Can you feed baby breast milk and formula
How to combine breast and bottle feeding
It can take several weeks for you and your baby to feel happy and confident with breastfeeding.
Once you've both got the hang of it, it's usually possible to offer your baby bottles of expressed milk or formula alongside breastfeeding.
This is sometimes called mixed or combination feeding.
Why combine breast and bottle?
You may want to combine breastfeeding with bottle feeding if you:
- are breastfeeding and want to use a bottle to offer your baby some expressed breast milk
- want to breastfeed for some of your baby's feeds, but give bottles of formula for 1 or more feeds
- are bottle feeding your baby and want to start breastfeeding
- need to leave your baby and want to make sure they have some milk while you're away
Introducing formula feeds can affect the amount of breast milk you produce. There is also a small amount of evidence to show babies may not breastfeed as well because they learn to use a different kind of sucking action at the bottle than at the breast.
These things can make breastfeeding more difficult, especially in the first few weeks when you and your baby are still getting comfortable with breastfeeding.
Your breastmilk supply will usually not be affected if you start bottle feeding your baby when they are a bit older, you are both comfortable with breastfeeding, and you breastfeed every day.
Introducing formula feeds
If you're combining breastfeeding with formula feeds both you and your baby can carry on enjoying the benefits of breastfeeding.
If you choose to introduce infant formula:
- it's best to do it gradually to give your body time to reduce the amount of milk it makes – this helps lower your chance of getting uncomfortable, swollen breasts, or mastitis
- if you're going back to work, start a few weeks beforehand to give both of you time to readjust
- if your baby is 6 months old or more and can drink milk from a cup, you may not need to introduce a bottle at all
For more information, see drinks and cups for babies.
Giving your baby their first bottle
It may take a while for a breastfed baby to get the hang of bottle feeding, because they need to use a different sucking action.
- it usually helps to give the first few bottles when your baby is happy and relaxed – not when they're very hungry
- it may help if someone else gives the first bottle feeds, so that your baby is not near you and smelling your breast milk
- you might want to try using a different position for bottle and breastfeeding
See more advice on how to bottle feed.
Restarting breastfeeding
If you want to start breastfeeding more and give your baby fewer bottles, it's a good idea to ask your midwife, health visitor or breastfeeding supporter for support.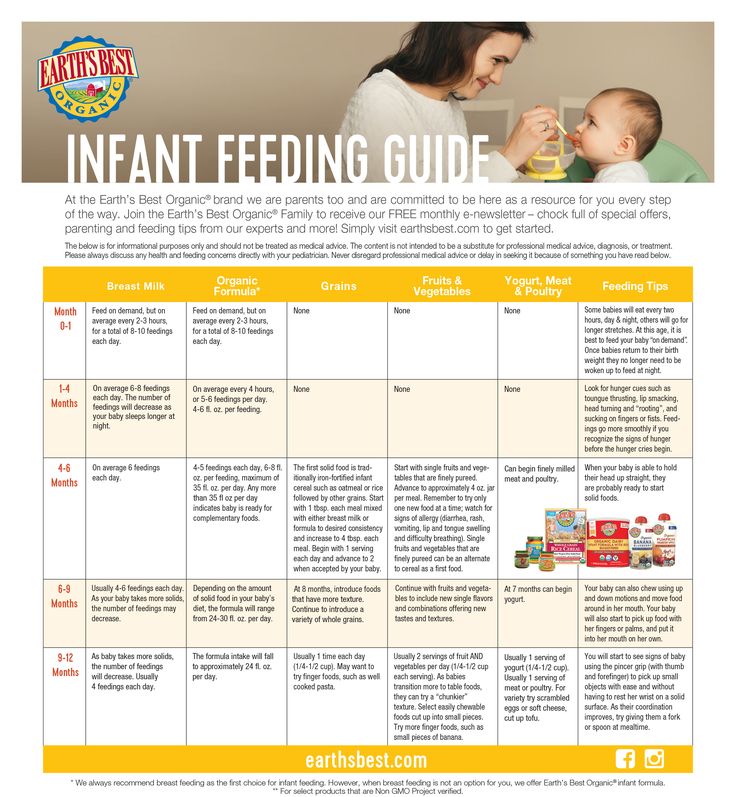
These tips may help too:
- Hold and cuddle your baby as much as possible, ideally skin to skin. This will encourage your body to make milk and your baby to feed.
- Express your breast milk regularly. Expressing releases the hormone prolactin, which stimulates your breasts to make milk. About 8 times a day, including once at night is ideal. It may be easier to express by hand to begin with – your midwife, health visitor or breastfeeding supporter can show you how.
- Try bottlefeeding while holding your baby skin to skin and close to your breasts.
- If your baby is latching on, feed little and often. Do not worry if your baby does not feed for long to begin with. See tips on how to get your baby properly positioned and attached.
- Choose times when your baby is relaxed, alert and not too hungry, and do not force your baby to stay at the breast.

- Decrease the number of bottles gradually, as your milk supply increases.
- Consider using a lactation aid (supplementer). A tiny tube is taped next to your nipple and passes into your baby's mouth so your baby can get milk via the tube as well as from your breast. This helps to support your baby as they get used to attaching to the breast. Your midwife, health visitor or breastfeeding supporter can give you more information.
See more tips on boosting your milk supply.
