interval of 2-3 days.
After healing of eczema, it is recommended to continue applying the drug 1-2 times a week for at least 2-4 weeks in order to achieve the best result. It is also recommended to use a moisturizer in the morning and evening, as well as every time after taking a bath or shower, even during periods without eczema.
It is also recommended to use a moisturizer in the morning and evening, as well as every time after taking a bath or shower, even during periods without eczema.
Children suffering from eczema that regularly flares up and worsens benefit from calcium permanganate baths even during good times. During periods of active eczema, baths with calcium permanganate can be done every day or every other day.
Cortisone-free anti-eczema ointments (Elidel®, Protopic®) are good alternatives to try for chronic eczema. These ointments are applied daily, twice a day. The advantage of these ointments is that they do not affect the thickness of the skin even with prolonged use, and also that they can be used in cases where treatment with cortisone ointments does not lead to the desired result and control of eczema is not established by treatment with cortisone ointments without risk. side effects.
For skin infections, the infection itself must be treated first, and then the above remedies should be applied.
Medical light or climate treatments for eczema may work. However, some patients may experience a temporary increase in eczema, which is probably due to sweat irritation. In addition, such treatment requires a lot of money and time, which makes it unacceptable for school-age children. This treatment is carried out exclusively by doctors specializing in skin diseases.
Achieving positive results depends on how well the patient is informed about the treatment. Eczema can be a very debilitating disease, but early treatment can in most cases bring it under control. Fortunately, the disease eventually subsides on its own, and 80% of patients recover by the age of 18. There is evidence to suggest that quality treatment of eczema leads to an improved prognosis.
Aggravating factors
Rough, tight clothing, rough wools, polyester, heavily dyed fabrics, moisture, stress, infections, food, chlorinated water, tobacco smoke, perfumes, allergies, alkaloid soaps, degreasing chemicals and exposure to heat.
The child knows what clothes cause itching!
Prevention of eczema
Prevention of eczema by controlling the mother's diet during pregnancy, or after the birth of the child, has no effect on the development of atopic eczema in the child. Research shows that symptoms of atopic eczema may be delayed in some cases in children who are breastfed for the first four to six months of life.
Where to get help
For mild sporadic eczema in children, getting advice from a nurse may be enough. In more complex cases, you should contact your doctor, who, if necessary, will write a referral to a specialist. The hospital free choice system in Norway allows for informed choice. On the Internet site www.frittsykehusvalg.no and free of charge on 800 41 004, you can find out about available eczema treatment sites and your rights in choosing a hospital.
People suffering from eczema and other skin diseases, as well as people who work with this group of patients, can communicate with specialists at the skin disease clinic, Villa Derma, Oslo University Hospital, by contacting the “skin phone” 23075803 , open for calls three hours a week according to the following schedule: Tuesday and Friday from 8 am to 9 am, Thursday from 12 am to 1 pm (check that this schedule is correct!).