Help and support with mixed feeding
If you have any questions or concerns about combining breast and bottle feeding:
- talk to your midwife, health visitor or breastfeeding supporter
- call the National Breastfeeding Helpline on 0300 100 0212 (9.30am to 9.30pm, every day)
- find breastfeeding support near you
Video: why combine breast and bottle feeding?
In this video, 3 mothers discuss ways to combine breast and bottle feeding.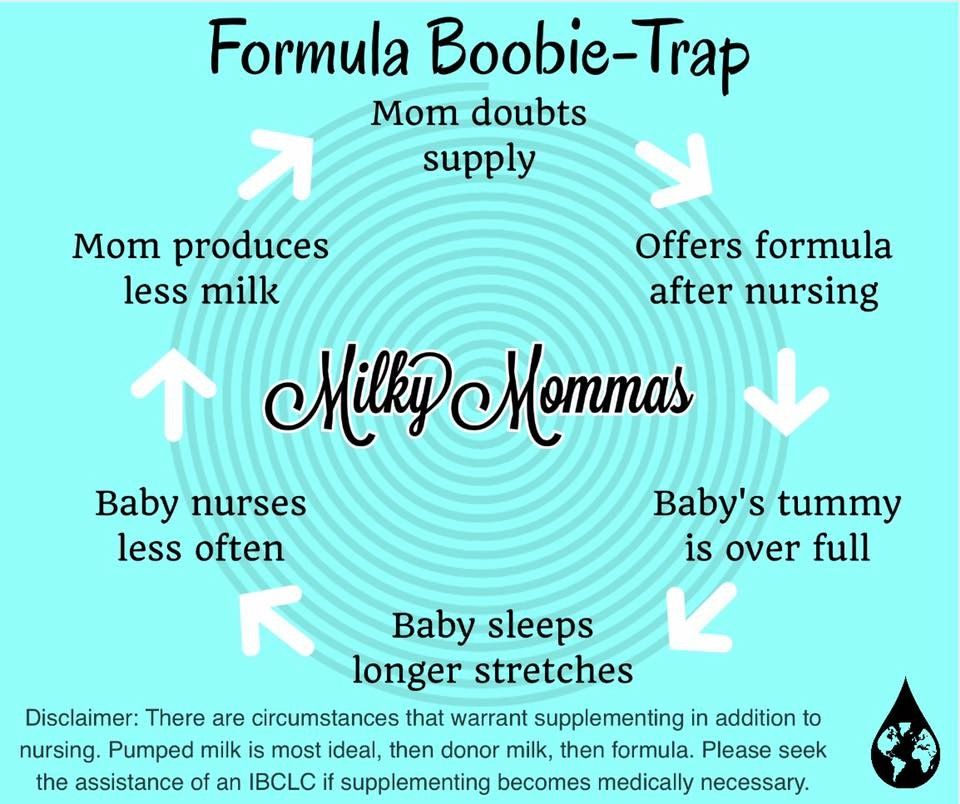
Media last reviewed: 22 March 2020
Media review due: 22 March 2023
Page last reviewed: 8 October 2019
Next review due: 8 October 2022
Formula Feeding and Breastfeeding: Can You Do Both?
Our editorial team personally selects each featured product. If you buy something through our links, we may earn an affiliate commission, at no cost to you.
Can you breastfeed and formula-feed a baby? The short answer is YES. It’s called combination feeding, or more commonly, combo feeding. If you’re looking to supplement and extend your breastfeeding journey or if you want to make feedings possible by other parents or care-takers, combo feeding can be a great solution.
We sat down with Tiffani Ghere, a pediatric dietician, certified specialist in Pediatric Nutrition, and Bobbie medical advisor. It turns out that formula milk and breast milk aren’t black and white options.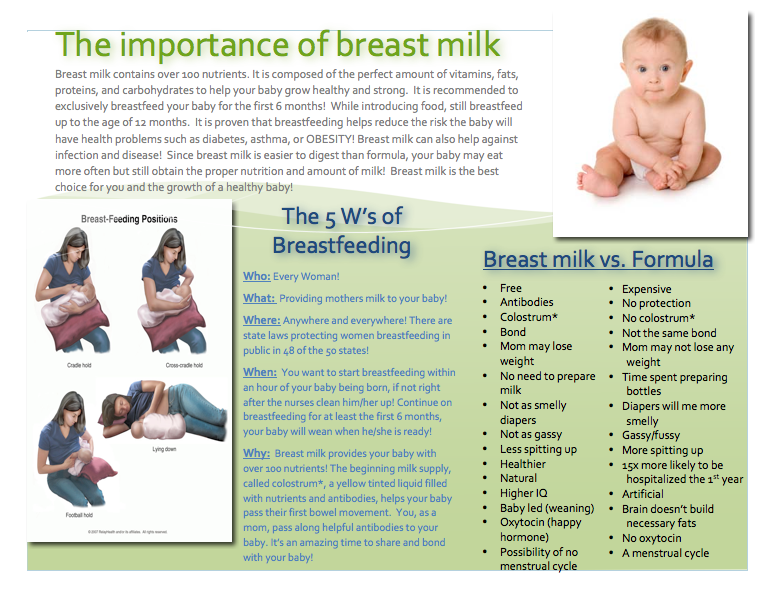 Here’s what we learned.
Here’s what we learned.
Table of Contents
- Is it ok to breastfeed and formula feed at the same time?
- 4 Tips to help ease your baby into combo feeding
- How does the transition from breast milk to baby formula affect mom?
- Benefits of breastfeeding for mom and baby
- Why parents choose formula feeding
- Doctors may recommend supplementation
- Our take on combo feeding
Is it ok to breastfeed and formula feed at the same time?
Often times, there’s a conversation about exclusively breastfeeding or exclusively formula feeding. It can make new parents feel that they have to make a choice. But did you know it’s actually quite easy to combo feed?
We’ll give you a few pointers about what to consider if you decide to have both bottles of baby formula and bottles of breast milk on your little one’s menu.
A mother’s intuition helps decide the feeding choice
Following your intuition is always best! Trust what you think is right for your baby. You have the power to make great decisions for your baby, so don’t let anyone sway you otherwise.
You have the power to make great decisions for your baby, so don’t let anyone sway you otherwise.
Talk to your health care providers and your baby’s pediatrician to feel confident in the decision that works best for you and your family.
Is nipple confusion a concern?
When you mix formula feeding and breastfeeding in a baby’s diet, they likely won’t fuss about the real nipple or bottle nipple. They may not even know the difference most of the time, and nipple confusion isn’t as prominent as most expect.
Some doctors may recommend exclusive breastfeeding for the first few weeks until you introduce a bottle of formula to give them an easier introduction.
Breastfeeding poop can be different than formula poop
Since there’s a different type of milk entering your baby’s system, it makes sense that it may exit differently, too. Keep this in mind and watch to see if your baby’s stool looks different or irregular. Formula poop can be different than breast milk poop.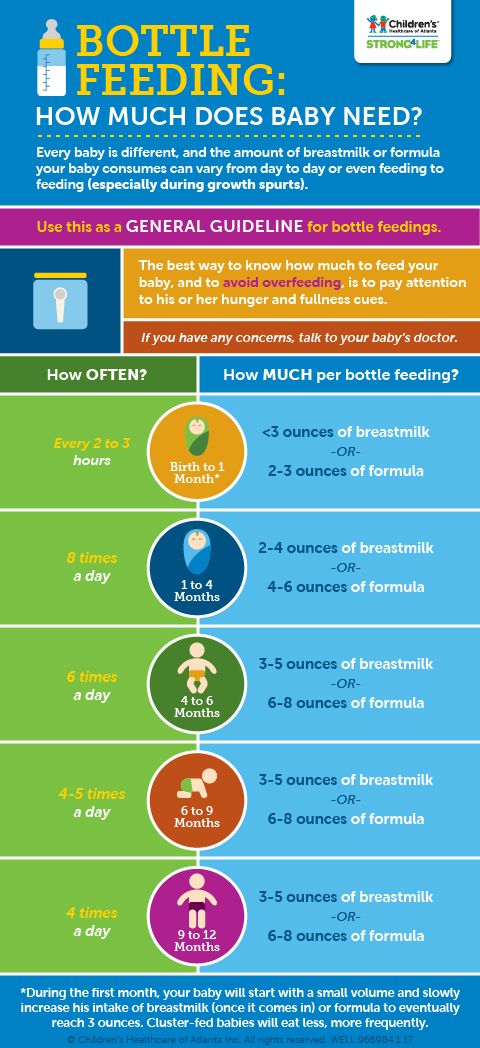
Make a note of how your baby is digesting their new diet, and seek the advice of your pediatrician if you have any concerns.
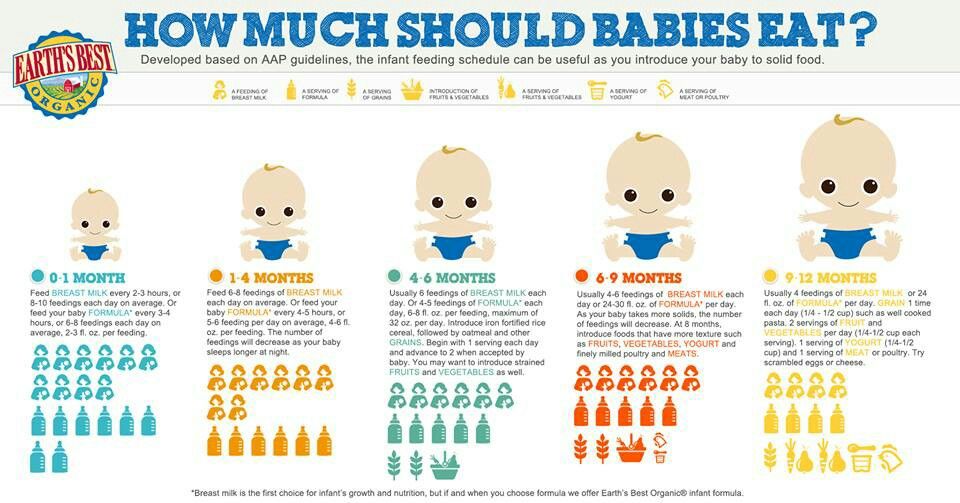
4 Tips to help ease your baby into combo feeding
If you’ve decided to start combo feeding, these helpful tips will make the transition easier for mom and baby alike.
1. Create similarities in the feedings
Give your baby as much of a similar experience as possible. This will give them a more familiar routine that they can look forward to, and it can help eliminate any nipple confusion they may experience.
Pro tip: When formula feeding, give your baby skin-to-skin contact and switch them from side to side to give the illusion of breastfeeding. This can help make the transition much easier for both you and your baby.
2. Space out formula feedings
Since organic baby formula and breast milk are two separate mixtures, it’s best to introduce the formula slowly to better support your baby’s digestion. You can slide in a bottle of formula a couple of hours after the initial feeding session to get your infant used to the taste. This can make things much easier for you in the long run.
You can slide in a bottle of formula a couple of hours after the initial feeding session to get your infant used to the taste. This can make things much easier for you in the long run.
Our breast milk supply provides nutrients that can only be found wholly in our breast milk. But, thanks to modern science, there are similarly-composed baby formulas in the shopping aisle.
That being said, pay attention to which baby formulas have the quality ingredients and sourcing that you are looking for. If organic or non-gmo products are important to you, there are options. If you are looking for cow’s milk vs. a vegan formula, you can specifically look for that as well.
Talk to your pediatrician about vitamin D supplements—whether you’re breastfeeding or bottle-feeding—to ensure your baby is getting all of the nutrients they need.
Shop Bobbie Organic Infant Formula
Bobbie Organic Infant Formula is a USDA Organic, EU-style infant formula that meets all FDA requirements. It is a complete nutrition milk-based powder modeled after breast milk and is easy on tummies. It is non-GMO and doesn't have corn syrup, palm oil, or maltodextrin. Learn more about Bobbie.
It is a complete nutrition milk-based powder modeled after breast milk and is easy on tummies. It is non-GMO and doesn't have corn syrup, palm oil, or maltodextrin. Learn more about Bobbie.
Shop Bobbie
4. Look for the “Feeling Full” signal
Your baby will become well-versed in telling you when he’s no longer hungry. Trust and watch to make sure his weight-gain patterns are normal as he grows and develops, as this is an excellent sign of properly taking to a combination diet.
How does the transition from breast milk to baby formula affect mom?
The transition from breast milk can affect your body’s milk production in a few ways. Medical experts suggest making a clean switch if you feel comfortable doing so or doing so gradually if that works best for you.
To ensure a smooth transition, you can try these techniques to start:
A new feeding routine can disrupt your body’s milk production
Expert Tip: Try starting with one bottle of formula per day.
A new routine might throw your body off its game, and your body’s milk production system may not understand the transition right away. If you’re pumping multiple times per day and then instantly move to pump only once per day, your milk supply can drop pretty rapidly and may not be there if you really need it down the line.
Some parents like to start by replacing the night bottle with formula. This can help by allowing other people to participate in feeding as well, and it can become part of the regular nighttime feeding routine.
Your body may struggle to adjust to the new routine
Expert Tip: Build up the formula usage slowly, and don’t stop pumping right away.
Your body may not demonstrate that it can handle the new routine. It may even cause breast engorgement or blocked milk ducts. If you’re struggling with the switch, you may need to build up the formula usage gradually.
Additionally, it’s okay to pump even if the milk is not being used. It may even get rid of the heaviness you might feel if the breast milk isn’t released. You can store up the extra breast milk and extend the feeding journey using both breast milk and formula.
It may even get rid of the heaviness you might feel if the breast milk isn’t released. You can store up the extra breast milk and extend the feeding journey using both breast milk and formula.
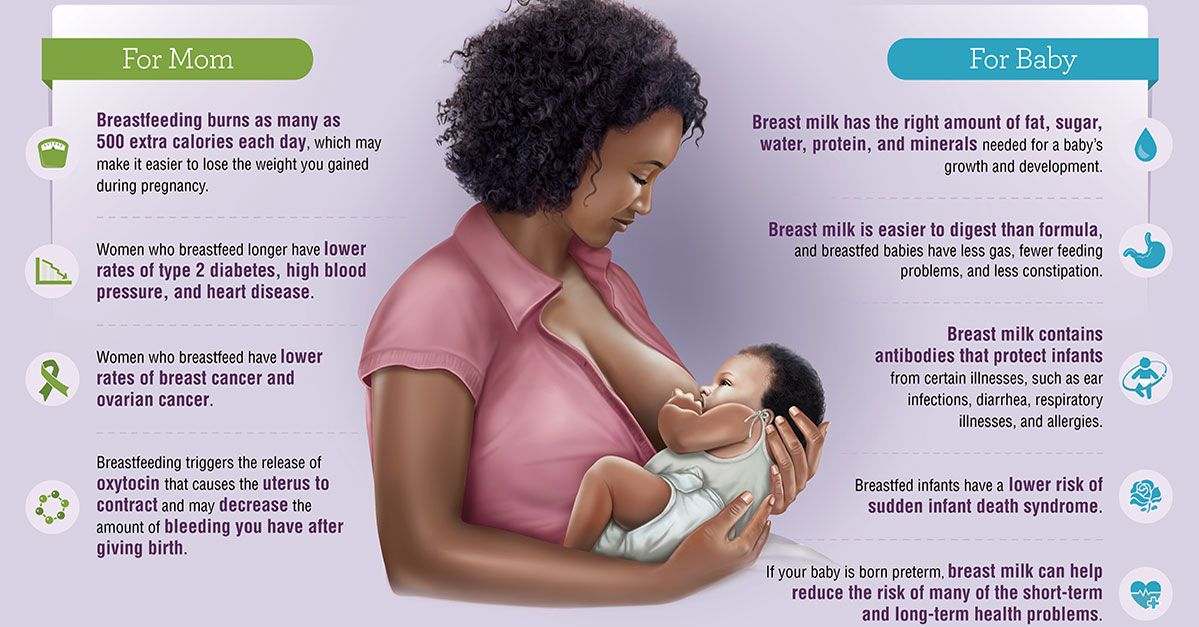
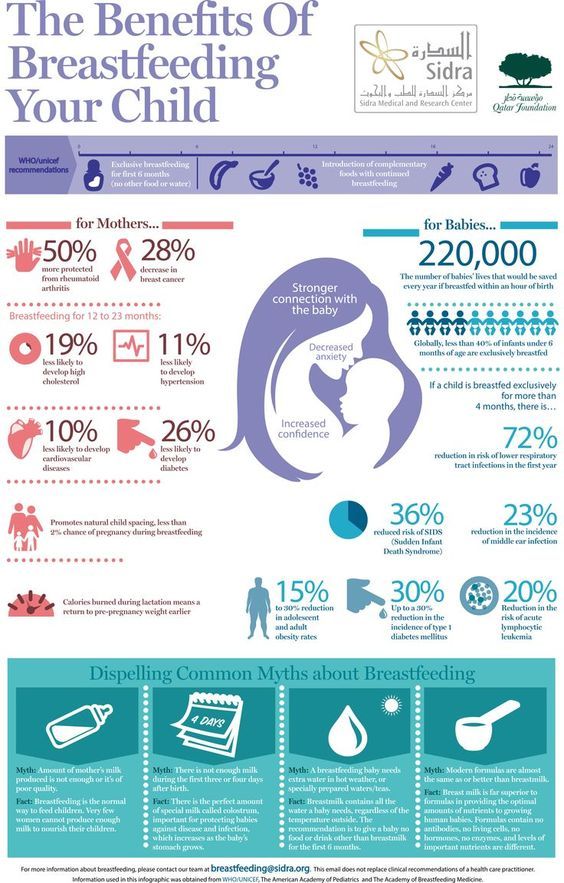
Benefits of breastfeeding for mom and baby
We don’t often talk about this, but breastfeeding delivers many benefits not only to your baby but also to you! The list of benefits to you and baby is long, here are a few key benefits worth mentioning:
- Babies may have a more well-supported immune system during childhood due to antibodies in breastmilk.
- Colostrum (found in breast milk) can support the baby’s digestive system to help with growth and proper functioning.
- Breast milk adapts as your baby grows.
- Even partial breastfeeding may promote quicker recovery after giving birth.
- Breastfeeding saves money.
- Breastfeeding may help lower the risk of certain diseases like ovarian cancer, breast cancer, and diabetes.
Why parents choose formula feeding
With all of life’s twists and turns, there are many reasons parents may formula feed from day one or choose to exclusively breastfeed before making the add or switch to baby formula. As with breastfeeding, there are amazing benefits for both you and your child when it comes to using baby formula:
As with breastfeeding, there are amazing benefits for both you and your child when it comes to using baby formula:
- Formula feeding is very convenient; babies can be fed any time they express hunger cues.
- Availability of the exact amount of milk needed means pumping doesn’t need space on your personal schedule.
- Allows teamwork–your partner and other caretakers have the ability to help feed if needed.
- Allows you the ability to schedule feedings, especially with low milk supply not being a concern.
- Allows you to be less worried about your diet, including the revived ability to consume alcohol.
Sometimes, the choice to nurse versus formula feed is truly out of your control. If a baby isn’t reacting well to your breastmilk, there could be a deficiency or even an allergy that needs to be addressed. It could also be related to how the baby’s body reacts to different ingredients or products.
It’s important to remember that there’s no reason to feel pressure that your breastfeeding journey didn’t go as planned. Adding formula, otherwise known as supplementing, to your breastfeeding routine is very common.
Adding formula, otherwise known as supplementing, to your breastfeeding routine is very common.
A doctor may recommend formula supplementation if:
- A newborn loses a percentage of their body weight during the first few days of life.
- A newborn gains significant weight after the first few days of birth.
- A baby becomes dehydrated and demonstrates this through fewer wet diapers.
- A baby appears dissatisfied after feeding and, therefore may need more nutrition.
Ghere also shared that, “Supplementing may start as early as the first few days of life if the baby has lost too much weight and/or mom’s milk supply hasn’t been established. Other moms begin around 3-4 weeks to get the baby used to some bottle feeding, to allow others to feed the baby, or if mom has to return to work.”
She even goes on to say that supplementation can support the mother’s health as well: “The truth is, supplementing happens whenever mom doesn’t have enough milk, the baby needs more than mom can supply, or someone other than mom is feeding the baby.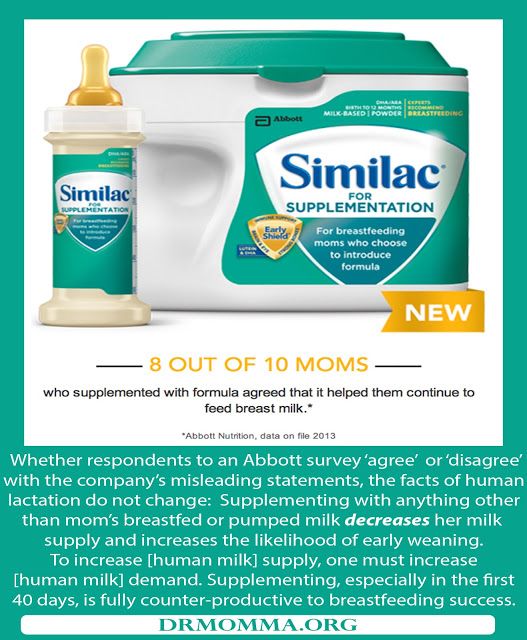 It’s not an all-or-nothing choice. New parents need options and the flexibility to meet both the baby’s and mom’s needs.”
It’s not an all-or-nothing choice. New parents need options and the flexibility to meet both the baby’s and mom’s needs.”
The decision or recommendation to supplement is always for the good of both parties, and no one would want it any other way!
Our take on combo feeding
So, is it ok to breast feed and formula feed a baby simultaneously?
After looking at both options and weighing the benefits of each, there really is no wrong decision when it comes to formula feeding versus breastfeeding. It is a personal choice, unique to each situation.
If you choose to breastfeed, formula feed, or both, this is perfectly fine unless otherwise directed by your pediatrician–we can’t stress enough that your pediatrician is the true expert to your specific journey with your little one! Remember, no two families’ journeys are the same!
Shop Bobbie Organic Infant Formula
Bobbie Organic Infant Formula is a USDA Organic, EU-style infant formula that meets all FDA requirements. It is a complete nutrition milk-based powder modeled after breast milk and is easy on tummies. It is non-GMO and doesn't have corn syrup, palm oil, or maltodextrin. Learn more about Bobbie.
It is a complete nutrition milk-based powder modeled after breast milk and is easy on tummies. It is non-GMO and doesn't have corn syrup, palm oil, or maltodextrin. Learn more about Bobbie.
Shop Bobbie
Sources:
What Is Colostrum? Nutrition, Benefits, and Downsides | Healthline
Combining Breastfeeding and Formula Feeding | VeryWell Family
Supplementing With Formula: Combining Breastfeeding and Bottles | What to Expect
The content on this site is for informational purposes only and not intended to be a substitute for professional medical advice, diagnosis or treatment. Discuss any health or feeding concerns with your infant's pediatrician. Never disregard professional medical advice or delay it based on the content on this page.
Combining breastfeeding and artificial feeding
Submitted by Elena Manchenko on Thu, 11/11/2021 - 10:47
Breastfeeding has many benefits for both you and your baby. However, there are situations when, in addition to milk, a child needs supplementary feeding with a mixture. For example, if the baby has health problems (due to premature birth or illness) or is not gaining weight well.
However, there are situations when, in addition to milk, a child needs supplementary feeding with a mixture. For example, if the baby has health problems (due to premature birth or illness) or is not gaining weight well.
If a baby cannot breastfeed due to illness, but is fed on your milk, he is still breastfed with all its benefits. nine0003
Talk to your doctor or nurse before giving formula to your baby. In some situations, it is necessary to weigh the child more often and monitor how he is gaining weight. This takes patience. If necessary, seek advice on inducing lactation, proper attachment of the baby to the breast, and choosing a comfortable position for feeding.
Supplementation with formula during breastfeeding is usually needed temporarily, for a short period. Many mothers, especially with their first child, worry about whether they are getting enough milk, especially if the baby cries shortly after eating or if the breasts feel empty. In fact, cases when a mother does not produce enough milk are rare. nine0003
In fact, cases when a mother does not produce enough milk are rare. nine0003
It is important to learn to understand whether the baby has eaten enough breast milk and to interpret its signals.
If your doctor recommends giving formula, ask them for advice on the following:
- How many times and how much to give formula
- How will you give formula (preferably from a cup)
- How long should you formula feed your baby
The color, smell and appearance of the baby's stool will change.
Breastfeeding risks associated with formula feeding:
- The baby will learn that bottled milk is easier than breastfeeding and may refuse to breastfeed.
- The breasts can become very enlarged and painful, which can lead to the cessation of milk production.
- The amount of milk may gradually decrease due to less consumption.
Causes and possible consequences of introducing formula while breastfeeding
- Some mothers do not feed their baby in the right mode (at first - from 10 to 12 feedings a day), cancel night feedings too early, and do not allocate enough time for breastfeeding.
- Bottles and nipples confuse the baby, so it is not recommended to use them during the first month or two.
- Use of nipple shields unnecessarily.
- Uncomfortable position or incorrect grip on the chest.
- Sometimes mother is tired, not self-confident, eats irregularly...
- And here comes the temptation... Impatient mothers fail to recognize the baby's signals and meet his needs, soon begin to give him formula from a bottle and go one step further from their original goal of breastfeeding.
How do I cancel the mixture?
If the reasons for introducing formula have been eliminated or you are determined to feed your baby only with your own milk:
- You can phase out the formula. nine0027 To stimulate lactation, let the baby suckle as much as he wants - in this way he will free her from milk, and his production will increase.
- Gradually reduce the amount of formula by 10 ml per serving daily or skip one serving of formula.

Be patient and don't rush to add formula. Remember that some babies compensate for physiological weight loss only after two weeks, and milk production gradually increases in accordance with the needs of the child. If formula is needed, it should be given in the smallest amount to meet the baby's needs and for as short a time as possible. Supplementing with formula unnecessarily can lead to failure in breastfeeding. nine0003
Don't let anyone tell you that formula is just as good for your baby as breast milk!
Australian Article
On
Cover Image
Image
© UNICEF Serbia/Pancic
Keywords
supplementation
Breast feed
infant formula
Category
Nutrition
Child Age
Month 1
Month 2 9002 9002 Month 3 9002
0035-6 months
7–9 months
10–12 months
Child Gender
Both
Parent Gender
Geneeric Content
License Content Content Content Content Content Content Content Content Content 9000 OFF 9000 OFF 9000 OFF
Off
Mandatory Content
Off
Breast milk and formula: what do they have in common?
1 Cribb VL et al.
Contribution of inappropriate complementary foods to the salt intake of 8-month-old infants. EUR J Clin Nutr . 2012;66(1):104. - Cribb V.L. et al., "Effects of inappropriate complementary foods on salt intake in 8-month-old infants". Yur J Klin Nutr. 2012;66(1):104.
2 Lönnerdal B. Nutritional and physiologic significance of human milk proteins. Am J Clin Nutr . 2003;77(6):1537 S -1543 S - Lönnerdahl B., "Biologically active proteins of breast milk". F Pediatrician Child Health. 2013;49 Suppl 1:1-7.
3 Savino F et al. Breast milk hormones and their protective effect on obesity. Int J Pediatric Endocrinol. 2009;2009:327505. - Savino F. et al., "What role do breast milk hormones play in protecting against obesity.
" Int J Pediatrician Endocrinol. 2009;2009:327505.
4 Hassiotou F, Hartmann PE. At the Dawn of a New Discovery: The Potential of Breast Milk Stem Cells. Adv Nutr . 2014;5(6):770-778. - Hassiot F, Hartmann PI, "On the threshold of a new discovery: the potential of breast milk stem cells." Adv. 2014;5(6):770-778.
5 Hassiotou F et al. Maternal and infant infections stimulate a rapid leukocyte response in breastmilk. Clinic Transl Immunology . - Hassiot F. et al., "Infectious diseases of the mother and child stimulate a rapid leukocyte reaction in breast milk." Clean Transl Immunology. 2013;2(4):e3.
6 Pannaraj PS et al. Association Between Breast Milk Bacterial Communities and Establishment and Development of the Infant Gut Microbiome. JAMA Pediatr. 2017;171(7):647-654. - Pannaraj P.
S. et al., "Bacterial communities in breast milk and their association with the emergence and development of the neonatal gut microbiome". nine0013 JAMA pediatric. 2017;171(7):647-654.
7 Bode L. Human milk oligosaccharides: every baby needs a sugar mama.Glycobiology. 2012;22(9):1147-1162. - Bode L., "Oligosaccharides in breast milk: a sweet mother for every baby." Glycobiology (Glycobiology). 2012;22(9):1147-1162.
8 Deoni SC et al. Breastfeeding and early white matter development: A cross-sectional study. neuroimage. nine0013 2013;82:77-86. - Deoni S.S. et al., Breastfeeding and early white matter development: a cross-sectional study. Neuroimage. 2013;82:77-86.
9 Birch E et al. Breast-feeding and optimal visual development. J Pediatr Ophthalmol Strabismus. 1993;30(1):33-38. - Birch, I. et al., "Breastfeeding and Optimum Vision Development." J Pediatrician Ophthalmol Strabismus.
1993;30(1):33-38.
10 Sánchez CL et al. The possible role of human milk nucleotides as sleep inducers. Nutr Neurosci . 2009;12(1):2-8. - Sanchez S.L. et al., "Nucleotides in breast milk may help the baby fall asleep." Nutr Neurosai. 2009;12(1):2-8.
11 Moukarzel S, Bode L. Human Milk Oligosaccharides and the Preterm Infant: A Journey in Sickness and in Health. Clin Perinatol. 2017;44(1):193-207. - Mukarzel S., Bode L., "Breast milk oligosaccharides and the full-term baby: a path to illness and health." Klin Perinatol (Clinical perinatology). 2017;44(1):193-207.
12 Beck KL et al. Comparative Proteomics of Human and Macaque Milk Reveals Species-Specific Nutrition during Postnatal Development. J Proteome Res . 2015;14(5):2143-2157. - Beck K.L. et al., "Comparative proteomics of human and macaque milk demonstrates species-specific nutrition during postnatal development.
" nine0013 G Proteome Res. 2015;14(5):2143-2157.
13 Michaelsen KF, Greer FR. Protein needs early in life and long-term health. Am J Clin Nutr . 2014;99(3):718 S -722 S . - Mikaelsen KF, Greer FR, Protein requirements early in life and long-term health. Am J Clean Nutr. 2014;99(3):718S-722S.
14 Howie PW et al. Positive effect of breastfeeding against infection. BMJ .1990;300(6716):11-16. — Howie PW, "Breastfeeding as a defense against infectious diseases." BMJ. 1990;300(6716):11-16.
15 Duijts L et al. Prolonged and exclusive breastfeeding reduces the risk of infectious diseases in infancy. Pediatrics , 2010;126(1): e 18-25. - Duitz L. et al., "Prolonged exclusive breastfeeding reduces the risk of infectious diseases in the first year of life.
" nine0013 Pediatrix (Pediatrics). 2010;126(1):e18-25.
16 Ladomenou F et al. Protective effect of exclusive breastfeeding against infections during infancy: a prospective study. Arch Dis Child . 2010;95(12):1004-1008. - Ladomenu, F. et al., "The effect of exclusive breastfeeding on infection protection in infancy: a prospective study." Arch Dis Child.2010;95(12):1004-1008.
17 Vennemann MM et al. Does breastfeeding reduce the risk of sudden infant death syndrome?. Pediatrics . 2009;123(3): e 406- e 410. - Wennemann M.M. et al., "Does Breastfeeding Reduce the Risk of Sudden Infant Death?" Pediatrix (Pediatrics). 2009;123(3):e406-e410.
18 Straub N et al. Economic impact of breast-feeding-associated improvements of childhood cognitive development, based on data from the ALSPAC.
Br J Nutr . 2016;1-6. - Straub N. et al., "Economic Impact of Breastfeeding-Associated Child Cognitive Development (ALSPAC)". Br J Nutr . 2016;1-6.
19 Heikkilä K et al. Breast feeding and child behavior in the Millennium Cohort Study. Arch Dis Child . 2011;96(7):635-642 - Heikkila K. et al., Breastfeeding and Child Behavior in a Millennial Cohort Study. Arch Dis Child. 2011;96(7):635-642.
20 Singhal A et al. Infant nutrition and stereoacuity at age 4–6 y. Am J Clin Nutr , 2007;85(1):152-159. - Singhal A. et al., Nutrition in infancy and stereoscopic visual acuity at 4-6 years of age. nine0013 Am F Clean Nutr. 2007;85(1):152-159.
21 Peres KG et al. Effect of breastfeeding on malocclusions: a systematic review and meta - analysis.
Acta Paediatr . 2015;104(467):54-61. - Perez K.G. et al., "The impact of breastfeeding on malocclusion: a systematic review and meta-analysis". Akta Pediatr. 2015;104(S467):54-61.
22 Horta B et al. nine0013 Long - term consequences of breastfeeding on cholesterol, obesity, systolic blood pressure and type 2 diabetes: a systematic review and meta - analysis. Acta Paediatr . 2015;104(467):30-37. - Horta B.L. et al., "Long-term effects of breastfeeding and their impact on cholesterol, obesity, systolic blood pressure, and type 2 diabetes: a systematic review and meta-analysis." Akta Pediatr. 2015;104(S467):30-37.
23 Lund-Blix NA. Infant feeding in relation to islet autoimmunity and type 1 diabetes in genetically susceptible children: the MIDIA Study. Diabetes Care . 2015;38(2):257-263.
- Lund-Blix N.A. et al., "Breastfeeding in the context of isolated autoimmunity and type 1 diabetes in genetically predisposed children: a study MIDIA ". Diabitis Care. 2015;38(2):257-263.
24 Amitay EL, Keinan-Boker L. Breastfeeding and Childhood Leukemia Incidence: A Meta-analysis and Systematic Review0. JAMA 90 Pediatr 2015;169(6): e 151025. - Amitai I.L., Keinan-Boker L., "Breastfeeding and incidence of childhood leukemia: a meta-analysis and systematic review". JAMA Pediatrics 2015;169(6):e151025.
25 Bener A et al. Does continued breastfeeding reduce the risk for childhood leukemia and lymphomas? Minerva Pediatr. 2008;60(2):155-161. - Bener A. et al., "Does long-term breastfeeding reduce the risk of leukemia and lymphoma in a child?". Minerva Pediatrician. 2008;60(2):155-161.
26 Dewey KG. Energy and protein requirements during lactation.
Annu Rev Nutr . 1997;17:19-36. - Dewey K. J., "Energy and Protein Requirements During Lactation". Anna Rev Nutr. 1997 Jul;17(1):19-36.
27 Victoria CG et al. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet. 2016;387(10017):475-490. - Victor S.J. et al., "Breastfeeding in the 21st century: epidemiology, mechanisms and long-term effects". Lancet (Lancet). 2016;387(10017):475-490.
28 Jordan SJ et al. Breastfeeding and Endometrial Cancer Risk: An Analysis From the Epidemiology of Endometrial Cancer Consortium. Obstet Gynecol . 2017;129(6):1059-1067. — Jordan S.J. et al., "Breastfeeding and the risk of endometrial cancer: an analysis of epidemiological data from the Endometrial Cancer Consortium". Obstet Ginecol (Obstetrics and Gynecology). 2017;129(6):1059-1067.
29 Li DP et al. Breastfeeding and ovarian cancer risk: a systematic review and meta-analysis of 40 epidemiological studies. Asian Pac J Cancer Prev . 2014;15(12):4829-4837. - Lee D.P. et al., "Breastfeeding and the risk of ovarian cancer: a systematic review and meta-analysis of 40 epidemiological studies." Asia Pas W Cancer Prev. 2014;15(12):4829-4837.
30 Peters SAE et al. Breastfeeding and the Risk of Maternal Cardiovascular Disease: A Prospective Study of 300,000 Chinese Women. J Am Heart Assoc . 2017;6(6). - Peters S.A. et al., "Breastfeeding and Maternal Risk of Cardiovascular Disease: A Prospective Study of 300,000 Chinese Women". J Am Hart Assoc. 2017;6(6):e006081. nine0013
31 U.S. Department of Health & Human Services [Internet].
Surgeon General Breastfeeding factsheet ; 2011 Jan 20 - Department of Health and Human Services [Internet], Breastfeeding Facts from the Chief Medical Officer, 20 January 2011 [cited 4 April 2018]
32 Doan T et al. nine0013 Breast-feeding increases sleep duration of new parents. J Perinat Neonatal Nurs . 2007;21(3):200-206. - Dawn T. et al., "Breastfeeding increases parental sleep duration." G Perinat Neonatal Nurs. 2007;21(3):200-206.
33 Menella JA et al. Prenatal and postnatal flavor learning by human infants. Pediatrics . 2001;107(6): E 88. - Menella J.A. et al., Prenatal and Postnatal Taste and Smell Recognition in Children. Pediatrix (Pediatrics). 2001;107(6):e88.
34 Forestell CA, Mennella JA. Early determinants of fruit and vegetable acceptance.